Abstract
Background:
Previous Canadian studies have identified problems regarding health care access for transgender (trans) and nonbinary people, but all-ages national data have been lacking. This study describes access to care among trans and nonbinary people in Canada, and compares health care access across provinces or regions.
Methods:
We conducted a bilingual, multimode cross-sectional survey (Trans PULSE Canada) from July 26 to Oct. 1, 2019. We recruited trans and nonbinary people aged 14 years and older using convenience sampling. We assessed 5 outcomes: having a primary care provider, having a primary care provider with whom the respondent was comfortable discussing trans health issues, past-year unmet health care need, medical gender affirmation status, and being on a wait-list to access gender-affirming medical care. Average marginal predictions were estimated from multivariable logistic regression models with multiply imputed data.
Results:
The survey included 2873 participants, and 2217 surveys were analyzed after exclusions. Of the 2217 trans and nonbinary respondents, most had a primary care provider (n = 1803; 81.4%, 95% confidence interval [CI] 79.8%–83.0%), with model-predicted probabilities from 52.1% (95% CI 20.2%–84.1%) in the territories to 92.9% (95% CI 83.5%–100.0%) in Newfoundland and Labrador. Of the respondents, 52.3% (n = 1150; 95% CI 50.3%–54.2%) had a primary care provider with whom they were comfortable discussing trans health issues, and 44.4% (n = 978; 95% CI 42.3%–46.4%) reported an unmet health care need. Among participants who needed gender-affirming medical treatment (n = 1627), self-defined treatment completion ranged from an estimated 16.8% (95% CI 0.6%–32.5%) in Newfoundland and Labrador to 59.1% (95% CI 52.5%–65.6%) in Quebec. Of those who needed but had not completed gender-affirming care at the time of the study (n = 1046), 40.7% (n = 416; 95% CI 37.8%–43.6%) were on a wait-list, most often for surgery. These outcomes, with the exception of having a provider with whom one is comfortable discussing trans issues, varied significantly by province or region (p < 0.05).
Interpretation:
Participants reported considerable unmet needs or delays in primary, general and gender-affirming care, with significant regional variation. Our results indicate that, despite efforts toward equity in access to care for trans and nonbinary people in Canada, inequities persist.
The term “transgender” (trans) describes individuals whose gender identities do not match their sex assigned at birth, which can encompass nonbinary identities (identities beyond girl/woman or boy/man).1 Trans and gender nonbinary individuals constitute an estimated 0.1% to 2% of the population globally,2 and 0.35% in the 2019 Canadian Census test.3 Health inequities experienced by trans and nonbinary populations have been increasingly documented over the past decade.4–6 These include higher rates of mental health concerns, driven in part by stigma and discrimination.6 In addition, many trans and nonbinary people require access to gender-affirming medical treatments (e.g., hormones and surgery),7 and completion of such treatment has been associated with reduced suicide risk among trans people in Ontario.8 These health inequities and trans-specific care needs necessitate facilitated health care access for trans and nonbinary communities. Primary care is generally the first engagement point with health care in Canada, including for gender-affirming treatment,9 and many frameworks on social determinants of health place quality health care services as a human right.10
Previous Canadian studies have highlighted problems regarding health care access for trans and nonbinary people. The 2009–2010 Trans PULSE Ontario study found that 17.2% of trans Ontarians did not have a family physician,11 as compared with 9.1% of Ontarians overall in 2011.12 Trans Ontarians were about 3 times more likely to report an unmet health care need when compared with the age-standardized Ontario population (33.2% v. 10.7%).13
Realizable access to gender-affirming care requires that trans and nonbinary people feel able to discuss their health needs with providers. However, among those with a regular family physician, about 37% reported discomfort discussing trans-specific health issues with that physician.14 Relationships with primary care providers are integral to long-term positive health outcomes for trans people. A survey of trans adolescents and young adults in Canada found that having a doctor who was aware of one’s gender identity and feeling comfort with a family doctor were positively associated with general and mental health.15
Existing quantitative data on access to trans health care in Canada largely come from the 2009–2010 Trans PULSE Ontario study.7–9,11,13,14 Much has changed in the intervening decade, including the introduction of province-wide continuing medical education and care navigation initiatives,16,17 and increased coverage for gender-affirming surgical care under provincial and territorial health insurance plans. In addition, as health care is primarily a provincial or territorial responsibility in Canada, it is critical to understand geographic variation in access to care for trans and nonbinary people. However, there is a paucity of national data on trans and nonbinary adolescents and adults.
Drawing on data from an all-ages, comprehensive national survey of trans and nonbinary people in Canada, this research describes access to primary, general and gender-affirming care among trans and nonbinary participants and compares access by province or region.
Methods
Study design
Trans PULSE Canada was a national, community-based research study on the health of transgender and gender nonbinary (collectively, “trans”) adolescents and adults in Canada, conducted in 2019. In addition to providing national and regional data, the study was designed to gather policy- and program-relevant information on 9 priority population subgroups within trans communities: Indigenous gender-diverse people, racialized people, immigrants, sex workers, people living in rural or remote areas, older adults, youth, nonbinary people and people with disabilities.
Data were collected through a multimode convenience sampling survey that could be completed in English or French online (an open survey posted on the study website), via paper copy (mailed out with a self-addressed, stamped return envelope), on an electronic tablet with 1 of 11 peer research associates, or by telephone (with or without a language interpreter in 1 of 98 languages).
The current analysis focuses on items from the sections of the survey on access to primary and gender-affirming care.
Setting and participants
Survey recruitment and data collection occurred from July 26 to Oct. 1, 2019. The target sample size was 3000. Eligible participants were 14 years of age or older, were living in Canada and indicated that their gender identity differed from their sex assigned at birth. The minimum age was set at 14 as it was thought that the same questionnaire would not be developmentally appropriate for younger youth.
The survey was promoted online (e.g., through mailing lists and social media), in person at sexual and gender minority–focused community spaces and events (e.g., pride festivals), and through outreach by peer research associates in Vancouver, Calgary, Edmonton, Saskatoon, Winnipeg, Southwestern Ontario, the Greater Toronto Area, downtown Toronto, Ottawa and Montréal. Peer research associates were well-connected trans and nonbinary community members hired through an open call and trained in person by the principal investigators. Promotional materials (available at https://transpulsecanada.ca/promotional-materials/) and activities targeted the broad trans and nonbinary community as well as the 9 priority populations.
Data collection
Participants were given a choice of response mode, and promotional materials included a toll-free phone number to request a paper copy or telephone survey. Participants were also given the choice of completing the full-length survey (~ 60 min) or a short-form (~ 10 min) containing key items from each section intended for top-line study reports available on the project website.
The electronic (online and tablet) survey was programmed in REDCap18 and preceded by a letter of information and consent; consent was implied by survey completion in all modes. Participants could remain anonymous but were invited to provide contact data for future research opportunities; contact data were stored in a separate secure database. No incentive was provided for participation. Paper surveys were entered into REDCap by a research assistant. Potentially duplicate entries were detected through manual review, and the most complete (or recent) entry was retained; IP addresses were not collected. Incomplete surveys were analyzed unless participants skipped all basic demographic questions (e.g., age, gender and ethnoracial background).
The questionnaire (Appendix 1, available at www.cmajopen.ca/content/9/4/E1213/suppl/DC1) collected information about social determinants of health (e.g., discrimination, social and family support, and gender affirmation), mental and physical health status, and health care access. Only eligibility questions were mandatory. There were between 2 and 8 items per page, depending on survey mode, and items were distributed over 23 (full online version) or 133 pages (full paper version). Participants in the online survey could review and change their previous answers.
For the 2019 survey, the research team adapted core survey items from Trans PULSE Ontario, a province-wide study conducted by members of the research team in 2009–2010.7–9 The 2009 survey was developed by a 10-person community-based research team and revised after reviews by the project’s 16-member Community Engagement Team. Measures were extensively revised to reflect changes in community language (e.g., emergence of nonbinary identities) and improve usability, and measures of some health domains not covered in the 2009–2010 survey were added. As in the earlier Ontario study, core measures were also selected for comparability with Statistics Canada surveys. Finally, over the course of a half-year community engagement process, for each of the 9 priority populations, a team composed of people with relevant lived or professional experience selected additional survey measures specific to each population. Members of the target population pretested the survey for clarity and for functionality of the electronic questionnaire.
Measures
All variables were self-reported. We considered 5 outcomes reflecting access to primary, general and gender-affirming health care: having a primary care provider, having a primary care provider with whom the respondent was comfortable discussing trans health issues, past-year unmet health care need, medical gender affirmation status, and being on a wait-list to access gender-affirming medical care.
“Access to a primary care provider” was coded as yes (v. no) if the participant reported having a current family doctor or nurse practitioner. This item was designed to be indirectly comparable to the 2018 Canadian Community Health Survey (CCHS) question on regular health care providers.19
“Access to a primary care provider with whom the participant feels comfortable discussing trans health issues” was based on previous research from Trans PULSE Ontario14 and coded as yes (v. no) if the participant had a primary care provider and felt very or mostly (v. somewhat or not at all) comfortable discussing trans health issues with the provider.
“Unmet health care need” was coded as yes (v. no) if the participant reported needing but not receiving health care (excluding home care) over the previous 12 months. This item matches the 2018 CCHS question on unmet health care need.19
“Completion of medical gender affirmation” was based on previous research from Trans PULSE Ontario.7 This item was assessed among those who indicated that they needed gender-affirming treatments, such as puberty blockers, hormones or surgery, and was categorized as complete, in process, or planning but not begun.
“On a wait-list for gender-affirming care” was included in the survey based on community consultation. This item was assessed among those who needed but had not completed gender-affirming care and was coded as yes (v. no) if the respondent indicated being on a wait-list for a mental health assessment, puberty blockers, hormones or surgery. In a sub-analysis, we describe the types of care participants were waiting for and median waiting times as of the survey date.
Province or territory was the exposure of interest. To avoid small cell sizes, we grouped together the territories (Northwest Territories, Nunavut and Yukon Territory) and the Maritime provinces (Prince Edward Island, New Brunswick and Nova Scotia). Owing to markedly different crude outcome frequencies, we did not group Newfoundland and Labrador with the Maritime provinces despite this being a part of the Atlantic region.
For comparability across provinces or regions, we adjusted for a set of demographic variables with the goal of standardizing the population structure. Selection of these variables was guided by the model of patient-centred access to care described by Levesque and colleagues;20 in particular, we adjusted for sociodemographic determinants of health service approachability, acceptability, availability, affordability and appropriateness that might vary by (without being caused by) geographic location. Therefore, covariates for all multivariable analyses included age (in years), lived gender (i.e., in day-to-day life,7 self-reported as man or boy, woman or girl, sometimes man/boy, sometimes woman/girl, nonbinary or similar identity), ethnoracial group (Indigenous, non-Indigenous racialized [identified as or were perceived as a person of colour21], or white), rurality (yes v. no, based on postal code), education (less than high school, high school graduate, or any postsecondary education), low-income household (Statistics Canada low-income measure22) and immigration history (born in Canada v. not).
Statistical analysis
We calculated covariate frequencies stratified by province or region in SAS 9.4 (SAS Institute Inc.). Participants who completed the short-form survey, who did not report province or territory of residence, or who were missing data on all outcomes (i.e., who did not complete health care access sections of the questionnaire) were excluded from these analyses.
To avoid bias due to complete-case analysis, in subsequent analyses we used multiple imputation by chained equations, using all variables listed in the Measures section in the imputation models. As the number of imputations should be at least the fraction of incomplete cases,23 we imputed 30 data sets and obtained pooled estimates using mi estimate commands in STATA 16 (StataCorp).
Proportions and 95% confidence intervals (CIs) for the 5 outcomes in the entire study population were estimated using the imputed data. Next, we estimated multivariable logistic regression models for the association between province or region and each outcome (multinomial logistic regression for medical gender affirmation). All 5 multivariable models were adjusted for the full set of covariates described above.
We used the mimrgns package to estimate average marginal predictions and their 95% CIs for each outcome by province or region. These predicted probabilities can be intuitively interpreted as the expected frequency of the outcome were the entire sample to live in the specified province or region. We used postestimation commands to perform F-tests for the overall effect of province or region.
Among participants who indicated being on a wait-list at the time of data collection, we calculated median wait times to date and used Wilcoxon rank-sum tests to explore differences by province or region, as well as sex assigned at birth (for surgery only); these data were not imputed.
The study team developed a set of weights to adjust the full-length survey data to the demographic characteristics of all participants (short and full-length versions). Application of these weights in the current analysis had no appreciable impact on estimated frequencies or regression coefficients, and thus we present unweighted data herein.
Ethics approval
The study was approved by research ethics boards at Western University, Unity Health Toronto and Wilfrid Laurier University.
Results
Of 2873 participants in the Trans PULSE Canada study, 2864 participated online (including at events hosted by peer associates), 3 in interviews with a peer associate, 6 by paper and none by telephone. A total of 266 (9.3%) completed the questionnaire in French, and 2607 (90.7%) participated in English. In total, 2301 (80.1%) participants completed the survey (i.e., submitted the final page).
In the current analysis, from the total number of participants (n = 2873), we excluded 392 who completed the short-form survey, 5 who did not report their province or territory of residence, and 259 who did not complete the health care access sections of the questionnaire. Of the 2217 remaining participants, 15.7% (n = 349) were missing data on at least 1 variable, most often low-income status (n = 205). Participants included in this analysis resided in all provinces and territories except Nunavut. Participant characteristics stratified by province or region are shown in Table 1.
Table 1:
Characteristics of participants included in the analysis, stratified by province or region (n = 2217)
| Characteristic | No. (%) of participants* | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| BC n = 430 |
AB n = 430 |
SK n = 81 |
MB n = 58 |
ON n = 780 |
QC n = 255 |
NL n = 27 |
Maritimes n = 146 |
NWT/YK n = 10 |
|
| Age, yr, median (IQR) | 30 (24–40) | 27 (22–35) | 26 (22–31) | 29 (24–36) | 28 (23–37) | 27 (22–33) | 25 (22–30) | 28 (22–35) | 35 (26–40) |
| Lived gender | |||||||||
| Man or boy | 122 (28.4) | 129 (30.0) | 19 (23.5) | 22 (37.9) | 243 (31.2) | 98 (38.4) | 12 (44.4) | 59 (40.4) | 4 (40.0) |
| Woman or girl | 140 (32.6) | 140 (32.6) | 23 (28.4) | 6 (10.3) | 216 (27.7) | 68 (26.7) | 9 (33.3) | 37 (25.3) | 1 (10.0) |
| Sometimes man/boy, sometimes woman/girl | 18 (4.2) | 31 (7.2) | 8 (9.9) | 4 (6.9) | 49 (6.3) | 4 (1.6) | 1 (3.7) | 11 (7.5) | 0 (0.0) |
| Nonbinary, genderqueer, agender or similar | 150 (34.9) | 129 (30.0) | 31 (38.3) | 26 (44.8) | 268 (34.4) | 85 (33.3) | 5 (18.5) | 39 (26.7) | 5 (50.0) |
| Missing | 0 (0.0) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 4 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Ethnoracial group | |||||||||
| Indigenous | 35 (8.1) | 42 (9.8) | 13 (16.0) | 7 (12.1) | 56 (7.2) | 12 (4.7) | 2 (7.4) | 6 (4.1) | 3 (30.0) |
| Racialized, non-Indigenous | 48 (11.2) | 38 (8.8) | 3 (3.7) | 8 (13.8) | 116 (14.9) | 17 (6.7) | 0 (0.0) | 6 (4.1) | 0 (0.0) |
| White | 343 (79.8) | 347 (80.7) | 65 (80.2) | 43 (74.1) | 600 (76.9) | 222 (87.1) | 25 (92.6) | 132 (90.4) | 7 (70.0) |
| Missing | 4 (0.9) | 3 (0.7) | 0 (0.0) | 0 (0.0) | 8 (1.0) | 4 (1.6) | 0 (0.0) | 2 (1.4) | 0 (0.0) |
| Education | |||||||||
| Less than high school | 47 (10.9) | 58 (13.5) | 12 (14.8) | 3 (5.2) | 59 (7.6) | 27 (10.6) | 1 (3.7) | 13 (8.9) | 3 (30.0) |
| High school | 43 (10.0) | 56 (13.0) | 10 (12.3) | 8 (13.8) | 70 (9.0) | 31 (12.2) | 2 (7.4) | 25 (17.1) | 0 (0.0) |
| Any college or university | 339 (78.8) | 313 (72.8) | 59 (72.8) | 46 (79.3) | 650 (83.3) | 196 (76.9) | 24 (88.9) | 108 (74.0) | 7 (70.0) |
| Missing | 1 (0.2) | 3 (0.7) | 0 (0.0) | 1 (1.7) | 1 (0.1) | 1 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Low-income household | |||||||||
| Yes | 169 (39.3) | 152 (35.3) | 31 (38.3) | 21 (36.2) | 314 (40.3) | 121 (47.5) | 12 (44.4) | 61 (41.8) | 3 (30.0) |
| No | 218 (50.7) | 221 (51.4) | 39 (48.1) | 35 (60.3) | 412 (52.8) | 115 (45.1) | 10 (37.0) | 72 (49.3) | 6 (60.0) |
| Missing† | 43 (10.0) | 57 (13.3) | 11 (13.6) | 2 (3.4) | 54 (6.9) | 19 (7.5) | 5 (18.5) | 13 (8.9) | 1 (10.0) |
| Rural | |||||||||
| Yes | 29 (6.7) | 18 (4.2) | 8 (9.9) | 4 (6.9) | 34 (4.4) | 15 (5.9) | 1 (3.7) | 12 (8.2) | 2 (20.0) |
| No | 394 (91.6) | 400 (93.0) | 71 (87.7) | 53 (91.4) | 725 (92.9) | 231 (90.6) | 25 (92.6) | 131 (89.7) | 8 (80.0) |
| Missing | 7 (1.6) | 12 (2.8) | 2 (2.5) | 1 (1.7) | 21 (2.7) | 9 (3.5) | 1 (3.7) | 3 (2.1) | 0 (0.0) |
| Born in Canada | |||||||||
| Yes | 333 (77.4) | 389 (90.5) | 75 (92.6) | 56 (96.6) | 677 (86.8) | 227 (89.0) | 26 (96.3) | 136 (93.2) | 9 (90.0) |
| No | 94 (21.9) | 39 (9.1) | 5 (6.2) | 2 (3.4) | 95 (12.2) | 28 (11.0) | 1 (3.7) | 10 (6.8) | 1 (10.0) |
| Missing | 3 (0.7) | 2 (0.5) | 1 (1.2) | 0 (0.0) | 8 (1.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Medical gender affirmation | |||||||||
| Complete | 102 (23.7) | 90 (20.9) | 15 (18.5) | 11 (19.0) | 195 (25.0) | 103 (40.4) | 3 (11.1) | 36 (24.7) | 4 (40.0) |
| In process | 167 (38.8) | 131 (30.5) | 26 (32.1) | 24 (41.4) | 254 (32.6) | 43 (16.9) | 10 (37.0) | 58 (39.7) | 2 (20.0) |
| Planning but not begun | 51 (11.9) | 81 (18.8) | 13 (16.0) | 6 (10.3) | 101 (12.9) | 29 (11.4) | 5 (18.5) | 20 (13.7) | 1 (10.0) |
| Not planning or unsure | 99 (23.0) | 116 (27.0) | 26 (32.1) | 16 (27.6) | 206 (26.4) | 67 (26.3) | 9 (33.3) | 26 (17.8) | 2 (20.0) |
| Missing | 11 (2.6) | 12 (2.8) | 1 (1.2) | 1 (1.7) | 24 (3.1) | 13 (5.1) | 0 (0.0) | 6 (4.1) | 1 (10.0) |
Note: AB = Alberta; BC = British Columbia; IQR = interquartile range; Maritimes = New Brunswick, Nova Scotia, Prince Edward Island; MB = Manitoba; NL = Newfoundland and Labrador; NWT/YK = Northwest Territories and Yukon; ON = Ontario; QC = Quebec; SK = Saskatchewan.
Unless stated otherwise.
Including participants aged 14–15 yr who were not asked income questions.
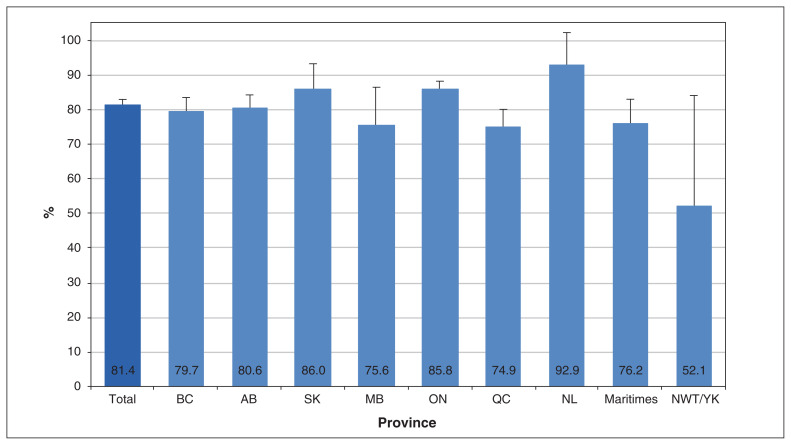
Primary and general health care
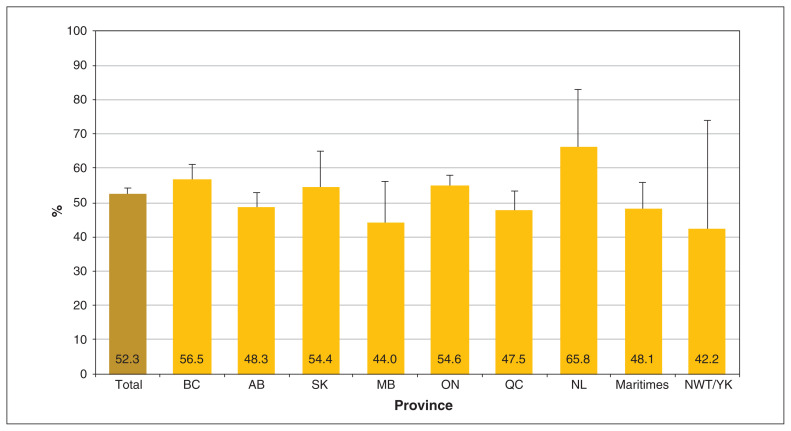
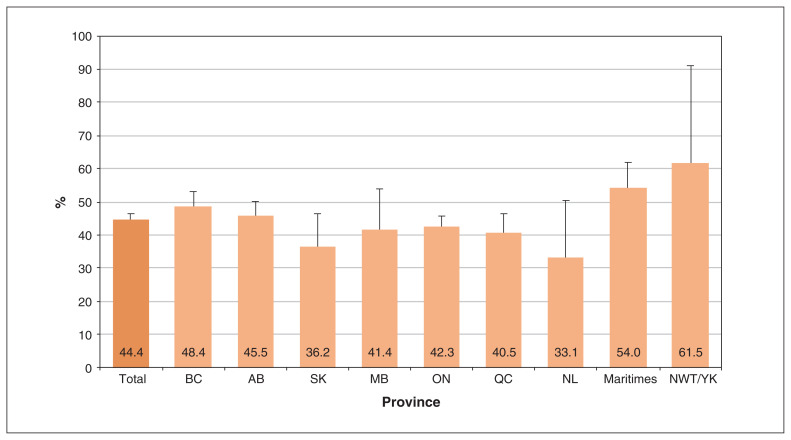
Most Trans PULSE Canada participants had a primary care provider (n = 1803; 81.4%, 95% CI 79.8%–83.0%), with considerable regional variation (Figure 1). The model-predicted probability of having a primary care provider varied significantly by region (p < 0.001), ranging from 52.1% (95% CI 20.2%–84.1%) in the territories to 92.9% (95% CI 83.5%–100.0%) in Newfoundland and Labrador. About half (n = 1150; 52.3%, 95% CI 50.3%–54.2%) of trans and nonbinary participants had a primary care provider with whom they felt mostly or very comfortable discussing trans health issues (Figure 2), with somewhat less variation by region (p = 0.046). Past-year unmet health care need was reported by 44.4% (n = 978; 95% CI 42.3%–46.4%) of participants, with more than one-third predicted to have unmet needs in every province or region (Figure 3; p for province/region = 0.03).
Figure 1:
Adjusted predicted probability of having a primary care provider among Trans PULSE Canada participants (n = 2217), 2019 (adjusted for age, lived gender, ethnoracial group, rurality, education, low-income household and immigration history). Error bars indicate 95% confidence intervals. Note: AB = Alberta; BC = British Columbia; Maritimes = New Brunswick, Nova Scotia, Prince Edward Island; MB = Manitoba; NL = Newfoundland and Labrador; NWT/YK = Northwest Territories and Yukon; ON = Ontario; QC = Quebec; SK = Saskatchewan.
Figure 2:
Adjusted predicted probability of having a primary care provider with whom the respondent is comfortable discussing trans issues, among Trans PULSE Canada participants (n = 2217), 2019 (adjusted for age, lived gender, ethnoracial group, rurality, education, low-income household and immigration history). Error bars indicate 95% confidence intervals. Note: AB = Alberta; BC = British Columbia; Maritimes = New Brunswick, Nova Scotia, Prince Edward Island; MB = Manitoba; NL = Newfoundland and Labrador; NWT/YK = Northwest Territories and Yukon; ON = Ontario; QC = Quebec; SK = Saskatchewan.
Figure 3:
Adjusted predicted probability of past-year unmet health care need among Trans PULSE Canada participants (n = 2217), 2019 (adjusted for age, lived gender, ethnoracial group, rurality, education, low-income household and immigration history). Error bars indicate 95% confidence intervals. Note: AB = Alberta; BC = British Columbia; Maritimes = New Brunswick, Nova Scotia, Prince Edward Island; MB = Manitoba; NL = Newfoundland and Labrador; NWT/YK = Northwest Territories and Yukon; ON = Ontario; QC = Quebec; SK = Saskatchewan.
Gender-affirming health care
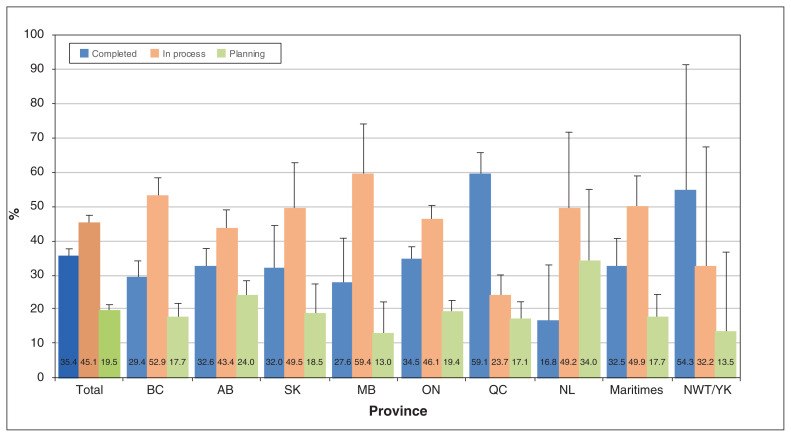
Among participants who needed gender-affirming medical treatments (n = 1627), overall, 35.4% (n = 559; 95% CI 33.3%–37.6%) had completed such care, with predicted probabilities from 16.8% (95% CI 0.6%–32.5%) in Newfoundland and Labrador to 59.1% (95% CI 52.5%–65.6%) in Quebec (Figure 4; p < 0.001).
Figure 4:
Adjusted predicted probabilities for medical gender affirmation status among Trans PULSE Canada participants needing gender-affirming care (n = 1627), 2019 (adjusted for age, lived gender, ethnoracial group, rurality, education, low-income household and immigration history). Error bars indicate 95% confidence intervals. Note: AB = Alberta; BC = British Columbia; Maritimes = New Brunswick, Nova Scotia, Prince Edward Island; MB = Manitoba; NL = Newfoundland and Labrador; NWT/YK = Northwest Territories and Yukon; ON = Ontario; QC = Quebec; SK = Saskatchewan.
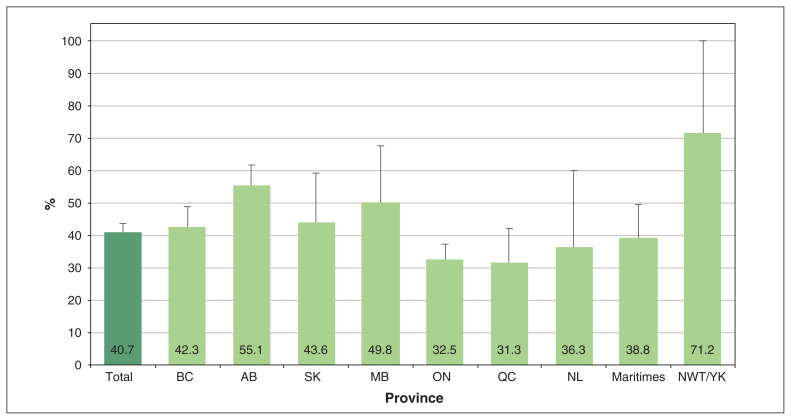
Of those who needed but had not completed gender-affirming care (n = 1046), 40.7% (n = 416; 95% CI 37.8%–43.6%) were on a wait-list for such care at the time of the study (Figure 5; p < 0.001). In Alberta and the territories, more than half of those still needing gender-affirming care were estimated to be on a wait-list. Nationally, of 416 participants on a wait-list for gender-affirming care, 82.0% (n = 341) were waiting for surgery, 14.9% (n = 62) for a mental health assessment, 13.2% (n = 55) for hormone therapy and 0.5% (n = 2) for puberty blockers (results not shown). The median time that participants had been on a wait-list at the time of the survey was 6.0 (interquartile range [IQR] 3.0–12.0) months for surgery, 5.5 (IQR 3.0–11.0) months for mental health assessments and 4.0 (IQR 2.0–6.0) months for hormones. Median time on a wait-list did not vary significantly by province or region (p values ranging from 0.2 to 0.6). Median time on a wait-list for surgery did not vary by sex assigned at birth (p = 0.2).
Figure 5:
Adjusted predicted probability of being on a wait-list for gender-affirming care, among Trans PULSE Canada participants needing but not having completed care (n = 1046), 2019 (adjusted for age, lived gender, ethnoracial group, rurality, education, low-income household and immigration history). Error bars indicate 95% confidence intervals. Note: AB = Alberta; BC = British Columbia; Maritimes = New Brunswick, Nova Scotia, Prince Edward Island; MB = Manitoba; NL = Newfoundland and Labrador; NWT/YK = Northwest Territories and Yukon; ON = Ontario; QC = Quebec; SK = Saskatchewan.
Interpretation
Among 2217 transgender and nonbinary residents of Canada surveyed in 2019, we found suboptimal access to both general and gender-affirming health care services. The geographic distribution of participants in this analysis was broadly similar to that of the Canadian population; however, there was a relatively lower proportion of respondents in Quebec (11.5%) and higher proportions in British Columbia and Alberta (19.4% each).24 Although most participants had a primary care provider, the estimated proportion with a primary care provider was lower than the national average in 2019 (85.5%).25 Realizable access to trans-competent care was less common, with between 42.2% and 65.8% of participants indicating that they had a primary care provider with whom they felt comfortable discussing trans health issues. Overall, 44.4% reported past-year unmet health care needs, far exceeding the CCHS estimate of 5.5% in 2017–2018.26 Comparisons with the general population should be interpreted in light of the younger age distribution of the trans population.10
In Ontario, data are available from a 2009–2010 provincewide respondent-driven sampling study, although results are not directly comparable owing to use of standardization in the present study and our wider age range (≥ 14 yr v. ≥ 16 yr). In the previous study, an estimated 82.8% of trans Ontarians had a family physician, about two-fifths had a primary care provider with whom they felt comfortable discussing trans health issues, and 33.2% had a past-year unmet health care need.11,13,14 Estimates in the current study are not substantially changed from the 2009–2010 data, indicating the persistence of profound inequities in access to care.
Interprovincial and interregional variation in health care access among trans and nonbinary people may reflect differences in provincial health insurance schemes, provider availability and continuing education of health care providers. For example, Quebec had the highest proportion of respondents indicating that they had completed medical gender affirmation, which may be related to the province having both a universal pharmacare program and the country’s largest gender-affirming surgical centre (which was, until recently, the only domestic provider of genital surgeries). Although other provincial and territorial health insurance plans will cover the costs of out-of-province surgery, travel and accommodation are generally the patient’s financial responsibility. Similarly, respondents from Quebec were least likely to be on a waitlist for gender-affirming care, followed by those in Ontario, where Canada’s first hospital-based gender-affirming surgical program is located.
That participants from Newfoundland and Labrador reported the best access to primary care may reflect the availability of a small number of trans-affirming health care providers in the St. John’s region who are sufficient to facilitate access locally, at least for trans and nonbinary individuals connected to trans community networks. Finally, although results should be interpreted cautiously owing to small numbers and wide CIs, respondents from the Yukon and Northwest Territories appeared to fare worse than other trans and nonbinary Canadians.
Future studies should examine reasons for inter-(and intra-) provincial variation in health care access, including qualitative studies and studies focused on providers and system factors, including the characteristics and types of health care delivery models (e.g., team-based v. individual) and health care navigation trajectories that produce better care outcomes. The recent addition of new gender measures to nationally representative surveys, including the CCHS, will permit population-based analyses of interprovincial and interterritorial differences in general health care access, and permit direct assessment of inequalities in comparison to the broader population.
Limitations
Our study has clear limitations. Data were self-reported, and data on wait times may be subject to recall bias; however, trans status is not systematically captured in Canadian health administrative data, and some outcomes (e.g., unmet health care need) can only be self-reported. This nonrandom convenience sample may not be representative of the trans and nonbinary population in Canada. Despite efforts to reduce participation bias (e.g., using a multimode survey) and to use adjustment to standardize the population structure across provinces and regions, regional differences may reflect a combination of true population differences and sampling artifacts. Trans PULSE Canada participants who chose the shorter 10-minute survey were not included in this analysis because they did not provide data on most included variables; however, the addition of weights to adjust for any associated bias had no discernible impact on results. In addition, small samples in some provinces and territories created imprecision in estimates, as indicated by wide CIs. Addressing this through grouping of the Maritimes and territories may obscure heterogeneity across those less populous individual provinces or territories. Provincial and regional estimates may obscure important within-province heterogeneity, such as intersectional inequalities by gender identity and race or ethnicity.11 Finally, we collected data on the time that people currently on wait-lists had been waiting, but not on the total wait time to care.
Conclusion
Since survey data on health care access among trans people in Canada were collected in Ontario in 2009–2010, multiple initiatives to expand and enhance trans health services have been implemented. Nevertheless, the findings of the current survey show that trans and nonbinary people in Canada continue to be medically underserved, with particularly stark levels of unmet health care need and substantial wait times for potentially urgent gender-affirming care. The existence of provincial and regional variation in access to both primary and gender-affirming care underscores the importance of continuing efforts to improve provider training and availability, public insurance coverage (including for travel and all aspects of surgical and pre- and postsurgical care) and care navigation supports for trans and nonbinary people across Canada.
Supplementary Material
Acknowledgements
The authors thank the 2873 trans and nonbinary people who participated in the survey and the more than 100 individuals who contributed to the project. The authors also thank Dr. Julia Temple Newhook for feedback on the interpretation.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Greta Bauer and Ayden Scheim obtained funding. Ayden Scheim conceived the manuscript. Ayden Scheim, Greta Bauer and Todd Coleman drafted the manuscript. Greta Bauer designed the figures. All authors developed the analysis plan, revised the manuscript for important intellectual content, approved the final version to be published and agreed to be accountable for all aspects of the work.
Funding: Trans PULSE Canada was funded by the Canadian Institutes of Health Research (PJT-159690).
Data sharing: As per the participant consent letter, Trans PULSE Canada data can be accessed only by members of the team’s Data Analysis Working Group.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/9/4/E1213/suppl/DC1.
References
- 1.Goldhammer H, Malina S, Keuroghlian AS. Communicating with patients who have nonbinary gender identities. Ann Fam Med. 2018;16:559–62. doi: 10.1370/afm.2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goodman M, Adams N, Corneil T, et al. Size and distribution of transgender and gender Nonconforming populations: a narrative review. Endocrinol Metab Clin North Am. 2019;48:303–21. doi: 10.1016/j.ecl.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Sex at birth and gender: technical report on changes for the 2021 Census. Ottawa: Statistics Canada; [accessed 2021 June 2]. modified 2020 July 17. Available https://www12.statcan.gc.ca/census-recensement/2021/ref/98-20-0002/982000022020002-eng.cfm. [Google Scholar]
- 4.Rich AJ, Scheim AI, Koehoorn M, et al. Non-HIV chronic disease burden among transgender populations globally: a systematic review and narrative synthesis. Prev Med Rep. 2020;20:101259. doi: 10.1016/j.pmedr.2020.101259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scandurra C, Mezza F, Maldonato NM, et al. Health of non-binary and genderqueer people: a systematic review. Front Psychol. 2019;10:1453. doi: 10.3389/fpsyg.2019.01453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reisner SL, Poteat T, Keatley J, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016;388:412–36. doi: 10.1016/S0140-6736(16)00684-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scheim AI, Bauer GR. Sex and gender diversity among transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. J Sex Res. 2015;52:1–14. doi: 10.1080/00224499.2014.893553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bauer GR, Scheim AI, Pyne J, et al. Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada. BMC Public Health. 2015;15:525. doi: 10.1186/s12889-015-1867-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rotondi NK, Bauer GR, Scanlon K, et al. Nonprescribed hormone use and self-performed surgeries: “do-it-yourself” transitions in transgender communities in Ontario, Canada. Am J Public Health. 2013;103:1830–6. doi: 10.2105/AJPH.2013.301348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raphael D, Bryant T, Mikkonen J, et al. Social determinants of health: the Canadian facts. Oshawa (ON): Ontario Tech University Faculty of Health Sciences and Toronto: York University School of Health Policy and Management; 2020. [Google Scholar]
- 11.Scheim AI, Zong X, Giblon R, et al. Disparities in access to family physicians among transgender people in Ontario, Canada. Int J Transgenderism. 2017;18:343–52. [Google Scholar]
- 12.Access to a regular medical doctor. Ottawa: Statistics Canada; 2011. [accessed 2021 Feb. 15]. modified 2013 Feb 11, Available: http://www.statcan.gc.ca/pub/82-625-x/2012001/article/11656-eng.htm. [Google Scholar]
- 13.Giblon R, Bauer GR. Health care availability, quality, and unmet need: a comparison of transgender and cisgender residents of Ontario, Canada. BMC Health Serv Res. 2017;17:283. doi: 10.1186/s12913-017-2226-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bauer GR, Zong X, Scheim AI, et al. Factors impacting transgender patients’ discomfort with their family physicians: a respondent-driven sampling survey. PLoS One. 2015;10:e0145046. doi: 10.1371/journal.pone.0145046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark BA, Veale JF, Greyson D, et al. Primary care access and foregone care: a survey of transgender adolescents and young adults. Fam Pract. 2018;35:302–6. doi: 10.1093/fampra/cmx112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trans Care BC [home page] Vancouver: Provincial Health Services Authority; [accessed 2021 Feb. 15]. Available: http://www.phsa.ca/transcarebc/ [Google Scholar]
- 17.Rainbow Health Ontario [home page] [accessed 2021 Feb. 15]. Available: https://www.rainbowhealthontario.ca.
- 18.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canadian Community Health Survey (CCHS) Ottawa: Statistics Canada; 2018. [accessed 2021 June 2]. modified 2018 Dec 19. Available: https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&a=1&&lang=en&Item_Id=839130. [Google Scholar]
- 20.Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chih C, Wilson-Yang JQ, Dhaliwal K, et al. Report: Health and well-being among racialized trans and non-binary people in Canada. Trans PULSE Canada. 2020. [accessed 2021 June 2]. Available: https://transpulsecanada.ca/results/report-health-and-well-being-among-racialized-trans-and-non-binary-people-in-canada/
- 22.Table 11-10-0232-01: Low income measure (LIM) thresholds by income source and household size. Ottawa: Statistics Canada; [accessed 2021 Feb. 18]. Available https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1110023201. [Google Scholar]
- 23.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–99. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 24.Table 17-10-0005-01: Population estimates on July 1st, by age and sex. Ottawa: Statistics Canada; [accessed 2021 Feb. 15]. Available https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501&pickMembers%5B0%5D=1.3&pickMembers%5B1%5D=2.1&cubeTimeFrame.startYear=2016&cubeTimeFrame.endYear=2020&referencePeriods=20160101%2C20200101. [Google Scholar]
- 25.Primary health care providers. Ottawa: Statistics Canada; 2019. 2020. [accessed 2021 Feb. 15]. Cat no 82-625-X. Available: https://www150.statcan.gc.ca/n1/en/pub/82-625-x/2020001/article/00004-eng.pdf?st=mhbe0C6F. [Google Scholar]
- 26.Canadian Community Health Survey: Public Use Microdata File, 2017/2018. Ottawa: Data Liberation Initiative, Statistics Canada; [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.