Abstract
Treatment gaps of 60-70%, reflecting, amongst many other factors, Human Resources shortfalls means that 150 million India never accessed mental healthcare. In Punjab, mental health training is required in primary health centers. A short-term synchronous training was conceptualized by the National Institute of Mental Health and Neurosciences. A total of 114 primary care doctors participated for the training. Substantial positive changes in knowledge, attitudes and practices were noted. Task sharing and capacity building initiatives can be undertaken during the pandemic to meet the demand for mental healthcare service delivery.
1. Background
Even before the pandemic began, mental health conditions (MHCs) in the population were on their way to being an unmitigated disaster for the Indian population. The overall lifetime prevalence for any MHC excluding alcohol or tobacco use was nearly 14% - roughly 210 million persons. Treatment gaps reflecting amongst many other factors, Human Resources shortfalls and access limitations mean that 60–70% i.e. 150 million of them never were able to access formal medical care. (Gururaj et al., 2016).
With the pandemic, these numbers, according to many experts have only risen while the accessibility and availability of mental health (MH) care resources have suffered strictures (Kola et al., 2021, Tandon, 2021a). A concerning statistic is the persistence of high numbers of suicide during the pandemic even with the commercial and mobility restrictions (Appleby, 2021, Tandon, 2021b). Some experts have warned of increases in suicides especially in India based on increased media reporting of suicides during the pandemic (Balaji and Patel, 2020). Also, a comprehensive report for the region states that depression and anxiety, alcohol use, somatic concerns, sleep related difficulties have shown sharp rises (Banerjee et al., 2020).
These symptoms have been associated with social isolation, increased loneliness, increased screen use, restricted avenues for support, significant life events such as job loss or financial or health related adversities. Unmitigated, these are poised to be the next overwhelming disaster. Along with the general population, the scale of the pandemic's disruptions and associated loss of life has affected healthcare workers too - an increase in their psychological morbidities, sleep related problems, burnout have been noted (Chew et al., 2020).
Making matters worse, the pandemic and its consequent public health strategies have curtailed outreach MH camps and community mobilizations of paraprofessionals and volunteers. MH care resources have been redeployed to aid with the acute care delivery for those with COVID 19 (Khichar et al., 2020, Mukherjee and Parashar, 2020). Prior to the pandemic, India’s MH care responses were on track to being scaled up and integrated with physical health care (Kumar et al., 2020; “National Mental Health Programme (NMHP)::(1982), National Health Mission,” n.d.). Essential to these objectives are capacity building and systems strengthening strategies.
The state of Punjab with its 22 districts has a population of 30 million (“State Profile – Government of Punjab, India,” n.d.). District Mental Health Program (DMHP) which is the essential implementation unit of India’s national mental health program is functional in all its districts (Khurana and Sharma, 2016). Greater synergism of the DMHP with the primary healthcare services is required (Sadh et al., 2019).
Increased awareness of MH issues especially those associated with substance use disorders was present; a further requirement was improved competencies for primary care doctors (PCDs) to screen, diagnose and provide basic management for various MHCs. Usual in person trainings became untenable, owing to the pandemic and consequent restrictions. Telemedicine approaches to delivering, mentoring and capacity building towards task sharing can provide a solution.
National Institute of Mental Health and Neurosciences (NIMHANS) has been a pioneer in such capacity building programs (Pahuja et al., 2020a). Many innovative models, courses and curricula have been developed (Manjunatha et al., 2018; Pahuja et al., 2020b). NIMHANS partners with State Health Administration to train primary care personnel (Manjunatha et al., 2019). Many novel approaches to enhance clinical learning over video conferencing platforms have been developed. Most of these initiatives had short term in-person visits and sensitization engagements (Kulkarni et al., 2018). However, on account of the pandemic and its restrictions this could not be undertaken. We provide here a report on engagement of PCDs in Punjab for a digital introductory MH training ( Table 1).
Table 1.
Details of participating primary care doctors.
| Participant details | Percentage |
|---|---|
| No of people working in a prison setting | 10.5% |
| No of doctors in district hospitals | 35.1% |
| Mental health training beyond internship | 22% |
| Perceived need for training | 99% |
2. Methods
A short-term synchronous training was conceptualized by NIMHANS. Training sessions included topics such as identification management, common mental disorders, severe mental disorders, substance use disorder ( Table 2).
Table 2.
Details of training program and feedback.
| S.no. | Topic | Number of participants | How would you rate the content of the session? | The session was interactive and engaging | The session highlighted issues I face in my practice |
|---|---|---|---|---|---|
| 1 | Introduction to the Program and Evaluation of Psychiatric Disorders – CSP Manual | 11 | 8.6 | 4.3 | 4 |
| 2 | Evaluation & Management of Common Mental Disorders | 24 | 9.5 | 4.8 | 4.4 |
| 3 | Evaluation & Management of Severe Mental Disorders | 43 | 9.2 | 4.6 | 4.3 |
| 4 | Evaluation & Management of Alcohol, Cannabis & Tobacco Use Disorders | 29 | 9.3 | 4.4 | 4.0 |
| 5 | Handling Psychiatric Emergency at Primary Care | 17 | 9.5 | 4.6 | 4.7 |
| 6 | Handling Special Population at primary care (Children, Adolescents, Perinatal and Geriatric population) | 31 | 9.0 | 4.3 | 4.3 |
3. Assessments
A survey of attitudes and practices prior to the training and follow up 1 month post training was completed to. All participants were provided an optional self-assessment quiz. This was available to them at the beginning of the training and 6 weeks after completion of the training. Each time the quiz remained accessible for 7 days post launch. The self-assessments contained case-based questions and highlighted common practice issues.
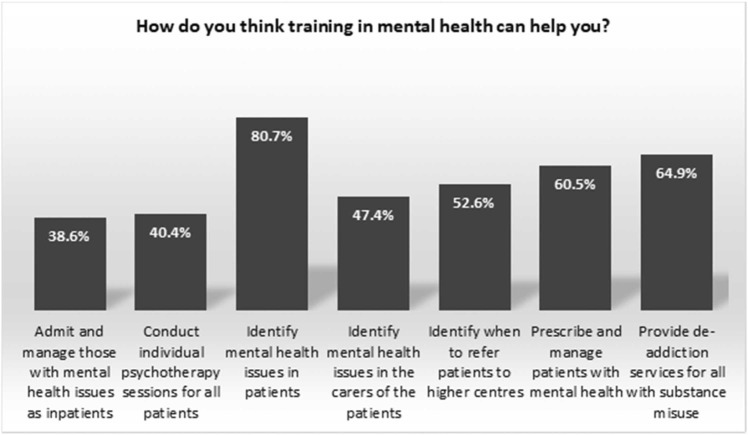
After each session that lasted for 90–120 min (refer Table 2), feedback forms were sent to gauge the scope for improvements. We also surveyed the PCDs for their perceived needs with regard to MH training and their expectations of how they would be helped (refer Fig. 1). The resource persons adopted adult learning principles (Adult Learning Theories and Principles, 2004). Sessions featured case-based discussions on clinical and management problems and possible solutions. The topics were included with groundings to their clinical and practical experiences managing MHCs especially in busy primary care outpatient departments. Discussions were participatory and inclusive in a supportive atmosphere.
Fig. 1.
Reported expectations from mental health training.
We present here the results of the various surveys and how they inform on proceeding forward with capacity building and task sharing during the pandemic. The training was conducted between January to March, 2021. All data from surveys were anonymized at the point of collection and stored securely in password protected cloud-based folders, with consent from participants. No prior ethical permissions were deemed necessary keeping in mind the ICMR guidelines regarding the research and publication of education related surveys (“ICMR, 2017). Permissions were sought from the directorate health services and state nodal officer for MH towards the analysis and publication of these surveys’ results.
We note there that the health administrators of Punjab facilitated the participation of PCDs by providing the requisite permissions. PCDs who completed the training and attended 75% of the sessions were provided with certificates of participation and appreciation by NIMHANS. Table 3.
Table 3.
Age, experience, pre training scores and post training scores of participants.
| Mean | Standard Deviation | Minimum value | Maximum value | Interquartile range | |
|---|---|---|---|---|---|
| Age | 32 | 6.44 | 23 | 56 | 7 |
| Experience | 4 | 5.2 | < 1 | 27 | 3 |
| Pre training knowledge test score | 11 | 3 | 4 | 17 | 5 |
| Post training knowledge test score | 15 | 4 | 7 | 19 | 6 |
4. Results
A total of 114 PCDs enrolled for the training. Their average age was 32 years and they reported a mean experience of four years. However, we note that reported experience varied across participants; ranging from a few months to even 27 years. Most were working in a primary health center with about 10% working in prison settings.
All PCDs informed they needed further training in providing MH care services. Most also reported having challenging situations and dissatisfaction in their care approaches to MHCs. They also indicated various expectations as depicted in Fig. 1.
Through the training, 37% improvements in knowledge scores of the participants on case-based scenarios were noted. These assessments were separated in time. Improvements in attitudes and practices towards MHCs were also noted. Participants’ feedback for each of the sessions were analyzed and are presented in Table 2. These demonstrate high participant engagement and satisfaction.
5. Discussions
These results show that MH training as part of capacity building for PCDs was feasible and benefited PCDs in gaining knowledge. The post training assessments were conducted 4–5 weeks after the completion of training indicating the retention of knowledge and could be expected to have translated into clinical practice. We note that most PCDs had very short periods of clinical experience. We note that a majority of the PCDs worked in primary health centers and did not have any MH training post their rotations in medical internship - an essential partial fulfillment for their recognition and qualification as medical doctors (“UG Curriculum, 2019). This could explain their readiness to participate in the online training. Almost all PCDs had taken up consultations for MH in the recent past and all reported a need for further training in providing MH care. We also note the very varied expectations that the PCDs reported about any MH training (Fig. 1). Table 2 also reports on the trainee perceptions with regard to each session.
In many aspects the training provided and the results we obtained are unique and provide optimistic support for the continuation and/or initiation of digitally delivered MH training for PCDs. Schedules permitting and with administrative willingness these trainings can be continued during the pandemic periods. We posit it would be time and cost efficient for state health administrations to foresee the increased burden of MH needs and build on the existing competencies of PCDs. In comparison with in-person training, remote MH training towards capacity building have proved just as effective with added benefits of saving time and costs (Delgoshaei et al., 2017, Khanra et al., 2021). We note some major differences from when remote MH training was conducted before and during the pandemic. The pandemic has mainstreamed MH concerns and impacts as never before and this has improved PCDs perceived need for training. Similar observations have been noted in a task shifting program in New York (Stevens et al., 2020). We also note that remote MH training too gained in acceptance with most even preferring such modes of delivery. We also point out here that along with the synchronous training we also provided video and document resources based on the discussions in sessions. Mentorship has been continued beyond the training to address clinical challenges and offer assistance in making diagnoses or initiating management strategies. An emphasis was also put on better educating PCDs on how to engage patients and families.
6. Strengths
To the best of the authors’ knowledge this is the first report of successful telementoring for MH care services during the COVID19 pandemic in a developing country. It is also the first report of continuing the MH related objectives of the National Health Mission and National Mental Health Programme during the pandemic in India. This paper reports on a successful MH teletraining towards capacity building of PCDs during the COVID 19 pandemic. Participatory, interactive, inclusive and experience-based sessions provided the bedrock for this initiative’s success. Regular feedback surveys demonstrated positive change and outcome.
7. Conclusions
Task sharing and capacity building initiatives can be undertaken during the pandemic to meet the demand for MH care service delivery. The pandemic has contextualized an opportunity for better integration of MH care service delivery within primary health settings. Remote digitally delivered MH teletraining can continue unabated during the pandemic with myriad benefits such as reduced cost, improved time efficiency and better safety noted on the horizon. We believe state health administrations would do best to initiate and/or continue such training programs towards realizing MH related objectives in the National Mental Health Programmes, National Health Mission and National Mental Health policy objectives.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The training program was funded and supported by the Directorate of Health Services, Department of Health and Family Welfare, Government of Punjab. Preparation of this manuscript, all assessments and analysis were conducted by NIMHANS.
References
- Adult Learning Theories and Principles, [WWW Document], 2004. URL https://www.wgu.edu/blog/adult-learning-theories-principles 2004.html#openSubscriberModal (accessed 13 August 2021).
- Appleby L. What has been the effect of covid-19 on suicide rates? BMJ. 2021:372. doi: 10.1136/BMJ.N834. [DOI] [PubMed] [Google Scholar]
- Balaji, M., Patel, V., 2020, Hunger, fear and isolation: An analysis of media reports of COVID-19 related suicides in India. https://doi.org/10.21203/RS.3.RS-99851/V1. [DOI] [PMC free article] [PubMed]
- Banerjee Vaishnav, Rao M., Raju T.S., Dalal M.S.V.K., Javed P., Saha A., Mishra G., Kumar K.K., Jagiwala, M.P V. Impact of the COVID-19 pandemic on psychosocial health and well-being in South-Asian (World Psychiatric Association zone 16) countries: a systematic and advocacy review from the Indian Psychiatric Society. Indian J. Psychiatry. 2020;62:343. doi: 10.4103/PSYCHIATRY.INDIANJPSYCHIATRY_1002_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew N.W., Lee G.K., Tan B.Y., Jing M., Goh Y., Ngiam N.J., Yeo L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., Sharma A.K., Komalkumar R., Meenakshi P., Shah K., Patel B., Chan B.P., Sunny S., Chandra B., Ong J.J., Paliwal P.R., Wong L.Y., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behav., Immun. 2020;88:559–565. doi: 10.1016/J.BBI.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgoshaei B., Mobinizadeh M., Mojdekar R., Afzal E., Arabloo J., Mohamadi E. Telemedicine: a systematic review of economic evaluations. Med. J. Islam. Repub. Iran. 2017;31:113. doi: 10.14196/MJIRI.31.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gururaj G., Varghese M., Benegal V., Rao G.N., Pathak K., Singh L.K., Mehta R.Y., Ram D., Shibukumar T.M., Kokane A., Lenin Singh R.K., Chavan B.S., Sharma P., Ramasubramanian C., Dalal P.K., Saha P.K., Deuri S.P., Giri A.K., Kavishvar A.B., Sinha V.K., Thavody J., Chatterji R., Akoijam B.S., das S., Kashyap A., Ragavan V.S., Singh S.K., Misra R. NMHS collaborators group. Natl. Ment. Health Surv. India. 2016;2015:16. [Google Scholar]
- ICMR, 2017, National Ethical Guidelines [WWW Document]. URL https://ethics.ncdirindia.org/ICMR_Ethical_Guidelines.aspx (accessed 13 August 2021).
- Khanra S., Mukherjee A., Goyal N., Das B., Munda S.K. Service utilization and saved travel cost in telepsychiatry consultation by outpatients at a psychiatric hospital in India during COVID-19 pandemic. Asian J. Psychiatry. 2021;57 doi: 10.1016/J.AJP.2021.102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khichar S., Midha N., Bohra G.K., Kumar D., Gopalakrishanan M., Kumar B., Sakthivadivel V., Garg M.K. Healthcare resource management and pandemic preparedness for COVID-19: a single centre experience from Jodhpur, India. Int. J. Health Policy Manag. 2020;9:493–495. doi: 10.34172/IJHPM.2020.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana S., Sharma S. National mental health program of India: a review of the history and the current scenario. Int. J. Community Med. Public Health. 2016;3:2696–2704. doi: 10.18203/2394-6040.IJCMPH20163191. [DOI] [Google Scholar]
- Kola L., Fmcpsych O., Health M. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;8:535–550. doi: 10.1016/S2215-0366(21)00025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni, K., Gowda, G.S., Malathesh, B.C., Kumar, S., Manjunatha, B.R., Shashidhara, H.N., Vinay, B., Manjunatha, N., Kumar, C.N., Math, S.B., 2018, Conference summary of “Ten days, on-site training of basic module of ‘primary care psychiatry program’ for primary care doctors of Uttarakhand.” Asian Journal of Psychiatry 36, 29–30. https://doi.org/10.1016/J.AJP.2018.05.028. [DOI] [PubMed]
- Kumar C.N., Chand P.K., Manjunatha N., Math S.B., Shashidhara H.N., Basavaraju V., Thirthalli J., Manjappa A.A., Parthasarathy R., Murthy P., Ibrahim F.A., Jagtap N., Jyrwa S., Reddy S., Arora S., Hawk M., Kumar S., Egan J., Mcdonald M. Impact evaluation of VKN–NIMHANS–ECHO model of capacity building for mental health and addiction. Methodol. Two Random Control. Trials. 2020;42:80–86. doi: 10.1177/0253717620969066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manjunatha, Kumar C.N., Math S.B., Thirthalli J. Designing and implementing an innovative digitally driven primary care psychiatry program in India. Indian J. Psychiatry. 2018;60:236. doi: 10.4103/PSYCHIATRY.INDIANJPSYCHIATRY_214_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manjunatha N., Kumar C., Math S., Basavaraju V., Shashidhara H., Parthasarathy P., Thirthalli J., Binukumar B. Karnataka Telemedicine Mentoring and Monitoring (KTM) program. Implement. Man. Prim. Care Psychiatry. 2019 [Google Scholar]
- Mukherjee A., Parashar R. Impact of the COVID-19 pandemic on the human resources for health in India and key policy areas to build a resilient health workforce. Gates Open Res. 2020:4. doi: 10.12688/GATESOPENRES.13196.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Mental Health Programme (NMHP), 1982. National Health Mission [WWW Document]. URL http://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1043&lid=359 (accessed 8.10.21).
- Pahuja E., Santosh K., Harshitha N., Fareeduzaffer, Manjunatha N., Gupta R., Kumar C., Math S., Chandra P. Diploma in primary care psychiatry: An innovative digitally driven course for primary care doctors to integrate psychiatry in their general practice. Asian J. Psychiatry. 2020:52. doi: 10.1016/J.AJP.2020.102129. [DOI] [PubMed] [Google Scholar]
- Pahuja Kumar, Uzzafar T.S., Manjunatha F., Kumar N., Gupta C.N., Math, S.B R. An impact of a digitally driven primary care psychiatry program on the integration of psychiatric care in the general practice of primary care doctors. Indian J. Psychiatry. 2020;62:690. doi: 10.4103/PSYCHIATRY.INDIANJPSYCHIATRY_324_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadh K., Kumar C.N., B C M., Kumar S., Chander R., Gowda G.S., Gowda V.B., H N S., Manjunatha N., Parthasarathy R., Rao G.N., Math S.B., Chandra P.S. Symposium summary on “Community Psychiatry and DMHP—An update.”. Asian J. Psychiatry. 2019;39:29–31. doi: 10.1016/J.AJP.2018.11.014. [DOI] [PubMed] [Google Scholar]
- State Profile – Government of Punjab, India [WWW Document], n.d. URL 〈https://punjab.gov.in/state-profile/〉 (accessed 8.17.21).
- Stevens C., Tosatti E., Ayer L., Barnes-Proby D., Belkin G., Lieff S., Martineau M. Helpers in plain sight: a guide to implementing mental health task sharing in community-based organizations. Help. Plain Sight: A Guide Implement. Ment. Health Task. Shar. Community-Based Organ. 2020 doi: 10.7249/TL317. [DOI] [Google Scholar]
- Tandon R. The bitter lessons of COVID-19: acknowledging and working through many points of tension. Asian J. Psychiatry. 2021;55 doi: 10.1016/J.AJP.2021.102545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon R. COVID-19 and suicide: Just the facts. Key learnings and guidance for action. Asian J. Psychiatry. 2021;60 doi: 10.1016/J.AJP.2021.102695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UG Curriculum | NMC, 2019, URL https://www.nmc.org.in/information-desk/for-colleges/ug-curriculum/ (accessed 13 August 2021).