Abstract
Background
Since the COVID-19 pandemic began, there have been concerns related to the preparedness of healthcare workers (HCWs). This study aimed to describe the level of awareness and preparedness of hospital HCWs at the time of the first wave.
Methods
This multinational, multicenter, cross-sectional survey was conducted among hospital HCWs from February to May 2020. We used a hierarchical logistic regression multivariate analysis to adjust the influence of variables based on awareness and preparedness. We then used association rule mining to identify relationships between HCW confidence in handling suspected COVID-19 patients and prior COVID-19 case-management training.
Results
We surveyed 24,653 HCWs from 371 hospitals across 57 countries and received 17,302 responses from 70.2% HCWs overall. The median COVID-19 preparedness score was 11.0 (interquartile range [IQR] = 6.0–14.0) and the median awareness score was 29.6 (IQR = 26.6–32.6). HCWs at COVID-19 designated facilities with previous outbreak experience, or HCWs who were trained for dealing with the SARS-CoV-2 outbreak, had significantly higher levels of preparedness and awareness (p<0.001). Association rule mining suggests that nurses and doctors who had a ’great-extent-of-confidence’ in handling suspected COVID-19 patients had participated in COVID-19 training courses. Male participants (mean difference = 0.34; 95% CI = 0.22, 0.46; p<0.001) and nurses (mean difference = 0.67; 95% CI = 0.53, 0.81; p<0.001) had higher preparedness scores compared to women participants and doctors.
Interpretation
There was an unsurprising high level of awareness and preparedness among HCWs who participated in COVID-19 training courses. However, disparity existed along the lines of gender and type of HCW. It is unknown whether the difference in COVID-19 preparedness that we detected early in the pandemic may have translated into disproportionate SARS-CoV-2 burden of disease by gender or HCW type.
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The transmission intensity is partially attributable to cycles of community spread [1–4] and healthcare workers (HCWs) are at particular risk. During the initial wave of transmission in China, 3.8% of COVID-19 patients were HCWs, whereas 9.0% of cases were HCWs in Italy [5, 6]. As of 30 November 2021, 770,536 HCWs in the United States had been infected; death status is available for 489,659 (63.55%) of them, of whom 2,890 had died [7]. SARS-CoV-2 infection has contributed to physical, mental, and emotional exhaustion of HCWs, potentially compromising patient care [8]. Heightening these risks has been the emergence of SARS-CoV-2 variants of concern, namely Alpha (B.1.1.7; first isolated in the United Kingdom; 175 countries now with the sequence), Beta (B.1.351; South Africa; 113 countries with sequence), Gamma (P.1; Brazil; 71 countries with sequence), Delta (B.1.617.2; India; 147 countries with sequence), and Omicron (B.1.1.529; South Africa and Botswana; 8 countries with sequence) [9]. COVID-19 awareness and preparedness among HCWs are vital to preventing transmission in healthcare facilities (HCFs) and safeguarding the workforce.
Early in the pandemic, the US Centers for Diseases Control and Prevention (CDC), the National Centre for Infectious Diseases in Singapore, and the World Health Organization (WHO) developed COVID-19 preparedness checklists [10]. We adapted these tools to evaluate the awareness and preparedness of HCWs globally with the aim of providing results to decision-makers who may be positioned to retool health systems for subsequent waves of COVID-19 and to inform responses to future infectious disease outbreaks.
Materials and methods
Study design and participants
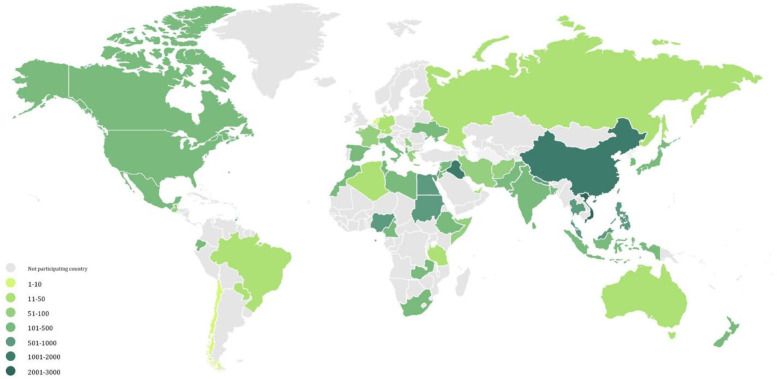
This multicenter, multinational, cross-sectional study of hospital HCWs was conducted between February and May 2020. Surveys were conducted in 371 HCFs across 57 countries and administrative regions (Fig 1 and S1 Table in S1 File). HCWs were invited to participate if they were involved in patient care, handling (or expected to care for) suspected COVID-19 patients, and provided informed written consent that was embedded on the first page of the questionnaire. After reading a descripton of the survey, individuals were asked if they agreed to participate. If they answered “YES” on the electronic form, the survey would begin. Respondents voluntarily participated and could withdraw consent at any time. We used convenience sampling with no restrictions on the number of hospitals and participants per country.
Fig 1. World map showing the distribution of study countries and study participants.
Note: Shade of green represents the number of participants per country.
Questionnaire design and scoring
Our questionnaire contained 32 questions in two sections. The first section consisted of six questions focused on general participant information. The second section included 26 questions related to participant awareness and preparedness against COVID-19. The last question solicited suggestions for improving preparedness. The awareness score was equal to the number of points accumulated over four topics with a maximum of 40 points. The maximum preparedness score was 15 based on responses from 15 questions.
We piloted the initial survey in English among 30 HCWs and revised accordingly. We then translated the instrument into 19 languages: Albanian, Arabic, Bengali, Chinese Mandarin, French, Hindi, Indonesian, Italian, Japanese, Korean, Kurdish, Nepali, Persian, Portuguese, Russian, Spanish, Thai, Urdu, and Vietnamese. We reverse-translated these versions, pre-tested them, and amended the final text as necessary. We used Cronbach’s alpha to estimate the reliability of single-administration test scores. This produced generally acceptable measures of 0.91 for preparedness, 0.61 for awareness, and 0.65 overall [11, 12]. Following survey administration, we extracted data, ran data quality checks, calculated overall awareness and preparedness scores, and stratified results by World Bank country classifications of high, upper-middle, lower-middle, and low income [13, 14].
Statistical analysis
We summarized participant characteristics using median and interquartile ranges for numeric variables, and tabulated the number of participants and percentages for categorical variables. We reviewed outcome measures as histograms and evaluated associations between participant characteristics and outcome measures using a multi-level linear regression model and random effects models. We assigned participants, hospitals, and countries to levels 1, 2, and 3. We then generated results by mean difference (MD) with 95% confidence intervals (CI) and P-values. Where at least one component question was not answered, we performed complete-case and imputed-data analyses in the multi-level model. In our complete-case analysis, missing responses were assigned zero points. For our imputed-data analysis, we estimated missing values with multiple imputation-by-chained-equation methods [15]. We included available data in the imputation model with 20 imputed datasets and 20 cycles per dataset.
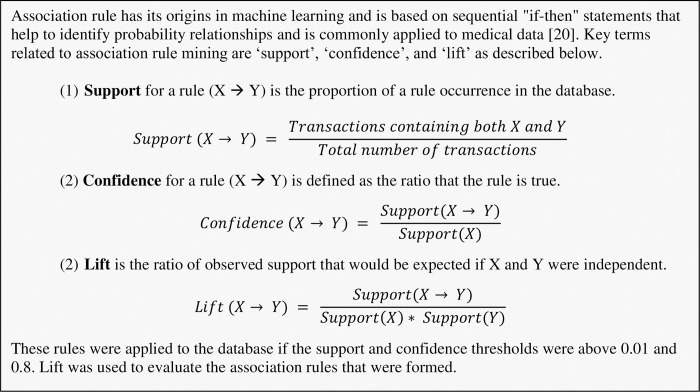
We assessed the effect of HCW training courses on awareness and preparedness for managing COVID-19 cases in the hospital by scatter plot and added smoothing lines with Loess method for groups with and without training. We then conducted association rule mining using an algorithm developed a priori [16] to identify otherwise undetectable relationships between HCW participation in training courses and their confidence in handling suspected COVID-19 patients, as well as their satisfaction in the medical equipment available in their hospitals for the pandemic response [17]. Participating HCWs by country are illustrated on the world map of Fig 1. We produced using the R ggplot2 package [18] and used R software version 3.6.3 to perform these analyses [19]. Key concepts of association rule mining [20], i.e. support, confidence, and lift, are outlined in Fig 2.
Fig 2. Fundamentals of association rule mining.
Ethics approval
The study protocol was approved by the Ethics Committee of the School of Tropical Medicine and Global Health, Nagasaki University, Japan [21], and by all participating healthcare facilities according to local guidelines (S2 Table in S1 File).
Results
Socio-demographic characteristics
A total of 17,302 valid surveys out of 24,653 (response rate: 70.18%) were received from HCWs, of which 16,954 reported their gender; 10,843 (64.0%) were women, and 6,045 (35.7%) were men, the remaining 66 participants did not want to report gender. Most participants were younger than 44 years of age (n = 14,257, 86.4%) and from Asia (n = 11,065, 64.0%). Nurses (n = 7,679, 44.7%) and lower-middle income countries (n = 7,461, 43.1%) were the most represented (Table 1 and S3 Table in S1 File).
Table 1. Sociodemographic characteristics, work experience, and workplace of participating healthcare workers.
| Characteristic | Participants, n (%) |
|---|---|
| Sociodemographic | |
| Median age in years (interquartile range) (n = 16,511) | 32.0 (27.0, 40.0) ¶ |
| Gender (n = 16,954) | |
| Women | 10,843 (64.0) |
| Men | 6,045 (35.7) |
| Prefer not to specify | 66 (0.4) |
| Profession (n = 17,195) | |
| Doctor | 6,328 (36.8) |
| Nurse | 7,679 (44.7) |
| Pharmacist | 769 (4.5) |
| Others | 2,419 (14.1) |
| Work experience and workplace | |
| Work experience, Range in years (n = 14,812) | 7.0 (3.0–15.0) ¶ |
| Hospital department (n = 17,025) | |
| Emergency department | 3,728 (21.9) |
| Intensive care unit | 2,428 (14.3) |
| Outpatient clinic | 2,454 (14.4) |
| Infectious disease department | 1,157 (6.8) |
| Respiratory department | 1,208 (7.1) |
| Others | 7,155 (42.0) |
| Type of hospital (n = 16,335) | |
| Designated to treat COVID-19 | 6,847 (41.9) |
| Not designated but able to treat COVID-19 | 5,036 (30.8) |
| Not designated and not able to treat COVID-19 | 4,452 (27.3) |
| Previous outbreak experience (n = 17,508) | |
| Experienced any outbreak (n = 17,045) | 7,508 (44.0) |
| Experienced SARS outbreak (n = 17,045) | 3,548 (20.8) |
| Experienced MERS outbreak (n = 17,045) | 1,819 (10.7) |
| Experienced bird flu outbreak (n = 17,045) | 4,858 (28.5) |
| Experienced other outbreaks (n = 17,045) | 1,474 (8.6) |
| Confirmed SARS-CoV-2 case where you are (n = 17,164) | |
| Yes, in my country | 7,071 (41.2) |
| Yes, in my city | 3,095 (18.0) |
| Yes, in my hospital | 2,300 (13.4) |
| Participated in training course for dealing with COVID-19 (n = 17,169) | 6,287 (36.6) |
| How satisfied you are with medical equipment in your hospital (n = 17,106) | |
| Very unsatisfied | 1,954 (11.4) |
| Unsatisfied | 3,922 (22.9) |
| Neutral | 4,524 (26.4) |
| Satisfied | 5,049 (29.5) |
| Very satisfied | 1,657 (9.7) |
| Have confidence in handling suspected COVID-19 patients (n = 17,138) | |
| Not at all | 2,849 (16.6) |
| To a little extent | 3,973 (23.2) |
| To some extent | 4,726 (27.6) |
| To a considerable extent | 3,712 (21.7) |
| To a great extent | 1,878 (11.0) |
Workplace characteristics and source of information
Participants had a median of seven years of work experience (n = 14,812; interquartile range [IQR] 3.0 to 15.0) and were most commonly from level 3 hospitals (n = 11,424; 67.0%) and emergency departments (n = 3–728; 21.9%) (Table 1). In total, 44.0% (n = 7,508) of HCWs had prior outbreak experience and 13.4% (n = 2,300) reported the presence of confirmed cases in their hospitals at the time of survey. Mainstream media was the primary source of information for HCWs (n = 13,659; 79.4%), followed by online social networks (n = 11,336; 65.9%), and government organizations (n = 9,603; 55.9%) (Table 1). Only 36.6% (n = 6,287) of HCWs had taken part in a COVID-19 training course. In total, 39.2% of participants were satisfied (29.5%) or very satisfied (9.7%) with available medical equipment. Most HCWs (n = 10,316; 84.4%) had some degree of confidence in handling suspected cases.
COVID-19 preparedness and awareness scores
In total, 15,689 (90.1%) and 16,419 (94.9%) participants completed all questions in the preparedness and awareness sections. There was high agreement in results generated by complete-case versus imputed-data analyses. Specifically, there were significant associations in 21 analyses of complete-case data, and 22 significant associations from imputed-data analyses. Collectively, 19 significant associations were concordant between the two analyses (Table 2).
Table 2. Multilevel models for preparedness and awareness scores of participating healthcare workers.
| Variable | Complete-case analysis | Imputed data analysis | ||||
|---|---|---|---|---|---|---|
| MD | (95% CI) | P-value | MD | (95% CI) | P-value | |
| Preparedness | ||||||
| Region | ||||||
| East Asia & Pacific | Reference | Reference | ||||
| Europe & Central Asia | -1.25 | (-2.74, 0.24) | 0.099 | -1.13 | (-2.59, 0.33) | 0.128 |
| Latin America & Caribbean | -2.96 | (-4.75, -1.17) | 0.001 * | -2.96 | (-4.73, -1.20) | 0.001 * |
| Middle East & North Africa | -3.20 | (-4.58, -1.81) | <0.001 * | -3.27 | (-4.64, -1.91) | <0.001* |
| North America | -2.24 | (-5.51, 1.03) | 0.180 | -3.15 | (-5.61, -0.69) | 0.012 * |
| South Asia | -2.36 | (-4.11, -0.61) | 0.008 * | -2.54 | (-4.26, -0.82) | 0.004 * |
| Sub-Saharan Africa | -4.32 | (-6.01, -2.62) | <0.001 * | -4.54 | (-6.21, -2.87) | <0.001* |
| Income level | ||||||
| High income | Reference | Reference | ||||
| Upper middle income | -0.18 | (-1.53, 1.17) | 0.794 | -0.11 | (-1.44, 1.22) | 0.874 |
| Lower middle income | -0.87 | (-2.41, 0.66) | 0.264 | -0.78 | (-2.29, 0.73) | 0.310 |
| Low income | -1.08 | (-3.14, 0.97) | 0.301 | -1.05 | (-3.08, 0.97) | 0.308 |
| Level of hospital | ||||||
| 1st level | Reference | Reference | ||||
| 2nd level | -0.29 | (-0.97, 0.39) | 0.406 | -0.12 | (-0.75, 0.52) | 0.721 |
| 3rd level | 0.08 | (-0.58, 0.74) | 0.805 | 0.29 | (-0.30, 0.87) | 0.339 |
| Type of hospital | ||||||
| Designated to treat COVID-19 | Reference | Reference | ||||
| Not designated but able to treat COVID-19 | -0.00 | (-0.52, 0.51) | 0.993 | -0.14 | (-0.57, 0.29) | 0.530 |
| Not designated & unable to treat COVID-19 | -0.72 | (-1.33, -0.11) | 0.020 * | -0.37 | (-0.81, 0.07) | 0.098 |
| Age (every 10-year increase) | 0.40 | (0.28, 0.53) | <0.001 * | 0.41 | (0.30, 0.52) | <0.001* |
| Gender | ||||||
| Women | Reference | Reference | ||||
| Men | 0.35 | (0.23, 0.47) | <0.001 * | 0.28 | (0.17, 0.38) | <0.001* |
| Other | -0.64 | (-1.71, 0.43) | 0.239 | -0.60 | (-1.34, 0.14) | 0.113 |
| Profession | ||||||
| Doctor | Reference | Reference | ||||
| Nurse | 0.66 | (0.54, 0.81) | <0.001 * | 0.67 | (0.55, 0.79) | <0.001* |
| Pharmacist | -0.86 | (-1.13, -0.59) | <0.001 * | -0.77 | (-1.02, -0.53) | <0.001* |
| Others | -0.57 | (-0.75, -0.39) | <0.001 * | -0.62 | (-0.77, -0.47) | <0.001* |
| Experience (every 10-year increase) | 0.10 | (-0.03, 0.24) | 0.136 | 0.06 | (-0.06, 0.18) | 0.337 |
| Experienced any outbreak | ||||||
| Yes | Reference | Reference | ||||
| No | -0.56 | (-0.67, -0.44) | <0.001 * | -0.52 | (-0.62, -0.42) | <0.001* |
| Confirmed COVID-19 case where you are | ||||||
| No | Reference | Reference | ||||
| Yes, in my country | 0.34 | (0.15, 0.53) | <0.001 * | 0.27 | (0.10, 0.44) | 0.002* |
| Yes, in my city | 0.28 | (0.04, 0.53) | 0.025 * | 0.20 | (-0.01, 0.41) | 0.063 |
| Yes, in my hospital | 0.65 | (0.35, 0.95) | <0.001 * | 0.50 | (0.24, 0.75) | <0.001* |
| Awareness | ||||||
| Region | ||||||
| East Asia & Pacific | Reference | Reference | ||||
| Europe & Central Asia | 0.81 | (-0.79, 2.41) | 0.321 | 0.57 | (-0.90, 2.03) | 0.448 |
| Latin America & Caribbean | 0.08 | (-1.82, 1.98) | 0.933 | 0.19 | (-1.55, 1.94) | 0.830 |
| Middle East & North Africa | -1.37 | (-2.86, 0.12) | 0.071 | -0.91 | (-2.30, 0.48) | 0.201 |
| North America | 0.67 | (-2.84, 4.19) | 0.707 | 0.56 | (-1.92, 3.04) | 0.659 |
| South Asia | -1.31 | (-3.19, 0.57) | 0.173 | -0.97 | (-2.73, 0.79) | 0.279 |
| Sub-Saharan Africa | -0.56 | (-2.38, 1.27) | 0.551 | -0.18 | (-1.89, 1.53) | 0.837 |
| Income level | ||||||
| High income | Reference | Reference | ||||
| Upper middle income | -1.71 | (-3.15, -0.26) | 0.020 * | -2.02 | (-3.34, -0.70) | 0.003* |
| Lower middle income | -1.48 | (-3.19, 0.16) | 0.078 | -1.54 | (-3.06, -0.02) | 0.047* |
| Low income | -1.21 | (-3.49, 1.00) | 0.283 | -1.73 | (-3.77, 0.31) | 0.097 |
| Level of hospital | ||||||
| 1st level | Reference | Reference | ||||
| 2nd level | -0.29 | (-1.01, 0.43) | 0.425 | 0.02 | (-0.56, 0.60) | 0.946 |
| 3rd level | 0.41 | (-0.28, 1.11) | 0.242 | 0.46 | (-0.09, 1.01) | 0.098 |
| Type of hospital | ||||||
| Designated to treat COVID-19 | Reference | Reference | ||||
| Not designated but able to treat COVID-19 | 0.17 | (-0.37, 0.70) | 0.542 | 0.03 | (-0.36, 0.42) | 0.892 |
| Not designated & unable to treat COVID-19 | -0.32 | (-0.96, 0.31) | 0.319 | -0.15 | (-0.59, 0.28) | 0.486 |
| Age (every 10-year increase) | -0.16 | (-0.34, 0.01) | 0.068 | -0.02 | (-0.16, 0.12) | 0.772 |
| Gender | ||||||
| Women | Reference | Reference | ||||
| Men | -0.02 | (-0.19, 0.15) | 0.791 | -0.11 | (-0.24, 0.02) | 0.103 |
| Other | -0.68 | (-2.19, 0.83) | 0.375 | -0.96 | (-1.87, -0.04) | 0.040* |
| Profession | ||||||
| Doctor | Reference | Reference | ||||
| Nurse | -1.97 | (-2.16, -1.78) | <0.001 * | -1.76 | (-1.91, -1.61) | <0.001* |
| Pharmacist | -1.56 | (-1.94, -1.18) | <0.001 * | -1.26 | (-1.57, -0.95) | <0.001* |
| Others | -2.44 | (-2.69, -2.19) | <0.001 * | -2.08 | (-2.28, -1.89) | <0.001* |
| Experience (every 10-year increase) | 0.06 | (-0.13, 0.25) | 0.547 | 0.01 | (-0.15, 0.16) | 0.953 |
| Experienced any outbreak | ||||||
| Yes | Reference | Reference | ||||
| No | -0.49 | (-0.66, -0.33) | <0.001 * | -0.26 | (-0.39, -0.13) | <0.001* |
| Confirmed COVID-19 case where you are | ||||||
| No | Reference | Reference | ||||
| Yes, in my country | 1.53 | (1.26, 1.80) | <0.001 * | 1.30 | (1.09, 1.52) | <0.001* |
| Yes, in my city | 1.75 | (1.40, 2.09) | <0.001 * | 1.57 | (1.30, 1.83) | <0.001* |
| Yes, in my hospital | 1.79 | (1.38, 2.21) | <0.001* | 1.62 | (1.30, 1.94) | <0.001* |
MD: mean difference; CI: confidence interval
*Statistically significant
Preparedness scores
The median preparedness score of all participants was 11.0 (n = 17,302; IQR 6.0 to 14.0). Results from the multi-level linear model suggest that socio-demographic characteristics had a significant effect on participant preparedness scores (Table 2). Relative to East Asia and the Pacific, preparedness scores were significantly lower in the complete-case analysis among participants from sub-Saharan Africa (MD -4.32; CI -6.01 to -2.62; P < 0.001), the Middle East and North Africa (MD -3.20; CI = -4.58 to -1.81; P < 0.001), Latin America and the Caribbean (MD -2.96; CI -4.75 to -1.17; P = 0.001), and South Asia (MD -2.36; CI -4.11 to -0.61; P = 0.008). Imputed-data from North America also had significantly lower preparedness scores (MD -3.15; CI = -5.61 to -0.69; P = 0.012) than those in East Asia and the Pacific region.
There was a significant increase in the participant preparedness score for every 10-year increase in age, whether in completed-case (MD 0.40; CI = 0.28 to 0.53; P < 0.001) or imputed-data sets (MD 0.41; CI 0.30 to 0.52; P < 0.001). Male participants (MD 0.35; CI 0.23 to 0.47; P < 0.001) and nurses (MD 0.66; CI 0.54 to 0.81; P < 0.001) had higher preparedness scores compared to women and doctors (Table 2). The type of HCF and prior pandemic experience had a significant effect on preparedness scores; HCWs at hospitals who were not designated and not able to treat COVID-19 patients had significantly lower preparedness scores (MD -0.72; CI -1.33 to -0.11; P = 0.020) in the complete-case analysis, a finding that did not persist with data imputations (MD -0.37; CI -0.81 to 0.07; P = 0.098). Participants with no previous outbreak experience had significantly lower preparedness scores in both completed-case (MD -0.56; CI -0.67 to -0.44; P < 0.001) and imputed-data (MD -0.52; CI -0.62 to -0.42; P < 0.001) analyses. Participants from hospitals with confirmed COVID-19 case(s) had the highest preparedness score in the complete-case analysis compared to hospitals without confirmed case(s) (MD 0.65; CI 0.35 to 0.95; P < 0.001), a finding that was also reflected in the imputed-data analysis (Table 2). The preparedness score for participants who had COVID-19 training averaged 12.90 ±2.97 compared to participants without training 7.98 ±4.33 (P = 0.001).
Awareness scores
The median awareness score was 29.6 of 40 possible points (n = 17,302; IQR 26.6 to 32.6). Table 2 shows results from the multilevel linear model. Among socio-demographic characteristics, only income level and profession had a significant effect on awareness scores. Participants from upper-middle income countries (MD -1.71; CI -3.15 to -0.26; P = 0.020) had significantly lower awareness scores compared to those from high income countries by complete-case analysis, a finding consistent with imputed data. Doctors served as the reference group, having the highest awareness scores, followed by pharmacists (MD -1.56; CI -1.94 to -1.18; P < 0.001), nurses (MD -1.97; CI -2.16 to -1.78; P < 0.001), and other professions (MD -2.44; CI -2.69 to -2.19; P < 0.001); results were also significant in the imputed-data analysis (Table 2). Individuals with no previous outbreak experience had significantly lower awareness scores than those with experience (MD -0.49; CI -0.66 to -0.33; P < 0.001) in the complete-case analysis, which was also reflected in the imputed data. Similarly, complete-case analyses showed participants with confirmed COVID-19 case(s) in their hospital, city, or country had significantly higher awareness scores (MD 1.79; CI 1.38 to 2.21; P < 0.001; 1.75; CI 1.40 to 2.09; P < 0.001; and 1.53; CI 1.26 to 1.80; P < 0.001), findings that were similar in the imputed-data (Table 2). HCWs who received COVID-19 training had a total awareness score of 29.3 ±4.00 which was significantly higher than a score of 28.9 ± 5.48 among HCWs without training (MD 0.40; CI: 0.25 to 0.56, P < 0.001).
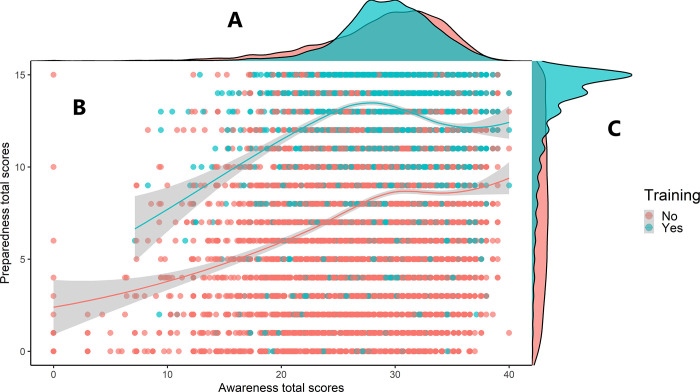
Fig 3 illustrates positive correlations between awareness and preparedness scores for those who received COVID-19 training and those who did not. A high number of participants with awareness scores between 28 and 30 were in the trained group, with preparedness scores between 13 and 15 points. No similar concentration was observed in the non-trained group.
Fig 3. Two multivariate cowplots illustrating the effect of training on preparedness and awareness.
Part A illustrates the distribution of awareness scores. Part B shows individual total scores of preparedness and awareness. The center lines were computed using Loess method with the shadow representing their 95% confidence intervals. Part C illustrates the distribution of preparedness scores.
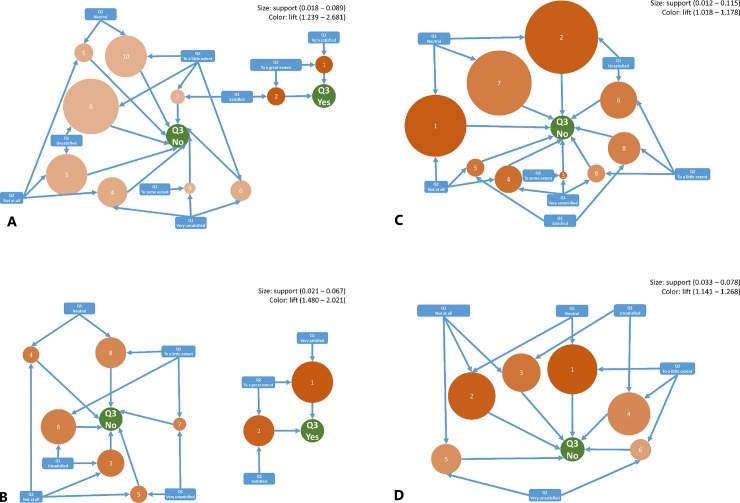
The mining algorithm produced 33 rules (Fig 4). Summaries of the support, confidence, and lift for each association rule are presented in S4 Table in S1 File. Nurses and doctors who were confident in handling suspected COVID-19 patients (to a ’great extent’) and satisfied in the current medical equipment for COVID-19 management (’very satisfied’) had participated in any training courses for dealing with COVID-19 with support levels of 0.067 and 0.028, confidence levels of 0.925 and 0.873, and lift levels of 2.021 and 2.681. Less confidence (’little extent’ or ’not confident’) and less satisfaction (’unsatisfied’ or ’very unsatisfied’) implied that they had not participated in any COVID-19 training with support levels of 0.021 and 0.089, confidence between 0.830 and 0.932, and lift of 1.244 and 1.685. Fig 4A illustrates relationships identified with association rule mining among survey responses from participant doctors. Question 1 queried the satisfaction level of doctors in the current medical equipment for the management of COVID-19; Question 2 elicited confidence of doctors in handling suspected COVID-19 patients; Question 3 accounted for participation of doctors in any training courses that dealt with COVID-19. Fig 4B–4D illustrate association rule mining among nurses, pharmacists, and other HCWs.
Fig 4.
A-D. Association rules between HCWs training, confidence in handling suspected COVID-19 patients, and satisfaction in the current medical equipment for the management of COVID-19 in HCWs hospitals. Note: Numbered circles represent the generated rules and their properties, where the size represents the rate at which these rules occur in the data (support), and the color represents the lift value in which the darker the circle, the higher the probability that the antecedents and consequents are connected. The arrows pointing toward the circle are the rule inputs (antecedents), and the arrows coming out are the rule outputs (consequents). Fig 4A–4D show the findings for doctors, nurses, pharmacists, and other HCWs, respectively, and visually display the generated rules shown in S4 Table in S1 File, which also contains information about the confidence index of these rules. For detailed interpretation of the figures, refer to S1 Text in S1 File.
Q1: Satisfaction level in the current medical equipment for the management of COVID-19.
Q2: Confidence level in handling suspected COVID-19 patients.
Q3: Participation in any training courses for dealing with COVID-19 outbreak.
Interpretation
The high level of agreement between complete-case data analysis and imputed-data analysis suggests that missing data did not skew our results. Overall, we found HCWs to be prepared for and aware of the COVID-19 pandemic to some extent. This level was the highest among nurses (for preparedness) and doctors (for awareness), findings that differ from earlier reports, particularly in regards to preparedness levels [22, 23]. Regardless, we might expect nurses to be more prepared since they were encourage to take on expanded roles in 2018 by international and national agencies (e.g., World Health Organization, International Council of Nurses, American Nurses Association, CDC) in rapid mobilization of responses in any pandemic [24]. We found an association between older age and greater preparedness in contrast to other studies outside infectious disease management [25–27].
Although disease burden continues to spread regardless of economic status, national wealth was significantly associated with the level of preparedness, which is consistent with reports from the literature. Studies from Saudi Arabia, for instance, showed higher preparedness levels from Yemen and Palestinian Territories [28–30]. This is reflected in the capacity of high-income countries to deploy large-scale testing in a short time period. An estimated 56.0% of HCWs lacked outbreak experience and, not surprisingly, their preparedness and awareness scores were significantly lower than measures among HCWs with some experience of SARS, MERS, and avian influenza outbreaks. Higher scores among older HCWs underscores the potential for sharing experiences between staff and hospitals, and the importance of preserving institutional memory. This experience can be tapped to foster South-South cooperation and form the basis of South-North exchange. Prior experience with SARS enabled countries and territories (e.g. Vietnam, Taiwan, and Hong Kong) to combat COVID-19 successfully in early stages [31–33].
Vietnam, despite being a low-resource country, and Hong Kong, with its relative proximity to Wuhan (923 km or 573 miles) and large numbers of international travelers, were both able to control the first wave of the pandemic by deploying a comprehensive government response that included travel bans and aggressive quarantine strategies, suspension of non-essential business, transportation, and schooling, and prioritizing rapid improvements in health care facilities [33, 34]. In Vietnam, following the 2003 outbreak of SARS and H1N1 in 2009, the Vietnamese Centers for Disease Control and Prevention led a national effort to upgrade infectious disease facilities and related equipment. Taiwan applied lessons from the SARS outbreak and had in place a framework for an integrated response to future pandemics [35].
General knowledge of COVID-19 is crucial for HCWs to be equipped adequately and manage suspected or confirmed cases. However, it is concerning that the majority of participants relied on the mainstream media (79.4%) and social media (65.9%) as their primary source of information. The WHO has warned that an ‘infodemic’ of widespread misinformation is a serious concern [36]. HCWs must carefully evaluate information to ensure that it is grounded in evidence. While the HCW interpersonal sources used may not be decisive, group sensemaking is especially important and time-sensitive when the international health community is suffering. However, HCW should always evaluate the credibility of the information by double-checking with trusted sources like WHO and other regional and national health agencies. The emergence of coronavirus variants underscores this importance. Government authorities need to provide accurate and timely guidance to HCWs. At the time of the survey, up to 30% of respondents could not identify some known COVID-19 symptoms or preventive measures to minimize the transmission (S5 Table in S1 File).
In Vietnam, many measures were used to disseminate accurate and updated information. The Vietnamese Ministry of Health, for example, regularly updated its website with news and the latest control measures. They also deployed mobile apps that provided official daily notices of detected clusters; the local app Zalo had approximately 100 million users at one time, contributing to awareness raising and preparedness of Vietnamese HCWs with daily and sometimes hourly updated news about COVID-19 [33].
In our survey, female HCWs had lower preparedness/awareness scores than male counterparts, which is consistent with reports from another preparedness study [29]. Female HCWs have had vastly higher rates of infection compared to males in Spain (n = 21,392; 75.5%), Italy (n = 14,350; 69.0%), and the United States (n = 6,776; 73.0%) [37, 38]. It is difficult to know whether the difference in preparedness between male and female HCWs that we detected in our global survey early in the pandemic later translated to female HCWs being disproportionately infected by SARS-CoV-2. Regardless, female HCWs need to be afforded equal training opportunities. Although specific training was associated with greater preparedness scores, this was accompanied by a minimal increase in awareness scores, suggesting that further improvements in training may be required. Similar to other studies, we observed an association between training and confidence levels of HCWs [39–41]. Thus, the introduction of training courses should be an essential part of preparedness and response plans.
Limitations
Firstly, this study was mainly conducted online among HCWs at a relatively early stage of the pandemic. This does not inherently bias our results, but it does limit the generalizability to facilities and HCWs that have Internet access. In addition, the high participation rates among HCWs in Asia, a region with prior experience managing the SARS and MERS epidemics, could mean our results overstate the true COVID-19 awareness and preparedness of HCWs in other regions of the world at the time of the survey. Finally, there is always a potential risk of bias in data collection when surveys are not completed in their entirety. We overcame this, however, by performing complete-case and imputed-data analyses in our multi-level models.
In addition, at the beginning of our study, we developed questions to survey HCWs preparedness mainly from the CDC’s healthcare professional SARS-CoV-2 preparedness checklist, which was considered the most up to date at the time [10]. The checklist had the same structure and content as the HCW preparedness checklist for MERS-CoV, which has not been updated since July 2013 [42]. Given the fact that our survey was based on the CDC’s latest guidance and our intention was to reach as many HCWs as possible around the globe, our survey questionnaire was translated into 19 different languages and distributed to 17,302 HCWs in 57 countries over a short period of time. However, as the COVID-19 became a pandemic, the CDC updated the checklist to be more specific for the disease. The initial checklist is now only applied for the transportation and admission of patients with suspected or confirmed COVID-19 [10]. Regarding the questions themselves to assess the HCWs’ awareness, we used multiple choice format to survey their awareness on symptoms of COVID-19. At the time of our survey, “red eyes” was not recognized as a manifestation of COVID-19 and, as a result, a majority of HCWs chose “false” for this symptom which was considered the right answer to the question. However, the answer should be “true” now due to more recent understandings of the disease [43].
Our study provides a first glance of HCWs worldwide and their preparedness toward a new emergent prone-disease pandemic. Follow-up research is suggested to compare the differences between current knowledge of HCWs and to measure the differences, and possible improvements, in awareness and preparedness of HCPs over time as the COVID-19 pandemic has gone through three waves.
Conclusion
We found an acceptable level of awareness and preparedness among HCWs specific to COVID-19 during the time of the survey, although there was disparity along gender lines, type of HCW, and previous experience of similar outbreaks. Training opportunities need to be gender-equitable to safeguard the workforce and stem SARS-CoV-2 transmission in HCF. Preparedness may be facilitated by increased South-South and South-to-North knowledge exchange to benefit from similar experiences of previous disease outbreaks.
Supporting information
(DOCX)
Acknowledgments
The authors also thank Dr. Kim Taehoon and Dr. Mervat Cohen for their critical review in Korean and Indonesian language translation.
The authors appreciate the contribution of collaborators below:
Study guarantors: Nguyen Tien Huy (Email: tienhuy@nagasaki-u.ac.jp; School of Tropical Medicine and Global Health, Nagasaki University, Japan) and R Matthew Chico (Email: Matthew.Chico@lshtm.ac.uk; London School of Hygiene & Tropical Medicine, UK). Nguyen Tien Huy is the lead of the TMGH-Global COVID-19 Collaborative.
Project Managers: Vuong Thanh Huan (Pham Ngoc Thach University of Medicine, Vietnam), Hosam Waleed Shaikhkhalil (Islamic University of Gaza, Palestine), Vuong Ngoc Thao Uyen (International University—Vietnam National University, Ho Chi Minh city, Vietnam), Ahmad Taysir Atieh Qarawi (Lower Westchester Medical Associates, P.C., USA), Shamael Thabit Mohammed Alhady (University of Gezira, Sudan), Nguyen Lam Vuong (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Le Van Truong (Traditional Medicine Hospital of Ministry of Public Security, Vietnam), Mai Ngoc Luu (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Shyam Prakash Dumre (Institute of Tropical Medicine, Nagasaki University, Japan), Atsuko Imoto (School of Tropical Medicine and Global Health, Nagasaki University, Japan), Peter N Lee (P.N.Lee Statistics and Computing Ltd, UK), Dao Ngoc Hien Tam (Asia Shine Trading & Service CO, LTD., Vietnam), Sze Jia Ng (Universiti Sains Malaysia, Malaysia), Mohammad Rashidul Hashan (Government of the People’s Republic of Bangladesh—Ministry of Health and Family Welfare, Bangladesh), Mitsuaki Matsui (School of Tropical Medicine and Global Health, Nagasaki University, Japan), Nguyen Tran Minh Duc (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Sedighe Karimzadeh (Sabzevar University of Medical Sciences, Sabzevar, Iran), Nut Koonrungsesomboon (Chiang Mai University, Thailand), Chris Smith (School of Tropical Medicine and Global Health, Nagasaki University, Japan; London School of Hygiene & Tropical Medicine, UK), Sharon E Cox (School of Tropical Medicine and Global Health, Nagasaki University, Japan; London School of Hygiene & Tropical Medicine, UK), Kazuhiko Moji (School of Tropical Medicine and Global Health, Nagasaki University, Japan), Kenji Hirayama (Institute of Tropical Medicine, Nagasaki University, Japan), Le Khac Linh (VinUniversity, Vietnam), Kirellos Said Abbas (Alexandria University, Egypt), Tran Nu Thuy Dung (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Tareq Mohammed Ali AL-Ahdal (Jordan University of Science and Technology, Jordan), Emmanuel Oluwadare Balogun (Ahmadu Bello University, Nigeria), Nguyen The Duy (University Hospital Giessen and Marburg, Germany), Mennatullah Mohamed Eltaras (Al-Azhar University, Egypt), Trang Huynh (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Nguyen Thi Linh Hue (Nguyen Trai Hospital, Vietnam), Bui Diem Khue (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Abdelrahman Gad (Ain Shams University, Egypt), Gehad Mohamed Tawfik (Ain Shams University, Egypt), Kazumi Kubota (Yokohama City University, Japan), Hoang-Minh NGUYEN (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Dmytro Pavlenko (Bogomolets National Medical University, Kyiv, Ukraine), Vu Thi Thu Trang (National Hospital of Traditional Medicine, Vietnam), Le Thuong Vu (University of Medicine and Pharmacy at Ho Chi Minh city, Vietnam), Hai-Yen Tran (International University—Vietnam National University, Ho Chi Minh city, Vietnam), Nguyen Thi Yen-Xuan (Cambridge University Hospital Foundation Trust, UK), Luong Thi Trang (Danang Oncology Hospital, Vietnam), Vinh Dong (American University of the Caribbean, Sint Maarten), Akash Sharma (University College of Medical Sciences & Guru Teg Bahadur Hospital, Dilshad Garden, Delhi, India), Vu Quoc Dat (Hanoi Medical University, Vietnam), Mohammed Soliman (Zagazig University, Egypt), Jeza Muhamad Abdul Aziz (University of Human Development, Sulaimani, Iraq), Jaffer Shah (Drexel University College of Medicine, Pennsylvania, USA), Pham Dinh Long Hung (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam), Yap Siang Jee (Universiti Sains Malaysia, Malaysia), Dang Thuy Ha Phuong (Pham Ngoc Thach University of Medicine, Vietnam), Tran Thuy Huong Quynh (Kansai Medical University, Osaka, Japan), Hoang Thi Nam Giang (The University of Danang, Vietnam), Vy Thi Nhat Huynh (University of Debrecen, Hungary), Nguyen Anh Thi (Toulouse III Paul Sabatier University, France), Nacir Dhouibi (University of Tunis El Manar, Tunisia), Truc Phan (Vinmec International Hospital, Vietnam), Duru Vincent C (Nnamdi Azikiwe University, Nigeria), Nguyen Hai Nam (Kyoto University, Japan), Sherief Ghozy (Mansoura University, Mansoura, Egypt).
National leads:
Afghanistan: Sayed Hamid Mousavi (Afghanistan National Charity Organization for Special Disease), Shafi Ullah Zahid (Jamhuriat Hospital), Kalimullah Wardak (Wazir Akbar Khan Hospital);
Bangladesh: Shyam Prakash Dumre (Nagasaki University), Farhana Nusrat (Sylhet MAG Osmani Medical College);
Brazil: Zainab Gandhi (C.U. Shah Medical College);
Cameroon: Joel Noutakdie Tochie (University of Yaounde 1);
Canada: Michael G. Blennerhassett (Queen’s University);
China: Yap Siang Jee (Universiti Sains Malaysia), Kefang Wang (Shandong University), Hongcan Shi (Yangzhou University);
Chile: Dmytro Pavlenko (Bogomolets National Medical University, Ukraine);
Ecuador: Estefanía Ochoa-Toasa (Laboratorio Clínico, Pontificia Universidad Católica del Ecuador, Laboratorio de Especialidades Medicas Ochoa&Ochoa), Shyam Prakash Dumre (Nagasaki University);
Egypt: Gehad Mohamed Tawfik (Ain Shams University), Kirellos Said Abbas (Alexandria University), Mostafa Elsayed Elsayed Hewalla (Alexandria University), Fatma A. Monib (Assiut University), Mahmoud Ali Alfadaly (Al-Azhar University-Damietta), Mona Hanafy Mahmoud (Ain shams university), Ezz eldeen Atef Derballa (Fayoum University);
Ethiopia: Zelalem Desalegn (Addis Ababa University), Tewodros Tesfa (Haramaya University);
Hong Kong: Rex Pui Kin Lam (The University of Hong Kong);
India: Akash Sharma (Guru Teg Bahadur Hospital), Shyam Prakash Dumre (Nagasaki University), Zahiruddin Quazi Syed (Datta Meghe Institute of Medical Sciences);
Indonesia: Harapan Harapan (Universitas Syiah Kuala), Ahmad Taysir Atieh Qarawi (Lower Westchester Medical Associates, P.C.);
Iran: Ali Khanmohamadi Hezave (Arak University of Medical Sciences);
Iraq: Mohammed Baqer Al-Jubouri (University of Baghdad), Selman Hussain Faris (University of Kerbala), Jeza Muhamad Abdul Aziz (University of Human Development, Sulaimani), Sadeq Al-Fayyadh (University of Baghdad), Salwa Ghazi Turki (University of Baghdad), Sabah Abdullah Jaafar (University of Al-Muthana), Iman Hussein Alwan (University of Baghdad);
Italy: Fabio Porru (Erasmus Medical Center, Rotterdam, The Netherlands), Stefano Greco (University of L’Aquila, Italy);
Japan: Kazumi Kubota (Yokohama City University), Atsuko Imoto (Nagasaki University), Nahoko Harada (University of Miyazaki), Anna Kubota (Keio University), Yoshiaki Iwashita (Shimane University Hospital), Takeshi Mizusawa (Niigata University), Emmanuel Oluwadare Balogun (Ahmadu Bello University, Nigeria);
Jordan: Tareq Mohammed Ali AL-Ahdal (Jordan University of Science and Technology), Mallak Alomoush (Hashmite University), Tareq Osaili (Jordan University of Science and Technology);
Libya: Marwa Saed Ali Emhamed (University of Tripoli);
Malaysia: Sze Jia Ng (Hospital Enche’ Besar Hajjah Khalsom), Ilham Ameera Ismail (Universiti Teknologi Mara), Kek Heng Chua (University of Malaya), Tengku Zetty Maztura Tengku Jamaluddin (Universiti Putra Malaysia);
Mexico: Dmytro Pavlenko (Bogomolets National Medical University, Ukraine), Brianda del Pilar Gómez Olvera (Autonomous University of Mexico State);
Morocco: Oumaima Outani (Faculty of Medicine and Pharmacy of Rabat);
Nepal: Shyam Prakash Dumre (Nagasaki University), Kamal Ranabhat (Tribhuvan University), Renu Bhandari Dumre (Nagasaki University);
Nigeria: Farouq Muhammad Dayyab (Infectious Diseases Hospital), Ahmad Abdulmajid Yakubu (Abubakar Tafawa Balewa University), Duru Vincent C (Nnamdi Azikiwe University), Deborah Tolulope Esan (Afe Babalola University), Pembi Emmanuel (State Ministry of Health, Adamawa State), Ahmadu Baba Usman (Federal Medical Centre Yola);
Pakistan: Ramesh Kumar (Health Services Academy Ministry of Health);
Palestine: Hosam Waleed Shaikhkhalil (Islamic University of Gaza), Ahmad Taysir Atieh Qarawi (Lower Westchester Medical Associates, P.C., USA), Emad I H Shaqoura (Islamic University of Gaza), Taj El-deen Shaat (Islamic University of Gaza), Loay Hidar Hamad (Islamic University of Gaza), Abdullah Rasmi Awwad (Islamic University of Gaza), Ahmad Samara (An-Najah National University);
Philippines: John Robert Carabeo Medina (University of the Philippines Manila), Allan Laurio Hilario (University of the Philippines Manila), Jose Ma. Moncada Angeles (University of the Philippines Manila), Fresthel Monica Marqueses Climacosa (University of the Philippines Manila), Van Jerwin Purificacion Mercado (University of the Philippines Manila);
Russia: Dmytro Pavlenko (Bogomolets National Medical University, Ukraine);
Serbia: Srdjan Stefanovic (University of Kragujevac);
South Africa: Indiran Govender (University of Pretoria);
Spain: Raigam Jafet Martinez-Portilla (Institut Clínic de Ginecologia, Obstetricia i Neonatologia);
Sri Lanka: N.D.B. Ehelepola (Teaching Hospital-Peradeniya), Rohitha Muthugala (Regional Virology Laboratory, Kandy);
Sudan: Anmar Homeida (Federal Ministry of Health), Shamael Thabit Mohammed Alhady (University of Gezira), Omer Ahmed (Federal Ministry of Health), Asma Yahya Ismail (Sudan International University);
Syria: Mosa Shibani (Syrian Private University), Basel Kouz (Damascus University);
Taiwan: Wen-Chien Ko (National Cheng Kung University Hospital);
Thailand: Surapon Nochaiwong (Chiang Mai University), Nut Koonrungsesomboon (Chiang Mai University), Shyam Prakash Dumre (Nagasaki University);
Tunisia: Nesrine Ben Hadj Dahman (University of Tunis El Manar);
UAE: Tareq Osaili (Jordan University of Science and Technology);
Ukraine: Dmytro Pavlenko (Bogomolets National Medical University, Ukraine), Tetiana Pavlenko (Oleksandriia Central City Hospital), Roman Pavlenko (Bogomolets National Medical University);
USA: George L. Anesi (University of Pennsylvania);
Vietnam: Truc Phan (Vinmec International Hospital), Tran Thuy Huong Quynh (Kansai Medical University, Osaka, Japan), Dang Thuy Ha Phuong (Pham Ngoc Thach University of Medicine), Luong Thi Trang (Danang Oncology Hospital), Pham Ba Tuyen (Traditional Medicine Hospital of Ministry of Public Security, Vietnam);
Zambia: Duncan Chanda (University Teaching Hospital);
Local collaborators:
Afghanistan: Hamed Shenwari (Jamhuriat Hospital); Sayed Maseehullah Hashimi (Rabia-e-Balkhi Hospital); Farwa Afzaly (Blossom Hospital); Abdul Wahid Noor (Ali Abad Hospital); Nasrat Alizai (Maiwand Hospital);
Albania: Irida Dajti, Jola Kërpaçi, Enxhi Vrapi (University Hospital of Obstetrics–Gynecology " Koço Gliozheni");
Algeria: Yassamine Ouerdane, Fella Ouerdane, Mohamed ElKhalil Bouaich, Imane Bakhtaoui (University Blida);
Australia: Dominic E Dwyer, Janette Taylor (Westmead Hospital);
Bangladesh: Orindom Shing Pulock, Susmita Dey Pinky, Tanjimul Hye Rafi, Senjuti Deepanwita (Chittagong Medical College); Alvee Ahsan, Raisa Nawal Mahboob (Mymensingh Medical College); Abdur Rafi, Ahsan Habib, Mohammad Fahim Faisal (Rajshahi Medical College); Soumik Kha Sagar, Farhana Rahman Luba, Saiful Islam Sourav, Sajibur Rahman (Sylhet MAG Osmani Medical College);
Brazil: Zainab Gandhi (C.U. Shah Medical College); Lirane Elize Defante Ferreto (Western Paraná State University), Moacir Antonio de Pauli Junior, Mirian Carla Bortolamedi da Silva (Hospital Regional do Sudoeste do Paraná); Guilherme Welter Wendt (Western Paraná State University);
Cameroon: Tebit Emmanuel KWENTI, Kouamo Gisele Wendy KAM (University of Buea); Nelson Njinyam (Banyo District Hospital); Elvins Tsaku (Centre Medical d’Arrondissement de Ngaoundal);
Canada: Nahal Farhani, Azar Bayat, Faith Tabije, Samreen Rizwan, Loreanne Kathleen Baino Manalac, Navreet Kaur Ubhi (Queen’s University);
Chile: José Tomás Ordóñez Aburto (University of La Frontera);
China: Jing Mou, Shouwei Zhang (The People’s Hospital of Rizhao); Cuiping Xu, Jianhong Qiao, Xingfeng Lin, Feifei Chen, Xiaorong Luan, Min zhang (Shandong University); Xiuli Wang, Li Chen (Shandong Provincial Third hospital); Xuejuan Cheng, Cuihua Song (The People’s Hospital of Zouping City); Ling Guo (Yidu central hospital of Weifang); MD Ariful Haque, Xiong Ying (Yan’an Affiliated Hospital of Kunming Medical University); Yongxiang Wang (Subei People’s Hospital); Jihong Lu (Yangzhou Hospital of Traditional Chinese Medicine); Kaizheng Gong (Yangzhou First People’s Hospital); Ying Zheng, Hongjuan Liu, Wenji Li (Yangzhou University); Wong Tin Wui (Universiti Teknologi MARA, Malaysia);
Ecuador: Gabriela Anasi Castillo, Santiago Ruales, María Marcela Bovera (Hospital de los Valles); Danny Patricio Flores Almeida, Denisse Miroslava Costales Quiroz (Hospital General Docente de Calderón); Ana Paola Capelo Rodriguez, Micaela Alejandra Navarrete Rengel, Oscar David Salazar Correa (Clínica Infes); Lucia Jeannete Zurita Salinas, Juan José Romero Carvajal, Cinthya Verónica Delgado Arteaga (Hospital Vozandes Quito);
Egypt: Rania Abdel Maguid, Hoda Aly Mohamed Omran, Ahmed Abdulgalil Yousif Mohammed, Atef Khairy Sharaf, Adel Reda Mustafa Hebashy, Reda Maher Moussa, Toka Aziz Fayze El-Ramly, Asmaa Reda Ahmed Ahmed Youssef, Mohamed Ibrahim Abdo Ibrahim, Chiristine Samuel Rezq, Mirna Ragy Shoukry, Mostafa Shehata Qatora, Mohammed Jawad Abuhassira, Mina Ragy Shoukry, Mostafa Mohamed Bastawesy, Ahmed ElSayed Bakry Mohamed Abdeltawab, Ayman Hafez Y, Mohamed A.Mekkawy (Alexandria University); Sara Mohammed Hashem, Amira Mohammed Mahmoud, Esraa G. Sayed, Mahmoud M.Saad, Abdelrahman G. Ramadan, Ahmed Mohamed Rashad, Aliaa Effat Said, Shehab Fathy Ahmed, Ziad Hassan Hamed, Mohamed Ashraf Salah, Mohamed Mahmoud Abdelkarem, Mahmoud Usama Fawzy, Rana Mahmoud Farghali, Nashwa Rafaat Foaud, Mariam Albatoul Nageh (Assiut University); Ahmed Hafez Saif Allam, Abdelrahman Amin Mahmoud Abdallah, Ahmed Gameel Nassef Abdallatif (Menoufia University); Mohamed Eid Alsadek, Mohammad Saad Isa, Ahmed Yousof, Alaa Saad Isa, Fathiya El-Raey, Abdallah Moustafa Ghanem, Atef Wahdan El-Rifai, Mennatullah Mohamed Eltaras, Ahmed Elsayad Salama, Mahmoud Abdulmonem Abulnaga, Nourhan Mohamed Hamdy, Aya Ali Abuzeid, Sarah Abd Elaziz Khader, Mai Alaa Eldin Temraz Elsebaie, Bassant Mohsen Taher Ragab, Youssef ElSaid Mohamed Shady, Abdallah Ashraf Mahmoud Ali, Abdelrahman Ashraf Mahmoud Ali, Dina Emad Said, Hawwa Abdullah Salih Albishari, Najma Abdelhady Mansour Mohammed, Eslam Mohamed Abd Elsalam (Ain Shams University); Noha Ali Abdelsamiee Ali (Al-Azhar University); Mohammed Salah Desokey, Abdelrahman Ahmad Elsamman, Ahmed Zakaria Khaleel, Mohamed Zaki Ali Eldahshory, Mohamed Moustafa Hussein (Aswan University Hospital); Sara S. Elsheikh, Dalia A. Deeb, Mohamed Refaat Badr (Zagazig University); Mohamed Fouad Ibrahim Abdrabo, Mohammed Maher Hadhoud (Tanta University); Gehad Taha Abdelwadoud, Nada Khaled Abdelsattar, Aya Ghiath Alrawi, Marwa Gamal Mustafa, Menna-Allah Sayed kamal, Hanaa Abdelmonem Hussien, Manar Mohammed Hosny, Taha Abdelsalam Ashraf Taha Abdelsalam, Alshaimaa Galal Mohamed, Hajar Ahmed Arafa, Mohamed Mahmoud Abd-ElGawad, Omnia Mohamed Abd Elsalam, Mahmoud Ahmed Farag, Radwa Hamdy Allam, Esraa Mostafa Kamal, Asmaa Khaled Mostafa, Mostafa Ramadan Mohamed, Habiba Safwat Ewais, Abdullah Ahmed Ahmed, Ahmed Taher Masoud, Mohamed Abdelmonem, Fatma Mohamed Sayed Manar Hamdy Mohammed, Ahmed Fares Ghannam (Fayoum University);
Ethiopia: Yirgu Gebrehiwot, Wondwossen Amogne (Tikur Anbessa Specialized Hospital); Tamrat Abebe (Addis Ababa University); Alem Abrha (Yekatit-12 Hospital Medical College); Mesay Arkew (Haramaya University); Daniel Gebretsadik (Wollo University); Chilot Yefredew (Dil-chora Referral Hospital);
France: Nguyen Duc, Malvy Denis, Perreau Pauline (University Hospital of Bordeaux); Constantin Jean-Michel (Sorbonne University);
Germany: Andreas Hecker, Matthias Hecker, Natascha Sommer (University Hospital of Giessen);
Greece: Dimitrios K. Manatakis, Panagiotis Vamvakas, Eleni Milisi (Athens Naval and Veterans Hospital);
Guatemala: Angel Alfonso Velarde Lopez, Ingrid Fabiola Castillo, Vicky De Falla (Liga Nacional Contra El Cáncer-INCAN);
Hong Kong: Grace Sin Man LAM (Pamela Youde Nethersole Eastern Hospital); Patrick Siu Chung LEUNG, Pauline Yeung NG, Wai Ching Simon SIN (The University of Hong Kong);
India: Subramaniam R, Suneesh Kuruvilla (Indira Gandhi Institute of Dental Sciences, Kothamangalam); Supram Hosuru Subramanya (Manipal College of Medical Sciences, Nepal); Ambica Rangaiah, Shashiraja Padukone (Bangalore Medical College and Research Institute); Suhrud Panchawagh, Shreepad Bhat (Smt. Kashibai Navale Medical College and General Hospital, Pune); Akshay Raut (R.C.S.M. Government Medical College, India); Ketty E Arce, Gerardo Alvarez-Uria (Rural Development Trust Hospital Bathalapalli); Sudhindra Baliga (Sharad Pawar Dental College); Chandrashekar Mahakalkar (Jawaharlal Nehru Medical College, Wardha);
Indonesia: Prattama Santoso Utomo (Universitas Gadjah Mada); Nurfanida Librianty (Universitas Indonesia); Ikram Ikram (Dr H Yuliddin Away Hospital); Nyoman Ananda Putri Prashanti (Bangli Hospital); Tri Novita Wulan Sari (Sungai Dareh Hospital);
Iran: Mehdi Harorani, Saeed Amini (Arak University of Medical Sciences); Behnam Masmouei (Shiraz University of Medical Sciences);
Iraq: Safad Riyadh Isam, Asmahan Adnan Abbas (University of Baghdad); Hayder Alaa Ahmed (Al-Nahrain University); Haneen Alaa Ahmed (Central Hospital for Pediatrics); Rangin Muhamad Hussein, Dashne Jalal Hama (Baxshin Hospital); Trifa Abdalla Mahmood, Darya Saeed Abdulateef, Heshu Sulaiman Rahman, Hemn Hassan Othman (University of Sulaimani); Dana Taib Gharib (Ministry of Health/ Directory of Sulaimani/ KCGH); Kawa Faraj Saadun (Respiratory and Chest Diseases Center, Asthma and Allergy Center); Staar Mohammed Qader (Tikrit University); Ahmed Saleh Hilal (North Oil Company- K1 Hospital); Hassan Abdullah Athbi, Ali Kareem Khudhair, Khamees Bandar Obaid, Ali Jabbar Abd Al-Husayn, Maytham Fawzy Salman, Haqi Ismael Mansoor, Zeki Sabah Musihb, Sajida Saadoon Oleiwi, Fatma Makee Mahmood (University of Kerbala); Ismael Hasan Jawad (Al Hilla Teaching Hospital); Raad Farhan Jabl (Ibn Al-Nafees Teaching Hospital);
Italy: Simone Piva, Ciro Paolillo (Spedali civili di Brescia); Sandro Mancinelli, Antonio Vinci, Fabio Ingravalle (University of Rome "Tor Vergata"); Maria Michela Gianino, Daniela Acquadro Maran (University of Torino), Riccardo Papalia (San Martino Hospital, Genova), Flavio Boraso (Azienda Sanitaria Locale Torino 3); Francesco Rosiello (University of Rome "La Sapienza"); Rosa Costantino, Gianluca Raffaele (Azienda Ospedaliera "Pugliese Ciaccio"); Aida Bianco, Davide Pepe, Francesca Licata, Silvia Mazzea ("Magna Græaecia" University of Catanzaro); Caterina De Filippo (Azienda Ospedaliera Universitaria "Mater Domini"); Davide Brunelli, Matteo Verzè, Fabrizio Nicolis (IRCCS Sacro Cuore Don Calabria Hospital); Diego Alberto Ramaroli, Stefano Tardivo (University of Verona); Angela Currà, Raffaele Bava (Ospedale Giulio Jazzolino); Antonella Rodinò, Matteo Galletta (Azienda Ospedaliera "Bianchi-Melacrino-Morelli”); Stefano Formentini, Mario Capasso (Ospedale Ca’ Foncello di Treviso);
Korea: Won Suk Choi (Korea University College of Medicine);
Japan: Yoshiaki Iwashita (Shimane University Hospital); Asami Ito (Mie University Hospital); Shinnosuke Morimoto (Kinan Hospital); Shinji Akitomi (National Defense Medical College); Rintaro Sawa (The Japan Medical Association Research Institute); Kaku Tamura (Japan Self-Defense Forces Central Hospital); Sachiyo Nagi, Tomohiko Sugishita, Daisuke Tokita, Kazunari Tanabe (Tokyo Women’s Medical University); Eri Tanaka, Chie Minamide, Kumiko Maeda (Hayama Heart Center); Hiromi Munakata, Makoto Hibino, Rie Suzuki (Shonan Fujisawa Tokushukai Hospital); Nobuaki Shinozaki, Morihiko Sato, Nobuyo Watanabe (Shonan Kamakura General Hospital); Yoshito Kadoya (Kyotango City Yasaka Hospital); Fumihiro Hayakawa (Shinshiro Municipal Hospital); Fumitoshi Yoshimine, Yoshihisa Hori, Youko Sugai (Niigata Prefectural Tokamachi Hospital); Yukiyoshi Kon, Sho Shimazu (Niigata Prefectural Sakamachi Hospital); Hayato Tsuruma, Atsushi Uchiyama (Sado Municipal Ryotsu hospital); Kyuma Ota (Niigata Prefectural Kakizaki Hospital); Kenji Takehara, Isao Miyairi (National Center for Child Health and Development); Shingo Kawaminami, Keisuke Kawahito (Tokushima Prefectural Kaifu hospital); Shusaku Mizukami (Nagasaki University); Joji Kayano, Kazuhiro Tanaka (Nagasaki Yuuai Hospital);
Jordan: Reem Hazza Ahmed Yahya Al-Jawlahi, Yousef Saleh Khader, Suleiman M. Momany, Faris Jamal ALAbed Abu Za’nouneh, Qusai Mohammad AlQudah, Ayham Mohammad Al Momani, Anas Abdel-Rauof Al-Nabulsi (Jordan University of Science and Technology); Fedaa Taha AlGhammaz (Irbid Specialty Hospital); Mohannad Diraneih (Amman Arab University); Khaled Ahamad Hasanein (Al-Essra Hospital); Jehad Sahli, Dania Alaawneh (The Hashemite University); Mo’men Ali Sisan (King Hussein Cancer Centre);
Lebanon: Ghassan Al-Awar, Georges Minassian, Rita Ayoub, Joelle Hassanieh (American University of Beirut);
Libya: Aliyah Mustafa Alshareef, Malak Masoud Ahmed Alduwayb, Safa Abdalhakem Elrais, Mohamed Omar M. Alhabbasi, Faeq Alhadi Ahmed, Adnan Alhadi Salah Ben-Abdallah, Marwa Mohammed Morgom, Muaad Alhussein Etturki (University of Tripoli); Mohammed Khayri Aboubeirah (Elmegib University);
Malaysia: Khasnur Abd Malek, Nur Fazlinda Md Shah (Universiti Teknologi MARA); Suat Moi Puah, Vijayan Munusamy, Ong Hang Cheng, Suvarnesh Tarumma, Siti Zuhairah Mohamad Razali, Mohd Afiq Mohd Nor, Sasheela Ponnampalavanar (University of Malaya); Ping Chin Lee, Jennifer Kui Ling Chee, Alvin Oliver Payus (Universiti Malaysia Sabah); Ping Yein Lee, Siti Zulaikha Zakariah, Rosni Ibrahim, Niazlin Mohd Taib, Syafinaz Amin-Nordin, Muhammad Mohd Isa, Aditya Adawiah Darwis, Fauziah Adnan (Universiti Putra Malaysia); Aishah Hani Azil, Umi Kalsom Ali, Azlin Mohd Yasin, Sharifah Azura Salleh (Universiti Kebangsaan Malaysia);
Mexico: Brianda del Pilar Gómez Olvera (Autonomous University of Mexico State);
Morocco: Zaineb Benslimane, Lina Boualila, Ihsane Skitioui, Belyamani Lahcen (Faculty of Medicine and Pharmacy of Rabat); Ghassane El Adib, Hamza Belakbyer (Faculty of Medicine and Pharmacy of Marrakech); Aymane Outani (Abokrat Health Institute); Ahmed Ayad (Faculty of Medicine Kasr Alainy);
Nepal: Kalyan Sapkota, Bhojraj Adhikari, Bijaya Dhakal (Bharatpur Hospital); Basu Dev Pandey, Anup Bastola, Sher Bahadur Pun, Shrawan Kumar Mandal (Sukraraj Tropical and Infectious Diseases Hospital); Pradeep Vaidya, Pradip Gyanwali, Amod Kumar Poudyal, Komal Raj Rijal, Prakash Ghimire (Tribhuvan University); Sujan Babu Marahatta, Durga Khadka Mishra (Manmohan Memorial Institute of Health Sciences); Dhiraj Acharya (The University of Chicago); Pukar Ghimire, Madhav Ghimire (College of Medical Sciences Teaching Hospital); Deelip Raj Neupane, Samip Thapaliya (Parkland Hospital); Roshan Chhetri, Deebya Raj Mishra, Shailesh Mani Pokharel (BP Koirala Institute of Health Sciences); Bidesh Bista, Samir Neupane, Bishesh Sharma Poudyal (Civil Hospital); Kishor Pandey (Nepal Academy of Science and Technoogy); Shishir Gokhale, Deependra Hamal, Rajani Shrestha (Manipal College of Medical Sciences); Kedar Prasad Ceintury, Kishor Bhandari, Achyut Raj Karki (Bir Hospital); Bishwanath Acharya (Thammasat University); Pardip Kumar Oli, Durga Laxmi Shrestha (Bheri Zonal Hospital); Mahendra Prasad Shrestha, Bibek Kumar Lal, Dipendra Raman Singh (Ministry of Health and Population); Meghnath Dhimal (Nepal Health Research Council);
Netherlands: Yvette Loeffen (Pediatrician ID Specialist);
New Zealand: Ibrahim S. Al-Buasidi (Christchurch School of Medicine, University of Otago); Sarah Metcalf (Christchurch Hospital);
Nigeria: Farouq Muhammad Dayyab (Infectious Disease Hospital); Garba Iliyasu (Aminu Kano Teaching Hospital); Abdulrazaq Garba Habib (Bayero University); Bashir Garba Ahmad, Faiza Sadauki Kibiya, Sani Umar (Muhammad Abdullahi Wase Teaching Hospital); Awwal Musa Borodo, Sulaiman Ibrahim Sulaiman, Amira Muhammad Awwal (Murtala Muhammad Specialist Hospital); Yunusa Sanusi (Hasiya Bayero Paediatric Hospital); Abdurrahman A Sadiq, Zuwaira Hassan, Ibrahim Mahmood Maigari (Abubakar Tafawa Balewa University Teaching Hospital); Ahmad Abdulmajid Yakubu, Hassan Shuaibu Musa, Yusuf Abdu Misau (Abubakar Tafawa Balewa University Clinic); Aisha Abdulmalik Abdullahi, Habiba Ismail, Adamu Muhammad (State Specialist Hospital Bauchi); Zulfa’u Abubakar Isah, Sumayya Muhammed (Primary Healthcare Center Kofar Ran Bauchi); Lukman Muhammad, Abdullahi Sani Gadama (Bayero University); Bako Abubakar Muhammad (Infectious Disease Hospital Bayara Bauchi); Muhammad Mustapha Mubarak, Murtala Abubakar, Muhammad Abdullahi Umar (General Hospital Gamawa Bauchi State); Robinson Yusuf, Adamu Lawiza Haruna, Khalid Abubakar Isah (Private Healthcare provider and Women and children Hospital); Dr Muhammad Jamilu Dauda, Sulaiman Aminu Tukur (Almanzoor Hospital Bauchi); Babatunde Adewale, Olusola Ajibaye, Adewale Ojogbede (Nigerian Institute of Medical Research); Bolanle Olarewaju Awoyomi (Federal Medical Centre); Adejuwon Adewale Adeneye (Lagos State University College of Medicine); Olawunmi Victoria Ajibaye (Lagos University Teaching Hospital); Oluwatoyin Ganiyu Olawale, Elon Isaac, Mohammed M Manga (Federal Teaching hospital, Gombe); Deborah Tolulope Esan, Tunrayo Oluwadare, Funmilayo Stella Oluwafemi (Afe Babalola University); Theophilus Olaide Esan, Segun Matthew Agboola (Federal Teaching Hospital, Ido-Ekiti); Lawal Ismail Akinlade, O. A Osinupebi, Osisanwo Deborah (Olabisi Onabanjo University Teaching Hospital); Oduyebo Oyinlola O, Olise Kingsley Ejechi, Adewole Monisade Francisca (Lagos University Teaching Hospital); Ahmadu Baba Usman (Federal Medical Centre (F.M.C) Yola); Pembi Emmanuel, Abdulmalik Yusufu Kadabiyu G. Jones, Owoseni Olufunke Abosede, Francis Ashesla Mercy, Okon Nsikak Joseph (State Ministry of Health, Adamawa State); Philip ThankGod Duru (Specialist Hospital Yola); Bulus Nuhu (IHVN Institute of Human Virology); Collins John, Nathan Shehu (Jos University Teaching Hospital);
Pakistan: Assad Hafeez (Health Services Academy Ministry of Health); Abdul Wali Khan, Manohar Lal (Federal General Polyclinic Services Hospital); Prof Dr. Jai Krishin (Pakistan Institute of Medical Sciences); Ramesh Kumar (Health Services Academy); Zafar Fatmi (Aga Khan University); Rashid Qadeer, Malaika Jawaid Siddiqui, Erfa Tahir (Dr. Ruth Pfau Civil Hospital); Ashraf Jahangeer Al’Saani, Ramsha Zafar, Asma Burney (Dow University Hospital); Ayesha Iqbal (Services Institute of Medical Sciences Lahore); Zair Hassan (Lady Reading Hospital); Iftikhar Ali (Paraplegic Centre Hayatabad Peshawar); Muneeb Jan (Khyber teaching hospital, Peshawar); Mehreen Zakir (Sir Syed Hospital); Tehnia Nuzhat (Maternity and Child health center Abdullah Gabol Goth);
Palestine: Omar Riad Alnajjar, Ibrahim Tawfeeq Abdulhadimaqadma, Nour Abdallah abo Shawish, Minyar Ismael Wali, Hitham ibrahem toman, Aya Yassin, Ali wael alhabash, Ahmed Bassam Abu Thaher, Ruba Shaqoura, Mohammed abo abdo, Marah Emad Abu Selmiya, Abd AlRahman Alashqer, Remah Tayseer Jneed, Ahlam Shaheen, Ahmed Al-azzamy, Maryam Shaheen, Eman Jalhum, Mahmoud Ahmad Abo Ouda, Shadi Nahed Aljerjawi, Alaa Naser Alsharef, Ahmed Emad Habboub, Ameer Helles, Motaz Zakaria Hammad, Osama Sweid (Islamic University of Gaza); Asil Nahed Aljerjawi, Salsabeel Hani Alhaw(Alazhar University of Gaza); Faris Hammad, Ihab N. Tahboub, Amjad Samara, Ala’a Samir Mohammad Alfuqaha, Moutaz W. Sweileh (An-Najah National University); Hasan Arafat (Istishari Arab Hospital);
Paraguay: Carlos Miguel Rios-González, Pablo Martinez Acosta (National University of Caaguazu);
Philippines: Paul Adrian Vidanes Pinlac, Angelica Anne Eligado Latorre, Kim Carmela Dee Co, Sharon Yvette Angelina Manalo Villanueva, Maria Margarita Maiquez Lota, Evalyn Alarkon Roxas (University of the Philippines Manila); Harold Robin Facing Laroa (Ospital ng Maynila Medical Center); Manila T. Villalon (Laguna Medical Center); Jehiel L. Fabon (Novaliches District Hospital); Denim E. Maghanoy (The Barrio Program Rural Health Physician); Nerissa G. Sabarre (Pasig City General Hospital);
Russia: Valeriya Mikhailova (First Moscow State Medical University); Mahir Gachabayov, Abakar Abdullaev (Vladimir City Emergency Hospital);
Serbia: Srdjan Stefanovic, Slobodan Jankovic, Milos Milosavljevic (University of Kragujevac); Danica Radomirovic, Milica Milosavljevic (General (Regional) Hospital of Kosovska Mitrovica);
Somalia: Abdulfatah Hassan Dhaqane, Hassan Yusuf Roble, Abdifatah Abdullahi Jalei, (Somali Sudanese Specialized Hospital), Shyam Prakash Dumre (Nagasaki University);
South Africa: Indiran Govender, Brett van Coppenhagen, Olga Maphasha (University of Pretoria);
Spain: Francesc Figueras Retuerta, Maria Dolores Gomez Roig (Institut Clínic de Ginecologia, Obstetricia i Neonatologia, Universitat de Barcelona); Rafael Sierra (Puerta del Mar University Hospital); Eva del Amo (Vall d’Hebron institut de Reçerca. Barcelona); Magda Campins (Vall d’Hebron institut de Reçerca. Barcelona);
Sri Lanka: H.S.K.Seneviratne, Ayodhya Priyadharshi Senanayake (Sirimavo Bandaranaike Specialized Children Hospital (SBSCH)), Chamara Dalugama (Teaching (General) Hospital-Peradeniya); DRRHB Dissanayake, MRM Rizky Aazath (District General Hospital-Nuwara Eliya); WMNP Buddhadasa, B.M.L.S.Basnayake (National Hospital-Kandy); WALP Weerasekara (District General Hospital-Trincomalee); KGCYSB Weerakoon (District Base Hospital-Teldeniya); Saranga Sumathipala, K.T.Rajith Jayasanka, Thilini Premadasa (Teaching Hospital Anuradhapura); Vaithehi Francis (Eastern University of Sri Lanka);
Sudan: Goutoof Abdelkhalig Elemam Yousif, Hadeel Hamza Mohammed Abaker, Mohamed Daffalla Awadalla Gismalla, Adam Mohamed Ibrahim Adam, Makarim Awad Moaz Omer, Rania Ahmed Elsiddig Hassan, Alaa Abaas Elsharief Mohammed Omer, Reham Abdelgader Alnaeem Babiker, Alkhansa Hamid Mohamed Alkhider, Elamin Abuobaida Elamin Mohamed, Maram Elgaylani Abdalla Eltayeb, Iman Hassan Mirgani Mohammed, Asma Mutasim Elrasheed Ghalib, Lamia MohyEldin Merghani Alkhder, Durar Amin Abdelbagi Musa, Mohammed Mutasim Ahmed Abudawa, Ola Mutasem Mohammed Dafallah, Omnia Ahmed Ben Ouf Mohamed (University of Gezira); Leena Hijazi Osman Ahmed (University of Kassala); Ibrahim Iyad Almharat, Khadiga Isameldin Elnour, Roa Abdel-Hafez Musa, Yousif Sultan Abdelrahim (University of Bakhtalruda); Samah Mohammed Ibrahim Zaroog, Fatima Hassan Mohammed Fadelalmawla (West Kordufan University); Namareg Mohamed Edris Khiri, Tagwaa Elser Mohammed Ahmed Babiker (University of Khartoum); Mohannad Shaban, Radi Tofaha Alhusseini, Mohammed Alfatih, Malik Ahmed Malik Ahmed, Mohamed Hamid Abdelsalam Mohamed, Mariam Mohamed Ali, Mohamed Faroug Ali Yassin, Jumaa Mohammed Abdallah Hamed, Ali Ahmed Rabih Idriss, Mohajer Ibrahim Hassan Ismaeil, Hussain Mohamed Ahmed Khalifa, Omer Saeed Mohamed Saeed, Ahmed Eltag Elnagi Adam, Mohamed Hajhamad Abdoalazez Mohamed Elamin, Yaseen Muhammed Abdelhafeez Hamid, Waad Elzamali Elmonower, Mohamed Abdulkarim Mohamed Abdulrahim, Baha Aldeen Abdalaziz Alshareif, Tebyan Elbagir Elshiekh Mohamed, Hajer Hatim Hassan Ahmed, Mohammed Atif Abbas Mohammed Ahmed (Alzaiem Alazhari University, Khartoum); Asrar Abobkr Ishag Dawood, Rashed Yagoub Adam Abdalla, Saddam Adam Alnour Mohammed, Mohammed Ibrahim Omer Abdalla (University of Bahri); Malaz Salah Osman Gurashi (University of Science and Technology); Rawan Raad Hassan Elrufai, Rawan Hassan Adm Idrys (Sudan University of Science and Technology); Alaa Eldirdiri Elgaili Eldirdiri (Ibn Sina University); Albokhary Salih Adam Abkar (Nahda College); Wishah Mohammednour Ahmed, Waad Eltayeb Ageib Elsheikh, Malaz NasrEldin Elaagib Ahmed, Elrasheed Ghalib Abdalrhman (Omdurman Islamic University); Tarig Abdelwahab Abdelrahim Elnour (Clinic of Khartoum Refinery Company);
Syria: Mosa Shibani, Abdallah Altorkmani, Ahmad Rmman, Bisher Sawaf, Mhd Amin Alzabibi, Hlma Ismail, Humam Armashi, Mohamad Ziab Chebat (Syrian Private University); Ahmad Alkhaledi, Danny Hadidi, Hind Kazem, Hiba Mardini, Sara Naoura, Omar Alneser, MHD Bahaa Aldin Alhaffar, Aram Abbas, Ibrahim Alorfhli, Ibrahim Shammas, Osama Al Habbal (Damascus University);
Taiwan: Nai-Ying Ko, Nan-Yao Lee (National Cheng Kung University Hospital);
Tanzania: Jaffu Othniel Chilongola, Florida Muro (Kilimanjaro Christian Medical Center);
Thailand: Krongkarn Sutham, Poramed Winichakoon, Chidchanok Ruengorn, Ratanaporn Awiphan (Chiang Mai University); Kittima Bangpattanasiri, Piamlarp Sangsayunh, Sakkarin Kungsukool, Anek Kanoksilp (Central Chest Institute of Thailand); Watsamon Jantarabenjakul, Opass Putcharoen, Leilani Paitoonpong, Gompol Suwanpimonkul (King Chulalongkorn Memorial Hospital); Thanyawee Puthanakit (Chulalongkorn University); Suparat Kanjanavanit, Rathakarn Kawila (Nakornping Hospital); Woravut Kowatcharakul (Sansai Hospital); Sirisak Nanta (Maesai Hospital);
Trinidad & Tobago: Rajeev Peeyush Nagassar, Darren Kendall Dookeeram, Keston Daniel, Saskia Ramkissoon-Bain (Eastern Regional Health Authority (ERHA)); Shyam Prakash Dumre (Nagasaki University);
Tunisia: Hamida Maghraoui (Rabta University Hospital); Amal Jebali, Salma Ben Saber, Wajdi Kacem, Nacir Dhouibi, Nouha Dissem, Ahmed Nefzi, Farah Bahri, Majdi Ben Romdhane, Faten Tlili (University of Tunis El Manar); Riadh Ben Rhaiem, Ines Trabelsi (University of Monastir); Hanen Ben Ammar, Emira Khelifa (Tunis El Manar University Razi Hospital); Zied Moatemri (Principal Military Hospital of Instruction of Tunis); Kawthar Dhib, Omar Mastouri, Chams Zarrad (University of Sousse); Ahlem Aissa (Enfidha Hospitals); Zeineb Teyeb, Abir Malouch (Hospital of Intern Security Forces); Mouna Gara, Asma Ladib, Lotfi Grati (El Omrane Hospital); Omar Ammous, Zahra Charmi, Mohamed Ksentini (Faculty of Medicine, University of Sfax);
UAE: Amina AI-Marzouqi (University of Sharjah-University Hospital);
Ukraine: Olha Tkachuk (Bogomolets National Medical University); Iryna Kudlatska-Tyshko, Ali Dzhemiliev (Shupyk National Medical Academy of Postgraduate Education);
USA: George L. Anesi (Hospital of the University of Pennsylvania); Robyn Scatena, Pavan V. Ganapathiraju (Norwalk Hospital & Danbury Hospital); Kelley M. Anderson (MedStar, Washington Hospital Center);
Vietnam: Le Ngoc Phu, Pham Thi Minh Chau, Tran Hoang Thanh Hang (Danang Hospital); Dinh Thanh Nhan, Nguyen Thi Phuong Diem (Family Hospital); Le Van Cuong, Le Van Sy, Do Xuan Tien (Thanh Hoa General Hospital); Nguyen Thi Minh Trang, Nguyen Thi Mai, Duong Thanh Trang Dai (Quang Nam Hospital for Women and Children); Ho Van Han, To Le Na, Dang Phuong Thinh (Nhan Dan Gia Dinh Hospital); Vo Nguyen Trung, Ha Manh Tuan (University Medical Center Campus No.2); Nguyen Minh Tuan, Du Tuan Quy, Truong Huu Khanh, Nguyen Thanh Hung, Ngo Ngoc Quang Minh (Children’s Hospital 1); Trinh Huu Tung, Pham Thai Son, Nguyen Xuan Thuy Quynh, Do Chau Viet, Nguyen Minh Ngoc (Children’s Hospital 2); Nguyen Thi Hien, Tran Quoc Hung, Nguyen Thi Hoai Phuong (Hue City Hospital); Nguyen Ngoc Linh, Nguyen Quoc Thang, Nguyen Tien Manh (My Duc Psychiatric Hospital); Nguyen Van Tien (Quynh Phu General Hospital); Ta Van Tram, Do Quang Thanh, Le Quang Tin (Tien Giang Center General Hospital); Mai Ngoc Luu, Lam Hoang Cat Tien, Le Thi Thu Thao, Nguyen Thanh Van (Nguyen Tri Phuong Hospital); Nguyen Van Dang, Truong Xuan Hung (199 Hospital); Vu Nam, Tran Thai Ha, Vu Thi Thu Trang (National hospital of traditional medicine); Le Thi Hoai Anh, Le Thi Thuy, Le Van Truong (Traditional Medicine Hospital of Ministry of Public Security, Vietnam); Tran-Thuy Nguyen, Nguyen Cong Huu, Pham Thi Thoa (E Hospital); Le Duc Tho, Pham Le Xuan Huy, Nguyen Van Thoai (Military Hospital 211); Vo Thi Thuy, Le Quang Duan, Doan Van Hoai Nam (Nghe An Northwest Regional Hospital); Nguyen Tri Thuc, Le Quoc Hung, Phung Manh Thang, Lam Viet Trung, Dang Vu Thong (Cho Ray Hospital); Le Thuong Vu (University of Medicine and Pharmacy at Ho Chi Minh city); Nguyen Duc Truong, Vu Truong Son, Tran Xuan Tiem (FV Hospital); Phan Thi Hang, Hoang Thi Diem Tuyet (Hung Vuong Hospital); Hoai-Nam Thai (University Medical Center Ho Chi Minh City), Dieu-Thuong Thi Trinh, Van-Dan Nguyen, Minh-Man Pham Bui (University of Medicine and Pharmacy at Ho Chi Minh City); Nguyen Thanh Phuoc, Dao Anh Dung (Cao Van Chi Hospital, Tay Ninh); Nguyen Tran Nam, Nguyen Trong Nhan, Vuong Kien Thanh, Lam Tuyet Trinh (City Children’s Hospital of Ho Chi Minh City);
Zambia: Duncan Chanda (University Teaching Hospital, Lusaka); Bright Nsokolo (Levy Mwanawasa General Hospital); Gershom Chongwe (Ndola Teaching Hospital); Katongo Mutengo (Livingstone Central Hospital).
Protocol and questionnaire translators:
Albanian: Irida Dajti, Jola Kërpaçi, Enxhi Vrapi, Jehona Neziraj, Eldona Hajdinaj, Klea Beqiraj, Amina Cani, Anila Sinani, Lorenc Bellani;
Arabic: Mona Hanafy Mahmoud, Kirellos Said Abbas, Fatima A. Monib, Dina Emad, Mina Ragy, Mirna Fawzy, Moosa Hani Shibani, Hosam Waleed Shaikhkhalil;
Bengali: Sajibur Rahman, Orindom Shing Pulock, Farhana Nusrat, Abdur Rafi, Ima Islam, Nahida Hannan Nishat, Muhammad Rashidul Hashan, Bishwanath Acharya, Shyam Prakash Dumre;
Chinese: Lim Yi Liang, Brenda Phang Joo Yee, Tan Geok Eng, Juwie Chuah, Phoong Yu Lian, Yap Siang Jee, Li Chuin Chong, Ahmad Taysir Atieh Qarawi, Ng Sze Jia, Nguyen Hai Nam;
French: Ahmad Taysir Atieh Qarawi, Nacir Dhouibi, Wiem Belhadj, Ahmed Nefzi, Fatin Tlili, Nesrine Ben Hadj Dahman, Nouha Dissem, Salma Ben Saber, Oumaima Outani, Zaineb Ben Slimane;
Hindi: Akash Sharma, Akshay Raut, Suhrud Panchawagh, Adnan Mansuri;
Indonesian: Ichan Pan, Harapan Harapan, Ally Molly;
Italian: Simone Piva, Daniela Acquadro Maran, Maria Michela Gianino, Fabio Porru, Riccardo Papalia;
Japanese: Koji Aoki, Akiko Saito, Yoshimi Nitta, Atsuko Imoto;
Kurdish: Trifa Abdalla Mahmood, Heshu Rahman, Darya Saeed, Kawa Faray, Dana Taib, Jeza Muhamad Abdul Aziz, Hemn Othman;
Nepali: Kamal Ranabhat, Renu Bhandari, Dhiraj Acharya, Bishwanath Acharya, Kishor Pandey, Shyam Prakash Dumre;
Persian: Fatemeh Oskouie, Fereydoon Khayeri, Naiemeh Seyedfatemi, Nahla Farhani, Sedighe Karimzadeh, Mona Mahmoud;
Portuguese: Filipa Ribeiro Lucas, Maria Margarida Ribeiro, Bernardo Soares;
Russian: Mariia Pavlenko, Dmytro Pavlenko, Roman Pavlenko;
Spanish: Julio Aguilar Morales, Antonio M Quispe, Briseida Jiménez Velázquez, María Fernanda Paz y Miño, Diana Lip Sosa, Riagam Jafet Martinez Portilla;
Thai: Nut Koonrungsesomboon, Watsamon Jantarabenjakul, Bishwanath Acharya, Shyam Prakash Dumre;
Urdu: Usman Ghani, Muhammad Saeed, Somia Iqtadar;
Vietnamese: Vuong Thanh Huan, Truc Phan, Mai Ngoc Luu, Vu Quoc Dat, Hoang Thi Nam Giang, Vuong Ngoc Thao Uyen, Hoang-Minh NGUYEN, Tran Nu Thuy Dung, Nguyen Phuc Nguyet Anh, Pham Thai Son, Minh-Man Pham Bui.
Data Validators:
Afghanistan: Tran Nu Thuy Dung;
Albania: Irida Dajti, Jola Kërpaçi, Enxhi Vrapi, Tran Nu Thuy Dung;
Algeria: Tran Nu Thuy Dung, Trang Huynh;
Bangladesh: Mennatullah Mohamed Eltaras;
Cameroon: Hoang-Minh NGUYEN;
Chile: Le Van Truong, Nguyen Thi Linh Hue;
China: Yap Siang Jee; Vy Thi Nhat Huynh, Hoang-Minh NGUYEN;
Ecuador: Raigam Jafet Martinez-Portilla, Tran Nu Thuy Dung;
Egypt: Mohammed Soliman, Mennatullah Mohamed Eltaras, Shamael Thabit Mohammed Alhady, Ezz eldeen Atef Derballa, Asmaa Khaled Mostafa, Nada khaled Abdelsattar, Abdullah Ahmed Ahmed, Taha Abdelsalam Ashraf Taha, Mahmoud Ahmed Farag, Hanaa Abdelmonem Hussien, Ahmed Taher Masoud, Mohamed Abdelmonem, Manar Hamdy Mohammed, Hoang-Minh NGUYEN, Trang Huynh;
Ethiopia: Hai-Yen Tran; Mohammed Soliman, Shamael Thabit Mohammed Alhady, Mennatullah Mohamed Eltaras;
France: Tran Nu Thuy Dung;
Greece: Le Van Truong, Vu Thi Thu Trang;
Guatemala: Raigam Jafet Martinez-Portilla, Tran Nu Thuy Dung;
India: Akash Sharma, Nguyen Thi Linh Hue, Yap Siang Jee, Mallak Alomoush, Mona Hanafy Mahmoud;
Indonesia: Kadek Agus Surya Dila (Pratama Giri Emas Hospital);
Iran: Tran Nu Thuy Dung;
Iraq: Jeza Muhamad Abdul Aziz, Tran Nu Thuy Dung;
Japan: Vu Thi Thu Trang, Atsuko Imoto, Le Van Truong, Koji Aoki, Akiko Saito;
Jordan: Mohammed Soliman, Mallak Alomoush, Hoang-Minh NGUYEN;
Lebanon: Trang Huynh;
Malaysia: Nguyen Anh Thi, Vy Thi Nhat Huynh, Dang Thuy Ha Phuong, Mohammed Soliman, Tran Thuy Huong Quynh, Vuong Ngoc Thao Uyen;
Mexico: Raigam Jafet Martinez-Portilla, Nguyen Thi Linh Hue, Le Van Truong;
Morocco: Hoang-Minh NGUYEN, Trang Huynh;
Nepal: Tran Nu Thuy Dung;
New Zealand: Trang Huynh;
Nigeria: Vu Thi Thu Trang, Le Van Truong;
Pakistan: Vu Thi Thu Trang, Le Van Truong;
Palestine: Hosam Waleed Shaikhkhalil;
Paraguay: Le Van Truong, Vu Thi Thu Trang;
Philippines: Luu Ngoc Mai, Vuong Ngoc Thao Uyen, Vy Thi Nhat Huynh, Tran Thuy Huong Quynh, Nguyen Anh Thi;
Russia: Dmytro Pavlenko, Nguyen Thi Linh Hue;
Serbia: Trang Huynh;
South Africa: Vu Thi Thu Trang, Le Van Truong;
Spain: Raigam Jafet Martinez-Portilla, Hai-Yen Tran;
Sri Lanka: Hai-Yen Tran;
Sudan: Mona Hanafy Mahmoud, Jeza Muhamad Abdul Aziz, Mohammed Soliman, Mennatullah Mohamed Eltaras, Pham Dinh Long Hung, Vuong Ngoc Thao Uyen;
Syria: Basel Kouz, Ahmad Alkhaledi, MHD Bahaa Aldin Alhaffar, Hoang-Minh NGUYEN, Trang Huynh;
Taiwan: Vuong Ngoc Thao Uyen;
Tanzania: Le Van Truong, Vu Thi Thu Trang;
Thailand: Luu Ngoc Mai, Pham Dinh Long Hung, Dang Thuy Ha Phuong;
Tunisia: Tran Nu Thuy Dung, Hoang-Minh NGUYEN, Trang Huynh;
UAE: Le Van Truong, Vu Thi Thu Trang;
Ukraine: Dmytro Pavlenko, Nguyen Thi Linh Hue;
USA: Le Van Truong, Vu Thi Thu Trang;
Vietnam: Tran Thuy Huong Quynh; Yen-Xuan Thi Nguyen; Luong Thi Trang; Pham Dinh Long Hung;
Zambia: Vu Thi Thu Trang, Le Van Truong.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
• TMGH-Global COVID19 project was supported in part by the School of Tropical Medicine and Global Health, Nagasaki University. • E.O.B (Emmanuel Oluwadare Balogun) is a FLAIR Research Fellow of the Royal Society, UK., and supported by the UK Government as part of the Global Challenge Research Fund (GCRF) through a partnership between the African Academy of Sciences and the Royal Society, UK (no. FLR\R1\190353 to EOB). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. • The funders (Lower Westchester Medical Associates, Asia Shine Trading & Service CO. LTD and P.N. Lee Statistics and Computing Ltd, UK) provided support in the form of salaries for authors [A.T.A.Q., D.N.H.T., P.N.L.], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘Author Contributions’ section.
References
- 1.Wu Y, Ho W, Huang Y, Jin D-Y, Li S, Liu S-L, et al. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet. 2020;395(10228):949–50. doi: 10.1016/S0140-6736(20)30557-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg Infect Dis. 2020;26(7):1470–7. doi: 10.3201/eid2607.200282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–28. doi: 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morens DM, Daszak P, Taubenberger JK. Escaping Pandora’s box—another novel coronavirus. N Engl J Med. 2020;382(14):1293–5. doi: 10.1056/NEJMp2002106 [DOI] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 6.Livingston E, Bucher K. Coronavirus Disease 2019 (COVID-19) in Italy. JAMA. 2020;323(14):1335. doi: 10.1001/jama.2020.4344 [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. COVID Data Tracker—Cases & Deaths among Healthcare Personnel. Center for Disease Control and Prevention; 2021. [cited 2021 November 2]. Available from: https://covid.cdc.gov/covid-data-tracker/#health-care-personnel. [Google Scholar]
- 8.Sasangohar F, Jones SL, Masud FN, Vahidy FS, Kash BA. Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesth Analg. 2020;131(1):106–111. doi: 10.1213/ANE.0000000000004866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Toole Á, Scher E, Underwood A, Jackson B, Hill V, McCrone JT, et al. Assignment of Epidemiological Lineages in an Emerging Pandemic Using the Pangolin Tool. Virus Evol. 2021;veab064. https://cov-lineages.org/index.html#global_reports doi: 10.1093/ve/veab064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Center for Disease Control and Prevention. Healthcare Professional Preparedness Checklist For Transport and Arrival of Patients With Confirmed or Possible COVID-19. Center for Disease Control and Prevention; 2020. [cited 2020 Jan 24]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/downloads/hcp-preparedness-checklist.pdf. doi: 10.3389/fpubh.2020.00502 [DOI] [Google Scholar]
- 11.Taber KS. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Research in Science Education. 2018;48(6):1273–96. [Google Scholar]
- 12.Ursachi G, Horodnic IA, Zait A. How Reliable are Measurement Scales? External Factors with Indirect Influence on Reliability Estimators. Procedia Economics and Finance. 2015;20:679–86. [Google Scholar]
- 13.World Bank Data Team. New country classifications by income level: 2019–2020. World Bank Blogs. NW Washington, DC 20433 USA; July 01, 2019. [cited 2020 June 30]. Available from: https://blogs.worldbank.org/opendata/new-country-classifications-income-level-2019-2020. [Google Scholar]
- 14.United Nations Development Programme. Human Development Report—Human Development Index (HDI). United Nations Development Programme;2019. [cited 2020 June 30]. Available from: http://hdr.undp.org/en/content/human-development-index-hdi. [Google Scholar]
- 15.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99. doi: 10.1002/sim.4067 [DOI] [PubMed] [Google Scholar]
- 16.Agrawal R, Srikant R. Fast algorithms for mining association rules. In: Bocca J, Jarke M, Zaniolo C, eds. VLDB94. Proceeding of the 20th International Conference on very large databases; 12–15 September 1994; Santiago, Chile. San Francisco: Morgan Kaufmann Publishers; 1994; 487–499. Available from: http://www.vldb.org/conf/1994/P487.PDF.
- 17.Hahsler M, Chelluboina S. Visualizing association rules: Introduction to the R-extension package arulesViz. R project module. 2011:223–38. Available from: cran.r-project.org/web/packages/arulesViz/vignettes/arulesViz.pdf. [Google Scholar]
- 18.Wickham H. ggplot2. WIREs Comp Stat. 2019;3(2):180–185. [Google Scholar]
- 19.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. Available from: https://www.R-project.org/. [Google Scholar]
- 20.Altaf W, Shahbaz M, Guergachi A. Applications of association rule mining in health informatics: a survey. Artif Intell Rev. 2017;47(3):313–40. [Google Scholar]
- 21.Qarawi ATA, Ng SJ, Gad A, Luu MN, Al-Ahdal TMA, Sharma A, et al. Study Protocol for a Global Survey: Awareness and Preparedness of Hospital Staff Against Coronavirus Disease (COVID-19) Outbreak. Front Public Health. 2021;9:853. doi: 10.3389/fpubh.2021.580427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yayi A, Laing V, Govule P, Onzima RADDM, Ayiko R. Performance of epidemic prevention, preparedness and response in West Nile Region, Uganda. Int J Public Health Res. 2015;3(5):228–33. [Google Scholar]
- 23.Daugherty EL, Carlson AL, Perl TM. Planning for the inevitable: preparing for epidemic and pandemic respiratory illness in the shadow of H1N1 influenza. Clinical infectious diseases. 2010;50(8):1145–54. doi: 10.1086/651272 [DOI] [PubMed] [Google Scholar]
- 24.Corless IB, Nardi D, Milstead JA, Larson E, Nokes KM, Orsega S, et al. Expanding nursing’s role in responding to global pandemics 5/14/2018. Nurs Outlook. 2018;66(4):412–5. doi: 10.1016/j.outlook.2018.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tsugawa Y, Newhouse JP, Zaslavsky AM, Blumenthal DM, Jena AB. Physician age and outcomes in elderly patients in hospital in the US: observational study. BMJ. 2017;357:j1797. doi: 10.1136/bmj.j1797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Southern WN, Bellin EY, Arnsten JH. Longer lengths of stay and higher risk of mortality among inpatients of physicians with more years in practice. Am J Med. 2011;124(9):868–74. doi: 10.1016/j.amjmed.2011.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142(4):260–73. doi: 10.7326/0003-4819-142-4-200502150-00008 [DOI] [PubMed] [Google Scholar]
- 28.Tripathi R, Alqahtani SS, Albarraq AA, Meraya AM, Tripathi P, Banji D, et al. Awareness and Preparedness of COVID-19 Outbreak Among Healthcare Workers and Other Residents of South-West Saudi Arabia: A Cross-Sectional Survey. Front Public Health. 2020;8(482). doi: 10.3389/fpubh.2020.00482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Ashwal FY, Kubas M, Zawiah M, Bitar AN, Mukred Saeed R, Sulaiman SAS, et al. Healthcare workers’ knowledge, preparedness, counselling practices, and perceived barriers to confront COVID-19: A cross-sectional study from a war-torn country, Yemen. PLoS One. 2020;15(12):e0243962. doi: 10.1371/journal.pone.0243962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alser O, Alghoul H, Alkhateeb Z, Hamdan A, Albarqouni L, Saini K. Healthcare workers preparedness for COVID-19 pandemic in the occupied Palestinian territory: a cross-sectional survey. BMC Health Serv Res. 2021;21(1):766. doi: 10.1186/s12913-021-06804-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwartz J, King C-C, Yen M-Y. Protecting healthcare workers during the coronavirus disease 2019 (COVID-19) outbreak: lessons from Taiwan’s severe acute respiratory syndrome response. Clin Infect Dis. 2020;71(15):858–60. doi: 10.1093/cid/ciaa255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ohara H. Experience and review of SARS control in Vietnam and China. Tropical Medicine and Health. 2004;32(3):235–40. [Google Scholar]
- 33.La V-P, Pham T-H, Ho M-T, Nguyen M-H, P Nguyen K-L, Vuong T-T, et al. Policy response, social media and science journalism for the sustainability of the public health system amid the COVID-19 outbreak: The vietnam lessons. Sustainability. 2020;12(7):2931. [Google Scholar]
- 34.Tran TPT, Le TH, Nguyen TNP, Hoang VM. Rapid response to the COVID-19 pandemic: Vietnam government’s experience and preliminary success. J Glob Health. 2020;10(2):020502. doi: 10.7189/jogh.10.020502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen SC. Taiwan’s experience in fighting COVID-19. Nat Immunol. 2021;22(4):393–4. doi: 10.1038/s41590-021-00908-2 [DOI] [PubMed] [Google Scholar]
- 36.Thomas Z. WHO says fake coronavirus claims causing ’infodemic’. BBC News; 13th February, 2020. Available from: https://www.bbc.com/news/technology-51497800.
- 37.The United Nations Enitity for Gender Equality and Empowerment of Women (UNWOMEN). COVID-19: Emerging gender data and why it matters. UNWOMEN; 2020. [Cited 2020 June 30]. Available from: https://dataunwomenorg/resources/covid-19-emerging-gender-data-and-why-it-matters. [Google Scholar]
- 38.Center for Disease Control and Prevention. Characteristics of Health Care Personnel with COVID-19—United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15);477–481. doi: 10.15585/mmwr.mm6915e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Byrd P, Ward O, Hamdorf J. The effect of a surgical skills course on confidence levels of rural general practitioners: An observational study. Surg J (N Y). 2016;2(4):e109–e112. doi: 10.1055/s-0036-1593737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lopez DG, Hamdorf JM, Ward AM, Emery J. Early trauma management skills in Australian general practitioners. ANZ J Surg. 2006;76(10):894–7. doi: 10.1111/j.1445-2197.2006.03901.x [DOI] [PubMed] [Google Scholar]
- 41.Hronis A, Roberts L, Kneebone I. Assessing the confidence of Australian mental health practitioners in delivering therapy to people with intellectual disability. Intellect Dev Disabil. 2018;56(3):202–11. doi: 10.1352/1934-9556-56.3.202 [DOI] [PubMed] [Google Scholar]
- 42.Center for Disease Control and Prevention. Healthcare Provider Preparedness Checklist for MERS-CoV. Center for Disease Control and Prevention; 2013. Available from: https://www.cdc.gov/coronavirus/mers/downloads/checklist-provider-preparedness.pdf. [Google Scholar]
- 43.Hu K, Patel J, Swiston C, et al. Ophthalmic Manifestations Of Coronavirus (COVID-19) [Updated 2021 May 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.