Summary
Background
Non-emergent clinical services were limited or suspended during the early stages of the coronavirus disease 2019 (COVID-19) pandemic in the United States (U.S.). This could adversely impact epidemics of public health importance, such as HIV, and access to testing, which is a cornerstone of prevention efforts.
Methods
In this observational study, we collected HIV testing and positivity rate clinical data from four geographically diverse U.S. healthcare systems in New Orleans, Louisiana; Minneapolis, Minnesota; Providence, Rhode Island; and, Seattle, Washington. Data from 2019 to 2020 were examined to assess changes in HIV testing in community-based, emergency department, and outpatient settings. Poisson regression was used to explore trends in HIV testing through phases of the COVID-19 pandemic.
Findings
In outpatient settings, there was a 68-97% reduction in the number of HIV tests per week during each state's stay-at-home order period, compared to during the pre-stay-at-home order period in early 2020. HIV testing remained reduced 11-54% after states transitioned to advisory phases. The HIV positivity rate increased slightly at outpatient settings, except in New Orleans where it fell.
Interpretation
We found a concerning trend of substantially decreased HIV testing across four geographically diverse sites. These findings suggest that new HIV infections within the U.S. may be undiagnosed and not yet linked to clinical care and services, as a consequence of the COVID-19 pandemic. Thus, augmented efforts to identify patients and link them to HIV services will be needed as healthcare settings return to full operation.
Funding
U.S. National Institute of Mental Health.
Keywords: HIV, COVID-19, Pandemic, HIV testing
Research in context.
Evidence before this study
Due to the COVID-19 pandemic, significant disruptions in medical services occurred worldwide. In our clinical experience, one change was reduced outpatient HIV testing. We searched PubMed for primary research articles documenting COVID-19-related changes in HIV testing worldwide, published from January 2020 through June 2021, with no language restrictions, using the terms “COVID*” AND (“HIV” OR “AIDS”) AND “test*”. Our search revealed reports documenting reduced HIV testing in Australia, Belgium, China, Japan, multiple regions of Kenya, Uganda, and numerous other European countries. Data from the U.S. showed reduced HIV testing among men in some states. Additionally, data showed mixed trends in HIV positivity rates, with some sites reporting decreases and some reporting no change. Explanations for these reductions included systemic disruptions in access to clinics and services offered, avoidance of HIV testing due to fear of COVID-19 exposure, reduced HIV acquisition risk behaviors due to the pandemic, and reduced use of pre-exposure prophylaxis (PrEP).
Added value of this study
Despite worldwide evidence showing that HIV testing has declined during the COVID-19 pandemic, limited data have chronicled the extent of these changes in the U.S. The U.S. could show different trends given the size and population of the country, plus the reliance on individual states to lead pandemic responses, rather than the national government. Moreover, most reports have focused on the first 3–6 months of the pandemic at a single site or geographic region. Our analyses show that HIV testing dramatically decreased in four major healthcare systems in large metropolitan areas in diverse regions of the U.S. during the initial nine months of the pandemic, compared to 2019, but that rates are rebounding. In 2019, 40,620 HIV tests were performed compared to 27,112 in 2020. Additionally, results revealed that HIV positivity rates were generally higher at most sites during the pandemic, although differences were not statistically significant, except in New Orleans, where positivity rates fell.
Implications of all the available evidence
Timely HIV diagnosis is a key factor in linking patients to care and reducing further transmission. These results highlight the significant impact the COVID-19 pandemic is having on HIV testing. It is likely that some progress made towards ending the HIV epidemic in the U.S. will be undermined by COVID-19 because individuals with HIV in the community might not be accessing timely testing, which is a key step towards linkage to care and eliminating new HIV transmissions.
Alt-text: Unlabelled box
Introduction
In mid-March 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19), the illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a global pandemic.1 The COVID-19 pandemic led to widespread lockdowns and quarantines in attempts to control the spread of the SARS-CoV-2 virus. In the medical community, many non-emergent outpatient clinical services were limited or suspended, many providers shifted encounters to telehealth, virology laboratories closed or de-prioritized non-COVID-19 activities, and physical spaces were reconfigured to reduce transmission risk or to account for the treatment of patients with COVID-19.2,3 Additionally, numerous patients avoided seeking services due to fear of COVID-19 exposure at the clinic or on public transportation to the clinic.4 Moreover, some patients de-prioritized seeking care due to acute needs related to the pandemic (e.g., unemployment, food insecurity).5 In sum, the COVID-19 pandemic triggered a number of changes in the healthcare landscape that significantly altered the availability and experience of seeking and obtaining medical services.
Although necessary, these changes had unintended consequences on other aspects of public health. For instance, international data early in the pandemic showed that COVID-19 restrictions impeded access to testing for HIV. Decreased HIV testing is a major public health concern worldwide as it undermines timely linkage to care and initiation of treatment, which is vital to patients’ health and halting the spread of infection.6 In the early months of the pandemic, HIV testing dropped by >50% in a Belgian hospital,4 31% in a large sexually transmitted infection (STI) Australian clinic,7 and 59% across four regions in China.8 Multiple disruptions were reported in Kenya, including less HIV clinic-based testing due to limited personal protective equipment and sanitization supplies, as well as reduced service hours,5 and suboptimal distribution of HIV self-testing kits despite increased demand.9 Simões et al.10 reported significant declines across Europe in the first six months of the pandemic, with HIV testing down >50% between March and May 2020 at most sites, but to a lesser degree between June and August 2020. In Japan, similar trends were observed.11 Interestingly, of the studies that also examined HIV diagnoses during the pandemic (i.e., HIV positivity rates), the data were mixed. For instance, the Belgian study showed a 75% reduction in diagnosed cases,4 whereas the Australian study showed no change.7 Overall, worldwide trends showed a decline in HIV testing, although these data were limited to the first 3-6 months of the pandemic, and positivity rates varied by site.
To our knowledge, only three studies examined HIV testing changes in the United States (U.S.). In a study of eight sexual health clinics in Arkansas, Missouri, and Oklahoma, HIV testing significantly decreased among men in the first four months of the pandemic.12 HIV positivity rates were not analyzed in this study. Data from Oregon showed similar trends over the first six months of the pandemic, although testing slightly rebounded after the initial 2, 3 pandemic months.13 During Oregon's stay-at-home order (March through May 2020), HIV diagnoses decreased by 36%, but this was not a statistically significant difference compared to periods before or after. A study of the first 5, 6 months of the pandemic revealed decreased HIV testing in emergency department (ED) sites in Illinois.14 This study also showed increased HIV positivity rates, relative to pre-pandemic years, perhaps because a higher proportion of tests were done in symptomatic (as compared to asymptomatic) individuals or that a higher proportion of tests were in high-risk asymptomatic individuals instead of low-risk individuals. These testing patterns are consistent with national testing data from commercial virology labs.15 However, more data are needed from the U.S.
In the U.S., it is recommended that all persons age 13 to 64 receive an HIV test at least once, with repeat testing at least annually for individuals at elevated risk. The majority of tests are performed in outpatient clinics but testing may also occur in hospitals, emergency departments, community-based organizations, mobile testing units, or other sites. Self-testing occurs but to our knowledge, is less common. Characterizing the impact of the COVID-19 pandemic on HIV testing rates will help guide public health outreach and resources to revive HIV prevention and testing efforts to address the HIV epidemic. State governments primarily led responses to COVID-19, which means that guidelines and restrictions varied by state and that a uniform national trend of the impact of COVID-19 in the U.S. might be unlikely. Additionally, in light of the multiple “waves” of COVID-19 in the U.S., longer-term pandemic data warrant analysis to determine how fluctuations in COVID-19 transmission, and subsequent changes in restrictions, impacted HIV testing. Examination of a longer time period would also allow for assessment of whether or not testing rates are rebounding. Lastly, further examination of HIV test positivity rates would help generate hypotheses about who might be seeking testing despite the pandemic.
As such, this study analyzed data from the start of the pandemic in March 2020 through December 2020, comparing results to data from a similar period in 2019 and the pre-pandemic phase of early 2020. Data were obtained from geographically diverse healthcare systems located in metropolitan areas of several U.S. regions, including New England, Pacific Northwest, Southeast, and Upper Midwest, to characterize regional differences and similarities. We hypothesized that overall outpatient HIV testing would be lower during the period from the onset of the pandemic through December 2020, compared to the same time period in 2019. However, the extent of these changes was largely unknown. We also explored how HIV positivity rates fluctuated during this period, relative to 2019, and hypothesized that positivity rates would be higher during the pandemic.
Methods
Data sources
De-identified data were collected from four large, geographically diverse, urban-based healthcare systems in the U.S.: the Rhode Island STI clinic, in Providence, RI; CrescentCare, in New Orleans, LA; Hennepin Healthcare, in Minneapolis, MN; and, University of Washington Healthcare System, in Seattle, WA. The Providence site is the major safety-net STI clinic serving the entire state. The site in New Orleans is a federally qualified health centre with no hospital affiliation but numerous community-based partners. In addition to outpatient clinic data, New Orleans also provided data from three community-based outreach sites that were able to remain operational as emergency sites during the 2020 shutdowns, compared to the 50 sites that they partnered with in 2019. The sites in Minneapolis and Seattle are large healthcare systems with multiple clinics that provide HIV testing and care. Emergency department (ED) data were available from these two healthcare systems. Obtained HIV testing data were from January 1, 2019 through December 31, 2020.
We obtained the number of COVID-19 cases (January 1, 2020–December 31, 2020) from the Department of Health at each state. All four states announced a stay-at-home order with varied starting and ending dates. Stay-at-home orders were in place for Louisiana from March 22, 2020 to May 15, 2020, Minnesota from March 27, 2020 to May 17, 2020, Rhode Island from March 28, 2020 to May, 9, 2020, and Washington from March 23, 2020 to June 1, 2020. All of these states entered an advisory phase after the stay-at-home order period (e.g. incremental openings, some restrictions on social activities, etc.) and maintained advisory phases through the end of 2020. HIV positive case data were censored from Minneapolis in weeks when there were <11 cases.
Procedures
We used de-identified data sets, pulled from electronic health record systems, and thus our study was determined to not be human subjects research by each site's institutional review board. In terms of HIV testing procedures, the Hennepin Healthcare (Minneapolis), the Rhode Island STI clinic (Providence), and University of Washington (Seattle) record systems were reviewed for all laboratory HIV Antigen/Antibody (“4th generation”) combination tests. CrescentCare (New Orleans) used a rapid testing algorithm across all testing programs.
Statistical analyses
We created graphs to present the rates of HIV testing and positivity, including possible changes, along with the number of COVID-19 cases in each state. The Kernel-weighted local polynomial smoothing method was used to generate smooth plots of the number of HIV testing over time. We used Poisson regression to explore the trend of HIV tests through phases of the COVID-19 pandemic, providing 95% confidence intervals. An alpha of 0.05 was used to indicate statistical significance. All analyses were performed in Stata 16.0.16
Role of the funding source
This study was funded by the National Institute of Mental Health (U.S.). The funders did not participate in the collection, analysis, and interpretation of data; in the writing of the report; or, in the decision to submit the paper for publication.
Results
HIV tests and HIV positivity rates at outpatient settings
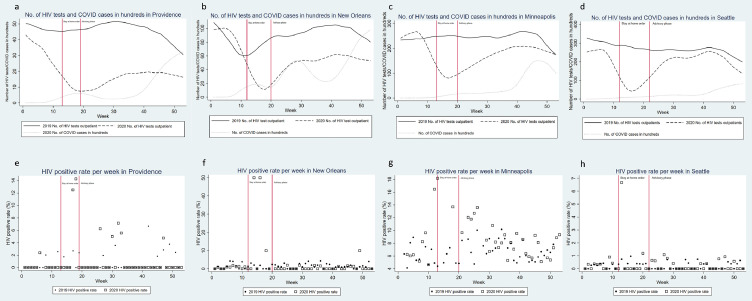
In 2019, 40,620 HIV tests were performed compared to 27,112 in 2020. The number of HIV tests per week at outpatient settings dropped significantly in 2020, compared to 2019 (Figure 1a–d). All states had a sharp decrease of HIV testing at outpatient settings during Weeks 9–19, 2020, while the COVID-19 pandemic was in an emerging phase in the U.S. An increasing trend of HIV tests was observed in all states after Week 19, 2020, when states lifted their stay-at-home orders. However, the number of HIV tests remained lower than in 2019. Overall, we observed a 27–59% [95%CI: 25%, 62%] reduction in the total number of HIV tests at outpatient settings in 2020 compared to 2019 in four large metropolitan areas (Table 1).
Figure 1.
HIV tests and HIV positive rates in outpatient settings. Figures 1(a)-1(d) show the number of HIV tests per week in 2019 and 2020. The numbers of COVID cases in 2020 are also presented in these figures. Figures 1(e)-1(h) indicate HIV positive rates per week in 2019 and 2020 in four states.
Table 1.
The total number of HIV tests and HIV positivity rate in four cities in 2019 and 2020.
| State | HIV tests |
Total No. of positive cases | Annual HIV positive rate |
||||
|---|---|---|---|---|---|---|---|
| Total No. | % reduction (95% confidence interval [CI])* | % | P-value⁎⁎ | ||||
| Providence, RI | |||||||
| Outpatient HIV tests | 0·65 | ||||||
| 2019 | 2441 | Ref | 16 | 0·66% | |||
| 2020 | 1005 | 59% (56–62%) | 8 | 0·80% | |||
| Minneapolis, MN | |||||||
| Outpatient HIV tests | 0·68 | ||||||
| 2019 | 12,836 | Ref | 750 | 5·84% | |||
| 2020 | 9314 | 27% (25–29%) | 569 | 6·11% | |||
| ED HIV tests | |||||||
| 2019 | 548 | Ref | . | . | |||
| 2020 | 477 | 13% (2–23%) | . | . | |||
| New Orleans, LA | |||||||
| Outpatient HIV tests | 0·01 | ||||||
| 2019 | 4718 | Ref | 63 | 1·34% | |||
| 2020 | 2900 | 39% (36–41%) | 21 | 0·72% | |||
| Community HIV tests | 0·008 | ||||||
| 2019 | 2471 | Ref | 16 | 0·65% | |||
| 2020 | 858 | 65% (62–68%) | 14 | 1·63% | |||
| Seattle, WA | |||||||
| Outpatient HIV tests | 0·58 | ||||||
| 2019 | 14286 | Ref | 30 | 0·21% | |||
| 2020 | 9819 | 31% (30–33%) | 24 | 0·24% | |||
| ED HIV tests | 0·89 | ||||||
| 2019 | 3320 | Ref | 29 | 0·87% | |||
| 2020 | 2739 | 17% (13–22%) | 23 | 0·84% | |||
Note: ED=Emergency Department.
*Results from Poisson regressions.
**P-values were calculated by Chi-square tests.
Figure 1e–h present HIV positivity rates per week at outpatient settings in 2019 and 2020 in four cities. These scatter plots show HIV positivity rates were higher before or around the end of stay-at-home orders in each state in 2020 and then show a flattened trend. Although the total number of HIV tests decreased in all cities, HIV positivity rates increased at outpatient settings in most areas, except New Orleans (Table 1). Despite these trends, differences were not statistically significant, except in New Orleans.
HIV tests and HIV positivity rates at community-based sites and emergency departments
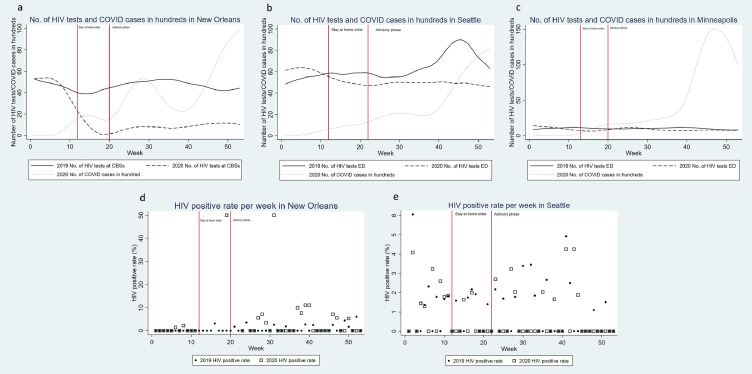
Figure 2a–c present the number of HIV tests per week in our Minneapolis site's ED, Seattle's ED, and New Orleans's community sites. At the community sites in New Orleans, we again observed a sharp decrease in the number of HIV tests starting at the time of the stay-at-home order in 2020. Since the lift of the stay-at-home order, the number of HIV tests at community sites in New Orleans was maintained at a low level. Overall, there was a 65% [95%CI: 62%, 68%] reduction in the total number of HIV tests at community sites in 2020 compared to 2019 in New Orleans (Table 1). Although the number of HIV tests dropped significantly at the community testing sites in New Orleans, HIV positivity rates were higher in 2020 than 2019 (1·63% vs. 0·65%), representing a statistically significant difference (p = 0·008). There was only a slight reduction in the total number of HIV tests in EDs in Minneapolis (13% [95%CI: 2%, 23%] reduction) and Seattle (17% [95%CI: 13%, 22%] reduction). In Seattle, the ED HIV positivity rate in 2020 was slightly lower than in 2019 (0·84% vs. 0·87%) and this difference was not statistically significant.
Figure 2.
HIV tests and HIV positive rates in community-based sites (CBS) or Emergency Departments (ED). Figures 2(a)-2(c) show the number of HIV tests in 2019 and 2020 at either CBS or ED in four states. Figures 2(d) and 2(e) show HIV positive rates in 2019 and 2020. Most weeks the Minneapolis ED had fewer than 11 positive cases, thus the data were censored in accordance with Hennepin Healthcare's privacy policies.
The number of HIV tests during different phases of COVID in 2020
In Poisson regression models, we found a 68-97% [95%CI: 65%, 98%] reduction in the number of HIV tests peer week during the stay-at-home order period compared to during the pre-stay-at-home order at outpatient settings in early 2020 in the four cities (Table 2). When states moved to advisory phases (i.e., lifting of some restrictions), the number of HIV tests remained 11–54% [95%CI: 7%, 59%] lower at outpatient settings compared to pre-stay-at-home orders.
Table 2.
HIV test reductions during COVID-19 restriction phases in four cities in 2020.
| State | % reduction (95% confidence interval [CI])* of No. of HIV tests |
|---|---|
| Providence, RI | |
| Outpatient HIV tests | |
| Pre-stay-at-home order | Ref |
| During state-at-home order | 76% (66–82%) |
| During the advisory phase | 54% (47–59%) |
| Minneapolis, MN | |
| Outpatient HIV tests | |
| Pre-stay-at-home order | Ref |
| During state-at-home order | 68% (65–71%) |
| During the advisory phase | 28% (24–31%) |
| ED HIV tests | |
| Pre-stay-at-home order | Ref |
| During state-at-home order | 58% (40–70%) |
| During the advisory phase | 25% (9–39%) |
| New Orleans, LA | |
| Outpatient HIV tests | |
| Pre-stay-at-home order | Ref |
| During state-at-home order | 97% (96–98%) |
| During the advisory phase | 42% (38%, 47%) |
| Community HIV tests | |
| Pre-stay-at-home order | Ref |
| During state-at-home order | 99% (98–99%) |
| During the advisory phase | 83% (80–85%) |
| Seattle, WA | |
| Outpatient HIV tests | |
| Pre-stay-at-home order | Ref |
| During state-at-home order | 78% (76–80%) |
| During the advisory phase | 11% (7–15%) |
| ED HIV tests | |
| Pre-stay-at-home order | Ref |
| During state-at-home order | 19% (9–28%) |
| During the advisory phase | 20% (13–27%) |
Note: ED=Emergency Department.
Results from Poisson regressions.
At the community testing sites in New Orleans, the number of HIV tests dropped by 99% [95%CI: 98%, 99%] during the stay-at-home order (Table 2). Even during the advisory phase, emergency outreach community sites provided limited numbers of HIV tests per week. In the Seattle ED, we observed a similar reduction in the number of HIV tests during the stay-at-home order period (19%; [95%CI: 9%, 28%] reduction) and the advisory phase (20%; [95%CI: 13%, 27%] reduction) when compared to the pre-stay-at-home order period in early 2020. In Minneapolis, the number of ED HIV tests dropped 58% [95%CI: 40%, 70%] and 25% [95%CI: 9%, 39%] during the stay-at-home order and the advisory phase, respectively.
Discussion
This is among the first studies to evaluate the impact of the COVID-19 pandemic on HIV testing rates in the U.S. As a result of pandemic restrictions, HIV prevention services, such as in-person HIV testing, were disrupted across the U.S. HIV testing is a critical component of effective HIV prevention and is performed at many community-based clinics, often at no charge, to facilitate diagnosis and timely treatment. As hypothesized, results from four geographically diverse U.S. sites, including two Ending the HIV Epidemic (EHE) priority jurisdictions (New Orleans and Seattle), showed overall decreases in HIV outpatient testing relative to a similar period of time pre-pandemic. Not surprisingly, outpatient HIV testing was at its lowest point during each state's stay-at-home order. Testing since lifting of stay-at-home orders through the end of 2020 showed a rebound at all locations. However, testing rates did not fully return to pre-pandemic levels in the period analyzed here. Although Washington was the state of the first known COVID-19 case in the U.S. and “waves” of infection varied across areas included here, the data show a somewhat consistent pattern in terms of testing changes. These data present a concerning picture of suppressed HIV outpatient testing, specifically in urban centres where individuals at risk for HIV infection might cluster.
Interestingly, data from emergency departments (Minneapolis and Seattle) show only slight reductions in testing rates pre- vs. during the COVID-19 pandemic. Neither site offers universal, opt-out HIV testing. However, HIV testing performed in EDs, such as those included here, may be risk factor or symptom driven. Rates of testing that are risk factor driven are likely to follow emergency room volume rates overall, and may account for modest fluctuations in HIV testing in this context. Additionally, there are overlapping symptoms of acute HIV and COVID-19, which could lead to more symptomatic screening in persons presenting to the ED with a viral illness. It might also be possible that individuals who were symptomatic with undetected, and therefore, untreated, HIV could also have been at increased risk for symptoms requiring emergency care. In fact, data collected during the pandemic show that patients with HIV might be more likely to initiate care in an ED setting, compared to outpatient or telehealth settings.17 To our knowledge, most EDs remained opened during the pandemic. This might have steered people towards seeking testing at the ED because they had no outpatient clinic option. Moreover, individuals seeking care for COVID-19 might have been tested for HIV as there are shared social determinants of health that correlate with risk of infection for both diseases.
In addition to examining HIV testing rates, we also assessed HIV positivity rates in our four healthcare systems. Overall trends show increased positivity rates during the pandemic, although differences were not statistically significant, so further evaluations in other regions would be useful to confirm these patterns. The trend towards higher positivity rate in our data might represent a selection bias as those seeking testing might be more likely to be symptomatic. Also, this might be driven by an individual's assessment of their HIV risk prior to COVID-19. People who perceived themselves to have recently been at high risk for HIV pre-COVID-19 might have self-selected to seek out testing despite the pandemic. Overall, U.S. governmental data18 show a downward trend in HIV diagnoses through 2020 in the geographic areas assessed here, suggesting that the trends are real. However, additional studies are needed to determine if these trends represent actual decreases in transmissions or are better explained by reduced testing and greater proportion of undiagnosed infections.
Accumulating data are mixed in terms of possible changes to HIV transmission risk behaviors during the pandemic. Men-who-have-sex-with men (MSM), who account for at least 66% of HIV incidence in the U.S.,19 reported concerns about being able to access testing, particularly in the context of other life challenges, including COVID-19’s impact on economic stability and mental health.20,21 However, in Sanchez and colleagues’ study,20 nearly half of MSM surveyed reported no change in their sexual activity or use of dating or “hook-up” apps during the pandemic. In a study from the United Kingdom, the vast majority of community-based MSM reported being sexually active outside their household (76%), although a similar proportion reported having less partners than pre-pandemic.22 In the Netherlands, 73% of MSM in a cohort study reported a decrease in casual sex partners during the COVID-19 pandemic.23 In contrast, data from the U.S. show that despite early trends of fewer risky sexual behaviors in the early stages of the pandemic, by April 2020, MSM reported increasing their sexual risk behaviors.24 In sum, these data are mixed, with no compelling reason to conclude that risky sexual behaviors associated with HIV infection substantially changed during the pandemic.
Among persons who use drugs, U.S. data do show some stability or improvement in HIV testing during the COVID-19 pandemic, particularly in hospitals. This is important as individuals who use injection drugs may be disproportionately affected by the COVID-19 and HIV epidemic. Individuals on methadone maintenance reported no change in or access to testing.25 Also, an increase in HIV testing was found among hospitalized individuals who use drugs.26 However, these are unique populations accessing treatment in specialized settings. For broader, community-based testing, the accumulating data show a downward trend in HIV testing.
Another factor related to reduced testing might be the reduced use of pre-exposure prophylaxis (PrEP) in some communities.18,27 Individuals taking PrEP are encouraged to be tested for HIV every three months. Data show that PrEP usage during the pandemic has decreased, likely leading to less in-clinic PrEP follow-up visits. For example, in Australia, over 40% of MSM who were previously on PrEP decided to discontinue use and they were subsequently less likely to seek HIV testing.28
In light of these results and this trend reported elsewhere, at-home HIV self-testing is receiving increased attention. Warmbrunn et al.29 highlight the importance of elevating at-home testing from an alternative testing option to a primary modality during the pandemic. Indeed, efforts are underway to amplify the reach of at-home self-testing. For example, in Brazil, among a large sample of MSM and transgender/non-binary individuals, most participants reported preferring at-home HIV testing to in-clinic, and 79% of individuals who had never completed an at-home test reported willingness to self-test.30
Limitations
This study has limitations. First, data were not complete for all sites, as HIV positivity rates were censored from Minneapolis if weekly cases were <11. However, we believe overall trends are captured in the data analyzed here. Second, because of the diversity of sites, we were unable to account for potential confounding variables, such as differences in clinic hours or availability of state resources for testing. Third, because the data were stripped of demographic information, we were unable to examine potential subgroup differences, such as those related to age, ethnicity, race, or PrEP use. Future studies will benefit from a more fine-grained analysis of who might have been disproportionately impacted during the pandemic. Fourth, these analyses did not account for at-home (i.e., self) HIV testing. Lastly, although these data came from large, urban settings and the largest metropolitan populations in their respective states, these data do not reflect statewide trends. While COVID-19 was ubiquitous, results from this study of four geographically diverse healthcare systems should be cautiously extrapolated to other geographically diverse sites.
Conclusions
To our knowledge, this study represents the largest and longest assessment of pandemic-related changes in HIV testing in the U.S. Although the data are mixed, it is highly likely that HIV continues to spread in communities. Pre-pandemic, 13% of people with HIV in the U.S. were undiagnosed19 and data showed that individuals who were unaware of their diagnosis accounted for approximately 40% of new HIV infections.31 As noted by Mitchell and colleagues,32 despite the possible fluctuations in HIV transmission due to reduced interpersonal contact and engagement in HIV risk related behaviors during the COVID-19 pandemic, the overall impact of reduced testing could lead to delayed antiretroviral treatment initiation, poor viral suppression, increased transmission risk, and ultimately, increased HIV-related deaths. As the pandemic resolves and restrictions ease, the healthcare industry should scale up testing, messaging to publicize the importance of testing, and routine HIV screening.
Declaration of interests
All authors declare no competing interests.
Acknowledgments
Contributors
E.M. and J.T. led the conception and design of the study. J.O., R.D.S., B.R.W., A.M.B., and A.L. identified, gathered, and interpreted the data sources to inform the analyses. E.M. and J.T. verified the underlying data. J.T. conducted the analyses and generated the figures and tables. J.V.B. and P.A.C. provided advice on situating results in the extant literature. All authors contributed to interpreting the results. E.M. wrote the first draft of the manuscript. All authors contributed to manuscript revision and critical review. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Data sharing
De-identified data from this study will be made available upon request, pending approval by the authors and their local institutions.
Acknowledgments
This study was funded by the National Institute of Mental Health (U.S.) by grants awarded to E.M. (R01 MH119919) and J.T. (K01 MH119960). P.A.C. is a co-investigator on R01 MH119919. We thank Kristine F. Lan, MSc, Harborview Medical Center, Seattle, WA, for assistance with data extraction.
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a Pandemic. Acta Bio Med Atenei Parm. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haleem A., Javaid M., Vaishya R. Effects of COVID-19 pandemic in daily life. Curr Med Res Pract. 2020;10(2):78–79. doi: 10.1016/j.cmrp.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shoptaw S., Goodman-Meza D., Landovitz RJ. Collective call to action for HIV/AIDS community-based collaborative science in the era of COVID-19. AIDS Behav. 2020;24(7):2013–2016. doi: 10.1007/s10461-020-02860-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Darcis G., Vaira D., Moutschen M. Impact of coronavirus pandemic and containment measures on HIV diagnosis. Epidemiol Infect. 2020;148:e185. doi: 10.1017/S0950268820001867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lagat H., Sharma M., Kariithi E., et al. Impact of the COVID-19 pandemic on HIV testing and assisted partner notification services, Western Kenya. AIDS Behav. 2020;24(11):3010–3013. doi: 10.1007/s10461-020-02938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen M.S., Chen Y.Q., McCauley M., et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–839. doi: 10.1056/NEJMoa1600693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chow E.P.F., Ong J.J., Denham I., Fairley CK. HIV testing and diagnoses during the COVID-19 pandemic in Melbourne, Australia. J Acquir Immune Defic Syndr. 2021;86(4):e114–e115. doi: 10.1097/QAI.0000000000002604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Booton R.D., Fu G., MacGregor L., et al. The impact of disruptions due to COVID-19 on HIV transmission and control among men who have sex with men in China. J Int AIDS Soc. 2021 doi: 10.1002/jia2.25697. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Odinga M.M., Kuria S., Muindi O., et al. HIV testing amid COVID-19: community efforts to reach men who have sex with men in three Kenyan counties. Gates Open Res. 2020;4:117. doi: 10.12688/gatesopenres.13152.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simões D., Stengaard A.R., Combs L., Raben D., ECIACo P. Impact of the COVID-19 pandemic on testing services for HIV, viral hepatitis and sexually transmitted infections in the WHO European Region, March to August 2020. Eurosurveillance. 2020;25(47) doi: 10.2807/1560-7917.ES.2020.25.47.2001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ejima K., Koizumi Y., Yamamoto N., et al. HIV testing by public health centers and municipalities and new HIV cases during the COVID-19 pandemic in Japan. J Acquir Immune Defic Syndr. 2021 doi: 10.1097/QAI.0000000000002660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hill B.J., Anderson B., Lock L. COVID-19 pandemic, pre-exposure prophylaxis (PrEP) care, and HIV/STI testing among patients receiving care in three HIV epidemic priority states. Aids Behav. 2021 doi: 10.1007/s10461-021-03195-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menza T.W., Zlot A.I., Garai J., Humphrey S., Ferrer J. The impact of the SARS-CoV-2 pandemic on human immunodeficiency virus and bacterial sexually transmitted infection testing and diagnosis in oregon. Sex Transm Dis. 2021;48(5):e59–e63. doi: 10.1097/OLQ.0000000000001385. [DOI] [PubMed] [Google Scholar]
- 14.Stanford K.A., McNulty M.C., Schmitt J.R., et al. Incorporating HIV screening with COVID-19 testing in an urban emergency department during the pandemic. JAMA Intern Med. 2021 doi: 10.1001/jamainternmed.2021.0839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delaney KP. Impact of COVID-19 on commercial laboratory testing for HIV in the United States. Virtual CROI; 2021.
- 16.StataCorp LLC; College Station, TX: 2019. Stata Statistical Software [computer program] [Google Scholar]
- 17.Khazanchi R., Winkelman T.N.A., Pandita D., Jelinek R., Shearer R.D., Bodurtha P.J. Patient characteristics and subsequent health care use by location of SARS-CoV-2 testing initiation in a safety-net health system. Jama Netw Open. 2021;4(6) doi: 10.1001/jamanetworkopen.2021.12857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Services USHaH. America's HIV epidemic analysis dashboard (AHEAD). https://ahead.hiv.gov. Published 2019. Accessed.
- 19.Vol. 2021. CDC; 2019. p. 32. (Diagnoses of HIV Infection in the United States and Dependent Areas). HIV Surveillance Report. [Google Scholar]
- 20.Sanchez T.H., Zlotorzynska M., Rai M., Baral SD. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. Aids Behav. 2020;24(7):2024–2032. doi: 10.1007/s10461-020-02894-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santos G.M., Ackerman B., Rao A., et al. Economic, mental health, HIV prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of cisgender gay men and other men who have sex with men. AIDS Behav. 2021;25(2):311–321. doi: 10.1007/s10461-020-02969-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hyndman I., Nugent D., Whitlock G.G., McOwan A., Girometti N. COVID-19 restrictions and changing sexual behaviours in HIV-negative MSM at high risk of HIV infection in London, UK. Sex Transm Infect. 2021 doi: 10.1136/sextrans-2020-054768. in press. [DOI] [PubMed] [Google Scholar]
- 23.van Bilsen W.P.H., Zimmermann H.M.L., Boyd A., et al. Sexual behavior and its determinants during COVID-19 restrictions among men who have sex with men in Amsterdam. J Acquir Immun Def Synd. 2021;86(3):288–296. doi: 10.1097/QAI.0000000000002581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pampati S., Emrick K., Siegler A.J., Jones J. Changes in sexual behavior, PrEP adherence, and access to sexual health services due to the COVID-19 pandemic among a cohort of PrEP-using MSM in the South. Jaids-J Acquir Immune Defic. 2021 doi: 10.1097/QAI.0000000000002640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mistler C.B., Curley C.M., Rosen A.O., et al. The impact of COVID-19 on access to HIV prevention services among opioid-dependent individuals. J Commun Health. 2021 doi: 10.1007/s10900-021-00979-0. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zubiago J., Murphy M., Guardado R., Daudelin D., Patil D., Wurcel A. Increased HIV testing in people who use drugs hospitalized in the first wave of the COVID-19 pandemic. J Subst Abuse Treat. 2021 doi: 10.1016/j.jsat.2020.108266. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krakower D., Solleveld P., Levine K., Mayer K. Proceedings of the 23rd International AIDS Conference. 2020. Impact of COVID-19 on HIV preexposure prophylaxis care at a Boston community health center. Virtual. [Google Scholar]
- 28.Hammoud M.A., Grulich A., Holt M., et al. Substantial decline in use of HIV preexposure prophylaxis following introduction of COVID-19 physical distancing restrictions in Australia: results from a prospective observational study of gay and bisexual men. Jaids J Acquir Immune Defic. 2021;86(1):22–30. doi: 10.1097/QAI.0000000000002514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Warmbrunn I., Green-Jones M., Outlaw AY. Utilizing alternative testing technology for human immunodeficiency virus (HIV) in the COVID era. Curr Emerg Hosp Med Rep. 2021:1–7. doi: 10.1007/s40138-021-00228-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoagland B., Torres T.S., Bezerra D.R.B., et al. High acceptability of PrEP teleconsultation and HIV self-testing among PrEP users during the COVID-19 pandemic in Brazil. Braz J Infect Dis. 2021;25(1) doi: 10.1016/j.bjid.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dailey A.F., Hoots B.E., Hall H.I., et al. Vital Signs: human immunodeficiency virus testing and diagnosis delays — United States. MMWR Morb Mortal Wkly Rep. 2017;66:1300–1306. doi: 10.15585/mmwr.mm6647e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mitchell K.M., Dimitrov D., Silhol R., et al. The potential effect of COVID-19-related disruptions on HIV incidence and HIV-related mortality among men who have sex with men in the USA: a modelling study. Lancet HIV. 2021 doi: 10.1016/S2352-3018(21)00022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]