Abstract
Ankylosing spondylitis (AS) is characterized by involvement of the spine and hip joints with progressive stiffness and loss of function. Functional impairment is significant, with spine and hip involvement, and is predominantly seen in the younger age group. Total hip arthroplasty (THA) for fused hips with stiff spines in AS results in considerable improvement of mobility and function. Spine stiffness associated with AS needs evaluation before THA. Preoperative assessment with lateral spine radiographs shows loss of lumbar lordosis. Spinopelvic mobility is reduced with change in sacral slope from sitting to standing less than 10 degrees conforming to the stiff pattern. Care should be taken to reduce acetabular component anteversion at THA in these fused hips, as the posterior pelvic tilt would increase the risk of posterior impingement and anterior dislocation. Fused hips require femoral neck osteotomy, true acetabular floor identification and restoration of the hip center with horizontal and vertical offset to achieve a good functional outcome. Cementless and cemented fixation have shown comparable long-term results with the choice dependent on bone stock at THA. Risks at THA in AS include intraoperative fractures, dislocation, heterotopic ossification, among others. There is significant improvement of functional scores and quality of life following THA in these deserving young individuals with fused hips and spine stiffness.
Keywords: Ankylosing spondylitis, Total hip arthroplasty, Stiff hips, Stiff spine, Spinopelvic mobility, Functional outcome
Core Tip: Progressive spine stiffness associated with stiff hips in ankylosing spondylitis (AS) results in mobility restriction and reduces the quality of life in young individuals. Preoperative planning for total hip arthroplasty (THA) in AS requires spinopelvic mobility assessment. Sacral slope change is reduced (< 10 degrees) with a predominant stuck sitting pattern and posterior pelvic tilt. Care needs to be exercised to reduce acetabular anteversion preventing posterior impingement and anterior dislocation. Risks at THA in AS include intraoperative fractures, postop dislocation (1.9%), heterotopic ossification, among others, with revision-free survivorship of 82% at 20 years. Significant functional and mobility improvement justifies THA in AS with stiff hips and spine.
INTRODUCTION
Ankylosing spondylitis (AS) belongs to the spondyloarthropathy group of disorders affecting the young with progressive stiffness of the spine and hip joints. Inflammation of the spine leads to progressive changes with ankylosis and decreased spinal mobility[1,2]. Chronic inflammation in AS of unknown etiology leads to progressive involvement of the spine, hips, knees, shoulders, among other joints[2-5]. Sacroiliac joints are involved in 100% of AS, followed by lumbosacral spine and cervical spine[4,6]. Hip disease is evident in 19%-36% of AS[4], and shoulder involvement is seen in 20% of the disease[7]. Small joints of the hand are rarely involved[6]. Early hip involvement is marked by synovitis with synovial thickening and increased synovial fluid, as evidenced) by magnetic resonance imaging even in asymptomatic hips with AS[8]. Hip involvement with inflammation and edema is accompanied by involvement of the sacroiliac joint, symphysis pubis and shoulders. Subcortical edema in AS is typical with inflammation of the insertion sites of the tendons, ligaments and capsule, referred to as enthesitis[4]. Inflammation with pathological new bone formation is characteristic of AS with hip and spine involvement. The hip joint radiographs reveal concentric osteoproliferation and acetabular erosion[4]. Synovial and capsular inflammation responsible for pain and decreased movement, with other incompletely specified mechanisms, eventually leads to hip degeneration in AS[4,8]. The hip disease progression seems more significant in males with younger age of onset, eventually requiring total hip arthroplasty (THA)[9-12]. Duration of hip disease in AS is reported as 10-20 years, which is less than duration of AS with spine involvement[4,5,13]. Younger age of onset is associated with more hip disease[4]. Disability is predominantly due to decreased mobility resulting in stiffness and activity restriction. Hip disease is seen largely in the younger age group with significant functional impairment[4,14]. Most AS hips have fixed deformities with stiff spines and loss of spinopelvic mobility. THA improves functional outcome in these patients with significant activity limitations and progressive stiffness in their spine and hips.
THA in AS provides significant improvement in the range of movement with marked improvement in function and mobility[15]. However, the associated risks for consideration are heterotopic ossification (HO), reduced range of movement and re-ankylosis after THA in AS[11].
EPIDEMIOLOGY
The estimated prevalence of Ankylosing Spondylitis (AS) globally is 0.1%-1.4%[16,17] Mean prevalence of 17.6 per 10000 has been reported in Asia[16], with approximately 0.31% (11 to 37.1 per 10,000) reported in China and 7 to 9.8 per 10000 in India[18]. Approximately 25%-50% of patients have hip joint involvement[19], with bilateral hip disease seen in 50%-90% of in AS[12,15,20,21]. Hip involvement in AS varies from 24%-36% according to data reported from Belgium, Spain and South America[4]. Functional impairment predominantly due to hip disease in AS is evident from functional indicator scores such as the Bath Ankylosing Spondylitis Functional Index[1,4]. The Bath Ankylosing Spondylitis Disease Activity Index and other indicators are used in the assessment of functional impairment due to hip disease in AS[4]. Hip involvement presents with varying degrees of stiffness, with bony ankylosis seen in about 40% at THA[22].
CONSIDERATIONS FOR THA IN AS
Progressive hip stiffness is seen in AS results in loss of function and limitation of activities of daily living. Hip stiffness combined with spine stiffness results in significant reduction of mobility. The progressive disease leads to fixed deformities of the hip. The fused hips at THA have flexion, abduction or extension deformities[11,23,24]. The individuals are unable to sit comfortably due to the absence of a normal spinopelvic mobility pattern that occurs from standing to sitting position.
AS with restricted spine and hip mobility presents with advanced disease for THA due to various social and other reasons. There is a significant reduction in the range of movement in these affected hips with fixed flexion and rotational deformities. AS with fused hips and stiff spines causes significant activity restriction and loss of function. The indication for THA is a significant loss of mobility rather than pain[15].
AS patients for THA need preoperative assessment and anesthetic evaluation for optimal perioperative care[15]. Airway, respiratory and cardiovascular status needs preoperative assessment. The medical management with disease-modifying antirheumatic drugs, such as anti-tumor necrosis factor alpha agents, must be stopped with rheumatology input and restarted later to minimize risks associated with wound healing reported at 0.9%[15].
Fused hips with AS have a loss of spinopelvic mobility from the stiffness of the spine and this needs to be recognized before THA for adequate preoperative planning. Preoperative templating is essential to plan for correct acetabular component size and restoration of the hip center. THA with cementless fixation would achieve a good outcome[11,23,25,26], however, cemented fixation would be required in hips with capacious femoral (Dorr C) and poor bone stock[15,21,27]. Cementless acetabular components may require additional screw fixation. Cementless fixation preserves bone stock which, would help in future revisions[15]. The bone stock could be compromised due to significant hip and spine stiffness with prolonged restriction of mobility. Comparison for both cemented and cementless fixation at THA have shown good long-term survivorship in AS[17,28].
APPROACHES FOR THA IN AS
THA in stiff hips with AS have fixed deformities[23]. Flexion deformity is the most common[3,10,11], and an extension abduction deformity occurs rarely[24]. External rotation deformities also coexist indicating contracture of the internal rotators and posterior capsule. The surgical approach for THA should ensure the release of the tight capsular tissue and soft tissue to enable full correction at THA. The flexion deformity would require a comprehensive anterior release while the abduction extension deformities would require the release of the lateral structures including the Iliotibial band
The posterior approach has been the most common in AS[11,15]. The lateral approach has also been used for THA in AS and has been advocated for its lower dislocation rates[29,30]. The modified lateral approach would not compromise the abductors further especially in AS, and this would ensure a comprehensive release in these fused hips with flexion deformity[29-32]. Anterior approach has been reported with favorable outcomes in AS with stiff hips[33,34].
The surgical approach chosen should ensure complete release to correct the fixed deformity in these fused hips without compromising the inherently weak abductors[15]. Trochanteric osteotomy aiding exposure has been associated with increased risk of HO. This approach has been gradually abandoned, although it improves exposure[11,15].
FUSED HIPS
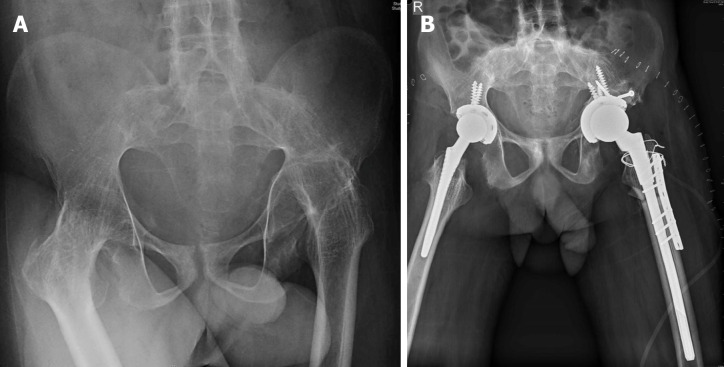
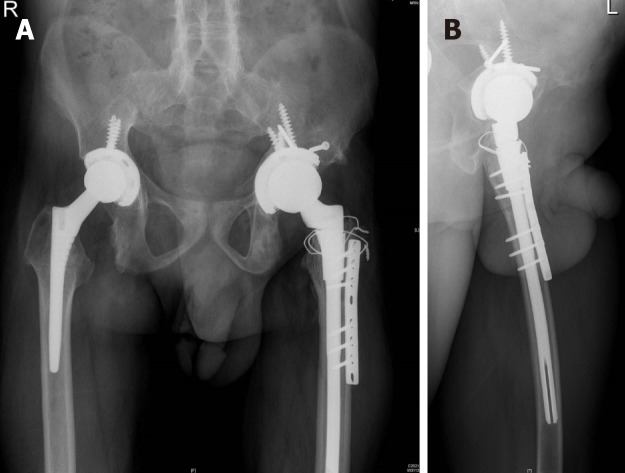
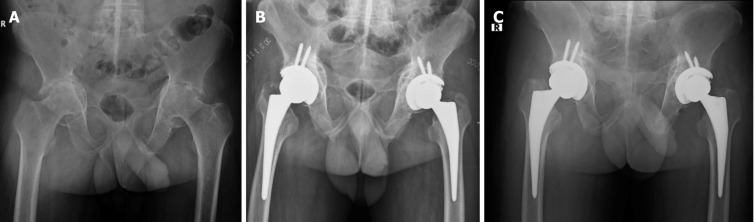
AS with progressive hip stiffness and bilateral hip involvement present as fused hips at THA. Hips with ankylosis require in situ femoral neck osteotomy, identification of acetabular margins, reaming into the femoral head and identification of true acetabular floor to achieve correct acetabular component placement (Figures 1 and 2). Femoral neck osteotomy needs to be done with care to prevent damage to the greater trochanter and the posterior acetabular margin[15]. Identification of the true floor is aided by the pulvinar tissue, with care exercised not to medialize the acetabulum[23]. Hip fusion could present with proximal migration of the hip center requiring restoration of the hip center. Subtrochanteric femoral shortening may be required in fused hips with a high hip center[35] (Figures 3 and 4).
Figure 1.

Bilateral fused hips with ankylosing spondylitis in a 43-year-old male at total hip arthroplasty-pre op.
Figure 2.

Bilateral fused hips-post op bilateral total hip arthroplasty (Pre op Figure 3) with cementless fixation in 43-year-old male.
Figure 3.
Bilateral fused hips and ankylosing spondylitis in a 31-year-old male. A: Proximal migration of the left hip with femoral head and acetabular type 3b acetabular deficiency; B: Bilateral total hip arthroplasty with left hip femoral shortening. Acetabulum medial wall fracture, defect managed with bone graft and screws for superior augmentation. Sacral slope wire for proximal femur incomplete split, femur plate for additional rotational stability.
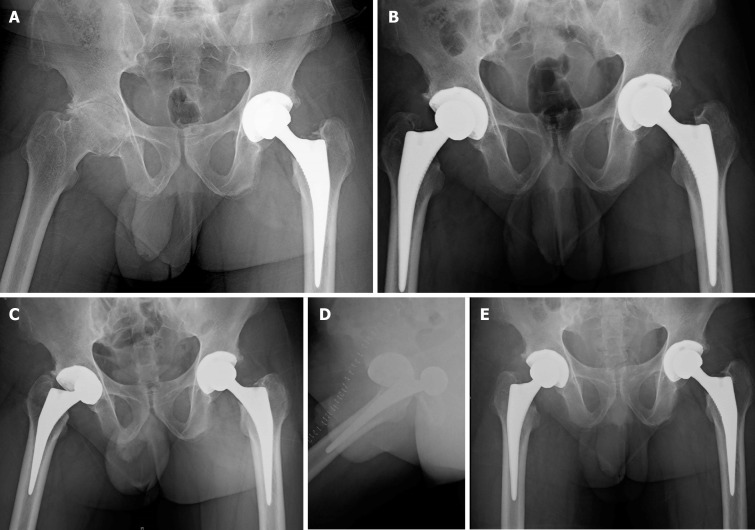
Figure 4.
Follow up bilateral fused hips total hip arthroplasty in 31-year-old male with proximal migration left hip (pre op Figure 3). A: 15 mo follow-up with osteotomy site union, acetabulum graft well united; B: Lateral view confirming osteotomy site union.
SPINE STIFFNESS WITH FUSED HIPS
Spinopelvic movement from standing to sitting is determined by three factors, which include the lumbar spine, spinopelvic mobility and hip flexion[36,37]. Spinopelvic mobility is dependent on sagittal pelvic movement as the anterior pelvic tilt, with lumbar lordosis in the standing position changes to the posterior tilt in the sitting position[38]. Spinopelvic mobility is an essential component in preoperative THA planning, which could lead to early or delayed complications[38-43]. Spinopelvic mobility patterns have also been well described, with recommendations for acetabular component placement at THA[38,39,44]. The preoperative assessment for THA includes a radiological spine assessment, especially with concurrent spinal involvement.
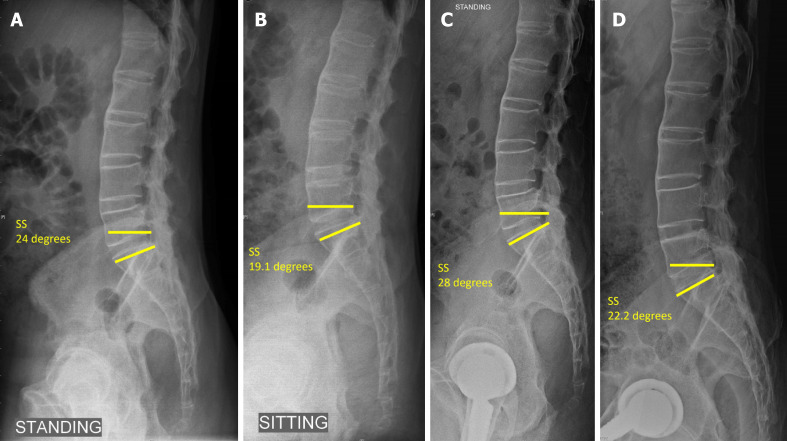
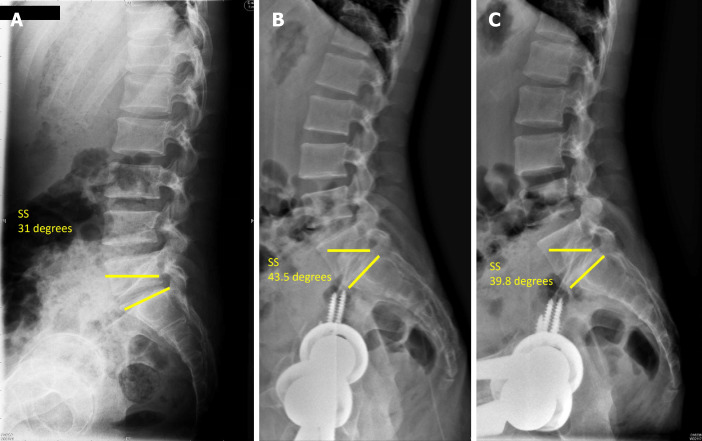
The spine in AS is stiff, and the normal change from sitting to standing is dependent on all three factors that are affected in AS. The change in sacral slope from sitting to standing (< 10 degrees) conforms to the stiff spine pattern[36-38,43]. The stuck sitting pattern with posterior pelvic tilt is common in AS (Figure 5). The stuck standing pattern is not infrequent in AS, as the lumbar spine stiffness may occur with lordosis (Figure 6).
Figure 5.
Lateral lumbosacral spine radiographs. A: Pre op standing; B: Sitting compared to; C: Post op standing; D: Sitting showing the change in sacral slope < 10 degrees with reduced sacral slope indicating posterior pelvic tilt and stuck sitting pattern in ankylosing spondylitis (sacral slope < 30 degrees on sitting and standing typical of stuck sitting pattern). SS: Sacral slope.
Figure 6.
Spinopelvic mobility in a 51-year-old male with flexion deformity and inability to sit comfortably prior to total hip arthroplasty, pre op and 29 mo post bilateral total hip arthroplasty ankylosing spondylitis. A: Pre op sacral slope (SS) standing; B: Post total hip arthroplasty SS standing; C: Sitting SS > 30 degrees sitting and standing demonstrates the stuck standing pattern. SS: Sacral slope.
Spine stiffness and altered spinopelvic mobility coexistent with hip disease in AS at THA has been described[41]. Spinopelvic mobility is gradually lost in these young individuals, with the stiffness of both hips and spine causing significant activity restriction. The posterior pelvic tilt with low pelvic incidence had marginal change (< 10 degrees) before and after THA (Figures 5 and 6) conforms to the stiff pattern. The spinopelvic mobility pattern would fall into the rigid unbalanced category[45].
The stiff spine requires preoperative assessment to evaluate change with THA[36,37,43,46]. Hu et al[47] have recommended correction of thoracolumbar kyphosis before THA. However, most AS individuals with stiff hips and spines undergo THA to achieve improvement in mobility and function. The understanding of the normal hip spine relationship and the different patterns brings out the importance of acetabular component anteversion in THA[36,38-40,45]. Progressive loss of spine mobility is common in AS with the loss of normal spinopelvic mobility. Spine stiffness with stiff hips in AS contributes to loss of spinopelvic mobility from sitting to standing. Preoperative assessment includes lateral radiographs of the lumbosacral spine in sitting and standing positions to evaluate the spinopelvic mobility pattern. Preoperative sitting radiographs may not be possible in AS with stiff hips, as these individuals with significant spine stiffness are often unable to sit with the thighs parallel to the floor.
Acetabular anteversion of 15-25 degrees needs to be reduced in these hips with decreased spinopelvic mobility[17,48]. Posterior pelvic tilt with spine stiffness has an associated risk of posterior impingement with subsequent anterior dislocation. Care should be taken to avoid excessive anteversion as this would increase the risk of posterior impingement and anterior dislocation[42,49]. The normal change in inclination and anteversion from sitting to standing is absent[38-40]. Dual mobility hips have been recommended for fused hips associated with a stiff lumbar spine and posterior pelvic tilt to reduce the risk of impingement and dislocation[38,40].
PROTRUSIO
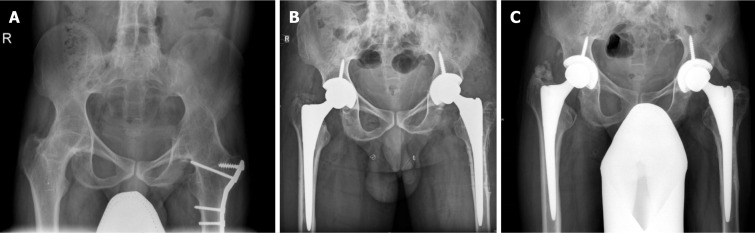
Protrusio in stiff hips is not uncommon in AS. The reason for the medialization of the femoral head beyond the ilioischial line is not fully understood[21,50,51]. Protrusio has been reported in about 17% of hip disease with AS[50]. Preoperative planning includes templating and medial defect bone grafting with reverse reaming for the protrusio with cementless acetabular components. Dislocation of the femoral head during THA in these cases could be challenging, and osteotomy of the neck and head removal may be necessary to avoid intraoperative fractures. The acetabular floor is prepared with caution to prevent medialization, and hip center restoration is essential with autogenous bone grafting and primary cementless acetabular fixation[52] (Figure 7). The protrusio in these hips may present with proximal migration and resorption of the femoral head as well.
Figure 7.
Bilateral hip protrusion in 48-year-old male with ankylosing spondylitis and fused sacroiliac joints. A: Pre op bilateral stiff hips; B: Post op total hip arthroplasty with bone grafting (autograft) reverse reaming for graft impaction; C: 1-year follow-up with graft integration.
FUNCTIONAL OUTCOME
THA in AS with stiff hips restores mobility with significant improvement in activity limitation. The mobility is restored with a significant increase in range of movement and good functional outcome[12,21,25,26,33]. Thirty-six item Short Form Survey scores and health-related quality of life are significantly affected in AS[53]. Functional scores have shown significant improvement for bilateral THA with an average change in HSS scores by 60.6 points reported[15]. Harris Hip Score showed improvement from 48 to 73 and 53 to 82 for historical and recent data in the same series[17] (Table 1). The improvement in functional outcome and quality of life have supported the increased incidence of THA in these stiff hips in AS.
Table 1.
Comparison of outcome of total hip arthroplasty in ankylosing spondylitis
|
Ref.
|
Patients (Hips)
|
Follow up in mo
|
Pain relief (%)
|
Final MHHS
|
ROM score/ Mean flexion
|
Approach
|
Complications (%)
|
| Bisla et al[58], 1976 | 23 (34) | 42.5 | 91 | NS | ROM-3 | NS | 5.88 |
| Resnick et al[59], 1976 | 11 (21) | 36 | NS | NS | NS | NS | 30 re-ankylosis; 6/20 hips |
| Williams et al[60], 1977 | 56 (99) | 36 | NS | NS | NS | NS | 10 |
| Baldursonn et al[61], 1977 | 10 (18) | 45.6 | 94 | NS | Flexion-90 | NS | 0 |
| Shanahan et al[62], 1982 | 12 (16) | 89 | 94 | NS | NS | NS | 6.25 |
| Finsterbush et al[63], 1988 | 23 (35) | 90 | NS | NS | Flexion-86 | NS | 14.28 |
| Walker et al[9], 1991 | 19 (29) | 58 | 97 | NS | ROM-4 | NS | 15; 3 hips re-ankylosis |
| Gualtieri et al[64], 1992 | 39 (73) | 90 | 89 | NS | NS | NS | 0 |
| Brinker et al[10], 1996 | 12 (20) | 75 | 90 | 89.1 | ROM-4 | Posterior, Lateral | 0 |
| Sochart et al[55], 1997 | 24 (43) | 276 | 100 | NS | ROM-4 | NS | 27.9 |
| Lehtimaki et al[56], 2001 | 54 (76) | 240 | NS | NS | NS | NS | 3.94 |
| Joshi et al[27], 2002 | 103 (181) | 120 | 96 | NS | NS | Lateral, Hardinge | 10.5 |
| Kim YL et al[65], 2007 | 12 (24) | 132 | NS | 82.3 | NS | Lateral | 12.5 |
| Bhan et al[11], 2008 | 54 (92) | 102 | 62 | 82.6 | ROM-4 | Posterior | 14 |
| Li et al[66], 2009 | 24 (39) | 36 | NS | 91 | ROM-4 | Posterolateral | 2.5 |
| Tang et al[12], 2000 | 58 (95) | 135.4 | 94 | 88.8 | ROM-4.2 | Posterior | 20 |
| Bangjian et al[54], 2012 | 12 (24) | 50.4 | 100 | 86.25 | Flexion-84 | Posterolateral | 8.3; 2 intraoperative femur fractures; 2 osteolysis, polyethylene wear |
| Malhotra et al[67], 2012 | 23 (32) | 42 | NS | 87.1 | ROM-4 | Posterior | 3.1 |
| Siavashi et al[68], 2014 | 77 (NA) | 12 | NS | 88.22 | ROM-5 | Posterior, lateral | 20.8 |
| Xu et al[26], 2017 | 54 (81) | 42 | NS | 86.1 | Flexion-82.5 | Posterolateral | 0 |
| Guo et al[69], 2019 | 26 (31) | 46.5 | 80.6 | 87.1 | Flexion90.8 | Smith Peterson; lateral, Posterior | 1 dislocation; Closed reduction; 12.9% HO |
| Bukowski BR et al[17], 2021 | 219 (309) | 16 yr (192 mo) | NS | 76 | NS | Transtrochanteric (45%); Posterior (25%); Anterolateral (29%) | 17.5% at 20 yr |
Complications as percentage. Revision, dislocation, fractures, infection. HO: Heterotopic ossification; ROM: Reduced range of movement; MHHS: Modified Harris Hip Score; NS: Not specified.
COMPLICATIONS
AS with stiff hips could present with poor bone stock due to prolonged immobility and stiffness. Care needs to be exercised during THA to prevent intraoperative fractures reported at 4.3%[11,15,27,54]. Wu et al[33] reported 1 case of greater trochanter fracture in their series with DAA for THA in AS. Fracture risk is associated with cementless fixation with inadequate bone stock. Fractures have been reported at femoral stem insertion managed with wiring and delayed weight bearing[15]. Bukowski et al[17] reported 3 proximal femur fractures and 1 acetabular fracture treated with femur wiring and acetabular component retention in their series. Hips for THA with poor bone stock and wide femoral canal (Dorr C) should be planned for cemented fixation. The identification of the medial wall during acetabular preparation and reaming is crucial in achieving the ideal component position at THA in fused hips. Restoration of the hip center with vertical and horizontal offset is essential in achieving THA with a good functional outcome.
Dislocation is a common mode of failure after THA in AS, with earlier reports of 3%-5% at 10 years[11]. Dislocation after THA in AS has been reported at 1.75% managed by closed reduction with successful outcome[15] (Figure 8). Eight dislocations requiring closed reduction were reported in a series of 309 AS hips[17]. Tang et al[12] reported 2 (2 out of 3) anterior dislocations in their series with posterior approach THA, attributed to hip hyperextension. Dislocation has been reported by Bhan et al[11] at 4.3% with the posterior approach and Joshi et al[27] reported a rate of 2.2% with the lateral approach. Wu et al[33] had reported two dislocations in the posterolateral approach when compared to DAA in their series. Cumulative dislocation requiring open or closed reduction has been reported at 1.9% at 2 years and 10 years and 2.9% at 20 years[17]. Dislocation was predominantly posterior with one out of three hips requiring revision with a constrained liner[17].
Figure 8.
Left total hip arthroplasty with right hip arthritis in a 34-year-old male with ankylosing spondylitis. A: Pre op stiff right hip; B: Post op right total hip arthroplasty; C: With dislocation at day 5 following a fall; D: Lateral view; E: 1-year follow-up after closed reduction.
The other complications reported included superficial wound infections requiring oral antibiotics in five hips and hematoma formation in five hips in THA for AS[17].
Nerve injuries have been reported with a slightly higher incidence (2.6%) after bilateral THA for AS[15]. Neuropraxia of the femoral, sciatic and peroneal nerves have been reported with recovery rates between 3 wk and 6 mo.
Long-term survivorship following THA in AS has been reported as 92%-100% at 10 years, with rates falling to 66%-81% at 15 years[12,27,55,56]. Aseptic loosening requiring revision in AS has been reported at 9.7%, 14% and 11% at 16-, 9- and 5-year follow-up, respectively[11,17,21]. Cemented fixation in AS had longer survivorship with lower revision rates compared to cementless fixation, which was considered to have better results[17,28].
HETEROTOPIC OSSIFICATION
The incidence of HO in AS after THA has been reported at 11%-13%, with findings of Brooker class 1 in most hips[21,28]. Brooker 3 or 4 (Figure 9), referred to as clinically relevant HO, was seen in 8% of hips[17]. Data in the literature suggest incidence of HO following THA in AS is 9%-77%[9,10]. Re-ankylosis has also been reported with significant HO following THA in AS associated with a reduced range of movement. Trochanteric osteotomy approach has been attributed to increased incidence of HO and re-ankylosis in earlier reports[3,11,57]. HO following THA in AS is probably due to chronic inflammation seen in the joint as well as the surrounding tissues with varying degrees of stiffness. Indomethacin plays an effective role in HO treatment and prevention in these cases[21]. Careful soft tissue handling and copious lavage to ensure removal of excess bone debris before closure after THA play a significant role in HO prevention in these stiff hips.
Figure 9.
Bilateral hip ankylosis in a 33-year-old male with ankylosing spondylitis. A: Pre op total hip arthroplasty, 12-year post op fracture fixation left proximal femur; B: Post op bilateral total hip arthroplasty; C: Follow-up with Brooker grade 3 heterotopic ossification left hip and good hip function (Harris hip score improved from 34 to 81 at 24 mo follow-up).
CONCLUSION
AS with stiff hips and spine have reduced mobility and function. THA enhances movement and functional activity with significant improvement in outcome. The spinopelvic mobility pattern in AS belongs to the stiff category with minimal change from sitting to standing (< 10 degrees). Preoperative sitting and standing spine lateral radiographs are essential for assessment. THA for fused hips in AS requires in situ femoral neck osteotomy, identification of the true acetabular floor and restoration of hip center, vertical and horizontal offset. Cementless and cemented THA have shown good long-term results. Care should be taken to avoid increased anteversion to avoid posterior impingement and anterior dislocation in fused hips with posterior pelvic tilt. Functional outcome significantly improves in these stiff hips. Risks with THA in AS includes intraoperative fractures (4.3%), dislocation (1.9% to 2.9 %), HO (13%), along with other factors including re-ankylosis (6%) and aseptic loosening (14%).
Stiff hips with spine stiffness in AS warrant THA with knowledge of spinopelvic mobility and overall risks to improve long-term functional outcomes.
Footnotes
Conflict-of-interest statement: The authors declare having no conflict of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: April 2, 2021
First decision: July 28, 2021
Article in press: November 24, 2021
Specialty type: Orthopedics
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cure E S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
Contributor Information
Anil Thomas Oommen, Unit 2, Department of Orthopaedics, Christian Medical College Hospital, Vellore 632004, Tamil Nadu, India. lillyanil@cmcvellore.ac.in.
Triplicane Dwarakanathan Hariharan, Unit 2, Department of Orthopaedics, Christian Medical College Hospital, Vellore 632004, Tamil Nadu, India.
Viruthipadavil John Chandy, Unit 2, Department of Orthopaedics, Christian Medical College Hospital, Vellore 632004, Tamil Nadu, India.
Pradeep Mathew Poonnoose, Unit 2, Department of Orthopaedics, Christian Medical College Hospital, Vellore 632004, Tamil Nadu, India.
Arun Shankar A, Unit 2, Department of Orthopaedics, Christian Medical College Hospital, Vellore 632004, Tamil Nadu, India.
Roncy Savio Kuruvilla, Unit 2, Department of Orthopaedics, Christian Medical College Hospital, Vellore 632004, Tamil Nadu, India.
Jozy Timothy, Unit 2, Department of Orthopaedics, Christian Medical College Hospital, Vellore 632004, Tamil Nadu, India.
References
- 1.Vander Cruyssen B, Vastesaeger N, Collantes-Estévez E. Hip disease in ankylosing spondylitis. Curr Opin Rheumatol. 2013;25:448–454. doi: 10.1097/BOR.0b013e3283620e04. [DOI] [PubMed] [Google Scholar]
- 2.Resnick D. Patterns of peripheral joint disease in ankylosing spondylitis. Radiology. 1974;110:523–532. doi: 10.1148/110.3.523. [DOI] [PubMed] [Google Scholar]
- 3.Sharma G. Hip Replacement in Patients with Ankylosing Spondylitis. Orthop Muscul Syst. 2013;3 [Google Scholar]
- 4.Vander Cruyssen B, Muñoz-Gomariz E, Font P, Mulero J, de Vlam K, Boonen A, Vazquez-Mellado J, Flores D, Vastesaeger N, Collantes E ASPECT-REGISPONSER-RESPONDIA working group. Hip involvement in ankylosing spondylitis: epidemiology and risk factors associated with hip replacement surgery. Rheumatology (Oxford) 2010;49:73–81. doi: 10.1093/rheumatology/kep174. [DOI] [PubMed] [Google Scholar]
- 5.Jang JH, Ward MM, Rucker AN, Reveille JD, Davis JC Jr, Weisman MH, Learch TJ. Ankylosing spondylitis: patterns of radiographic involvement--a re-examination of accepted principles in a cohort of 769 patients. Radiology. 2011;258:192–198. doi: 10.1148/radiol.10100426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forouzesh S, Bluestone R. The clinical spectrum of ankylosing spondylitis. Clin Orthop Relat Res. 1979:53–58. [PubMed] [Google Scholar]
- 7.Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007;369:1379–1390. doi: 10.1016/S0140-6736(07)60635-7. [DOI] [PubMed] [Google Scholar]
- 8.Söker G, Gülek B, Tufan MA, Söker E, Kelle B, Öztürk AB. Early Diagnosis of Hip Joint Involvement of Ankylosing Spondylitis Using Magnetic Resonance Imaging in the Absence of Clinical and X-Ray Findings. Arch Rheumatol. 2014;29:99–104. [Google Scholar]
- 9.Walker LG, Sledge CB. Total hip arthroplasty in ankylosing spondylitis. Clin Orthop Relat Res. 1991:198–204. [PubMed] [Google Scholar]
- 10.Brinker MR, Rosenberg AG, Kull L, Cox DD. Primary noncemented total hip arthroplasty in patients with ankylosing spondylitis. Clinical and radiographic results at an average follow-up period of 6 years. J Arthroplasty. 1996;11:802–812. doi: 10.1016/s0883-5403(96)80180-x. [DOI] [PubMed] [Google Scholar]
- 11.Bhan S, Eachempati KK, Malhotra R. Primary cementless total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis. J Arthroplasty. 2008;23:859–866. doi: 10.1016/j.arth.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Tang WM, Chiu KY. Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthroplasty. 2000;15:52–58. doi: 10.1016/s0883-5403(00)91155-0. [DOI] [PubMed] [Google Scholar]
- 13.Jeong H, Eun YH, Kim IY, Kim H, Lee J, Koh EM, Cha HS. Characteristics of hip involvement in patients with ankylosing spondylitis in Korea. Korean J Intern Med. 2017;32:158–164. doi: 10.3904/kjim.2015.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baraliakos X, Braun J. Hip involvement in ankylosing spondylitis: what is the verdict? Rheumatology (Oxford) 2010;49:3–4. doi: 10.1093/rheumatology/kep298. [DOI] [PubMed] [Google Scholar]
- 15.Lin D, Charalambous A, Hanna SA. Bilateral total hip arthroplasty in ankylosing spondylitis: a systematic review. EFORT Open Rev. 2019;4:476–481. doi: 10.1302/2058-5241.4.180047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dean LE, Jones GT, MacDonald AG, Downham C, Sturrock RD, Macfarlane GJ. Global prevalence of ankylosing spondylitis. Rheumatology (Oxford) 2014;53:650–657. doi: 10.1093/rheumatology/ket387. [DOI] [PubMed] [Google Scholar]
- 17.Bukowski BR, Clark NJ, Taunton MJ, Freedman BA, Berry DJ, Abdel MP. Primary Total Hip Arthroplasty in Patients With Ankylosing Spondylitis. J Arthroplasty . 2021;36:S282–S289. doi: 10.1016/j.arth.2021.01.054. [DOI] [PubMed] [Google Scholar]
- 18.Zhao J, Huang C, Huang H, Pan JK, Zeng LF, Luo MH, Liang GH, Yang WY, Liu J. Prevalence of ankylosing spondylitis in a Chinese population: a systematic review and meta-analysis. Rheumatol Int. 2020;40:859–872. doi: 10.1007/s00296-020-04537-0. [DOI] [PubMed] [Google Scholar]
- 19.Burki V, Gossec L, Payet J, Durnez A, Elhai M, Fabreguet I, Koumakis E, Meyer M, Paternotte S, Roure F, Dougados M. Prevalence and characteristics of hip involvement in spondyloarthritis: a single-centre observational study of 275 patients. Clin Exp Rheumatol. 2012;30:481–486. [PubMed] [Google Scholar]
- 20.Hamadouche M, Kerboull L, Meunier A, Courpied JP, Kerboull M. Total hip arthroplasty for the treatment of ankylosed hips : a five to twenty-one-year follow-up study. J Bone Joint Surg Am. 2001;83:992–998. doi: 10.2106/00004623-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Saglam Y, Ozturk I, Cakmak MF, Ozdemir M, Yazicioglu O. Total hip arthroplasty in patients with ankylosing spondylitis: Midterm radiologic and functional results. Acta Orthop Traumatol Turc. 2016;50:443–447. doi: 10.1016/j.aott.2016.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kubiak EN, Moskovich R, Errico TJ, Di Cesare PE. Orthopaedic management of ankylosing spondylitis. J Am Acad Orthop Surg. 2005;13:267–278. doi: 10.5435/00124635-200507000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Feng DX, Zhang K, Zhang YM, Nian YW, Zhang J, Kang XM, Wu SF, Zhu YJ. Bilaterally Primary Cementless Total Hip Arthroplasty for Severe Hip Ankylosis with Ankylosing Spondylitis. Orthop Surg. 2016;8:352–359. doi: 10.1111/os.12254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gautam D, Malhotra R. Total Hip Arthroplasty in Ankylosing Spondylitis With Extension Contracture of Hips. J Arthroplasty. 2019;34:71–76. doi: 10.1016/j.arth.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 25.Dabir S, Ramanath S, Shah H, Rudramurthy M, Patil SS. Surgical technique and outcome of uncemented THR using HA coated stems in fused and deformed hips due to ankylosing spondylitis. Hip Int. 2015;25:142–145. doi: 10.5301/hipint.5000197. [DOI] [PubMed] [Google Scholar]
- 26.Xu J, Zeng M, Xie J, Wen T, Hu Y. Cementless total hip arthroplasty in patients with ankylosing spondylitis: A retrospective observational study. Medicine (Baltimore) 2017;96:e5813. doi: 10.1097/MD.0000000000005813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joshi AB, Markovic L, Hardinge K, Murphy JC. Total hip arthroplasty in ankylosing spondylitis: an analysis of 181 hips. J Arthroplasty. 2002;17:427–433. doi: 10.1054/arth.2002.32170. [DOI] [PubMed] [Google Scholar]
- 28.Kilgus DJ, Namba RS, Gorek JE, Cracchiolo A, Amstutz HC. Total hip replacement for patients who have ankylosing spondylitis. The importance of the formation of heterotopic bone and of the durability of fixation of cemented components. J Bone Joint Surg Am. 1990;72:834–839. [PubMed] [Google Scholar]
- 29.Peters RM, van Beers LWAH, van Steenbergen LN, Wolkenfelt J, Ettema HB, ten Have BLEF, Rijk PC, Stevens M, Bulstra SK, Poolman RW, Zijlstra WP. Similar Superior Patient-Reported Outcome Measures for Anterior and Posterolateral Approaches After Total Hip Arthroplasty: Postoperative Patient-Reported Outcome Measure Improvement After 3 mo in 12,774 Primary Total Hip Arthroplasties Using the Anterior, Anterolateral, Straight Lateral, or Posterolateral Approach. J Arthroplasty . 2018;33:1786–1793. doi: 10.1016/j.arth.2018.01.055. [DOI] [PubMed] [Google Scholar]
- 30.Pai VS. A modified direct lateral approach in total hip arthroplasty. J Orthop Surg (Hong Kong) 2002;10:35–39. doi: 10.1177/230949900201000107. [DOI] [PubMed] [Google Scholar]
- 31.Mulliken BD, Rorabeck CH, Bourne RB, Nayak N. A modified direct lateral approach in total hip arthroplasty: a comprehensive review. J Arthroplasty. 1998;13:737–747. doi: 10.1016/s0883-5403(98)90024-9. [DOI] [PubMed] [Google Scholar]
- 32.Frndak PA, Mallory TH, Lombardi AV Jr. Translateral surgical approach to the hip. The abductor muscle "split". Clin Orthop Relat Res. 1993:135–141. [PubMed] [Google Scholar]
- 33.Wu H, Cheng WD, Jing J. Total hip arthroplasty by direct anterior approach in the lateral position for the treatment of ankylosed hips. Eur J Orthop Surg Traumatol. 2020;30:993–1001. doi: 10.1007/s00590-020-02655-w. [DOI] [PubMed] [Google Scholar]
- 34.Zhu XB, Yuan LL, Han GS, Han JZ, Zhou JS. [Short term effect of total hip arthroplasty through direct anterior approach for the treatment of ankylosing spondylitis with hip flexion deformity] Zhongguo Gu Shang. 2019;32:141–145. doi: 10.3969/j.issn.1003-0034.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 35.Oommen AT, Chandy VJ, Jeyaraj C, Kandagaddala M, Hariharan TD, Arun Shankar A, Poonnoose PM, Korula RJ. Subtrochanteric femoral shortening for hip centre restoration in complex total hip arthroplasty with functional outcome. Bone Jt Open. 2020;1:152–159. doi: 10.1302/2633-1462.15.BJO-2020-0023.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Innmann MM, Merle C, Gotterbarm T, Ewerbeck V, Beaulé PE, Grammatopoulos G. Can spinopelvic mobility be predicted in patients awaiting total hip arthroplasty? Bone Joint J. 2019;101-B:902–909. doi: 10.1302/0301-620X.101B8.BJJ-2019-0106.R1. [DOI] [PubMed] [Google Scholar]
- 37.Innmann MM, Merle C, Phan P, Beaulé PE, Grammatopoulos G. How Can Patients With Mobile Hips and Stiff Lumbar Spines Be Identified Prior to Total Hip Arthroplasty? J Arthroplasty. 2020;35:S255–S261. doi: 10.1016/j.arth.2020.02.029. [DOI] [PubMed] [Google Scholar]
- 38.Lum ZC, Coury JG, Cohen JL, Dorr LD. The Current Knowledge on Spinopelvic Mobility. J Arthroplasty. 2018;33:291–296. doi: 10.1016/j.arth.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 39.Ike H, Dorr LD, Trasolini N, Stefl M, McKnight B, Heckmann N. Spine-Pelvis-Hip Relationship in the Functioning of a Total Hip Replacement. J Bone Joint Surg Am. 2018;100:1606–1615. doi: 10.2106/JBJS.17.00403. [DOI] [PubMed] [Google Scholar]
- 40.Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R, Dorr LD. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017;99-B:37–45. doi: 10.1302/0301-620X.99B1.BJJ-2016-0415.R1. [DOI] [PubMed] [Google Scholar]
- 41.Blizzard DJ, Penrose CT, Sheets CZ, Seyler TM, Bolognesi MP, Brown CR. Ankylosing Spondylitis Increases Perioperative and Postoperative Complications After Total Hip Arthroplasty. J Arthroplasty. 2017;32:2474–2479. doi: 10.1016/j.arth.2017.03.041. [DOI] [PubMed] [Google Scholar]
- 42.Lazennec JY, Brusson A, Rousseau M-A. Hip-Spine Relations: An Innovative Paradigm in THR Surgery. In: Samo K Fokter, editor. Recent advances in arthroplasty 2012. [Google Scholar]
- 43.Luthringer TA, Vigdorchik JM. A Preoperative Workup of a "Hip-Spine" Total Hip Arthroplasty Patient: A Simplified Approach to a Complex Problem. J Arthroplasty. 2019;34:S57–S70. doi: 10.1016/j.arth.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 44.Kanawade V, Dorr LD, Wan Z. Predictability of Acetabular Component Angular Change with Postural Shift from Standing to Sitting Position. J Bone Joint Surg Am. 2014;96:978–986. doi: 10.2106/JBJS.M.00765. [DOI] [PubMed] [Google Scholar]
- 45.Phan D, Bederman SS, Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J. 2015;97-B:1017–1023. doi: 10.1302/0301-620X.97B8.35700. [DOI] [PubMed] [Google Scholar]
- 46.Morton J, Eftekhary N, Schwarzkopf R, Vigdorchik JM. The spinopelvic relationship made simple: What every hip surgeon needs to know to prevent instability in high-risk patients undergoing total hip arthroplasty. Seminars in Arthroplasty . 2018;29:274–281. [Google Scholar]
- 47.Hu J, Qian BP, Qiu Y, Wang B, Yu Y, Zhu ZZ, Jiang J, Mao SH, Qu Z, Zhang YP. Can acetabular orientation be restored by lumbar pedicle subtraction osteotomy in ankylosing spondylitis patients with thoracolumbar kyphosis? Eur Spine J. 2017;26:1826–1832. doi: 10.1007/s00586-016-4709-8. [DOI] [PubMed] [Google Scholar]
- 48.Lazennec JY, Boyer P, Gorin M, Catonné Y, Rousseau MA. Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res. 2011;469:1103–1109. doi: 10.1007/s11999-010-1732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Esposito CI, Carroll KM, Sculco PK, Padgett DE, Jerabek SA, Mayman DJ. Total Hip Arthroplasty Patients With Fixed Spinopelvic Alignment Are at Higher Risk of Hip Dislocation. J Arthroplasty. 2018;33:1449–1454. doi: 10.1016/j.arth.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 50.Gusis SE, Riopedre AM, Penise O, Maldonado Cocco JA. Protrusio acetabuli in seronegative spondyloarthropathy. Semin Arthritis Rheum. 1993;23:155–160. doi: 10.1016/s0049-0172(05)80036-8. [DOI] [PubMed] [Google Scholar]
- 51.Ries MD. Total hip arthroplasty in acetabular protrusio. Orthopedics. 2009;32 doi: 10.3928/01477447-20090728-12. [DOI] [PubMed] [Google Scholar]
- 52.Mullaji A. Acetabular protrusio: a problem in depth. Orthopaedic Proceedings. 2013:95–30. [Google Scholar]
- 53.Yang X, Fan D, Xia Q, Wang M, Zhang X, Li X, Cai G, Wang L, Xin L, Xu S, Pan F. The health-related quality of life of ankylosing spondylitis patients assessed by SF-36: a systematic review and meta-analysis. Qual Life Res. 2016;25:2711–2723. doi: 10.1007/s11136-016-1345-z. [DOI] [PubMed] [Google Scholar]
- 54.Bangjian H, Peijian T, Ju L. Bilateral synchronous total hip arthroplasty for ankylosed hips. Int Orthop. 2012;36:697–701. doi: 10.1007/s00264-011-1313-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sochart DH, Porter ML. Long-term results of total hip replacement in young patients who had ankylosing spondylitis. Eighteen to thirty-year results with survivorship analysis. J Bone Joint Surg Am. 1997;79:1181–1189. doi: 10.2106/00004623-199708000-00010. [DOI] [PubMed] [Google Scholar]
- 56.Lehtimäki MY, Lehto MU, Kautiainen H, Lehtinen K, Hämäläinen MM. Charnley total hip arthroplasty in ankylosing spondylitis: survivorship analysis of 76 patients followed for 8-28 years. Acta Orthop Scand. 2001;72:233–236. doi: 10.1080/00016470152846538. [DOI] [PubMed] [Google Scholar]
- 57.Wilde AH, Collins HR, Mackenzie AH. Reankylosis of the hip joint in ankylosing spondylitis after total hip replacement. Arthritis Rheum. 1972;15:493–496. doi: 10.1002/art.1780150504. [DOI] [PubMed] [Google Scholar]
- 58.Bisla RS, Ranawat CS, Inglis AE. Total hip replacement in patients with ankylosing spondylitis with involvement of the hip. J Bone Joint Surg Am. 1976;58:233–238. [PubMed] [Google Scholar]
- 59.Resnick D, Dwosh IL, Goergen TG, Shapiro RF, D'Ambrosia R. Clinical and radiographic "reankylosis" following hip surgery in ankylosing spondylitis. AJR Am J Roentgenol. 1976;126:1181–1188. doi: 10.2214/ajr.126.6.1181. [DOI] [PubMed] [Google Scholar]
- 60.Williams E, Taylor AR, Arden GP, Edwards DH. Arthroplasty of the hip in ankylosing spondylitis. J Bone Joint Surg Br. 1977;59-B:393–397. doi: 10.1302/0301-620X.59B4.925047. [DOI] [PubMed] [Google Scholar]
- 61.Baldursson H, Brattström H, Olsson T. Total hip replacement in ankylosing spondylitis. Acta Orthop Scand. 1977;48:499–507. doi: 10.3109/17453677708989738. [DOI] [PubMed] [Google Scholar]
- 62.Shanahan WR Jr, Kaprove RE, Major PA, Hunter T, Baragar FD. Assessment of longterm benefit of total hip replacement in patients with ankylosing spondylitis. J Rheumatol. 1982;9:101–104. [PubMed] [Google Scholar]
- 63.Finsterbush A, Amir D, Vatashki E, Husseini N. Joint surgery in severe ankylosing spondylitis. Acta Orthop Scand. 1988;59:491–496. doi: 10.3109/17453678809148770. [DOI] [PubMed] [Google Scholar]
- 64.Gualtieri G, Gualtieri I, Hendriks M, Gagliardi S. Comparison of cemented ceramic and metal-polyethylene coupling hip prostheses in ankylosing spondylitis. Clin Orthop Relat Res. 1992:81–85. [PubMed] [Google Scholar]
- 65.Kim YL, Shin SI, Nam KW, Yoo JJ, Kim YM, Kim HJ. Total hip arthroplasty for bilaterally ankylosed hips. J Arthroplasty. 2007;22:1037–1041. doi: 10.1016/j.arth.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 66.Li J, Xu W, Xu L, Liang Z. Hip resurfacing arthroplasty for ankylosing spondylitis. J Arthroplasty. 2009;24:1285–1291. doi: 10.1016/j.arth.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 67.Malhotra R, Kannan A, Kumar V, Nagaraj C, Marimuthu K, Khatri D. Hip resurfacing arthroplasty in inflammatory arthritis a 3-to 5-year follow-up study. J Arthroplasty. 2012;27:15–20. doi: 10.1016/j.arth.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 68.Siavashi B, Mohseni N, Zehtab MJ, Ramim T. Clinical outcomes of total hip arthroplasty in patients with ankylosed hip. Arch Bone Jt Surg. 2014;2:25–30. [PMC free article] [PubMed] [Google Scholar]
- 69.Guo HZ, Yang CX, Tang ZP, Wang CX. The effects of total hip arthroplasty in treating hip bony fusion in young and middle-aged patients with ankylosing spondylitis. J Orthop Surg Res. 2019;14:253. doi: 10.1186/s13018-019-1288-5. [DOI] [PMC free article] [PubMed] [Google Scholar]