Dear Editor,
Most of the infected patients completely recovered after COVID-19 infection. However, a substantial proportion of patients who have been infected with SARS-CoV-2 continue to have symptoms long past the time that they recovered from the initial phases of COVID-19 disease. Clinicians worldwide called these long-term effects of COVID-19 as “Long-Haul COVID-19”.1 The knowledge about long COVID-19 is evolving day by day. Multiple articles published in the Journal of Infection discussed the persistent symptoms, quality of life, and functional status post recovery.2, 3, 4 Long COVID symptoms were reported in 12 countries and none were from LMIC.5 The proportion of the Indian Population who have been experiencing the symptoms following the recovery is unknown. Understanding the burden of post COVID-19 symptoms is vital in planning the health systems for essential Post COVID care. We rapidly assessed the burden of persistent post COVID-19 symptoms and functional status after 12-14 weeks among those recovered from COVID-19 in Chennai, Tamil Nadu, India.
We obtained the line list of COVID-19 positive cases between February 25 and March 09, 2021, from the COVID-19 surveillance unit of Chennai, India. During the period, RT-PCR was the only method of testing and having any of the comorbidity or requiring oxygen therapy were the criteria for hospitalization. We defined persistent Post COVID-19 symptoms as clinical symptoms that develop during or after an infection consistent with COVID-19, persistent for more than 12 weeks and are not attributable to alternative clinical diagnoses.1 The assessment was done during June 11-20, 2021. A team of doctors tele-consulted all these COVID-19 case-patients aged >18 years during the 12-14 post recovery period of COVID-19. The team collected data on persistent symptoms and ruled out the possible differential diagnosis based on the reported symptoms. They also evaluated the functional status of activities of daily living using post COVID-19 functional scale (PCFS).6 The PCFS was evaluated between the time of the interview and the pre-COVID-19 diagnosis. The team graded the persistent breathlessness reported by the participants using modified Medical Research Council (mMRC) dyspnoea scale.7 Mean, Standard deviation (SD), and proportions were calculated as appropriate. We estimated odds ratio (OR) with 95% confidence interval (95% CI) for the association between hospitalization, persistent symptoms and functional limitations. We computed the adjusted OR (aOR) with 95% CI using multiple logistic regression after adjusting for age, gender, having any comorbidity, and hospitalisation. P value <0.05 was considered as statistically significant.
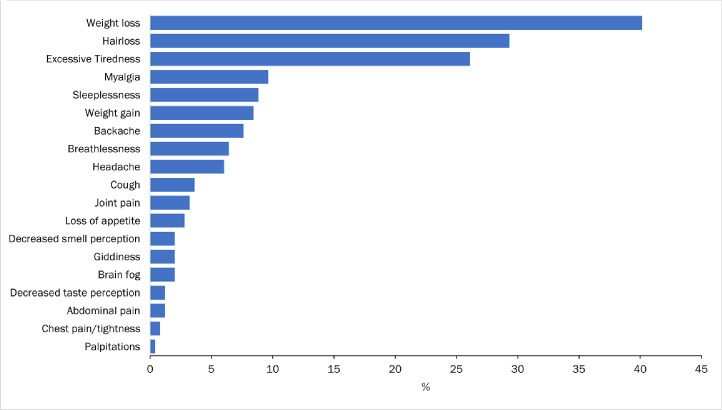
We contacted all the 1241 case-patients who were found positive for COVID-19 between February 25, 2021, and March 09, 2021. Of the 1241, 1001 (81%) responded. The mean age (SD) of the case-patients was 46.9 (16.1) years and 596 (60%) were females, 341 (34%) had at least one of the comorbidities. Eight-hundred and fifty-two (85%) of the case-patients experienced symptoms during active phase of COVID-19, 482 (48%) were hospitalised. All the 482 who were hospitalised either had a comorbidity or required oxygen therapy. Among the hospitalised, 137 (28%) required oxygen support. Almost one in four (24%) reported at least one of the symptoms as persistent (Figure 1 ). Among the 249 who reported symptoms post recovery, 136 (55%) were males. Persistent symptoms were higher among the age group 45-59 years (40%), followed by 30-44 years (24%). Four percent of those who remained asymptomatic during the active phase of infection also reported symptoms. Weight loss (40%), Hair loss (29%), Fatigue/Tiredness (26%), myalgia (10%), and sleeplessness (9%) were the most common reported symptoms (Figure 1). Of the 1001 case-patients, sixteen reported persistent breathlessness and none had dyspnoea more than grade 3 of mMRC dyspnoea scale.
Figure 1.
Persistent post COVID-19 symptom reported by those recovered after 12-14 weeks, Chennai, Tamil Nadu, India, 2021 (n=249).
Based on PCFS scale, 868 (87%) participants did not report any functional limitations in the activities of daily living, and they have been carrying out with the same intensity when compared to period of pre-COVID diagnosis. Around 106 (11%) reported negligible differences in the day-to-day activities. Despite symptoms they were performing all day-to-day activities without assistance. Twenty-four (2%) reported that their usual activities reduced due to symptoms and anxiety and 3 (0.3%) participants reported that their functional status affected drastically and required constant support for the activities of daily living when compared to period of pre-COVID diagnosis.
On bivariate analysis, having at least one comorbidity and hospitalised for severe COVID-19 were significantly associated with persistent post COVID-19 symptoms (Table 1 ). On multivariate analysis, hospitalised for severe COVID-19 was independently associated with persistent post COVID-19 symptoms (aOR= 2.2, 95% CI= 1.6-3.1) (Table 1). Severe limitations of the functional status were significantly higher among those with comorbidity than those who did not [aOR= 2.7, 95% CI= 1.2-6.8].
Table 1.
Predictors of persistent post COVID-19 symptoms, Tamil Nadu, India, 2021
| Exposures | # Reported persistent symptom (n=249) | % | # Reported no persistent symptom (n=752) | % | OR | 95% CI | aOR* | 95% CI* |
|---|---|---|---|---|---|---|---|---|
| Aged >45 years | 143 | 57 | 402 | 53 | 1.8 | 0.9-1.6 | ||
| Male gender | 147 | 59 | 449 | 60 | 1 | 0.7-1.3 | ||
| Having at least one comorbidity | 98 | 39 | 243 | 32 | 1.4 | 1.0-1.8 | 1.2 | 0.8-1.6 |
| Hospitalised for severe COVID-19 during active phase of infection | 157 | 63 | 325 | 43 | 2.2 | 1.7-3.0 | 2.2 | 1.6-3.1 |
| # Severe limitation in ADL (n= 27) | % | Nil to negligible limitation in ADL (n= 974) | % | OR | 95% CI | aOR* | 95% CI* | |
| Aged >45 years | 19 | 70 | 526 | 54 | 2 | 0.9-4.6 | ||
| Male gender | 18 | 67 | 578 | 59 | 1.4 | 0.6-3.0 | ||
| Having at least one comorbidity | 17 | 63 | 324 | 33 | 3.4 | 1.5-7.5 | 2.7 | 1.2-6.8 |
| Hospitalised for severe COVID-19 during active phase of infection | 20 | 74 | 462 | 47 | 3.2 | 1.3-7.6 | 2.4 | 1.0-6.0 |
*Adjusted for all the exposures
The prevalence of at least one persistent symptom in our study was lower than the studies from high income countries.5 , 8 Weakness, general malaise, fatigue, brain fog, and breathlessness were the most commonly reported long COVID-19 symptoms in high income countries.5 On the other hand, weight loss, hair loss, and excessive tiredness were the most common reported symptoms in our setting. Globally, almost one in four reported brain fog and breathlessness post COVID-19 compared to 2% and 6% respectively in Chennai. Our study also found that hospitalisation for severe COVID-19 was the predictor for long COVID-19 which is consistent with the findings from other studies.9
Although our study provides the estimates of burden of long COVID-19 and functional status post recovery, it suffers from a few limitations. We collected follow up data among hospitalized individuals for a two week period. The non-response was 20% which might have lead on under or over estimate of the prevalence. Also, we could not stratify the case-patients as ICU and non-ICU admissions. Due to overwhelmed health system during the pandemic, the ICU services were provided in the non-ICU wards also; hence, the team faced difficulties in eliciting accurate hospitalisation history. Thus we analysed the whole data among hospitalized case-patients. Lastly, the cross-sectional study design did not permit us to establish the temporality between the exposure and outcome. Longitudinal follow-ups, prospective cohort study or establishing registry in clinical settings is critical to understand the post COVID-19 sequel in the long term.
References
- 1.Post COVID Conditions (e.g. Long COVID). Available at https://www.idsociety.org/covid-19-real-time-learning-network/disease-manifestations–complications/post-covid-syndrome/. Accessed October 4, 2021, n.d.
- 2.Fernández-de-las-Peñas César Martín-Guerrero, José D., Navarro-Pardo Esperanza Rodríguez-Jiménez, Jorge Pellicer-Valero, Oscar J. Post-COVID functional limitations on daily living activities are associated with symptoms experienced at the acute phase of SARS-CoV-2 infection and internal care unit admission: A multicenter study. J Infect. 2021;0(0) doi: 10.1016/j.jinf.2021.08.009. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.César Fernández-de-las-Peñas, Víctor Gómez-Mayordomo, I de-la-Llave-Rincón Ana, María Palacios-Ceña, Jorge Rodríguez-Jiménez, Florencio Lidiane L., et al. Anxiety, depression and poor sleep quality as long-term post-COVID sequelae in previously hospitalized patients: A multicenter study. J Infect. 2021;83(4):496–522. doi: 10.1016/j.jinf.2021.06.022. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.M Garratt Andrew, Waleed Ghanima, Gunnar Einvik, Knut Stavem. Quality of life after COVID-19 without hospitalisation: Good overall, but reduced in some dimensions. J Infect. 2021;82(5):186–230. doi: 10.1016/j.jinf.2021.01.002. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Melina Michelen, Lakshmi Manoharan, Natalie Elkheir, Vincent Cheng, Andrew Dagens, Claire Hastie, et al. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021;6(9) doi: 10.1136/bmjgh-2021-005427. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.A Klok Frederikus, Boon Gudula J.A.M., Stefano Barco, Matthias Endres, Miranda Geelhoed J.J., Samuel Knauss, et al. The Post-COVID-19 Functional Status scale: a tool to measure functional status over time after COVID-19. Eur Respir J. 2020;56(1) doi: 10.1183/13993003.01494-2020. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Modified Medical Research Council Dyspnea Scale in GOLD Classification Better Reflects Physical Activities of Daily Living | Respiratory Care. Available at http://rc.rcjournal.com/content/63/1/77. Accessed October 4, 2021, n.d. [DOI] [PubMed]
- 8.César Fernández-de-las-Peñas, Domingo Palacios-Ceña, Víctor Gómez-Mayordomo, L Florencio Lidiane, L Cuadrado María, Gustavo Plaza-Manzano, et al. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur J Intern Med. 2021;92:55–70. doi: 10.1016/j.ejim.2021.06.009. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.M Iqbal Fahad, Kyle Lam, Viknesh Sounderajah, M Clarke Jonathan, Hutan Ashrafian, Ara Darzi. Characteristics and predictors of acute and chronic post-COVID syndrome: A systematic review and meta-analysis. EClinicalMedicine. 2021;36 doi: 10.1016/j.eclinm.2021.100899. Doi: [DOI] [PMC free article] [PubMed] [Google Scholar]