ABSTRACT
Type 2 diabetes (T2D) is an independent risk factor for acute ischemic stroke (AIS), but the underlying mechanisms remain elusive. Because the gut microbiota plays a causal role in both T2D and AIS, we wondered whether gut dysbiosis in T2D aggravates stroke progression. We recruited 35 T2D, 90 AIS, 60 AIS with T2D (AIS_T2D) patients, and 55 healthy controls and found that AIS and T2D had an additive effect on AIS_T2D patient gut dysbiosis by exhibiting the largest difference from the heathy controls. In addition, we found that the degree of gut dysbiosis associated with T2D was positively correlated with the National Institutes of Health Stroke Scale (NIHSS), modified Rankin score (mRS), and Essen stroke risk score in patients with AIS, including AIS and AIS_T2D patients. Compared with mice colonized with gut microbiota from healthy controls poststroke modeling, germfree (GF) mice colonized with gut microbiota from T2D patients showed exacerbated cerebral injury and impaired gut barrier function. Specifically, exacerbated brain injury and gut barrier dysfunction in T2D-treated GF mice were significantly associated with a reduction in short-chain fatty acid (SCFA)-producing bacteria. Our study showed that T2D and AIS have an additive effect on AIS_T2D patient gut microbiota dysbiosis. T2D-associated gut microbiota dysbiosis is associated with stroke severity in AIS patients and aggravates stroke progression in mice.
IMPORTANCE We demonstrated an additive effect of type 2 diabetes (T2D) and acute ischemic stroke (AIS) on AIS with T2D (AIS_T2D) patient gut microbiota dysbiosis, and gut dysbiosis associated with T2D was positively correlated with stroke severity in AIS patients. Through animal experiments, we found that cerebral injury was exacerbated by fecal microbiota transplantation from T2D patients compared with that from healthy controls, which was associated with a reduction in short-chain fatty acid (SCFA)-producing bacteria. This study provided a novel view that links T2D and AIS through gut microbial dysbiosis.
KEYWORDS: gut microbiota, acute ischemic stroke, type 2 diabetes
INTRODUCTION
Stroke is one of the most common causes of death and disability worldwide and is the leading cause of death and disability-adjusted life-years in China (1, 2). Among many modifiable risk factors, type 2 diabetes mellitus (T2D) is an independent risk factor for the progression of ischemic stroke (3). Individuals with T2D have a 1.5 to 3 times higher risk of stroke than nondiabetic individuals (4), and diabetic patients experience more adverse events and subsequent mortality after stroke (5). According to a study in the United Kingdom, the hazard ratio for ischemic stroke in diabetic individuals is 2.3 (95% CI 2.0 to 2.7) compared with that in nondiabetic individuals (6).
For metabolic disorders such as T2D and cardio-cerebrovascular diseases such as stroke, there is a newly identified common risk factor, the gut microbiome (7, 8). Studies of people from different ethnicities have found that individuals with T2D showed reduced butyrate-producing bacteria leading to gut inflammation (9). A preclinical trial study confirmed that microbiota transplantation from lean donors improved insulin sensitivity in male recipients with metabolic syndrome, suggesting a causal connection between T2D and gut microbiota (10, 11). In addition, gut microbiota and its metabolites are also associated with stroke, i.e., ischemic stroke causes gut microbiota dysbiosis, and such dysbiosis may exacerbate brain infarction poststroke (8, 12). The microbiome-derived metabolite trimethylamine-N-oxide contributes to the progression of atherosclerosis (13, 14).
Because T2D is an independent risk factor for stroke, it is very intriguing to explore the role of the gut microbiome in this correlation. Here, we hypothesized that T2D aggravates stroke progression by inducing gut microbiota dysbiosis. We compared the similarities and differences in the gut microbiome in acute ischemic stroke (AIS) patients, T2D patients, and AIS patients complicated with T2D (AIS_T2D). In addition, we evaluated the role of gut microbiota dysbiosis associated with T2D in aggravating stroke progression.
RESULTS
AIS and T2D had an additive effect on gut microbiota dysbiosis in AIS_T2D patients.
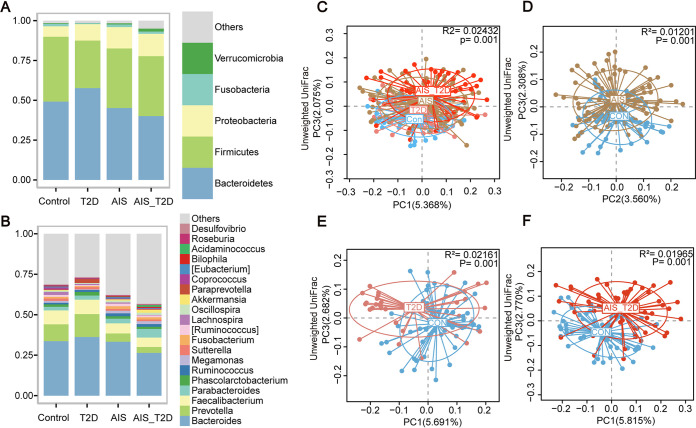
Our study recruited 90 AIS patients, 60 AIS_T2D patients, 35 T2D patients, and 55 healthy controls. The characteristics of the study participants are included in Table 1. For all individuals involved in the present study, most of their gut bacteria fell into the phyla Bacteroidetes, Firmicutes, Proteobacteria, and Fusobacteria, and at the genus level, Bacteroides, Prevotella, Faecalibacterium, and Parabacteroides occupied the highest abundance (Fig. 1A and B).
TABLE 1.
Characteristics of the healthy controls, AIS patients, T2D patients, and AIS_T2D patientsa
| Value for: |
||||
|---|---|---|---|---|
| Parameter | Healthy controls | AIS patients | T2D patients | AIS_T2D patients |
| No. | 55 | 90 | 35 | 60 |
| Age | 61 (4) | 61 (18) | 65 (11) | 63 (16) |
| Sex, M | 0.5636 | 0.6556 | 0.6571 | 0.6500 |
| BMI, kg/m2 | 23.00 (5.00) | 23.66 (3.94) | 24.00 (3.00)* | 23.87 (2.88) |
| WBC, 109/L | 5.86 (1.79) | 7.49 (3.15)*** | 7.04 (2.67)* | 8.22 (4.16)*** |
| LYM, 109/L | 2.01 (0.83) | 1.83 (0.69) | 1.90 (0.63) | 2.02 (0.92) |
| NEU, 109/L | 3.18 (1.11) | 4.65 (2.59)*** | 3.38 (2.08) | 5.13 (3.33)*** |
| MONO, 109/L | 0.33 (0.11) | 0.47 (0.19)*** | 0.35 (0.24) | 0.47 (0.20)*** |
| RBC, 1012/L | 4.71 (0.59) | 4.78 (0.74) | 5.09 (0.92)* | 4.91 (0.79) |
| HGB, g/L | 143.00 (23.00) | 140.00 (18.25) | 147.00 (28.00) | 141.50 (27.50) |
| PLT, 109/L | 234 (86) | 228.50 (73.50) | 196 (68)* | 217 (93.00) |
| GLU, mmol/L | 4.84 (0.71) | 5.05 (1.32) | 6.81 (3.24)*** | 8.60 (3.96)*** |
| BUN, mmol/L | 4.90 (1.77) | 5.00 (2.41) | 5.41 (1.55) | 5.48 (1.80) |
| Cr, μmol/L | 66 (18) | 79.00 (28.00)*** | 69 (18.25) | 73 (40.75) |
| UA, μmol/L | 333 (100) | 368 (112.00) | 350 (102) | 346 (130.25) |
| TP, g/L | 68.90 (5.20) | 64.30 (7.00)*** | 71.90 (4.20)** | 65.90 (7.75)** |
| ALB, g/L | 42.30 (3.80) | 38.35 (5.25)*** | 42.10 (1.60) | 39.30 (5.25)*** |
| GLB, g/L | 26.40 (5.00) | 25.70 (5.07) | 29.80 (2.10)** | 26.30 (4.70) |
| SBP, mmHg | 124 (18) | 142 (25)*** | 132 (33)* | 143 (36)*** |
| DBP, mmHg | 72 (15) | 84 (21)*** | 73 (20) | 82 (14)*** |
| TC, mmol/L | 4.94 (0.82) | 4.53 (1.750) | 4.99 (1.88) | 4.78 (1.415) |
| LDL, mmol/L | 3.05 (0.66) | 2.91 (1.33) | 2.98 (1.59) | 3.11 (1.150) |
| HDL, mmol/L | 1.23 (0.34) | 0.95 (0.320)*** | 1.18 (0.27) | 0.91 (0.305)*** |
| VLDL, mmol/L | 0.58 (0.28) | 0.62 (0.415) | 0.66 (0.45) | 0.70 (0.495)** |
| TG, mmol/L | 1.06 (0.59) | 1.22 (0.840)** | 1.26 (0.71)* | 1.84 (1.025)*** |
For all records except number and gender, data represent the median (interquartile range). For all records except gender, the P values represent the results of the Wilcoxon rank sum test. The P value of gender represents the result of Pearson’s chi-square test. BMI, body mass index; WBC, white blood cell count; LYM, lymphocytes; NEU, neutrophils; MONO, monocytes; RBC, red blood cells; HGB, hemoglobin; PLT, platelets; GLU, glucose; BUN, blood urea nitrogen; Cr, creatinine; UA, uric acid; TP, total protein; ALB, albumin; GLB, globulin; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; LDL, low-density lipoprotein; HDL, high-density lipoprotein; VLDL, very low-density lipoprotein; TG, triglycerides. *, P < 0.05; **, P < 0.01; ***, P < 0.001 versus healthy controls.
FIG 1.
Gut microbiota composition among the AIS (n = 86), T2D (n = 35), AIS_T2D (n = 59), and control groups (n = 55). Average relative abundances of the predominant bacterial taxa at the phylum (A) and genus (B) levels. The overall PCoA showing the gut microbial composition pattern of the AIS, T2D, AIS_T2D, and control groups (C). Obvious dysbiosis of the gut microbiome in unweighted UniFrac-based PCoA plots of AIS patients (D), T2D patients (E), and AIS_T2D patients (F) compared with the control group. AIS, acute ischemic stroke; PCoA, principal coordinate analysis.
Specifically, compared with healthy controls, AIS patients and T2D patients exhibited similar differences in gut microbial alteration patterns. Principal coordinate analysis (PCoA) based on unweighted UniFrac distance showed that the spatial distributions of both AIS patients and T2D patients were significantly different from those of healthy controls (Fig. 1C to E). Linear discriminant analysis effect size (LEfSe) analysis revealed that AIS patients showed an increased abundance of Proteobacteria, Gammaproteobacteria, Enterobacteriaceae, Deltaproteobacteria, and Desulfovibrionaceae. In contrast, Prevotella, Faecalibacterium, Lachnospira, and Coprococcus were decreased in AIS patients (Fig. S1A). Compared with healthy controls, Enterobacteriaceae, Lactobacillales, Lactobacillaceae, and Lactobacillus were significantly enriched, while Lachnospira was decreased in T2D patients (Fig. S1B). Furthermore, AIS_T2D patients showed a clear separation from healthy controls in PCoA (Fig. 1F). Compared with those in healthy controls, Enterobacteriaceae and Desulfovibrionaceae were significantly enriched, while Bacteroides, Faecalibacterium, Lachnospira, and Coprococcus were significantly depleted in AIS_T2D patients (Fig. S1C). Together, AIS and T2D have an additive effect on gut microbiota dysbiosis in AIS_T2D patients.
LEfSe analysis showed obvious dysbiosis of the gut microbiome of AIS patients (A), T2D patients (B), and AIS_T2D patients (C) compared with the control group. AIS, acute ischemic stroke; LEfSe, linear discriminant analysis effect size. Download FIG S1, TIF file, 17.6 MB (17.6MB, tif) .
Copyright © 2021 Chen et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
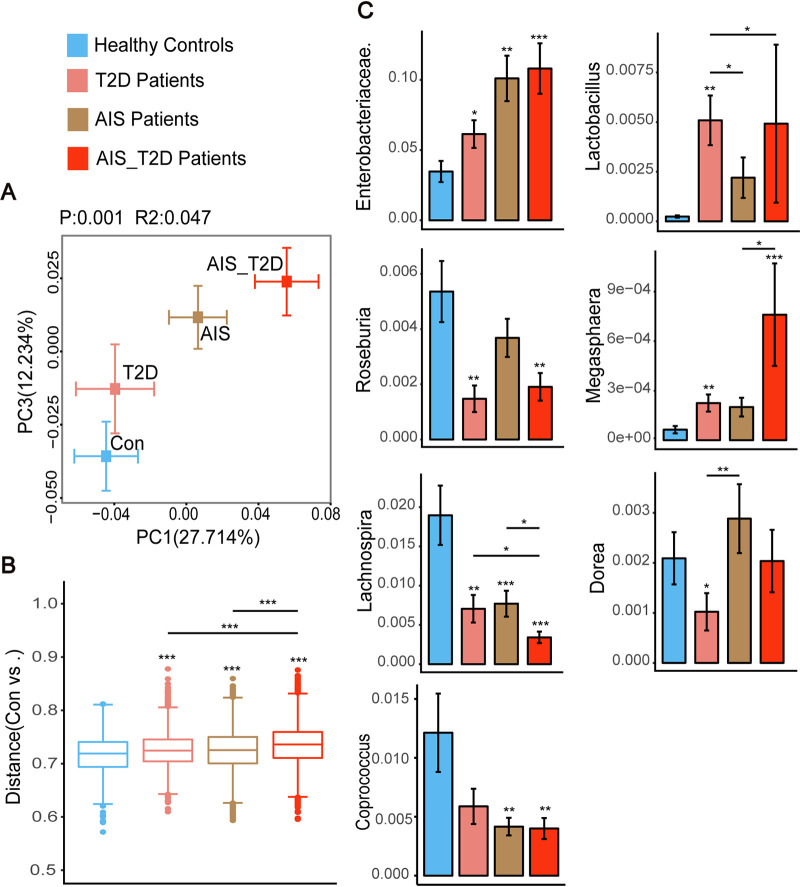
The gut microbiota configurations of AIS or T2D patients exhibited alterations in the same direction as healthy controls, while AIS_T2D patients showed a greater distance from healthy controls than the AIS and T2D groups did in the same direction, according to ordination analysis (Fig. 1C and Fig. 2A). The unweighted UniFrac distance revealed that AIS_T2D patients exhibited a significantly greater distance than both AIS patients and T2D patients (Fig. 2B). To further explore the gut microbial alteration patterns among AIS, T2D, and AIS_T2D patients, we further analyzed the abundance of selected bacteria according to LEfSe analysis and found similar microbial alteration patterns among the three patient groups. AIS_T2D patients showed the highest abundance of Enterobacteriaceae, Lactobacillus, and Megasphaera and the lowest abundance of Lachnospira and Coprococcus (Fig. 2C). T2D patients and AIS_T2D patients both exhibited a lower abundance of Roseburia than healthy controls. T2D patients exhibited the lowest abundance of Dorea among the four groups of people.
FIG 2.
AIS and T2D had an additive effect on the gut microbiota composition of AIS_T2D patients. (A) Different microbial patterns were exhibited in the PCoA based on weighted UniFrac distances. (B) Box plot illustrating the unweighted UniFrac distances of different patient groups to controls. (C) The relative abundance of selected bacteria using the Wilcoxon rank sum test. *, P < 0.05; **, P < 0.01; and ***, P < 0.001 based on the Wilcoxon rank sum test. AIS, acute ischemic stroke; PCoA, principal coordinate analysis.
The T2D gut microbial dysbiosis index was significantly positively correlated with the severity and prognosis of patients with AIS.
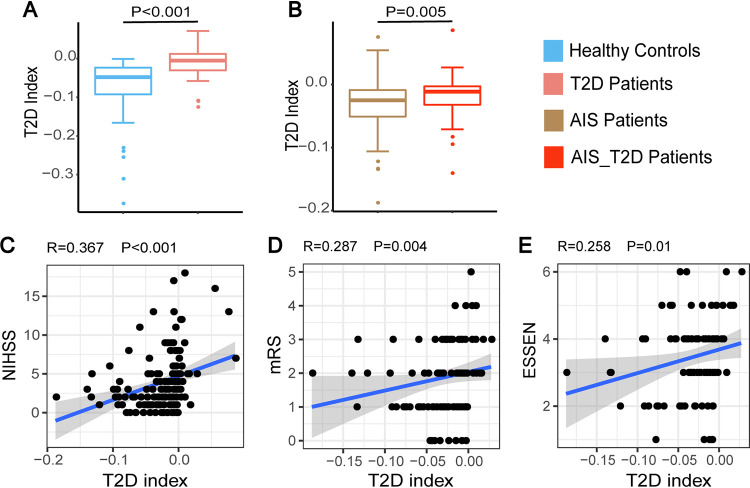
To further explore this additive effect on the gut microbiota, we established a gut microbial index to represent the overall gut dysbiosis associated with T2D. This index was formulated by the accumulated abundance of positively and negatively T2D-associated operational taxonomic units (OTUs) valued by their significance. We found that this index could reliably reflect gut dysbiosis in T2D with significantly higher indices in T2D patients than in healthy controls (Fig. 3A). This index also reflected gut dysbiosis in AIS_T2D patients with significantly higher indices than in AIS patients (Fig. 3B).
FIG 3.
The T2D gut microbial index was significantly associated with the severity and prognosis of patients with AIS. (A–B) The T2D gut microbial index significantly distinguished between T2D patients and healthy controls (A) and between AIS_T2D patients and AIS patients (B). (C–E) The T2D gut microbial index was significantly positively correlated with the NIHSS score (C), Essen stroke risk score (D), and mRS score (E) in patients with AIS. AIS, acute ischemic stroke; NIHSS, National Institutes of Health Stroke Scale; mRS, modified Rankin score.
To explore whether this T2D gut microbial index was correlated with the severity and prognosis of patients with AIS, including AIS and AIS_T2D patients, we conducted Spearman correlation analysis between the T2D index and the neurological function scores, including National Institutes of Health Stroke Scale (NIHSS) on admission and modified Rankin score (mRS) and Essen stroke risk scores at chronic stage. We found that the NIHSS score, mRS score, and Essen stroke risk score were significantly positively correlated with the T2D gut microbial index (Fig. 3C to E), indicating that gut dysbiosis evaluated by the T2D gut microbial index was associated with the severity and prognosis of stroke patients.
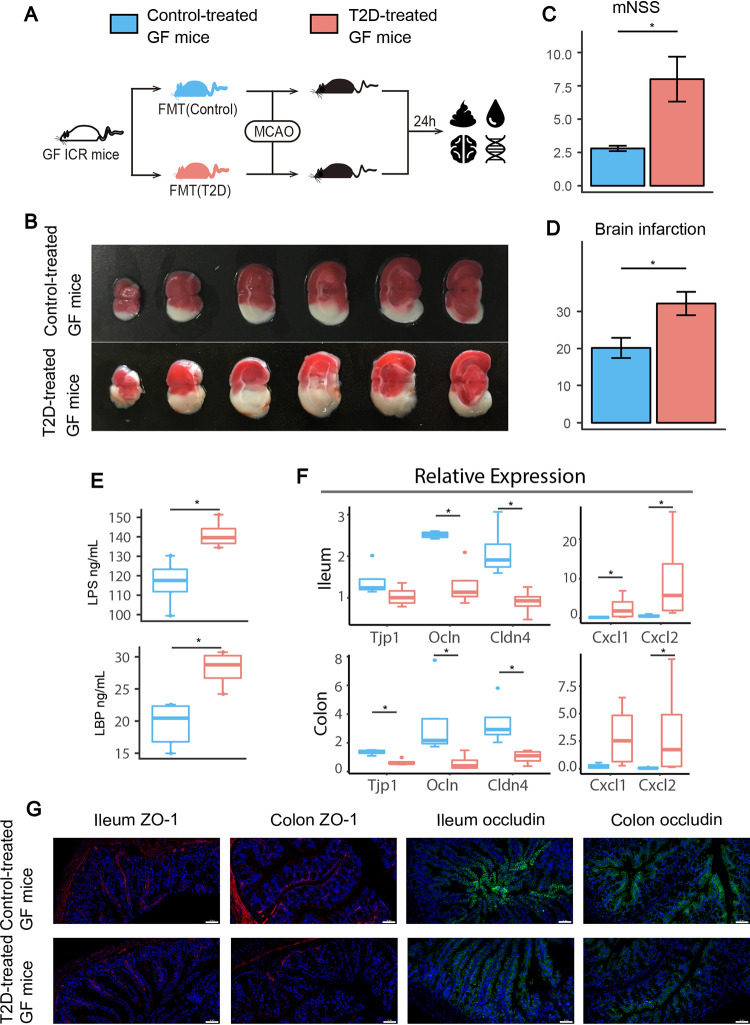
Transplantation of fecal samples from T2D patients exacerbated brain infarction poststroke.
To investigate whether gut dysbiosis associated with T2D contributes to brain injury or neurological deficits after stroke, we transplanted fecal samples from T2D patients and healthy controls to germfree (GF) mice and subsequently conducted middle cerebral artery occlusion (MCAO) (Fig. 4A). T2D-treated GF mice exhibited significantly larger brain infarction and a higher modified neurological severity score (mNSS) than the control group (Fig. 4B to D). In addition, gut microbiota associated with T2D impaired the gut barrier in GF mice. Serum lipopolysaccharide (LPS) and LPS-binding protein (LBP) levels were significantly increased in T2D-treated GF mice (Fig. 4E). Relative expression levels of tight junction proteins, including Tjp1, Ocln, and Cldn4, in the colon and Ocln and Cldn4 in the ileum were significantly decreased in T2D-treated GF mice (Fig. 4F). Immunofluorescence revealed that ZO-1 and occludin were abnormally distributed along the epithelial sheet, and the staining for both proteins was weaker and more disrupted in ileum and colon tissues in T2D-treated GF mice than in the control group (Fig. 4G). Furthermore, proinflammatory cytokines such as Cxcl1 and Cxcl2 were significantly increased in T2D-treated GF mice compared with those in the control group (Fig. 4F). Together, fecal microbiota transplantation (FMT) from T2D individuals exacerbated cerebral injury and impaired gut barrier function after stroke.
FIG 4.
T2D-treated GF mice exhibited exacerbated cerebral injury and gut barrier dysfunction. (A) Experimental design of FMT and MCAO surgery in GF mice. (B) Representative images of TTC-stained coronal brain sections. (C–D) Comparison of the brain infarction ratio and mNSS between GF mice transplanted with fecal samples from healthy controls (n = 5, blue) and T2D patients (n = 4, red). (E) Serum LBP and LPS levels in control and T2D-treated GF mice. (F) Relative expression of the Tjp1, Ocln, Cldn4, Cxcl1, and Cxcl2 genes and (G) immunofluorescent staining for occludin and ZO-1 (magnification, ×200) in mouse ileum and colon tissues. Scale bar 50 μm. *, P < 0.05 and **, P < 0.01 based on the Wilcoxon rank sum test. FMT, fecal microbiota transplantation; MCAO, middle cerebral artery occlusion; mNSS, modified neurological severity score.
Short-chain fatty acid (SCFA)-producing bacteria are significantly negatively associated with stroke progression in T2D-treated GF mice.
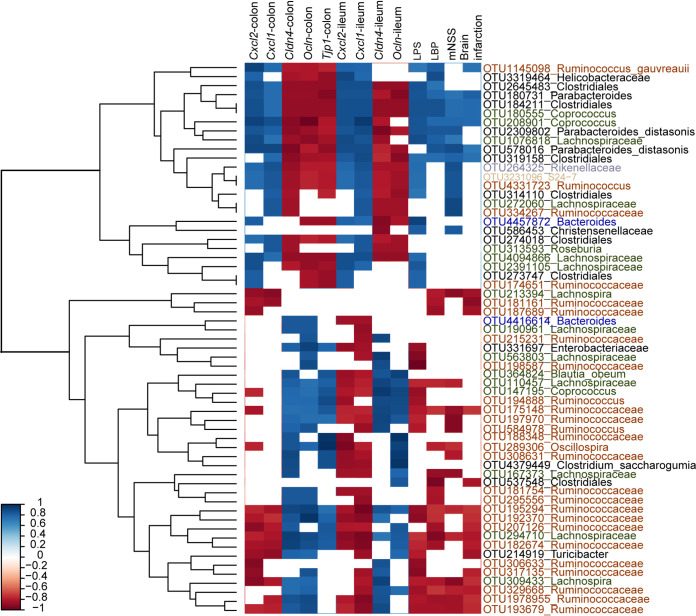
To explore which OTU was associated with brain injury poststroke in T2D-treated GF mice, correlation analysis was performed. As shown in Fig. 5, a total of 61 OTUs were significantly correlated with mouse outcome indices. Twenty-two OTUs, namely, two OTUs from Lachnospira, 13 OTUs from Ruminococcaceae, three OTUs from Lachnospiraceae, OTU584978 from Ruminococcus, OTU289306 from Oscillospira, OTU537538 from Clostridiales, and OTU214919 from Turicibacter, were significantly negatively correlated with exacerbated brain infarction, neurological deficits and gut barrier dysfunction in T2D-treated GF mice. In contrast, a total of 16 OTUs, namely, OTU1145098 from Ruminococcus gauvreauii, OTU180731 from Parabacteroides, three OTUs from Clostridiales, two OTUs from Coprococcus, two OTUs from Parabacteroides distasonis, two OTUs from Lachnospiraceae, OTU264325 from Rikenellaceae, OTU3231096 from S24-7, OTU4331723 from Ruminococcus, OTU334267 from Ruminococcaceae, and OTU586453 from Christensenellaceae, showed significantly positive correlations with brain injury and gut barrier dysfunction in T2D-treated GF mice. Two controversial OTUs in Bacteroides showed the difference. OTU4416614 was positively correlated with gut barrier dysfunction, and OTU4457872 showed the opposite correlation.
FIG 5.
Heatmap demonstrating the important OTUs and their correlation relationships with brain injury and gut barrier dysfunction in GF mice. A total of 61 OTUs were significantly correlated with the above indices. The boxes shown in red are negatively correlated, and the boxes in blue are positively correlated. The magnitude of the correlation is illustrated by the intensity of the color. OTUs, operational taxonomic units.
Based on the correlation results, OTUs that showed remarkable correlations with brain infarction, neurological deficits or gut barrier dysfunction were mainly from Ruminococcaceae, Lachnospira, and S24-7. Specifically, SCFA-producing bacteria, such as Ruminococcaceae and Lachnospira, showed a negative correlation with stroke progression and gut barrier dysfunction in T2D-treated GF mice (Table 2). Mean while, S24-7, an LPS-producing bacterium, showed a positive correlation. Collectively, SCFA-producing bacteria were negatively associated with stroke progression and gut barrier dysfunction.
TABLE 2.
Spearman’s correlation for different bacteria and mouse injury indices after MCAO
| Bacteria | Target | R | P value |
|---|---|---|---|
| Ruminococcaceae | Cerebral infarction ratio | –0.900 | 0.002 |
| mNSS | –0.825 | 0.000 | |
| LBP | –0.800 | 0.014 | |
| LPS | –0.767 | 0.021 | |
| Ocln in ileum | 0.738 | 0.046 | |
| Cldn4 in ileum | 0.833 | 0.015 | |
| Cxcl1 in ileum | –0.810 | 0.022 | |
| Ocln in colon | 0.762 | 0.037 | |
| Cldn4 in colon | 0.738 | 0.046 | |
| Cxcl1 in colon | –0.786 | 0.028 | |
| Cxcl2 in colon | –0.786 | 0.028 | |
| Lachnospira | Cerebral infarction ratio | –0.683 | 0.050 |
| mNSS | –0.908 | 0.000 | |
| LBP | –0.700 | 0.043 | |
| LPS | –0.750 | 0.026 | |
| Cldn4 in ileum | 0.905 | 0.005 | |
| Cxcl1 in ileum | –0.738 | 0.046 | |
| Cxcl1 in colon | –0.762 | 0.037 | |
| Cxcl2 in colon | –0.833 | 0.015 | |
| S24-7 | Cerebral infarction ratio | 0.740 | 0.029 |
| mNSS | 0.638 | 0.073 | |
| LBP | 0.773 | 0.019 | |
| LPS | 0.798 | 0.013 | |
| Ocln in ileum | –0.723 | 0.045 | |
| Cldn4 in ileum | –0.771 | 0.027 | |
| Ocln in colon | –0.747 | 0.035 |
We performed an additional KEGG functional analysis using Phylogenetic Investigation of Communities by Reconstruction of Unobserved States (PICRUSt) based on 16S rRNA gene sequences. The two groups of GF-treated mice formed significantly different clusters in the principal-component analysis (PCA) plot (Fig. S2A). A total of 78.4% of the variation was captured by the first principal component (PC1). Among the 6,916 affiliated KEGG pathways, 1,591 were shown to achieve a statistically significant difference at P < 0.05, and among them, 22 are shown in Fig. S2B based on P < 10−5. Notably, significant elevation of glycerol uptake facilitator protein and peroxiredoxin and a decrease in putative tributyrin esterase were observed in T2D-treated GF mice compared with control-treated GF mice according to the KEGG Orthologs (KO) database (Fig. S2B).
Differences between functional predictions in the KO hierarchy generated by PICRUSt analysis between T2D-treated GF mice and control-treated GF mice. PCA plots of predicted functions (A). The mean proportion of sequences followed by proportional differences and error bars were generated by STAMP software (B). The P value was calculated by Fisher’s exact test, and the threshold was 10-5. KO, KEGG Orthology; PICRUSt, Phylogenetic Investigation of Communities by Reconstruction of Unobserved States; PCA, principal components analysis. Download FIG S2, TIF file, 26.1 MB (26.1MB, tif) .
Copyright © 2021 Chen et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
DISCUSSION
Diabetes patients usually experience increased adverse events and subsequent mortality after stroke, which is a growing challenge for health care systems (15). In this study, the gut microbial composition of AIS patients resembled that of T2D patients. Both AIS patients and T2D patients revealed a remarkable alteration in gut microbial composition by exhibiting a decreased abundance of commensal or beneficial bacteria, including Prevotella, Faecalibacterium, Lachnospira, and Coprococcus, in accordance with previous studies (12, 16). Faecalibacterium, Lachnospira, and Coprococcus are known to be SCFA-producing bacteria. SCFAs play critical roles at both the intestinal and extraintestinal levels, including maintaining intestinal barrier functions, reducing the severity of mucosal inflammation, promoting intestinal oxidative status, enhancing colon motility functions, and improving many pathologies (17, 18). In addition, SCFAs also help to improve metabolic functions in T2D by inhibiting inflammation and insulin resistance, augmenting GLP-1 secretion, and ameliorating β-cell function (19). On the other hand, opportunistic pathogens, such as Proteobacteria and Enterobacteriaceae, showed a growth advantage in both AIS patients and T2D patients. Proteobacteria is proposed as a marker for dysbiosis of the microbial community and a potential diagnostic criterion for metabolic and immune disorders (20) and is also enriched in hosts with glucose intolerance utilizing artificial sweeteners and dietary emulsifiers (21). Enterobacteriaceae is regarded as a major harmful member of the human symbiotic microbial community, triggering enteropathy and interfering with the development of mucosal immunity and healthy gut microbes (22). Enterobacteriaceae has also been identified as an independent risk factor in predicting early-stage recovery for AIS patients (8).
AIS_T2D patients showed the highest extent of gut microbial dysbiosis with increased abundance of opportunistic pathogens belonging to the phylum Proteobacteria and reduced commensal or beneficial bacteria, implying that AIS and T2D had an additive effect on gut microbiota dysbiosis in AIS_T2D patients. Previous studies suggested that the additive effects of the gut microbiota were mediated by gut dysbiosis, diet, and lifestyle changes (23, 24). Here, we identified an additive effect contributed by diseases, such as AIS and T2D, and superficially addressed this association, requiring future studies to investigate the underlying mechanism.
We emphasize an important role for gut dysbiosis associated with T2D in exacerbating the severity and prognosis of stroke. By formulating a T2D gut microbial dysbiosis index, we found that T2D gut microbial indices showed a significantly positive correlation with the NIHSS, Essen stroke risk score, and mRS score, supporting an important role of gut dysbiosis as a risk factor in predicting the severity and poor outcomes of stroke patients. Similarly, an index formulated based on gut dysbiosis of stroke patients was also significantly associated with brain injury (25). By conducting FMT of T2D-associated gut microbiota on GF mice, we found that gut dysbiosis associated with T2D may exacerbate the aggregation of brain injury and neurological defects poststroke. In addition, FMT of T2D-associated gut microbiota induces gut barrier dysfunction in GF mice, including elevated serum LBP and LPS levels and impairment of tight junction protein distribution. LBP plays a key role in endotoxin signaling and binds to LPS to stimulate cell activation. As a glycolipid located in the outer membrane of Gram-negative bacteria, LPS can potently induce protective and potentially harmful inflammatory responses. Increased plasma endotoxin activity in AIS patients is associated with unfavorable short-term functional outcomes (26). Changes in commensal and pathogenic microorganisms may induce intestinal mucosal barrier disruption (27), which may contribute to brain infarction exacerbation.
Here, we further identified 25 OTUs in the Ruminococcaceae family that were closely related to mouse outcome indices, namely, 22 OTUs that were negatively associated with worse brain injury or gut barrier dysfunction and three OTUs positively associated with these indices. Both OTUs in Lachnospira were negatively associated with impaired brain injury and gut barrier dysfunction. Ruminococcaceae and Lachnospira are both SCFA-producing bacteria that orchestrate the epithelial barrier to maintain gut integrity (28, 29), restore gut barrier function (30, 31), and prevent translocation and dissemination of gut bacteria and related components. In addition to SCFAs, alterations in gut microbial composition, such as increased abundance of LPS-producing bacteria, can also affect gut barrier integrity (32). As expected, S24-7 and Rikenellaceae from LPS-producing bacterial families showed opposite correlations compared with those of the SCFA-producing bacteria. S24-7 contributed to cerebral cavernous malformation lesion formation through the LPS-TLR4 pathway associated with disruption of the gut barrier (33) and showed a positive correlation with immune responses, including NF-κB activity (34). Decreased abundance of Ruminococcaceae and increased Rikenellaceae were observed in high-fat diet mice (35). Here, we provide relationships between the gut microbiota and brain infarction and gut barrier dysfunction indices. There were four mice in the T2D-treated GF mouse group and five in the control group. The number of GF mice was rather limited. Future studies that define the causative relationship between SCFA- or LPS-producing bacteria and brain injury poststroke are required.
In the analysis of predicted metabolic profiles, we found that functional pathways involved in energy metabolism and oxidative stress were significantly elevated in T2D-treated mice compared with control-treated GF mice. Our results indicated that the energy metabolism pathway may be influenced by gut microbial dysbiosis in T2D patients and correlated with exacerbated brain injury poststroke. Evidence has shown that the gut microbiota may affect the lipid metabolism process of the host and is associated with many risk factors for stroke, including obesity (36), diabetes (11, 24) and atherosclerosis (37). Our results showed a short-term effect of gut microbial metabolism dysbiosis on brain injury poststroke. Another study showed that lipid metabolism may exacerbate stroke outcome by developing depression poststroke. Therefore, exacerbated brain injury and gut barrier dysfunction in T2D-treated GF mice may be mediated by the gut microbiome and metabolic dysbiosis. Future studies are needed to focus on the potential energy metabolism functions and their interactions with stroke outcome.
MATERIALS AND METHODS
Clinical study design and sample collection.
The human observational study was approved by the Ethics Committee of Southern Medical University (NFEC-2016-148). Written informed consent was obtained from all subjects. Patients diagnosed with AIS, including AIS patients and AIS_T2D patients, were consecutively recruited if they met the following criteria: (i) presented with ischemic stroke due to cerebral infarction (according to standard clinical criteria with supporting cerebral imaging evidence consisting of either computed tomography or magnetic resonance imaging and magnetic resonance angiography); (ii) had no evidence of hemorrhagic infarction; (iii) were >18 years of age; (iv) were admitted between 2 and 7 days after stroke onset; and (v) had a NIHSS <16 on admission. The exclusion criteria included the following: (i) severe comorbidities; (ii) unstable medical condition; (iii) chronic inflammatory disease; and (iv) treatment with antibiotics during the preceding 1 month. Patients with AIS were assessed by the NIHSS on admission and mRS and Essen stroke risk scores at 2 years poststroke. NIHSS is the most widely used measure of neurologic severity caused by AIS (38). The Essen stroke risk score and mRS score are used for risk stratification and quantification of the severity and outcome in AIS patients, respectively (39, 40). The World Health Organization (WHO) criteria were used for the definition of T2D (41). The participants were consecutively recruited from Nanfang Hospital (Southern Medical University, Guangzhou, China). A total of 90 AIS patients, 60 AIS patients with T2D, and 35 T2D patients were recruited to participate in this study. The first available fecal sample after admission and the clinical data were collected from all participating patients.
The control group included 55 healthy people who resided in Guangzhou City for more than 5 years. They had no cardiovascular or cerebrovascular diseases. The exclusion criteria for the control group were the same as those described above. Fresh fecal samples and demographic information were collected for the control group. All samples were frozen at −80°C until analysis.
16S RNA sequencing and microbiome data analysis.
In the clinical study, bacterial genomic DNA was extracted from fecal samples using the PowerSoil DNA Extraction Kit (Mo Bio) following the manufacturer’s specifications (42). A total of 240 individually processed human fecal gDNA extractions were PCR amplified. The barcoded primers 514F (GTGCCAGCMGCCGCGGTAA) and 805R (GGACTACHVGGGTWTCTAAT) were used to amplify the 16S rRNA gene V4 variable region. The PCR cycle conditions were as follows: 94°C for 2 min; followed by 30 cycles at 94°C for 30 s, 54°C for 30 s, and 72°C for 45 s; and a final elongation at 72°C for 5 min (43). All PCR amplicons were mixed together and sequenced using Illumina paired-end sequencing following the manufacturer’s protocol. The raw sequences were preprocessed and quality controlled using QIIME 2 with default parameters (44) and then demultiplexed and clustered into species-level OTUs with 97% similarity. OTU generation was based on the USEARCH algorithm (45).
In animal experiments, fecal samples of GF mice after they received FMT were collected. DNA extraction was performed according to the QIAamp minikit manufacturer’s instructions. Amplification and sequencing of bacterial 16S rRNA genes were performed by the Illumina ISEQ 100 platform following the manufacturer’s protocol. The raw sequences were denoised with DADA2 (1.6.0) to generate amplicon sequence variants (ASVs).
Representative sequences were determined because of sequence frequency, classified by Greengenes v13_8 and aligned using the PyNAST algorithms (46). According to the representative sequence alignment, we used Fast-Tree to determine the phylogenetic relationships (47). UniFrac distances were used to analyze the β-diversity by illustrating the phylogenetic dissimilarity among samples. PCoA is a dimensionality reduction method that describes the relationship among samples based on the distance matrix and visualizes the unsupervised grouping pattern of the microbiome. The Adonis test was performed using QIIME 2 software to analyze the multidimensional microbiome data. LEfSe was used to compare the discriminative data between groups (48). LEfSe determines the abundant features most different between the conditions in accordance with biologically meaningful categories by emphasizing statistical significance, biological consistency, and effect relevance. For each differential feature in LEfSe analysis, we calculated a linear discriminant analysis value to represent the difference in the feature between groups. KEGG functions in GF mice were predicted by using PICRUSt. The differences in KEGG pathways between T2D-treated GF mice and control-treated GF mice were determined by using statistical analysis of metagenomic profiles (STAMP) (49).
T2D gut microbial dysbiosis index.
We formulated a T2D index to represent the overall gut dysbiosis associated with T2D. The index is calculated as
We filtered the bacterial genera that exhibited a prevalence lower than 10%. The Wilcoxon rank sum test was used between T2D patients and healthy controls, and 11 significantly different genera were selected (P < 0.05), including Porphyromonas, Lactobacillus, Blautia, Dorea, Lachnospira, Roseburia, Megasphaera, Catenibacterium, Cetobacterium, and two genera from Enterobacteriaceae. This formula was used to calculate the T2D gut microbial dysbiosis index.
Animal experimental design.
GF mice. The GF mouse experiment was performed in accordance with the institutional guidelines and regulations and was approved by the Ethics Committee of Jinan University (IACUC-20180409-02). GF male ICR mice were raised in the Experimental Animal Research Center at Jinan University. Throughout the experiment, they were given the same standard chow and autoclaved water ad libitum and housed in a controlled environment (23°C; inverted 12-h daylight cycle; 40% humidity). The general health status of the mice was checked by investigators every day. All mice were 8 weeks old and were comparable to normal health before the intervention. This experiment was performed in sterile environment.
FMT. Fecal samples were frozen at −80°C until they were chosen and used in FMT, and all samples were handled under anaerobic conditions. Samples of T2D participants (n = 3, male) and healthy controls (n = 3, male) were randomly chosen. Each fecal sample (0.1 g) was mixed with 1.5 mL of sterile physiological saline, and pools were made from equal volumes of the donor suspensions. The suspensions were mixed and centrifuged (2,000 rpm, 10 min), and the supernatants were collected. Then, 200 μL of supernatant was administered to each mouse by gastric gavage. The GF mice were randomized into two groups, which were transplanted with fecal samples from T2D patients or healthy controls every other day for 1 week. Two groups of mice were bred separately in different cages to prevent normalization of their gut microbiota.
MCAO, evaluation of brain infarct sizes, and mouse neurological deficits.
MCAO and evaluation of brain infarct lesions were performed as described by Xu et al. (8). GF mice were occluded for 60 min. The overall mortality rate during this procedure was 10%. At 24 h after MCAO, neurological deficits were evaluated by the mNSS, in which the severity of injury was graded on a scale of 0 to 14 (50). All evaluation processes were conducted by two investigators who were blinded to the experimental groups. Then, the mice were anaesthetized, and samples were collected for further analysis.
Blood samples.
Blood samples of GF mice were collected from the orbital plexus vein and centrifuged to obtain serum for biochemical analyses. Mouse serum LPS and LBP levels were determined using ELISA kits (Elisalab) according to the manufacturer’s protocol.
Quantitative determination of mRNA levels in intestinal tissue.
The relative transcription levels of mRNAs for ZO-1, occludin, claudin-4, chemokine (C-X-C motif) ligand 1, and chemokine (C-X-C motif) ligand 2 encoded by the Tjp1, Ocln, Cldn4, Cxcl1, and Cxcl2 genes, respectively, were determined by qRT-PCR. Ileum and colon tissues acquired from GF mice were homogenized using a Mini Beadbeater (TIANGEN), and RNA was extracted by the TRIzol reagent method (Thermo Fisher Scientific). cDNA was generated with TaKaRa reverse transcription reagents. Real-time PCR was performed by using a ViiA 7 real-time PCR system (TaKaRa). We analyzed the data with the comparative Ct method. Target gene transcription of each sample was normalized to the respective levels of β-actin mRNA. The primers used in this study are listed in Table 3.
TABLE 3.
Primers used in quantitative real-time PCR in this study
| Organism | Target gene | Sequence |
|---|---|---|
| Mus musculus | Tjp1 | 5′-CTCCAGGTGCTTCTCTTGCT-3′ 5′-TATCTTCGGGTGGCTTCACT-3′ |
| Mus musculus | Ocln | 5′-ACGGACCCTGACCACTATGA-3′ 5′-TCAGCAGCAGCCATGTACTC-3′ |
| Mus musculus | Cldn4 | 5′-ATCGTTGTCCGCGAGTTCTA-3′ 5′-GCTTGTCGTTGCTACGAGGT-3′ |
| Mus musculus | Cxcl1 | 5′-TGCACCCAAACCGAAGTCAT-3′ 5′-TTGTCAGAAGCCAGCGTTCAC-3′ |
| Mus musculus | Cxcl2 | 5′-TCCAGGTCAGTTAGCCTTGC-3′ 5′-CGGTCAAAAAGTTTGCCTTG-3′ |
| Mus musculus | Actb | 5′-AGAGGGAAATCGTGCGTGAC-3′ 5′-CAATAGTGATGACCTGGCCGT-3′ |
Immunofluorescence.
GF mouse ileum and colon tissues were removed, washed with PBS, and fixed in 4% paraformaldehyde, dehydrated, cleared, and embedded in paraffin. The paraffin sections were deparaffinized, rehydrated, and treated with EDTA antigen retrieval buffers. The slides were immunostained with anti-ZO-1 (1:100, Proteintech Group) and anti-occludin (1:50, Proteintech Group) antibodies overnight at 4°C, followed by incubation with a goat anti-rabbit Cy3-conjugated secondary antibody (1:200, Servicebio) for 1 h in total darkness. DAPI was used for nuclei staining. Fluorescence images were captured using a Nikon Eclipse Ti-SR fluorescence microscope at a magnification of ×20.
Statistical analysis.
Statistical analysis was implemented using R3.5.1 and SPSS 20.0 (IBM, USA). The mean ± SEM and percentages were used to express continuous and discrete data. The Wilcoxon rank sum test was used to determine significant differences between different groups. Bonferroni adjustment was used for multiple comparisons. Pearson’s chi-square test was used to determine the significant differences in categorical data between two groups. Correlation analysis was calculated by the Spearman correlation test. P < 0.05 was considered statistically significant.
Data availability.
The raw data for 16S rRNA gene sequences in this study are available from the Sequence Read Archive (https://www.ncbi.nlm.nih.gov/bioproject) at accession number PRJNA743790.
Supplementary Material
ACKNOWLEDGMENTS
We gratefully acknowledge all the workers from the Experimental Animal Research Center at Jinan University for their support during the GF mouse experiment.
K.X. and W.S. conceived the study and designed the research. K.X., X.C., Q.W., J.Z., and G.X. performed the sampling, collected clinical patient data, processed samples, and conducted the experiments. K.X. and Y.H. analyzed the data. X.G. and H.W. performed the animal experiments. K.X., W.S., and Y.H. wrote the manuscript and revised the article. All authors have read and approved the final version of the manuscript.
This study was funded by the National Natural Science Foundation of China (NSFC31800415, NSFC82022044, NSFC81800746, and NSFC32171155), China Postdoctoral Science Foundation (2018M630967), and Science and Technology Program of Guangzhou, China (201904010091).
We declare no conflict of interest.
Contributor Information
Wei Song, Email: songwei75@smu.edu.cn.
Kaiyu Xu, Email: xukaiyu09@smu.edu.cn.
Joshua E. Elias, Chan Zuckerberg Biohub
Xiaoquan Su, Qingdao University.
REFERENCES
- 1.Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, Wang L, Jiang Y, Li Y, Wang Y, Chen Z, Wu S, Zhang Y, Wang D, Wang Y, Feigin VL. 2017. Prevalence, incidence, and mortality of stroke in China: Results from a nationwide population-based survey of 480,687 adults. Circulation 135:759–771. doi: 10.1161/CIRCULATIONAHA.116.025250. [DOI] [PubMed] [Google Scholar]
- 2.Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, Liu J, Zhang M, Qi J, Yu S, Afshin A, Gakidou E, Glenn S, Krish VS, Miller-Petrie MK, Mountjoy-Venning WC, Mullany EC, Redford SB, Liu H, Naghavi M, Hay SI, Wang L, Murray CJL, Liang X. 2019. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 394:1145–1158. doi: 10.1016/s0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hankey GJ. 2017. Stroke. Lancet 389:641–654. doi: 10.1016/S0140-6736(16)30962-X. [DOI] [PubMed] [Google Scholar]
- 4.Heden Stahl C, Lind M, Svensson AM, Kosiborod M, Gudbjornsdottir S, Pivodic A, Clements M, Rosengren A. 2017. Long-term excess risk of stroke in people with Type 2 diabetes in Sweden according to blood pressure level: a population-based case-control study. Diabet Med 34:522–530. doi: 10.1111/dme.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liao CC, Shih CC, Yeh CC, Chang YC, Hu CJ, Lin JG, Chen TL. 2015. Impact of diabetes on stroke risk and outcomes: two nationwide retrospective cohort studies. Medicine (Baltimore, MD) 94:e2282. doi: 10.1097/MD.0000000000002282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, Stehouwer CD, Lewington S, Pennells L, Thompson A, Sattar N, White IR, Ray KK, Danesh J, Emerging Risk Factors Collaboration . 2010. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375:2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R. 2008. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57:1470–1481. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 8.Xu K, Gao X, Xia G, Chen M, Zeng N, Wang S, You C, Tian X, Di H, Tang W, Li P, Wang H, Zeng X, Tan C, Meng F, Li H, He Y, Zhou H, Yin J. 2021. Rapid gut dysbiosis induced by stroke exacerbates brain infarction in turn. Gut 70:1486–1494. doi: 10.1136/gutjnl-2020-323263. [DOI] [PubMed] [Google Scholar]
- 9.Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S, Prifti E, Vieira-Silva S, Gudmundsdottir V, Pedersen HK, Arumugam M, Kristiansen K, Voigt AY, Vestergaard H, Hercog R, Costea PI, Kultima JR, Li J, Jørgensen T, Levenez F, Dore J, Nielsen HB, Brunak S, Raes J, Hansen T, Wang J, Ehrlich SD, Bork P, Pedersen O, MetaHIT consortium . 2015. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528:262–266. doi: 10.1038/nature15766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JF, Dallinga-Thie GM, Ackermans MT, Serlie MJ, Oozeer R, Derrien M, Druesne A, Van Hylckama Vlieg JE, Bloks VW, Groen AK, Heilig HG, Zoetendal EG, Stroes ES, de Vos WM, Hoekstra JB, Nieuwdorp M. 2012. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 143:913–916.e7. doi: 10.1053/j.gastro.2012.06.031. [DOI] [PubMed] [Google Scholar]
- 11.Komaroff AL. 2017. The microbiome and risk for obesity and diabetes. JAMA 317:355–356. doi: 10.1001/jama.2016.20099. [DOI] [PubMed] [Google Scholar]
- 12.Yin J, Liao SX, He Y, Wang S, Xia GH, Liu FT, Zhu JJ, You C, Chen Q, Zhou L, Pan SY, Zhou HW. 2015. Dysbiosis of gut microbiota with reduced trimethylamine-N-oxide level in patients with large-artery atherosclerotic stroke or transient ischemic attack. J Am Heart Assoc 4:e002699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. 2013. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 368:1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu W, Gregory JC, Org E, Buffa JA, Gupta N, Wang Z, Li L, Fu X, Wu Y, Mehrabian M, Sartor RB, McIntyre TM, Silverstein RL, Tang WHW, DiDonato JA, Brown JM, Lusis AJ, Hazen SL. 2016. Gut microbial metabolite TMAO enhances platelet hyperreactivity and thrombosis risk. Cell 165:111–124. doi: 10.1016/j.cell.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Einarson TR, Acs A, Ludwig C, Panton UH. 2018. Economic burden of cardiovascular disease in type 2 diabetes: a systematic review. Value Health 21:881–890. doi: 10.1016/j.jval.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 16.Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D, Peng Y, Zhang D, Jie Z, Wu W, Qin Y, Xue W, Li J, Han L, Lu D, Wu P, Dai Y, Sun X, Li Z, Tang A, Zhong S, Li X, Chen W, Xu R, Wang M, Feng Q, Gong M, Yu J, Zhang Y, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto JM, Zhang Z, Chen H, Yang R, Zheng W, Li S, Yang H, et al. 2012. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490:55–60. doi: 10.1038/nature11450. [DOI] [PubMed] [Google Scholar]
- 17.Rios-Covian D, Ruas-Madiedo P, Margolles A, Gueimonde M, de Los Reyes-Gavilan CG, Salazar N. 2016. Intestinal short chain fatty acids and their link with diet and human health. Front Microbiol 7:185. doi: 10.3389/fmicb.2016.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM. 2013. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res 54:2325–2340. doi: 10.1194/jlr.R036012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Puddu A, Sanguineti R, Montecucco F, Viviani GL. 2014. Evidence for the gut microbiota short-chain fatty acids as key pathophysiological molecules improving diabetes. Mediators Inflamm 2014:162021. doi: 10.1155/2014/162021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shin NR, Whon TW, Bae JW. 2015. Proteobacteria: microbial signature of dysbiosis in gut microbiota. Trends Biotechnol 33:496–503. doi: 10.1016/j.tibtech.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Chassaing B, Koren O, Goodrich JK, Poole AC, Srinivasan S, Ley RE, Gewirtz AT. 2015. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 519:92–96. doi: 10.1038/nature14232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kau AL, Planer JD, Liu J, Rao S, Yatsunenko T, Trehan I, Manary MJ, Liu TC, Stappenbeck TS, Maleta KM, Ashorn P, Dewey KG, Houpt ER, Hsieh CS, Gordon JI. 2015. Functional characterization of IgA-targeted bacterial taxa from undernourished Malawian children that produce diet-dependent enteropathy. Sci Transl Med 7:276ra24. doi: 10.1126/scitranslmed.aaa4877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fei N, Zhao L. 2013. An opportunistic pathogen isolated from the gut of an obese human causes obesity in germfree mice. ISME J 7:880–884. doi: 10.1038/ismej.2012.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.He Y, Wu W, Wu S, Zheng HM, Li P, Sheng HF, Chen MX, Chen ZH, Ji GY, Zheng ZD, Mujagond P, Chen XJ, Rong ZH, Chen P, Lyu LY, Wang X, Xu JB, Wu CB, Yu N, Xu YJ, Yin J, Raes J, Ma WJ, Zhou HW. 2018. Linking gut microbiota, metabolic syndrome and economic status based on a population-level analysis. Microbiome 6:172. doi: 10.1186/s40168-018-0557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xia GH, You C, Gao XX, Zeng XL, Zhu JJ, Xu KY, Tan CH, Xu RT, Wu QH, Zhou HW, He Y, Yin J. 2019. Stroke Dysbiosis Index (SDI) in gut microbiome are associated with brain injury and prognosis of stroke. Front Neurol 10:397. doi: 10.3389/fneur.2019.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klimiec E, Pera J, Chrzanowska-Wasko J, Golenia A, Slowik A, Dziedzic T. 2016. Plasma endotoxin activity rises during ischemic stroke and is associated with worse short-term outcome. J Neuroimmunol 297:76–80. doi: 10.1016/j.jneuroim.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Martens EC, Neumann M, Desai MS. 2018. Interactions of commensal and pathogenic microorganisms with the intestinal mucosal barrier. Nat Rev Microbiol 16:457–470. doi: 10.1038/s41579-018-0036-x. [DOI] [PubMed] [Google Scholar]
- 28.Gonzalez A, Krieg R, Massey HD, Carl D, Ghosh S, Gehr TWB, Ghosh SS. 2019. Sodium butyrate ameliorates insulin resistance and renal failure in CKD rats by modulating intestinal permeability and mucin expression. Nephrol Dial Transplant 34:783–794. doi: 10.1093/ndt/gfy238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feng W, Wu Y, Chen G, Fu S, Li B, Huang B, Wang D, Wang W, Liu J. 2018. Sodium butyrate attenuates diarrhea in weaned piglets and promotes tight junction protein expression in colon in a GPR109A-dependent manner. Cell Physiol Biochem 47:1617–1629. doi: 10.1159/000490981. [DOI] [PubMed] [Google Scholar]
- 30.Hu ED, Chen DZ, Wu JL, Lu FB, Chen L, Zheng MH, Li H, Huang Y, Li J, Jin XY, Gong YW, Lin Z, Wang XD, Xu LM, Chen YP. 2018. High fiber dietary and sodium butyrate attenuate experimental autoimmune hepatitis through regulation of immune regulatory cells and intestinal barrier. Cell Immunol 328:24–32. doi: 10.1016/j.cellimm.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 31.Matheus VA, Monteiro L, Oliveira RB, Maschio DA, Collares-Buzato CB. 2017. Butyrate reduces high-fat diet-induced metabolic alterations, hepatic steatosis and pancreatic beta cell and intestinal barrier dysfunctions in prediabetic mice. Exp Biol Med (Maywood) 242:1214–1226. doi: 10.1177/1535370217708188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kang C, Wang B, Kaliannan K, Wang X, Lang H, Hui S, Huang L, Zhang Y, Zhou M, Chen M, Mi M. 2017. Gut microbiota mediates the protective effects of dietary capsaicin against chronic low-grade inflammation and associated obesity induced by high-fat diet. mBio 8:e00470. doi: 10.1128/mBio.00900-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang AT, Choi JP, Kotzin JJ, Yang Y, Hong CC, Hobson N, Girard R, Zeineddine HA, Lightle R, Moore T, Cao Y, Shenkar R, Chen M, Mericko P, Yang J, Li L, Tanes C, Kobuley D, Vosa U, Whitehead KJ, Li DY, Franke L, Hart B, Schwaninger M, Henao-Mejia J, Morrison L, Kim H, Awad IA, Zheng X, Kahn ML. 2017. Endothelial TLR4 and the microbiome drive cerebral cavernous malformations. Nature 545:305–310. doi: 10.1038/nature22075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu HX, Rocha CS, Dandekar S, Wan YJ. 2016. Functional analysis of the relationship between intestinal microbiota and the expression of hepatic genes and pathways during the course of liver regeneration. J Hepatol 64:641–650. doi: 10.1016/j.jhep.2015.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daniel H, Gholami AM, Berry D, Desmarchelier C, Hahne H, Loh G, Mondot S, Lepage P, Rothballer M, Walker A, Bohm C, Wenning M, Wagner M, Blaut M, Schmitt-Kopplin P, Kuster B, Haller D, Clavel T. 2014. High-fat diet alters gut microbiota physiology in mice. ISME J 8:295–308. doi: 10.1038/ismej.2013.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cani PD, Van Hul M, Lefort C, Depommier C, Rastelli M, Everard A. 2019. Microbial regulation of organismal energy homeostasis. Nat Metab 1:34–46. doi: 10.1038/s42255-018-0017-4. [DOI] [PubMed] [Google Scholar]
- 37.Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, Britt EB, Fu X, Wu Y, Li L, Smith JD, DiDonato JA, Chen J, Li H, Wu GD, Lewis JD, Warrier M, Brown JM, Krauss RM, Tang WH, Bushman FD, Lusis AJ, Hazen SL. 2013. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med 19:576–585. doi: 10.1038/nm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yoshimura S, Lindley RI, Carcel C, Sato S, Delcourt C, Wang X, Chalmers J, Anderson CS, for the ENCHANTED Investigators . 2018. NIHSS cut point for predicting outcome in supra- vs infratentorial acute ischemic stroke. Neurology 91:e1695–e1701. doi: 10.1212/WNL.0000000000006437. [DOI] [PubMed] [Google Scholar]
- 39.Rothwell PM, Algra A, Chen Z, Diener HC, Norrving B, Mehta Z. 2016. Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: time-course analysis of randomised trials. Lancet 388:365–375. doi: 10.1016/S0140-6736(16)30468-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Andersen SD, Gorst-Rasmussen A, Lip GY, Bach FW, Larsen TB. 2015. Recurrent stroke: the value of the CHA2DS2VASc score and the Essen stroke risk score in a nationwide stroke cohort. Stroke 46:2491–2497. doi: 10.1161/STROKEAHA.115.009912. [DOI] [PubMed] [Google Scholar]
- 41.Alberti KG, Zimmet PZ, WHO Consultation . 1998. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553. doi:. [DOI] [PubMed] [Google Scholar]
- 42.Peng X, Yu KQ, Deng GH, Jiang YX, Wang Y, Zhang GX, Zhou HW. 2013. Comparison of direct boiling method with commercial kits for extracting fecal microbiome DNA by Illumina sequencing of 16S rRNA tags. J Microbiol Methods 95:455–462. doi: 10.1016/j.mimet.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 43.Zhou HW, Li DF, Tam NF, Jiang XT, Zhang H, Sheng HF, Qin J, Liu X, Zou F. 2011. BIPES, a cost-effective high-throughput method for assessing microbial diversity. ISME J 5:741–749. doi: 10.1038/ismej.2010.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Pena AG, Goodrich JK, Gordon JI, Huttley GA, Kelley ST, Knights D, Koenig JE, Ley RE, Lozupone CA, McDonald D, Muegge BD, Pirrung M, Reeder J, Sevinsky JR, Turnbaugh PJ, Walters WA, Widmann J, Yatsunenko T, Zaneveld J, Knight R. 2010. QIIME allows analysis of high-throughput community sequencing data. Nat Methods 7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Edgar RC. 2010. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26:2460–2461. doi: 10.1093/bioinformatics/btq461. [DOI] [PubMed] [Google Scholar]
- 46.Caporaso JG, Bittinger K, Bushman FD, DeSantis TZ, Andersen GL, Knight R. 2010. PyNAST: a flexible tool for aligning sequences to a template alignment. Bioinformatics 26:266–267. doi: 10.1093/bioinformatics/btp636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Price MN, Dehal PS, Arkin AP. 2009. FastTree: computing large minimum evolution trees with profiles instead of a distance matrix. Mol Biol Evol 26:1641–1650. doi: 10.1093/molbev/msp077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, Huttenhower C. 2011. Metagenomic biomarker discovery and explanation. Genome Biol 12:R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parks DH, Beiko RG. 2010. Identifying biologically relevant differences between metagenomic communities. Bioinformatics 26:715–721. doi: 10.1093/bioinformatics/btq041. [DOI] [PubMed] [Google Scholar]
- 50.Li Y, Chopp M, Chen J, Wang L, Gautam SC, Xu YX, Zhang Z. 2000. Intrastriatal transplantation of bone marrow nonhematopoietic cells improves functional recovery after stroke in adult mice. J Cereb Blood Flow Metab 20:1311–1319. doi: 10.1097/00004647-200009000-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
LEfSe analysis showed obvious dysbiosis of the gut microbiome of AIS patients (A), T2D patients (B), and AIS_T2D patients (C) compared with the control group. AIS, acute ischemic stroke; LEfSe, linear discriminant analysis effect size. Download FIG S1, TIF file, 17.6 MB (17.6MB, tif) .
Copyright © 2021 Chen et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Differences between functional predictions in the KO hierarchy generated by PICRUSt analysis between T2D-treated GF mice and control-treated GF mice. PCA plots of predicted functions (A). The mean proportion of sequences followed by proportional differences and error bars were generated by STAMP software (B). The P value was calculated by Fisher’s exact test, and the threshold was 10-5. KO, KEGG Orthology; PICRUSt, Phylogenetic Investigation of Communities by Reconstruction of Unobserved States; PCA, principal components analysis. Download FIG S2, TIF file, 26.1 MB (26.1MB, tif) .
Copyright © 2021 Chen et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Data Availability Statement
The raw data for 16S rRNA gene sequences in this study are available from the Sequence Read Archive (https://www.ncbi.nlm.nih.gov/bioproject) at accession number PRJNA743790.