Abstract
Introduction
(Background)
The role of pharmacists revolves around providing the highest levels of care to society and ensuring the provision of medicine to all patients. However, with the spread of coronavirus disease 2019 (COVID −19), pharmacists as a very important part of healthcare professionals’ team are responsible for fighting against the disease regardless of their setting of practice. The role of pharmacists will undergo a little change to extend and include other roles in order to ensure the safety of the community and limit the virus spread. Also, they will be required to obtain information from reliable sources, and to be up to date, so they can be reliable advisors to the community and raise their awareness.
Objectives
The purpose of this review is to highlight community and hospital pharmacists’ roles during (COVID-19) global pandemic, and to clearly illustrate how they are contributing to maintain pharmacy services continuity, supporting other healthcare professionals, and facilitating the patient’s education.
Summary
Clinical pharmacists provide direct patient care through monitoring adverse drug reactions, ensuring individualized treatment, performing evidence-based practice, and evaluating drugs in clinical trials. On the other hand, community pharmacists which are the most accessible healthcare providers by the community increase their awareness regarding the preventive measures, balance medicines supply and demand, provide drive-thru and home delivery services, offer telehealth counselling, psychological support, refer suspected COVID-19 patients, and provide vaccination when available.
Conclusion
Innovative pharmacists’ roles have emerged to adapt to changes during COVID-19 pandemic, however, they may be needed in the post COVID-19 world as well.
Keywords: COVID-19, Clinical pharmacist, Hospital pharmacist, Community pharmacist, Pharmacist role
1. Introduction
In December 2019, a newly infectious zoonotic disease caused by the most recently discovered coronavirus strain called SARS CoV-2, which stands for severe acute respiratory syndrome coronavirus 2 started to spread from China to neighboring countries. Wuhan city, the capital of Hubei province was the epicenter of the new outbreak (Basheti et al., 2020). Coronavirus is a broad group of viruses responsible for causing symptoms in the majority of cases. The symptoms may appear after an incubation period that usually ranges from 2 to 14 days from getting infected with the virus, including dry cough, fever, shortness of breath and muscle pain. In some cases, symptoms can be severe and life threatening, especially for the elderly and those with comorbidities who may suffer from complications, such as acute respiratory distress syndrome, acute renal failure, pneumonia and multi-organ dysfunction (Al-Quteimat and Amer, 2020, Visacri et al., 2020). While some patients may remain asymptomatic or with slightly negligible symptoms during the whole period of infection and are still able to infect other people (Al-Quteimat and Amer, 2020).
On the eleventh of February 2020, it was named as SARS-CoV-2 by the coronavirus study group of the international committee on taxonomy of viruses. Then, the disease was named as coronavirus disease 2019 (COVID −19) by the world health organization (WHO) (Li et al., 2020). After a month had passed, on the eleventh of March 2020, the spread of the disease globally was approaching 100 countries, overpassing international boundaries asynchronously, which made the WHO reclassify the disease as a pandemic (Bahlol and Dewey, 2020).
Data from previously published epidemiology studies confirms the possibility of transmission of COVID-19 from infected individuals to other uninfected ones, whether they were having symptoms or not, by many ways. The most common way responsible for COVID-19 spread is person-to-person transmission via respiratory droplets generated by exhalation during breathing, sneezing, coughing, or even speaking. In addition, touching contaminated surfaces can also transmit the virus when the person touches his or her mouth, nose, or eyes (Kamps and Hoffmann, 2020).
With the onset of the pandemic, healthcare systems in many countries around the world are beginning to develop plans and strategies to be adopted to overcome COVID-19 (Mahendra et al., 2020). Over time, the virus can spread over a wide range if precautionary measures and preventive methods are not taken into consideration. Some environments can stimulate and catalyze the spread of the virus among individuals as well. Examples of environments that may lead to virus outbreak in societies are closed work facilities, schools and universities, busy shopping centers, friends and colleagues’ gatherings, homeless communities and shelters, and much more (Kamps and Hoffmann, 2020).
One of the first precautionary measures that have been done by many countries in the world with the beginning of the pandemic is the complete closure of cities, or what is called lockdown. It is worth to mention that pharmacies were one of the few places that continued to receive community members and meet their needs (Mahendra et al., 2020). The expected result of the lockdown is to reduce the transmission of COVID-19, leading to reduced new cases, hospital admissions, intensive care unit (ICU) admission and may decrease the mortality rate as well. In addition to that, applying social distancing between individuals, wearing masks in crowded places, strict washing or sanitizing hands frequently, and reducing the time inside malls or shopping centers, can minimize the risk of the transmission (Kamps and Hoffmann, 2020).
It is very important to combine efforts in order to achieve the best desired outcomes in any tasks. With the beginning of the global pandemic, this was an essential duty that has to be done by the medical staff while fighting against COVID-19.
The management cycle of COVID-19 pandemic including disease management and outbreak control would not be complete without the participation of pharmacists, as they are the first members of care providers (Mahendra et al., 2020). Currently, pharmacists became a very important part of the healthcare professionals’ team, they are patients’ educators and advisors, and not just drug experts. Pharmacists have a very important role as healthcare professionals, depending on their setting of practice, whether they are working in community pharmacies, industries, or as clinical pharmacists. All settings are taking over many responsibilities and activities in fighting the virus and limiting its spread, as well as controlling COVID-19 infodemic (Erku et al., 2020). The role of pharmacists should be supported in all countries by healthcare policymakers to provide appropriate care to all society members. The International Pharmaceutical Federation (FIP) highlighted the important role that pharmacists have to ensure during the outbreak (Mahendra et al., 2020). On the fifth of February 2020, useful guidelines and information about COVID-19 outbreaks have been published by FIP. Its aim was to help community pharmacists and hospital pharmacists to increase their knowledge, and it was titled as (Coronavirus 2019-nCoV outbreak: information and interim guidelines for pharmacists and the pharmacy workforce) (Ung, 2020). Then on the nineteenth of March 2020, FIP has published other guidelines to clarify further information about pharmacists’ responsibilities during this pandemic (Basheti et al., 2020). Much more guidelines have been published by the American Medical Association (AMA), American Pharmacists Association (APA), and the American Society of Health-system Pharmacists (ASHP) (Bragazzi et al., 2020).
Clinical pharmacists that work in many patient care facilities such as; hospitals or medical centers, and provide direct patient care and medication management have an active role during the pandemic. These roles may include; monitoring drug adverse reactions, conducting pharmacovigilance, evaluation of drugs use in clinical trials, and ensuring individualized treatment (Meng et al., 2020).
Other pharmacists that work in community pharmacies are in the frontline in dealing with patients. They are the most readily available and easiest accessible healthcare givers by the community. Their duty is to ensure the community safety by providing telehealth services, (Li et al., 2020) home medicines delivery services, educating the community about the importance of personal and environment sanitization, (Ung, 2020) maintaining a stable supply of pharmaceuticals hygiene products, and supporting people psychologically (Zheng et al., 2020). Furthermore, Community pharmacists are able to engage in screening of suspected cases, and providing immunization when the vaccine is available.
The objective of this review is to shed the light on the possible roles of community and hospital pharmacists during COVID-19 global pandemic. As well as, to highlight how pharmacists are contributing to this pandemic to maintain the continuity of pharmacy services, facilitate patients’ education, and relieve pressure on other areas of the healthcare sector.
2. Combating medication misinformation
Not only the pandemic is growing but also the wrong information regarding COVID-19 and counterfeit drugs are growing as well. This is considered as serious as the pandemic itself. According to the WHO, COVID-19 pandemic has been associated with excessive amount of information which is described as “infodemic”. Some of the information may be false, as a result, people can get confused and find difficulties in differentiating between truth and falsity (Erku et al., 2020). Social media plays a part in misinformation as it spreads myths that do not relate to reality (Bragazzi et al., 2020). Those myths may generate fear among people from different age groups. Since anyone can post anything on the social media, people should first check the authenticity of the source (Schellack et al., 2020).
Pharmacists are healthcare professionals that can play a key role in combating medication misinformation. They can be considered as reliable and credible source of information because they follow the recommendations of health authorities and other professional associations (Erku et al., 2020). Pharmacists have to be aware of the latest changes in this pandemic and update their knowledge all the time in order to deliver new and accurate information to patients and help them distinguish fact from myth, therefore reduce the level of panic and worry which may affect mental health (Elbeddini et al., 2020b).
Pharmacists may use many ways to convey essential information to people including brochures, text messages, apps, and websites using guidelines from FIP for example. In addition, they can conduct informative sessions with questions and answers in different places such as schools, community centers, (International Pharmaceutical Federation, 2020) and they can carry campaigns to promote the correct use of drugs information (Erku et al., 2020).
An example of the wrong information that has spread at the beginning of this pandemic is that chloroquine and hydroxychloroquine are the potential treatment for COVID-19 which resulted in their unreasonable stockpiling. With the confusion many people tried to take unproven fake and even toxic cures for COVID-19 including methanol, which led to hundreds of deaths in Iran, cocaine, chloroform, and exposing the body to high temperatures or having a hot bath. Also, taking non-steroidal anti-inflammatory drugs (NSAIDs) including ibuprofen, and taking vitamin C and D has spread on the social media as cures for COVID-19 (Erku et al., 2020).
Other myths have spread among people in social media. For instance, low temperatures can help eradicate the virus, transmission of the virus can be facilitated by mosquitoes, and consuming garlic can protect individuals from developing the infection, and much more. All these misconceptions can be encountered by the pharmacists who are responsible for providing people with facts and raising public awareness (Schellack et al., 2020).
Furthermore, pharmacists are responsible to direct and advise people not to obtain any drug from unregistered online shops, especially with the surge of fake drugs. They also should check any suspicious product and defective testing kits and other equipment, and warn others of them (Erku et al., 2020).
3. Hospital/Clinical pharmacists’ roles:
3.1. Monitoring of adverse drug reactions
Close monitoring of safety, effectiveness, and adverse reactions of drugs used to treat COVID-19 patients must be done by the clinical pharmacists as one of the priorities (Meng et al., 2020). Since there is no specific treatment for COVID-19 till now, and the effect of off-label drugs that are used for this disease is unclear, clinical pharmacists have many essential duties to do. They should conduct pharmacovigilance to detect any adverse drug reaction (ADR) early in order to modify the treatment regimen. In addition, these adverse reactions should be recorded and reported in an accurate way. The pharmacists have to be very careful because some of the drugs may cause dangerous side effects or adverse events such as cardiotoxicity or hemolytic anemia, or they can be teratogenic as well (Song et al., 2020). Thus, they need to be able to evaluate and analyze them as minor, moderate, and severe reactions. Then they have to provide the clinicians with this important information as it is needed to build up a clinical experience on using those off-label drugs (Ying et al., 2020).
Chloroquine (CQ) and hydroxychloroquine (HCQ) are not recommended to be used due to the lack of data of their use in COVID-19 patients in terms of safety and efficacy, specifically because of their narrow therapeutic window. Therefore, high doses are associated with increased risk of toxicity and adverse events, so the patient needs to be closely observed inside the hospital setting by the clinical pharmacist. Nausea, vomiting, headache, convulsions, vision impairment, and heart arrhythmia are indicators of CQ, HCQ toxicity. If the patient has QT-prolongation, epilepsy, retinal disease, or myasthenia gravis, it is contraindicated to give CQ or HCQ, and the clinical pharmacist should develop the treatment plan with the clinician in order to highlight these issues and to optimize the drug therapy. Moreover, if HCQ and azithromycin are given together, monitoring with additional caution is needed because both of them can cause prolongation in QT-interval and torsade de pointes which may result in heart death (Schellack et al., 2020).
3.2. Management of drug interactions
With the aim of preventing worsening of the symptoms in COVID-19 patients, it is very important to avoid any drug-drug interaction or drug-food interaction, which is a main responsibility of the pharmacists as they are the drug experts. They have a vital role in supporting the management of medication regimens and diet. Antiviral drugs that are used to treat COVID-19 patients are linked to many interactions; therefore, the pharmacist should ensure that they are not combined with drugs that possibly interact with them, especially for patients with comorbidities who are taking other medications. For example, lopinavir-ritonavir combination product (Kaletra) which is metabolized by the liver enzyme CYP3A should not be given with atorvastatin, nifedipine, or any other drug that is metabolized by the same enzyme, instead, they should be administered separately by intervals. Also, the pharmacist has to instruct the patient not to consume any type of food that changes the effect of the CYP3A enzyme like grapefruit or honey (Song et al., 2020). Another drug-drug interaction is when lopinavir-ritonavir and amiodarone are given together, this combination must be given with cautious monitoring of the heart rate of the patient because lopinavir-ritonavir may increase the amiodarone concentration in the blood (Ying et al., 2020).
3.3. Pharmaceutical care for certain patients’ groups
Clinical pharmacists in each hospital should deliver the maximum possible pharmaceutical care for people infected with COVID-19, and they should pay extra attention to ladies who are pregnant or lactating, elderly, and children. If the symptoms are severe in these patients and they are going to receive drugs, the responsible clinical pharmacist should participate in the development of the treatment plan. While doing that, he or she must take some points into consideration. For example, doses should be adjusted for children, and the status of kidney and liver function should be observed in elderly suffering from other underlying diseases or having a weakened immunity. Also, regarding pregnant women, they should not receive drugs with Food and Drug Administration (FDA) Pregnancy Category D, only Category B or C can be allowed after weighing the benefit/ risk ratio. In addition, continuous monitoring of the vital signs of the mothers and their fetuses should be done. As for lactating women, they should be advised by the pharmacists to suspend breastfeeding, and isolate themselves from their babies to protect them from the infection and any harm that could happen because of the drugs excretion in the breast milk (Song et al., 2020).
3.4. Pharmaceutical care for patients with comorbidities
Pharmacists should assure offering special care and guidance to patients with combined underlying diseases, (Zheng et al., 2020) such as cardiovascular diseases, diabetes, chronic obstructive pulmonary disease (COPD), malignancies, organ transplantation or infections. Each one of these combined underlying health conditions can increase the risk of severe disability and experiencing dangerous symptoms from COVID-19. This can be similar to what is seen with chronic liver and kidney failure patients and those with compromised immune system. The condition may be even worse in patients suffering from comorbidities (Song et al., 2020). Pharmacists should educate these patients about the correct medicine administration. Also, the importance of medication adherence and how this can retain their conditions under control should be stated. For example, pharmacists should check blood pressure (BP) more frequently for patient with usual elevated readings, and an immediate medical intervention shall be done if the results were abnormal. Moreover, patients with cardiovascular diseases who are receiving warfarin need a close monitoring of the international normalized ratio (INR) by the clinical pharmacist, and they should observe ADRs like bleeding or clotting (Zheng et al., 2020).
There is a high possibility of disease progression and deterioration of the patient’s condition especially if he or she suffers from other combined chronic diseases. Patients who suffer from comorbidities besides their infection with COVID-19 need an intense pharmaceutical care by the clinical pharmacists, as they have a higher risk of developing serious complications. Their dosage should be adjusted if necessary and their clinical indicators such as BP, INR and blood glucose level should be monitored carefully, because their drug regimens are more complex, and their disease management is even more challenging. Also, in this case the safety and efficacy of the drugs may be affected and many drug-drug interactions may occur (Song et al., 2020).
Many antiviral drugs that are used nowadays to decrease the viral load in a COVID-19 patient may interact with other drugs that are used to manage other conditions, for example; lopinavir-ritonavir may depress diabetes and can enhance the anti-hypertensive effect of nifedipine, and ribavirin possibly will diminish the anticoagulant effect of warfarin. Therapeutic drug monitoring (TDM) can help in optimizing the dose to a therapeutic level and minimizing toxicity. Some drugs including lopinavir-ritonavir and anti- infective drugs such as voriconazole need a careful TDM (Song et al., 2020). It is not totally clear until now what is the best treatment strategy for COVID-19, and whether some medical conditions like diabetes need a special treatment, therefore; monitoring drug-drug interactions is highly significant to avoid symptoms aggravation. For instance, COVID-19 patients receiving steroids have a risk of developing hyperglycemia. On the contrary, patients with diabetes receiving HCQ will have a better glycemic control (Kamps and Hoffmann, 2020).
3.5. Monitoring of convalescent plasma therapy
Convalescent plasma therapy (CPT) is a procedure that involves the use of blood taken from individuals that have recovered from an illness and be transferred to other hospitalized patients who are in critical condition and have rapid disease progression. This therapy can help patients to recover, strengthens their fight against the virus by providing a passive immunity, lessen the severity, and shorten the duration of illness (Song et al., 2020). Convalescent patients in China were requested from the National Health Commission (NHC) to donate blood and help in treating other patients (Zhai et al., 2020). In order to get a high neutralization positive titer of virus-specific antibodies in the convalescent plasma, (Song et al., 2020) it should be collected within two weeks after recovery (Zhai et al., 2020). While plasma infusion, blood cells and pathogens will be removed, plasma and antibodies will remain. As there is no approved treatment for COVID-19 until now, the Federal Agency of the United States (US FDA) approved the use of CPT during COVID-19 pandemic. Pharmacists are an integral part of the team that conduct CPT as many roles are assigned to them to do before the procedure. They help clinicians in assessing patients’ symptoms, recording allergy history, contraindications, and patients’ clinical conditions, and formulate the dose of the infusion which usually range between (4–5 mL/Kg), based on patients’ weight and clinical status. Pharmacists also can help in monitoring and recording adverse effects of the plasma transfusion like dyspnea, hypotension, circulation overload, and infectious transfusion reaction in every step until the procedure is done, and participate in managing them (Song et al., 2020).
One of the drawbacks of CPT is the difficulty of gaining plasma during convalescence. Further evaluation of the safety and efficacy of this therapy while using it to treat COVID-19 is needed (Zhai et al., 2020).
3.6. Development of personalized treatment by an interdisciplinary team
Pharmacists play a crucial and important role in collaboration with the healthcare team to ensure the best care for patients with COVID-19. As a part of a multidisciplinary diagnosis and treatment team (MDT), clinical pharmacists should use their skills, experience, and pharmacological knowledge to provide individualized drug regimens based on the patient’s symptoms, kidney and liver function, and any pharmacokinetic parameters for the drug. The nutritional status is a very important vital sign that should be considered and one of the important treatments is the nutritional treatment in very ill patients, thus nutritional pharmacists as a part of multidisciplinary collaborative team in the hospital should assign nutritional treatment plan according to severity of the case of patients with COVID-19, at the same time, they help in assessment of venous thromboembolism (VTE) and any other complications among the patients (Li et al., 2020).
3.7. Treatment protocols and drug formulary
China National Health Commission (CNHC) has published updated guidelines for the control of COVID-19 infection. Many of the medications used in these guidelines are not approved or designed for treatment of COVID-19, they are used for this indication depending on the experience that was used previously for management of SARS outbreak in China in 2003. Clinical pharmacists had a significant role in collaboration with the physicians and other healthcare providers to ensure the safe and effective use of medications (Meng et al., 2020). Clinical pharmacists contribute in designing treatment protocols with the ICU nurses and physicians, as they are responsible for providing updates for these protocols. Moreover, they provide inpatient rounds, efficient supply of medications, management of drug shortages, allocating drug management recommendations for the benefit of their colleagues, and designing a drug formulary depending on the evidence-based drug information such as the indication of the drug, appropriate dose, ADRs, drug-drug interactions (Elbeddini et al., 2020a, Meng et al., 2020). Due to the huge concern about the drug shortages, pharmacists can assist the physicians in finding the suitable drug alternatives for COVID-19 patients (Meng et al., 2020).
Clinical pharmacists engage in the antimicrobial stewardship programs which can help in management of viral infections including COVID-19, and then create treatment protocols. Furthermore, they monitor the use and efficacy of antibacterial agents in case of secondary infection appeared for COVID-19 patients (Elbeddini et al., 2020a).
Clinical pharmacists as a frontline have published drug manuals for assisting medical personnel in understanding the appropriate drug use, dosage, and the possibility of dose adjustments for special groups of population including elderly, children, pregnant women, and patients undergoing renal dialysis. In China, Pharmacy Administration Commission of Chinese Hospital Association (CHAPAC) has created the drug formulary in Fangcang shelter hospital for management of patients with COVID-19 (Meng et al., 2020). In addition, CNHC has published guidelines for treatment of COVID-19 patients. These guidelines include the recommended use of lopinavir-ritonavir, umifenovir, and CQ (Liu et al., 2020).
For the diagnosis and appropriate management of Coronavirus pneumonia, the Chinese Pharmaceutical Association Committee (CPA) and the Hunan Pharmaceutical Association have released the drug information and drug formulary manuals (Liu et al., 2020).
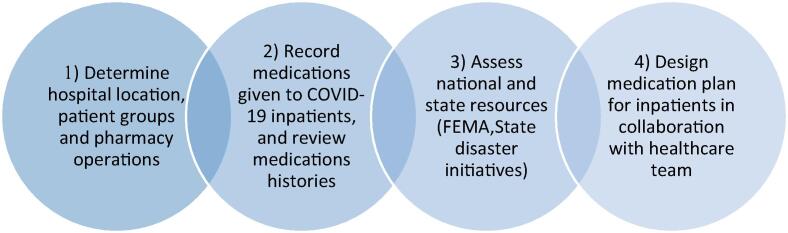
During this emergency, many field hospitals have been established to decrease the load on other health institutions. It is important to create formulary guidelines in order to offer pharmacy services in the field hospital, and this is the responsibility of pharmacy departments. (Fig. 1) describes the process of field hospital formulary development by Michigan Medicine pharmacy department (Bazzell et al., 2020).
Fig. 1.
Field hospital formulary development process by Michigan Medicine pharmacy department. FEMA: Federal Emergency Management Agency.
3.8. Involvement in making medication evidence-based decisions
As there is no drug that has been presented to prevent or cure COVID-19, and several drugs are still in clinical trials to do extensive tests for their safety and effectiveness, (Li et al., 2020, Song et al., 2020) many tasks have been performed by clinical pharmacists to take the best decisions regarding medication and perform drugs evaluation. They are responsible for designing individualized drug dosage regimens for hospitalized COVID-19 patients. Also, clinical pharmacists should always weigh benefits over risks while taking decisions regarding the medications, and should take clinical research and guidance into consideration. Many clinical guidelines have been published from different countries including China, US, and WHO authorities as well (Song et al., 2020). In Canada, McMaster Evidence-based Medical Center organized a global evidence-based guideline for drugs used to treat COVID-19, and pharmacists from Peking University Third Hospital (PUTH) in China took over manuscription of antiviral drugs and drug evaluation (Li et al., 2020). On March 2020, Cochrane library, PubMed Embase, and Chinese databases were renewed methodically, to ensure documenting evidence-based guidance. Moreover, recent COVID-19 treatment options were provided by ASHP, to help healthcare professionals, especially hospital pharmacists gain a better treatment understanding (Song et al., 2020). CNHC developed national diagnosis and treatment guidance, and pharmacists participated in conducting evidence-based evaluations of the effectiveness of drugs, like CQ, lopinavir-ritonavir, and interferon, to be a reference while treating COVID-19 patients. Furthermore, medications evidence-based evaluations conducted by pharmacists can be a good reference for dosage regimen and precautions of some drugs such as ribavirin, and to search for the suitable route of administration, and to know which drug can be taken by inhalation (Li et al., 2020).
3.9. Evaluation of clinical trials drugs and providing vaccines development information
Clinical pharmacists are actively involved in the process of clinical trials. Firstly, they formulate the drugs that will be experimented, and then they explore their safety and effectiveness(Meng et al., 2020) by launching a database of clinical drug research that contains medical records (Li et al., 2020). Also, they supervise the use of the experimental drugs, and regulate their storage and disposal (Liu et al., 2020). With the beginning of COVID-19 infection in China, there was no targeted drug to prevent its spread or treat it (Li et al., 2020). Therefore, it was necessary to exploit pharmacist’s expertise in drugs and vaccines clinical trials (Elbeddini et al., 2020a).
There are many investigational drug-controlled trials that have been done globally for new agents, in the form of two-arm comparisons, or drug repurposing for already approved drugs. They are done with the supervision of clinical pharmacists, in an attempt to explore the safest and the most active prophylaxis and treatment regimens (Gross and MacDougall, 2020). Clinical pharmacists are responsible of getting individuals joined in such ongoing trials (Al-Quteimat and Amer, 2020).
Antiviral drugs were some of these drugs that have been studied to check their activity against the virus, and to determine if they can be approved as a treatment of COVID-19. 229 studies from a total of 591 were interventional clinical trials, and have been registered in the Chinese Clinical Trials Registry (ChiCTR) on the eighteenth of April 2020 (Meng et al., 2020).
For instance, the efficacy and safety of the use of HCQ sulfate for COVID-19 patients with severe cases were studied in PUTH in China, to standardize the treatment and adopt the optimum dosing regimen (Li et al., 2020). The same studies were done for phosphate CQ, after it killed the virus in cell cultures. Also, 760 patients infected with COVID-19 participated in two placebo-controlled trials of the antiviral drug remdesivir in the beginning of February 2020 in China. Moreover, the safety of steroids drugs has been studied to ensure that they will not cause harm in conjunction to their anti-inflammatory effect while using them for COVID-19 patients (Liu et al., 2020).
Furthermore, some in-vitro studies support the use of antiviral drugs, lopinavir-ritonavir or immune-modulating agents like interferons. If lopinavir-ritonavir were used in the treatment regimen, pharmacists should ensure their safe delivery, and monitor ADRs and possible drug-drug interactions (Gross and MacDougall, 2020). Pharmacists should frequently review pharmaceutical recommendations, (Al-Quteimat and Amer, 2020) and present all new data to clinicians to keep them updated while treating COVID-19 patients, (Gross and MacDougall, 2020) because variations are expected as information about COVID-19 virus gathered (Al-Quteimat and Amer, 2020).
In addition to drugs clinicals trials, many vaccines have entered clinical trials studies in several countries, hoping to stop the spread of COVID-19. In China, recombinant Coronavirus vaccine, adenovirus type-5 vector (Ad5-nCoV) has entered phase 1 clinical trial, also nucleic acid vaccine (mRNA-1273) in US as well. Clinical pharmacists are responsible for delivering scientific information to the patients regarding vaccines development, in addition to following subjects who are participating in vaccines clinical trials to record any adverse reaction could happen to them after taking the vaccine. Then, data about vaccines safety and effectiveness will be collected by clinical pharmacists to support further clinical researches (Song et al., 2020).
3.10. Control of inpatient prescription and drugs dispensing remotely
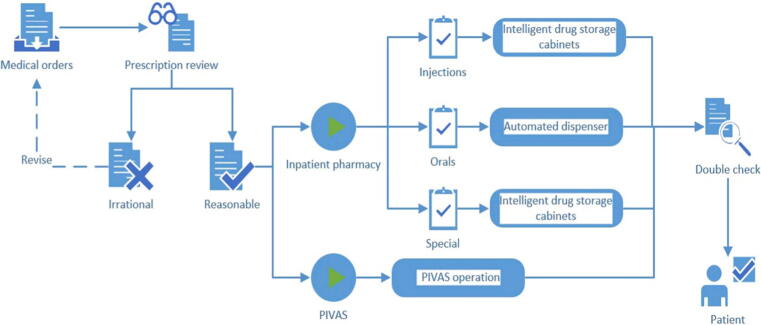
For the sake of reducing the spread of COVID-19 infection, especially through person-to-person, medical institutions have tried to invent new methods that can ensure patients safety during dispensing their medications. Once a medical order is placed, clinical pharmacists will review the prescription professionally and carefully to exclude any irrational prescription, avoid medication errors and assure the optimum outcomes for the patients. Clinical Decision Support System (CDSS) can be used while reviewing the prescriptions to enhance healthcare services based on patient and health information. Intelligent drug storage cabinets and automated dispensers were used for the delivery of several dosage forms. An exception for drugs that need intravenous administration, Pharmacy Intravenous Admixture Services (PIVAS) are used to provide efficient and safe intravenous preparations to the patients. (See Fig. 2) (Li et al., 2020).
Fig. 2.
Innovative model of medication dispensing during the COVID-19 pandemic.
In Saudi Arabia, Johns Hopkins Aramco Healthcare have been used automated drug dispensing systems, especially in ICUs and isolation areas, to ensure their sterilization. Around 85% of medication orders were performed using them. Moreover, in order to reduce the throng in the central pharmacy, more medications were added to the automated system with an increased par level (stocking period). In addition, to prevent any cross-infection or errors, any drug removed from the system is not allowed to be returned back (Arain et al., 2020).
3.11. Clinical pharmacist’s telehealth services
The lockdown and suspension of public transportation in many countries to lower the virus transmission has increased the need for telehealth services (Li et al., 2020). According to the US Health Resources and Services Administration, telehealth is the implementation of telecommunication technologies and electronic information to enhance long-distance pharmaceutical care, patient education, health administration and community health (Segal et al., 2020). It is somewhat a new concept which has reached a high degree of importance during this pandemic (Saghir et al., 2020). In the US in the early 2000 s, there were not a lot of pharmacists, thus they started providing telehealth services. However, those services were restricted to some patients, for example, those who lived in the countryside or had no access to medical care (Segal et al., 2020).
In order to reduce the number of unnecessary hospital visits in China, online pharmacy services have been established including free medicine consultation through “WeChat”, (Liu et al., 2020) which is a media platform having many features such as private or group chat, voice or video calls, text or voice message, and additional functions that help clinical pharmacists to check patients’ needs, their status, and any experienced drug adverse reaction. Using the technology for providing distant pharmaceutical care resulted in many advantages including reduced risk of cross infections, and saved resources (protective gears) so that they can be used where they are much needed (Hua et al., 2020).
With the help of telehealth, clinical pharmacists can follow up with patients discharged after being admitted with COVID-19 and who are at a high risk for readmission. They can counsel and educate the patient, manage medication therapy, and check any adverse event (Sin et al., 2020). For example, elderly (65 years old or more) often have many comorbidities and they take multiple drugs, as a result they suffer more of adverse events. The platform “GeriMedRisk” as a part of telehealth services helps reduce adverse events occurrence in elderly patients so that decrease drug-related hospital admissions (Elbeddini and Yeats, 2020). Moreover, twenty-seven clinical pharmacists volunteers with medication therapy management (MTM) qualifications were chosen by the Beijing Pharmacist Association to establish an online service named “cloud pharmacy care” where they respond to patients’ inquiries and consult them on drug-related problems, chronic drug management, and psychological counselling, from 8 a.m. till 8p.m (Li et al., 2020). Telehealth was used by clinical pharmacists to complete diabetic patients’ medication histories, teach them about their medications, and discuss with the physician about medication change suggestions. The effectiveness of using telehealth in diabetes management was similar to that of actual visits (Segal et al., 2020).
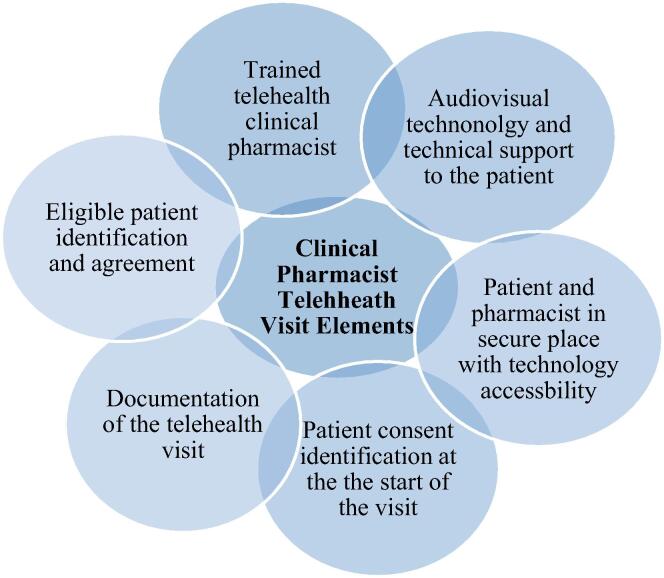
By using mobile phones/computers, patients at their homes can have an interactive audiovisual telehealth visit with the clinical pharmacist. They can use Skype, Zoom, Google Hangouts, etc. After getting the patient’s agreement, clinical pharmacist schedules a telehealth appointment. Then, the patient is provided with a hyperlink to enter the appointment. At the beginning of the session, the clinical pharmacist confirms identity of the patient and whether other people are attending the session. Also, the pharmacist introduces himself/herself and any attending student. Patient’s responses and pharmacist’s information are kept as a video or written report and uploaded into the electronic medical record. (Fig. 3) shows the elements of a clinical pharmacist telehealth visit (Segal et al., 2020).
Fig. 3.
Elements of a clinical pharmacist telehealth visit.
There are several advantages of telehealth visits such as individualized communication, building rapport with the patient, visually assessing patient’s technique of administrating injection, using verbal and nonverbal language, and avoiding crowd in a limited space clinic or hospital so there is a chance for more caregivers to attend which results in more information retention. In addition, the pharmacist is able to share the computer screen with the patient to emphasize important points. Any auxiliary handout can be sent to the patient after the appointment via mail or email. The patient can wait in a virtual waiting room till the discussion between the healthcare team is finished. Documentation of the telehealth visit is shared with other healthcare providers and a treatment plan is designed. Then the patient is invited back to the main virtual room to decide on a treatment (Segal et al., 2020).
On the other hand, there are some limitations of telehealth visits, for instance some patients may face difficulty going through the needed preparation to conduct a telehealth appointment. The pharmacist should be prepared to use another way (phone call) to contact the patients in case of inability to set up the required components and help them to do so. Other limitations include unavailability of computers, and weak or no Internet service. In such cases, a conventional phone call or in-person actual visit can be done (Segal et al., 2020).
Telehealth services are very useful especially for people in distant areas from healthcare facilities, thus it would be better if they are continued being provided even after the ending of this pandemic.
3.12. Clinical pharmacist’s psychological support
The constant fear that people feel of being infected with COVID-19 at any moment or being already diagnosed with it have posed nearly the whole world. It is a stigma that can affect patients’ mental and emotional health negatively and cause psychological tension to the community (Song et al., 2020). Stigmatization is a discrimination against distinguishable group of people due to lack of awareness (Centers for Disease Control and Prevention, 2020). Infected individuals can face this problem and it makes them susceptible to be avoided or rejected by their societies. In addition to the negative impact on mental and emotional well-being, this can affect their education, employment, housing, or being verbally abused. The Centers for Disease Control and Prevention (CDC) has recognized the importance of ending COVID-19 stigma and how this can make the infected individuals more pliable to withstand and recover quickly. Pharmacists can help prevent stigma by spreading facts, correcting negative information, and educating individuals about how the virus transmits, limiting fear and nervousness from the disease. Additionally, pharmacists should assure people that no person or specific nationality can spread COVID-19 more than others (Al-Quteimat and Amer, 2020). Also, because of disease progression and sudden change of the daily life routine, COVID-19 patients need full attention and pharmaceutical care from pharmacists regarding their mental and psychological condition, to avoid experiencing any unwanted symptoms like anxiety disorders, panic, and pessimism and to have positive outlooks. There are many ways of mental and psychological support that can be implemented depending on the condition of the patient. For all patients that have been diagnosed with COVID-19, a well-timed and full of optimism counselling should be provided to the patients to help them follow up with disease information and to boost confidence. For patients with mild to moderate psychological problems, pharmacists can give them some pieces of advice on how to get rid of their negative energy and strengthen their immunity by doing some exercises as an example. In case of patients with severe psychological problems, pharmacists should refer them to psychiatrists to provide psychological treatment and get a better control. If the patients already suffer from mental problems, their compliance to the psychotropic drugs should be monitored closely by the pharmacists (Song et al., 2020).
4. Community pharmacists’ roles
4.1. Raising awareness about personal and environmental hygiene
Pharmacists play a very critical role in increasing awareness among individuals, ensuring the safety of the personnel, providing consulting services, and reducing the chance of transmitting the infection through the items in the pharmacy. Additionally, implementing preventive measures such as regular hand hygiene among the customers and staff members and regular disinfection of surfaces. By doing such measures, they are ensuring the safety of the public, and decreasing the chance of transmission of the virus. Community pharmacists should educate the public to use disinfectants and hand rub alcohols in a proper way (Ung, 2020).
Patients education may also include the proper use and selection of masks, social distancing and when the patients are outdoor. In addition to that, pharmacists provide the community with the basic knowledge about the onset symptoms to be able to distinguish between the common cold, flu and COVID-19 and educate patients with suspected symptoms such as runny nose, sneezing and cough to isolate themselves at home and to seek the medical advice from the pharmacists about the symptomatic treatment options if the disease continued to progress (Zheng et al., 2020).
4.2. Control of vitamins and OTC products misuse during COVID-19 pandemic
The most commonly accessed drugs by the patients that can be sold in any medical store without the need for a prescription are Over the Counter (OTC) drugs. Pharmacists as a part of the healthcare team should know when to refer patients or when to dispense OTC medications according to the patient’s condition. The inappropriate use of OTC drugs may lead to many dangerous effects. Patients use OTC drugs because they are self-administered and they think that they are safe and they neglect the side effects that may happen in certain patient groups (Lall and Singh, 2020). During this pandemic, public got panicked and started to use medications including home remedies inappropriately without the investigation of their safety. Social media played a role in posting misinformation about the use of medications during COVID-19. Many individuals started to use OTC medications, antibiotics, herbal remedies irrationally. Ivermectin is an anti-helminthic used to treat certain parasitic infections sold as an OTC medication in some countries, people started to use it for management of COVID-19 infection, therefore the WHO started to give cautions about the inappropriate use of these drugs. So, the pharmacists here play a major role in increasing awareness about the rational use of OTC products such as painkillers paracetamol and ibuprofen due to their increased demand and other remedies based on therapeutic needs with legislation and professional standards (Malik et al., 2020). The Pharmacy Guild of Australia and the Pharmaceutical Society of Australia (PSA) have published certain limitations to limit the inappropriate dispensing of prescription medications and other OTC medicines during COVID-19 pandemic with the aid of National Pharmaceutical Services Association (NPSA). They decided to limit dispensing certain classes of OTC products to a one unit per purchase. Certain OTC list products included salbutamol inhalers, children analgesics, and adrenaline autoinjectors were limited from dispensing between Australians and their supply was maintained to only confirmed diagnostic cases. Pharmacists has been asked to place paracetamol pediatric formulations near the counter area to make sure that they are dispensed in an appropriate way and maintain the equity of supply between individuals (The Pharmacy Guild of Australia, 2020).
Pharmacists have a crucial role in educating people about the misconception of taking vitamin supplements in treating COVID-19 infection. They should be updated about the new data of studies that would refuse or encourage the use of dietary supplements and should advice the patients that social media is not a source to take reliable information. The British National Institute for Health and Care Excellence (NICE) confirms that there is no evidence till now that vitamin D is effective in preventing or treating COVID-19. Therefore, pharmacists have a significant role in giving advice to the normal healthy individuals that they should not take more than 100 µg of vitamin D to prevent any undesirable harmful effects (National Institue for Health and Care Excellence, 2020).
Vitamin C (ascorbic acid) major role in enhancing the immunity is well known. Pharmacists may dispense the regular doses of vitamin C and increase the awareness about the harmful effects that happen with higher doses (Harvard University, 2020). Zinc can efficiently support the immune system as well (COVID-19 Treatment Guidelines Panel, 2020).
The first preventive measures people should perform are regular hand washing, wearing masks, social distancing, then the use of vitamins and the doses required should be determined by the pharmacists to reduce the risk of toxicity and the undesirable ADRs. After that pharmacists should help the patients to get the trusted information and clarify the misconceptions about consuming OTC products and vitamins.
4.3. Relieving overloaded hospitals and pharmacist’s prescribing roles
With the beginning of current public health crisis, healthcare services began to be more focused on responding to COVID-19 cases, and medical centers were and still busy with providing the necessary care for infected people, and at the same time, people will continue to complain about other symptoms or conditions unrelated to COVID-19. The severity and the nature of these symptoms can range from mild to severe that need more attention and medical intervention. Community pharmacists are relieving a great pressure from general practitioners, by managing minor cases in community pharmacies settings and reducing non-urgent general practitioner (GP) visits by more than 50%. Examples of minor illnesses that can affect many people globally and can be managed by OTC drugs provided by community pharmacists are shown in (Fig. 4). Statistics from United Kingdom (UK) have shown that more than 10% of GP visits and 5% of emergency department visits are mild illness cases and can be treated efficiently by community pharmacists with a high level of patient satisfaction. A list of broad range of mild conditions that do not need GP visits has been developed. There are chosen plans in UK and Canada contain OTC and specific prescription drugs that can be dispensed by community pharmacists to patients suffering from mild conditions. This can help a lot in maximizing the care of COVID-19 patients in hospitals, but one negative financial impact is that some patients who are qualified to get free of charge healthcare including consultation and medications after getting prescriptions from their physicians will need to pay out-of-pocket for OTC drugs if they got treated by community pharmacists without a prescription. Although it is not permissible to allow community pharmacists to prescribe medicines to patients in most countries, however it is realistic to give them the right to provide this service to ensure that all patients are provided with the highest level of care and they can easily get their medications during this global pandemic, where it may be difficult for them to visit their prescribers to preserve the continuity of repeated prescriptions. In Ireland and UK, community pharmacists are allowed to dispense regular medications for patients having recent prescriptions. Usually, urgent requests for drugs are received by elderly and patients with chronic conditions, so community pharmacists have taken the responsibility for providing these emergency supply requests during this crisis, but with a commitment to a limited quantity of drugs. For example, in Ireland the limit is five days’ supply in most cases, and it may need to be extended. These pharmaceutical services have shown how the skills of pharmacists can be altered and adapted to situations to reduce the load on general practice (Cadogan and Hughes, 2020).
Fig. 4.
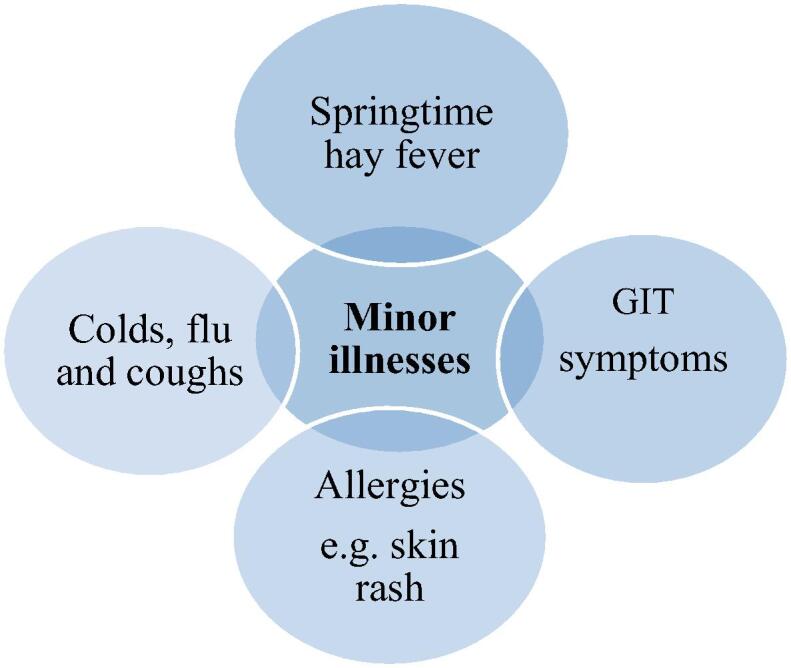
Examples of minor illnesses managed by OTC drugs.
4.4. Balancing supply and demand related to COVID −19
During this pandemic there has been a huge and unpredicted demand on food, medical supplies, and household supplies such as tissue papers and disinfectants. People started to get panic about the significant reduction in these essential things. There have been a lot of patients stockpiling medications and other medical supplies such as face masks and gloves. This increase in demand has led to medication shortages and insufficient supply of medicines. Medicine shortages have a considerable impact on patients and may lead to many consequences which threaten patient safety and result in negative outcomes. In addition to that, it may completely exhaust the resources of the pharmacy that make pharmacists search for other suitable therapeutic alternatives, spend time for compounding or even communicate with clinicians to change the prescriptions to other medications that are available (Cadogan and Hughes, 2020, Zheng et al., 2020).
As community pharmacists are the most reachable healthcare providers by the public, they are significantly trusted by the patients to maintain the continuity of supply of medications or other COVID-19 preventive products such as face masks, gloves, and alcohol sanitizers. Pharmacists do a great effort to reassure the patients about the continued availability of medications, specifically OTC drugs, due to the increased demand by the public to get these medications, and prescription medications as well (Liu et al., 2020). They should maintain the continuity of supply of medicines for chronic disease conditions such as asthma inhalers, antihypertensive drugs, and drugs for cardiovascular and kidney diseases. In addition, drugs used for fever and body aches such as paracetamol painkiller should be maintained (World Health Organization. Regional Office for Europe, 2020). Pharmacists in China have worked with drug companies to ensure drug supply for patients with special diseases including cancer, hepatitis, and irritable bowel diseases. Information about drug availability and its stores location is monitored online or by using mobile apps. (Cadogan and Hughes, 2020, Zheng et al., 2020).
One of the most important preventive measure that should be taken during the COVID-19 outbreak is wearing a mask. Masks can highly help to prevent the spread of the infection between individuals. As mentioned by the WHO, wearing a surgical mask in combination with hand sterilization and other protective measures can extremely minimize the spread of COVID-19 infection in the affected areas. The role of pharmacists is clear in maintaining the continued supply of masks and other protective necessities and educating people how to use them properly. Moreover, community pharmacists have to direct the public to the right selection of face masks, and to stock them as needed without causing any mask shortages (Ung, 2020).
Pharmacists in Macau have contributed in helping consumers differentiate between surgical masks with their protective filtration efficiency and other fake unprotective ones. Additionally, they guarantee the masks supply in a reasonable price range that could be afforded by all individuals by setting a reference price which could prevent any irrational pricing elsewhere. Thus, community pharmacists must be trained properly to fulfill the community patients’ various needs in combination with rational use of medications (Ung, 2020).
In some countries, there has been a collaboration between pharmacists, general practitioners, and territory authorities in order to enable the therapeutic substitution if the prescribed medicine was not available during the time of dispensing without previous approval from the prescriber (American Pharmacists Association, 2020a, Erku et al., 2020). This measure highlights the significant role of pharmacists in maintaining an uninterrupted supply of medicines.
In Australia, there has been a huge demand for HCQ. The Therapeutic Goods Administration (TGA) has restricted prescribing this medication by the medical specialists. Therefore, pharmacists in this case have been involved as stewards to provide the prescribers with the updated new legislative changes which are carried out by the TGA (Erku et al., 2020). In the US, twenty-two states have published guidelines for the pharmacists to use their professional judgment during filling HCQ prescriptions to ensure the patients ongoing need for this medicine, for example; for treatment of pre-existing conditions such as Lupus. Pharmacists ensure the implementation of these restrictions and educate the public about the dramatic need for such changes during this pandemic (Aruru et al., 2020).
It is possible for the pharmacists currently to apply the concept of post-dated prescriptions. Pharmacists would ask the patients politely if they are really in need for this medication and not asking for medicines for stockpiling purpose (Mahendra et al., 2020).
4.5. Patients’ referral and testing
As COVID-19 infection started to spread to extended areas in China, policymakers have reinforced a regular inspection by adding checkpoints and testing of suspicious cases to prevent further spreading of the disease. To promote the pandemic control, appropriate referral of suspected cases to designated medical institutions is a very important measure to reduce transmission of COVID-19 infection among the individuals (Ung, 2020). Community pharmacists are the first point of contact by patients with health-related concerns. Thus, pharmacy staff have a significant role in assisting the healthcare team and minimizing the spread of COVID-19 infection in the community, through appropriate patient screening with body temperature measurements. Pharmacists can find out the suspected patients through clinical symptoms such as flu, cough, fever, and shortness of breath, or if they asked for anti-flu medications (Amariles et al., 2020, Mahendra et al., 2020). Pharmacists may check the epidemiological history of the patients, for example if they were abroad for the last fourteen days or if they had any direct contact with a person with a confirmed case of COVID-19 (Zheng et al., 2020). In this case, pharmacists shall direct the patients to the nearest flu clinics, government clinics or hospitals (Mahendra et al., 2020). Patients are going to be isolated in a designated medical institution or facilities if they are immunocompromised or their case is very critical (International Pharmaceutical Federation, 2020, England and Improvement, 2020).
Community pharmacists are trusted by the patients through their contribution in testing COVID-19, and they are nearby and highly accessible in any time (Strand et al., 2020). By testing for people pharmacists will stop them from going to care facilities, in this case, they are freeing up the time for other healthcare providers to manage the most urgent and critical cases (American Pharmacists Association, 2020a). Pharmacy staff should be trained and have the facility requirements prior testing. It is important for the pharmacies to be granted a certificate of waiver from the Centers for Medicare and Medicaid Services (CMS) that regulates all laboratory tests in the US through Clinical Laboratory Improvement Amendments (CLIA) and to have the tests that are authorized by the FDA. During the implementation of COVID-19 tests, pharmacists can coordinate with an authorized laboratory partner and coordinate tests through public health laboratories (American Pharmacists Association, 2020b). CDC have offered guidance to pharmacies for the infection control. They can be empowered to participate in routine testing for COVID-19 especially when less invasive methods are in place. One of the tests is COVID-19 RNA detection (RT-PCR) which can be done by collecting nasopharyngeal swab specimen from the individuals (England and Improvement, 2020, Poh and Lin, 2020).
Pharmacy staff should be trained and educated by an institution through approved training sessions to know more about the proper way of testing and the Personal Protective Equipment (PPE) procedures to reduce contagion risk prior to implementing the tests (Aruru et al., 2020, Sin et al., 2020).
Community Pharmacists were at the frontline as a part of the emergency team group fighting against COVID-19. They had a direct role in management of infected cases and physical assessment activities. The Rite Aid Corporation and the Consumer Value Stores (CVS) pharmacies in North America rolled out a point-of-care testing by drive-through testing stations. Community pharmacies in Nebraska have already begun offering testing services for COVID-19 (Bragazzi et al., 2020).
Department of Health and Human Services (HHS) in the US has authorized all pharmacists across the country to provide COVID-19 diagnostic tests that are approved by the US FDA, under the Public Readiness and Emergency Preparedness (PREP) Act (US Department of Health and Human Services, 2020).
It was expected that by the fall of 2020, a lot of pharmacies will be providing one of these services, offering home testing kits, collecting specimens and sending them to their laboratory partner. In addition, gathering specimens for point-of-care antibody surveillance. CMS are supporting the pharmacists and reimbursing them for their significant roles in COVID-19 testing (Strand et al., 2020).
4.6. Providing immunization
US pharmacists have experienced being immunizers for many years(Hayden and Parkin, 2020) (after receiving the required training) (Merks et al., 2020). They have enhanced rates of immunization by reaching people with less opportunity to be immunized, and keeping them updated on immunizations. An easy access to community pharmacists allows for a large coverage (Hayden and Parkin, 2020). In 2009 during H1N1 pandemic, community pharmacists’ help led to an increase in vaccine doses given to 80% of the population in a short time (Cadogan and Hughes, 2020). And in 2013, further 4.1 million adults in the US were immunized (against influenza) due to the contribution of pharmacists. It is recommended that state pharmacists immunization authority includes all the vaccines approved by FDA along with COVID-19 new vaccine (American Pharmacists Association, 2020a).
Aiming to decrease the overload on the healthcare systems, extended roles of pharmacists including immunization should be introduced by policymakers in many regions (Merks et al., 2020). Once a COVID-19 vaccine is available, pharmacists should be allowed to immunize the population, (Elbeddini et al., 2020a) as they have proved their ability to be immunizers after completing the suitable training in some countries.
4.7. Drive-through service
Community pharmacies as a form of healthcare facilities are working hard during the pandemic to ensure continuous delivery of pharmacy services by managing innovative methods while safeguarding all the preventative procedures recommended by the WHO. An example of value-added services (VAS) that has been popularized globally during COVID-19 pandemic is “Drive-through pharmacy” or “Drive-thru pharmacy”. Although this is not a very recent service, as it was first presented in the US in 1990 s to improve the patients' satisfaction, it seems to grow recently and can achieve many advantages during this crisis. The most important advantage is reducing the chances of virus spread by limiting human interactions. From 2008 to 2020, many countries around the world have started providing this service for varies objectives and impacts. Examples of these countries from the earliest to the most recent are UK, Malaysia, Australia, Taiwan, Jordan, Croatia, and recently United Arab Emirates (UAE) and Qatar (Hussain et al., 2020).
Thumbay pharmacy in the UAE has started providing 24-hour “drive-through pharmacy service”, in addition to Doha city in Qatar, both were launched for the sake of ensuring consumers safety and social distancing in line with COVID-19 precautions. The process is very simple and similar to fast-food drive-through services, patients will come by their cars and receive their pre-packed medications without stepping out of them, thus medicines will continue to be provided while ensuring patients and pharmacists safety by limiting their contacts. Other positive impacts of drive-thru pharmacies unrelated to COVID −19 pandemic are lessen patients waiting time in the pharmacies by providing fast delivery of medicines, limit car-parking problems, fast prescription refilling, and help parents with children to easily pick up their medications. On the other hand, drive-thru pharmacy services can have some drawbacks such as medication errors due to interruptions at the windows, limited time for advising and counselling. Community pharmacists should provide a standardized pharmacy practice and make a balance between facilitating medications dispensing during this crisis, and ensure providing adequate counselling or even leaflets and written instructions to the patients (Hussain et al., 2020).
4.8. Home delivery service
The appropriate supply of medicines is very significant especially for elderly and high-risk group patients during this public health emergency, so many pharmacies have organized the home delivery of medicines (International Pharmaceutical Federation, 2020). Patients with AIDS, asthma, tuberculosis, diabetes, hypertension, and COPD or with other chronic conditions are more vulnerable to the risk of COVID-19 infection. Those patients will expose themselves to a large group of people during collecting their medications either by using congested public transport or waiting in line at facilities. The Metropolitan Health Center (MMC) decided to support the better-controlled patients by receiving pre-packaged medications from the pharmacy or by other volunteer groups (Brey et al., 2020).
This crisis opened the door for online dispensing of prescriptions and home delivery of medicines to the appropriate patients. Community pharmacists can get the prescriptions from the patients by online means (Zheng et al., 2020). These solutions can contribute significantly in limiting the access to the pharmacy especially for the high-risk patients under home quarantine or elderly or immunocompromised patients, as well as enhancing the workflows to ensure social distancing (Al-Quteimat and Amer, 2020). Pharmacists’ response to COVID-19 have differed between the countries. For instance, pharmacists in New Zealand (NZ) have been supported by the government for their contribution during COVID-19 pandemic. They have created hotline numbers to encourage the phone consultations and prescription orders for home delivery to minimize the need for in-person interactions, and to prevent the undue patients visits to the pharmacy. Also, pharmacists in Australia have been encouraged to use the remote dispensing of prescriptions by contacting the physicians to receive a digital copy of the prescription, for example faxed prescriptions, or by using electronic transfer of prescriptions (ETP) (Bukhari et al., 2020).
Pharmacy staff in Ireland follow the appropriate instructions on the Pharmaceutical Society of Ireland (PSI) delivery guidance on the safe and organized delivery of medicines. So, if the volunteers were aligned to deliver the required medicine, the pharmacist should supervise them and a confidentiality agreement between them should be signed. Pharmacists are integral component of the healthcare system, they contact the patients and make sure about the proper use, storage, and disposal of the medications. In addition to that, they should always review the therapeutic effect of the prescribed medicines. Pharmacists provide the telephone number of the pharmacy for the patient’s counselling, or if they have any queries or issues about their medicines. The pharmacy staff ensure the medicines were placed in a sealed bag and they print a sticker with verified patient name, addresses, and their contact number on the parcels. Pharmacists may keep a record sheet or email of delivery with them to make sure the appropriate delivery has been made and the right medicine received by the right patient (Health Service Executive, 2020).
Different countries have extremely supported these services. Pharmacies in the higher income commonwealth countries such as the UK, Australia and NZ move towards these new models of delivery (Chan et al., 2020). Also, pharmacists in China have used all the possible resources to ensure the patients’ safety. Innovative methods can be used to promote the dispensing process and sending drugs safely to patients with critical cases at their homes. They have the responsibility to review the prescriptions efficiently and accurately using the CDSS to ensure the medication safety, also to reduce the risk of medication errors and any irrational prescriptions or drug-drug interactions (Li et al., 2020).
The Italian Federation of Community Pharmacy Owners in coordination with the Italian Red Cross has introduced a free delivery service which is available 24 h per day to serve the elderly patients, and home quarantine patients (International Pharmaceutical Federation, 2020).
In Spain, the General Council of Pharmacists has contributed with the Red Cross with the permission of the Ministry of Health to offer the delivery services to patients with mobility problems, diabetes, chronic respiratory diseases, and cardiovascular diseases to facilitate distribution of medications to them without leaving their homes. The network consists of 22,102 pharmacies and more than 200,000 Red Cross volunteers (Merks et al., 2020).
4.9. Quarantined patients’ home care
According to the WHO, patients with severe symptoms of COVID-19 infection should be isolated in hospitals to be managed in case of any complications happened and to ensure their proper monitoring. Also, in case the inpatient setting is not safe and limited capacity and resources are available. Patients are recommended to be isolated at home if they do not suffer from severe symptoms or any chronic diseases such as cardiovascular diseases, lung diseases or any underlying conditions such as renal failure. COVID-19 patients with mild symptoms may take the supervision and counseling of the pharmacists or any other members of the healthcare team. Pharmacists play an important role in educating patients and household members to maintain the proper hygiene and to prevent the spread of the infection to the other members of the family (International Pharmaceutical Federation, 2020). Pharmacists may advice the patients to follow all the guidelines recommended by the WHO for the proper cleaning of the home environment and the measures that should be taken in case their condition got worse (Zheng et al., 2020).
4.10. Community pharmacist’s telehealth services
Just like clinical pharmacists, community pharmacists worldwide have shifted to telehealth. They are meeting their clients using online video/phone call to check their adherence to their medications (Bragazzi et al., 2020). Pharmacists should guide patients with chronic disorders to self-monitor their medications safety and effectiveness. For that reason, mobile apps have been used by the community pharmacists in China, also to consult patients and inform them about the drugs availability and their supply (Zheng et al., 2020). In the US, community pharmacies in the rural areas have been providing pharmaceutical services through the telehealth means. Telehealth was shown to be effective in asthma management in community settings. Additionally, telehealth can be beneficial for community pharmacists to help patients differentiate COVID-19 infection from sessional flu according to their signs and symptoms, then refer them for testing to a suitable medical facility, (Ibrahim et al., 2020). and direct them on symptoms management (Elbeddini and Yeats, 2020).
4.11. Community pharmacist’s psychological support
In addition to the effective contribution of clinical pharmacists in supporting the psychological health of COVID-19 patients, also community pharmacists’ role in this area is worthy mentioned. It is very important to pay attention to the psychological conditions of the patients, and to provide support to those with excessive fear and refer them if they are suffering from advanced conditions to psychiatrists for further assessments. Moreover, community pharmacists can help patients and public to know COVID-19 facts, so this can help them to be more optimistic and continue doing their work as usual, and advise them to do some exercises to get rid of negative feelings and boost their immune system (Zheng et al., 2020).
4.11.1. Pharmacy setting changes and infection control
During this current health distress, a lot of guiding principles about preventive measures have been published to all healthcare providers including physicians, nurses, and pharmacists in general to implement them while carrying out their work. But it is also known that community pharmacists specifically are the frontline warriors and the first point of interaction with the public, so their role is very crucial, and safe management of their pharmacies should be secured (Mahendra et al., 2020).
Many pharmacy setting changes have been adopted to control COVID-19 infection and ensure patients and staff safety (Mahendra et al., 2020). Firstly, it is important to know how the virus transmits to control it and limit its spread (International Pharmaceutical Federation, 2020). These changes that are being followed by a lot of community pharmacies worldwide include; maintaining safe distancing (2 m) between all individuals and this can be done using physical barriers to hinder interpersonal closeness or by doing colorful floor marking, covering the dispensing area with a plastic shield, reducing the number of patients that can enter the pharmacy at once based on the area available, restricting the access to OTC products to avoid contaminating them, using baskets instead of hands to exchange money, medicines and prescriptions. Also, instructional posters can be placed on doors and read by patients before entering the pharmacy. Moreover, providing disinfectants for pharmacists and public and avoiding touching facial T-zone is important. Furthermore, several protective measures must be followed by community pharmacists to keep them safe, such as wearing masks and lab coats all the time and to be changed frequently or using disposable ones, leaving the important objects only at the counter and avoid doing any tests such as BP and blood sugar measurements for suspected patients (Mahendra et al., 2020).
Cleaning the pharmacy is important and happens regularly in normal conditions, however this must be done more strictly during this pandemic. Also, objects that can be used frequently by many pharmacists such as light switches, doorknobs, chairs, and tables must be sterilized periodically with great care, because they can easily transmit the infection. Moreover, wastes should be managed and disposed regularly and in the correct manner (Mahendra et al., 2020). In addition, other healthcare providers should be encouraged to contact community pharmacists by phones or messages if necessary, and avoid pharmacy visits. Home delivery services should be provided in case it was not available previously, also pharmacists should be required to complete short online training course about infection control to be a role model for public and educate them properly (Arain et al., 2020).
If a case is suspected, an isolation room must be available inside the pharmacy in order to isolate the patient until the arrival of the emergency staff. This room ensures that the patient will not spread the virus and must contain little furniture for the patient to use. Once the patient has left the pharmacy, the room should be sterilized and cleaned well (International Pharmaceutical Federation, 2020).
It is necessary to continue applying all of these pharmacy setting changes and infection control measures and precautions even if the virus spreading stopped for an appropriate period of time to ensure that another outbreak will not occur.
4.11.2. Limitations of pharmacists’ involvement in disasters management and how to solve it
There are many challenges facing pharmacists in crises management, such as in the current situation of the COVID-19 pandemic. Many pharmacists do not have the training and curriculum required in the pharmacy field to manage these crises, and at the same time there is a misconception by many people who think that the pharmacists role is only limited in selling and dispensing medicines, those people do not know the nature of work of pharmacists in the wide pharmacy field which constitutes a major obstacle in front of pharmacists or results in unwillingness to carry out tasks or join training programs that aims to teach how to deal with disasters management. Therefore, there must be a legislative support for pharmacists by the policymakers to increase their recognition in the society as an integral part of the healthcare team and allowing them to accomplish specific tasks aimed at enhancing their value in society and improve their ability to manage diseases and deal with disasters efficiently. In addition to that, boosting their role to be an integral part in the training programs and gain the skills required for professional management of crises (Saghir et al., 2020).
4.11.3. Pharmacists’ role in the post COVID −19 era (Aftermath)
Certainly, the indispensable roles of pharmacists will continue even after COVID-19 world. They will follow the gradual return to normal life carefully and continue improving global health, so the world can re-build trust and return interconnected as it was before. Influenza vaccination will be essential in winter seasons because of symptoms similarity with COVID-19 and to avoid further crowding in healthcare facilities. Pharmacists will be an active part of immunization operations against influenza if the disease persists and against COVID-19 when it becomes available. Also, they will keep following the ongoing clinical trials and researches to develop a very efficient treatment for COVID-19, if an effective one is announced, they will be responsible about its manufacturing, monitoring their drug-drug interactions, packaging, storage, and distribution (Bragazzi et al., 2020).
5. Conclusion
Along with pharmacists’ conventional roles which have been more remarkable with current circumstances, many of the novel roles have emerged and spread to adapt to changes during this pandemic in order to ensure continuity of healthcare services and alleviate pressure on other healthcare systems. However, it will be better to continue performing some of the new roles even after the pandemic of COVID-19 is resolved.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Osama Mohamed Ibrahim, Email: oibrahim@sharjah.ac.ae.
Rana M. Ibrahim, Email: ribrahim@sharjah.ac.ae.
Yousra A. Ibrahim, Email: yosraazhari16@gmail.com.
Eiman A. Madawi, Email: eiman.madawi@gmail.com.
Maryam Y. Al Deri, Email: maryamaldeiri@gmail.com.
References
- Al-Quteimat O.M., Amer A.M. SARS-CoV-2 outbreak: How can pharmacists help? Res. Soc. Adm. Pharm. 2020;26:30238–30240. doi: 10.1016/j.sapharm.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amariles, P., Ledezma-Morales, M., Salazar-Ospina, A., Hincapié-García, J.A., 2020. How to link patients with suspicious COVID-19 to health system from the community pharmacies? A route proposal. Res. Soc. Adm. Pharm. doi:10.1016/j.sapharm.2020.03.007. [DOI] [PMC free article] [PubMed]
- American Pharmacists Association, 2020a. Executive Summary: PharmacyPharmacists as Front-Line Responders for COVID-19 Patient Care [WWW Document]. URL https://www.pharmacist.com/sites/default/files/Pharmacists_COVID19_4_3_2020.pdf (accessed 6.3.20).
- American Pharmacists Association, 2020b. Pharmacy Models for COVID-19 Testing Pharmacy Models for COVID-19 [WWW Document]. URL https://apha.us/TestingModels (accessed 9.13.20).
- Arain S., Thalapparambath R., Al Ghamdi F.H. COVID-19 pandemic: Response plan by the Johns Hopkins Aramco Healthcare inpatient pharmacy department. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aruru M., Truong H.A., Clark S. Pharmacy Emergency Preparedness and Response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res. Soc. Adm. Pharm. 2020;30323–30328 doi: 10.1016/j.sapharm.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahlol M., Dewey R.S. Pandemic preparedness of community pharmacies for COVID-19. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basheti I.A., Nassar R., Barakat M., Alqudah R., Abufarha R., Muqatash T., Saini B. Pharmacists’ readiness to deal with the coronavirus pandemic: Assessing awareness and perception of roles. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzell B., Wagner D., Durant K.M., Callahan B. Insights on developing a field hospital formulary and medication distribution process in preparation for a second surge of COVID-19 cases. Am. J. Heal. Pharm. 2020;77:1763–1770. doi: 10.1093/ajhp/zxaa232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bragazzi N.L., Mansour M., Bonsignore A., Ciliberti R. The Role of Hospital and Community Pharmacists in the Management of COVID-19: Towards an Expanded Definition of the Roles, Responsibilities, and Duties of the Pharmacist. Pharmacy. 2020;8:140. doi: 10.3390/pharmacy8030140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brey Z., Mash R., Goliath C., Roman D. Home delivery of medication during Coronavirus disease 2019, Cape Town, South Africa: Short report. African J. Prim. Heal. Care Fam. Med. 2020;12:2449. doi: 10.4102/PHCFM.V12I1.2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukhari N., Rasheed H., Nayyer B., Babar Z.U.D. Pharmacists at the frontline beating the COVID-19 pandemic. J. Pharm. Policy Pract. 2020;13:8. doi: 10.1186/s40545-020-00210-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadogan C.A., Hughes C.M. On the frontline against COVID-19: Community pharmacists’ contribution during a public health crisis. Res. Soc. Adm. Pharm. 2020;30292 doi: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2020. Reducing Stigma [WWW Document]. URL https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/reducing-stigma.html (accessed 9.15.20).
- Chan A.H.Y., Rutter V., Ashiru-Oredope D., Tuck C., Babar Z.U.D. Together we unite: The role of the Commonwealth in achieving universal health coverage through pharmaceutical care amidst the COVID-19 pandemic. J. Pharm. Policy Pract. 2020;13:13. doi: 10.1186/s40545-020-00214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Treatment Guidelines Panel, 2020. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines [WWW Document]. Natl. Institutes Heal. URL https://www.covid19treatmentguidelines.nih.gov/ (accessed 11.18.20).
- Elbeddini A., Prabaharan T., Almasalkhi S., Tran C. Pharmacists and COVID-19. J. Pharm. Policy Pract. 2020;13:36. doi: 10.1186/s40545-020-00241-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbeddini A., Wen C.X., Tayefehchamani Y., To A. Mental health issues impacting pharmacists during COVID-19. J. Pharm. Policy Pract. 2020;13:46. doi: 10.1186/s40545-020-00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbeddini A., Yeats A. Pharmacist intervention amid the coronavirus disease 2019 (COVID-19) pandemic: From direct patient care to telemedicine. J. Pharm. Policy Pract. 2020;13:23–26. doi: 10.1186/s40545-020-00229-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erku D.A., Belachew S.A., Abrha S., Sinnollareddy M., Thomas J., Steadman K.J., Tesfaye W.H. When fear and misinformation go viral: Pharmacists’ role in deterring medication misinformation during the “infodemic” surrounding COVID-19. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross A.E., MacDougall C. Roles of the clinical pharmacist during the COVID-19 pandemic. J. Am. Coll. Clin. Pharm. 2020;3:564–566. doi: 10.1002/jac5.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvard University, 2020. Treatments for COVID-19 [WWW Document]. Harvard Heal. Publ. URL https://www.health.harvard.edu/diseases-and-conditions/treatments-for-covid-19 (accessed 11.19.20).
- Hayden J.C., Parkin R. The challenges of COVID-19 for community pharmacists and opportunities for the future. Ir. J. Psychol. Med. 2020;37:198–203. doi: 10.1017/ipm.2020.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Service Executive, 2020. Home delivery of medicines by public servants and volunteers during the COVID-19 pandemic.
- Hua X.L., Gu M., Zeng F., Hu H., Zhou T., Zhang Y., Shi C. Pharmacy administration and pharmaceutical care practice in a module hospital during the COVID-19 epidemic. J. Am. Pharm. Assoc. 2020;60:431–438. doi: 10.1016/j.japh.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain R., Dawoud D.M., Babar Z.U.D. Drive-thru pharmacy services: A way forward to combat COVID-19 pandemic. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim O.M., Ibrahim R.M., Al Meslamani A.Z., Al Mazrouei N. Role of telepharmacy in pharmacist counselling to coronavirus disease 2019 patients and medication dispensing errors. J. Telemed. Telecare. 2020 doi: 10.1177/1357633X20964347. [DOI] [PubMed] [Google Scholar]
- International Pharmaceutical Federation, 2020. COVID-19: Guidelines for Pharmacists and the Pharmacy Workforce.
- Kamps, B.S., Hoffmann, C., 2020. COVID Reference, 4th ed. Steinhaeuser Verlag.
- Lall S., Singh N. Over the counter drug use: Assessing the perception of the community. Int. J. Res. Pharm. Sci. 2020;11:3580–3584. doi: 10.26452/ijrps.v11i3.2514. [DOI] [Google Scholar]
- Li H., Zheng S., Liu F., Liu W., Zhao R. Fighting against COVID-19: Innovative strategies for clinical pharmacists. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Luo P., Tang M., Hu Q., Polidoro J.P., Sun S., Gong Z. Providing pharmacy services during the coronavirus pandemic. Int. J. Clin. Pharm. 2020;42:299–304. doi: 10.1007/s11096-020-01017-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahendra D.D., Bhushan P.R., Mahendra D.Y. Community pharmacists: Frontline COVID-19 warriors and the approaches for the safe management of the pharmacies during the pandemic. World J. Adv. Res. Rev. 2020;6:176–185. doi: 10.30574/wjarr. [DOI] [Google Scholar]
- Malik M., Tahir M.J., Jabbar R., Ahmed A., Hussain R. Self-medication during Covid-19 pandemic: challenges and opportunities. Drugs Ther. Perspect. 2020;36:565–567. doi: 10.1007/s40267-020-00785-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng L., Huang J., Qiu F., Sun S. Roles of the Chinese clinical pharmacist during the COVID-19 pandemic. J. Am. Coll. Clin. Pharm. 2020 doi: 10.1002/jac5.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merks P., Jakubowska M., Drelich E., Świeczkowski D., Bogusz J., Bilmin K., Sola K.F., May A., Majchrowska A., Koziol M., Pawlikowski J., Jaguszewski M., Vaillancourt R. The legal extension of the role of pharmacists in light of the COVID-19 global pandemic. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institue for Health and Care Excellence, 2020. COVID-19 rapid evidence summary: vitamin D for COVID-19 [WWW Document]. URL www.nice.org.uk/guidance/es28 (accessed 11.15.20).
- NHS England and NHS Improvement, 2020. Novel Coronavirus (COVID-19) Standard Operating Procedure: Community pharmacy [WWW Document]. URL http://psnc.org.uk/tees-lpc/wp-content/uploads/sites/11/2020/02/covid-19-primary-care-sop-community-pharmacy-v1.pdf (accessed 9.12.20).
- Poh A., Lin W. Role of the pharmacist during the COVID-19 pandemic: a time to rethink strategies. Singapore Med. J. 2020 doi: 10.11622/smedj.2020098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saghir S., Hashmi F.K., Khadka S., Rizvi M. Paradigm Shift in Practice: The Role of Pharmacists in COVID-19 Management. Eur. J. Med. Sci. 2020;2:60–64. doi: 10.46405/ejms.v2i2.93. [DOI] [Google Scholar]
- Schellack N., Coetzee M., Schellack G., Gijzelaar M., Hassim Z., Milne M., Bronkhorst E., Padayachee N., Singh N., Kolman S., Gray A.L. COVID-19: Guidelines for pharmacists in South Africa. South. African J. Infect. Dis. 2020;35:206. doi: 10.4102/sajid.v35i1.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal E.M., Alwan L., Pitney C., Taketa C., Indorf A., Held L., Lee K.S., Son M., Chi M., Diamantides E., Gosser R. Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. Am. J. Heal. Pharm. 2020;77:1403–1408. doi: 10.1093/ajhp/zxaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin J.H., Ian Richards I., Ribisi M.S. Maintaining comprehensive pharmacy services during a pandemic: Recommendations from a designated COVID-19 facility. Am. J. Heal. Pharm. 2020;77:1522–1528. doi: 10.1093/ajhp/zxaa194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Z., Hu Y., Zheng S., Yang L., Zhao R. Hospital pharmacists’ pharmaceutical care for hospitalized patients with COVID-19: Recommendations and guidance from clinical experience. Res. Soc. Adm. Pharm. 2020;3:30314. doi: 10.1016/j.sapharm.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strand M.A., Bratberg J., Eukel H., Hardy M., Williams C. Community Pharmacists’ Contributions to Disease Management During the COVID-19 Pandemic. Prev. Chronic Dis. 2020;17 doi: 10.5888/pcd17.200317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Pharmacy Guild of Australia, 2020. Limits on dispensing and sales of prescription and over-the-counter medicines [WWW Document]. URL https://www.guild.org.au/news-events/news/2020/limits-on-dispensing-and-sales-of-prescription-and-over-the-counter-medicines (accessed 11.19.20).
- Ung C.O.L. Community pharmacist in public health emergencies: Quick to action against the coronavirus 2019-nCoV outbreak. Res. Soc. Adm. Pharm. 2020;16:583–586. doi: 10.1016/j.sapharm.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services, 2020. Guidance for Licensed Pharmacists, COVID-19 Testing, and Immunity under the PREP Act.
- Visacri, M.B., Figueiredo, I.V., Lima, T. de M., 2020. Role of pharmacist during the COVID-19 pandemic: A scoping review. Res. Soc. Adm. Pharm. doi:10.1016/j.sapharm.2020.07.003 [DOI] [PMC free article] [PubMed]
- World Health Organization. Regional Office for Europe, 2020. Strengthening the health systems response to COVID-19: Technical guidance #4 [WWW Document]. URL https://apps.who.int/iris/bitstream/handle/10665/332572/WHO-EURO-2020-677-40412-54174-eng.pdf?sequence=1&isAllowed=y (accessed 6.2.20).
- Ying W., Qian Y., Kun Z. Drugs supply and pharmaceutical care management practices at a designated hospital during the COVID-19 epidemic. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai P., Ding Y., Wu X., Long J., Zhong Y., Li Y. The epidemiology, diagnosis and treatment of COVID-19. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng S.Q., Yang L., Zhou P.X., Li H.B., Liu F., Zhao R.S. Recommendations and guidance for providing pharmaceutical care services during COVID-19 pandemic: A China perspective. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]