Abstract
Background:
Osteochondral lesions of the talus (OLTs) are common injuries in young, active patients. Microfracture is an effective treatment for lesions less than 150 mm2 in size. Most commonly employed postoperative protocols involve delaying weightbearing for 6 to 8 weeks (DWB), though one study suggests that early weightbearing (EWB) may not be detrimental to patient outcomes. The goal of this research is to compare outcomes following EWB and DWB protocols after microfracture for OLTs.
Methods:
We performed a prospective, randomized, multicenter clinical trial of subjects with unilateral, primary, unifocal OLTs treated with microfracture. Thirty-eight subjects were randomized into EWB (18 subjects) and DWB (20 subjects) at their first postsurgical visit. The EWB group began unrestricted WB at that time, whereas the DWB group were instructed to remain strictly nonweightbearing for an additional 4 weeks. Primary outcome measures were the American Academy of Orthopaedic Surgery (AAOS) Foot and Ankle score and numeric rating scale (NRS) pain score.
Results:
The EWB group demonstrated significant improvement in AAOS Foot and Ankle Questionnaire scores at the 6-week follow-up appointment as compared to the DWB group (83.1 ± 13.5 vs 68.7 ± 15.8, P = .017). Following this point, there were no significant differences in AAOS scores between groups. At no point were NRS pain scores significantly different between the groups.
Conclusions:
EWB after microfracture for OLTs was associated with improved AAOS scores in the short term. Thereafter and through 2 years’ follow-up, no statistically significant differences were seen between EWB and DWB groups.
Level of Evidence:
Level II, prospective randomized trial.
Keywords: osteochondral lesions of the talus, rehabilitation, early weightbearing, ankle arthroscopy
Introduction
Osteochondral lesions of the talus (OLTs) are common injuries, occurring in up to half of ankle sprains and nearly three-quarters of ankle fractures 15,19 and in 27 per 100 000 person-years in young, active patients. 20 Nonoperative management of OLTs yields satisfactory results in 41% to 59% of cases and is attempted for Berndt and Hardy stage I and II lesions. 1,12 Those that do not recover with nonoperative management are candidates for operative intervention, for whom multiple operative options are available. Arthroscopic microfracture has been demonstrated to be an effective treatment technique for lesions less than 150 mm. 1,16,17,24 Microfracture results in the formation of fibrocartilage to fill articular cartilage defects, and has reported success rates of up to 85%. 4,11,22,23
Although there is no established gold standard for rehabilitation, most series on microfracture report strict nonweightbearing (NWB) for 6 to 8 weeks postoperatively. 4,11,22,23 This is intended to protect the site from shear forces and allow for the development of mature fibrocartilage. However, prolonged NWB is burdensome to patients, and anecdotally, many of our patients prior to this study reported noncompliance. 21 Despite the use of NWB in the postoperative period, cartilage degradation at the microfracture site has been shown at 1-year follow-up. Reported clinical outcomes tend to decrease as little as 2 years postoperatively. 2,7 -9
The purpose of this study was to determine what clinical consequence, if any, would occur if early weightbearing was allowed after microfracture for an osteochondral lesion of the talus. We hypothesized that there would be no difference in validated patient-reported outcome measure scores or pain scores between early and delayed weightbearing groups after microfracture for an OLT.
Patients/Methods
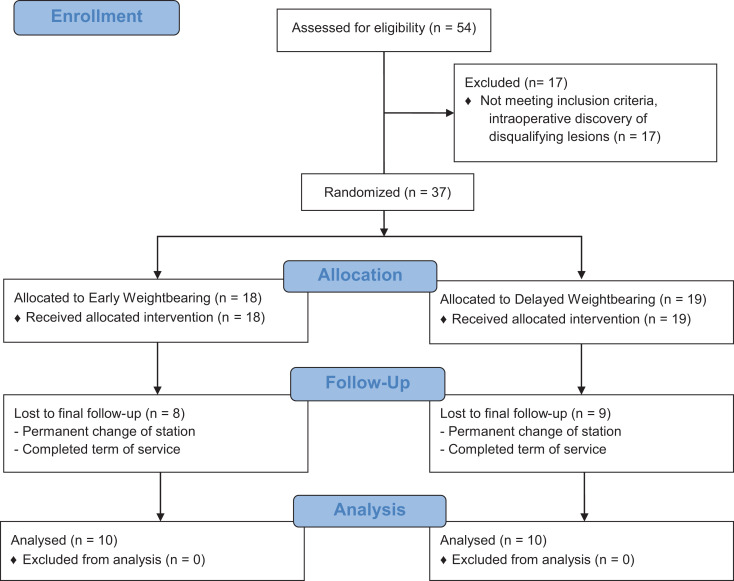
We performed a prospective, randomized, multicenter clinical trial. Patients were randomly assigned to 2 parallel groups in a 1:1 randomization ratio. The trial was conducted at 2 large military medical centers. Subjects aged 18-50 years with unilateral, primary, unifocal lesions were considered for inclusion. Subjects were excluded if they required a concomitant bony procedure (eg, calcaneal osteotomy), were pregnant, diagnosed with an inflammatory arthropathy, had a lesion larger than 150 mm2, preexisting arthritic changes on plain radiographs, multiple OLTs in 1 ankle, bifocal (kissing) lesions, or contralateral foot or ankle disease. Prior surgery on the affected ankle was grounds for exclusion; however, concomitant soft tissue procedure (eg, Brostrom) or anterior cheilectomy was allowed (Figure 1).
Figure 1.
CONSORT flow diagram.
All subjects were assessed with plain radiography as well as magnetic resonance imaging. The primary outcome measures were the American Academy of Orthopaedic Surgeons (AAOS) Foot and Ankle Outcomes Questionnaire and numeric rating scale (NRS) for pain. 5,12,13 The AAOS score is a validated, patient-based outcome instrument that measures function and provides a normative value for the background population. The NRS asks patients to rate their pain from 1 to 10 on a vertical grading line. This technique for pain measurement has high validity and ease of use and is preferred by patients. 10 Outcome measures were collected preoperatively and at the 6-week, 3-month, 6-month, 1-year, and 2-year time points. The treating surgeon scored each lesion on the Ferkel and Cheng, Anderson, and Outerbridge systems. 1,7
Subjects underwent ankle arthroscopy with standard anterolateral and anteromedial portals. The OLT was identified and characterized based on size, location, and depth. Concomitant pathology was noted and addressed as indicated intraoperatively. Microfracture was performed in accordance with the protocol established by Steadman et al. 20 All patients were treated by fellowship-trained foot and ankle orthopedic surgeons.
All patients were initially placed in a bulky posterior splint and made NWB for the first 2 weeks postoperatively to reduce the chance of developing a synovial fistula. 3 At 2 weeks, rigid immobilization was removed and the patients were placed in a removable walking boot, and physical therapy focusing on passive and active range of motion was initiated. Subjects were randomized to either the early (EWB) or delayed (DWB) groups at the 2-week visit.
Randomization was achieved through use of a computerized random number generator. Envelopes with the randomization assignment were prepared by a nonclinical research coordinator, then sealed until at the time of first follow-up. Patients were enrolled by the operating surgeon. As subjects were responsible for maintaining the appropriate weightbearing status, blinding was not possible.
Pre hoc power analysis was performed to detect an effective size of 15 points on the AAOS Foot and Ankle Questionnaire, indicating 24 patients per arm would be required with α = 0.05. To account for 10% loss to follow-up, a total of 54 patients were required. Results were compared using the Student t test and sequential measures analysis.
Results
Fifty-four subjects were enrolled from 2011 to 2015. Seventeen subjects who were enrolled failed screening criteria, leaving 39 enrolled in the study eligible for randomization (18 EWB, 20 DWB). There was no crossover between the groups. Screen failures were due to findings of lesions >1.5 cm2 and multifocal lesions. Patients were followed for 2 years after surgery. At the time of surgery, the average age of subjects in our cohort was 34.1 (range, 21-50) years. Eighty-six percent of subjects were male. The mechanisms of injury were as follows: 6 falls, 6 traumas, 16 twisting injuries, and 9 unknown. The lesions were predominantly lateral (64%), and most were graded Outerbridge III (55%), Ferkel III and IV (respectively, 40% and 25%), and Anderson III (63%). 6,18 Concomitant procedures included Brostrom-Gould, loose body removal, anterior cheilectomy, and peroneus brevis repair (Table 1). No significant differences were found in demographic characteristics, lesion locations, lesion stages, or injury mechanisms between groups. There were no operative complications reported. No patient underwent reoperation on the study ankle within the 2-year follow-up period.
Table 1.
Concomitant Procedures Undertaken in Addition to Diagnostic Arthroscopy and Microfracture of OLTs Are Tabulated by Study Group.
| EWB Subject | Concomitant Procedure | DWB Subject | Concomitant Procedure |
|---|---|---|---|
| 1 | Anterior cheilectomy, Brostrom-Gould | 1 | Brostrom-Gould |
| 2 | Brostrom-Gould | 2 | Brostrom-Gould |
| 3 | Loose body removal, Brostrom-Gould | 3 | Brostrom-Gould |
| 4 | Brostrom-Gould | 4 | Peroneus brevis repair |
| 5 | Anterior cheilectomy | 5 | Anterior cheilectomy |
| 6 | Loose body removal |
Abbreviations: DWB, delayed weightbearing; EWB, early weightbearing; OLTs, osteochondrous lesions of the talus.
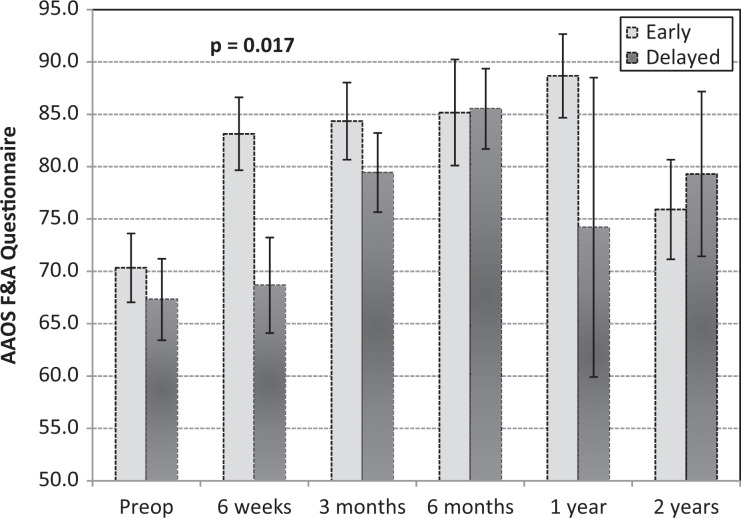
The EWB cohort demonstrated significantly improved AAOS scores at the 6-week follow-up visit compared to the DWB group (83.1 ± 13.5 vs 68.7 ± 15.8, P = .017; Figure 2). At the other time points, no significant differences were observed between the 2 cohorts. At 6 weeks, AAOS scores in the EWB group were significantly higher than preoperative values (P = .010). By 3 months, the DWB cohort was also significantly improved over preoperative status (P = .037). Thereafter, average AAOS scores were higher than preoperative values in both cohorts. This difference failed to reach statistical significance at the 2-year point in the EWB group, and the 1-year point in the DWB group.
Figure 2.
AAOS Foot and Ankle Questionnaire scores are displayed from preoperative values through 2 years of follow-up. AAOS, American Academy of Orthopaedic Surgery foot and ankle score.
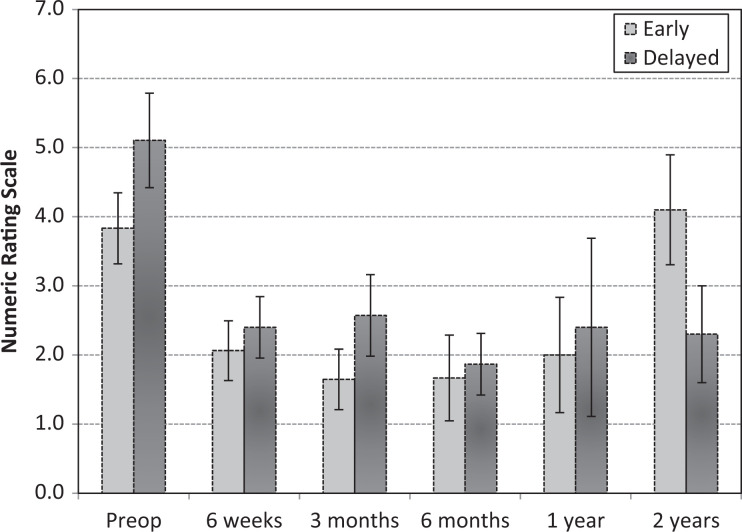
There were no significant differences in NRS pain scores between the 2 cohorts at any time point (Table 2). Both cohorts reported significantly improved pain compared to baseline by 6 weeks postoperatively. Thereafter, the average NRS scores were lower than preoperative baseline, except at the 2-year point in the EWB group, where NRS was increased but not significantly different (3.8 vs 4.1, P = .370; see Figure 3).
Table 2.
Statistical Comparison of Early and Delayed Weight-Bearing Cohorts Is Tabulated.a
| Early Weightbearing | Delayed Weightbearing | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| NRS | N | Mean | SE | SM | N | Mean | SE | SM | t test |
| Preop | 18 | 3.8 | 0.51 | n/a | 19 | 5.1 | 0.68 | n/a | 0.149 |
| 6 wk | 16 | 2.1 | 0.43 | < 0.001 | 20 | 2.5 | 0.44 | < 0.001 | 0.595 |
| 3 mo | 17 | 1.6 | 0.44 | < 0.001 | 14 | 2.6 | 0.59 | < 0.001 | 0.209 |
| 6 mo | 12 | 1.7 | 0.83 | < 0.001 | 15 | 1.9 | 0.45 | < 0.001 | 0.79 |
| 1 y | 9 | 2 | 0.83 | < 0.001 | 5 | 2.4 | 1.29 | 0.019 | 0.79 |
| 2 y | 10 | 4.1 | 0.8 | 0.37 | 10 | 2.3 | 0.7 | < 0.001 | 0.107 |
| AAOS | N | Mean | SE | SM | N | Mean | SE | SM | |
| Preop | 18 | 70.3 | 3.3 | n/a | 19 | 67.3 | 3.9 | n/a | 0.559 |
| 6 wk | 15 | 83.1 | 3.5 | < 0.001 | 12 | 68.7 | 4.6 | 0.5 | 0.017 |
| 3 mo | 17 | 84.4 | 3.7 | < 0.001 | 14 | 79.4 | 3.8 | 0.003 | 0.361 |
| 6 mo | 12 | 85.2 | 5.1 | < 0.001 | 15 | 85.5 | 3.8 | < 0.001 | 0.954 |
| 1 y | 9 | 88.7 | 4 | < 0.001 | 5 | 74.2 | 14.3 | 0.253 | 0.378 |
| 2 y | 10 | 75.9 | 4.75 | 0.219 | 10 | 79.3 | 7.9 | 0.046 | 0.716 |
Abbreviations: AAOS, American Academy of Orthopaedic Surgery foot and ankle score; NRS, numeric rating scale; SE, standard error; SM, sequential measures.
aOf note, the sequential measures (SM columns) analysis compares preoperative values of that group to subsequent time points.
Figure 3.
Numeric rating scale pain scores are displayed from preoperative values through 2 years of follow-up.
Discussion
In this study comparing EWB to DWB following microfracture for treatment of OLT, we found that the EWB group had significantly improved AAOS scores at 6 weeks after surgery relative to baseline score, whereas significant improvement over baseline score did not occur in the DWB group until 3 months after surgery. Thereafter, both groups demonstrated improvement in AAOS scores through 2 years’ follow-up. We believe that these data suggest that patients will bear weight early if permitted, and functionally benefit during that time period. No significant detrimental effects from EWB were seen in our study. These results agree with those of another larger study of weightbearing after microfracture (which was powered to demonstrate noninferiority through 2 years). 14
Both groups demonstrated significant improvement in pain as measured by NRS by the 6-week visit. This improved outcome was maintained except at the 2-year time point in the EWB group, where there was a nonsignificant increase in pain over baseline. This increase in pain is accounted for by one outlier with a new, acute injury. There were no significant differences in NRS scores between the groups at any time point.
There is no established gold standard for rehabilitation after microfracture of the talus, and while many protocols encourage delayed weightbearing, earlier weightbearing and mobilization is preferable if long-term outcomes are not compromised. As delayed weightbearing has been correlated with decreased social functioning measured with the RAND-36 questionnaire in the setting of Achilles tendon injuries. 12 The practice of delayed weightbearing after bone marrow stimulation was first challenged in the knee literature. 5,8 Good results have been reported with early weightbearing after microfracture or chondroplasty of femoral condyle osteochondral defects. Although the ankle and knee function in different biomechanical environments, the knee has significantly more degrees of freedom than the constrained tibiotalar articulation. As such, it stands to reason that early weightbearing may be safe in the ankle as well as the knee. One prior study reported on 81 patients randomized to EWB and DWB following microfracture for OLTs. 16 They showed non-inferiority of early weightbearing from 3 months to 2 years of follow-up. They did not report on the earlier 6-week time point. Notably, the patient-reported outcomes measure used in this study has not been validated. 6,18 We acknowledge several limitations to this study. Notably, this is a small study and poor follow-up leaves us underpowered to demonstrate noninferiority at 1- and 2-year follow-up for our primary outcome measure. Despite this, we demonstrated significant improvement in AAOS scores at early follow-up. Second, use of the AAOS Foot and Ankle Questionnaire makes comparison with prior studies in the field difficult, though the AAOS questionnaire is validated and has excellent testing characteristics, which may yield more reliable data in future studies. 18 We did not assess compliance with the weightbearing restrictions in the delayed group and cannot confirm that these patients adhered to the protocol. Follow-up through 2 years may not reveal differences between the groups that could become apparent at longer term. However, we anticipated that most complications related directly to early weightbearing would appear within the first few months after surgery. Lastly, as our study included many active duty service members, it may not be generalizable to the general population. Active duty service members undergo significant physical training and may have less ability to modify their activity.
Conclusions
In this study of early vs delayed weight-bearing following microfracture for the treatment of OLT, the early weightbearing group demonstrated greater improvement in patient outcome scores at 6 weeks after surgery than the delayed weightbearing group. However, differences between the 2 groups were not found at subsequent time points. These findings suggest that it may be reasonable to consider EWB following microfracture for the treatment of OLTs.
Supplemental Material
Supplemental Material, FAO838832-ICMJE for Early vs Delayed Weightbearing After Microfracture of Osteochondral Lesions of the Talus: A Prospective Randomized Trial by J. Banks Deal, Jeanne C. Patzkowski, Adam T. Groth, Paul M. Ryan, Thomas C. Dowd, Patrick M. Osborn, Claude D. Anderson, James R. Ficke and Kevin L. Kirk in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: J. Banks Deal Jr, MD, Adam T. Groth, MD, Thomas C. Dowd, MD, and Kevin L. Kirk, DO, report this is part sponsored by a research grant from the American Orthopaedic Foot & Ankle Society. ICMJE forms for all authors are available online.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Supported by a grant from the American Orthopaedic Foot & Ankle Society with funding from the Orthopaedic Foot & Ankle Foundation.
ORCID iD: J. Banks Deal Jr, MD, CPT,  https://orcid.org/0000-0002-5385-4240
https://orcid.org/0000-0002-5385-4240
References
- 1. Anderson IF, Crichton KJ, Grattan-Smith T, Cooper RA, Brazier D. Osteochondral fractures of the dome of the talus. J Bone Joint Surg Am. 1989;71(8):1143–1152. [PubMed] [Google Scholar]
- 2. Angermann P, Jensen P. Osteochondritis dissecans of the talus: long-term results of surgical treatment. Foot Ankle. 1989;10(3):161–163. [DOI] [PubMed] [Google Scholar]
- 3. Barber FA, Click J, Britt BT. Complications of ankle arthroscopy. Foot Ankle. 1990;10(5):263–266. [DOI] [PubMed] [Google Scholar]
- 4. Donnenwerth MP, Roukis TS. Outcome of arthroscopic debridement and microfracture as the primary treatment for osteochondral lesions of the talar dome. Arthroscopy. 2012;28(12):1902–1907. [DOI] [PubMed] [Google Scholar]
- 5. Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37(4):378–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM. Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int. 2007;28(2):154–161. [DOI] [PubMed] [Google Scholar]
- 7. Ferkel RD. Ankle and subtalar arthroscopy. In: Kelikian AS, ed. Operative Treatment of the Foot and Ankle. New York, NY: Appleton & Lange; 1999. [Google Scholar]
- 8. Ferkel RD, Zanotti RM, Komenda GA, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 2008;36(9):1750–1762. [DOI] [PubMed] [Google Scholar]
- 9. Furukawa T, Eyre DR, Koide S, Glimcher MJ. Biochemical studies on repair cartilage resurfacing experimental defects in the rabbit knee. J Bone Joint Surg Am. 1980;62(1):79–89. [PubMed] [Google Scholar]
- 10. Gagliese L, Weizblit N, Ellis W, Chan VW. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain. 2005;117(3):412–420. [DOI] [PubMed] [Google Scholar]
- 11. Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25(12):1478–1490. [DOI] [PubMed] [Google Scholar]
- 12. Guyton GP. Theoretical limitations of the AOFAS scoring systems: an analysis using Monte Carlo modeling. Foot Ankle Int. 2001;22(10):779–787. [DOI] [PubMed] [Google Scholar]
- 13. Johanson NA, Liang MH, Daltroy L, Rudicel S, Richmond J. American Academy of Orthopaedic Surgeons lower limb outcomes assessment instruments. Reliability, validity, and sensitivity to change. J Bone Joint Surg Am. 2004;86(5):902–909. [DOI] [PubMed] [Google Scholar]
- 14. Lee DH, Lee KB, Jun ST, Seon JK, Kim MS, Sung IH. Comparison of early versus delayed weightbearing outcomes after microfracture for small to midsized ostechondral lesions of the talus. Am J Sports Med. 2012;40(9):2023–2028. [DOI] [PubMed] [Google Scholar]
- 15. Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg Am. 2009;91(2):333–339. [DOI] [PubMed] [Google Scholar]
- 16. McCullough CJ, Venugopal V. Osteochondritis dissecans of the talus: the natural history. Clin Orthop Relat Res. 1979;144:264–268. [PubMed] [Google Scholar]
- 17. Murawski CD, Kennedy JG. Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 2013;95(11):1045–1054. [DOI] [PubMed] [Google Scholar]
- 18. Orr JD, Dutton JR, Fowler JT. Anatomic location and morphology of symptomatic, operatively treated osteochondral lesions of the talus. Foot Ankle Int. 2012;33(12):1051–1057. [DOI] [PubMed] [Google Scholar]
- 19. Saxena A, Eakin C. Articular talar injuries in athletes: results of microfracture and autogenous bone graft. Am J Sports Med. 2007;35(10):1680–1687. [DOI] [PubMed] [Google Scholar]
- 20. Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;391(suppl):S362–S369. [DOI] [PubMed] [Google Scholar]
- 21. Suchak AA, Bostick GP, Beaupre LA, Durand DC, Jomha NM. The influence of early weight-bearing compared with non-weight-bearing after surgical repair of the Achilles tendon. J Bone Joint Surg Am. 2008;90(9):1876–1883. [DOI] [PubMed] [Google Scholar]
- 22. Tol JL, Struijs PA, Bossuyt PM, Verhagen RA, van Dijk CN. Treatment strategies in osteochondral defects of the talar dome: a systematic review. Foot Ankle Int. 2000;21(2):119–126. [DOI] [PubMed] [Google Scholar]
- 23. Zengerink M, Struijs PA, Tol JL, van Dijk CN. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zengerink M, Szerb I, Hangody L, Dopirak RM, Ferkel RD, van Dijk CN. Current concepts: treatment of osteochondral ankle defects. Foot Ankle Clin. 2006;11(2):331–359. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO838832-ICMJE for Early vs Delayed Weightbearing After Microfracture of Osteochondral Lesions of the Talus: A Prospective Randomized Trial by J. Banks Deal, Jeanne C. Patzkowski, Adam T. Groth, Paul M. Ryan, Thomas C. Dowd, Patrick M. Osborn, Claude D. Anderson, James R. Ficke and Kevin L. Kirk in Foot & Ankle Orthopaedics