Key Points
Question
What are the absolute and relative risks of perpetrating violence toward others in individuals with schizophrenia spectrum disorders compared with the general population?
Findings
In this systematic review of 24 studies, the absolute risk of perpetrating violence in a subgroup of register-based studies was less than 1 in 20 in women with schizophrenia spectrum disorders and less than 1 in 4 in men with schizophrenia spectrum disorders over a 35-year period. The elevated relative risk for all violence-perpetration outcomes was higher for women with schizophrenia spectrum disorders than for men with schizophrenia spectrum disorders, but with substantial heterogeneity in the findings.
Meaning
Violence perpetration outcomes may be an important target for prevention and to reduce stigma in people with schizophrenia spectrum disorders.
This systematic review evaluates risk of perpetrating interpersonal violence in individuals with schizophrenia spectrum disorders compared with general population control individuals.
Abstract
Importance
Violence perpetration outcomes in individuals with schizophrenia spectrum disorders contribute to morbidity and mortality at a population level, disrupt care, and lead to stigma.
Objective
To conduct a systematic review and meta-analysis of the risk of perpetrating interpersonal violence in individuals with schizophrenia spectrum disorders compared with general population control individuals.
Data Sources
Multiple databases were searched for studies in any language from January 1970 to March 2021 using the terms violen* or homicid* and psychosis or psychoses or psychotic or schizophren* or schizoaffective or delusional and terms for mental disorders. Bibliographies of included articles were hand searched.
Study Selection
The study included case-control and cohort studies that allowed risks of interpersonal violence perpetration and/or violent criminality in individuals with schizophrenia spectrum disorders to be compared with a general population group without these disorders.
Data Extraction and Synthesis
The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines and the Meta-analyses of Observational Studies in Epidemiology (MOOSE) proposal. Two reviewers extracted data. Quality was assessed using the Newcastle-Ottawa Quality Assessment Scale. Data were pooled using a random-effects model.
Main Outcomes and Measures
The main outcome was violence to others obtained either through official records, self-report and/or collateral-report, or medical file review and included any physical assault, robbery, sexual offenses, illegal threats or intimidation, and arson.
Results
The meta-analysis included 24 studies of violence perpetration outcomes in 15 countries over 4 decades (N = 51 309 individuals with schizophrenia spectrum disorders; reported mean age of 21 to 54 years at follow-up; of those studies that reported outcomes separately by sex, there were 19 976 male individuals and 14 275 female individuals). There was an increase in risk of violence perpetration in men with schizophrenia and other psychoses (pooled odds ratio [OR], 4.5; 95% CI, 3.6-5.6) with substantial heterogeneity (I2 = 85%; 95% CI, 77-91). The risk was also elevated in women (pooled OR, 10.2; 95% CI, 7.1-14.6), with substantial heterogeneity (I2 = 66%; 95% CI, 31-83). Odds of perpetrating sexual offenses (OR, 5.1; 95% CI, 3.8-6.8) and homicide (OR, 17.7; 95% CI, 13.9-22.6) were also investigated. Three studies found increased relative risks of arson but data were not pooled for this analysis owing to heterogeneity of outcomes. Absolute risks of violence perpetration in register-based studies were less than 1 in 20 in women with schizophrenia spectrum disorders and less than 1 in 4 in men over a 35-year period.
Conclusions and Relevance
This systematic review and meta-analysis found that the risk of perpetrating violent outcomes was increased in individuals with schizophrenia spectrum disorders compared with community control individuals, which has been confirmed in new population-based longitudinal studies and sibling comparison designs.
Introduction
Schizophrenia spectrum disorders are associated with a range of adverse outcomes. These include suicide,1 premature mortality,2 experiencing violence3 and contact with the criminal justice system,4 and deficits across broader social domains.5 Perpetration of interpersonal violence is also associated with these diagnoses, an outcome with considerable implications for individuals, families, caregivers, those who experience interpersonal violence, and public services. Examining such associations poses particular challenges. Public perceptions around dangerousness in mental illness can contribute to stigma,6 and a focus on violence risk may inadvertently increase this. The contribution of mental illness to violent crime is often overstated, such as in media reports on mass shootings,7 which can bias public perceptions, and such issues have been integral to the appraisal of epidemiological evidence.8 However, failure to acknowledge associations with violence perpetration in turn risks leaving clinical needs unmet in psychiatric services. An accurate and balanced understanding of the nuanced association between mental illness and violence perpetration, development of effective prevention, and balanced communication and contextualization of research evidence may be one approach to reducing stigma.
At a population level, violence is a leading cause of premature mortality and morbidity. Public health approaches to tackling violence focus on prevention and delineating modifiable risk factors, such as mental illness, to inform interventions.9 In schizophrenia spectrum disorders, the public health importance of violence perpetration has been reinforced by recent estimates of its economic impact.10 Updated and precise estimates of violence perpetration risk are needed to inform prevention in health services.
A previous systematic review11 identified 20 primary studies from 11 countries that reported a substantial increase in risk of violence perpetration in individuals with schizophrenia compared with people without schizophrenia, and a doubling of risk with substance misuse comorbidity. However, the search period for this review ended in February 2009. Since then, several large population investigations have been conducted.2,12 These newer studies provide improved approaches to examine confounding, test comorbidities, and allow for examination of additional outcomes. Although other systematic reviews have been conducted,13,14 to our knowledge, no recent quantitative analyses have integrated these new data. This longer-term perspective provides more precision for risk estimates, subgroup analyses, and meta-regressions. The current study therefore provides an updated systematic review and meta-analysis of the risk of violence perpetration in individuals with schizophrenia spectrum disorders compared with general population control individuals.
Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline (eFigure 1 in the Supplement)15 and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guideline16 (eTable 1 in the Supplement). The review was registered on PROSPERO (CRD42020224942). Risk of bias was assessed using the Newcastle-Ottawa Quality Assessment Scale.17
Search Strategy
In a previous review,11 MEDLINE, Embase, and PsycInfo databases were searched from January 1970 to February 2009. For the update, we searched PubMed, PsycInfo, and Global Health from March 1, 2009, to March 17, 2021. No limits were imposed on country or age range.
Eligibility Assessment
Identification of schizophrenia spectrum disorders in included studies was from clinical diagnosis or based on diagnostic criteria. See the eMethods in the Supplement for full eligibility criteria. Applying these criteria, 416 relevant articles were identified from updated searches, 25 of which (reporting on 24 studies) met eligibility criteria.
Data Extraction
A standardized form was used to extract data on study design, location, last year of follow-up (study period), diagnostic definition, comparison group (including any use of sibling controls), definition and ascertainment of violence, violence perpetration outcomes in individuals with schizophrenia spectrum disorders and control individuals, outcome period, sample size, mean age, and information on comorbid substance misuse, personality disorder, experiencing violence, and treatment. If separate data were available for a range of psychoses, we chose schizophrenia spectrum disorders where possible, including schizophrenia and nonschizophrenia psychoses (ICD-10 codes F20-F29), and excluding affective, drug-induced, and organic psychoses. Where separate data were available for male and female individuals, these were disaggregated for analysis. See the eMethods in the Supplement for details of absolute risk data extraction. Where applicable, authors were contacted for additional data. Two authors extracted data (D.W., G.G.), and discrepancies were resolved by consensus.
Meta-analysis
We combined eligible studies from this update with data from the original review11 for analysis to ensure that the current review presents the most comprehensive synthesis of available information.18,19 To avoid duplication, where studies included overlapping populations or where articles were superseded by updated investigations in the same population, we included the study that used a longitudinal design or the study with the largest sample of individuals with schizophrenia spectrum disorders. Applying these methods, 10 studies were excluded from pooled analyses (eTable 2 in the Supplement).3,20,21,22,23,24,25,26,27,28
Data for analysis were considered across 4 violence perpetration outcome classifications. First, a broad interpersonal violence perpetration definition (any physical assault, robbery, sexual offenses, illegal threats or intimidation, and arson). Within this classification male, female, and data combined by sex were grouped separately using nonoverlapping samples, and subgroup analyses (not in protocol but added based on reviewer suggestion) were undertaken to examine for sources of heterogeneity (substance misuse comorbidity, geographical region of study, study quality, study type, nature of control group, patient sample, and outcome measure). While data from studies that included homicide, sexual offenses, or arson within their broad violent outcome definition were included within this classification, if a study considered only 1 of those specific offenses in isolation, it was considered separately. Data included within separate classifications for homicide, sexual offenses, and arson were either disaggregated from studies that used a broad definition but also reported separated offenses or from studies that considered only these outcomes (ie, no broad violence category). A total of 12 studies of homicide,21,29,30,31,32 arson,33,34,35 and sexual offenses36,37,38,39 were included in these separate classifications that were not otherwise included in the broader violence perpetration classification owing either to reporting only that specific offense or to issues of population overlap that did not apply within the separate offense classification. Within the arson classification, meta-analysis was not undertaken owing to the clinical heterogeneity of fire-setting definitions.
Statistical Analysis
We generated unadjusted pooled odds ratios (ORs) with 95% CIs for risk of violence perpetration outcomes using random-effects meta-analysis. Heterogeneity was examined using Cochran Q and the I2 statistic. Analyses were undertaken using R version 3.6.1 (the R Foundation)40 and the R package meta.41 The Mantel-Haenszel method was used to combine odds ratios from 2 × 2 tables, with continuity correction of 0.5 in studies with zero cell frequencies.
Results
Interpersonal Violence Perpetration as Outcome
Twenty-four studies were included (N = 51 309 individuals with schizophrenia spectrum disorders; reported mean age of 21 to 54 years at follow-up; of those studies that reported outcomes separately by sex, there were 19 976 male individuals and 14 275 female individuals), 16 of which were from the original review (n = 9954 individuals with schizophrenia spectrum disorders [19.4%]), and 8 of which were identified from updated searches (n = 41 355 [80.6%]). Studies were based in 15 countries: 5 from the US,42,43,44,45,46 3 from Sweden,2,47,48 2 from Israel reported in 3 publications,49,50,51 2 from Denmark,52,53 2 from Finland reported in 3 articles,54,55,56 1 from Switzerland reported in 3 publications,57,58,59 and 1 each from Australia,12 Austria,60 Canada,61 Czech Republic,62 Egypt,63 Ethiopia,64 Germany,65 New Zealand66 and the UK.67 See the Table for a summary of included studies and eTable 3 in the Supplement for additional details.
Table. Summary of Studies Reporting Violence Perpetration Outcomes in Individuals With Schizophrenia Spectrum Disorders Compared With General Population Control Individuals Included in Meta-analysesa.
| Source | Sex | No. scz (% viol scz) | Outcome period | Ascertainment of violence | Diagnosis | Nature of clinical contact | Country | Study period | Definition of violence |
|---|---|---|---|---|---|---|---|---|---|
| Sosowsky et al,46 1980 | Male and femaleb | 171 (4.7) | ≤6.5 y | Register | Schizophrenia | Admitted to and discharged from state hospital | US | 1975 | Violent crimes |
| Ortmann et al,52 1981 | Male | 86 (2.3) | 8 y | Register | Schizophrenia and ICD-8 paranoid states; other psychoses and unspecified psychosis (excluding alcohol use disorder, organic, and affective psychosis) | Psychiatric hospitalization younger than age 26 y | Denmark | 1978 | Violent offenses (excluding sexual) |
| Swanson et al,45 1990 | Male | 114 (12.7) | 1 y | Self-report | Schizophrenia or schizophreniform disorder | Community sample | US | 1983 | Diagnostic Interview Schedule items indicating self-reported violent behavior |
| Lindqvist et al,48 1990 | Male | 330 (8.5) | 15 y | Register | Schizophrenia | Community sample | Sweden | 1986 | Assault, unlawful deprivation of liberty, unlawful threats |
| Female | 314 (1.3) | ||||||||
| Modestin et al,59 1996 | Male | 282 (5.3) | 21 y | Register | Schizophrenia | Hospitalized at least once during study period | Switzerland | 1987 | Violent crimes (excluding sexual) |
| Modestin et al,57 1995 | Female | 226 (0.4) | 26 y | Register | Schizophrenia and other psychoses | All patients hospitalized in 1987 | Switzerland | 1985 to 1987 | Violent crimes (excluding sexual) |
| Räsänen et al,55 1998; Tiihonen et al,54 1997 | Male | 67 (11.9) | 12 y | Register | Schizophrenia, schizophreniform and schizoaffective disorders, paranoid psychosis, and other psychoses (excluding affective and organic) | Birth cohort members with diagnoses on hospital discharge registers (treated in all mental and general hospitals) | Finland | 1992 | Homicide, assault, robbery, arson, violation of domestic peace |
| Female | 25 (0) | Schizophrenia | |||||||
| Stueve et al,50 1998 | Male | 51 (25.5) | 5 y | Self-report | Psychotic or bipolar disorders | Community- based | Israel | 1992 | Self-reported measures of fighting and weapon use |
| Female | 50 (24.0) | ||||||||
| Arseneault et al,66 2000 | Male and femaleb | 39 (33.3) | 1 y | Register and self-report | Schizophrenia spectrum disorder | Community-based (in year before interview 1.6% of study members overall spent on average 25 d in a psychiatric hospital) | New Zealand | 1994 | Violent convictions (including illegal threats, presenting an offensive weapon, rape, manual assault, assault, robbery, and homicide), and self-reported violence scale (simple assault, aggravated assault, robbery, rape, and gang fighting) |
| Brennan et al,53 2000 | Male | 2185 (11.0) | 29 y | Register | Schizophrenia and other psychoses (including reactive, paranoid, and unspecified; excluding organic and affective) | Members of a birth cohort hospitalized with schizophrenia | Denmark | 1991 | Murder, attempted murder, rape, violence against authority, assault, domestic violence, robbery |
| Female | 2473 (1.7) | ||||||||
| Monahan et al,43 2000 | Male and femaleb | 189 (9.5) | 20 wk | Register, collateral, and self-report | Schizophrenia and other psychotic disorders (schizophreniform, schizoaffective, delusional disorder, brief reactive psychosis) | Inpatients postdischarge | US | 1995 | Acts of battery that resulted in physical injury, sexual assaults, and assaultive acts that involved the use of a weapon or threats made with a weapon in hand |
| Haller et al,60 2001 | Male and femaleb | 1325 (3.9) | 12 y | Register | Schizophrenia, schizoaffective and delusional disorders | Previous inpatient or outpatient treatment | Austria | 1997 | Violent crime |
| Corrigan et al,44 2005 | Male and femaleb | 42 (11.9) | 1 y | Self-report | Nonaffective psychosis | Community sample | US | 1992 | Serious trouble with the law or physical fight resulting in injury |
| Hodgins et al,67 2007 | Male | 10 (35.0) | 31 y | Register | Schizophrenia and other psychoses | Inpatients | UK | 2005 | Violence against another person, sexual offenses (excluding prostitution-related offenses), and robbery |
| Female | 5 (11.8) | ||||||||
| Elonheimo et al,56 2007 | Male | 14 (7.1) | 4 y | Register | Psychotic disorder (including schizophrenia and schizophreniform psychosis) | Community sample (assessed at military call-up) | Finland | 2004 | Assault (“various kinds”), battery, robbery |
| Soyka et al,65 2007 | Male and femaleb | 1662 (3.7) | 7-12 y | Register | Schizophrenia | Postdischarge former inpatients | Germany | 2002 | Physical assault, aggravated assault or battery, threatening or invasion of privacy, sexual abuse of a child, robbery, illegal restraint, manslaughter (including attempted and involuntary), murder, sexual assault, rape, holding someone at gunpoint |
| Elbogen et al,42 2009 | Male and femaleb | 294 (9.2) | 3 y | Self-report | Schizophrenia and other psychoses | Community sample | US | 2005 | Self-reported violence, including using weapons in a fight, arson, forcible sex, substance-related violence, domestic violence |
| Eriksson et al,47 2011 | Male | 377 (24.7) | 35 y | Register | Schizophrenia | Discharged at least once from hospital | Sweden | 2005 | Serious violent conviction (homicide, manslaughter, assault, robbery, assaulting or threatening an officer, forcible confinement, and sexual assault [excluding attempts]) |
| Short et al,12 2013 | Male and femaleb | 4168 (10.0) | 35 y | Register-based | Schizophrenia disorder (including schizoaffective disorder, paraphrenia, shared psychotic disorder, delusional disorders, unspecified nonorganic psychosis) | All persons diagnosed with psychosis in public mental health system | Australia | 2005 | Guilty of a violent offense, including all contact sex offenses and any physical assaults involving force or causing harm |
| Fazel et al,2 2014 | Male | 14 621 (3.5) (6.0) and (10.7) | 1, 2, and 5 y Postdiagnosis | Register | Schizophrenia and other nonaffective psychosis | National patient register identifying any hospital admission 1972 and later; outpatient appointments 2001 and later | Sweden | 2009 | Violent conviction (homicide, attempted homicide, aggravated assault, common assault, robbery, arson, any sexual offense [rape, sexual coercion, child molestation, sexual harassment], illegal threats or intimidation) |
| (16.6) | Mean 9.5 y | ||||||||
| Female | 9676 (0.8), (1.5), (2.7) | 1, 2, and 5 y Postdiagnosis | |||||||
| (5.4) | Mean 9.5 y | ||||||||
| Fleischman et al,51 2014 | Male | 1746 (23.9) | 13.6 y | Register (court records) | Schizophrenia | Persons admitted to psychiatric hospitals, day hospitals, or psychiatric units in general hospitals | Israel | NR | Violent crimes (murder, attempted murder, assault, rape, threats, and robbery) for which convicted (control individuals), or either convicted or deemed mentally incompetent to stand trial |
| Female | 1441 (4.3) | ||||||||
| Tsigebrhan et al,64 2014 | Male and femaleb | 92 (27.2) | 1 y | Self-report | Schizophrenia and schizoaffective disorder | Community sample | Ethiopia | 2011 | MacArthur interview for past-year violence against others (used a weapon, hit someone hard, purposely set a fire, forced sexual intercourse, fought when drinking alcohol or chewing khat, involved in a fight that came to blows, started a fight) |
| Refaat et al,63 2015 | Male and femaleb | 30 (86.7) | 1 wk | Self-report | Schizophrenia | Outpatients either experiencing short-term relapse or receiving maintenance antipsychotic treatment and coming in for follow-up | Egypt | NR | Physical violence grade 3-5 on Modified Overt Aggression Scale (stroked, pushed, scratched, or pulled hair of others without injury; attacked others causing mild injury or serious injury) |
| Černý et al,62 2018 | Male | 93 (41.9) | 6 mo | Self-report, collateral, and file review | Schizophrenia, delusional disorder, acute polymorphic psychotic disorder, schizoaffective disorder | Inpatients hospitalized >3 d | Czech Republic | 2009 | MacArthur Community Violence Interview for past 6-mo moderate violence (simple assault without injury or weapon use) and serious violence (any assault with a lethal weapon, any threat with a lethal weapon in hand, any sexual assault) |
| Female | 65 (38.5) | ||||||||
| Casiano et al,61 2020 | Male and femaleb | 9046 (3.4) | 1 y | Register | Psychotic disorder (including schizophrenia, delusional disorders, acute and transient psychotic disorders, schizoaffective disorder, drug-induced psychosis, and other and nonspecified psychosis) | Community-based sample (diagnoses coded on inpatient or outpatient health care contact) | Canada | 2012 | Violent charges laid down by police and tracked by a Manitoba Justice database; violence inclusive of assault, sexual, and other violent crimes (Canadian criminal codes listed in study appendix) |
Abbreviations: NR, not reported; Scz, individuals with schizophrenia spectrum disorders; viol scz, individuals with schizophrenia spectrum disorders who developed at least one violence perpetration outcome.
For additional study details, see eTable 3 in the Supplement.
Data required for pooled analyses were not reported separately by sex.
Characteristics of Included Studies
For outcomes, 15 studies used register-based measures of violent criminality2,12,46,47,48,51,52,53,55,56,59,60,61,65,67 (n = 50 250 [97.9%]) and 9 used self- or informant-report measures (n = 1059 [2.1%]) either solely42,44,45,50,62,63,64 or in combination with register-based data.43,66 Ten studies included only individuals with schizophrenia spectrum disorders who had at least 1 inpatient hospitalization43,46,47,51,52,53,59,62,65,67 (n = 11 011 [21.5%]), whereas 14 studies (n = 40 298 [78.5%]) identified individuals with schizophrenia spectrum disorders in the community or who had been in contact with a broader range of inpatient and outpatient care settings.2,12,42,44,45,48,50,55,56,60,61,63,64,66 Thirteen reports were considered overall good quality (scoring 7 to 9 of 9 overall and evenly across domains on the Newcastle-Ottawa Quality Assessment Scale),2,12,43,45,47,51,52,53,55,56,61,62,66 and 11 were considered poor to fair (eTable 4 in the Supplement).42,44,46,48,50,59,60,63,64,65,67 The mean (SD; interquartile range) quality score was 7.0 (1.5; 6-8).
Male Data
There were 19 976 male individuals with schizophrenia spectrum disorders. The random-effects pooled OR for the risk of violence perpetration in individuals with schizophrenia spectrum disorders compared with general population control individuals in this group was 4.5 (95% CI, 3.6-5.6), with substantial heterogeneity (I2 = 85%; 95% CI, 77-91) (Figure 1).
Figure 1. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration.
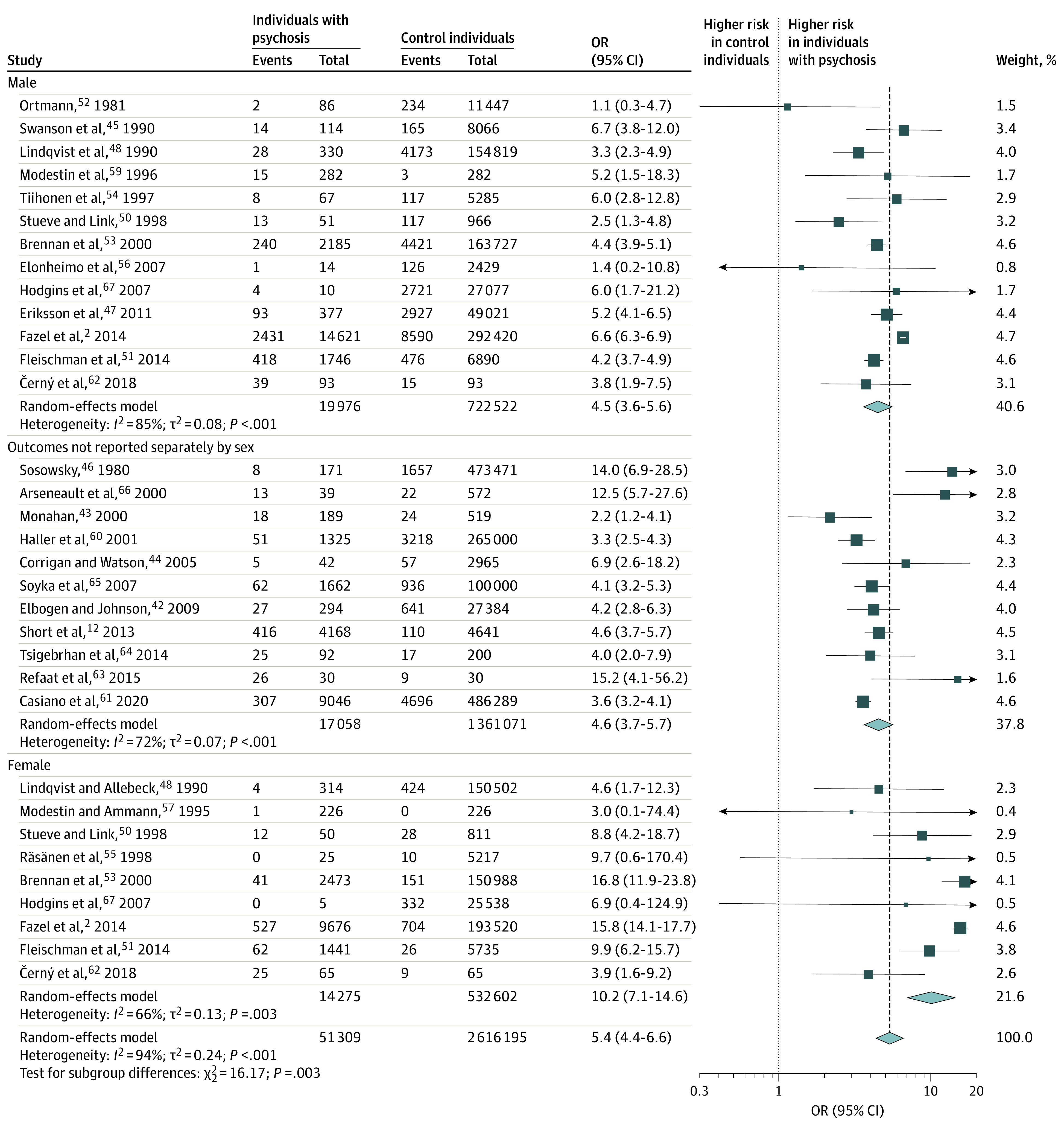
Odds ratio (OR) of violence perpetration outcomes in individuals with schizophrenia spectrum disorders compared with general population control individuals.
Female Data
Among the 14 275 female individuals with schizophrenia spectrum disorders, the random-effects pooled OR for the risk of violence perpetration in individuals with schizophrenia spectrum disorders compared with general population control individuals was 10.2 (95% CI, 7.1-14.6), with substantial heterogeneity (I2 = 66%; 95% CI, 31-83) (Figure 1). Excluding 3 studies of female individuals with schizophrenia55,57,67 (n = 256) with no events in either individuals with schizophrenia spectrum disorders or control individuals made no material difference to risk estimates (pooled OR, 10.3; 95% CI, 7.0-15.1).
Studies That Did Not Report Outcomes Separately by Participant Sex
Data from 11 studies with 17 058 individuals with schizophrenia spectrum disorders were not available separately by sex (Figure 1). Risk of violence perpetration was increased compared with general population control individuals (random-effects pooled OR, 4.6; 95% CI, 3.7-5.7), with substantial heterogeneity (I2 = 72%; 95% CI, 48-85).
Register-Based Outcomes and Study Quality
When restricting analysis to studies that used exclusively register-based violence perpetration outcomes (n = 50 250) (eFigure 2 in the Supplement), the pooled OR for violence perpetration in male individuals was 4.6 (95% CI, 3.6-5.9; I2 = 88%; 95% CI, 79-93); in female individuals, the OR was 12.8 (95% CI, 9.5-17.4; I2 = 48%; 95% CI, 0-78); and in studies where sex was not reported separately, it was 4.3 (95% CI, 3.4-5.4; I2 = 78%; 95% CI, 47-91). When studies were grouped by quality, pooled OR for studies rated good (n = 46 425) was 5.7 (95% CI, 4.3-7.5; I2 = 96%; 95% CI, 95-97) and for studies rated poor to fair (n = 4884) was 4.6 (95% CI, 3.7-5.9; I2 = 48%; 95% CI, 6-71) (eFigure 3 in the Supplement). Subgroup analysis by study design showed that findings were comparable (eFigure 4 in the Supplement).
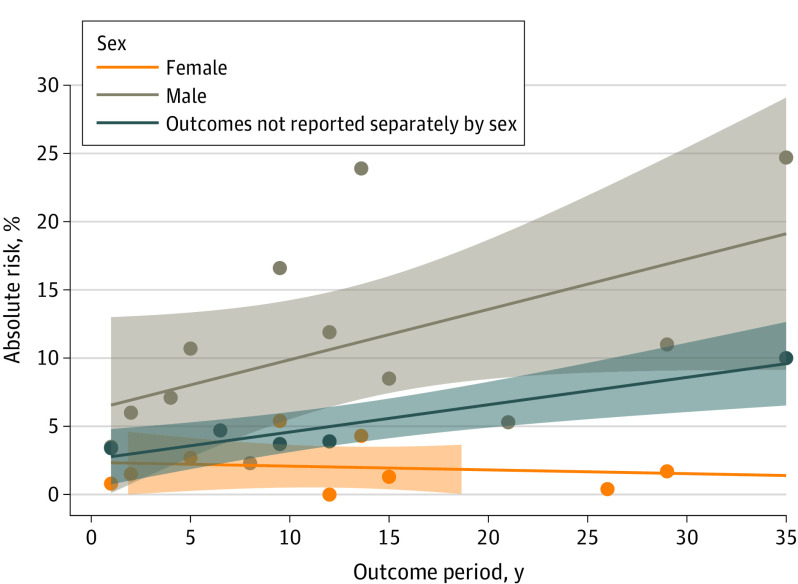
Absolute Risks
Absolute rates of violence perpetration in included studies of register-based violent outcomes ranged from 2.3% to 24.7% in men with schizophrenia spectrum disorders and from 0% to 5.4% in women with schizophrenia spectrum disorders, over outcome periods that ranged from 1 year to lifetime measures spanning up to 35 years (Table; Figure 2).
Figure 2. Absolute Risks of Violence Perpetration in Individuals With Schizophrenia Spectrum Disorders.
Outcome period and absolute risk of violence perpetration in individuals with schizophrenia spectrum disorders in studies included in meta-analyses reporting register-based violent outcomes. Data using self- and collateral-report measures were excluded from comparison owing to lower severity threshold. Linear regression lines with 95% CIs are presented by sex.
Substance Misuse and Other Comorbidity
Seventeen studies2,12,42,43,44,45,47,50,51,53,54,55,59,61,62,63,64,65 included data on substance comorbidity among individuals with schizophrenia spectrum disorders, either under a broad substance misuse definition12,42,43,45,50,51,53,61,63,65 or separately for drug use2,44,47,59,62,64 and alcohol use.2,44,47,54,55,59,62,64 A variety of descriptors were used to define the comorbidity; in studies that described misuse (without or without dependence),42,43,44,45,50,51,53,54,55,59 or use disorders,2,12,61 prevalence ranges were reported for men and women (eTable 3 in the Supplement). In 13 studies,12,42,43,44,45,50,51,53,54,59,63,65 data allowed violence perpetration in individuals with schizophrenia spectrum disorders with or without substance misuse comorbidity to be compared with general population groups separately. The pooled odds of violence perpetration in individuals with schizophrenia spectrum disorders without substance misuse comorbidity (n = 11 079) was 3.5 (95% CI, 2.6-4.6; I2 = 81%; 95% CI, 68-89) (eFigure 5 in the Supplement), and in individuals with schizophrenia spectrum disorders with substance misuse comorbidity (n = 3586), it was 9.9 (95% CI, 7.2-13.5; I2 = 82%; 95% CI, 69-89) (eFigure 6 in the Supplement).
Information on other comorbidities was limited. One study reported on comorbid antisocial personality disorder.62 No included studies provided treatment information.
Geographical Region
Subgroup analyses were undertaken for studies undertaken in Europe (n = 33 836), North America (n = 9856), Australia and New Zealand (n = 4207), and Africa (n = 122). Relative risk estimates for violence perpetration among individuals with schizophrenia spectrum disorders compared with general population control individuals did not significantly vary by region (eFigure 7 in the Supplement).
Familial Confounding
Two included studies, conducted in Sweden2 and Israel,51 used population registers to examine risk of violence perpetration in individuals with schizophrenia spectrum disorders and their unaffected siblings (n = 33 892 unaffected siblings) in addition to comparing individuals with schizophrenia spectrum disorders with general population control individuals. Both studies found relative risks of violence perpetration in unaffected siblings remained significantly increased compared with population control individuals, but to a lesser degree than in the corresponding patient samples (eFigure 8 in the Supplement), indicating familial confounding. When comparing violence perpetration in individuals with schizophrenia spectrum disorders with their unaffected siblings, the study in Sweden2 reported a ratio of ORs of 4.2 (95% CI, 3.8-4.5) and the study in Israel51 an OR of 2.8 (95% CI, 2.5-3.3).
Inpatient and Community Samples
When data were grouped according to samples identified by a history of psychiatric hospital admission or using a wider definition of outpatient or inpatient psychiatric settings, there were no significant differences in relative risk estimates (inpatient pooled OR, 5.4; 95% CI, 4.1-7.0; combined community and inpatient pooled OR, 5.5; 95% CI, 4.0-7.4) (eFigure 9 in the Supplement).
Homicide Perpetration as Outcome
Eight studies were identified with homicide perpetration as an outcome (Figure 3; eTable 5 in the Supplement). All used official sources for outcomes. There was an increase in risk of homicide perpetration in individuals with schizophrenia spectrum disorders compared with those without (Figure 3), leading to a random-effects pooled OR of 17.7 (95% CI, 13.9-22.6) with substantial heterogeneity (I2 = 70%; 95% CI, 39-85). Excluding 1 study (n = 282 [0.4%])59 with no events in the control group did not materially change the pooled risk estimate (OR, 17.9; 95% CI, 14.1-22.8). Four studies were rated good quality21,29,30,51 and 4 were rated poor to fair31,32,59,60 (eTable 4 in the Supplement).
Figure 3. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Homicide Perpetration.
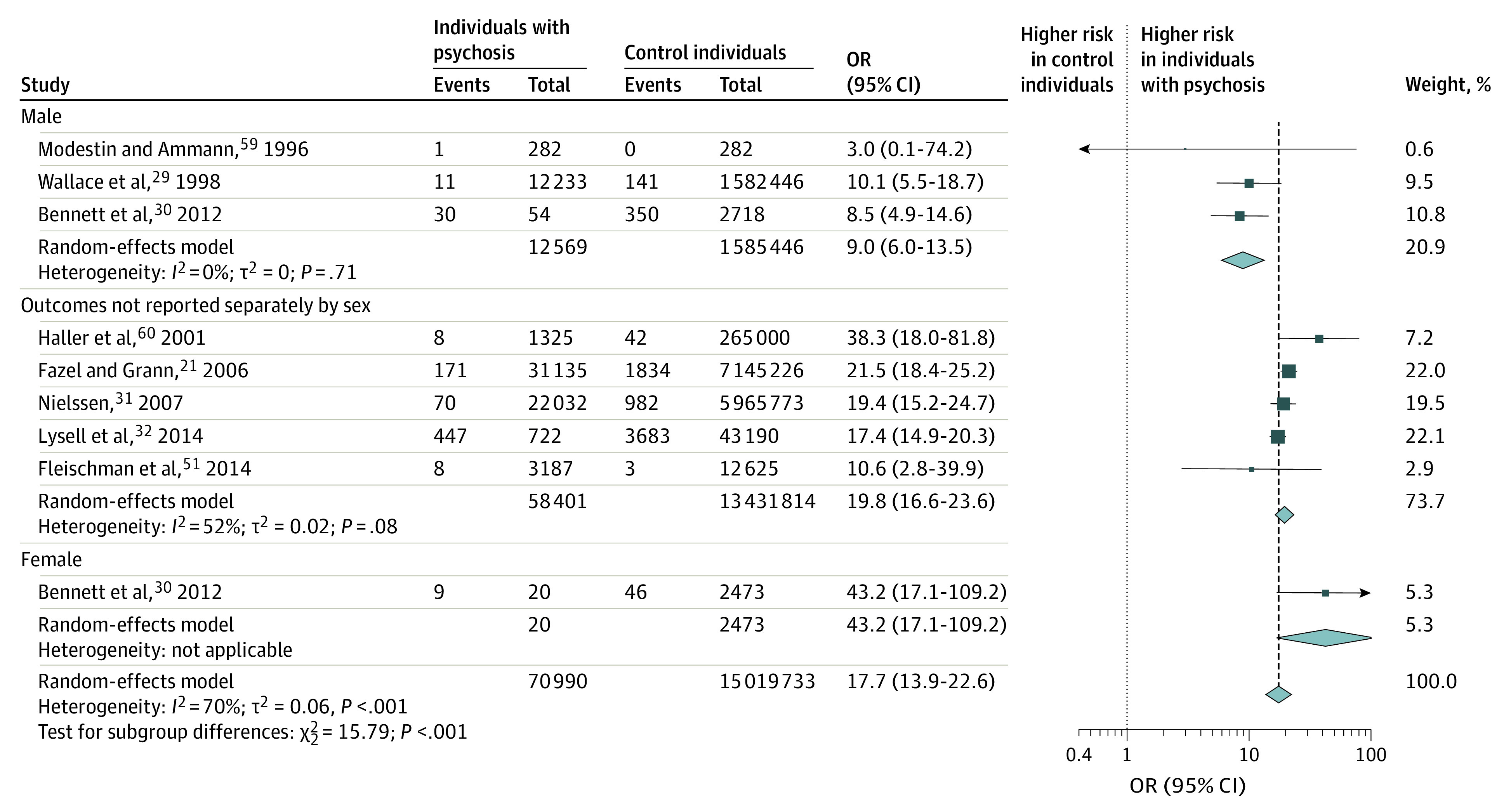
Odds ratio (OR) of homicide perpetration outcomes in individuals with schizophrenia spectrum disorders compared with general population control individuals.
Sexual Offense Perpetration as Outcome
Nine studies22,36,37,38,39,51,52,59,64 were included in a meta-analysis of sexual offense perpetration outcomes (Figure 4; eTables 4 and 6 in the Supplement). All but 2 studies38,64 used a register-based outcome. Risk was increased in individuals with schizophrenia spectrum disorders compared with control individuals, with a random-effects pooled OR of 5.1 (95% CI, 3.8-6.8) with moderate heterogeneity (I2 = 54%; 95% CI, 7-78) (Figure 4).
Figure 4. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Sexual Offense Perpetration.
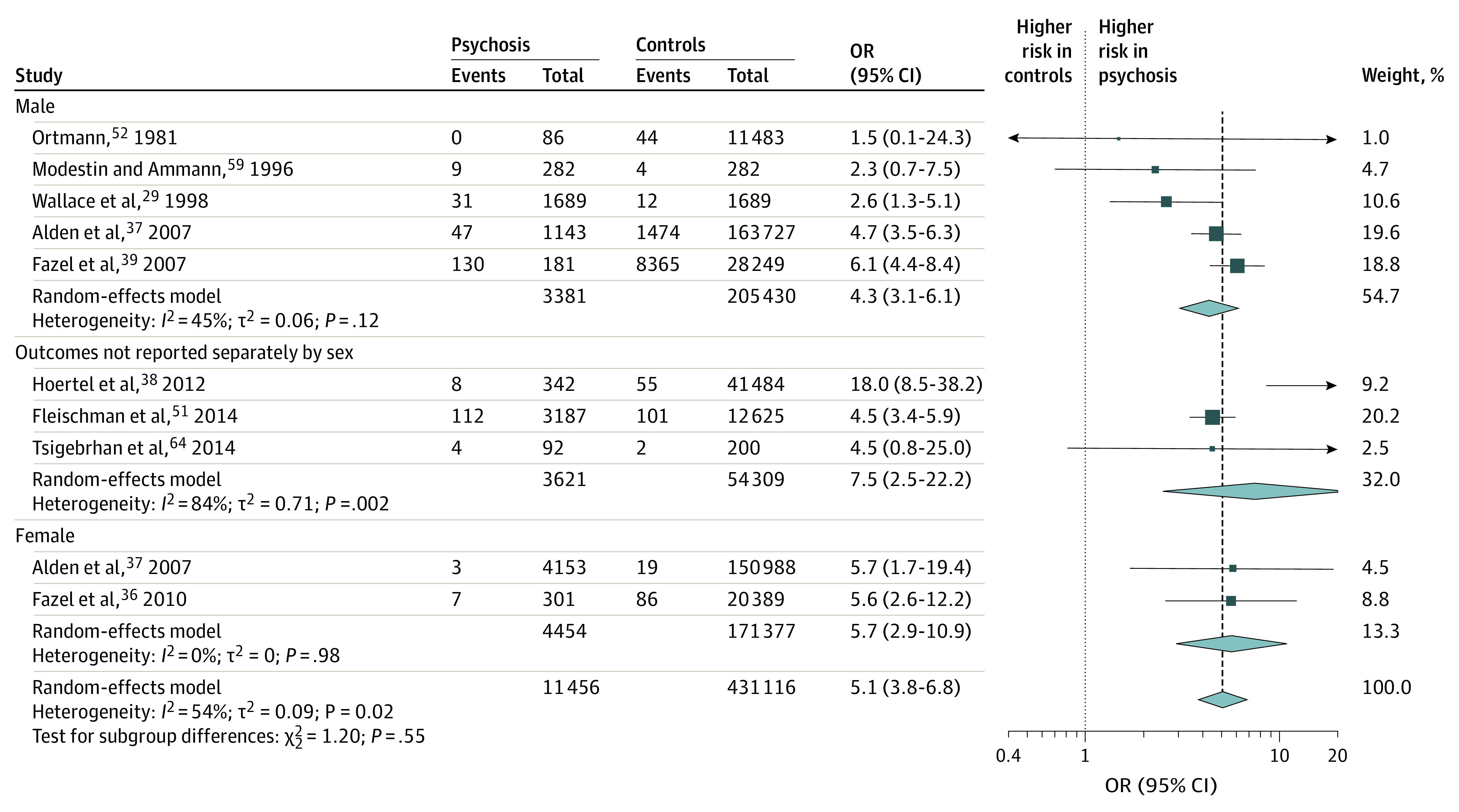
Odds ratio (OR) of sexual offense perpetration outcomes in individuals with schizophrenia spectrum disorders compared with general population control individuals.
Arson as Outcome
Four studies presented data on risk of arson. Findings ranged from no association between schizophrenia and self-reported fire-setting in 1 study64 to 2 register-based studies of arson and related convictions that showed a significant positive association with schizophrenia spectrum disorder diagnosis, with ORs of 18 (95% CI, 12-26) in male individuals and 23 (95% CI, 13-41) in female individuals in a study in Sweden,33 and 7 (95% CI, 4-13) in a study in Australia that did not report outcomes separately by sex of participants34 (eResults in the Supplement). Meta-analysis was not considered owing to the heterogeneity of arson outcomes.
Discussion
This systematic review and meta-analysis included 51 309 individuals with schizophrenia spectrum disorders from 24 studies in 15 countries over 4 decades and investigated risk of violence perpetration outcomes. Additionally, we examined data on homicide perpetration and studies reporting sexual offense perpetration and arson as outcomes. Our findings update and extend a previous meta-analysis11 in 4 main ways.
First, the study included more than double the number of individuals with schizophrenia spectrum disorders in the meta-analysis of violence perpetration outcomes than the previous meta-analysis. This is despite deploying strict exclusion criteria to avoid double-counting of individuals in pooled analyses that excluded otherwise eligible studies. The improved precision of the current study is principally owing to the inclusion of 4 large, high-quality register-based studies conducted since the previous review.2,12,51,61 Despite studies from the last decade contributing most of the data, estimates for the relative risk of violence perpetration have remained broadly stable based on visual inspection of the forest plots (Figure 1).
Second, we pooled risks of sexual offense perpetration. Primary studies varied as to whether they included sexual offenses in an overall definition of violent offending or provided separate data on these offenses. Although there have been descriptive reviews of associations with sexual offending,68 to our knowledge this is the first quantitative synthesis. Data on arson and fire-setting were more limited, although 2 register-based studies reported a significant increased association with schizophrenia spectrum disorders.
Third, we summarized information on absolute risks of violent crime perpetration and on the time period over which these outcomes occurred. Time periods ranged from 1 to 35 years in register-based studies, and absolute risks varied considerably over time and between sexes. Absolute risks were less than 1 in 20 (or 5%) in female individuals with schizophrenia spectrum disorders and less than 1 in 4 men.
Fourth, large register-based studies undertaken since the original review11 provided more power to investigate confounding. We replicated in pooled analyses the finding that violence perpetration risk was reduced but remained increased relative to control samples when individuals with substance misuse comorbidity were excluded.12,51 In individuals with schizophrenia spectrum disorders and substance misuse comorbidity, there was increased odds of around 10-fold compared with general population control individuals, whereas in individuals with noncomorbid schizophrenia spectrum disorders, this was around 3-fold compared with general population control individuals. Additionally, the contribution of familial factors has now been estimated in studies that have compared risks of violence perpetration in individuals with schizophrenia spectrum disorders, their unaffected siblings, and general population control individuals. These investigations reported residual risk among unaffected siblings and therefore some familial confounding, but risk remains elevated among affected individuals compared with their unaffected siblings.2,51 The latter finding further confirms the independent association between schizophrenia and violence perpetration.
There are several implications of our findings for clinical services and future research. In clinical settings, risks in absolute terms, particularly in young men, are typically high enough to be considered of routine clinical importance to prevent. This is reflected to a limited extent in clinical guidelines, but guidance on assessing and managing risk could be improved.69 Likewise, the importance of comorbid substance misuse has been further highlighted, reinforcing the need to prioritize the assessment and treatment of comorbid substance misuse disorders in clinical services. The applicability of findings to a particular clinical setting is a limitation of pooling data from individuals at different stages of illness and treatment in a variety of geographical and health care settings. However, the amount of data included has allowed for exploration of some relevant factors, such as variation by region, patient samples, and substance misuse comorbidity. This improves the ability of clinicians to consider the extent to which findings may apply to their practice.
This replication of relative risk estimates for violence perpetration with the inclusion of larger data sets suggests that further small studies of the relative risk of violence in schizophrenia are not priorities. Future epidemiological research could focus on specific offenses or outcomes, such as sexual offenses and arson. Violence perpetration as an outcome is necessarily broad, but there may be important differences in clinical and risk profiles between more specific violence perpetration outcomes.
This meta-analysis found robust associations between schizophrenia spectrum disorders and violence perpetration, but did not answer the question of the nature of causal pathways and whether they are present. Empirical studies have suggested that symptoms such as persecutory delusions may be causally linked to violence.70 The current study found that the association between schizophrenia spectrum disorders and violence perpetration remained, albeit with reduced estimates, after adjusting for substance misuse and familial confounders, which can exist on the causal pathway and explain a proportion of the association. However, other background, psychiatric, and socioeconomic factors unaccounted for in these pooled analyses can contribute to this pathway, and there is research in support of early conduct problems,71 adverse childhood experiences,72 and economic disadvantage.73 Large prospective studies are needed to further evaluate causality.74 For clinicians, the multifactorial association means that a key priority should be to refine approaches to individualized risk assessment and management. Scalable prediction tools offer one way to translate contemporary knowledge on risk factors (including sociodemographic, familial, and treatment factors) into clinical practice and achieve a more stratified approach to assessing and managing clinical needs around violence risk.75
There was little information on treatment effects. There is evidence from pharmacoepidemiological studies that antipsychotics can reduce violence perpetration outcomes.76,77,78,79 This needs confirmation in randomized trials, and violence perpetration should be a routine outcome in effectiveness trials of pharmacological and nonpharmacological interventions. One question is how risk of violence perpetration in individuals with schizophrenia spectrum disorders treated with antipsychotic medication compares with that risk in general population samples. One population study in Sweden found rates of violent offenses of 33 per 1000 person-years during treatment with olanzapine compared with 96 offenses per 1000 person-years prior to treatment.77 To what extent these treatment effects bring rates of violence perpetration down toward baseline population levels requires comparison with matched groups.
Limitations
This study has limitations. Most data in pooled analyses used register-based violence perpetration outcomes, which offer advantages over self- or informant-rated measures in that they objectively cross a severity threshold for clinical relevance and resource implications, do not rely on ongoing contact with health services, and avoid interrater variability and recall bias. A limitation is to what extent these measures may be confounded by differential treatment of individuals with mental disorders by the justice system. However, a study examining the Dunedin cohort found that associations with mental disorders were similar when using self- or informant-report and official court records, suggesting that the degree of underreporting is similar in individuals with schizophrenia spectrum disorders and control individuals when using either outcome.66 In terms of other limitations, only 3 studies presented information on experiencing interpersonal violence61,62,64 and 1 on the contribution of childhood trauma.62 The importance of the overlap between risk of experiencing violence and perpetrating violence is increasingly recognized.3,61,80 Further, although analyses did not reveal significant differences in risk estimates when studies were grouped by quality, variation between studies in the level of matching of comparison groups is an additional consideration to explain heterogeneity, as this was only partially captured by the quality rating. A study of more than half a million individuals using population registers in Denmark replicated findings of increased risk of violence perpetration in individuals with schizophrenia spectrum disorders (with incident rate ratios of 6 in men and 18 in women),81 but could not be included in pooled analyses because the study lacked the necessary tabular data.
Conclusions
This review has quantitatively summarized the association between schizophrenia spectrum disorders and violence perpetration outcomes. Prevention of violence perpetration should be a target for clinical services that assess and treat individuals with these disorders. New work should consider preventive approaches, including the improvement of the clinical assessment of risk and targeted resource allocation to treat modifiable factors. Violence perpetration outcomes should be routinely collected in studies of the effectiveness of clinical services and therapeutic interventions.
eMethods.
eTable 1. Meta-Analyses of Observational Studies in Epidemiology (MOOSE) Checklist
eFigure 1. Flow Diagram for Updated Searches
eTable 2. Eligible studies reporting violent and homicide outcomes in people with schizophrenia spectrum disorders compared to general population controls identified in updated searches but not included in meta-analysis
eTable 3. Additional details of studies reporting violent outcomes in people with schizophrenia spectrum disorders compared to general population controls included in meta-analysis
eTable 4. Quality Assessment of Studies Included in Meta-Analyses
eFigure 2. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration in Register Studies
eFigure 3. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration By Study Quality
eFigure 4. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration By Study Design
eFigure 5. Forest Plot of Association Between Schizophrenia Spectrum Disorders Without Substance Misuse Comorbidity and Violence Perpetration
eFigure 6. Forest Plot of Association Between Schizophrenia Spectrum Disorders With Substance Misuse Comorbidity and Violence Perpetration
eFigure 7. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration by Region
eFigure 8. Odds of Violence Perpetration in Schizophrenia Spectrum Disorders and Unaffected Siblings Compared to General Population
eFigure 9. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration by Patient Sample
eTable 5. Details of studies reporting homicide perpetration as outcome in people with schizophrenia spectrum disorders compared to general population controls included in meta-analysis
eTable 6. Details of studies reporting sexual offence perpetration as outcome in people with schizophrenia spectrum disorders compared to general population controls included in meta-analysis
eResults
eReferences
References
- 1.Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24(4_suppl):81-90.doi: 10.1177/1359786810385490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fazel S, Wolf A, Palm C, Lichtenstein P. Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: a 38-year total population study in Sweden. Lancet Psychiatry. 2014;1(1):44-54. doi: 10.1016/S2215-0366(14)70223-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sariaslan A, Arseneault L, Larsson H, Lichtenstein P, Fazel S. Risk of subjection to violence and perpetration of violence in persons with psychiatric disorders in Sweden. JAMA Psychiatry. 2020;77(4):359-367. doi: 10.1001/jamapsychiatry.2019.4275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yee N, Matheson S, Korobanova D, et al. A meta-analysis of the relationship between psychosis and any type of criminal offending, in both men and women. Schizophr Res. 2020;220:16-24. doi: 10.1016/j.schres.2020.04.009 [DOI] [PubMed] [Google Scholar]
- 5.Immonen J, Jääskeläinen E, Korpela H, Miettunen J. Age at onset and the outcomes of schizophrenia: a systematic review and meta-analysis. Early Interv Psychiatry. 2017;11(6):453-460. doi: 10.1111/eip.12412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lok P, Dijk S. Violence and mental illness: five minutes with…Seena Fazel. BMJ. 2019;366:l5199. doi: 10.1136/bmj.l5199 [DOI] [PubMed] [Google Scholar]
- 7.US Department of Justice Federal Bureau of Investigation . A study of pre-attack behaviors of active shooters in the United States between 2000-2013. Accessed September 15, 2021. https://www.fbi.gov/file-repository/pre-attack-behaviors-of-active-shooters-in-us-2000-2013.pdf/view?mod=article_inline
- 8.Varshney M, Mahapatra A, Krishnan V, Gupta R, Deb KS. Violence and mental illness: what is the true story? J Epidemiol Community Health. 2016;70(3):223-225. doi: 10.1136/jech-2015-205546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . Global Status Report on Violence Prevention 2014. Accessed September 15, 2021. https://www.who.int/publications/i/item/9789241564793
- 10.Senior M, Fazel S, Tsiachristas A. The economic impact of violence perpetration in severe mental illness: a retrospective, prevalence-based analysis in England and Wales. Lancet Public Health. 2020;5(2):e99-e106. doi: 10.1016/S2468-2667(19)30245-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med. 2009;6(8):e1000120. doi: 10.1371/journal.pmed.1000120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Short T, Thomas S, Mullen P, Ogloff JR. Comparing violence in schizophrenia patients with and without comorbid substance-use disorders to community controls. Acta Psychiatr Scand. 2013;128(4):306-313. doi: 10.1111/acps.12066 [DOI] [PubMed] [Google Scholar]
- 13.Nederlof AF, Muris P, Hovens JE. The epidemiology of violent behavior in patients with a psychotic disorder: a systematic review of studies since 1980. Aggress Violent Behav. 2013;18(1):183-189. doi: 10.1016/j.avb.2012.11.018 [DOI] [Google Scholar]
- 14.Lamsma J, Harte JM. Violence in psychosis: conceptualizing its causal relationship with risk factors. Aggress Violent Behav. 2015;24:75-82. doi: 10.1016/j.avb.2015.05.003 [DOI] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stroup DF, Berlin JA, Morton SC, et al. ; Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group . Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008-2012. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 17.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed April 15, 2021. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 18.Moher D, Tsertsvadze A, Tricco AC, et al. When and how to update systematic reviews. Cochrane Database Syst Rev. 2008;(1):MR000023. doi: 10.1002/14651858.MR000023.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Tsertsvadze A. Systematic reviews: when is an update an update? Lancet. 2006;367(9514):881-883. doi: 10.1016/S0140-6736(06)68358-X [DOI] [PubMed] [Google Scholar]
- 20.Fazel S, Långström N, Hjern A, Grann M, Lichtenstein P. Schizophrenia, substance abuse, and violent crime. JAMA. 2009;301(19):2016-2023. doi: 10.1001/jama.2009.675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fazel S, Grann M. The population impact of severe mental illness on violent crime. Am J Psychiatry. 2006;163(8):1397-1403. doi: 10.1176/ajp.2006.163.8.1397 [DOI] [PubMed] [Google Scholar]
- 22.Wallace C, Mullen PE, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry. 2004;161(4):716-727. doi: 10.1176/appi.ajp.161.4.716 [DOI] [PubMed] [Google Scholar]
- 23.Eriksson A. Schizophrenia and Criminal Offending—Risk Factors and the Role of Treatment. Dissertation. Karolinska Institutet Stockholm; 2008. https://openarchive.ki.se/xmlui/bitstream/handle/10616/38625/thesis.pdf?sequence=1&isAllowed=y [Google Scholar]
- 24.Sariaslan A, Larsson H, Fazel S. Genetic and environmental determinants of violence risk in psychotic disorders: a multivariate quantitative genetic study of 1.8 million Swedish twins and siblings. Mol Psychiatry. 2016;21(9):1251-1256. doi: 10.1038/mp.2015.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuja-Halkola R, Pawitan Y, D’Onofrio BM, Långström N, Lichtenstein P. Advancing paternal age and offspring violent offending: a sibling-comparison study. Dev Psychopathol. 2012;24(3):739-753. doi: 10.1017/S095457941200034X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moberg T, Stenbacka M, Tengström A, Jönsson EG, Nordström P, Jokinen J. Psychiatric and neurological disorders in late adolescence and risk of convictions for violent crime in men. BMC Psychiatry. 2015;15:299. doi: 10.1186/s12888-015-0683-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Okuda M, Olfson M, Wang S, Rubio JM, Xu Y, Blanco C. Correlates of intimate partner violence perpetration: results from a national epidemiologic survey. J Trauma Stress. 2015;28(1):49-56. doi: 10.1002/jts.21986 [DOI] [PubMed] [Google Scholar]
- 28.Lysell H, Dahlin M, Långström N, Lichtenstein P, Runeson B. Killing the mother of one’s child: psychiatric risk factors among male perpetrators and offspring health consequences. J Clin Psychiatry. 2016;77(3):342-347. doi: 10.4088/JCP.15m09564 [DOI] [PubMed] [Google Scholar]
- 29.Wallace C, Mullen P, Burgess P, Palmer S, Ruschena D, Browne C. Serious criminal offending and mental disorder. case linkage study. Br J Psychiatry. 1998;172(6):477-484. doi: 10.1192/bjp.172.6.477 [DOI] [PubMed] [Google Scholar]
- 30.Bennett D, Ogloff J, Mullen P, Thomas S. A study of psychotic disorders among female homicide offenders. Psychol Crime Law. 2012;18(3):231-243. doi: 10.1080/10683161003752311 [DOI] [Google Scholar]
- 31.Nielssen OB, Westmore BD, Large MM, Hayes RA. Homicide during psychotic illness in New South Wales between 1993 and 2002. Med J Aust. 2007;186(6):301-304. doi: 10.5694/j.1326-5377.2007.tb00905.x [DOI] [PubMed] [Google Scholar]
- 32.Lysell H, Runeson B, Lichtenstein P, Långström N. Risk factors for filicide and homicide: 36-year national matched cohort study. J Clin Psychiatry. 2014;75(2):127-132. doi: 10.4088/JCP.13m08372 [DOI] [PubMed] [Google Scholar]
- 33.Anwar S, Långström N, Grann M, Fazel S. Is arson the crime most strongly associated with psychosis? a national case-control study of arson risk in schizophrenia and other psychoses. Schizophr Bull. 2011;37(3):580-586. doi: 10.1093/schbul/sbp098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ducat L, Ogloff JR, McEwan T. Mental illness and psychiatric treatment amongst firesetters, other offenders and the general community. Aust N Z J Psychiatry. 2013;47(10):945-953. doi: 10.1177/0004867413492223 [DOI] [PubMed] [Google Scholar]
- 35.Hoertel N, Le Strat Y, Schuster J-P, Limosin F. Gender differences in firesetting: results from the national epidemiologic survey on alcohol and related conditions (NESARC). Psychiatry Res. 2011;190(2-3):352-358. doi: 10.1016/j.psychres.2011.05.045 [DOI] [PubMed] [Google Scholar]
- 36.Fazel S, Sjöstedt G, Grann M, Långström N. Sexual offending in women and psychiatric disorder: a national case-control study. Arch Sex Behav. 2010;39(1):161-167. doi: 10.1007/s10508-008-9375-4 [DOI] [PubMed] [Google Scholar]
- 37.Alden A, Brennan P, Hodgins S, Mednick S. Psychotic disorders and sex offending in a Danish birth cohort. Arch Gen Psychiatry. 2007;64(11):1251-1258. doi: 10.1001/archpsyc.64.11.1251 [DOI] [PubMed] [Google Scholar]
- 38.Hoertel N, Le Strat Y, Schuster JP, Limosin F. Sexual assaulters in the United States: prevalence and psychiatric correlates in a national sample. Arch Sex Behav. 2012;41(6):1379-1387. doi: 10.1007/s10508-012-9943-5 [DOI] [PubMed] [Google Scholar]
- 39.Fazel S, Sjöstedt G, Långström N, Grann M. Severe mental illness and risk of sexual offending in men: a case-control study based on Swedish national registers. J Clin Psychiatry. 2007;68(4):588-596. doi: 10.4088/JCP.v68n0415 [DOI] [PubMed] [Google Scholar]
- 40.R Core Team . R: a language and environment for statistical computing. Vienna ARFfSC, 2019. https://www.R-project.org/
- 41.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153-160. doi: 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2009;66(2):152-161. doi: 10.1001/archgenpsychiatry.2008.537 [DOI] [PubMed] [Google Scholar]
- 43.Monahan J. Reducing violence risk. In: Hodgins S, ed. Violence Among the Mentally Ill. Springer; 2000:19-34. doi: 10.1007/978-94-011-4130-7_2 [DOI] [Google Scholar]
- 44.Corrigan PW, Watson AC. Findings from the National Comorbidity Survey on the frequency of violent behavior in individuals with psychiatric disorders. Psychiatry Res. 2005;136(2-3):153-162. doi: 10.1016/j.psychres.2005.06.005 [DOI] [PubMed] [Google Scholar]
- 45.Swanson JW, Holzer CE III, Ganju VK, Jono RT. Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys. Hosp Community Psychiatry. 1990;41(7):761-770. doi: 10.1176/ps.41.7.761 [DOI] [PubMed] [Google Scholar]
- 46.Sosowsky L. Explaining the increased arrest rate among mental patients: a cautionary note. Am J Psychiatry. 1980;137(12):1602-1605. doi: 10.1176/ajp.137.12.1602 [DOI] [PubMed] [Google Scholar]
- 47.Eriksson A, Romelsjö A, Stenbacka M, Tengström A. Early risk factors for criminal offending in schizophrenia: a 35-year longitudinal cohort study. Soc Psychiatry Psychiatr Epidemiol. 2011;46(9):925-932. doi: 10.1007/s00127-010-0262-7 [DOI] [PubMed] [Google Scholar]
- 48.Lindqvist P, Allebeck P. Schizophrenia and crime. a longitudinal follow-up of 644 schizophrenics in Stockholm. Br J Psychiatry. 1990;157:345-350. doi: 10.1192/bjp.157.3.345 [DOI] [PubMed] [Google Scholar]
- 49.Stueve A, Link BG. Violence and psychiatric disorders: results from an epidemiological study of young adults in Israel. Psychiatr Q. 1997;68(4):327-342. doi: 10.1023/A:1025443014158 [DOI] [PubMed] [Google Scholar]
- 50.Stueve A, Link BG. Gender differences in the relationship between mental illness and violence: evidence from a community-based epidemiological study in Israel. Soc Psychiatry Psychiatr Epidemiol. 1998;33(1)(suppl 1):S61-S67. doi: 10.1007/s001270050211 [DOI] [PubMed] [Google Scholar]
- 51.Fleischman A, Werbeloff N, Yoffe R, Davidson M, Weiser M. Schizophrenia and violent crime: a population-based study. Psychol Med. 2014;44(14):3051-3057. doi: 10.1017/S0033291714000695 [DOI] [PubMed] [Google Scholar]
- 52.Ortmann J. Psykisk Afvigelse Og Kriminel Adfærd: En Undersøgelse Af 11.533 Mænd Født I 1953 I Det Metropolitane Område København. Justitsministerie; 1981. [Google Scholar]
- 53.Brennan PA, Mednick SA, Hodgins S. Major mental disorders and criminal violence in a Danish birth cohort. Arch Gen Psychiatry. 2000;57(5):494-500. doi: 10.1001/archpsyc.57.5.494 [DOI] [PubMed] [Google Scholar]
- 54.Tiihonen J, Isohanni M, Räsänen P, Koiranen M, Moring J. Specific major mental disorders and criminality: a 26-year prospective study of the 1966 northern Finland birth cohort. Am J Psychiatry. 1997;154(6):840-845. doi: 10.1176/ajp.154.6.840 [DOI] [PubMed] [Google Scholar]
- 55.Räsänen P, Tiihonen J, Isohanni M, Rantakallio P, Lehtonen J, Moring J. Schizophrenia, alcohol abuse, and violent behavior: a 26-year followup study of an unselected birth cohort. Schizophr Bull. 1998;24(3):437-441. doi: 10.1093/oxfordjournals.schbul.a033338 [DOI] [PubMed] [Google Scholar]
- 56.Elonheimo H, Niemelä S, Parkkola K, et al. Police-registered offenses and psychiatric disorders among young males: the Finnish “from a boy to a man” birth cohort study. Soc Psychiatry Psychiatr Epidemiol. 2007;42(6):477-484. doi: 10.1007/s00127-007-0192-1 [DOI] [PubMed] [Google Scholar]
- 57.Modestin J, Ammann R. Mental disorders and criminal behaviour. Br J Psychiatry. 1995;166(5):667-675. doi: 10.1192/bjp.166.5.667 [DOI] [PubMed] [Google Scholar]
- 58.Modestin J, Wuermle O. Criminality in men with major mental disorder with and without comorbid substance abuse. Psychiatry Clin Neurosci. 2005;59(1):25-29. doi: 10.1111/j.1440-1819.2005.01327.x [DOI] [PubMed] [Google Scholar]
- 59.Modestin J, Ammann R. Mental disorder and criminality: male schizophrenia. Schizophr Bull. 1996;22(1):69-82. doi: 10.1093/schbul/22.1.69 [DOI] [PubMed] [Google Scholar]
- 60.Haller R, Kemmler G, Kocsis E, Maetzler W, Prunlechner R, Hinterhuber H. Schizophrenia and violence. results of a comprehensive inquiry in an Austrian providence. Article in German. Nervenarzt. 2001;72(11):859-866. doi: 10.1007/s001150170020 [DOI] [PubMed] [Google Scholar]
- 61.Casiano H, Hensel JM, Chartier MJ, et al. The intersection between criminal accusations, victimization, and mental disorders: a Canadian population-based study. Can J Psychiatry. 2020;65(7):492-501. doi: 10.1177/0706743720919660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Černý M, Hodgins S, Kučíková R, et al. Violence in persons with and without psychosis in the Czech Republic: risk and protective factors. Neuropsychiatr Dis Treat. 2018;14:2793-2805. doi: 10.2147/NDT.S167928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Refaat N, Fahmy M, El-Leithy W, Hassan H, El-Moez A. Frequency, severity and types of aggressive behavior among patients with schizophrenia at psychiatry outpatients clinic in comparison to normal controls. AJP. 2015;26(2):164-171.doi: 10.12816/0014483 [DOI] [Google Scholar]
- 64.Tsigebrhan R, Shibre T, Medhin G, Fekadu A, Hanlon C. Violence and violent victimization in people with severe mental illness in a rural low-income country setting: a comparative cross-sectional community study. Schizophr Res. 2014;152(1):275-282. doi: 10.1016/j.schres.2013.10.032 [DOI] [PubMed] [Google Scholar]
- 65.Soyka M, Graz C, Bottlender R, Dirschedl P, Schoech H. Clinical correlates of later violence and criminal offences in schizophrenia. Schizophr Res. 2007;94(1-3):89-98. doi: 10.1016/j.schres.2007.03.027 [DOI] [PubMed] [Google Scholar]
- 66.Arseneault L, Moffitt TE, Caspi A, Taylor PJ, Silva PA. Mental disorders and violence in a total birth cohort: results from the Dunedin Study. Arch Gen Psychiatry. 2000;57(10):979-986. doi: 10.1001/archpsyc.57.10.979 [DOI] [PubMed] [Google Scholar]
- 67.Hodgins S, Alderton J, Cree A, Aboud A, Mak T. Aggressive behaviour, victimization and crime among severely mentally ill patients requiring hospitalisation. Br J Psychiatry. 2007;191:343-350. doi: 10.1192/bjp.bp.106.06.029587 [DOI] [PubMed] [Google Scholar]
- 68.Lewis ET III, Dwyer RG. Psychosis and sexual offending: a review of current literature. Int J Offender Ther Comp Criminol. 2018;62(11):3372-3384. doi: 10.1177/0306624X17740016 [DOI] [PubMed] [Google Scholar]
- 69.Whiting D, Lichtenstein P, Fazel S. Violence and mental disorders: a structured review of associations by individual diagnoses, risk factors, and risk assessment. Lancet Psychiatry. 2021;8(2):150-161. doi: 10.1016/S2215-0366(20)30262-5 [DOI] [PubMed] [Google Scholar]
- 70.Coid JW, Ullrich S, Kallis C, et al. The relationship between delusions and violence: findings from the East London First Episode Psychosis Study. JAMA Psychiatry. 2013;70(5):465-471. doi: 10.1001/jamapsychiatry.2013.12 [DOI] [PubMed] [Google Scholar]
- 71.Lichtenstein P, Cederlöf M, Lundström S, et al. Associations between conduct problems in childhood and adverse outcomes in emerging adulthood: a longitudinal Swedish nationwide twin cohort. J Child Psychol Psychiatry. 2020;61(7):798-806. doi: 10.1111/jcpp.13169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125(4):e778-e786. doi: 10.1542/peds.2009-0597 [DOI] [PubMed] [Google Scholar]
- 73.Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med. 2015;128:316-326. doi: 10.1016/j.socscimed.2014.12.031 [DOI] [PubMed] [Google Scholar]
- 74.Appelbaum PS. In search of a new paradigm for research on violence and schizophrenia. Am J Psychiatry. 2019;176(9):677-679. doi: 10.1176/appi.ajp.2019.19070678 [DOI] [PubMed] [Google Scholar]
- 75.Fazel S, Wolf A, Larsson H, Lichtenstein P, Mallett S, Fanshawe TR. Identification of low risk of violent crime in severe mental illness with a clinical prediction tool (Oxford Mental Illness and Violence tool [OxMIV]): a derivation and validation study. Lancet Psychiatry. 2017;4(6):461-468. doi: 10.1016/S2215-0366(17)30109-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fazel S, Zetterqvist J, Larsson H, Långström N, Lichtenstein P. Antipsychotics, mood stabilisers, and risk of violent crime. Lancet. 2014;384(9949):1206-1214. doi: 10.1016/S0140-6736(14)60379-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bhavsar V, Kosidou K, Widman L, et al. Clozapine treatment and offending: a within-subject study of patients with psychotic disorders in Sweden. Schizophr Bull. 2020;46(2):303-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chang Z, Lichtenstein P, Långström N, Larsson H, Fazel S. Association between prescription of major psychotropic medications and violent reoffending after prison release. JAMA. 2016;316(17):1798-1807. doi: 10.1001/jama.2016.15380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sariaslan A, Leucht S, Zetterqvist J, Lichtenstein P, Fazel S. Associations between individual antipsychotics and the risk of arrests and convictions of violent and other crime: a nationwide within-individual study of 74 925 persons. Psychol Med. 2021;1-9. doi: 10.1017/S0033291721000556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sariaslan A, Lichtenstein P, Larsson H, Fazel S. Triggers for violent criminality in patients with psychotic disorders. JAMA Psychiatry. 2016;73(8):796-803. doi: 10.1001/jamapsychiatry.2016.1349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stevens H, Laursen TM, Mortensen PB, Agerbo E, Dean K. Post-illness-onset risk of offending across the full spectrum of psychiatric disorders. Psychol Med. 2015;45(11):2447-2457. doi: 10.1017/S0033291715000458 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eTable 1. Meta-Analyses of Observational Studies in Epidemiology (MOOSE) Checklist
eFigure 1. Flow Diagram for Updated Searches
eTable 2. Eligible studies reporting violent and homicide outcomes in people with schizophrenia spectrum disorders compared to general population controls identified in updated searches but not included in meta-analysis
eTable 3. Additional details of studies reporting violent outcomes in people with schizophrenia spectrum disorders compared to general population controls included in meta-analysis
eTable 4. Quality Assessment of Studies Included in Meta-Analyses
eFigure 2. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration in Register Studies
eFigure 3. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration By Study Quality
eFigure 4. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration By Study Design
eFigure 5. Forest Plot of Association Between Schizophrenia Spectrum Disorders Without Substance Misuse Comorbidity and Violence Perpetration
eFigure 6. Forest Plot of Association Between Schizophrenia Spectrum Disorders With Substance Misuse Comorbidity and Violence Perpetration
eFigure 7. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration by Region
eFigure 8. Odds of Violence Perpetration in Schizophrenia Spectrum Disorders and Unaffected Siblings Compared to General Population
eFigure 9. Forest Plot of Association Between Schizophrenia Spectrum Disorders and Violence Perpetration by Patient Sample
eTable 5. Details of studies reporting homicide perpetration as outcome in people with schizophrenia spectrum disorders compared to general population controls included in meta-analysis
eTable 6. Details of studies reporting sexual offence perpetration as outcome in people with schizophrenia spectrum disorders compared to general population controls included in meta-analysis
eResults
eReferences