Abstract
Objective
Investigate healthcare providers, caregivers, and patient perspectives on tracheostomy care barriers during COVID-19.
Study design
Cross-sectional anonymous survey
Setting
Global Tracheostomy Collaborative Learning Community
Methods
A 17-item questionnaire was electronically distributed, assessing demographic and occupational data; challenges in ten domains of tracheostomy care; and perceptions regarding knowledge and preparedness for navigating the COVID-19 pandemic.
Results
Respondents (n = 115) were from 20 countries, consisting of patients/caregivers (10.4%) and healthcare professionals (87.0%), including primarily otolaryngologists (20.9%), nurses (24.3%), speech-language pathologists (18.3%), respiratory therapists (11.3%), and other physicians (12.2%). The most common tracheostomy care problem was inability to communicate (33.9%), followed by mucus plugging and wound care. Need for information on how to manage cuffs and initiate speech trials was rated highly by most respondents, along with other technical and knowledge areas. Access to care and disposable supplies were also prominent concerns, reflecting competition between community needs for routine tracheostomy supplies and shortages in intensive care units. Integrated teamwork was reported in 40 to 67% of respondents, depending on geography. Forty percent of respondents reported concern regarding personal protective equipment (PPE), and 70% emphasized proper PPE use.
Conclusion
While safety concerns, centering on personal protective equipment and pandemic resources are prominent concerns in COVID-19 tracheostomy care, patient-centered concerns must also be prioritized. Communication and speech, adequate supplies, and care standards are critical considerations in tracheostomy. Stakeholders in tracheostomy care can partner to identify creative solutions for delays in restoring communication, supply disruptions, and reduced access to tracheostomy care in both inpatient and community settings.
Keywords: Tracheostomy, Survey, Healthcare professional, COVID-19
1. Introduction
As the COVID-19 pandemic has unfolded, the controversial questions of tracheostomy timing, techniques, and early outcomes [1], [2], [3], [4], [5], [6] have sometimes eclipsed the softer voices of patients, caregivers, and front-line workers. Yet, these perspectives are critical, as they can surface underappreciated or neglected needs across the continuum of care [7], [8], [9], [10] and survivorship [11].
The number of critically ill patients requiring mechanical ventilation and tracheostomy continues to climb, and the corresponding needs for routine tracheostomy care and related survivorship care have grown [12], [13], [14]. As the pandemic has persisted, staff shortages, difficult working conditions, and constrained resources have thus led to a convergence of interrelated crises, one around safe clinical care and another of burnout, reflecting corrosive effects on the morale of patients and practitioners [15], [16]. Hospitals and healthcare systems across the globe increasingly recognize the cumulative psychological toll of the pandemic, which is evident in the record numbers of departures of nursing staff and allied health professionals [17].
Deepening our understanding of barriers relating to tracheostomy care is a necessary step in rising to meet them. Even before the COVID-19 era, international efforts to improve tracheostomy care were gaining momentum, recognizing that tracheostomy care is fraught with complexity [18], [19], [20]. These efforts have assumed new urgency amid the pandemic. Each successive wave layers new challenges relating to clinical care and the struggle to maintain connection and meaning for professionals, patients, and families [21]. Spiking tracheostomy numbers, safety concerns, and looming shortages have stressed hospitals and communities. Challenges may arise in enabling the establishment of effective person-centered communication [22], [23], [24], [25], [26], [27], [28], shortages in personal protective equipment (PPE) [29], or access to expertise, equipment, and supplies [10], [30]. In addition, caregivers in community settings often perceived significant challenges, particularly if they have chronic illnesses themselves or must provide complicated or unsupported care [31].
The COVID-19 pandemic greatly magnified the barriers to achieving high-reliability tracheostomy care inside and outside the hospital, and there remains little agreement on how to prioritize efforts. To begin to address this knowledge gap, we conducted an international survey inviting perspectives from diverse stakeholders, including multidisciplinary healthcare professionals engaged in tracheostomy care, individuals with tracheostomy, and caregivers. This panoramic view, spanning specialties and geographies, probed several distinct facets of tracheostomy care during the pandemic, which imposed a stress test on the already fraught area of patient care. Understanding the most common problems in tracheostomy care, recognizing the most pervasive concerns, and identifying how care is affected by COVID-19 can help identify the most pressing areas for future training and clinical support to optimize tracheostomy care.
2. Methods
2.1. Study design
A cross-sectional descriptive study was conducted using an anonymous online survey.
2.2. Sample
A convenience sample of participants of a Global Tracheostomy Collaborative (GTC) educational webinar on pandemic tracheostomy care was invited to participate. Participants included a global audience of otolaryngologists, critical care physicians, nurses, speech-language pathologists, respiratory therapists, individuals with tracheostomy, family members, and caregivers registered prior to an educational virtual symposium series. No participants were individually recruited for this study. Participants were included based on their live attendance at the webinar (live or recorded version), with no exclusion criteria specified. The survey was announced live by the webinar organizers during the online event.
2.3. Survey development
The survey was designed to assess perceptions regarding tracheostomy care during the COVID-19 pandemic, emphasizing barriers to care and associated concerns (Supplemental Fig. 1). The survey was formulated based on meetings with focus groups involved in tracheostomy care, including members of the Educational Committee and Patient & Family Committee of Global Tracheostomy Collaborative. The instrument reflects expertise from otolaryngology – head and neck surgery, nursing, speech-language pathology, respiratory care, critical care, and patient and family perspective. The survey instrument was iteratively assessed for clarity and to ensure bias reduction consistent with prior survey development for national/international distribution to American Academy of Otolaryngology – Head Neck Surgery (AAO-HNS), American Academy of Facial Plastic and Reconstructive Surgery (AAFPRS), American Head and Neck Society (AHNS), Society of Otorhinolaryngology Head-Neck Nurses (SOHN), and Global Tracheostomy Collaborative (GTC) [7], [32], [33], [34], [35], [36], [37]. The usability and technical functionality of the final survey were pilot tested by the study team prior to distribution.
Supplemental Fig. 1.
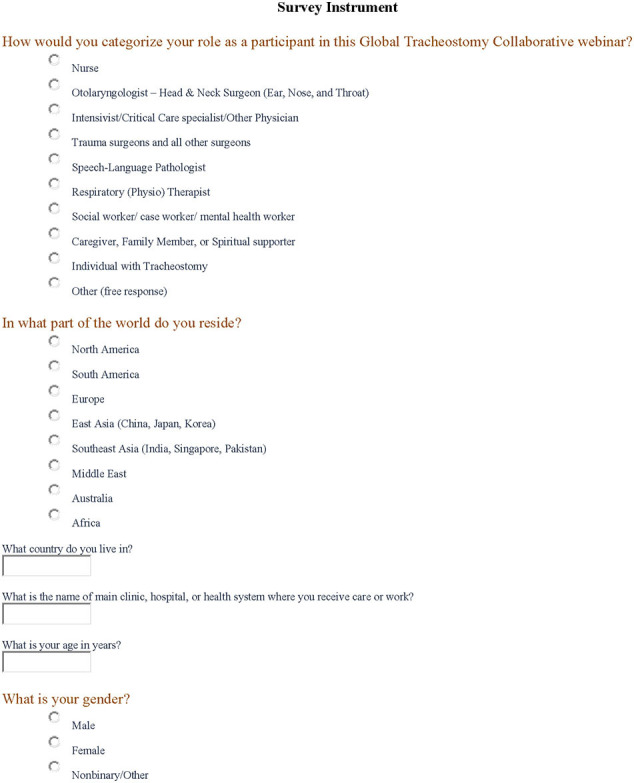
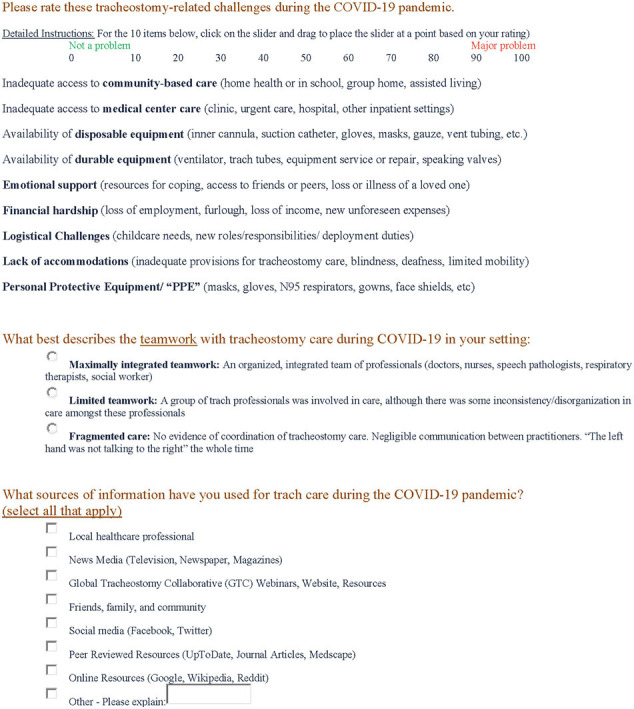
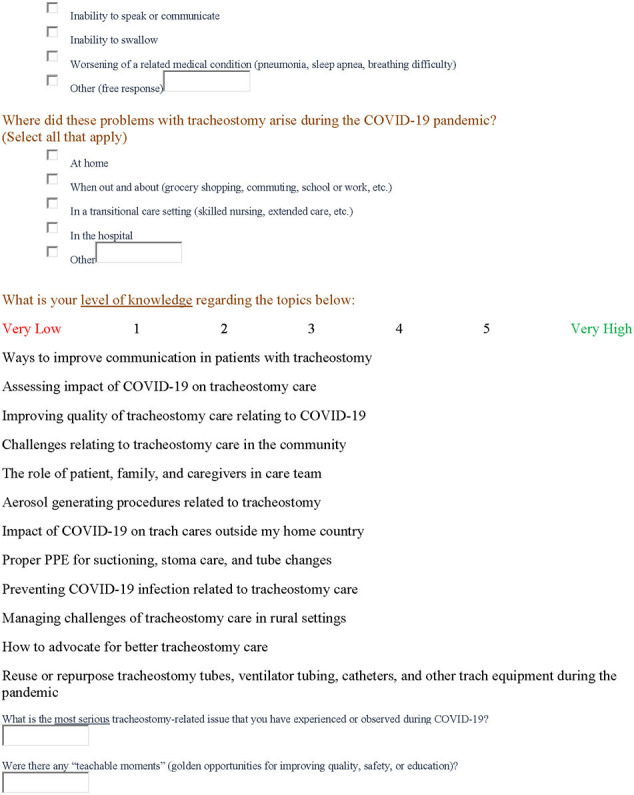
Survey instrument.
The core domains, evaluated in the context of COVID-19 included: (1) demographics and occupations of respondents, (2) care settings where tracheostomy issues occurred, (3) challenges in nine domains of tracheostomy care, (4) perceptions of teamwork, (5) sources of information for tracheostomy care, (6) the relative importance of knowledge and technical areas, (7) problems encountered during tracheostomy care, and (8) the perceived level of knowledge in specific tracheostomy topics. The questionnaire collected demographic data, including sex, age, category (e.g., healthcare provider, family member) or profession of the participant, and country of residence. The questionnaire used was an unvalidated tool consisting of those items identified on iterative assessment to be most relevant by the GTC webinar organizers. Items varied between free-text, single and multiple answer selection, sliding scale, and numbered scale response options. The final survey consisted of seventeen questions, including closed and open-ended questions.
2.4. Data collection
The single-page survey was electronically distributed in English to registrants for a symposium on navigating public needs for health professionals and individuals and families living with tracheostomy on May 5, 2020, and was open for three months. A survey was delivered to each visitor of the website link provided voluntarily without incentive. The provided link served the sole purpose of delivering the survey, which included the estimated length of time to complete the survey, the purpose of data collection, and the organization collecting and retaining responses. All participants provided written informed consent prior to participation. The project was reviewed and approved by the Institutional Review Board of the University of Michigan Medical School (IRB #: HUM00208783). Surveys were collected and stored with the Qualtrics online survey platform [38]. No identifying data was collected during the process to ensure complete participant anonymity. Data were stored on the Qualtrics platform with individual password-protected access limited to the study team.
2.5. Data analysis
Descriptive statistics are presented as means, frequencies, or percentages of overall responses. The results for each survey item are compared between geographical location and profession or type of respondent. Comparisons are described in narrative format. Survey items with sliding scale responses (0−100) were stratified into five equal levels. All statistical analyses were conducted using RStudio software version 1.2.1335 [39] and Stata 17 [40]. Data were manually checked for completeness prior to analysis. This study followed the Checklist for Reporting Results of Internet Surveys (CHERRIES) guidelines [41].
3. Results
One-hundred-fifteen participants completed the survey. The overall response rate was 22% (n = 115/515) of possible session participants to whom the survey was delivered. Respondents were primarily female (67.8%), had a mean age of 46.8 years (SD: 10.6), and were most often based in the United States, the United Kingdom/Europe, or Australia. Most were healthcare professionals (87.0%), with the most significant proportion of these nurses (24.3%), followed by otolaryngologists (20.9%) or speech-language pathologists (18.3%). Individuals with a tracheostomy, caregivers, or family members made up 10.4% of the respondents. No surveys were excluded for incomplete responses.
Demographic information is summarized in Table 1 .
Table 1.
Demographics of survey respondents.
| Overall (N = 115) | |
|---|---|
| Sex | |
| Female | 78 (67.8%) |
| Male | 37 (32.2%) |
| Age | |
| Mean (SD) | 46.8 (10.6) |
| Median [Min, Max] | 46 [22, 78] |
| Type of participant | |
| Caregiver, family member, or spiritual supporter | 5 (4.3%) |
| Individual with tracheostomy | 7 (6.1%) |
| Nurse | 28 (24.3%) |
| Otolaryngologist | 24 (20.9%) |
| Other physician | 14 (12.2%) |
| Respiratory therapist | 13 (11.3%) |
| Speech-language pathologist | 21 (18.3%) |
| Other | 3 (2.6%) |
| Country | |
| Australia | 12 (10.4%) |
| Brazil | 2 (1.7%) |
| Canada | 2 (1.7%) |
| Colombia | 1 (0.9%) |
| Finland | 1 (0.9%) |
| Germany | 1 (0.9%) |
| Greece | 1 (0.9%) |
| India | 2 (1.7%) |
| Indonesia | 1 (0.9%) |
| Iraq | 1 (0.9%) |
| Ireland | 4 (3.5%) |
| Israel | 2 (1.7%) |
| Italy | 2 (1.7%) |
| Netherlands | 1 (0.9%) |
| Pakistan | 1 (0.9%) |
| South Africa | 1 (0.9%) |
| Sweden | 1 (0.9%) |
| Taiwan | 1 (0.9%) |
| United Kingdom | 35 (30.4%) |
| United States | 43 (37.4%) |
3.1. Tracheostomy-related challenges
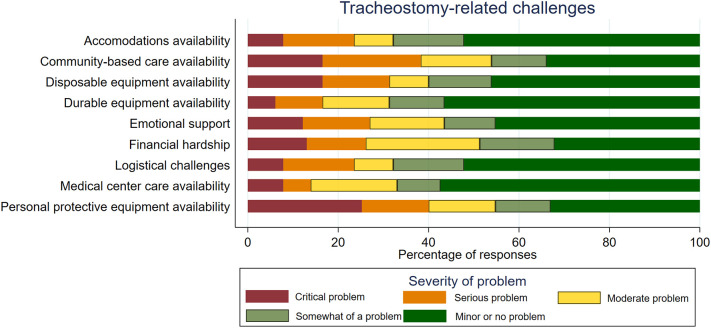
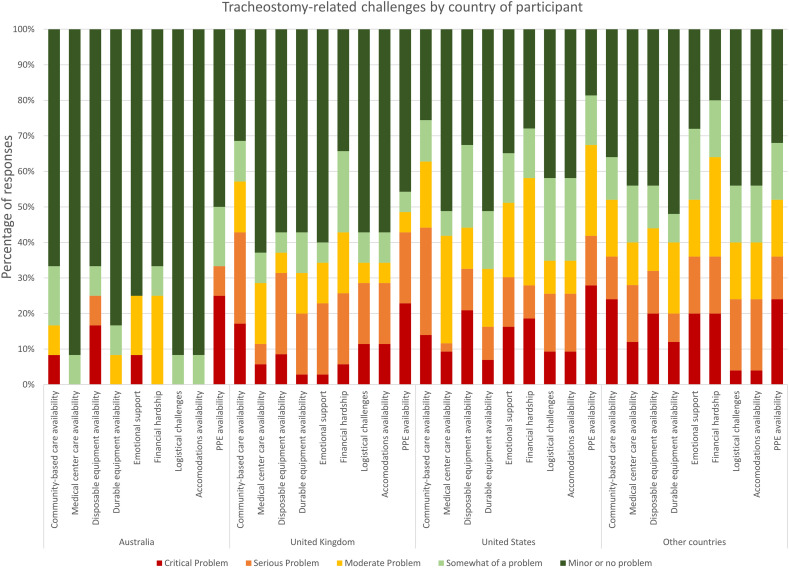
Responses to tracheostomy-related challenges included limited availability of personal protective equipment (40.0%), difficulty accessing community-based care (38.2%), and procuring disposable equipment (31.3%). Respondents also noted concern regarding access to medical center care and durable equipment (Fig. 1 ). Responses were relatively consistent across geographical regions, with PPE availability being the most consistently reported problem (Fig. 2 ).
Fig. 1.
Reported severity of tracheostomy-related challenges in care during the COVID-19 pandemic.
Fig. 2.
Severity of challenges in tracheostomy care during the COVID-19 pandemic, stratified by respondent country.
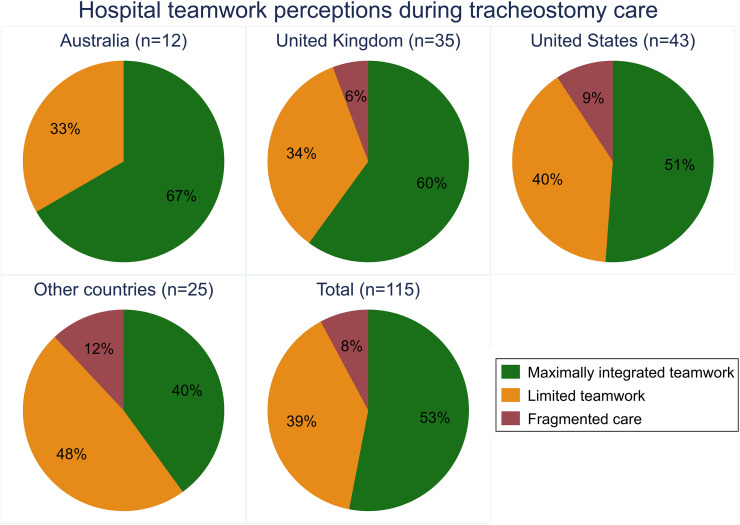
3.2. Perceptions of hospital teamwork
Respondents from Australia and the United Kingdom were most likely to perceive the teamwork at their local or associated facility as having maximally integrated teamwork (66.7% and 60.0%, respectively). Only 51% of respondents from the United States responded similarly (Fig. 3 ), with lower rates among other countries.
Fig. 3.
Perceptions of hospital teamwork in tracheostomy care settings during the COVID-19 pandemic, stratified by respondent country.
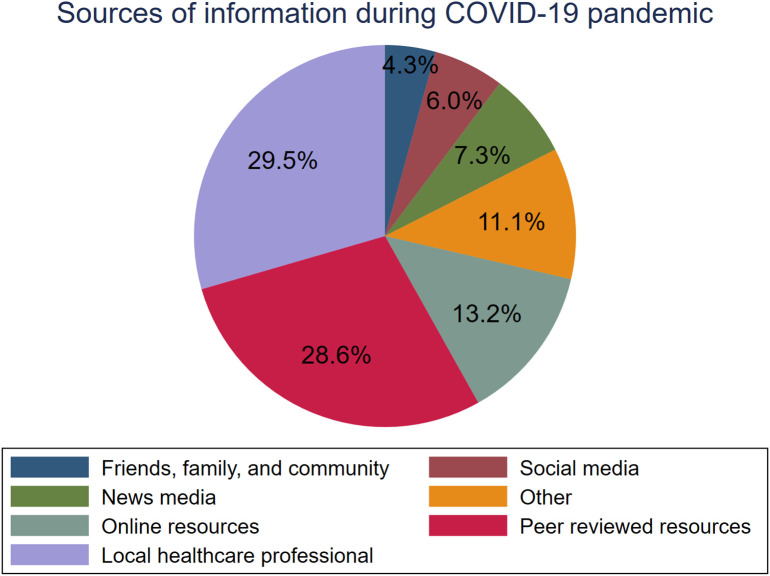
3.3. Sources of information during COVID-19
Local healthcare professionals (60.0%) and peer-reviewed resources (58.3%) were reported as the most used sources of information. Respondents were less likely to rely on friends, family, and community members (8.7%), social media (12.2%), or news media (14.7%) for information about healthcare during the COVID-19 pandemic (Fig. 4 ).
Fig. 4.
Trusted sources of information for healthcare information during the COVID-19 pandemic, in percentages of responses.
3.4. Importance of aspects of tracheostomy care during COVID-19
The importance of 14 knowledge and technical areas of tracheostomy care had similar patterns of responses. Management of cuffs and initiation of speech trials was most frequently considered “not important” or “slightly important” (24.4%). The most frequent “very important” to “extremely important” response was knowledge on protecting oneself from others (86.1%). Other aspects were most often reported as having at least moderate importance (Table 2 ).
Table 2.
Respondent perceptions of importance of tracheostomy knowledge and technical areas during the COVID-19 pandemic.
| Topic | Not important | Slightly important | Moderately important | Very important | Extremely important | |
|---|---|---|---|---|---|---|
| Knowledge areas | How to protect family if I have COVID-19 | 5.22% | 7.83% | 7.83% | 24.35% | 54.78% |
| How to protect myself from others | 4.35% | 4.35% | 5.22% | 24.35% | 61.74% | |
| Where to get PPE | 5.22% | 3.48% | 8.70% | 25.22% | 57.39% | |
| How to recognize COVID-19 signs/symptoms | 4.35% | 4.35% | 11.30% | 22.61% | 57.39% | |
| What to do if infection is suspected | 4.35% | 6.96% | 11.30% | 17.39% | 60.00% | |
| Where to find medical supplies | 5.22% | 5.22% | 12.17% | 25.22% | 52.17% | |
| Who is available to contact for help | 8.70% | 6.96% | 17.39% | 19.13% | 47.83% | |
| Technical areas | How to use PPE properly | 4.35% | 6.96% | 7.83% | 10.43% | 70.43% |
| How to handle trach emergencies | 10.43% | 6.96% | 9.57% | 17.39% | 55.65% | |
| When/how to suction trach tube | 11.30% | 7.83% | 19.13% | 9.57% | 52.17% | |
| When/how to clean trach tube | 10.43% | 8.70% | 19.13% | 9.57% | 52.17% | |
| When/how to change trach tube | 11.30% | 9.57% | 18.26% | 8.70% | 52.17% | |
| Use of humidification devices | 8.70% | 9.57% | 14.78% | 12.17% | 54.78% | |
| How to manage cuffs/initiate speech trials | 18.26% | 6.09% | 11.30% | 11.30% | 53.04% | |
3.5. Tracheostomy care issues during COVID-19
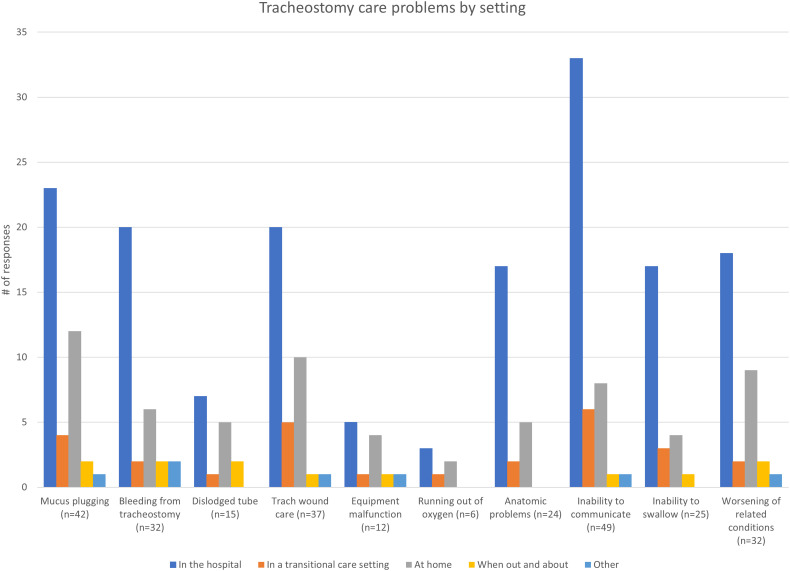
The most frequently reported problems with tracheostomy care during the COVID-19 pandemic were the inability to communicate (33.9%) and mucus plugging of tracheostomy (30.4%). These problems were followed in prevalence by concerns relating to tracheostomy wound care, worsening of underlying health conditions, bleeding from tracheostomy, and inability to swallow. The least-reported problems were running out of oxygen (3.5%) and equipment malfunction (8.7%). Most participants experienced these challenges in a hospital setting (59.1%) or at home (24.3%) (Fig. 5 ).
Fig. 5.
Frequency of reported problems in tracheostomy care during the COVID-19 pandemic, stratified by the setting where respondents experienced those problems.
4. Discussion
This study on challenges in tracheostomy care complements the spirited national discourse on aerosol-generating procedures [42], [43], [44], [45], [46] and overall pandemic related acute-care practices in tracheostomy care [47], [48], [49], [50]. This survey of a diverse sample of healthcare professionals, patients, and families identified pervasive concerns regarding tracheostomy-related communication and safety for both patients and professionals. There was a high degree of commonality among respondents based in the United States, Europe, and Australia in these responses. Concerns regarding availability and education regarding the proper use of PPE were prominently highlighted, but so also were patient-centered and quality-of-life aspects of care, echoing longstanding concerns around speech and communication in tracheostomy care [51], [52]. Additional marked concerns during the COVID-19 pandemic included the availability and reliability of durable equipment and access to medical center care. The most trusted sources of information were local healthcare professionals and peer-reviewed resources.
The literature surrounding tracheostomy care during the COVID-19 pandemic has primarily focused on technical aspects, such as timing and technique for insertion, selection of candidates for tracheostomy, and infection control [14], [53]. However, the psychological toll on healthcare workers of providing care during COVID-19 is also increasingly recognized [54], [55]. This study uncovered some of these stressors and anxieties concerning those encountered in the workplace and family safety concerns. Unfortunately, similar studies spanning diverse geographies and fields of practice, including patient and family voices, have seldom been reported in the context of the pandemic.
Although shortages of PPE are context-specific, common economic and systematic forces may precipitate shortages of equipment. A combination of hospital cost-reduction models (particularly in the United States), demand shock, government-level failures, and supply chain deficiencies act together to cause PPE shortages [29]. This study suggests that those PPE shortages and safety are a prominent concern for patients, caregivers, and healthcare workers internationally. Findings from this study also agree with a national survey in the United Kingdom that found that two-thirds of front-line healthcare professionals felt there was not enough PPE available to them [56]. Likewise, a survey of 637 healthcare workers in Australia showed that while most understood the importance of using PPE, only a quarter felt like PPE supplies were always adequate [57]. However, PPE shortages were not present in all geographic or practice settings; US otolaryngologists reported “always” or “usually” having necessary PPE in a survey of residency programs [58].
As the acute phase of COVID-19 wanes in much of the world, it is increasingly important to address the unmet needs of patients, families, and other caregiver stakeholders moving forward. A holistic rehabilitation framework to recovery must encompass function, activities, and societal participation [59]. Persistent functional impairment of breathing, speaking, and swallowing as sequelae of device-related injury will have lasting effects on the wellbeing of many COVID-19 survivors [60]. Quality of life is commonly hindered further by the persistent loss of taste and smell, which typically occurs after other COVID-19 symptoms and can persist for up to two weeks and beyond [61], impacting nutrition [62], [63]. In addition, the loss of verbal communication has a profound effect on autonomy and quality of life for individuals with tracheostomy [64]. The patient-caregiver communication in tracheostomy care is often complicated with feelings of powerlessness, continual misunderstandings, resignation, and anger during periods of communication difficulty [22] and may last beyond tracheostomy decannulation [65].
The challenges relating to communication that existed prior to the COVID-19 pandemic are more acute in pandemic-era hospital care. Physical distancing and limiting of hospital visitation are necessary infection control measures but inevitably contribute to heightened emotional isolation [66] and loss of communicative connection [21]. A randomized study of mask-wearing and non-mask-wearing physicians demonstrated that masks disrupt facial visual cues and significantly negatively impact perceptions of empathy [67]. Where empathy through physical touch and facial expressions is hindered by PPE and physical distancing, a healthcare provider can instead express empathy by validating patient emotions, exploring feelings, and making supportive statements [68]. A recent systematic review highlights the variety of options for enhancing verbal communication with individuals with tracheostomy [69], including: (1) communication boards, (2) electrolarynx, (3) computer-assisted augmentative and alternative communication, and (4) several types of speaking tracheostomy tubes [70], for patients that cannot tolerate cuff deflation. While the efficacy of interventions to enable communication is varied due to study design, a person-centered and multidisciplinary team approach may optimize the chosen communication option to meet the diverse needs of each individual [71].
This study also demonstrates that hospitals' communication and teamwork during the pandemic were often perceived as limited or fragmented. Effective leadership during periods like the COVID-19 pandemic and adequate planning to meet surges in demand [72] are critically important. Mayo [73] outlines several interventions to enhance teamwork mechanisms during COVID-19, including (1) clarifying roles and interdependencies; (2) using handoff guides, closed-loop communication, and debriefing; and (3) practicing inclusivity by encouraging other professions to speak up, and paying attention to uniquely expressed information from others. Additionally, interprofessional education and training can foster shared understanding in diverse groups of healthcare professionals in acute care situations [74]. Not the least of the barriers in improving hospital teamwork is the aggravation of anxiety, depression, and stress among healthcare workers during COVID-19, as detailed in a systematic review [54]. Supporting healthcare workers and fostering effective teamwork in this period of heightened demand continues to be an issue requiring multiple and simultaneous interventions.
While this study begins to address a critical gap in knowledge, the COVID-19 pandemic is an evolving phenomenon. As such, the perceptions highlighted in this study likely shifted with changing hospital conditions. Frequent assessment of the barriers to safe and effective tracheostomy care for both healthcare workers and families should be used to help inform a robust intervention strategy. Further research into the experiences of individuals with tracheostomy and their caregivers during COVID-19 will be important in addressing key quality-of-life and safety concerns for this public health crisis and those to come.
4.1. Limitations
Several limitations of this study should be considered. First, this survey was based on a convenience sample of registered participants for educational offerings on navigating tracheostomy challenges during COVID-19. This audience is not necessarily representative of all healthcare workers' perceptions, even those engaged in tracheostomy care or individuals with tracheostomy or caregivers. Additionally, respondents to this survey might tend to be more sensitive to challenges or concerns in tracheostomy care given the context of its delivery. Second, there were limited participants from countries other than the United States, United Kingdom, and Australia, so generalizability to other world regions may be limited. This limitation is particularly significant concerning resource-restricted settings (low-and-middle-income countries), likely explaining relatively low rates of critical issues, such as running out of oxygen. Also, the delivery of the survey was in English, which excluded non-English speakers. Third, questions were crafted to permit meaningful answers whether patient, family, or health professional respondent, but merging perspectives precluded granular analysis of role. While the survey used a mix of open and closed-ended questions, further exploration with in-depth interviews and a guiding theoretical framework may have led to a more nuanced understanding of study concepts. Finally, although the contributors have significant experience in survey development, the survey instrument was developed de novo and is unvalidated.
5. Conclusion
Perceived barriers in providing tracheostomy care during COVID-19 take many forms, from PPE availability and communicating with individuals with tracheostomy to disruptions in hospital teamwork. Communication difficulties emerged as the prime challenge during tracheostomy care, stressing the acute need to prioritize this problem. Interventions at the hospital unit level can alleviate many of these challenges but require steadfast institutional leadership and collaboration across disciplines. Efforts to continually assess the barriers to safe and effective tracheostomy care among healthcare workers and families should continue to be a priority.
The following is the supplementary data related to this article.
Funding
This study was funded by The National Institutes of Health [grant number 5-R017433], and the Uniformed Services University of the Health Sciences, TriService Nursing Research Program [grant number 11052-N2103GR].
Disclaimer
This research was sponsored by the TriService Nursing Research Program, Uniformed Services University of the Health Sciences; however, the information or content and conclusions do not necessarily represent the official position or policy of, nor should any official endorsement be inferred by, the TriService Nursing Research Program, the Uniformed Services University of the Health Sciences, the Department of Defense, or the U.S. Government.
References
- 1.Angel L.F., et al. Percutaneous dilational tracheostomy for coronavirus disease 2019 patients requiring mechanical ventilation. Crit Care Med. 2021;49(7):1058–1067. doi: 10.1097/CCM.0000000000004969. [DOI] [PubMed] [Google Scholar]
- 2.Bier-Laning C., et al. Tracheostomy during the COVID-19 pandemic: comparison of international perioperative care protocols and practices in 26 countries. Otolaryngol Head Neck Surg. 2021;164(6):1136–1147. doi: 10.1177/0194599820961985. [DOI] [PubMed] [Google Scholar]
- 3.Hernandez G., et al. Early tracheostomy for managing ICU capacity during the COVID-19 outbreak: a propensity-matched cohort study. Chest. 2021;S0012-3692(21):01125–01129. doi: 10.1016/j.chest.2021.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Livneh N., et al. Early vs. Late tracheostomy in ventilated COVID-19 patients - a retrospective study. Am J Otolaryngol. 2021;42(6) doi: 10.1016/j.amjoto.2021.103102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahmood K., et al. Tracheostomy for COVID-19 respiratory failure: multidisciplinary, multicenter data on timing, technique, and outcomes. Ann Surg. 2021;274(2):234–239. doi: 10.1097/SLA.0000000000004955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rozenblat T., et al. The value of tracheostomy of critically ill COVID-19 patients - a multicentral study. Am J Otolaryngol. 2021;43(1) doi: 10.1016/j.amjoto.2021.103230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCormick M.E., et al. Life after tracheostomy: patient and family perspectives on teaching, transitions, and multidisciplinary teams. Otolaryngol Head Neck Surg. 2015;153(6):914–920. doi: 10.1177/0194599815599525. [DOI] [PubMed] [Google Scholar]
- 8.Nakarada-Kordic I., et al. A systematic review of patient and caregiver experiences with a tracheostomy. Patient. 2018;11(2):175–191. doi: 10.1007/s40271-017-0277-1. [DOI] [PubMed] [Google Scholar]
- 9.Pritchett C.V., et al. Inpatient nursing and parental comfort in managing pediatric tracheostomy care and emergencies. JAMA Otolaryngol Head Neck Surg. 2016;142(2):132–137. doi: 10.1001/jamaoto.2015.3050. [DOI] [PubMed] [Google Scholar]
- 10.Ward E., Pandian V., Brenner M.J. The primacy of patient-centered outcomes in tracheostomy care. Patient. 2018;11(2):143–145. doi: 10.1007/s40271-017-0283-3. [DOI] [PubMed] [Google Scholar]
- 11.Haines K.J., et al. Transitions of care after critical illness-challenges to recovery and adaptive problem solving. Crit Care Med. 2021;49(11):1923–1931. doi: 10.1097/CCM.0000000000005095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allgood S., et al. Acquired laryngeal and subglottic stenosis following COVID-19-preparing for the coming deluge. J Clin Nurs. 2021;00:1–5. doi: 10.1111/jocn.15992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meister K.D., et al. Multidisciplinary safety recommendations after tracheostomy during COVID-19 pandemic: state of the art review. Otolaryngol Head Neck Surg. 2021;164(5):984–1000. doi: 10.1177/0194599820961990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGrath B.A., et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8(7):717–725. doi: 10.1016/S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond N.E., et al. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers' depression, anxiety, and stress levels. Aust Crit Care. 2021;34(2):146–154. doi: 10.1016/j.aucc.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elliott R., et al. Critical care health professionals’ self-reported needs for wellbeing during the COVID-19 pandemic: a thematic analysis of survey responses. Aust Crit Care. 2021;S1036-7314(21):00133–00138. doi: 10.1016/j.aucc.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.2021 NSI National Health Care Retention & RN Staffing Report. 2021. https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf [cited 2021 November 8]; Available from:
- 18.Bedwell J.R., et al. Multidisciplinary tracheostomy care: how collaboratives drive quality improvement. Otolaryngol Clin North Am. 2019;52(1):135–147. doi: 10.1016/j.otc.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Brenner M.J., et al. Global tracheostomy collaborative: data-driven improvements in patient safety through multidisciplinary teamwork, standardisation, education, and patient partnership. Br J Anaesth. 2020;125(1):e104–e118. doi: 10.1016/j.bja.2020.04.054. [DOI] [PubMed] [Google Scholar]
- 20.McGrath B.A., et al. Improving tracheostomy care in the United Kingdom: results of a guided quality improvement programme in 20 diverse hospitals. Br J Anaesth. 2020;125(1):e119–e129. doi: 10.1016/j.bja.2020.04.064. [DOI] [PubMed] [Google Scholar]
- 21.Freeman-Sanderson A., Rose L., Brodsky M.B. Coronavirus disease 2019 (COVID-19) cuts ties with patients' outside world. Aust Crit Care. 2020;33(5):397–398. doi: 10.1016/j.aucc.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tolotti A., et al. The communication experience of tracheostomy patients with nurses in the intensive care unit: a phenomenological study. Intensive Crit Care Nurs. 2018;46:24–31. doi: 10.1016/j.iccn.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Brodsky M.B., Freeman-Sanderson A., Brenner M.J. Voice, swallow, and airway impairment after late tracheostomy: defining features of COVID-19 survivorship. Laryngoscope. 2021;131(7):E2311. doi: 10.1002/lary.29562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haring C.T., et al. Effect of augmentative technology on communication and quality of life after tracheostomy or total laryngectomy. Otolaryngol Head Neck Surg. 2021;00:1–6. doi: 10.1177/01945998211013778. 1945998211013778. [DOI] [PubMed] [Google Scholar]
- 25.Martin K.A., et al. Standard versus accelerated speaking valve placement after percutaneous tracheostomy: a randomized controlled feasibility study. Ann Am Thorac Soc. 2021;18(10):1693–1701. doi: 10.1513/AnnalsATS.202010-1282OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zaga C.J., et al. Speech-language pathology guidance for tracheostomy during the COVID-19 pandemic: an international multidisciplinary perspective. Am J Speech Lang Pathol. 2020;29(3):1320–1334. doi: 10.1044/2020_AJSLP-20-00089. [DOI] [PubMed] [Google Scholar]
- 27.Pandian V., et al. Speech and safety in tracheostomy patients receiving mechanical ventilation: a systematic review. Am J Crit Care. 2019;28(6):441–450. doi: 10.4037/ajcc2019892. [DOI] [PubMed] [Google Scholar]
- 28.Rouhani M.J., et al. A prospective study of voice, swallow, and airway outcomes following tracheostomy for COVID-19. Laryngoscope. 2021;131(6):E1918–E1925. doi: 10.1002/lary.29346. [DOI] [PubMed] [Google Scholar]
- 29.Cohen J., Rodgers Y.V.M. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev Med. 2020;141 doi: 10.1016/j.ypmed.2020.106263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ridley E.J., Freeman-Sanderson A., Haines K.J. Surge capacity for critical care specialised allied health professionals in Australia during COVID-19. Aust Crit Care. 2021;34(2):191–193. doi: 10.1016/j.aucc.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karaca T., Altinbas Y., Aslan S. Caring for patients with a tracheostomy at home: a descriptive, cross-sectional study to evaluate health care practices and caregiver burden. Wound Manag Prev. 2019;65(3):22–29. [PubMed] [Google Scholar]
- 32.Brenner M.J., et al. Oral intubation attempts in patients with a laryngectomy: a significant safety threat. Otolaryngol Head Neck Surg. 2021;164(5):1040–1043. doi: 10.1177/0194599820960728. [DOI] [PubMed] [Google Scholar]
- 33.Cognetti D.M., et al. Current state of overlapping, concurrent, and multiple-room surgery in otolaryngology: a National Survey. Otolaryngol Head Neck Surg. 2017;157(6):998–1004. doi: 10.1177/0194599817723897. [DOI] [PubMed] [Google Scholar]
- 34.Cramer J.D., et al. Intraoperative sentinel events in the era of surgical safety checklists: results of a National Survey. OTO Open. 2020;4(4) doi: 10.1177/2473974X20975731. 2473974X20975731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goldman J.L., et al. Mortality and major morbidity after tonsillectomy: etiologic factors and strategies for prevention. Laryngoscope. 2013;123(10):2544–2553. doi: 10.1002/lary.23926. [DOI] [PubMed] [Google Scholar]
- 36.Swords C., et al. Multidisciplinary tracheostomy quality improvement in the COVID-19 pandemic: building a global learning community. Ann Otol Rhinol Laryngol. 2021;130(3):262–272. doi: 10.1177/0003489420941542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xie Y., et al. Adverse events in facial plastic surgery: data-driven insights into systems, standards, and self-assessment. Am J Otolaryngol. 2021;42(1) doi: 10.1016/j.amjoto.2020.102792. [DOI] [PubMed] [Google Scholar]
- 38.Qualtrics software 2020. https://www.qualtrics.com 23 January 2021]; Available from:
- 39.RStudio, PBC; Boston, MA, USA: 2020. RStudio: integrated development for R. [Google Scholar]
- 40.StataCorp . StataCorp LLC; College Station, TX: 2021. Stata Statistical Software: Release 17. [Google Scholar]
- 41.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J Med Internet Res. 2004;6(3) doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Balakrishnan K., et al. COVID-19 pandemic: what every otolaryngologist-head and neck surgeon needs to know for safe airway management. Otolaryngol Head Neck Surg. 2020;162(6):804–808. doi: 10.1177/0194599820919751. [DOI] [PubMed] [Google Scholar]
- 43.Berges A.J., et al. Quantifying viral particle aerosolization risk during tracheostomy surgery and tracheostomy care. JAMA Otolaryngol Head Neck Surg. 2021;147(9):797–803. doi: 10.1001/jamaoto.2021.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brenner M.J., Feller-Kopman D., De Cardenas J. POINT: tracheostomy in patients with COVID-19: should we do it before 14 days?Yes. Chest. 2021;159(5):1723–1727. doi: 10.1016/j.chest.2021.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pandian V., Murgu S., Lamb C.R. COUNTERPOINT: tracheostomy in patients with COVID-19: should we do it before 14 Days?No. Chest. 2021;159(5):1727–1729. doi: 10.1016/j.chest.2020.12.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith J.D., et al. The difficult airway and aerosol-generating procedures in COVID-19: timeless principles for uncertain times. Otolaryngol Head Neck Surg. 2020;163(5):934–937. doi: 10.1177/0194599820936615. [DOI] [PubMed] [Google Scholar]
- 47.Al Omari A., et al. Assessment of the harms and potential benefits of tracheostomy in COVID-19 patients: narrative review of outcomes and recommendations. Am J Otolaryngol. 2021;42(4) doi: 10.1016/j.amjoto.2021.102972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brenner M.J., McGrath B.A., Pandian V. Small steps towards better tracheostomy care during the evolving COVID-19 pandemic. J Intensive Care Med. 2021;36(12):1513–1515. doi: 10.1177/08850666211049087. 8850666211049087. [DOI] [PubMed] [Google Scholar]
- 49.Givi B., et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020;146(6):579–584. doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 50.Schultz M.J., Teng M.S., Brenner M.J. Timing of tracheostomy for patients with COVID-19 in the ICU-setting precedent in unprecedented times. JAMA Otolaryngol Head Neck Surg. 2020;146(10):887–888. doi: 10.1001/jamaoto.2020.2630. [DOI] [PubMed] [Google Scholar]
- 51.Freeman-Sanderson A., et al. A consensus statement for the management and rehabilitation of communication and swallowing function in the ICU: a global response to COVID-19. Arch Phys Med Rehabil. 2021;102(5):835–842. doi: 10.1016/j.apmr.2020.10.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McGrath B.A., Wallace S. The UK National Tracheostomy Safety Project and the role of speech and language therapists. Curr Opin Otolaryngol Head Neck Surg. 2014;22(3):181–187. doi: 10.1097/MOO.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 53.Pandian V., et al. Critical care guidance for tracheostomy care during the COVID-19 pandemic: a global, multidisciplinary approach. Am J Crit Care. 2020;29(6):e116–e127. doi: 10.4037/ajcc2020561. [DOI] [PubMed] [Google Scholar]
- 54.Vizheh M., et al. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. 2020:1–12. doi: 10.1007/s40200-020-00643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Young K.P., et al. Health care workers’ mental health and quality of life during COVID-19: results from a mid-pandemic, national survey. Psychiatr Serv. 2020;72(2):122–128. doi: 10.1176/appi.ps.202000424. [DOI] [PubMed] [Google Scholar]
- 56.Iqbal M.R., Chaudhuri A. COVID-19: results of a national survey of United Kingdom healthcare professionals' perceptions of current management strategy - a cross-sectional questionnaire study. Int J Surg. 2020;79:156–161. doi: 10.1016/j.ijsu.2020.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Halcomb E., et al. The experiences of primary healthcare nurses during the COVID-19 pandemic in Australia. J Nurs Scholarsh. 2020;52(5):553–563. doi: 10.1111/jnu.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yu K., et al. A survey of personal protective equipment use among US otolaryngologists during the COVID-19 pandemic. Am J Otolaryngol. 2020;41(6) doi: 10.1016/j.amjoto.2020.102735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.World Health Organization ICF: International Classification of Functioning, Disability and Health. 2001. https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health
- 60.Pandian V., et al. COVID-19 survivorship: how otolaryngologist-head and neck surgeons can restore quality of life after critical illness. Am J Otolaryngol. 2021;42(3) doi: 10.1016/j.amjoto.2021.102917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Santos R.E.A., et al. Onset and duration of symptoms of loss of smell/taste in patients with COVID-19: a systematic review. Am J Otolaryngol. 2021;42(2) doi: 10.1016/j.amjoto.2020.102889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hopkins C., et al. Early recovery following new onset anosmia during the COVID-19 pandemic - an observational cohort study. J Otolaryngol Head Neck Surg. 2020;49(1):26. doi: 10.1186/s40463-020-00423-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Martin-Martinez A., et al. COVID-19 is associated with oropharyngeal dysphagia and malnutrition in hospitalized patients during the spring 2020 wave of the pandemic. Clin Nutr. 2021;S0261-5614(21) doi: 10.1016/j.clnu.2021.06.010. 00297–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hess D.R. Facilitating speech in the patient with a tracheostomy. Respir Care. 2005;50(4):519–525. [PubMed] [Google Scholar]
- 65.Freeman-Sanderson A.L., et al. Quality of life improves for tracheostomy patients with return of voice: a mixed methods evaluation of the patient experience across the care continuum. Intensive Crit Care Nurs. 2018;46:10–16. doi: 10.1016/j.iccn.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 66.Rosenbluth G., et al. Communicating effectively with hospitalized patients and families during the COVID-19 pandemic. J Hosp Med. 2020;15(7):440–442. doi: 10.12788/jhm.3466. [DOI] [PubMed] [Google Scholar]
- 67.Wong C.K., et al. Effect of facemasks on empathy and relational continuity: a randomised controlled trial in primary care. BMC Fam Pract. 2013;14:200. doi: 10.1186/1471-2296-14-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Houchens N., Tipirneni R. Compassionate communication amid the COVID-19 pandemic. J Hosp Med. 2020;15(7):437–439. doi: 10.12788/jhm.3472. [DOI] [PubMed] [Google Scholar]
- 69.Ten Hoorn S., et al. Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Crit Care. 2016;20(1):333. doi: 10.1186/s13054-016-1483-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pandian V., et al. Optimizing communication in mechanically ventilated patients. J Med Speech Lang Pathol. 2014;21(4):309–318. [PMC free article] [PubMed] [Google Scholar]
- 71.Rose L., et al. Interventions to enable communication for adult patients requiring an artificial airway with or without mechanical ventilator support. Cochrane Database Syst Rev. 2021;10 doi: 10.1002/14651858.CD013379.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Marshall A.P., et al. A critical care pandemic staffing framework in Australia. Aust Crit Care. 2021;34(2):123–131. doi: 10.1016/j.aucc.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mayo A.T. Teamwork in a pandemic: insights from management research. BMJ Leader. 2020;4:53–56. [Google Scholar]
- 74.Mitchell R., et al. Balancing cognitive diversity and mutual understanding in multidisciplinary teams. Health Care Manage Rev. 2017;42(1):42–52. doi: 10.1097/HMR.0000000000000088. [DOI] [PubMed] [Google Scholar]