Introduction
During catheter ablation for Wolff-Parkinson-White (WPW) syndrome, an accessory pathway potential (APP) is sometimes observed at the optimal ablation site. Herein, we describe a case in which an APP remained after right-sided anteroseptal accessory pathway (AP) ablation. Moreover, selective block of the ventricular end (AP-ventricle junction) of the AP was confirmed by parahisian pacing (PHP).
Case report
The patient was a 59-year-old Japanese man without any medical history except for experiencing palpitations since his adolescence. He was diagnosed with WPW syndrome on a 12-lead electrocardiogram (ECG). Although he had undergone catheter ablation at another hospital 9 years ago, the procedure was unsuccessful. His symptoms were refractory to antiarrhythmic drugs. Thereafter, he was referred to our center for repeat ablation. Physical examination and blood tests revealed no abnormal findings. A 12-lead ECG showed a negative delta wave in lead V1, which was considered to be a septal AP. ECG at the time of tachycardia showed 151/min of narrow QRS-complex tachycardia. Echocardiography showed no abnormal findings.
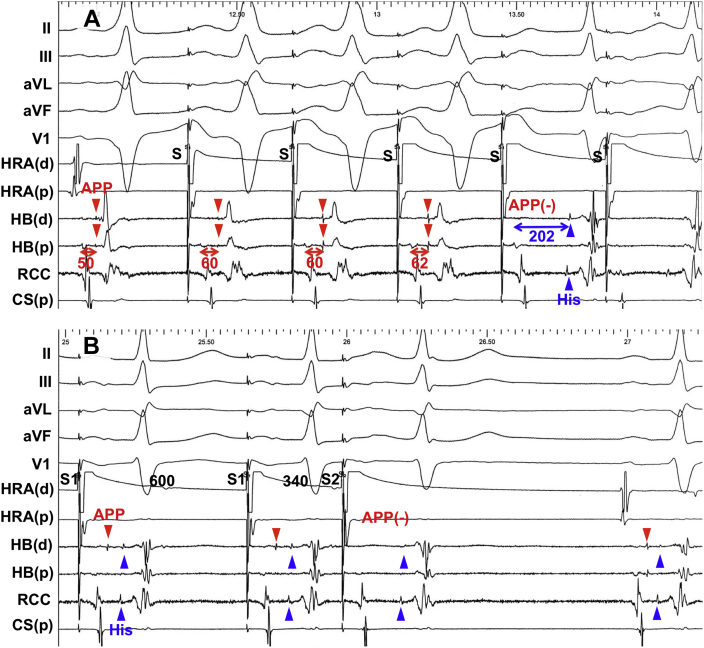
An electrophysiological study was performed after obtaining written informed consent. Multipolar electrode catheters were placed in the high right atrium, His bundle (HB), tricuspid valve annulus, coronary sinus, right coronary cusp, and right ventricle apex. The AH and HV interval time during sinus rhythm were 75 and -3 ms, respectively. APP and His deflection were simultaneously recorded in the HB electrode. PHP revealed constant ventriculoatrial conduction interval regardless of His capture. Continuous atrial pacing revealed constant A-APP interval and manifestation of preexcitation; then, the clinical tachycardia was induced, following the loss of APP and preexcitation (Figure 1A). APP was observed just after the V wave on the HB electrode during tachycardia. A single ventricular extrastimulus during HB refractoriness could reset tachycardia. Atrial activation sequence during tachycardia was consistent with that in ventricular pacing during sinus rhythm. Based on these findings, the tachycardia was diagnosed as orthodromic reentrant tachycardia through septal AP.
Figure 1.
Atrial pacing before and after ablation. A: Accessory pathway potential (APP) and His deflection are indicated as red and blue arrows, respectively. Continuous atrial pacing shows constant A-APP interval with manifestation of preexcitation and induced clinical tachycardia with loss of APP. B: Remaining potentials after ablation are verified by atrial extrastimulation. This shows disappearance of potentials indicated by the red arrow and decremental conduction of potentials indicated by the blue arrow. This finding can confirm that the potential indicated by the red arrow is APP, and the potential indicated by the blue arrow is His deflection. CS = coronary sinus; d = distal; HB = His bundle; HRA = high right atrium; p = proximal; RCC = right coronary cusp; S = stimulus.
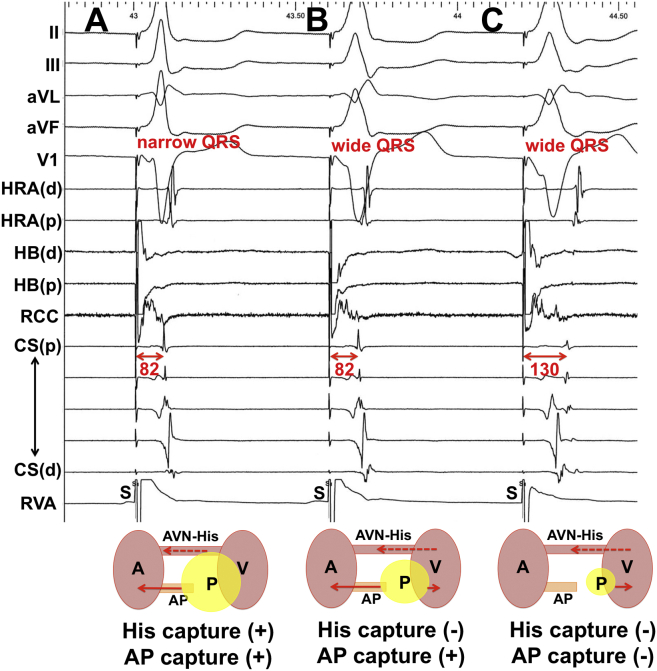
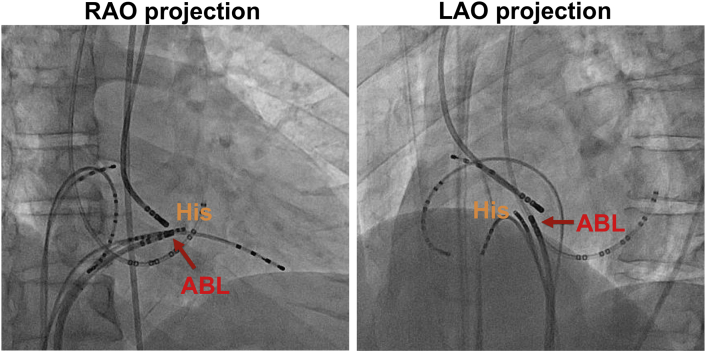
APP was mapped with an ablation catheter during sinus rhythm at the right septum. In addition, radiofrequency application was started at low energy (20 W) at the ventricular side of the AP to reduce the risk of atrioventricular node (AVN) injury. Thereafter, the delta wave on the surface ECG and APP on the ablation catheter disappeared in 2.5 seconds after ablation (the catheter position is shown in Supplemental Figure 1). However, the APP on the HB electrode remained even after the delta wave disappeared (Figure 2 and Figure 1B). Ventricular pacing revealed the disappearance of retrograde AP conduction and remaining retrograde AVN conduction. When PHP was performed, high-output pacing showed HB capture (narrow QRS), and the time interval from stimulus to atrial electrogram (stim-A) was 82 ms (Figure 3A). The lower-output pacing did not result in HB capture and resulted in wide QRS morphology. However, stim-A was consistent with that during high-output pacing, suggesting that the distal end of the remaining AP was selectively captured (Figure 3B). More lower-output pacing resulted in the capture of ventricular muscle alone and stim-A was prolonged (noncapture of AP). The differences of retrograde atrial activation sequences in Figure 3B and 3C revealed the existence of 2 different ventriculoatrial conductions: via the AVN and the remaining proximal fiber of the AP. These findings could explain the selective AP–ventricle junction ablation. Orthodromic reentrant tachycardia was never inducible by any pacing maneuver or provocation tests. The patient’s symptoms and the delta wave on ECG have not recurred in the 10 years since catheter ablation.
Figure 2.
Intracardiac electrograms during accessory pathway ablation. Both accessory pathway potential (APP) on ablation catheter and the delta wave on the surface electrocardiogram disappear after catheter ablation. However, APP remains on the other electrode (red arrow). The small potential (His deflection) can be clearly confirmed on the electrodes of the ablation catheter, His bundle (HB), and right coronary cusp (RCC) after ablation (blue arrow). ABL = ablation catheter; CS = coronary sinus; d = distal; HRA = high right atrium; p = proximal.
Figure 3.
Parahisian pacing after accessory pathway (AP) ablation. A: High-output pacing with both His and AP capture reveals retrograde AP and atrioventricular node (AVN) conduction. B: Lower-output pacing with AP capture alone reveals retrograde AP conduction. C: However, more lower-output pacing without His or AP capture reveals no retrograde AP conduction (retrograde AVN conduction alone). The differences of retrograde atrial activation patterns in (b) and (c) proves the existence of 2 retrograde conductions via the AVN and the remaining proximal fiber of AP. A = atrium; ABL = ablation catheter; APP = accessory pathway potential; CS = coronary sinus; d = distal; HB = His bundle; HRA = high right atrium; P = pacing; p = proximal; RCC = right coronary cusp; V = ventricle.
Discussion
In this case, antegrade and retrograde AP conduction was eliminated by catheter ablation, regardless of the existence of residual APP. In addition, PHP revealed that the distal side of the AP could be selectively ablated. To the best of our knowledge, there have been no similar clinical reports.
Jackman and colleagues1 reported the effectiveness of catheter ablation for WPW syndrome, and the APP recording site has been used as one of the indices for the optimal ablation site.1, 2, 3, 4 APP was first reported in 1983,5 and its electrophysiological properties have since been validated. Antegrade AP conduction block occurs more often under atrial pacing or antiarrhythmic drug administration at the AP-ventricle junction than at the atrium-AP junction or intra-AP site. This characteristic can explain the concealment of WPW syndrome.6, 7, 8 The hypothesis to explain this specific block site is that small current through the AP (with small myocardial mass) might be fractionated and dispersed throughout the ventricular muscle (with large myocardial mass). Therefore, this current becomes insufficient to activate each ventricular myocardium (called “impedance mismatch”).9,10 The present case is rare owing to the presence of a local conduction block within the AP at the ventricular end by catheter ablation. In general, APP elimination is not used as an endpoint of AP ablation. In this case, excessive application to eliminate APP may pose a risk of AVN injury. Thus, it is important to confirm AP conduction block even if APP remains after ablation.
Conclusion
We encountered a case in which APP remained after right anteroseptal AP ablation. Moreover, successful selective ventricular end of AP (AP-ventricle junction) ablation could be confirmed by PHP.
Key Teaching Points.
-
•
Residual accessory pathway potential (APP) after catheter ablation may be acceptable, if antegrade and retrograde conduction block through accessory pathway (AP) can be verified.
-
•
Originally AP tends to be blocked at the ventricular end, and it explains the concealment of Wolff-Parkinson-White syndrome.
-
•
Parahisian pacing may be useful to evaluate the conduction property of the septal AP, regardless of residual APP.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
Funding Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.hrcr.2021.09.004.
Appendix. Supplementary data
Supplemental Figure 1.
Catheter position during ablation. ABL = ablation catheter; LAO = left anterior oblique; RAO = right anterior oblique.
References
- 1.Jackman W.M., Wang X.Z., Friday K.J., et al. Catheter ablation of accessory atrioventricular pathways (Wolff-Parkinson-White syndrome) by radiofrequency current. N Engl J Med. 1991;324:1605–1611. doi: 10.1056/NEJM199106063242301. [DOI] [PubMed] [Google Scholar]
- 2.Otomo K., Gonzalez M.D., Beckman K.J., et al. Reversing the direction of paced ventricular and atrial wavefronts reveals an oblique course in accessory AV pathways and improves localization for catheter ablation. Circulation. 2001;104:550–556. doi: 10.1161/hc3001.093499. [DOI] [PubMed] [Google Scholar]
- 3.Calkins H., Kim Y.N., Schmaltz S., et al. Electrogram criteria for identification of appropriate target sites for radiofrequency catheter ablation of accessory atrioventricular connections. Circulation. 1992;85:565–573. doi: 10.1161/01.cir.85.2.565. [DOI] [PubMed] [Google Scholar]
- 4.Silka M.J., Kron J., Halperin B.D., et al. Analysis of local electrogram characteristics correlated with successful radiofrequency catheter ablation of accessory atrioventricular pathways. Pacing Clin Electrophysiol. 1992;15:1000–1007. doi: 10.1111/j.1540-8159.1992.tb03093.x. [DOI] [PubMed] [Google Scholar]
- 5.Prystowsky E.N., Browne K.F., Zipes D.P. Intracardiac recording by catheter electrode of accessory pathway depolarization. J Am Coll Cardiol. 1983;1:468–470. doi: 10.1016/s0735-1097(83)80074-6. [DOI] [PubMed] [Google Scholar]
- 6.Kuck K.H., Friday K.J., Kunze K.P., Schlüter M., Lazzara R., Jackman W.M. Sites of conduction block in accessory atrioventricular pathways. Basis for concealed accessory pathways. Circulation. 1990;82:407–417. doi: 10.1161/01.cir.82.2.407. [DOI] [PubMed] [Google Scholar]
- 7.Jackman W.M., Friday K.J., Scherlag B.J., et al. Direct endocardial recording from an accessory atrioventricular pathway: localization of the site of block, effect of antiarrhythmic drugs, and attempt at nonsurgical ablation. Circulation. 1983;68:906–916. doi: 10.1161/01.cir.68.5.906. [DOI] [PubMed] [Google Scholar]
- 8.Winters S.L., Gomes J.A. Intracardiac electrode catheter recordings of atrioventricular bypass tracts in Wolff-Parkinson-White syndrome: techniques, electrophysiologic characteristics and demonstration of concealed and decremental propagation. J Am Coll Cardiol. 1986;7:1392–1403. doi: 10.1016/s0735-1097(86)80162-0. [DOI] [PubMed] [Google Scholar]
- 9.De la Fuente D., Sasyniuk B., Moe G.K. Conduction through a narrow isthmus in isolated canine atrial tissue. A model of the W-P-W syndrome. Circulation. 1971;44:803–809. doi: 10.1161/01.cir.44.5.803. [DOI] [PubMed] [Google Scholar]
- 10.Inoue H., Zipes D.P. Conduction over an isthmus of atrial myocardium in vivo: a possible model of Wolff-Parkinson-White syndrome. Circulation. 1987;76:637–647. doi: 10.1161/01.cir.76.3.637. [DOI] [PubMed] [Google Scholar]