Abstract
Fibro-osseous lesions are a poorly defined category of conditions affecting the jaws and craniofacial bones, and include developmental lesions, reactive or dysplastic lesions, and neoplasms. Fibrous dysplasia and ossifying fibroma are the 2 main types of fibro-osseous lesions affecting the jaw, and ossifying fibroma is a true benign neoplasm of the bone-forming tissues with several well-recognized variants ranging from innocuous to extensively aggressive lesions. However, multiple simultaneous fibro-osseous lesions of the jaw bones involving all quadrants are exceedingly rare. One such case diagnosed by conventional radiography and computed tomography is discussed here.
Keywords: Fibroma, Ossifying; Tomography, X-Ray Computed; Diagnosis; Radiology
Fibro-osseous lesions in jaw bones include fibrous dysplasia, ossifying fibroma, florid osseous dysplasia, and focal osseous dysplasia.1 These represent a histologically similar but radiographically diverse category of lesions. Ordinarily, ossifying fibromas occur as solitary lesions, but in rare instances, they are seen at multiple sites. Earlier reports include Takeda and Fujioka,2 who described multiple lesions in 3 jaw quadrants, and Hauser et al.,3 who presented a case of bilateral ossifying fibromas in the maxillary sinuses. Subsequently, Hwang et al.4 reported a case of ossifying fibromas in all quadrants with 18 years of follow-up. Bertolini et al.5 reported a case of multiple ossifying fibromas in the maxilla and the mandible. More recently, Canger et al.6 reported 2 cases of familial multiple ossifying fibromas involving 2 quadrants in the mandible and the maxilla. Earlier, Yih et al.7 reported familial multiple ossifying fibromas with involvement of 3 quadrants. Hence, the purpose of this case report was to present the clinical and radiological features of multiple simultaneous fibro-osseous lesions of the jaw bones involving all quadrants in order to facilitate the proper diagnosis of this rarely reported condition. To the best of the authors' knowledge, this is the first reported case of multiple ossifying fibromas with simultaneous presentation in all 4 quadrants, and the imaging features of these lesions on panoramic radiography and computed tomography (CT) made it possible to distinguish this rare entity from similar-appearing lesions to achieve a better treatment outcome.
Case Report
A 14-year-old girl from eastern Nepal reported to the authors' clinic with progressive facial disfigurement in the past 3 years due to swelling in the left maxilla. No history of associated trauma or systemic or local infectious conditions was elicited. The associated symptoms of left nasal stuffiness and difficulty in breathing were noted starting 6 months ago. The patient's family and medical history were non-contributory. Upon physical examination, a solitary diffuse, non-tender, bony hard swelling measuring 4×3 cm was noted in the left maxilla. An intraoral examination revealed a swelling in the left maxillary alveolar region that was non-tender and bony-hard on palpation (Fig. 1). The adjacent dentition and oral mucosa showed no abnormalities. A provisional diagnosis of fibrous dysplasia was given, with ossifying fibroma, central giant cell granuloma, and benign odontogenic tumour considered as differential diagnoses.
Fig. 1. Intraoral photograph shows diffuse enlargement of the left maxillary alveolus.

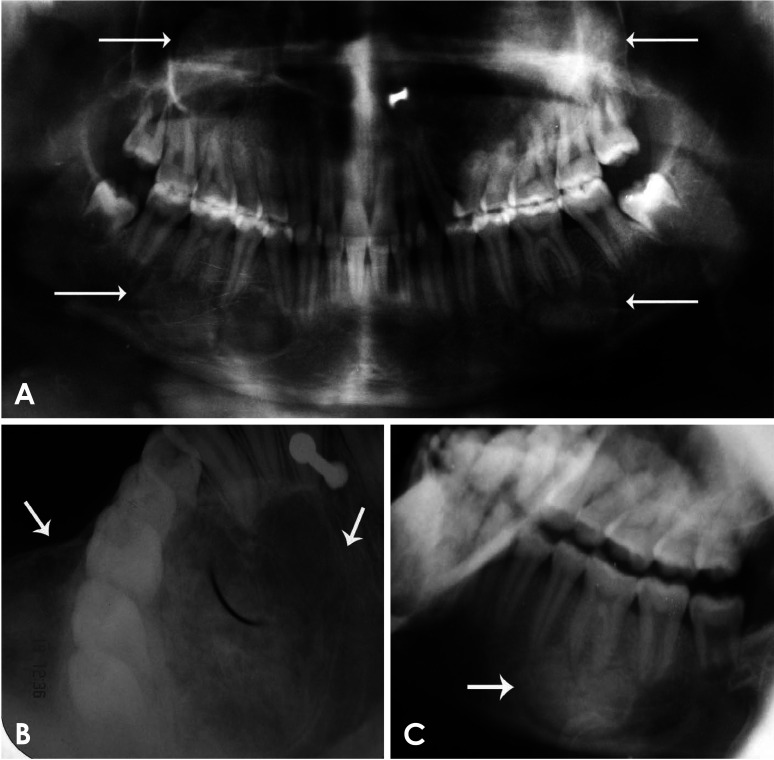
Panoramic radiography revealed radiopaque discrete lesions in all 4 quadrants with a peripheral radiolucent rim. The right maxillary alveolus presented with a smaller lesion measuring 1×2 cm that raised the floor of the maxillary sinus in a dome-shaped manner. The mandibular lesions were localized on both the right and left second premolar to first molar regions, and measured 3×2 cm. The most radiopaque area was located centrally, particularly in the mandibular lesions. The lesions showed displacement of the adjacent tooth roots, the mandibular canal, and maxillary sinus floor (Fig. 2A). A maxillary occlusal topographic radiograph revealed an expansile radiopaque lesion measuring 4×3 cm extending to the mid-palatine suture in the left maxillary quadrant (Fig. 2B). A lateral oblique radiograph of the left mandibular body showed a radiopaque lesion with a peripheral radiolucent rim (Fig. 2C). Computed tomography (CT) coronal and axial images revealed expansile osteogenic lesions in the 4 quadrants (Fig. 3), with the lesion in the left maxilla being the largest. No evident breach was noted in the antral walls except for the left lateral nasal wall. Radiographic diagnoses of fibrous dysplasia, ossifying fibroma, and osseous dysplasia including florid osseous dysplasia were considered.
Fig. 2. A. Panoramic radiograph shows radioopaque discrete lesions in all 4 quadrants (arrows) with a peripheral radiolucent rim. Displacement of the mandibular canal inferiorly and opacification of the right and left maxillary sinuses with the floor displaced superiorly are observed. B. Left maxillary occlusal topographic image shows an expansile radiopaque lesion (arrows) extending to the mid-palatine suture. C. Lateral oblique left mandible body shows a radiopaque lesion (arrows) with peripheral radiolucent rim.
Fig. 3. A and B. Axial computed tomographic (CT) images of the osteomeatal complex show the heterogeneous osteogenic expansile lesion completely occupying the left antrum with displacement of the lateral nasal wall. A smaller completely ossified lesion in the right antrum is also noticed. C and D. Coronal CT images show expansile destruction of the left maxillary sinus and a smaller lesion in the right maxillary sinus.
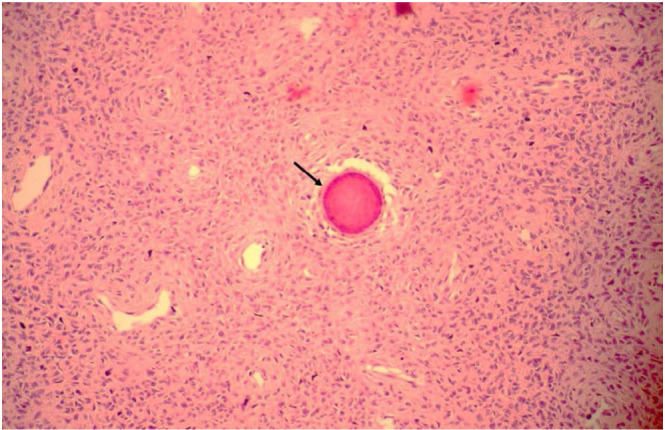
The patient was advised to receive an evaluation of serum calcium and alkaline phosphatase levels along with routine hematological investigations, which were within the normal limits. Biopsies of the maxillary lesions and both mandibular lesions were performed under local anaesthesia. The histological examination revealed predominant fibrous tissue with ossifications and cementum-like material suggestive of fibro-osseous lesions. The presence of cementum-like material and ossifications strongly suggested ossifying fibromas (Fig. 4). Surgery was then planned in a phased manner. Considering the age of the patient, a conservative approach with aggressive curettage was performed under general anaesthesia. The most extensive and symptomatic of the lesions in the left and right maxilla were aggressively curetted after obtaining bony access into the maxillary sinus by intraoral approaches on 2 separate occasions.
Fig. 4. Histopathology of mandibular lesions after biopsy showing fibrous stroma with plump spindle-shaped fibroblasts with spherical eosinophilic cementum-like areas (arrow) (H&E stain, original magnification ×10).
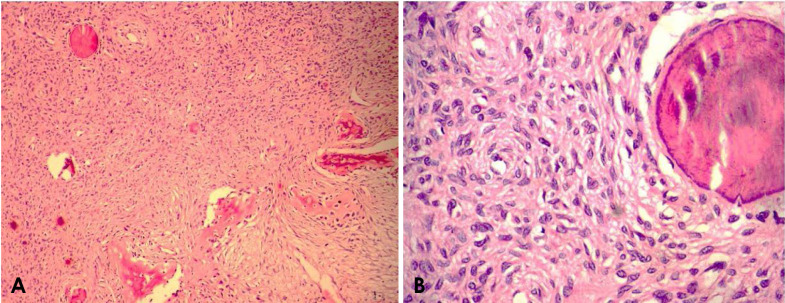
On gross appearance, the left maxillary lesion was friable and obtained as multiple fragmented bits of fibrous tissue (Fig. 5). Histopathology with routine haematoxylin and eosin staining showed a predominantly fibrous stroma with plump spindle-shaped fibroblasts arranged in whorled patterns (Fig. 6). Areas of ossification and irregularly shaped immature cellular bony trabeculae representing woven bone were noted dispersed throughout the lesion. Some areas of spherical eosinophilic calcifications with basophilic concentric reversal lines, suggestive of psammoma bodies, were noted. The histological features were strongly suggestive of ossifying fibroma.
Fig. 5. Gross appearance of the tumour excised from the left maxillary sinus.

Fig. 6. A. Histopathology of maxillary lesions after surgical excision shows fibrous stroma with a whorled pattern of arrangement of fibroblasts and woven bone trabeculae (H&E stain, original magnification ×10). B. Whorled pattern of arrangement of fibroblasts with an eosinophilic cementum-like structure is seen (H&E stain, original magnification ×45).
The patient remained asymptomatic for 2 years of follow-up. However, she was reluctant to undergo further surgery for the mandibular lesions or any further investigations.
Discussion
Ossifying fibroma is a true benign neoplasm of the bone-forming tissues with several well-recognized variants ranging from innocuous to extensively aggressive lesions. Three overlapping clinico-pathological entities are recognized: 1) conventional ossifying fibroma, 2) juvenile trabecular ossifying fibroma, and 3) juvenile psammomatoid ossifying fibroma.8,9 Ossifying fibromas most frequently occur in female patients with an incidence peak in the third and fourth decades of life. Seventy percent of cases of ossifying fibroma involve the mandible, but a significant percentage (22%) is found in the molar region of the maxilla, in the ethmoidal and orbital regions, and rarely in the petrous bone.10 Ossifying fibromas ordinarily occur as solitary lesions, but in rare instances when they are seen at multiple sites2,3,4,5 or show familial6,7 or sequential presentations, they hint at stronger underlying genetic defects that should be explored. Pimenta et al.11 demonstrated mutations of the HRPT2 gene in ossifying fibroma and suggested that ossifying fibroma might arise due to haplo-insufficiency of the HRPT2 gene, possibly explaining the genetic basis of multiple ossifying fibroma. However, Toyosawa et al.12 concluded that the HPRT2 mutation seen in hyperparathyroid-jaw tumour syndrome was not common in the development of ossifying fibroma, and therefore may not be useful as a routine marker for diagnosis.
Radiographically, ossifying fibroma can present in 3 overlapping stages ranging from immature cyst-like radiolucencies and scattered radiopaque foci to dense sclerotic lesions. The margins of ossifying fibroma lesions usually are well defined, with a transition zone of less than 1 mm, as seen in our case. A thin, radiolucent line, representing a fibrous capsule, may separate the lesion from the surrounding bone. Juvenile ossifying fibromas tend to be more radiopaque than conventional lesions and sometimes may have a “ground glass” appearance or may form dense lobulated masses.8,10 However, ossifying fibroma is best visualized by CT in the sinonasal regions, where it tends to fill the paranasal sinuses and destroy bone - a feature noted in the left maxillary lesion in the case presented herein. Kashyap et al.13 reported a case of ossifying fibroma of the maxilla involving the maxillary sinus and ethmoid sinus in a 40-year-old female patient, in which CT coronal sections showed an ill-defined expansile mass lesion completely occluding the right maxillary sinus, extending inferiorly up to the right maxillary alveolus. Ossifying fibroma may present a variable radiographic appearance; unlike the above description, in another case described by Pérez-García et al.,14 a radiolucent zone surrounded by a poorly delimited sclerotic halo was evident on radiography in a 22-year-old male patient, and the lesion was diagnosed as ossifying fibroma after surgical resection. A diagnostic dilemma exists for gnathic fibro-osseous lesions between ossifying fibroma and focal osseous dysplasia. However, ossifying fibromas are known to be aggressive lesions characterized by expansion, tooth displacement, and root resorption, which can differentiate them from focal osseous dysplasia, as noted in the present case.1 Another type of reactive bony lesion is gigantiform cementoma; this rare form of ossifying fibroma, occurs exclusively in the jaws and involves 2, 3, or 4 quadrants. Radiographically, mixed radiolucent-radiopaque expansile lesions are evident - that is, floccular calcifications are seen within a large radiolucent mass.15
Ossifying fibroma affecting the jaws is histologically confirmed not as an ossifying fibroma, but only as a fibroosseous lesion.1 While fibrous dysplasia shows thin irregular-shaped woven bone that resembles membranous ossification, ossifying fibroma has a moderately cellular, dense fibrous stroma with prominent calcified spherules corresponding to ossicles and cementicles, as seen in our case. Moreover, fibrous dysplasia shows strong immunoreactivity for osteocalcin in calcified materials, whereas ossifying fibroma stains weakly.12
The management of ossifying fibroma is usually conservative surgery unless extensive involvement of adjacent structures indicates otherwise. If a sudden growth spurt demonstrates aggressive behaviour, recurrence occurs after curettage, or extensive erosion of the multilocular type is seen, en bloc resection should be considered for definitive treatment.2,3,4,5,6
To conclude, the present rare case, which involved a simultaneous multi-quadrant presentation of fibro-osseous lesions with features suggestive of ossifying fibroma, cannot be attributed to a matter of chance alone. The recent discovery of the inactivation of the HPRT2 gene and its probable role in the pathogenesis of ossifying fibroma should be explored. Moreover, a thorough clinico-radiological correlation with a histopathological examination is recommended for accurate diagnosis and treatment, which is usually conservative surgery unless extensive involvement of adjacent structures necessitates en bloc resection to reduce the risk of recurrence.
Footnotes
Conflicts of Interest: None
References
- 1.MacDonald-Jankowski DS. Ossifying fibroma: a systematic review. Dentomaxillofac Radiol. 2009;38:495–513. doi: 10.1259/dmfr/70933621. [DOI] [PubMed] [Google Scholar]
- 2.Takeda Y, Fujioka Y. Multiple cemento-ossifying fibromas. Int J Oral Maxillofac Surg. 1987;16:368–371. doi: 10.1016/s0901-5027(87)80161-3. [DOI] [PubMed] [Google Scholar]
- 3.Hauser MS, Freije S, Payne RW, Timen S. Bilateral ossifying fibromas of the maxillary sinus. Oral Surg Oral Med Oral Pathol. 1989;68:759–763. doi: 10.1016/0030-4220(89)90168-0. [DOI] [PubMed] [Google Scholar]
- 4.Hwang EH, Kim HW, Kim KD, Lee SR. Multiple cemento-ossifying fibroma: report of an 18-year follow-up. Dentomaxillofac Radiol. 2001;30:230–234. doi: 10.1038/sj.dmfr.4600608. [DOI] [PubMed] [Google Scholar]
- 5.Bertolini F, Caradonna L, Bianchi B, Sesenna E. Multiple ossifying fibroma of the jaws: a case report. J Oral Maxillofac Surg. 2002;60:225–229. doi: 10.1053/joms.2002.29832. [DOI] [PubMed] [Google Scholar]
- 6.Canger EM, Celenk P, Kayipmaz S, Alkan A, Gunhan O. Familial ossifying fibromas: report of two cases. J Oral Sci. 2004;46:61–64. doi: 10.2334/josnusd.46.61. [DOI] [PubMed] [Google Scholar]
- 7.Yih WY, Pederson GT, Bartley MH., Jr Multiple familial ossifying fibromas: relationship to other osseous lesions of the jaws. Oral Surg Oral Med Oral Pathol. 1989;68:754–758. doi: 10.1016/0030-4220(89)90167-9. [DOI] [PubMed] [Google Scholar]
- 8.Silvestre-Rangil J, Silvestre FJ, Requeni-Bernal J. Cemento-ossifying fibroma of the mandible: presentation of a case and review of the literature. J Clin Exp Dent. 2011;3:e66–e69. [Google Scholar]
- 9.Mohapatra M, Banushree CS, Nagranjan K, Pati D. Cemento-ossifying fibroma of mandible: an unusual case report and review of literature. J Oral Maxillofac Pathol. 2015;19:405. doi: 10.4103/0973-029X.174646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasia and cemento-ossifying fibromas. II. A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:540–549. doi: 10.1016/s1079-2104(97)90271-7. [DOI] [PubMed] [Google Scholar]
- 11.Pimenta FJ, Gontijo Silveira LF, Tavares GC, Silva AC, Perdigão PF, Castro WH, et al. HRPT2 gene alterations in ossifying fibroma of the jaws. Oral Oncol. 2006;42:735–739. doi: 10.1016/j.oraloncology.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 12.Toyosawa S, Yuki M, Kishino M, Ogawa Y, Ueda T, Murakami S, et al. Ossifying fibroma vs fibrous dysplasia of the jaw: molecular and immunological characterization. Mol Pathol. 2007;20:389–396. doi: 10.1038/modpathol.3800753. [DOI] [PubMed] [Google Scholar]
- 13.Kashyap RR, Nair GR, Gogineni SB. Asymptomatic presentation of aggressive ossifying fibroma: a case report. Case Rep Dent. 2011;2011:523751. doi: 10.1155/2011/523751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pérez-García S, Berini-Aytés L, Gay-Escoda C. Ossifying fibroma of the upper jaw: report of a case and review of literature. Med Oral. 2004;9:333–339. [PubMed] [Google Scholar]
- 15.Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol. 2008;2:177–202. doi: 10.1007/s12105-008-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]