Abstract
Introduction and importance
Covid-19 is an important disease that still occupies our agenda, and as time passes, we have been observing its extrapulmonary manifestations. In this study, we presented a case of spontaneous thoracolumbar epidural hematoma, which we could not attribute to any cause other than Covid-19.
Case presentation
We presented a 55-year-old female patient whose etiology could not be found to be compatible with the literature. In the formation of this disease, we did not have any positive findings except for Covid-19, which she had 20 days ago. The patient had no history of anticoagulant or antiaggregant drug use. He had no history of trauma and no signs. Hematological tests were normal. We evacuated the hematoma in the T12-L1 vertebral canal after laminectomy and the pathology result was compatible with hematoma.
Clinical discussion
Although spontaneous spinal epidural hematoma is rare, many factors are blamed for its etiology. Many extrapulmonary complications of Covid-19 stand out in the literature. The fact that the patient had Covid-19 did not affect the neurosurgical approach, but we think that it is useful to examine the complaints of patients with Covid-19 more systematically.
Conclusion
Spontaneous spinal epidural hematomas are rare. Making the correct diagnosis often takes time and is difficult. Decompression surgery is at the forefront as a treatment option. However, conservative treatment can be performed in suitable patients. As we saw in this case, we should consider Covid-19 among the etiological causes.
Keywords: Covid-19, Spinal epidural hematoma, Spinal Canal
Highlights
-
•
The etiology of spontaneous spinal epidural hematoma is multifactorial.
-
•
Covid-19 is one of these etiological factors.
-
•
Etiological cause does not change the approach to spontaneous spinal hematoma.
1. Introduction and importance
Covid-19 SARS-CoV-2 is a pandemic that still causes high mortality and morbidity in our world. In addition to known pulmonary complications, Covid 19 causes many different and extrapulmonary findings and diseases as time passes [1], [2]. Among these, one of the subjects in neurosurgery practice is spontaneous spinal epidural hematomas. Its incidence is 0.1 per 10 million people [3]. Diagnosis is difficult and delayed due to its rarity and atypical symptoms. The main non-traumatic etiological causes are coagulation disorders, vascular malformations, tumors, pregnancy, and uncontrolled hypertension, respectively [4]. We presented a case of spontaneous spinal epidural hematoma that developed after Covid-19 disease in accordance with the SCARE 2020 guideline [5].
2. Case presentation
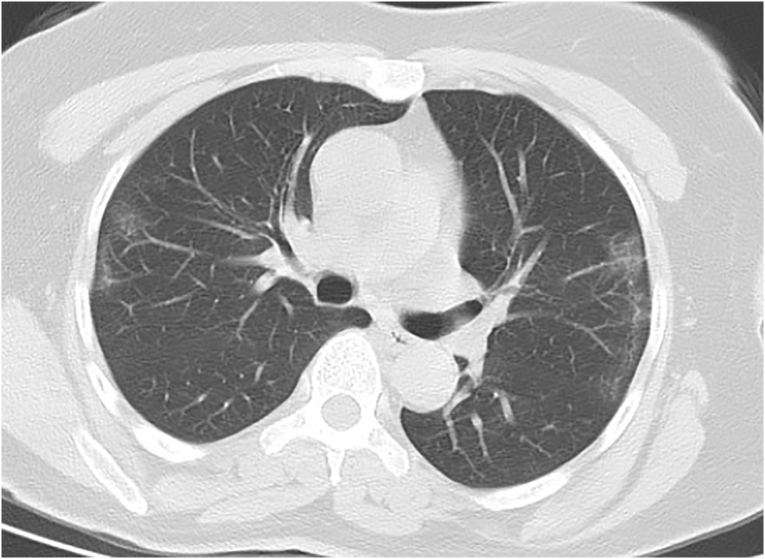
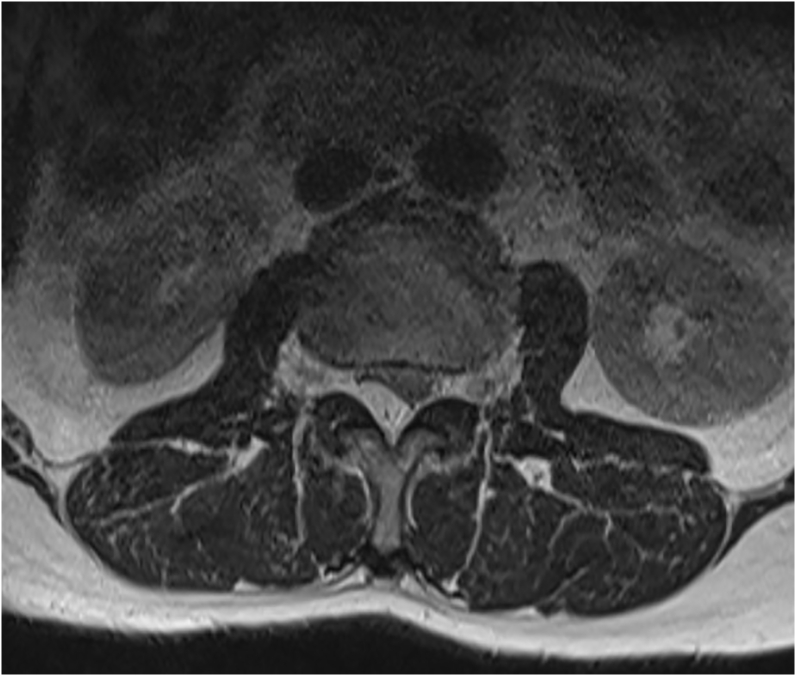
A 55-year-old female patient came to our outpatient clinic with complaints of severe low back pain and weakness in her feet. In the anamnesis of the patient, whose general condition was good, it was seen that she had covid-19 about 20 days ago. Covid-19 PCR test was positive and typical covid-19 findings were found in thorax tomography according to RSNA classification [6] (Fig. 1). The patient had no history of trauma. In the physical examination, the patient had a minimal motor deficit in right thigh flexion, and the external neurological examination was found to be normal. No swelling and ecchymosis were detected in the dorsal region on inspection. There was no comorbid disease. She had no history of anticoagulant and anti-aggregant drug use and was not found in all past medical data. A lumbar MRI was planned and the patient was admitted to the ward. In the lumbar MRI, a mass lesion with a caudal length of 3 cm and a diameter of 1,5 cm at the widest point was seen, located on the right posterolateral side of the T12-L1 vertebral canal, which was isointense in t1 sequence and hyperintense in t2 sequence (Fig. 2, Fig. 3) Epidural hematoma, epidural abscess, and epidural mass were considered in the differential diagnosis. Contrast-enhanced MRI was seen and no significant contrast enhancement was observed. In the pre-operative examinations, the patient's INR was 1.14. When the infection parameters were evaluated, the white blood cell was found to be 7.3 × 103/μl, and the C-reactive protein was found to be in the normal range of 4.9 mg/L. The advantages and disadvantages of conservative and surgical treatment were explained to the patient and the decision to operate was taken and the patient was operated on by Z.O. After laminectomy, the epidural hematoma was encountered and evacuated. There was no other situation that would cause doubt in the surgical observation (Fig. 4). After the intervention, the patient's deficit improved and her pain decreased. In the post-operative period, the patient adapted to the recommended treatments such as wound care and rest. Hematology consultation was made for possible hematological diseases. Additional hematological studies and peripheral smear were performed and a hematological disease was not considered. As a result of pathology, no malignancy was detected, it was compatible with hematoma.
Fig. 1.
Thoracic computed tomography with typical Covid-19 findings.
Fig. 2.
Pre-operative axial MRI image of the mass lesion.
Fig. 3.
Pre-operative sagittal MRI image of the mass lesion.
Fig. 4.

Intra-operative view of epidural hematoma.
3. Clinical discussion
Spontaneous epidural hematoma is a very rare disease that can be a neurological emergency. It constitutes 0.3–0.9% of all epidural space-occupying lesions [7]. When the etiological causes are examined, hematological disorders come first. This is followed by vascular malformations and tumors. Examples of uncontrolled hypertension, pregnancy, and cocaine use appear in the literature [8]. In our case, it is interesting that the patient had no trauma history and findings, hematological tests were within normal limits, and no arteriovenous malformation or tumor was detected in the surgical observation and pathology result. The only positive finding we have is that the patient had Covid-19 20 days before the symptoms started. When we examine the literature, other cases are encountered among the extrapulmonary findings of Covid 19. However, there are very limited cases related to this issue. In a case presented by Yang-Lim, a C2-C6 epidural hematoma case of a 79-year-old patient with Covid-19 is presented [9]. In another study by Scalia et al., an epidural hematoma extending from the clivus to the T6 level was detected at the age of 55 [10]. No surgery was performed because the hematoma was followed up and regressed. However, due to acute motor deficit in our case, surgery was planned and performed. In addition, and as a result, we proved that there is a hematoma pathologically.
4. Conclusion
Spontaneous spinal epidural hematoma is a rare disease and is not usually in the foreground in the differential diagnosis. Decompression surgery is suitable for the surgical approach, but it has a place in conservative treatment in appropriate cases. Although the literature information is limited, it is useful to keep in mind Covid-19 among its etiological causes.
Source of funding
No financial support was received for the study.
Ethical approval
N/A.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Research registration
N/A.
Guarantor
The Guarantor is Adem Kurtuluş, MD
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
All authors contributed equally.
Declaration of competing interest
All authors declare that they have no conflict of interest.
References
- 1.Gupta A., Madhavan M.V., Sehgal K., Nair N., Mahajan S., Sehrawat T.S., et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 2.Aydin S., Öz G., Dumanli A., Balci A., Gencer A. A case of spontaneous pneumothorax in Covid-19 pneumonia. J. Surg. Res. 2020;03(02):96–101. [Google Scholar]
- 3.Eto F., Tatsumura M., Iwabuchi S., Ogawa T., Mammoto T., Hirano A. Clinical features of spontaneous spinal epidural hematoma. J. Rural. Med. 2019;14(2):206–210. doi: 10.2185/jrm.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thiele R.H., Hage Z.A., Surdell D.L., Ondra S.L., Batjer H.H., Bendok B.R. Spontaneous spinal epidural hematoma of unknown etiology: case report and literature review. Neurocrit. Care. 2008;9(2):242–246. doi: 10.1007/s12028-008-9083-x. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Jaergere T., Krdzalic J., Fasen B., Kwee R. Radiological Society of North America chest classification system for reporting COVID-19 pneumonia: interobserver variability and correlation with RT-PCR. Cardiothorac Imaging. 2020 doi: 10.1148/ryct.2020200213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang P., Xin X.T., Lan H., Chen C., Liu B. Spontaneous cervical epidural hematoma during pregnancy: case report and literature review. Eur. Spine J. 2011;20(SUPPL. 2):176–179. doi: 10.1007/s00586-010-1484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Z., Jiao Q., Xu J., Wang X., Li S., You C. Spontaneous spinal epidural hematoma: analysis of 23 cases. Surg. Neurol. 2008;69(3):253–260. doi: 10.1016/j.surneu.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 9.Lim S.W.Y., Wong E. Spontaneous epidural hematoma of the cervical spine in an elderly woman with recent COVID-19 infection: a case report. Am. J. Case Rep. 2020;21:1–4. doi: 10.12659/AJCR.926784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scalia G., Umana G.E., Marrone S., Graziano F., Giuffrida A., Ponzo G., et al. Spontaneous anterior cervicothoracic spinal epidural hematoma extending to clivus in SARS-CoV-2 infection. Surg. Neurol. Int. 2021;12(181):1–4. doi: 10.25259/SNI_40_2021. [DOI] [PMC free article] [PubMed] [Google Scholar]