Abstract
There are few known determinants of sedentary behaviour (SB) in children. We generated and compared profiles associated with risk of excess SB among children (n = 294) both at 8–10 and 10–12 years of age (Visits 1 and 2, respectively), using data from the QUebec Adipose and Lifestyle InvesTigation in Youth. Excess SB was measured by accelerometry and defined as >50% of total wear time at <100 counts/minutes. Recursive partitioning analyses were performed with candidate individual-, family-, and neighbourhood-level factors assessed at Visit 1, and distinct groups at varying risk of excess SB were identified for both timepoints. From the ages of 8–10 to 10–12 years, the prevalence of excess SB more than doubled (24.5% to 57.1%). At Visit 1, excess SB was greatest (73%) among children simultaneously not meeting physical activity guidelines, reporting >2 h/day of weekday non-academic screen time, living in low-dwelling density neighbourhoods, having poor park access, and living in neighbourhoods with greater disadvantage. At Visit 2, the high-risk group (70%) was described by children simultaneously not meeting physical activity guidelines, reporting >2 h/day of non-academic screen time on weekends, and living in neighbourhoods with low disadvantage. Risk factors related to individual lifestyle behaviours are generally consistent, and neighbourhood factors generally inconsistent, as children age from late childhood to pre-adolescence. Multiple factors from developmental, behavioural and contextual domains increase risk for excess sedentary behaviour; these warrant consideration to devise effective prevention or management strategies.
Abbreviations: SB, Sedentary behavior; PA, Physical activity; QUALITY, QUebec Adipose and Lifestyle InvesTigation in Youth; MVPA, Moderate to vigorous physical activity; BMI, Body mass index; RPA, Recursive partitioning analyses
Keywords: Sedentary behaviour, Obesity prevention, Neighbourhood, Body mass index, Children, Adolescence
1. Background
Children and adolescents in developed nations devote much of their discretionary time to sedentary pursuits. Sedentary behaviour (SB) is characterised by energy expenditure ≤ 1.5 metabolic equivalents (Tremblay et al., 2017, Bejarano et al., 2019, Bringolf-Isler et al., 2018, Goon et al., 2020, Lotoski et al., 2021), involving predominantly prolonged sitting, watching television, reading, using the computer and other mobile devices, or passive transportation. Canadian children and youth are sedentary an average of 8.3 h per day, representing approximately 62% of their waking hours (Larouche et al., 2016), with similar trends being reported in American children and adolescents (Yang et al., 2019). Systematic reviews on tracking of SB show that risk categories in early childhood track into middle childhood (Jones et al., 2013) and adolescence (Biddle et al., 2010), and that the amount of time spent engaged in SB steadily increases as children age (Pearson et al., 2017). This is of great concern to public health as SB is a major determinant of obesity in children and adolescents, independently of level of physical activity (PA) (Rezende et al., 2014, Tremblay et al., 2011).
Factors from multiple domains interact to influence health behaviours such as SB, including individual-, family-, and broader contextual-level characteristics (Sallis et al., 2015). A growing number of studies on correlates and potential determinants of SB among children and adolescents have reported on these relationships. For example, at the individual level, age has consistently been reported to be positively associated with SB time (Stierlin et al., 2015). Although several studies observed sex-related differences in SB (e.g.: (Aznar et al., 2017, LeBlanc et al., 2015), findings are not consistent across studies, as illustrated in a systematic review of after-school SB among children aged 5–18 years (Arundell et al., 2016). Few associations between family-level correlates (e.g., parental education, family income) and SB have been observed. Hoffmann and colleagues reported an inverse association between household income and SB (Hoffmann et al., 2017), while Atkin and colleagues observed a positive association between SES and objectively measured SB (Atkin et al., 2013). At the neighbourhood level, a variety of features have been investigated, including perceived traffic-related and general area-level safety (Bringolf-Isler et al., 2018, Júdice et al., 2021, Lenhart et al., 2017, Parker et al., 2019), presence of green spaces and PA facilities (Goon et al., 2020, Parker et al., 2019, Hinckson et al., 2017), and walkability, street connectivity, land use mix and density of destinations (Hinckson et al., 2017, Sallis et al., 2018, Bejarano et al., 2019, Bringolf-Isler et al., 2018, Goon et al., 2020, Lotoski et al., 2021). However, as concluded in several systematic reviews, few neighbourhood-level features are consistently associated with SB (Stierlin et al., 2015, Arundell et al., 2016, Parajára et al., 2020). Conceptual and methodological issues may underlie these inconsistencies, including differences in variable selection, measurement, operationalization, and analytic approach used to examine associations (Ding et al., 2011, Dunton et al., 2009, Carter and Dubois, 2010). Moreover, an important shortcoming of most studies of determinants of SB is the lack of consideration of their intercorrelated nature (Leal et al., 2012, Timperio et al., 2017), obscuring potential synergistic or antagonistic effects on SB observed with different combinations of attributes (Timperio et al., 2017).
Synergistic effects are typically tested using interaction terms in regression models (Diez Roux and Mair, 2010). This approach may be limited when complex, non-linear associations are modeled. Analyses based on recursive partitioning methods can overcome this limitation (Strobl et al., 2009). Recursive partitioning analysis, or RPA generates classification trees based on binary splits between higher and lower risk groups using combinations of risk factor variables (Breiman et al., 1984), and is particularly well-suited for cross-level and higher order interactions (Van Hulst et al., 2015).
The objectives of this paper were to 1) generate risk profiles based on combinations of individual-, family-, and neighbourhood-level characteristics, and 2) examine their association with excess SB among children at ages 8–10 years and again at ages 10–12 years.
2. Methods
2.1. Design, recruitment, and sample
The complete methodology of QUALITY has been published elsewhere (Lambert et al., 2012). Briefly, families were recruited using a school-based strategy, with flyers distributed to all grade 2 to 5 students (ages 8 to 10 years) enrolled in schools within a 75 km perimeter of 3 metropolitan areas in the province of Quebec, Canada. Eligibility criteria required participants to have at least one parent living with obesity, based on self-reported weight, height, and waist circumference (WC); to be 8–10 years old at the time of recruitment; and to have both biological parents available for the study. Written informed consent was obtained from parents, and assent was provided by children. Recruitment began in 2006 and was completed in 2008. All participants were White. Baseline (Visit 1) data were collected for 630 children and both biological parents; a 2 year follow-up (Visit 2) assessment was completed in 89% of participants in 2011 when children were aged 10–12 years. At each visit, data collection included accelerometry, interviewer-administered questionnaires for children, self-administered questionnaires for parents, and anthropometrics for children and parents assessed by a trained nurse. Neighbourhood audits were also conducted at Visit 1 for all families residing in the Montréal, Québec Metropolitan area (n = 506/630). The analytic sample comprised participants with complete data at both visits including valid accelerometer measures (a minimum of 4 days of >10 h of wear was required) and neighbourhood audits (n = 294). The Ethics Review Boards of Centre Hospitalier Universitaire Sainte-Justine and Institut Universitaire de Cardiologie et de Pneumologie du Québec at Université Laval approved the study.
2.2. Measures
Participants’ PA and SB were measured using a waist-worn uniaxial accelerometer (Actigraph LS 7164 activity monitor, Actigraph LLC, Pensacola, FL, USA), which was to be worn for 7-days during waking hours, with removal for sleep. A minimum of 4 days of >10 h of wear time was required for data to be considered valid (Bejarano et al., 2019). Non-wear time was defined as at least 60 consecutive minutes of zero counts, with allowance for 1 to 2 consecutive minutes between 0 and 100 counts (Colley et al., 2011).
The amount of sedentary time in minutes/day was calculated using the standardised cut- point of <100 counts per minute (Evenson et al., 2008) at Visits 1 and 2. Participants were classified as engaging in excess SB if they spent ≥ 50% of their time sedentary (i.e. ≥ 300 min for 10 h of wear time). This cut-point is based on the mean time children ages 9–18 years spend engaging in sedentary behaviour, as reported in a pooled analysis of accelerometry studies in this population (Ekelund et al., 2012).
Individual-, family- and neighbourhood-level factors used to identify risk profiles are described below; only variables measured at baseline (Visit 1) were included. Among the individual factors, moderate to vigorous physical activity (MVPA) was calculated using the standardised cut-points for children proposed by Evenson et al. (Evenson et al., 2008). Data were dichotomised into adhering (≥60 min/day in MVPA) or not adhering (<60 min/day in MVPA) to the current Canadian physical activity recommendations for youth (Tremblay et al., 2016). Participants also self-reported the average number of hours per day of television and number of hours per day of computer/video games, during both weekdays and weekends. Hours of weekday screen time and hours of weekend screen time were calculated by summing the hours reported for television and computer/video game for weekdays and for weekends. Only non-academic screen time was recorded. Both measures of screen time were dichotomised as >2 h per day of screen time versus ≤ 2 h per day, following the recommendations of the American Academy of Paediatrics (Co and Media, 2013). At the family-level, total annual household income, adjusted for the number of people living in the household, was obtained from parent-completed questionnaires. Finally, neighbourhood characteristics, computed for the 500-meter network buffer centred on the participant’s residence, were assessed at Visit 1 using two sources: MEGAPHONE, a geographic information system (GIS) that characterizes social, built and natural environmental factors, and on-site neighbourhood audits. MEGAPHONE was designed to investigate the relationship between environmental factors and health outcomes in the Montreal region (Centre de Recherche du CHUM., 2021). Density of dwellings, land use mix, street connectivity, and neighbourhood disadvantage (detailed below) were captured using this data source.
On-site assessments were completed using the validated QUALITY Neighbourhood Audit tool (Roberge et al., 2021), which was adapted from an existing instrument (Paquet et al., 2010). Audits were conducted by independent pairs of trained observers who walked every street within 500 m road network buffers centred on participants’ residences, using an observation grid to score 60 built environment indicators. Inter-rater reliability was substantial (kappa >0.60) (Landis and Koch, 1977) for most of the indicators used in our analyses. Signs of neighbourhood physical disorder and access to parks were also captured using this source.
Dwelling density was dichotomised into upper two (high-dwelling density) versus lower three (low-dwelling density) quintiles. Land use mix (LUM) was computed using an entropy index (Zagorskas, 2016) that measures the homogeneity or diversity of land use within a neighbourhood. This index ranges from 0 to 1, where 1 corresponds to a maximally mixed area and 0 to an entirely homogeneous area. Since high LUM values are associated with higher physical activity levels (Jia et al., 2021), this measure was dichotomised into lower and middle (low LUM) versus upper (high LUM) tertiles of the distribution. Street connectivity was defined as the number of 3- or 4-way intersections in the neighbourhood buffer zone. Higher street connectivity typically indicates more densely constructed neighbourhoods with shorter, more walkable block sizes. Street connectivity was dichotomised into lower and middle (lower connectivity) versus upper (higher connectivity) tertiles. Parks were defined as public open spaces in which children could engage in active play. Participants were classified having access to four or more parks within the 500-meter network buffer centred on their residence (yes, no). Signs of neighbourhood physical disorder (any, none) was determined by any presence of graffiti, litter, or deteriorated roadways and buildings. An additional neighbourhood-level measure, an index of neighbourhood disadvantage, was computed based on principal components analysis with the following measures (percentages) from the 2006 Canadian Census: households living below Statistics Canada’s low-income cut-point (Statistics Canada. Low income cut-offs, 1992), single parent families, unemployed, having moved in the past year, and owner occupied residences. Higher values indicate greater disadvantage. As these factors manifested substantial skewness in their distribution, all were categorised as lower two versus upper tertiles, unless otherwise specified.
2.3. Covariates
Children’s age, sex, pubertal development stage (assessed by a trained nurse using the 5-stage Tanner scales (Diez Roux and Mair, 2010, Strobl et al., 2009), dichotomised as prepubertal [Tanner 1] versus puberty initiated [Tanner >1]), body mass index (BMI) percentile (height [meters2] and weight [kilogram]) were measured by a trained nurse. These were assessed during clinic visits, using an electronic scale for weight and a stadiometer for height, according to standardised protocols, (Lambert et al., 2012) with age- and sex-specific BMI [kilogram/meters2] percentiles calculated according World Health Organisation values (de Onis et al., 2007).
Parental education (>1 parent with a university degree versus no parent with a university degree), and mother and fathers’ BMI (height [stadiometer] and weight [electronic scale] were used to calculate BMI [kilogram/meters2]) were collected at Visit 1 and were included as control variables in multivariate logistic regression analyses.
2.4. Statistical analysis
Separate recursive partitioning analyses (RPA) were used to identify clusters of risk factors associated with excess SB at each time point. RPA is a nonparametric procedure that iteratively evaluates predictor variables to identify optimal binary splits, yielding groups with highest and lowest probabilities of the outcome of interest. This process is repeated until either a subpopulation contains one class of individuals or is too small to be further divided. The result is a classification tree of branching partitions. To correct for potential overfitting, cross-validation was performed using the 10-fold method and 1-Standard Error rule, in which the cross-validated error estimate is no >1-Standard Error larger than the best tree (Strobl et al., 2009). Analyses were conducted using R version 3.2.1 (R Core Team, 2013), using the RPART package (Therneau et al., 2016). In this study, the same 10 factors, 3 individual-level factors (meeting PA guidelines, >2 h/day of screen time on week days, and >2 h/day of screen time on weekend days), one family-level factor (total adjusted annual household income), and 6 neighbourhood-level factors (disadvantage, physical disorder, presence of ≥ 4 parks, dwelling density, land use mix, and street connectivity), were submitted to RPA, based on evidence of associations with SB. The distribution of these 10 factors and the cut- points applied in the RPA are summarised in Table 1.
Table 1.
Distribution of variables retained for recursive partitioning analysis.
| Variable | Mean (SD) | Median | Range (minimum-maximum) | Cut-points for categorization |
|---|---|---|---|---|
| Sedentary behaviour, average minute/day, out of 600 min (Visit 1) | 266.38 (46.77) | 269.50 | (144.93–412.67) | <300 min/day ≥ 300 min/day |
| Sedentary behaviour, average minute/day, out of 600 min (Visit 2) | 310.95 (52.03) | 310.68 | (310.68–594.69) | <300 min/day ≥ 300 min/day |
| Moderate to vigorous physical activity, average min/day | 50.65 (25.80) | 46.57 | (2.43–184.00) | <60 min/day ≥ 60 min/day |
| Screen time weekend day, hours/day | 3.90 (2.94) | 3.0 | (0–13) | ≤ 2 h per day >2 h per day |
| Screen time weekday, hours/day | 2.36 (2.01) | 2.0 | (0–14) | ≤ 2 h per day >2 h per day |
| Neighbourhood disadvantage | 0 (1) | −0.30 | (-1.67–3.83) | <−.58 −0.58 to <0.11 ≥ 0.11 |
| Presence of parks | 2.13 (1.75) | 2.0 | (0–8) | <4 parks ≥ 4 parks |
| Dwelling density; number of private dwellings/Hectare | 16.22 (17.00) | 10.62 | (0.06–82.2) | < 8.29 8.29 to <13.20 ≥ 13.20 |
| Land use mix | 0.36 (0.16) | 0.35 | (0–0.75) | 0 to <0.28 0.28 to <0.42 ≥ 0.42 |
| Street connectivity; number of intersections | 77.94 (39.48) | 75.0 | (0–206) | 0 to <59.00 59.00 to <91.00 ≥ 91.00 |
| Neighbourhood physical disorder, number of signs | 0.45 (0.75) | 0 | (0–3) | 0 ≥ 1 |
| Household income ($CAD) | 43,063 (18722) | 44,907 | (2887–86603) | <25000$ ≥ 25000$ |
Multivariable logistic regression models were subsequently used to examine the associations between the groups identified by RPA and excess SB for both 8–10- and 10–12-year age groups. Models were controlled for children’s age, sex, pubertal status, and child’s BMI percentile, as well as parental education, and parents’ BMI collected at Visit 1. The lowest risk group was the reference category, and the remaining groups were determined based on the group specific variables that were retained, and they were entered in the model as indicator variables.
3. Results
A sample of 294 Montréal participants provided complete data at both visits (Table 2). Prevalence of excess SB was 24.5% (72/294) and 57.1% (166/294) at ages 8–10 (Visit 1) and 10–12 years (Visit 2), respectively. At both time points, a greater proportion of participants who were excessively sedentary were older, had initiated puberty, and had a higher BMI percentile. Furthermore, a lower proportion of participants who were excessively sedentary met PA guidelines (5.6% and 7.7% at Visit 1 and Visit 2, respectively). There were no differences at either Visit 1 or Visit 2 between those classified as excessively sedentary and those who were not with respect to other characteristics examined.
Table 2.
Distribution of characteristics by level of SB among 294 participants, at ages 8–10 years (Visit 1) and 10–12 years (Visit 2).
| Visit 1 Excess SB (n = 72) |
Visit 1 No excess SB (n = 222) |
Visit 2 Excess SB (n = 168) |
Visit 2 No excess SB (n = 126) |
|
|---|---|---|---|---|
| Individual
characteristics Mean/Proportion (95% confidence interval) | ||||
| Age, years, mean | 9.9 (9.8 – 10.1) | 9.4 (9.3–9.5) | 11.9 (11.8–12.0) | 11.2 (11.1–11.4) |
| Sex, boys, % | 55.6 (43.9–67.2) | 57.2 (50.7–63.8) | 50.0 (42.4–57.6) | 65.9 (57.5–74.2) |
| Puberty initiated, % | 31.9 (21.0–42.8) | 15.8 (10.9–20.6) | 75.9 (69.3–82.5) | 46.4 (37.6–55.2) |
| Met physical activity guidelines, % | 5.6 (0.2–10.9) | 40.1 (33.6–46.6) | 7.7 (3.7–11.8) | 38.9 (30.3–47.5) |
| Body mass index percentile, mean | 73.9 (67.4–80.5) | 64.4 (60.7–68.2) | 71.6 (67.3–75.8) | 60.9 (55.9–65.9) |
| >2 h/day of screen time on weekdays, % | 44.4 (32.8–56.0) | 38.5 (32.0–44.9) | 56.0 (48.4–63.5) | 46.8 (38.0–55.6) |
| >2 h/day of screen time on weekends, % | 72.2 (61.7–82.7) | 61.5 (55.0–68.0) | 82.7 (76.9–88.5) | 82.4 (75.7–89.1) |
| Average minutes of SB, mean | 327.0 (321.7–332.2) | 248.5 (243.9–253.0) | 345.2 (339.3–351.0) | 263.9 (259.0–268.9) |
| Family characteristics | ||||
| Household income <25000$, % | 15.5 (7.0–24.0) | 14.4 (9.8–19.1) | 12.5 (7.5–17.5) | 17.6 (10.9–24.3) |
| ≥ 1 parent with a university degree, % | 62.5 (51.1–73.8) | 55.4 (48.8–62.0) | 57.1 (49.6–64.7) | 57.1 (48.4–65.8) |
| Maternal BMI, mean | 29.1 (27.6–30.6) | 29.1 (28.2–29.9) | 29.8 (28.5–31.1) | 29.5 (28.4–30.5) |
| Paternal BMI, mean | 31.6 (30.2–32.9) | 30.2 (29.5–31.0) | 31.2 (30.1–32.3) | 30.9 (29.4–32.4) |
| Neighbourhood characteristics | ||||
| Street connectivity, mean | 77.1 (68.1–86.1) | 75.5 (70.4–80.6) | 73.8 (67.9–79.7) | 78.7 (72.0–85.5) |
| Land use mix, mean | 0.34 (0.31–0.38) | 0.35 (0.32–0.37) | 0.34 (0.32–0.36) | 0.35 (0.32–0.38) |
| High area disadvantage, % | 31.9 (21.1–42.8) | 33.8 (27.5–40.0) | 30.4 (23.3–37.4) | 37.3 (28.8–45.8) |
| Presence of physical disorder, % | 33.3 (22.3–44.3) | 31.2 (24.9–37.4) | 33.5 (26.3–40.8) | 29.3 (21.2–37.4) |
| ≥ 4 parks, % | 20.8 (11.3–30.3) | 19.8 (14.5–25.1) | 17.9 (12.0–23.7) | 23.0 (15.6–30.4) |
| High dwelling density, % | 27.8 (17.3–38.2) | 31.5 (25.3–37.7) | 31.6 (24.5–38.6) | 29.4 (21.3–37.3) |
Five of the 10 factors submitted into RPA were retained in the classification tree generated for outcomes at 8–10 years of age. This resulted in 6 groups, with increasing likelihood of excess SB, based on meeting PA guidelines, weekday screen time, dwelling density, access to parks, and neighbourhood disadvantage. The probability of excess SB and the risk factors characterising each group at ages 8–10 years are presented in Fig. 1. Group 1, representing 32% of the sample, had the lowest probability of excess SB (4%), and was defined by adherence to PA guidelines. Group 6, representing 4% of the sample, had the highest probability of excess SB (73%), and was described by children who simultaneously did not meet PA guidelines, reported >2 h per day of screen time on weekdays, lived in neighbourhoods with a low-density of dwellings and high area disadvantage, and had poor access to parks in their residential neighbourhood.
Fig. 1.
Classification tree of risk factors for excess SB in 294 participants at 8–10 years old.
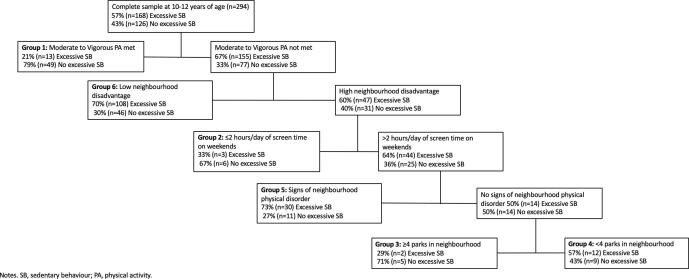
For these same participants, at 10–12 years, the classification tree generated 6 groups based on 5 factors (Fig. 2). Factors retained included meeting PA guidelines, screen time on weekends, access to parks, neighbourhood physical disorder, and neighbourhood disadvantage. Group 1, representing 21% of the sample, had the lowest probability risk of excess SB, and was described by adherence to PA guidelines. Groups 6 and 5 had the highest probability risk of excess SB (70% and 73%, respectively). Group 6, representing 52% of the sample, was described by children who did not adhere to PA guidelines and lived in neighbourhoods with low disadvantage. Group 5, representing 14% of the sample, was described by children who did not adhere to PA guidelines, lived in neighbourhoods with high disadvantage, engaged in >2 h per day of screen time on weekend days, and lived in neighbourhoods with signs of physical disorder.
Fig. 2.
Classification tree of risk factors for excess SB in 294 participants at 10–12 years old.
Compared to 8–10-year-old children from Group 1, those from Groups 2 to 6 had sequentially increasing odds of excess SB. Adjusted odds ratios ranged from 10.3 (95% confidence intervals 3.3–32.1) for Group 2, to 98.2 (95% confidence intervals 16.3–591.9) for Group 6 (Table 3). Similarly, compared to 10–12-year-old children from Group 1, those from Groups 2 to 6 also had sequentially increasing odds of excess SB (Table 4). Findings were strongly consistent, with the varying size of the confidence intervals reflecting the precision of the estimates.
Table 3.
Associations between risk subgroups identified using recursive partitioning analysis and excess sedentary behaviour at ages 8–10 years, among 294 QUALITY participants.
| Excess SB at
8–10 years of age |
||
|---|---|---|
| OR (95% CI) | ORadj‡‡ (95% CI) | |
| Group 1* (n = 93)† | Reference | Reference |
| Group 2 (n = 123)‡ | 9.2 (3.1, 27.0) | 10.3 (3.3, 32.1) |
| Group 3 (n = 32)§ | 11.7 (3.4, 40.2) | 13.6 (3.7, 50.9) |
| Group 4 (n = 3)¶ | 9.5 (1.8, 51.4) | 11.4 (2.0, 68.3) |
| Group 5 (n = 25)# | 14.8 (4.18, 53.4) | 11.3 (2.9, 44.3) |
| Group 6 (n = 11)** | 59.3 (11.3, 312.9) | 98.2 (16.3, 591.9) |
Abbreviations: adj, adjusted; OR, odd ratio; CI, confidence interval.
lowest risk of excess sedentary behaviour.
Group 1 consisted of participants who met moderate to vigorous physical activity guidelines.
Group 2 consisted of participants who did not meet moderate to vigorous physical activity guidelines and engaged in ≤ 2 h/day of screen time on week days.
Group 3 consisted of participants who did not meet moderate to vigorous physical activity guidelines, engaged in >2 h/day of screen time on week days, and resided in a high-dwelling density neighbourhood.
Group 4 consisted of participants who did not meet moderate to vigorous physical activity guidelines, engaged in >2 h/day of screen time on week days, resided in a low-dwelling density neighbourhood, and ≥ 4 parks were located in their residential neighbourhood.
Group 5 consisted of participants who did not meet moderate to vigorous physical activity guidelines, engaged in >2 h/day of screen time on week days, resided in a low-dwelling density neighbourhood, <4 parks were located in their residential neighbourhood, and with low neighbourhood disadvantage.
Group 6 consisted of participants who did not meet moderate to vigorous physical activity guidelines, engaged in >2 h/day of screen time on week days, resided in a low-dwelling density neighbourhood, <4 parks were located in their residential neighbourhood, and with high neighbourhood disadvantage.
Adjusted for child’s age, sex (boy/girl), puberty (initiated/not), body mass index percentile, parent’s education (>1 with university degree/no parent with university degree), mother’s body mass index, and father’s body mass index.
Table 4.
Associations between risk subgroups identified using recursive partitioning analysis and excess sedentary behaviour at ages 10–12 years among 294 QUALITY participants.
| Excess SB at
10–12 years of age |
||
|---|---|---|
| OR (95% CI) | ORadj‡‡ (95% CI) | |
| Group 1* (n = 62)† | Reference | Reference |
| Group 2 (n = 9)‡ | 1.9 (0.4, 8.5) | 1.2 (0.2, 6.4) |
| Group 3 (n = 7)§ | 1.5 (0.3, 8.7) | 1.6 (0.3, 10.1) |
| Group 4 (n = 21)¶ | 5.0 (1.7, 14.5) | 3.8 (1.2, 12.2) |
| Group 5 (n = 41)# | 10.3 (4.1, 25.9) | 7.1 (2.7, 19.1) |
| Group 6 (n = 154)** | 8.9 (4.4, 17.9) | 6.5 (3.0, 13.9) |
Abbreviations: adj, adjusted; OR, odd ratio; CI, confidence interval.
lowest risk of excess sedentary behaviour; † Group 1 consisted of participants who met moderate to vigorous physical activity guidelines.
Group 2 consisted of participants who did not meet moderate to vigorous physical activity guidelines, lived in a high disadvantage neighbourhood, and engaged in ≤ 2 h/day of screen time on weekends.
Group 3 consisted of participants who did not meet moderate to vigorous physical activity guidelines, lived in a high disadvantage neighbourhood, >2 h/day of screen time on weekends, resided in a neighbourhood with no signs of neighbourhood physical disorder, and had ≥ 4 parks were located in their residential neighbourhood.
Group 4 consisted of participants who did not meet moderate to vigorous physical activity guidelines, lived in a high disadvantage neighbourhood, >2 h/day of screen time on weekends, and resided in a neighbourhood with no signs of neighbourhood physical disorder, and had <4 parks were located in their residential neighbourhood.
Group 5 consisted of participants who did not meet moderate to vigorous physical activity guidelines, lived in a high disadvantage neighbourhood, >2 h/day of screen time on weekends, and resided in a neighbourhood with signs of neighbourhood physical disorder;
Group 6 consisted of participants who did not meet moderate to vigorous physical activity guidelines and lived in a low disadvantage neighbourhood;
adjusted for child’s age, sex (boy/girl), puberty (initiated/not), body mass index percentile, parent’s education (>1 with university degree/no parent with university degree), mother’s body mass index, and father’s body mass index.
4. Discussion
We generated risk profiles for excess SB in a sample of 294 children, spanning a key developmental period, during which time youth start to transition towards greater autonomy and increased interaction with their environment. In our sample, the prevalence of excess SB more than doubled over a two-year time span, from 24% at age 8 to 10 years, to 57% at age 10 to 12 years. These proportions mirror dramatic age-related increases in SB reported in other studies (Yang et al., 2019). The final set of risk factors retained at both timepoints shared several similarities, notably with individual-level predictors emerging as more discriminating than neighbourhood-level ones. The various group combinations, and hence the resulting risk profiles differed. However, not meeting PA guidelines was the most discriminating predictor at both time points. The second most discriminating predictor was >2 h a day screen time, but patterns differed by age, as well as by neighbourhood disadvantage (the latter only among 10–12 year olds).
Presence of neighbourhood physical disorder was a risk factor for excess SB for children at ages 10 to 12 years old, but not at ages 8 to 10 years old. Similar findings have been reported in a cross-sectional study of Canadian youth aged 10 to 16 years: greater neighbourhood disorder was associated with increased television viewing, and computer, and video game use (Carson and Janssen, 2012). Children aged 10–12 years who enjoy greater independence and lower parental supervision may have greater freedom and opportunity to play outdoors. However, concerns related to safety associated with neighbourhood disorder may result in minimising time spent in the residential vicinity (Carson and Janssen, 2012; R Core Team, 2013). Consequently, greater neighbourhood disorder may act as a barrier to outdoor play and limit children to indoor pursuits, which are typically dominated by screen time activities.
Neighbourhood disadvantage was a risk factor for high SB at both 8–10 years old and 10–12 years old, albeit in opposing directions. When participants were aged 8–10 years old, living in a neighbourhood with greater disadvantage increased the risk of high SB. Conversely, at 10–12 years of age, living in neighbourhoods with greater disadvantage was associated with a decreased risk of excess SB. These findings may suggest that as children approach adolescence and autonomy increases, neighbourhoods that were not appealing to younger children needing or preferring adult company become benign or even attractive, offering more opportunities and alternatives to sedentary pursuits. Alternately, these diverging associations could be related to different age-related social norms in neighbourhoods with differing area disadvantage.
Engaging in >2 h per day of screen time was a risk factor for excess SB, albeit during weekdays at age 8–10 years (Fig. 1), and during weekends at age 10–12 years. In their study of children aged 9–10 years, using accelerometer data, Steele and colleagues (Steele et al., 2010) observed that more sedentary time was accumulated during the weekends than on weekdays. This may reflect less weekday discretionary time among older children.
Living in neighbourhoods with low dwelling density was associated with an increased risk of excess SB only among children aged 8–10 years. Dwelling density may be especially relevant for younger children as higher dwelling density may reflect a feeling of safety in numbers or of adequate supervision while out in the neighbourhood. In contrast, lower dwelling density may reflect fewer infrastructures for PA, decreased opportunities for outdoor play, fewer nearby friends, and possibly increased concerns about neighbourhood safety among parents of younger children. While studies on housing density and SB are sparse, Vanwolleghem and colleagues (Vanwolleghem et al., 2016) reported that higher residential density is associated with greater daily walking in children. We observed that having reduced access to neighbourhood parks was a risk factor for excess SB at all ages. Other studies have shown positive associations between availability of local parks and children’s PA (Reuben et al., 2020). It is possible that poorer access to parks decreases incentives for outdoor play, further increasing time spent indoors engaged in sedentary pursuits.
Our findings support the notion that characteristics that place children at greater risk of excess SB evolve over time, and they are consistent with studies reporting an age-related increase in excess SB (Stierlin et al., 2015). The strengths of this study include the use of objective, validated accelerometer-based measures of SB (Ridgers et al., 2012, Lubans et al., 2011), and the repeated analyses in a cohort of participants at two developmentally significant timepoints. Furthermore, available data from QUALITY allowed for multiple levels of influence to be examined, as well as use and availability of in-person validated measures of neighbourhood characteristics. Moreover, the use of recursive partitioning allowed us to examine complex interactions arising from the combined impact of multiple individual-, family-, and neighbourhood-level factors. Among the limitations of this study, it should be noted that the study population is based on children at risk for obesity due to parental obesity and that generalisability to a general paediatric population is unknown. Generalisability may also be limited due to the relatively small data set used in this study, which is to be expected given the rigorously phenotyped nature of this cohort. Small samples contribute to the instability of the classification tree, notably resulting in groups with lower numbers of participants. Finally, classification trees are sensitive to minor changes in sample characteristics; using RPA in a different study sample is likely to yield a different classification tree. Nevertheless, the methodological approach used in the analysis is generalizable to other settings and behaviours, and its application across a diversity of populations is encouraged.
5. Conclusions
The findings of this study further highlight pre-adolescence as a critical transition period during which SB increases dramatically. Risk factors related to lifestyle behaviours are generally consistent, and neighbourhood factors generally inconsistent, as children age from late childhood to pre-adolescence. Complex interactions involving developmental, behavioural and contextual factors warrant further investigation in order to devise strategies to effectively prevent or reduce excess sedentary behaviour.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors thank all the children and their families who have generously given their time to this study. Elena Tresierra-Farbridge and Alexa Nordine provided tireless editing and proofing assistance. TAB is an FRQ-S Senior Scholar, MH is a J2 Scholar, and MEM and AVH are J1 Scholars.
Ethics approval and consent to participate
The Ethics Review Boards of Centre Hospitalier Universitaire Sainte-Justine and Institute Universitaire de Cardiologie et de Pneumologie du Québec at Université Laval approved the study. Written informed consent was obtained from the parents, and assent was provided by the children.
Funding
The QUALITY cohort is funded by the Canadian Institutes of Health Research (Nos. OHF-69442, NMD-94067, MOP-97853, MOP-119512), the Heart and Stroke Foundation of Canada (No. PG-040291) and the Fonds de la Recherche du Québec – Santé. QUALITY Residential and School Built Environment complementary studies were funded by HSFC and CIHR, respectively.
References
- Arundell L., Fletcher E., Salmon J., Veitch J., Hinkley T. The correlates of after-school sedentary behavior among children aged 5–18 years: a systematic review. BMC Public Health. 2016;16:58. doi: 10.1186/s12889-015-2659-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin A.J., Corder K., van Sluijs E.M. Bedroom media, sedentary time and screen-time in children: a longitudinal analysis. International Journal of Behavioral Nutrition and Physical Activity. 2013;10(1):1–10. doi: 10.1186/1479-5868-10-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aznar S., Lara M.T., Queralt A., Molina-Garcia J. Psychosocial and Environmental Correlates of Sedentary Behaviors in Spanish Children. Biomed Res Int. 2017;2017:1–6. doi: 10.1155/2017/4728924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bejarano C.M., Carlson J.A., Cushing C.C., Kerr J., Saelens B.E., Frank L.D., Glanz K., Cain K.L., Conway T.L., Sallis J.F. Neighborhood built environment associations with adolescents' location-specific sedentary and screen time. Health Place. 2019;56:147–154. doi: 10.1016/j.healthplace.2019.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle S.J.H., Pearson N., Ross G.M., Braithwaite R. Tracking of sedentary behaviours of young people: a systematic review. Prev. Med. 2010;51(5):345–351. doi: 10.1016/j.ypmed.2010.07.018. [DOI] [PubMed] [Google Scholar]
- Breiman L., Friedman J., Stone C.J., Olshen R.A. CRC Press; 1984. Classification and regression trees. [Google Scholar]
- Bringolf-Isler B., de Hoogh K., Schindler C., Kayser B., Suggs L., Dössegger A., Probst-Hensch N. Sedentary Behaviour in Swiss Children and Adolescents: Disentangling Associations with the Perceived and Objectively Measured Environment. Int J Environ Res Public Health. 2018;15(5):918. doi: 10.3390/ijerph15050918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson V., Janssen I. Neighborhood disorder and screen time among 10–16 year old Canadian youth: a cross-sectional study. International journal of behavioral nutrition and physical activity. 2012;9(1):1–11. doi: 10.1186/1479-5868-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter M.A., Dubois L. Neighbourhoods and child adiposity: a critical appraisal of the literature. Health Place. 2010;16(3):616–628. doi: 10.1016/j.healthplace.2009.12.012. [DOI] [PubMed] [Google Scholar]
- Centre de Recherche du CHUM. 2021 [Available from: http://megaphone.crchum.qc.ca/geonetwork/srv/en/main.home.
- Colley R.C., Garriguet D., Janssen I., Craig C.L., Clarke J., Tremblay M.S. Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011;22(1):15. [PubMed] [Google Scholar]
- Communications Co, Media. Children, adolescents, and the media. Pediatrics. 2013;132(5):958-61. [DOI] [PubMed]
- de Onis M., Onyango A.W., Borghi E., Siyam A., Nishida C., Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Rezende LFM, Lopes MR, Rey-López JP, Matsudo VKR, do Carmo Luiz O. Sedentary behavior and health outcomes: an overview of systematic reviews. PloS one. 2014;9(8):e105620. [DOI] [PMC free article] [PubMed]
- Diez Roux A.V., Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Ding D., Sallis J.F., Kerr J., Lee S., Rosenberg D.E. Neighborhood environment and physical activity among youth a review. Am J Prev Med. 2011;41(4):442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- Dunton G.F., Kaplan J., Wolch J., Jerrett M., Reynolds K.D. Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10(4):393–402. doi: 10.1111/j.1467-789X.2009.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A. Moderate to Vigorous Physical Activity and Sedentary Time and Cardiometabolic Risk Factors in Children and Adolescents JAMA. 307 7 2012 704 12. [DOI] [PMC free article] [PubMed]
- Evenson K.R., Catellier D.J., Gill K., Ondrak K.S., McMurray R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008;26(14):1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- Goon S., Kontulainen S., Muhajarine N. Neighborhood Built Environment Measures and Association with Physical Activity and Sedentary Time in 9–14-Year-Old Children in Saskatoon. Canada. Int J Environ Res Public Health. 2020;17(11):3837. doi: 10.3390/ijerph17113837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinckson E., Cerin E., Mavoa S., Smith M., Badland H., Stewart T., Duncan S., Schofield G. Associations of the perceived and objective neighborhood environment with physical activity and sedentary time in New Zealand adolescents. Int J Behav Nutr Phys Act. 2017;14(1) doi: 10.1186/s12966-017-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann B., Kettner S., Wirt T., Wartha O., Hermeling L., Steinacker J.M., Kobel S. Sedentary time among primary school children in south-west Germany: amounts and correlates. Arch Public Health. 2017;75(1) doi: 10.1186/s13690-017-0230-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia P., Pan X., Liu F., He P., Zhang W., Liu L., Zou Y., Chen L. Land use mix in the neighbourhood and childhood obesity. Obes Rev. 2021;22(S1) doi: 10.1111/obr.v22.S110.1111/obr.13098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R.A., Hinkley T., Okely A.D., Salmon J.o. Tracking physical activity and sedentary behavior in childhood: a systematic review. Am. J. Prev. Med. 2013;44(6):651–658. doi: 10.1016/j.amepre.2013.03.001. [DOI] [PubMed] [Google Scholar]
- Júdice P.B., Magalhães J.P., Rosa G.B., Henriques-Neto D., Hetherington-Rauth M., Sardinha L.B. Sensor-based physical activity, sedentary time, and reported cell phone screen time: A hierarchy of correlates in youth. J Sport Health Sci. 2021;10(1):55–64. doi: 10.1016/j.jshs.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert M., Van Hulst A., O'Loughlin J., Tremblay A., Barnett T.A., Charron H., Drapeau V., Dubois J., Gray-Donald K., Henderson M., Lagace G., Low N.C., Mark S., Mathieu M.-E., Maximova K., McGrath J.J., Nicolau B., Pelletier C., Poirier P., Sabiston C., Paradis G. Cohort profile: the Quebec adipose and lifestyle investigation in youth cohort. Int J Epidemiol. 2012;41(6):1533–1544. doi: 10.1093/ije/dyr111. [DOI] [PubMed] [Google Scholar]
- Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. biometrics. 1977;33(1):159. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- Larouche R., Garriguet D., Gunnell K.E., Goldfield G.S., Tremblay M.S. Outdoor time, physical activity, sedentary time, and health indicators at ages 7 to 14: 2012/2013 Canadian Health Measures Survey. Health Rep. 2016;27(9):3–13. [PubMed] [Google Scholar]
- Leal C., Bean K., Thomas F., Chaix B. Multicollinearity in associations between multiple environmental features and body weight and abdominal fat: using matching techniques to assess whether the associations are separable. Am J Epidemiol. 2012;175(11):1152–1162. doi: 10.1093/aje/kwr434. [DOI] [PubMed] [Google Scholar]
- LeBlanc A.G., Katzmarzyk P.T., Barreira T.V., Broyles S.T., Chaput J.-P., Church T.S., Fogelholm M., Harrington D.M., Hu G., Kuriyan R., Kurpad A., Lambert E.V., Maher C., Maia J., Matsudo V., Olds T., Onywera V., Sarmiento O.L., Standage M., Tudor-Locke C., Zhao P., Tremblay M.S., Sun Q. Correlates of Total Sedentary Time and Screen Time in 9–11 Year-Old Children around the World: The International Study of Childhood Obesity, Lifestyle and the Environment. PLoS ONE. 2015;10(6):e0129622. doi: 10.1371/journal.pone.0129622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart C.M., Wiemken A., Hanlon A., Perkett M., Patterson F. Perceived neighborhood safety related to physical activity but not recreational screen-based sedentary behavior in adolescents. BMC Public Health. 2017;17(1):722. doi: 10.1186/s12889-017-4756-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotoski L., Fuller D., Stanley K.G., Rainham D., Muhajarine N. The Effect of Season and Neighbourhood-Built Environment on Home Area Sedentary Behaviour in 9–14 Year Old Children. Int J Environ Res Public Health. 2021;18(4):1968. doi: 10.3390/ijerph18041968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubans DR, Hesketh K, Cliff D, Barnett L, Salmon J, Dollman J, et al. A systematic review of the validity and reliability of sedentary behaviour measures used with children and adolescents. Obesity reviews. 2011;12(10):781-99. [DOI] [PubMed]
- Parajára M.d.C., de Castro B.M., Coelho D.B., Meireles A.L. Are neighborhood characteristics associated with sedentary behavior in adolescents? A systematic review. Int J Environ Health Res. 2020;30(4):388–408. doi: 10.1080/09603123.2019.1597833. [DOI] [PubMed] [Google Scholar]
- Parker K.E., Salmon J.o., Villanueva K., Mavoa S., Veitch J., Brown H.L., Timperio A. Ecological correlates of activity-related behavior typologies among adolescents. BMC Public Health. 2019;19(1) doi: 10.1186/s12889-019-7386-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquet C., Cargo M., Kestens Y., Daniel M. Reliability of an instrument for direct observation of urban neighbourhoods. Landscape Urban Plann. 2010;97(3):194–201. [Google Scholar]
- Pearson N., Haycraft E., P. Johnston J., Atkin A.J. Sedentary behaviour across the primary-secondary school transition: A systematic review. Prev Med. 2017;94:40–47. doi: 10.1016/j.ypmed.2016.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. 2013.
- Reuben A., Rutherford G.W., James J., Razani N. Association of neighborhood parks with child health in the United States. Prev. Med. 2020;141:106265. doi: 10.1016/j.ypmed.2020.106265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridgers N.D., Salmon J., Ridley K., O'Connell E., Arundell L., Timperio A. Agreement between activPAL and ActiGraph for assessing children's sedentary time. International Journal of Behavioral Nutrition and Physical Activity. 2012;9(1):1–8. doi: 10.1186/1479-5868-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberge J.-B., Perkova P., Contreras G., Kakinami L., Henderson M., Barnett T.A. Validation of desk-based audits to monitor the obesogenic potential of neighbourhoods: a pilot study in the QUALITY cohort. BMC Public Health. 2021 doi: 10.1186/s12942-022-00301-8. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J.F., Owen N., Fisher E. Ecological models of health behavior. Health behavior: Theory, research, and practice. 2015;5(43–64) [Google Scholar]
- Sallis J.F., Conway T.L., Cain K.L., Carlson J.A., Frank L.D., Kerr J., Glanz K., Chapman J.E., Saelens B.E. Neighborhood built environment and socioeconomic status in relation to physical activity, sedentary behavior, and weight status of adolescents. Prev Med. 2018;110:47–54. doi: 10.1016/j.ypmed.2018.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. Low income cut-offs (1992 base) after tax 2015 [Available from: http://www.statcan.gc.ca/pub/75f0002m/2013002/tbl/tbl01-eng.htm.
- Steele R.M., van Sluijs E.M., Sharp S.J., Landsbaugh J.R., Ekelund U., Griffin S.J. An investigation of patterns of children's sedentary and vigorous physical activity throughout the week. International Journal of Behavioral Nutrition and Physical Activity. 2010;7(1):1–8. doi: 10.1186/1479-5868-7-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stierlin A.S., De Lepeleere S., Cardon G., Dargent-Molina P., Hoffmann B., Murphy M.H., Kennedy A., O’Donoghue G., Chastin S.FM., De Craemer M. A systematic review of determinants of sedentary behaviour in youth: a DEDIPAC-study. Int J Behav Nutr Phys Act. 2015;12(1) doi: 10.1186/s12966-015-0291-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strobl C., Malley J., Tutz G. An introduction to recursive partitioning: rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychol. Methods. 2009;14(4):323–348. doi: 10.1037/a0016973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Therneau T, Atkinson B, Ripley B, Ripley MB. Package ‘rpart’. Available online: cran ma ic ac uk/web/packages/rpart/rpart pdf (accessed on 20 April 2016). 2015.
- Timperio A., Crawford D., Ball K., Salmon J.o. Typologies of neighbourhood environments and children's physical activity, sedentary time and television viewing. Health Place. 2017;43:121–127. doi: 10.1016/j.healthplace.2016.10.004. [DOI] [PubMed] [Google Scholar]
- Tremblay M.S., LeBlanc A.G., Kho M.E., Saunders T.J., Larouche R., Colley R.C., Goldfield G., Gorber S. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. International journal of behavioral nutrition and physical activity. 2011;8(1):98. doi: 10.1186/1479-5868-8-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay M.S., Carson V., Chaput J.P., Connor Gorber S., Dinh T., Duggan M., et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S311–S327. doi: 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- Tremblay M.S., Aubert S., Barnes J.D., Saunders T.J., Carson V., Latimer-Cheung A.E., Chastin S.F.M., Altenburg T.M., Chinapaw M.J.M. Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1) doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hulst A., Roy-Gagnon M.-H., Gauvin L., Kestens Y., Henderson M., Barnett T.A. Identifying risk profiles for childhood obesity using recursive partitioning based on individual, familial, and neighborhood environment factors. Int J Behav Nutr Phys Act. 2015;12(1):17. doi: 10.1186/s12966-015-0175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanwolleghem G., Schipperijn J., Gheysen F., Cardon G., De Bourdeaudhuij I., Van Dyck D. Children’s GPS-determined versus self-reported transport in leisure time and associations with parental perceptions of the neighborhood environment. Int. J. Health Geographics. 2016;15(1):1–12. doi: 10.1186/s12942-016-0045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Cao C., Kantor E.D., Nguyen L.H., Zheng X., Park Y., Giovannucci E.L., Matthews C.E., Colditz G.A., Cao Y. Trends in Sedentary Behavior Among the US Population, 2001–2016. JAMA. 2019;321(16):1587. doi: 10.1001/jama.2019.3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagorskas J. GIS-based Modelling and Estimation of Land Use Mix in Urban Environment. International Journal of Environmental Science. 2016;1:284–293. [Google Scholar]