Abstract
Background:
Breast cancer screening in Ontario, Canada, was deferred during the first wave of the COVID-19 pandemic, and a prioritization framework to resume services according to breast cancer risk was developed. The purpose of this study was to assess the impact of the pandemic within the Ontario Breast Screening Program (OBSP) by comparing total volumes of screening mammographic examinations and volumes of screening mammographic examinations with abnormal results before and during the pandemic, and to assess backlogs on the basis of adherence to the prioritization framework.
Methods:
A descriptive study was conducted among women aged 50 to 74 years at average risk and women aged 30 to 69 years at high risk, who participated in the OBSP. Percentage change was calculated by comparing observed monthly volumes of mammographic examinations from March 2020 to March 2021 with 2019 volumes and proportions by risk group. We plotted estimates of backlog volumes of mammographic examinations by risk group, comparing pandemic with prepandemic screening practices. Volumes of mammographic examinations with abnormal results were plotted by risk group.
Results:
Volumes of mammographic examinations in the OBSP showed the largest declines in April and May 2020 (> 99% decrease) and returned to prepandemic levels as of March 2021, with an accumulated backlog of 340 876 examinations. As of March 2021, prioritization had reduced the backlog volumes of screens for participants at high risk for breast cancer by 96.5% (186 v. 5469 expected) and annual rescreens for participants at average risk for breast cancer by 13.5% (62 432 v. 72 202 expected); there was a minimal decline for initial screens. Conversely, the backlog increased by 7.6% for biennial rescreens (221 674 v. 206 079 expected). More than half (59.4%) of mammographic examinations with abnormal results were for participants in the higher risk groups.
Interpretation:
Prioritizing screening for those at higher risk for breast cancer may increase diagnostic yield and redirect resources to minimize potential long-term harms caused by the pandemic. This further supports the clinical utility of risk-stratified cancer screening.
As of June 2021, there have been over 178 million cases of COVID-19 and over 3.8 million deaths worldwide. 1 The province of Ontario had recorded more than 542 000 cases and 9000 deaths in the same time period.2 To mitigate the spread of COVID-19 and preserve health system capacity for testing and treatment of COVID-19 cases, in March 2020, the Ontario government directed health care providers to ramp down elective surgeries and nonemergent clinical activities and to cease or reduce to minimal levels all nonessential health care services.3 On Mar. 23, 2020, Ontario Health recommended that all cancer screening services be deferred, and correspondence regarding these services was suspended. Screening services were permitted to resume on May 26, 2020, in accordance with operational public health requirements,3 and correspondence restarted in January 2021.
Among Canadian women, breast cancer is the leading incident cancer and second-leading cause of cancer death.4 Offering women at higher risk more tailored breast screening may improve detection of breast cancer at an early stage and reduce the risk that cancer will be detected between screening examinations. Such cancers, known as interval cancers, are more likely than screen-detected cancers to have a poor prognosis. 5–7 The Ontario Breast Screening Program (OBSP) recommends annual mammographic screening to women aged 50 to 74 years who have certain risk factors that put them at higher than average risk of developing breast cancer.8 As well, the program provides annual magnetic resonance imaging (MRI) in addition to mammographic examinations to women aged 30 to 69 years at high risk for breast cancer.9
Routine data monitoring during the pandemic has shown that there was a substantial decline in screening mammographic examination volumes, and consequently a substantial backlog has accumulated (Rebecca Truscott: personal communication; 2020). Given ongoing capacity constraints due to the gradual resumption of services during the pandemic and the potential risks of deferred screening and cancer diagnosis, a framework to resume breast cancer screening using an approach to prioritize services according to breast cancer risk was developed.10 The framework was based on cancer detection rates in the OBSP (for women at average risk)8 and the High Risk OBSP9 and on screening guidelines.11,12
The purpose of this study was to compare the total screening volumes and the volumes of screens with abnormal results in the OBSP (for women at average risk) and High Risk OBSP before (January 2019 to February 2020) and during the first year of the COVID-19 pandemic (March 2020 to March 2021) on the basis of the recommended framework for screening higher risk groups.10 In addition, the potential impact of adherence to the recommended framework on estimated screening backlogs was examined.
Methods
Design and setting
We conducted a descriptive study to quantify the impact of the COVID-19 pandemic on OBSP total screening volumes and volumes of screens with abnormal results among women aged 50 to 74 years who were at average risk for breast cancer and among women aged 30 to 69 years who were at high risk. Information on screening visits for all women screened within the OBSP was obtained from the program’s Integrated Client Management System (ICMS).
The OBSP has operated since 1990 to deliver a population-based breast screening program to eligible women and has provided digital mammography since 2006.8 The OBSP was expanded in July 2011 to screen women aged 30 to 69 years at high risk for breast cancer with annual mammographic examinations and with MRI examinations (or screening breast ultrasonography if MRI is contraindicated).9 At OBSP sites, quality assurance on equipment exceeds that specified by the Canadian Association of Radiologists’ Mammography Accreditation Program (CAR-MAP), and radiologists and technologists are accredited under CAR-MAP.
Population and screening criteria
Although most women aged 50 to 74 years are screened every 2 years in Ontario, those with certain risk factors that put them at higher risk for breast cancer are screened annually in the OBSP (www.cancercareontario.ca/obsp). Women aged 50 to 74 years are not eligible for screening in the OBSP if they have previously had breast cancer, if they have had a mastectomy, if they have breast implants, if they have breast cancer symptoms or if they have had a screening mammographic examination within the last 11 months; however, some may be eligible for the High Risk OBSP (see criteria outlined below).
Women aged 50 to 74 years are eligible for annual screening in the OBSP if they meet at least 1 of the following criteria: they have a documented pathology of high-risk lesions; they have 2 or more first-degree female relatives with breast cancer at any age; they have 1 first-degree female relative with breast cancer under the age of 50 years; they have 1 first-degree male relative with breast cancer at any age; they have a personal history of ovarian cancer; they have 1 first-degree female relative with ovarian cancer at any age; they have mammographic density equal to or greater than 75% at the time of screening; or the radiologist recommends annual screening at the time of their examination.
Women aged 30 to 69 years are eligible for the High Risk OBSP if they meet at least 1 of the following criteria: they have a deleterious mutation in BRCA1 or BRCA2 or other gene(s) predisposing them to a markedly elevated breast cancer risk; they are an untested first-degree relative of a gene mutation carrier; they have a family history and an estimated personal lifetime breast cancer risk of at least 25%; or they had radiation therapy to the chest before 30 years of age and at least 8 years previously. Women who meet at least 1 of the criteria for the High Risk OBSP are eligible even if they have a history of breast cancer, they have breast implants or they have had a unilateral mastectomy. Women can be referred directly to the High Risk OBSP by their physician if they are known to meet at least 1 of the high-risk criteria or if a genetic assessment of their personal lifetime risk of breast cancer has determined that they are eligible for high-risk breast screening.
Framework for prioritization
A prioritization framework for OBSP mammography services during the COVID-19 pandemic10 was developed by Ontario Health (Cancer Care Ontario), which advises the province on cancer care. It was distributed to OBSP sites in June 2020 and to primary care providers in July 2020 (Table 1). OBSP diagnostic mammography for breast assessment was ranked as priority I. For screening mammography, High Risk OBSP screening mammography was ranked as priority II (initial screens and rescreens). All other OBSP screening mammography (average risk) was ranked as priority III in the following order: initial screens (priority IIIa), annual or 1-year rescreens (priority IIIb), then all other rescreen mammography (priority IIIc), on the basis of the length of screening delay.
Table 1:
Prioritization framework for OBSP mammographic examinations during the COVID-19 pandemic
| Priority | Service | Description |
|---|---|---|
| I | Breast assessments | OBSP diagnostic mammograms should be triaged based on site capacity, in the following order:
|
| II | High Risk OBSP | High Risk OBSP screening mammograms |
| III | OBSP (average risk) | Where capacity challenges exist, screening mammograms should be booked in the following order: |
Note: Reproduced with permission from Ontario Health. BI-RADS = Breast Imaging-Reporting and Data System, OBSP = Ontario Breast Screening Program.
The management of BI-RADS 3 follow-up cases, and prioritization within this framework, is at the discretion of the reporting radiologist.
Annual (ongoing) screening recall recommendation due to family history of breast and/or ovarian cancer or a history of high-risk pathology lesions.
One-year (temporary) screening recall recommendation due to high breast density ≥ 75% or as recommended by the reporting radiologist.
Data sources
Data collected routinely and entered into the ICMS at each visit by OBSP site staff include number of screens, screen date, screen type (initial or rescreen), radiologist findings, and recommendations for further assessment. ICMS accuracy is maintained by online validation and quality checks during data entry, generated audit reports and random chart reviews.
Monthly OBSP screening mammographic examination volumes from January 2019 to March 2021 were stratified by the screen type, in accordance with the framework: high-risk initial screens and rescreens, average-risk initial screens, average-risk annual rescreens (including 1-year rescreens) and average-risk biennial rescreens. An active OBSP site was defined as any site that performed at least 1 screening mammographic examination each month.
Statistical analysis
OBSP screening mammographic examination volumes for women aged 50 to 74 years who were at average risk for breast cancer and women aged 30 to 69 years who were at high risk were included in all analyses. OBSP screening volumes were plotted and percentage change was calculated by comparing the observed monthly mammographic examination volumes from March 2020 to March 2021 with those during the same months in 2019. Proportions of mammographic examination volumes by risk group and screen type were compared for the time periods of January to December 2019 and January to February 2020 (prepandemic), March to May 2020 (service suspension) and June 2020 to March 2021 (service resumption and release of prioritization framework).
Estimated cumulative monthly backlog volumes of screening mammographic examinations were plotted from March 2020 to March 2021, showing prepandemic and pandemic screening practices. Backlog volumes were estimated as the difference between the monthly 2019 volumes and the corresponding volumes for March 2020 to March 2021.
For pandemic screening practices, observed proportions of monthly mammographic examination volumes by risk group were applied. For prepandemic screening practices, the 2019 proportions of monthly mammographic examination volumes for each risk group were assumed (1.8% for screens for women in the high-risk group, 16.7% for initial screens, 21.1% for annual rescreens and 60.4% biennial rescreens for women in the average-risk group). Volumes of screens with abnormal results were also plotted by risk group before (January 2019 to February 2020) and during the pandemic (March 2020 to March 2021).
Ethics approval
This study was granted a waiver from the requirement of ethics review, because it complied with privacy regulations and fell into the category of program evaluation as specified by the University of Toronto Research Ethics Office.
Results
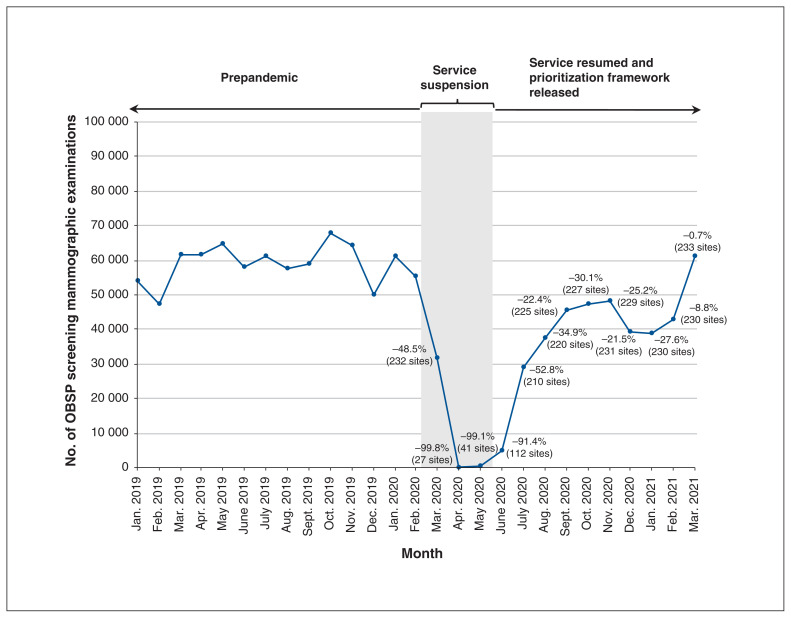
There were 232 OBSP sites operating in March 2020 before the COVID-19 pandemic was declared. This number dropped to 27 in April 2020, but it steadily increased once services resumed to 233 sites by March 2021, as a new site was added in 2020 (Figure 1). OBSP mammographic examination volumes began to decline sharply in March 2020 (−48.5%), with the largest reductions recorded in April (−99.8%) and May (−99.1%) as compared with 2019 volumes for those months. Volumes began to increase in June 2020 and returned to prepandemic levels by March 2021.
Figure 1:
Monthly volumes of OBSP screening mammographic examinations (January 2019 to March 2021) with percentage change from 2019 volumes for the period March 2020 to March 2021. OBSP = Ontario Breast Screening Program.
Volumes of screening mammographic examinations by risk group
There were 426 967 screening mammographic examinations performed during the pandemic from March 2020 to March 2021 (Table 2, Table 3). The proportion of screens in the High Risk OBSP (priority II) increased from 1.9% in March 2020 to 11.8% in May 2020 and 9.4% in June 2020, remaining at greater than 2% throughout the pandemic study period. The proportion of annual rescreens for women at average risk (priority IIIb) also increased from 19.7% in March 2020 to 24.7% in June 2020, with the greatest increase at 33.3% in March 2021. Although the proportion of initial screens for women at average risk (priority IIIa) decreased slightly to 12.4% in June 2020, volumes increased to 16.2% in March 2021. The proportion of biennial rescreens for women at average risk (priority IIIc) decreased from 61.4% in March to 53.5% in June 2020, and although it increased to 60.5% in October 2020, it later declined to 48.4% in March 2021.
Table 2:
Volumes of screening mammographic examinations in the OBSP before the COVID-19 pandemic (January 2019 to February 2020) and during service suspension (March 2020 to May 2020), by risk group
| Risk group | No. (%) of screening mammographic examinations | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Prepandemic period | Period of service suspension during the pandemic | |||||
|
|
|
|||||
| 2019 n = 706 363 |
Jan. 2020 n = 61 332 |
Feb. 2020 n = 55 167 |
Mar. 2020 n = 31 650 |
Apr. 2020 n = 149 |
May 2020 n = 609 |
|
| High Risk OBSP | ||||||
|
| ||||||
| Initial screens and rescreens (priority II) | 12 366 (1.8) | 1097 (1.8) | 1024 (1.9) | 609 (1.9) | 1 (0.7) | 72 (11.8) |
|
| ||||||
| OBSP (average risk) | ||||||
|
| ||||||
| Initial screens (priority IIIa) | 118 134 (16.7) | 10 703 (17.5) | 9798 (17.8) | 5394 (17.0) | 17 (11.4) | 108 (17.7) |
|
| ||||||
| Annual rescreens (priority IIIb) | 149 057 (21.1) | 12 288 (20.0) | 10 583 (19.2) | 6221 (19.7) | 43 (28.9) | 127 (20.9) |
|
| ||||||
| Biennial rescreens (priority IIIc) | 426 806 (60.4) | 37 244 (60.7) | 33 762 (61.2) | 19 426 (61.4) | 88 (59.1) | 302 (49.6) |
Note: OBSP = Ontario Breast Screening Program.
Table 3:
Volumes of screening mammographic examinations in the OBSP after service was resumed and the framework was released (June 2020 to March 2021) and during the total pandemic period (March 2020 to March 2021), by risk group
| Risk group | No. (%) of screening mammographic examinations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Service resumption and release of framework during the pandemic | Total* n = 426 967 |
||||||||||
| June 2020 n = 5005 |
July 2020 n = 28 904 |
Aug. 2020 n = 37 392 |
Sept. 2020 n = 45 556 |
Oct. 2020 n = 47 390 |
Nov. 2020 n = 48 120 |
Dec. 2020 n = 39 096 |
Jan. 2021 n = 39 025 |
Feb. 2021 n = 43 021 |
Mar. 2021 n = 61 050 |
||
| High Risk OBSP | |||||||||||
| Initial screens and rescreens (priority II) | 472 (9.4) | 1294 (4.5) | 1325 (3.5) | 1519 (3.3) | 1412 (3.0) | 1487 (3.1) | 1334 (3.4) | 1273 (3.3) | 1186 (2.8) | 1272 (2.1) | 13 256 (3.1) |
| OBSP (average risk) | |||||||||||
| Initial screens (priority IIIa) | 621 (12.4) | 4218 14.6) | 5655 (15.1) | 6948 (15.3) | 7522 (15.9) | 7877 (16.4) | 6677 (17.1) | 8063 (20.7) | 8831 (20.5) | 9903 (16.2) | 71 834 16.8) |
| Annual rescreens (priority IIIb) | 1234 (24.7) | 7095 (24.5) | 9028 (24.1) | 10 156 (22.3) | 9774 (20.6) | 10 354 (21.5) | 8151 (20.8) | 7545 (19.3) | 9543 (22.2) | 20 328 (33.3) | 99 599 (23.3) |
| Biennial rescreens (priority IIIc) | 2678 (53.5) | 16 297 (56.4) | 21 384 (57.2) | 26 933 (59.1) | 28 682 (60.5) | 28 402 (59.0) | 22 934 (58.7) | 22 144 (56.7) | 23 461 (54.5) | 29 547 (48.4) | 242 278 56.7) |
Note: OBSP = Ontario Breast Screening Program.
The total pandemic period included in this study (March 2020 to March 2021).
Backlog volumes of screening mammographic examinations by risk group
The cumulative backlog volume was estimated to be 340 876 as of March 2021; however, after the prioritization framework was introduced, the size of the backlog was reduced for annual screening for women at high risk and average risk compared with prepandemic screening practices (Figure 2). The backlog volumes of screening mammographic examinations for women at high risk (priority II) were reduced by 96.5% (186 v. 5469 expected) and the backlog volumes for annual rescreens (priority IIIb) were reduced by 13.5% (62 432 v. 72 202 expected). Conversely, there was a minimal decline in initial screen (priority IIIa) backlog volumes (56 584 v. 57 127 expected) and an increase of 7.6% in biennial rescreen backlog volumes (priority IIIc) (221 674 v. 206 079 expected).
Figure 2:
Estimated monthly backlog volumes of OBSP screening mammographic examinations (March 2020 to March 2021), by risk group. As of March 2021, an estimated backlog of 340 876 screening mammographic examinations had accumulated. After June 2020, the backlog was estimated under 2 scenarios: prepandemic screening practices and pandemic screening practices. OBSP = Ontario Breast Screening Program.
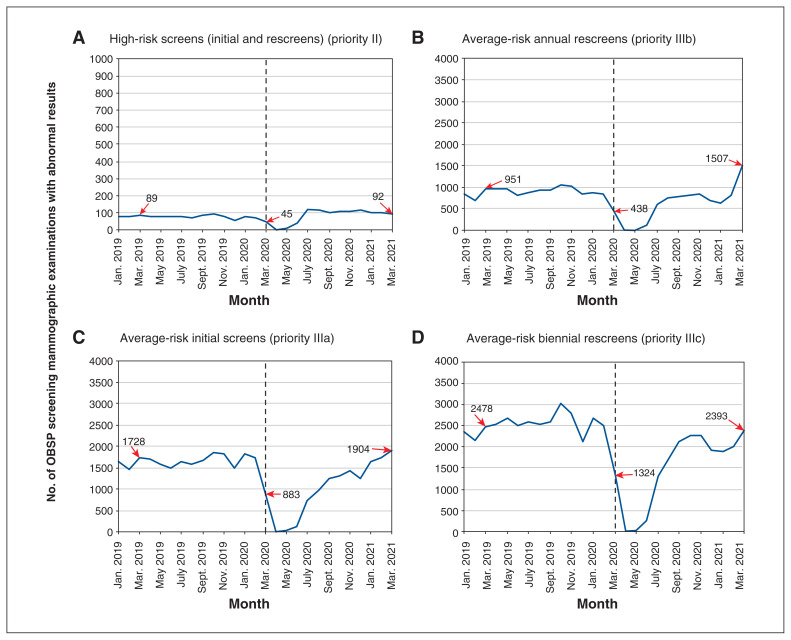
Volumes of screens with abnormal results by risk group
Volumes of screening mammographic examinations with abnormal results showed a pattern similar to that of total screening volumes, with 2690 in March 2020 compared with 5246 in March 2019 (a 48.7% decline) (Figure 3). The volumes then steadily increased by 11.0% to 5896 in March 2021, with a greater proportion for higher risk groups (3503; 59.4%).
Figure 3:
Volume of OBSP screening mammographic examinations with abnormal results (January 2019 to March 2021), by risk group. OBSP = Ontario Breast Screening Program. The individual numbers in the panels are the values at the beginning and end of the pandemic study period (March 2020 and March 2021) and in a comparison month before the pandemic (March 2019).
Interpretation
Early in the COVID-19 pandemic, there was a substantial decline in the volumes of screening mammographic examinations in Ontario: volumes declined by more than 99% during the peak months of the first pandemic wave while services were deferred. Volumes returned to historic levels by March 2021. Similar reductions have been reported in other jurisdictions, including the United Kingdom, the United States and Taiwan.13–15
As of March 2021, we found that an estimated backlog of 340 876 screening mammographic examinations had accumulated, representing almost a third of the 1.1 million screen-eligible people. The majority (221 674; 65%) of the estimated backlog consisted of women at average risk who were on a biennial screening schedule and who were returning for a rescreen. Less than 1% of the backlog consisted of mammographic examinations for participants in the High Risk OBSP.
Patterns consistent with some adherence to the prioritization framework were evident; the shift to a greater proportion of volumes in both screens for participants in the High Risk OBSP and annual rescreens for women at average risk from June 2020 to March 2021 probably reflects the priority given by OBSP sites and primary care providers to participants at higher risk. Although the proportion of initial screens for women at average risk decreased slightly in the early months of the pandemic, both the total screening volumes and the volumes of screens with abnormal results later increased. This may reflect the suspension and then restart of correspondence for women who were turning 50 years of age (who comprise the majority of the women receiving initial screens).
Most importantly, implementation of the prioritization framework reduced the backlog for higher risk groups during the pandemic, with a corresponding increase in the volumes of mammographic examinations with abnormal results. It is well known that women who have a substantial family history,16–18 who have an inherited predisposition,19 who had therapeutic chest radiation before age 3020 or who have extensive mammographic density21,22 are at much higher risk of developing breast cancer. Continuing screening for these women during the pandemic is therefore essential to reduce the potential harms of detecting later stage disease and interval cancers.
One UK modelling study projected increases in avoidable death from breast cancer (7.9%–9.6%) resulting from diagnostic delays because of the pandemic.23 Another study estimated reductions in breast cancer survival associated with a 3-month surgical delay of up to 2.7% for stage I cancers, 5.9% for stage II cancers and 9.8% for stage III cancers, depending on subtype and age.24 In addition, prioritization of higher risk groups may be more efficient, as a recent systematic review found that risk-based screening was more cost-effective than screening based on standard age-based guidelines,25 and several international research consortia are studying the benefit–harm trade-offs.26
One challenge of prioritizing those who are at greater risk for breast cancer is the growth in the backlog of women at average risk who are returning for a biennial rescreen. This study estimated that the cumulative backlog of biennial rescreens may be 206 079, even without prioritization of higher risk groups. Monthly volumes of mammographic examinations with abnormal results began to reach or exceed prepandemic levels in early 2021 as total screening volumes returned to prepandemic levels. This may be partially due to the greater volume of higher risk screens but could also reflect the effects of participants being overdue for screening. However, for participants on a biennial recall schedule, a delay of up to 1 year still falls within the screening interval recommended by the Canadian Task Force on Preventive Health Care (2–3 years for the population aged 50–74 years at average risk).11
Limitations
This study has several strengths, including complete coverage of the Ontario population participating in organized screening and the use of a high-quality, timely breast screening database. However, our comparison of volumes before and during the pandemic has limitations, including that we did not account for other events that may have occurred at the same time as the pandemic or factors such as system and local barriers to increasing resource capacity and participant decisions about undergoing screening. People screened outside of the OBSP were not included, although this would represent a small proportion of all people undergoing breast screening.
As correspondence resumed in January 2021, we were not able to evaluate the full impact of this change. Backlog estimates should also be interpreted carefully as they are based on 2019 prepandemic volumes and risk group distributions and assume compliance with screening recommendations.
Conclusion
As the pandemic is ongoing, this study highlights that adherence to the prioritization of organized screening services for those at higher risk of breast cancer should be maintained along with correspondence. Even though a substantial total backlog persists, prioritization can shift the backlog from higher risk groups to average-risk groups with corresponding increases in the volumes of mammographic examinations with abnormal results. This may ultimately improve diagnostic yield and redirect resources where capacity is constrained to minimize potential long-term harms of the pandemic. Given the emerging evidence on personalized risk-based approaches to early detection of breast cancer, our study results further support the clinical utility of risk-stratified cancer screening.
Supplementary Material
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Anna Chiarelli, Natasha Gray, Gabriela Espino-Hernandez, Julia Gao and Meghan Walker contributed to the acquisition, analysis and interpretation of the data. Anna Chiarelli, Julia Gao, Gabriela Espino-Hernandez and Meghan Walker drafted the manuscript. All of the authors contributed to the conception and design of the work, revised the manuscript critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: This study was conducted with the support of Ontario Health (Cancer Care Ontario) through in-kind contributions.
Data sharing: Ontario Health is prohibited from making the data used in this research publicly accessible if it includes potentially identifiable personal health information and/or personal information as defined in Ontario law, specifically the Personal Health Information Protection Act (PHIPA) and the Freedom of Information and Protection of Privacy Act (FIPPA). Upon request, data de-identified to a level suitable for public release may be provided.
Disclaimer: The opinions, results, views and conclusions reported in this publication are those of the authors and do not necessarily reflect those of Ontario Health (Cancer Care Ontario). No endorsement by Ontario Health (Cancer Care Ontario) is intended or should be inferred.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/9/4/E1205/suppl/DC1.
References
- 1.WHO coronavirus disease (COVID-19) dashboard. Geneva: World Health Organization; [accessed 2021 June 21]. updated 2021 June 21. Available https://covid19.who.int/ [Google Scholar]
- 2.Coronavirus disease (COVID-19): outbreak update. Ottawa: Government of Canada; [accessed 2021 June 21]. updated 2021 June 21. Available: www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html. [Google Scholar]
- 3.COVID-19 — directive #2 for health care providers (regulated health professionals or persons who operate a group practice of regulated health professionals) Toronto: Ministry of Health; [accessed 2020 Oct. 29]. updated 2020 May 26. Available: www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/directives/RHPA_professionals.pdf. [Google Scholar]
- 4.Canadian Cancer Statistics Advisory Committee. Canadian cancer statistics 2019. Toronto: Canadian Cancer Society; 2019. [Google Scholar]
- 5.Gilliland FD, Joste N, Stauber PM, et al. Biologic characteristics of interval and screen-detected breast cancers. J Natl Cancer Inst. 2000;92:743–9. doi: 10.1093/jnci/92.9.743. [DOI] [PubMed] [Google Scholar]
- 6.Chiarelli AM, Edwards SA, Sheppard AJ, et al. Favourable prognostic factors of subsequent screen-detected breast cancers among women aged 50–69. Eur J Cancer Prev. 2012;21:499–506. doi: 10.1097/CEJ.0b013e328350b0f4. [DOI] [PubMed] [Google Scholar]
- 7.Cowan WK, Angus B, Gray JC, et al. A study of interval breast cancer within the NHS breast screening programme. J Clin Pathol. 2000;53:140–6. doi: 10.1136/jcp.53.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chiarelli AM, Blackmore KM, Mirea L, et al. Annual vs biennial screening: diagnostic accuracy among concurrent cohorts within the Ontario Breast Screening Pogram. J Natl Cancer Inst. 2020;112:400–9. doi: 10.1093/jnci/djz131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiarelli AM, Blackmore KM, Muradali D, et al. Performance measures of magnetic resonance imaging plus mammography in the High Risk Ontario Breast Screening Program. J Natl Cancer Inst. 2020;112:136–44. doi: 10.1093/jnci/djz079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.COVID-19 tip sheet for screening and assessment services in the Ontario Breast Screening Program. 13 — guidance for OBSP screening and assessment services — 2020-06-19. Toronto: Ontario Health (Cancer Care Ontario); 2020. [acccessed 2021 Jun. 21]. Available: www.cancercareontario.ca/sites/ccocancercare/files/assets/COVID-19TipSheet13-GuidanceForOntarioBreastScreeningProgramServices.pdf. [Google Scholar]
- 11.Klarenbach S, Sims-Jones N, Lewin G, et al. Recommendations on screening for breast cancer in women aged 40–74 years who are not at increased risk for breast cancer. CMAJ. 2018;190:E1441–51. doi: 10.1503/cmaj.180463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Warner E, Messersmith H, Causer P, et al. Magnetic resonance imaging screening of women at high risk for breast cancer. Toronto: Cancer Care Ontario; 2012. (Evidence-based Series 15-11). [endorsed 2018 Jan] [Google Scholar]
- 13.London JW, Fazio-Eynullayeva E, Palchuk MB, et al. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform. 2020;4:657–65. doi: 10.1200/CCI.20.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Preventive cancer screenings during COVID-19 pandemic. Verona (WI): Epic Health Research Network; 2020. [Google Scholar]
- 15.Peng SM, Yang K, Chan WP, et al. Impact of the COVID-19 pandemic on a population-based breast cancer screening program. Cancer. 2020;126:5202–5. doi: 10.1002/cncr.33180. [DOI] [PubMed] [Google Scholar]
- 16.Collaborative Group on Hormonal Factors in Breast Cancer. Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet. 2001;358:1389–99. doi: 10.1016/S0140-6736(01)06524-2. [DOI] [PubMed] [Google Scholar]
- 17.Pharoah PD, Day NE, Duffy S, et al. Family history and the risk of breast cancer: a systematic review and meta-analysis. Int J Cancer. 1997;71:800–9. doi: 10.1002/(sici)1097-0215(19970529)71:5<800::aid-ijc18>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 18.Bevier M, Sundquist K, Hemminki K. Risk of breast cancer in families of multiple affected women and men. Breast Cancer Res Treat. 2012;132:723–8. doi: 10.1007/s10549-011-1915-2. [DOI] [PubMed] [Google Scholar]
- 19.Claus EB, Schildkraut JM, Thompson WD, et al. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77:2318–24. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2318::AID-CNCR21>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 20.Travis LB, Hill DA, Dores GM, et al. Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA. 2003;290:465–75. doi: 10.1001/jama.290.4.465. [DOI] [PubMed] [Google Scholar]
- 21.Boyd NF, Guo H, Martin LJ, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356:227–36. doi: 10.1056/NEJMoa062790. [DOI] [PubMed] [Google Scholar]
- 22.McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15:1159–69. doi: 10.1158/1055-9965.EPI-06-0034. [DOI] [PubMed] [Google Scholar]
- 23.Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–34. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sud A, Jones ME, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020;31:1065–74. doi: 10.1016/j.annonc.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jayasekera J, Mandelblatt JS. Systematic review of the cost effectiveness of breast cancer prevention, screening, and treatment interventions. J Clin Oncol. 2020;38:332–50. doi: 10.1200/JCO.19.01525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pashayan N, Antoniou A, Ivanus U, et al. Personalized early detection and prevention of breast cancer: ENVISION consensus statement. Nat Rev Clin Oncol. 2020;17:687–705. doi: 10.1038/s41571-020-0388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.