Highlights
-
•
Uptake of HPV vaccination & testing was abysmally low despite good knowledge of it.
-
•
Unvaccinated and untested women were more willing to accept HPV test than vaccination.
-
•
Knowing CC patient, being employed & unmarried predicted HPV vaccination & testing.
-
•
Recommendation by HCP & friend/relative were motivators for HPV vaccination & test.
-
•
Fear, cost & non-recommendation by HCP were barriers to HPV vaccination & testing.
Abbreviations: AOR, Adjusted odd ratio; CC, Cervical cancer; CI, Confidence interval; COR, Crude odd ratio; HCP, Healthcare provider; HDI, Human development indices; HPV, Human papillomavirus; HrHPV, High risk HPV; IQR, Interquartile range; LMIC, Low and middle income countries; LrHPV, Low risk HPV; P-value, Probability value; SD, Standard deviation; SPSS, Statistical Package for Social Sciences; %, Percentage
Keywords: HPV vaccination; HPV testing; Predictors; Motivators; Barriers; Cervical cancer; Lagos, Nigeria
Abstract
Human papillomavirus (HPV) vaccination and HPV based cervical screening are scientifically proven ways to prevent and eliminate cervical cancer (CC). Unfortunately, these measures are yet to be widely accepted or utilized. Our study aimed to explore the individual-related factors that predict HPV vaccination and testing, its motivating factors and barriers among urban women in Lagos, Nigeria. This was a descriptive cross-sectional study among 208 consenting women who attended a community health awareness program in Surulere, Lagos, Nigeria, in September 2019. Structured questionnaires were interviewer administered and analysis was done using SPSS version 23. The uptake of HPV vaccination and testing was 29.0% and 3.0% respectively. Being employed [adjusted odds ratio (AOR) = 60.45, CI = 10.64–343.46, P < 0.001] and unmarried (AOR = 33.33, CI = 12.5–100.0, P < 0.001) predicted HPV vaccination uptake while being unmarried was the only predictor of uptake of HPV testing [crude odds ratio (COR) = 7.69, CI = 1.01–100.00, P = 0.039]. Knowing someone with CC (AOR = 21.64, CI = 4.87–96.16, P < 0.001) and being unmarried (AOR = 5.56, CI = 1.45–20.00, P = 0.012) predicted increased willingness to be vaccinated. Being unmarried (AOR = 5.26, CI = 1.89–14.29, P = 0.002) and knowing someone with CC (AOR = 6.41, CI = 2.68–15.33, P < 0.001) predicted willingness to do HPV testing. Recommendation by healthcare provider (HCP), friends/relatives and media were major motivators for HPV vaccination & testing while fear, cost, no recommendation by HCP, inaccessibility & lack of awareness were major barriers. There is need to urgently address these identified factors that affect HPV vaccination and testing in order to improve its acceptability and uptake rate in our environment.
1. Introduction
Cervical cancer (CC) is a preventable malignancy with an easily detectable premalignant phase. However, the burden of CC has remained high in many low and middle income countries (LMIC) including Nigeria. The current GLOBOCAN statistics showed that 77.6% and 80.9% of all new cases and deaths due to CC respectively occurred in countries with low and medium human development indices (HDI) particularly in Asia & Africa. In these countries, CC is the 2nd most common female malignancy after breast cancer, in contrast to countries with very high HDI where it ranks as the 11th most common female cancer (Sung et al., 2021).
The discovery of Human papillomavirus (HPV) as the necessary cause of CC has profoundly transformed the practice of CC prevention and screening (Bhatla and Singhal, 2020, Chrysostomou et al., 2018). Persistent high risk HPV (hrHPV) infection is associated with risk of developing high grade pre-cancer lesion which progresses to CC if untreated. Seventy percent of CC are attributed to hrHPV 16 & 18 infections, while additional 20% are attributed to hrHPV 31, 33, 45, 52, 58 (Chrysostomou et al., 2018, Cervical Cancer Screening and Prevention, 2016). This has led to the development of vaccines targeting these common strains as a primary preventive measure (Bhatla and Singhal, 2020). Gardasil, a tetravalent vaccine targeting hrHPV 16 & 18 and low risk HPV (lrHPV) 6 &11 was first licensed for use in 2006. This was followed by Cervarix, a bivalent vaccine against hrHPV 16 & 18 in 2007 and Gardasil 9, a nonavalent vaccine that protects against seven hrHPVs (16, 18, 31, 33, 45, 52, 58) and two lrHPVs (6 & 11) in 2014 (Cervical Cancer Screening and Prevention, 2016, Alsous et al., 2021).
The World Health Organization (WHO) recommends that all girls within the ages of 9 to 14 years should be vaccinated and countries with high CC burden should include HPV vaccination into their country’s national immunization program if it is feasible, sustainable and cost-effective (World Health Organization (WHO), 2016). As at June 2020, only 31% of African countries had commenced national HPV vaccination program compared to 85% and 77% in America and Europe respectively (Bruni et al., 2021). Rwanda was the first African country to start a national HPV immunization program while Senegal recently became the first in West Africa (Kuehn, 2019). Nigeria is yet to commence her national immunization program despite her proposed target to attain high coverage among children aged 9-13yrs by year 2022 (Nigeria National Cancer Control Plan (NNCCP), 2018). Primary prevention of pre-cancer lesions and CC with HPV vaccination alone cannot completely prevent or eliminate CC and its precursor lesions. This is because the currently available HPV vaccines only protect against 70–90% of the hrHPV serotypes causing CC. Hence, the need for continued CC screening to detect early precursor lesions.
Over the years, CC screening with cytology has led to significant reduction in the incidence of CC in many developed countries (Bhatla and Singhal, 2020, Velentzis et al., 2017). However, following the discovery of HPV as the cause of CC, focus has shifted to the use of HPV testing for CC screening. This is due to some limitations of cervical cytology such as low sensitivity, high false negativity, subjective interpretation by cyto-pathologist and the need for frequent repeated testing (Bhatla and Singhal, 2020, Chrysostomou et al., 2018, Annekathryn, 2015). There has been a gradual paradigm shift in the use of HPV testing from reflex testing to co-testing with cytology and now to primary HPV testing (Bhatla and Singhal, 2020, Cervical Cancer Screening and Prevention, 2016) due to its higher sensitivity at detecting high grade lesions (Bhatla and Singhal, 2020, Mustafa et al., 2016). A negative HPV test gives more assurance of reduced risk of CC, thus allows for longer interval for screening compared to cytology or visual inspection with acetic acid (Bhatla and Singhal, 2020, Chrysostomou et al., 2018, Velentzis et al., 2017). This is particularly important in LMIC where multiple clinic visits and follow-up for repeated screening is not practicable. In addition, the use of HPV testing is more reliable in detecting glandular and precursor lesions of cervical adenocarcinomas compared to cytology (Bhatla and Singhal, 2020, Annekathryn, 2015). These advantages make HPV testing a more cost-effective screening strategy in any country irrespective of her economic status (Bhatla and Singhal, 2020). The Society of Obstetrics and Gynaecology of Nigeria (SOGON) clinical practice guideline on the prevention of cervical cancer in Nigeria recommended the use of HPV testing as the primary cervical screening strategy and the use of HPV vaccination for all girls and women between the ages of 9 and 26 years as primary preventive strategy (Akinola et al., 2018). Currently, HPV vaccination and testing are only offered by few hospitals in Lagos, Nigeria at high cost to the patient. HPV testing is infrequently recommended by clinicians to evaluate abnormal cytology rather than been used as a primary screening modality, while HPV vaccination are administered to interested clients by healthcare providers on one-on-one basis.
Several factors influence the acceptability and uptake of HPV vaccination and testing in countries where there are no organized cervical cancer prevention program. Lack of governmental commitment, individual, community and health system related factors affect the uptake of these preventive measures (Nabirye et al., 2020, Kisaakye et al., 2018, Santhanes et al., 2018, Harun et al., 2019). These factors are key determinants of acceptability and uptake of HPV vaccination and testing. The study aimed to explore the individual-related factors that predict the uptake and willingness to accept these preventive measures among urban women in Lagos, Nigeria. It also assessed the factors that served as barriers and motivators for these measures.
2. Methods
2.1. Study design and population
This was a cross-sectional descriptive study conducted among women living at Masha area in Surulere, Lagos, Nigeria, during a community based health awareness program in September 2019. The study area comprised of communities such as Oninigogoro, Shitta, Obele, Lawanson, Kilo, Aguda and Iponri. Women living in these communities were invited to participate in the health awareness program through their community leaders, local residential associations, women societies and religious leaders over a period of one month prior to the health program. Study participants were recruited by convenient sampling method. All women who attended the health awareness program were informed about the purpose of the study and those within the age of ≥ 18 years who gave informed consent were recruited to participate in the study. Women below the age of 18 years and who were unwilling to participate in the study were excluded from the study. Ethical approval for the study was obtained from the Lagos University Teaching Hospital ethics committee (ADM/DCST/HREC/APP/3454). Sample size was calculated using appropriate formula (n = Z2 p (1 − p)/d2) (Charan and Biswas, 2013) with an absolute error margin of 5% (d = 0.05), type 1 error of 5% (Z = 1.96), and uptake of HPV vaccination (p) of 13.3% (Chiang et al., 2016). The calculated minimum sample size was 177 and after adjusting for a non-response rate of 15%, the final sample size was 204.
2.2. Instrument of survey and data collection
The instrument of survey was a structured questionnaire designed to elicit information on participants’ socio-demographic characteristics, reproductive characteristics, knowledge and perception about HPV, HPV vaccination and HPV testing. Information on the uptake of HPV vaccination and testing, motivating factors and barriers to uptake of HPV vaccination and testing were obtained. Willingness to receive HPV vaccination, to vaccinate daughter and to do HPV testing were also assessed. Knowledge and perception score was calculated for HPV, HPV vaccination and HPV testing by using a similar scoring system used in previous study (Okunowo and Adaramoye, 2018). The questionnaires were interviewer administered by trained personnel. Details on the information obtained, the scoring system and its categorization are documented in the appendix A “Instrument of the survey, data collection and analysis” in the supplementary file.
2.3. Data analysis
Participants’ data was anonymized and entered into Excel spreadsheet and data cleaning and validation was done. Data was analysed using Statistical Package for Social Sciences (SPSS) version 23.0, IBM Corp., Armonk, NY, USA. Test for normality was done using the Shapiro-Wilk’s test. Descriptive statistics were computed for all relevant data and presented in tables or charts. Normally distributed and skewed continuous variables were expressed as mean with standard deviation (SD) and median with interquartile range (IQR) respectively. Analysis was stratified based on these dichotomized outcomes. Bivariate analysis was done using Student’s t-test (or Mann Whitney U test) and Pearson’s Chi- square test or Fischer’s exact test. Multivariable regression analysis was conducted using stepwise backward elimination technique for variables with P-value < 0.2. The level of statistical significance was set at a P-value < 0.05 and confidence interval at 95%. Comprehensive information on the data analysis process is included in the appendix A “Instrument of the survey, data collection and analysis” in the supplementary file.
3. Results
Two hundred and eight (208) eligible women participated in the study out of 245 women that attended the health awareness program giving a response rate of 84.9%. Among these, 200 (96.2%) participants had complete data and were included in the analysis.
3.1. Socio-demographic & reproductive characteristics of study participants
Table 1 shows the socio-demographic and reproductive characteristics of the study participants. The mean age of the participants was 41.9 ± 13.1 years (range 21–65 years). Most of the participants were married [60.0% (120/200)] with tertiary education [76.0% (152/200)], skilled occupation [55.5% (111/200)] and median parity of 2 (0–3).
Table 1.
Socio-demographic characteristics.
| Variables | Frequency (n = 200) | Percentage (%) |
|---|---|---|
| Age (yrs) | ||
| 21 – 30 | 40 | 20.0 |
| 31 – 40 | 79 | 39.5 |
| 41 – 50 | 27 | 13.5 |
| 51 – 60 | 19 | 9.5 |
| >60 | 35 | 17.5 |
| Mean age = 41.9 ± 13.1 | Range = 21 – 65 | |
| Tribe | ||
| Hausa | 6 | 3.0 |
| Igbo | 57 | 28.5 |
| Yoruba | 137 | 68.5 |
| Occupation | ||
| Skilled | 111 | 55.5 |
| Semi-skilled | 56 | 28.0 |
| Unskilled | 5 | 2.5 |
| Unemployed | 28 | 14.0 |
| Religion | ||
| Christianity | 154 | 77.0 |
| Islam | 46 | 23.0 |
| Education | ||
| None | 9 | 4.5 |
| Primary | 5 | 2.5 |
| Secondary | 34 | 17.0 |
| Tertiary | 152 | 76.0 |
| Marital status | ||
| Single | 45 | 22.5 |
| Married | 120 | 60.0 |
| Separated | 5 | 2.5 |
| Widow | 30 | 15.0 |
| Parity | ||
| 0 | 56 | 28.0 |
| 1 – 4 | 122 | 61.0 |
| ≥5 | 22 | 11.0 |
| Median parity = 2 (IQR = 0–3) | Range = 0 – 7 |
3.2. Knowledge and perception of HPV infection, its related disease (cervical cancer) and its preventive measures
The detail information on participants’ knowledge and perception about HPV & its associated disease (cervical cancer), HPV vaccination and HPV testing is shown on Tables S1, S2 and S3 respectively in the supplementary file. Ninety-one percent (182/200) of the participants had good knowledge and perception about HPV testing with mean score of 3.4 ± 1.2 (range 0–4) while only 76.5% (153/200) of participants had good knowledge and perception about HPV vaccination with mean score of 4.5 ± 2.5 (range 0–6). The mean total knowledge and perception score was 12.6 ± 5.7, with 78.5% (157/200) having good knowledge and perception about HPV & its prevention (Table 2). The sources of information on HPV & its preventive measures were enumerated on Table S5 in the supplementary file. Majority of the participants [70% (140/200)] knew someone who had cervical cancer disease (Table S6 in the supplementary file).
Table 2.
Knowledge and perception about HPV & its preventive practice
| Variables | Frequency n = 200 | Percent (%) |
|---|---|---|
| Knowledge & perception about HPV & its infection | ||
| Good | 122 | 61.0 |
| Poor | 78 | 39.0 |
| Mean knowledge score = 4.7 ± 3.6 Range = 0 – 8 Knowledge & perception about HPV vaccination |
||
| Good | 153 | 76.5 |
| Poor | 47 | 23.5 |
| Mean knowledge score = 4.5 ± 2.5 Range = 0 – 6 |
||
| Knowledge & perception about HPV testing | ||
| Good | 182 | 91.0 |
| Poor | 18 | 9.0 |
| Mean knowledge score = 3.4 ± 1.2 Range = 0 – 4 |
||
| Knowledge & perception about HPV & its preventive practices | ||
| Good | 157 | 78.5 |
| Poor | 43 | 21.5 |
| Mean knowledge score = 12.6 ± 5.7 Range = 0 – 18 |
3.3. Willingness and uptake of HPV vaccination and testing
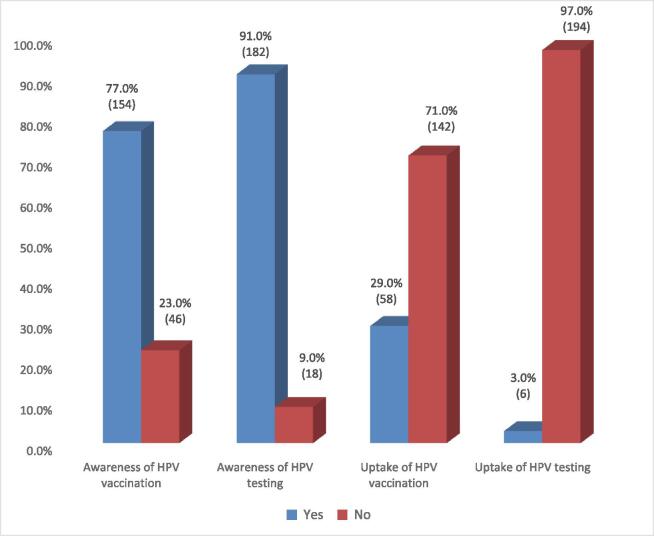
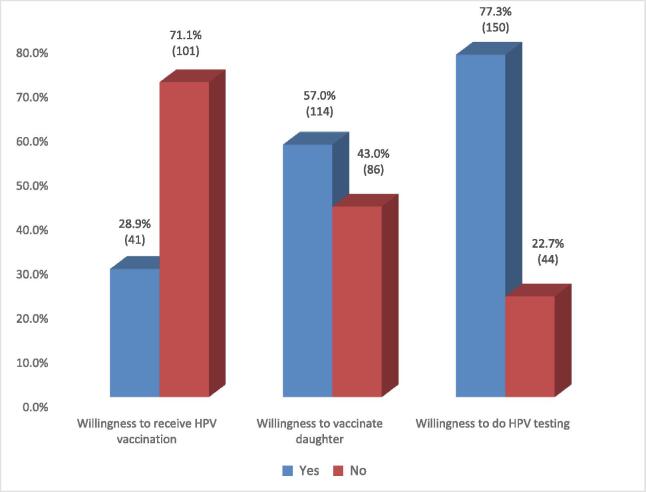
Participants had high level of awareness of HPV vaccination and testing with higher awareness rate for HPV testing [91.0% (182/200)] than HPV vaccination [77.0% (154/200)]. On the contrary, the uptake of HPV vaccination and testing was very low among the participants with HPV testing accounting for lower uptake [3.0% (6/200)] than HPV vaccination [29.0% (58/200)] (Fig. 1). Among the no-uptake group, respondents were more willing to do HPV test than receiving HPV vaccine [77.3% (150/194) vs 28.9% (41/142) respectively]. Only 57% (114/200) of the participants were willing to vaccinate their daughters (Fig. 2).
Fig. 1.
Awareness and uptake of HPV vaccination and testing among study participants.
Fig. 2.
Willingness of participants to receive HPV vaccination, vaccinate daughter and to do HPV testing.
3.4. Motivators and barriers to uptake of HPV vaccination and testing
The leading motivations for the uptake of HPV vaccination were HCP recommendation [63.8% (37/58)], friend/relative recommendation [34.5% (20/58)], knowledge of someone who has taken the vaccine [6.9% (4/58)] and recommendation by electronic media [5.2% (3/58)]. Likewise, motivators for doing HPV testing were HCP’s recommendation [83.3% (5/6)], friend/relative recommendation [33.3% (2/6)], recommendation by electronic media [33.3% (2/6)] and fear of developing CC [33.3% (2/6)] (Table 3). Barriers to the uptake of HPV vaccination and testing are enumerated in Table S4 in the supplementary file. The most common barriers to HPV vaccination were fear of vaccine [60.6% (86/142)], not knowing where to get vaccine [52.1% (74/142)], negative recommendation by people [51.4% (73/142)] and no recommendation by HCP [38.0% (54/142)]. Likewise, lack of recommendation by HCP [65.5% (127/194)], high cost & non-affordability [53.1% (103/194)], not knowing where to do test [41.8% (81/194)] and perception that method of doing test is embarrassing [36.6% (71/194)] were the major barriers to HPV testing.
Table 3.
Motivations for uptake of HPV vaccination and testing.
| Frequency | Percent (%) | |
|---|---|---|
| Motivations for receiving HPV vaccination (multiple response) | n = 58 | |
| Recommendation by HCP | 37 | 63.8 |
| Recommendation by friend or relative | 20 | 34.5 |
| Knowledge of someone who has taken the vaccine | 4 | 6.9 |
| Recommendations by electronic media* | 3 | 5.2 |
| Recommendation by print media# | 1 | 1.7 |
| Recommendation by workshops/Seminars/Outreaches | 1 | 1.7 |
| Recommendation by religious bodies¥ | 1 | 1.7 |
| Partner’s support | 1 | 1.7 |
| Motivations for doing HPV testing (multiple response) | n = 6 | |
| Recommendation by HCP | 5 | 83.3 |
| Recommendation by friend or relative | 2 | 33.3 |
| Recommendations by electronic media* | 2 | 33.3 |
| Fear of developing cervical cancer | 2 | 33.3 |
| Knowledge of someone that has done the test | 1 | 16.7 |
| Knowledge of someone who has cervical cancer | 1 | 16.7 |
| Affordability | 1 | 16.7 |
| Partner’s support | 1 | 16.7 |
*Televisions/radios/internet/social media.
#Newspapers/magazines/books.
¥Churches/Mosques.
3.5. Univariable predictors of HPV vaccination and testing
Table 4 shows the univariate predictors of the uptake of HPV vaccination and testing including willingness to vaccinate daughter, to receive HPV vaccination and to do HPV testing among the no-uptake participants. Being unmarried [crude odd ratio (COR) = 25.00, CI = 10.00–50.00, P < 0.001], having no prior pregnancy (COR = 6.67, CI = 3.33–14.29, P < 0.001), tertiary education (COR = 6.06, CI = 2.07–17.78, P < 0.001), counselling by HCP (COR = 4.59, 1.55–13.55, P = 0.003) and knowing someone with CC (COR = 4.34, CI = 1.84–10.25, P < 0.001) were significantly associated with increased odds of uptake of HPV vaccination. Likewise, being employed (COR = 3.92, CI = 1.13–13.53, P = 0.021), good knowledge and perception of HPV & its prevention (COR = 3.87, 1.44–10.42, P = 0.005), awareness of HPV vaccine (COR = 3.40, CI = 1.35–8.53, P = 0.007) and Yoruba ethnicity (COR = 3.34, CI = 1.52–7.34, P = 0.002) were significantly associated with increased uptake of HPV vaccination. Factors significantly associated with increased willingness to receive HPV vaccination among unvaccinated women were knowing someone with CC (COR = 20.30, CI = 4.65–88.63, P < 0.001), good knowledge and perception of HPV & its prevention (COR = 10.97, CI = 2.50–48.11, P < 0.001), awareness of HPV vaccine (COR = 11.95, CI = 2.73–52.36) and being unmarried (COR = 4.76, CI = 1.33–16.67, P = 0.010). With regards to willingness to vaccinate daughters, knowing someone with CC (COR = 20.88, CI = 9.01–48.40, P < 0.001), good knowledge and perception of HPV & its prevention (COR = 13.88, CI = 5.49–35.07, P < 0.001) and awareness of HPV vaccine (COR = 12.96, CI = 5.40–31.11, P < 0.001) were significantly associated with increased willingness to vaccinate daughter. Other factors included being employed (COR = 2.79, CI = 1.22–6.42, P = 0.013), Yoruba ethnicity (COR = 2.61, CI = 1.41–4.81, P = 0.002), counselling by HCP (COR = 2.27, CI = 1.11–4.64, P = 0.022), being unmarried (COR = 2.22, CI = 1.23–4.00, P = 0.007) and tertiary education (COR = 2.19, CI = 1.13–4.25, P = 0.019).
Table 4.
Univariate predictors of HPV vaccination and testing.
| Variables |
Predictors of uptake of HPV vaccination |
Predictors of willingness to be
vaccinated |
Predictors of willingness to vaccinate
daughter |
Predictors of uptake of HPV testing |
Predictors of willingness to do HPV
testing |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| COR | 95% CI | P value | COR | 95% CI | P value | COR | 95% CI | P value | COR | 95% CI | P value | COR | 95% CI | P value | |
| Age | |||||||||||||||
| ≤ 35 years | 0.71 | 0.37 – 1.34 | 0.286 | 1.02 | 0.49–2.13 | 0.959 | 1.08 | 0.61–1.92 | 0.794 | 3.32 | 0.59–18.55 | 0.207 | 0.74 | 0.37–1.47 | 0.387 |
| > 35 years | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Tribe | |||||||||||||||
| Yoruba | 3.34 | 1.52 – 7.34 | 0.002 | 1.75 | 0.80–3.82 | 0.158 | 2.61 | 1.41–4.81 | 0.002 | 0.45 | 0.09–2.28 | 0.382 | 0.69 | 0.32–1.47 | 0.333 |
| Others | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Occupation | |||||||||||||||
| Employed | 3.92 | 1.13 – 13.53 | 0.021 | 1.80 | 0.63–5.18 | 0.270 | 2.79 | 1.22–6.42 | 0.013 | 0.31 | 0.05–1.78 | 0.200 | 0.58 | 0.19–1.79 | 0.340 |
| Unemployed | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Religion | |||||||||||||||
| Christianity | 0.48 | 0.24 – 0.96 | 0.036 | 1.55 | 0.58–4.18 | 0.383 | 0.73 | 0.37–1.44 | 0.368 | 1.51 | 0.17–13.26 | 1.000 | 1.33 | 0.62–2.87 | 0.466 |
| Islam | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Educational status | |||||||||||||||
| Tertiary education | 6.06 | 2.07 – 17.78 | < 0.001 | 2.22 | 0.93–5.33 | 0.070 | 2.19 | 1.13–4.25 | 0.019 | 1.60 | 0.18–14.03 | 1.000 | 1.06 | 0.49–2.30 | 0.892 |
| Secondary & below | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Marital status | |||||||||||||||
| Unmarried | 25.00 | 10.00–50.00 | < 0.001 | 4.76 | 1.33–16.67 | 0.010 | 2.22 | 1.23–4.00 | 0.007 | 7.69 | 1.01–100.00 | 0.039 | 6.67 | 2.56–16.67 | < 0.001 |
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Pregnancy status | |||||||||||||||
| Never pregnant | 6.67 | 3.33–14.29 | < 0.001 | 0.66 | 0.20–2.13 | 0.493 | 1.82 | 0.91–3.57 | 0.087 | 1.67 | 0.29–9.09 | 0.627 | 3.70 | 1.27–11.11 | 0.012 |
| Ever pregnant | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Knows someone with cervical cancer | |||||||||||||||
| Yes | 4.34 | 1.84 – 10.25 | < 0.001 | 20.30 | 4.65–88.63 | < 0.001 | 20.88 | 9.01–48.40 | < 0.001 | 0.85 | 0.15–4.79 | 1.000 | 10.86 | 5.03–23.46 | < 0.001 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Knowledge & perception of HPV & its prevention | |||||||||||||||
| Good | 3.87 | 1.44 – 10.42 | 0.005 | 10.97 | 2.50–48.11 | <0.001 | 13.88 | 5.49–35.07 | < 0.001 | 1.38 | 0.16–12.15 | 1.000 | 3.64 | 1.73–7.64 | < 0.001 |
| Poor | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Counselled by healthcare workers | |||||||||||||||
| Yes | 4.59 | 1.55 – 13.55 | 0.003 | 0.86 | 0.38–1.97 | 0.724 | 2.27 | 1.11–4.64 | 0.022 | 1.26 | 0.14–11.08 | 1.000 | 3.16 | 1.48–6.73 | 0.002 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Awareness of HPV vaccine | |||||||||||||||
| Yes | 3.40 | 1.35 – 8.53 | 0.007 | 11.95 | 2.73–52.36 | < 0.001 | 12.96 | 5.40–31.11 | < 0.001 | – | – | – | – | – | – |
| No | 1.00 | 1.00 | 1.00 | – | – | ||||||||||
| Awareness of HPV testing | |||||||||||||||
| Yes | – | – | – | – | – | – | – | – | – | 0.48 | 0.05–4.35 | 1.000 | 1.47 | 0.49–4.44 | 0.545 |
| No | – | – | – | 1.00 | 1.00 | ||||||||||
COR = Crude odd ratio; #CI = Confidence interval.
Marital status was the only significant factor associated with the uptake of HPV testing. Unmarried women were eight times likely to undergo HPV testing compared to their married counterparts (COR = 7.69, CI = 1.01–100.00, P = 0.039). Knowing someone with CC (COR = 10.86, CI = 5.03–23.46, P < 0.001) and being unmarried (COR = 6.67, CI = 2.56–16.67, P < 0.001) were associated with the highest odds of willingness to do HPV testing. Having no prior pregnancy (COR = 3.70, CI = 1.27–11.11, P = 0.012), good knowledge and perception about HPV & its prevention (COR = 3.64, CI = 1.73–7.64, P < 0.001) and counselling by HCP (COR = 3.16, CI = 1.48–6.73, P = 0.002) were also significantly associated with willingness to do HPV testing in the future.
3.6. Multivariable predictors of HPV vaccination and testing
After modelling, the independent predictors of the uptake of HPV vaccination were being employed [adjusted odd ratio (AOR) = 60.45, CI = 10.64–343.46, P < 0.001], being unmarried (AOR = 33.33, CI = 12.5–100.0, P < 0.001), tertiary education (AOR = 12.87, CI = 3.10–53.43, P < 0.001) and having no prior pregnancy (AOR = 4.35, CI = 1.20–16.67, P = 0.025). Likewise, knowing someone with CC and being unmarried significantly predicted increased willingness to receive HPV vaccination among unvaccinated women (AOR = 21.64, CI = 4.87–96.16, P < 0.001 and AOR = 5.56, CI = 1.45–20.00, P = 0.012 respectively). The factors that significantly predicted willingness to vaccinate daughters were knowing someone with CC (AOR = 24.99, CI = 10.24–61.00, P < 0.001), being employed (AOR = 4.78, CI = 1.78–12.86, P = 0.002) and Yoruba ethnicity (AOR = 2.58, CI = 1.19–5.61, P = 0.017). Unmarried status remained the only significant predictor of the uptake of HPV testing while being unmarried and knowing someone with CC were the only significant predictors of willingness to do HPV testing among untested women (AOR = 5.26, CI = 1.89–14.29, P = 0.002 & AOR = 6.41, CI = 2.68–15.33, P < 0.001 respectively) (Table 5).
Table 5.
Multivariate prediction models for HPV vaccination and testing.
| Variables |
Predictors of uptake of HPV vaccination |
Predictors of willingness to be
vaccinated |
Predictors of willingness to vaccinate
daughter |
Predictors of uptake of HPV testing |
Predictors of willingness to do HPV
testing |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | P value | AOR | 95% CI | P value | AOR | 95% CI | P value | AOR | 95% CI | P value | AOR | 95% CI | P value | |
| Tribe | |||||||||||||||
| Yoruba | – | – | – | – | – | – | 2.58 | 1.19–5.61 | 0.017 | – | – | – | – | – | – |
| Others | 1.00 | ||||||||||||||
| Occupation | |||||||||||||||
| Employed | 60.45 | 10.64–343.46 | < 0.001 | – | – | – | 4.78 | 1.78–12.86 | 0.002 | – | – | – | – | – | – |
| Unemployed | 1.00 | 1.00 | |||||||||||||
| Educational status | |||||||||||||||
| Tertiary education | 12.87 | 3.10 – 53.43 | < 0.001 | 2.03 | 0.76–5.43 | 0.161 | 2.01 | 0.85–4.78 | 0.114 | – | – | – | – | – | – |
| Secondary & below | 1.00 | 1.00 | 1.00 | ||||||||||||
| Marital status | |||||||||||||||
| Unmarried | 33.33 | 12.50– 100.00 | < 0.001 | 5.56 | 1.45–20.00 | 0.012 | – | – | – | 7.69 | 1.01–100.00 | 0.039 | 5.26 | 1.89–14.29 | 0.002 |
| Married | 1.00 | 1.00 | 1.00 | 1.00 | |||||||||||
| Pregnancy status | |||||||||||||||
| Never pregnant | 4.35 | 1.20 – 16.67 | 0.025 | – | – | – | – | – | – | – | – | – | – | – | – |
| Ever pregnant | 1.00 | ||||||||||||||
| Knows someone with cervical cancer | |||||||||||||||
| Yes | – | – | – | 21.64 | 4.87–96.16 | < 0.001 | 24.99 | 10.24–61.00 | < 0.001 | – | – | 6.41 | 2.68–15.33 | < 0.001 | |
| No | 1.00 | 1.00 | 1.00 | ||||||||||||
AOR = Adjusted odd ratio; CI = Confidence interval.
4. Discussion
This study evaluated the uptake and predictors of HPV vaccination and testing among urban women in Lagos, Nigeria. It also examined the predictors of the willingness to receive HPV vaccine and do HPV testing among the non-uptake group and to vaccinate daughter. The various factors that served as motivators and barriers to HPV vaccination and testing were also assessed by the study.
A large proportion (70%) of the participants knew women who had CC. This finding reflects the high prevalence and burden of CC disease in the country. Nigeria has a huge population and she contributes significantly to the CC cases seen in the West African sub-region. This underscores the need to improve the delivery, acceptability and uptake of CC preventive measures among the populace. The uptake of HPV vaccination (29.0%) and testing (3.0%) was abysmally low among the participants. This is comparable to reports of other studies in Nigeria and other developing countries where the uptake of at least one dose of HPV vaccination and HPV testing ranged between 2.6% and 49.0% (Alsous et al., 2021, Nabirye et al., 2020, Kisaakye et al., 2018, Chiang et al., 2016, Ebu et al., 2021 Jan 6, Swarnapriya et al., 2015, Oluwole et al., 2019); and 1% and 5.3% (Okunowo and Smith-Okonu, 2020, Ngetich et al., 2020) respectively. Due to lack of official registration of HPV vaccination and testing in the country, there are no official data to compare our findings with. The good level of knowledge and perception about HPV & it prevention observed in the study did not positively influenced the uptake of HPV vaccination & testing as seen in other studies (Teame et al., 2019, Woldetsadik et al., 2020). This is similar to reports in other studies where knowledge did not correlate with increased uptake of preventive health practices (Santhanes et al., 2018, Ebu et al., 2021 Jan 6, Fishman et al., 2014, Bakheit and Buharooon, 2004). Theoretical knowledge is different from practical knowledge and good knowledge alone does not necessarily translate to uptake of health intervention (Dowell, 1969, Danka, 2009). Human behaviour is a complex process that is modified by several factors apart from knowledge (Ajzen, 1991, McGaw et al., 2012). Women were more willing to do HPV testing (77.3%) than accept HPV vaccination (28.9%) or vaccinate daughters (57%) despite a higher rate of HPV vaccination uptake (29%) compared to HPV testing uptake (3%). The probable reason for higher willingness to do HPV testing was the better level of knowledge & perception about HPV testing (91%) compared to that of HPV vaccination (76.5%). Likewise, lower uptake of HPV testing is probably due to the low recommendation of HPV testing by HCP as this was the major barrier to the uptake of HPV testing (65.5%) compared to that of HPV vaccination (38.0%). Similarly, the leading motivator for HPV testing in our study was recommendation by HCP, as five out of the six women (83.3%) who had HPV testing indicated that HCP was their major motivator compared to that of HPV vaccination (63.8%). It may also be as a result of hesitancy or apathy toward HPV vaccination among women who had not been vaccinated which has been reported in some studies (McRee et al., 2014, Szilagyi et al., 2020, Karafillakis et al., 2019).
We found that being employed (AOR = 60.45), unmarried (AOR = 33.33), tertiary education (AOR = 12.87) and having no prior pregnancy (AOR = 4.35) were the only independent predictors of the uptake of HPV vaccination. This is similar to findings in Uganda (Kisaakye et al., 2018) and Ghana (Ebu et al., 2021). It was not surprising that being employed had highest impact on the likelihood of receiving HPV vaccination as having a good occupation is associated with uptake of preventive healthcare interventions/practices (Teame et al., 2019, Damiani et al., 2012); and financial capability to afford vaccination. Unmarried women were more likely to have received HPV vaccination compared to unmarried women because married women are more likely to have initiated sexual activities with their partners and may no longer consider HPV vaccination as beneficial. Similarly, being married may confer a false sense of protection against contracting HPV infection which makes the woman believe she is not at risk of HPV related diseases. Education has always remained a key predictor of knowledge and uptake of preventive health measures (Okunowo and Adaramoye, 2018, Rakowski et al., 2004). The more educated the woman is, the higher her chances of utilizing CC preventive measures like HPV vaccination as found in our study and other studies (Kisaakye et al., 2018, Ebu et al., 2021 Jan 6).
Marital status and knowledge of someone with CC were the significant predictors of willingness to receive HPV vaccination among unvaccinated women. This is comparable to findings in other studies (Okunowo et al., 2018, Mortensen, 2010) and shows that experiential knowledge of a disease condition significantly influence human’s behavior and attitude towards the disease in contrast to just theoretical knowledge alone. A high proportion of unvaccinated women were unwilling to receive HPV vaccine and being married reduces the likelihood of accepting HPV vaccination. It is imperative to examine the factors responsible for such attitude in order to identify appropriate interventions that would cause behavioural change and increase acceptability of HPV vaccination. The willingness to vaccinate daughter was lower than that observed in another study in Lagos (Ezenwa et al., 2013) and Ghana (Coleman et al., 2011). The likelihood of vaccinating daughter was significantly higher among women who were employed, of Yoruba ethnicity and knew someone with CC. Marital status was the only significant predictor of the uptake of HPV testing among the participants with unmarried women having higher likelihood of doing HPV test. Similarly, being unmarried and knowing someone with CC were the independent predictors of willingness to do HPV testing. This is contrary to finding by Esber et al. (Esber et al., 2017) where recommendation by HCP was a significant predictor of willingness to do HPV testing.
The key motivating factor for the uptake of HPV vaccination and testing was recommendation by HCP. Similar findings have been reported in other studies on uptake of CC preventive measures (Ebu et al., 2021 Jan 6, Okunowo and Smith-Okonu, 2020, McRee et al., 2014, Okunowo et al., 2018, Mortensen, 2010, Tatar et al., 2018). This illustrates the invaluable contributions HCP make in promoting the adoption of HPV vaccination and testing. Recommendations from friends/relatives and electronic media also contributed immensely as sources of motivations for uptake of HPV vaccination and testing similar to findings in other studies (Ebu et al., 2021 Jan 6, Okunowo and Smith-Okonu, 2020, Okunowo et al., 2018, Tatar et al., 2018). Humans are social beings, as a result human interaction is a key determinant of human behaviour. Vantage use of all information channels including social media platforms are essential for dissemination of health information to young people.
Common barriers to the uptake of HPV vaccination and testing found in our study have been observed in many studies and reviews (Ebu et al., 2021 Jan 6, Swarnapriya et al., 2015, Okunowo and Smith-Okonu, 2020, McRee et al., 2014, Karafillakis et al., 2019, Okunowo et al., 2018, Mortensen, 2010, Tatar et al., 2018). Fears and worries about HPV vaccine is usually related to the perceived safety and side effects of the vaccine which is an aftermath of misinformation within the community. Health education on media platforms, in the communities and by HCP is essential to correct this misinformation, negative beliefs, and ultimately encourage uptake. In addition, the issue of cost and accessibility needs to be promptly addressed by all stakeholders to encourage utilization.
4.1. Limitations and strength
A limitation of this study was its relatively small sample size. It however provided vital evidence on the factors that influence HPV vaccination and testing in our environment. A large population based study is recommended to further examine how these factors influence the uptake and acceptability of these preventive measures. Another limitation of our study was its failure to assess the impact of sexual behaviors on the uptake and acceptability of HPV preventive measures. A major strength of this study was its unique ability to comprehensively assess the uptake and willingness to accept HPV vaccination and testing, the knowledge and perception about these preventive measures, the factors that influenced and predicted HPV vaccination and testing, in addition to evaluating the motivators and barriers to their uptake in one study. This is the first study to the best of our knowledge to report such a comprehensive evaluation on HPV vaccination and testing in a single original research paper.
5. Conclusion
The uptake of HPV vaccination and testing was low among the study participants. Women showed more willingness to do HPV testing than to receive HPV vaccine. Being employed, unmarried and knowing someone with CC were the key predictors of increased uptake and willingness to accept HPV vaccination and testing. The core motivators were recommendations by HCP, friends/relatives and media while the major barriers were lack of HCP recommendation, fear of HPV vaccine, high cost and lack of access. Critical evaluation of these factors by stakeholders are essential in identifying appropriate interventions to improve the current abysmal level of HPV vaccination and testing which are essential tools for CC prevention and possible eradication in our environment.
6. Submission declaration
The work described has not been published previously, nor is it under consideration for publication elsewhere.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Adeyemi A. Okunowo: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. Aloy O. Ugwu: Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. Jubril O. Kuku: Project administration, Resources, Validation, Writing – review & editing. Adaiah P. Soibi-Harry: Project administration, Resources, Writing – review & editing. Bolanle O. Okunowo: Formal analysis, Visualization, Writing – review & editing. Nneoma K. Ani-Ugwu: Project administration, Resources, Writing – review & editing. Benedetto O. Osunwusi: Resources, Writing – review & editing. Muisi A. Adenekan: Resources, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors thank all those who have one way or the other contributed to the successful execution of the study and writing of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2021.101643.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ajzen Icek. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- Akinola Oluwarotimi I, Aimakhu Christopher O, Ezechi Oliver C, Fasubaa Olusola B. Society of obstetrics and gynecology of Nigeria – Clinical practice guidelines: Guidelines for the prevention of cervical cancer. Trop. J. Obstet. Gynaecol. 2018;35(3):371–376. doi: 10.4103/TJOG.TJOG_88_18. [DOI] [Google Scholar]
- Alsous M.M., Ali A.A., Al-Azzam S.I., Abdel Jalil M.H., Al-Obaidi H.J., Al-abbadi E.I., Hussain Z.K., Jirjees F.J. Knowledge and awareness about human papillomavirus infection and its vaccination among women in Arab communities. Sci. Rep. 2021;11:786. doi: 10.1038/s41598-020-80834-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annekathryn, G., 2015. HPV testing as a screen for cervical cancer. BMJ, 350, h2372. Doi 10.1136/bmj.h2372. [DOI] [PubMed]
- Bakheit N.M., Buharooon A.L. The knowledge, attitude, and practice of Pap smear among local school teachers in the Sharjah district. Middle East J. Fam. Med. 2004;4(4):43–54. [Google Scholar]
- Bhatla N., Singhal S. Primary HPV screening for cervical cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 2020;65:98–108. doi: 10.1016/j.bpobgyn.2020.02.008. [DOI] [PubMed] [Google Scholar]
- Cervical Cancer Screening and Prevention, 2016. Practice Bulletin No. 168. American College of Obstetricians and Gynecologists. Obstet. Gynecol. 128(4), e111–30. [DOI] [PubMed]
- Bruni L., Saura-Lázaro A., Montoliu A., Brotons M., Alemany L., Diallo M.S., et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev. Med. 2021;144:106399. doi: 10.1016/j.ypmed.2020.106399. [DOI] [PubMed] [Google Scholar]
- Charan Jaykaran, Biswas Tamoghna. How to calculate sample size for different study designs in medical research? Indian J. Psychol. Med. 2013;35(2):121–126. doi: 10.4103/0253-7176.116232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang V., Wong H., Yeung P., Choi Y., Fok M., Mak O.I., Wong H., Wong K., Wong S., Wong Y., Wong E. Attitude, acceptability and knowledge of HPV vaccination among local university students in Hong Kong. Int. J. Environ. Res. Public Health. 2016;13(5):486. doi: 10.3390/ijerph13050486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrysostomou A.C., Stylianou D.C., Constantinidou A., Kostrikis L.G. Cervical cancer screening programs in Europe: The transition towards HPV vaccination and population-based HPV testing. Viruses. 2018;10(12):729. doi: 10.3390/v10120729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman Maame Aba, Levison Judy, Sangi-Haghpeykar Haleh. HPV vaccine acceptability in Ghana, West Africa. Vaccine. 2011;29(23):3945–3950. doi: 10.1016/j.vaccine.2011.03.093. [DOI] [PubMed] [Google Scholar]
- Damiani Gianfranco, Federico Bruno, Basso Danila, Ronconi Alessandra, Bianchi Caterina Bianca Neve Aurora, Anzellotti Gian Marco, Nasi Gabriella, Sassi Franco, Ricciardi Walter. Socioeconomic disparities in the uptake of breast and cervical cancer screening in Italy: a cross sectional study. BMC Public Health. 2012;12(1) doi: 10.1186/1471-2458-12-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danka I. Practical knowledge versus knowledge as Practice. Human Affairs. 2009;19:397–407. Https://doi.org/10.2478/v10023-009-0052-6. [Google Scholar]
- Dowell L.J. The relationship between knowledge and practice. J. Educ. Res. 1969;62(5):201–205. doi: 10.1080/00220671.1969.10883815. [DOI] [Google Scholar]
- Ebu N.I., Abotsi-Foli G.E., Gakpo D.F. Nurses' and midwives' knowledge, attitudes, and acceptance regarding human papillomavirus vaccination in Ghana: a cross-sectional study. BMC Nurs. 2021 Jan 6;20(1):11. doi: 10.1186/s12912-020-00530-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esber A., McRee A.L., Norris Turner A., Phuka J., Norris A. Factors influencing Malawian women's willingness to self-collect samples for human papillomavirus testing. J. Fam. Plann. Reprod. Health Care. 2017;43(2):135–141. doi: 10.1136/jfprhc-2015-101305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezenwa B.N., Balogun M.R., Okafor I.P. Mothers’ human papillomavirus knowledge and willingness to vaccinate their adolescent daughters in Lagos, Nigeria. Int. J. Womens Health. 2013;5:371–377. doi: 10.2147/IJWH.S44483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishman J., Taylor L., Kooker P., Frank I. Parent and adolescent knowledge of HPV and subsequent vaccination. Pediatrics. 2014;134(4):e1049–e1056. doi: 10.1542/peds.2013-3454. [DOI] [PubMed] [Google Scholar]
- Harun S.N.F., Sahani M., Johari M.Z. Factors affecting the decision making of HPV vaccination uptake among female youth in klang valley (Influencing Factors): a qualitative study. Glob. J. Health Sci. 2019;11(1):36–45. [Google Scholar]
- Karafillakis Emilie, Simas Clarissa, Jarrett Caitlin, Verger Pierre, Peretti-Watel Patrick, Dib Fadia, De Angelis Stefania, Takacs Judit, Ali Karam Adel, Pastore Celentano Lucia, Larson Heidi. HPV vaccination in a context of public mistrust and uncertainty: a systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum. Vaccin. Immunother. 2019;15(7-8):1615–1627. doi: 10.1080/21645515.2018.1564436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisaakye E., Namakula J., Kihembo C., Kisakye A., Nsubuga P., Babirye J.N. Level and factors associated with uptake of Human papillomavirus infection vaccine among female adolescents in Lira District, Uganda. Pan. Afr. Med. J. 2018;31:184. doi: 10.11604/pamj.2018.31.184.14801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehn B. Summit Leaders Urge Greater HPV Vaccination in Africa. JAMA. 2019;322(19):1853. doi: 10.1001/jama.2019.17713. [DOI] [PubMed] [Google Scholar]
- McGaw C., Tennant I., Harding H., Cawich S., Crandon I., Walters C. Healthcare workers’ attitudes to and compliance with infection control guidelines in the operating department at the university hospital of the West Indies, Jamaica. Int. J. Infect. Control. 2012;v8:i3 doi: 10.3396/ijic.v8i3.023.12. [DOI] [Google Scholar]
- McRee Annie-Laurie, Gilkey Melissa B., Dempsey Amanda F. HPV vaccine hesitancy: findings from a statewide survey of health care providers. J. Pediatr. Health Care. 2014;28(6):541–549. doi: 10.1016/j.pedhc.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen, G.L., 2010. Drivers and barriers to acceptance of human papillomavirus vaccination among young women: a qualitative and quantitative study. BMC Public Health 10, 68. http://www.biomedcentral.com/1471-2458/10/68. [DOI] [PMC free article] [PubMed]
- Mustafa Reem A., Santesso Nancy, Khatib Rasha, Mustafa Ahmad A., Wiercioch Wojtek, Kehar Rohan, Gandhi Shreyas, Chen Yaolong, Cheung Adrienne, Hopkins Jessica, Ma Bin, Lloyd Nancy, Wu Darong, Broutet Nathalie, Schünemann Holger J. Systematic reviews and meta-analyses of the accuracy of HPV tests, visual inspection with acetic acid, cytology, and colposcopy. Int. J. Gynecol. Obstet. 2016;132(3):259–265. doi: 10.1016/j.ijgo.2015.07.024. [DOI] [PubMed] [Google Scholar]
- Nabirye J., Okwi L.A., Nuwematsiko R., Kiwanuka G., Muneza F., Kamya C., Babirye J.N. Health system factors influencing uptake of Human Papillomavirus (HPV) vaccine among adolescent girls 9–15 years in Mbale District, Uganda. BMC Public Health. 2020;20(1):171. doi: 10.1186/s12889-020-8302-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngetich, E., Nzisa, I., Osoti, A., 2020. Uptake and determinants of cervical cancer prevention services among female college students in Kenya: A cross-sectional survey. bioRxiv 05.04.076513; doi: https://doi.org/10.1101/2020.05.04.076513.
- Okunowo A.A., Adaramoye V.O. Women's Knowledge on Ovarian Cancer Symptoms and Risk Factors in Nigeria: An Institutional-based Study. J. Epidemiol. Glob. Health. 2018;8(1–2):34–41. doi: 10.2991/j.jegh.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okunowo Adeyemi A., Daramola Ebunoluwa S., Soibi-Harry Adaiah P., Ezenwankwo Francis C., Kuku Jubril O., Okunade Kehinde S., Anorlu Rose I. Women's knowledge of cervical cancer and uptake of Pap smear testing and the factors influencing it in a Nigerian tertiary hospital. J. Cancer Res. Pract. 2018;5(3):105–111. [Google Scholar]
- Okunowo Adeyemi Adebola, Smith-Okonu Shakirat Tinuola. Cervical cancer screening among urban Women in Lagos, Nigeria: Focus on barriers and motivators for screening. Niger. J. Gen. Pract. 2020;18(1):10–16. doi: 10.4103/NJGP.NJGP_6_19. [DOI] [Google Scholar]
- Oluwole Esther O, Idowu Oluwaseun M, Adejimi Adebola A, Balogun Mobolanle R, Osanyin Gbemisola E. Knowledge, attitude and uptake of human papillomavirus vaccination among female undergraduates in Lagos State, Nigeria. J. Family Med. Prim. Care. 2019;8(11):3627–3633. doi: 10.4103/jfmpc.jfmpc_520_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigeria National Cancer Control Plan (2018 - 2022). Available at https://www.iccp-portal.org/system/files/plans/NCCP_Final%20%5B1%5D.pdf. Accessed 7 February 2021.
- Rakowski William, Breen Nancy, Meissner Helen, Rimer Barbara K, Vernon Sally W, Clark Melissa A, Freedman Andrew N. Prevalence and correlates of repeat mammography among women aged 55–79 in the Year 2000 National Health Interview Survey. Prev. Med. 2004;39(1):1–10. doi: 10.1016/j.ypmed.2003.12.032. [DOI] [PubMed] [Google Scholar]
- Santhanes D., Yong C.P., Yap Y.Y., Saw P.S., Chaiyakunapruk N., Khan T.M. Factors influencing intention to obtain the HPV vaccine in South East Asian and Western Pacific regions: A systematic review and meta-analysis. Sci. Rep. 2018;8(1):3640. doi: 10.1038/s41598-018-21912-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021;71(3):209–249. doi: 10.3322/caac.v71.310.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- Swarnapriya K., Kavitha D., Reddy G.M. Knowledge, Attitude and Practices Regarding HPV Vaccination among Medical and Para Medical in Students, India a Cross Sectional Study. Asian Pac. J. Cancer Prev. 2015;16(18):8473–8477. doi: 10.7314/apjcp.2015.16.18.8473. [DOI] [PubMed] [Google Scholar]
- Szilagyi Peter G., Albertin Christina S., Gurfinkel Dennis, Saville Alison W., Vangala Sitaram, Rice John D., Helmkamp Laura, Zimet Gregory D., Valderrama Rebecca, Breck Abigail, Rand Cynthia M., Humiston Sharon G., Kempe Allison. Prevalence and characteristics of HPV vaccine hesitancy among parents of adolescents across the US. Vaccine. 2020;38(38):6027–6037. doi: 10.1016/j.vaccine.2020.06.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatar Ovidiu, Thompson Erika, Naz Anila, Perez Samara, Shapiro Gilla K., Wade Kristina, Zimet Gregory, Gilca Vladimir, Janda Monika, Kahn Jessica, Daley Ellen, Rosberger Zeev. Factors associated with human papillomavirus (HPV) test acceptability in primary screening for cervical cancer: A mixed methods research synthesis. Prev. Med. 2018;116:40–50. doi: 10.1016/j.ypmed.2018.08.034. [DOI] [PubMed] [Google Scholar]
- Teame Hirut, Gebremariam Lemlem, Kahsay Tsega, Berhe Kidanemaryam, Gebreheat Gdiom, Gebremariam Gebrehiwot, Erbil Nülüfer. Factors affecting utilization of cervical cancer screening services among women attending public hospitals in Tigray region, Ethiopia, 2018; Case control study. PLoS ONE. 2019;14(3):e0213546. doi: 10.1371/journal.pone.0213546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velentzis L.S., Caruana M., Simms K.T., Lew J., Shi J., Saville M., et al. How will transitioning from cytology to HPV testing change the balance between the benefits and harms of cervical cancer screening? Estimates of the impact on cervical cancer, treatment rates and adverse obstetric outcomes in Australia, a high vaccination coverage country. Int. J. Cancer. 2017;141:2410–2422. doi: 10.1002/ijc.30926. [DOI] [PubMed] [Google Scholar]
- Woldetsadik A.B., Amhare A.F., Bitew S.T., Pei L., Lei J., Han J. Socio-demographic characteristics and associated factors influencing cervical cancer screening among women attending in St. Paul’s Teaching and Referral Hospital, Ethiopia. BMC Women's Health. 2020;20:70. doi: 10.1186/s12905-020-00927-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO), 2016. Guide to Introducing HPV Vaccine into National Immunization Programmes. Available at https://apps.who.int/iris/bitstream/handle/10665/253123/9789241549769-eng.pdf. Accessed 7 February 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.