Abstract
Hallux valgus is a common condition that results from a complex positional deformity of the first ray. The bunion or medial prominence that results from the lateral deviation and pronation of the hallux is only one component of the 3-dimensional deformity. Hallux valgus can lead to considerable pain and altered joint mechanics. The precise biomechanical etiology remains under debate. Predisposing factors include female sex, age, constricting footwear, and family history. Metatarsus adductus, equinus contracture, hammertoe deformity, and pes planus often coexist with hallux valgus. Nonoperative treatment involves patient education, shoe modifications, toe pads and positioning devices, and activity modifications. Surgery is considered in patients who fail nonoperative treatment with the goal of pain relief, correction of the deformity, improved first ray stability, and improved quality of life. More than 100 different procedures have been described to treat hallux valgus; they include combinations of soft tissue balancing, metatarsal osteotomies, and fusion of either the metatarsophalangeal (MTP) or tarsometatarsal (TMT) joint. The choice of procedures depends on the severity and location of the deformity as well as surgeon preference. Recent advances in operative techniques include minimally invasive surgery and correction of rotational deformity.
Keywords: hallux valgus, bunion, metatarsal osteotomy, Lapiplasty
Introduction
Hallux valgus is a complex positional deformity of the first ray that leads to altered joint mechanics, dysfunction, and progressive pain often at the medial eminence of the first metatarsophalangeal (MTP) joint. Hallux valgus is a common condition with an estimated prevalence of 23% in adults 18-65 years of age and 35.7% in those older than 65 years. There is a higher prevalence in females with varying ratios reported in the literature, ranging from as low as 2:1 or as high as 15:1 females affected for every male. 60,62,72
Etiology
Although the precise biomechanical etiology of hallux valgus is not well understood, it is known that the medial prominence or bunion is the result of both the medial deviation of the first metatarsal and the lateral deviation and pronation of the hallux. A number of factors have been identified that create a predisposition for the development of hallux valgus, including female gender, age, constricting footwear, and genetics. 16,19 Hallux valgus is more common in females, which is likely related to differences in footwear, osseous anatomy, generalized ligamentous laxity, and first ray hypermobility in females. 70 Constricting footwear, such as high heels, is considered an extrinsic predisposing factor for hallux valgus because of increased first metatarsal loading and valgus stress at the first MTP joint as the foot slides forward into the narrow toe-box during gait. 14,54,58 The prevalence of hallux valgus increases with age because of alterations in joint mechanics and plantar loading patterns that occur with aging. 83 Hallux valgus also appears to have a strong genetic predisposition. In a large Level IV study, 90% of patients with hallux valgus had at least 1 similarly affected family member (n = 350). Although the exact inheritance pattern remains unclear, it is suspected that inheritance is autosomal dominant with incomplete penetrance. 72 Other potential predisposing factors for hallux valgus include metatarsus adductus, first ray hypermobility, pes planus, equinus contracture, ligamentous laxity, and length of the first metatarsal. 28
Pathophysiology
The first ray is inherently unstable because its stability depends on several static and dynamic structures at the first metatarsophalangeal (MTP) and first tarsometatarsal (TMT) joints. The first stage in hallux valgus deformity is thought to be attenuation of the medial supporting structures of the first ray, which results in medial deviation of the first metatarsal and lateral deviation and pronation of the hallux, causing a progressive varus deformity at the first TMT joint. As the metatarsal head drifts medially and rotates (in the frontal plane), its position in relation to the sesamoid apparatus is altered. As a result, the first metatarsal head now rests on the medial sesamoid, while the lateral sesamoid rests in the first intermetatarsal (IM) space. In addition, the deformity at the MTP joint subsequently allows the hallux flexor and extensor tendons to bowstring laterally, exerting a further deforming force while the displaced abductor hallucis plantar flexes and pronates the phalanx. The medial prominence at the first MTP joint is due to increased prominence of the first metatarsal head. 22,47,66,70,90
Concomitant Disorders
Metatarsus adductus
The prevalence of metatarsus adductus is high in patients with hallux valgus. 3 Concomitant metatarsus adductus is believed to make corrective surgical procedures more difficult and result in higher recurrence rates for patients with hallux valgus, related to increased forefoot adduction, loss of a buttress effect of the lesser metatarsals, and underestimation of the degree of deformity using IMA because of second metatarsal adduction. 2,97 A comprehensive approach must be taken to adequately correct hallux valgus with concomitant metatarsus adductus, which may require addressing the second and third metatarsal, as well as any other associated lesser toe deformities. 84
Hammertoe
Hammertoe deformity has been shown to have a strong association with hallux valgus. Most consider hammertoe to be chiefly a secondary deformity as the hallux “crowds” the second toe position. This deformity is also thought to result from the long flexor tendon overpowering the intrinsic tendons. 33,56 Additionally, the hallux valgus deformity impedes normal function of the forefoot during the gait cycle transferring pressure from the great toe and overloading the lesser metatarsal heads. 96
Achilles tendon contracture
Hallux valgus is associated with a higher prevalence of Achilles tendon contracture. 23 A tight Achilles tendon results in increased forefoot pronation and increased valgus forces on the foot. As a result, the peroneus longus loses its stabilizing effect on the first metatarsal in the frontal plane, which results in decreased stability of the first ray and medial column of the foot. 4,39,40,77,78 The first line of treatment is Achilles tendon stretching exercises.
Medial column collapse (pes planus)
Flatfoot deformity has a strong association with hallux valgus deformity as a result of its effect on medial column stability. 85 Pes planus results in increased pronation of the first ray, which increases loading at the medial and plantar aspect of the first ray during heel rise. 70 The first line of treatment for pes planus is orthotics, but this does not directly treat the hallux valgus deformity.
Clinical Evaluation
History
Patients with hallux valgus typically present with pain on the medial aspect of the forefoot. Patients may also report pain of the lesser toes due to associated hammertoe deformity or the transfer metatarsalgia related to altered gait patterns. Patients may report a noticeable bump or prominence on the medial aspect of the forefoot. There may also be complaints of difficulty with certain types of footwear because of the medial prominence at the first MTP joint. Patients typically describe persistent symptoms despite already attempting footwear or activity modifications.
Physical Examination
The physical examination involves a thorough foot evaluation in both a seated and standing position. The foot should be inspected for any skin changes or lesions, toenail changes, and general position of the first ray. Determine the specific location of pain based on history and palpation of the foot. Pain at the medial eminence is typical of patients with hallux valgus. Patients may also report generalized pain at the first MTP joint, pain related to lesser toe deformities, or pain at the lesser metatarsal heads due to transfer metatarsalgia. A thorough neurovascular examination is important to rule out neurovascular insufficiency. The first ray should be assessed for range of motion, ligamentous laxity or contractures, and passive correction of the deformity, including internal rotation of the hallux to allow for assessment of the reducibility of the first ray in the frontal plane. 21 The first MTP joint should be fully evaluated for any skin changes, pain, crepitus, or decreased motion consistent with arthritic changes. It is important to evaluate for any other concomitant processes including hammertoe deformity, pes planus, equinus of the Achilles complex, or first ray hypermobility.
Radiographic Examination
Weight-bearing anteroposterior (AP), lateral, and axial sesamoid views of the affected limb should be obtained. The hallux valgus angle (HVA), 1-2 intermetatarsal angle (IMA), and distal metatarsal articular angle (DMAA) are all measured from the AP view (Figure 1A). 13 The DMAA is the angle formed between the distal articular surface and longitudinal axis of the first metatarsal (Figure 2). It is used to assess first MTP joint congruity, and <10 degrees is considered normal. 17 The reliability of the HVA and IMA has been confirmed in multiple studies, while the DMAA has proven less reliable. 17,19,49 Changes in the DMAA may be more related to rotation of the metatarsal head than true angulation changes, which could explain the poor reliability of this measurement. Consideration should also be given to the hallux valgus interphalangeus (HVI) angle, formed from the longitudinal axis of the distal phalanx and proximal phalanx, because an adjunctive procedure such as an Akin osteotomy may be necessary for complete correction of the deformity when an increased HVI angle is noted. 17
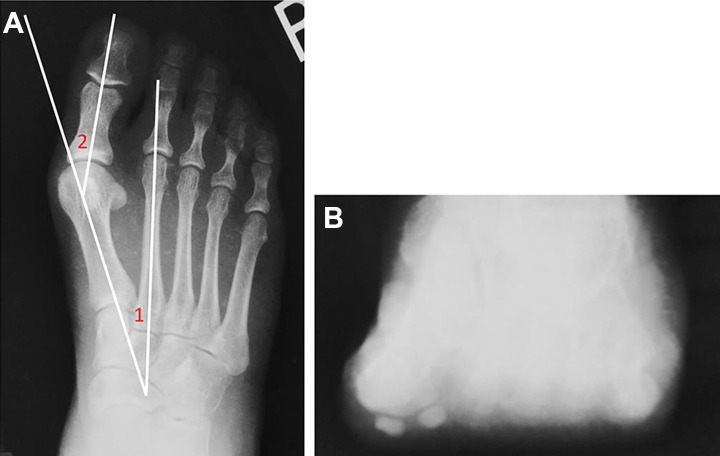
Figure 1.
(A) Traditional hallux valgus measures demonstrated on anteroposterior (AP) radiographs. The number 1 corresponds to the first-second intermetatarsal angle (IMA); the number 2 corresponds to the hallux valgus angle (HVA). (B) Shows the axial sesamoid view demonstrating the normal anatomic location of the sesamoids in relation to the crista.
Figure 2.

The distal metatarsal articular angle (DMAA) is shown, which can be used to assess first metatarsophalangeal (MTP) joint congruity.
The sesamoid axial view is important to evaluate the position of the sesamoids in relation to the cristae of the first metatarsal head and to evaluate for subluxation of the sesamoids or rotation of the first metatarsal (Figure 1B). The presence of a “round sign” evaluates the shape of the lateral edge of the first metatarsal head on AP radiographs and can also be used to assess rotation of the first metatarsal. 63 It is important to evaluate the first MTP joint for any evidence of arthritic changes. Weight-bearing computed tomographic (CT) scanning is emerging as a valuable tool to provide a 3-dimensional analysis of hallux valgus to further clarify the pathogenesis of the deformity. 44,45
Classification Systems
Traditional classification methods have used the AP view on radiographs to determine severity of hallux valgus in the frontal plane based on the HVA, IMA, and DMAA. Normal is defined as HVA <15 degrees, IMA <9 degrees, and DMAA <10 degrees. Mild deformity corresponds to HVA <20 degrees and IMA <11 degrees. Moderate hallux valgus involves an HVA of 20 to 40 degrees and an IMA of 11 to 16 degrees. Severe deformity corresponds to an HVA >40 degrees and an IMA >16 degrees (Table 1, Figure 3). 19,88
Table 1.
Traditional Radiographic Classification of Hallux Valgus Deformity (Severity Based).
| Severity of Deformity | Hallux Valgus Angle (HVA) | First-Second Intermetatarsal Angle (IMA) | Treatment |
|---|---|---|---|
| Normal | <15° | <9° | None |
| Mild | <20° | 9-11° | Distal osteotomy ± soft tissue procedure |
| Moderate | 20-40° | 11-16° | Proximal osteotomy ± soft tissue procedure |
| Severe | >40° | >16° | Proximal osteotomy or first tarsometatarsal arthrodesis ± soft tissue procedure |
Figure 3.
Traditional severity-based hallux valgus classification shows (A) mild hallux valgus, (B) moderate hallux valgus, and (C) severe hallux valgus.
A new classification system of hallux valgus has been proposed that takes into account the complex triplanar nature of the deformity. It focuses on determining the apex of the deformity using the anatomic center of rotation of angulation (CORA) principle. 35 The triplane hallux valgus classification system uses AP, lateral, and axial radiographs to categorize the deformity into 4 types. Type 1 involves increased HVA and IMA, no first metatarsal pronation, and no evidence of first MTP joint degeneration. Type 2 involves increased HVA and IMA along with first metatarsal pronation either with (2b) or without (2a) sesamoid subluxation on axial radiographs. Type 3 involves increased HVA and IMA, first metatarsal pronation, and metatarsus adductus >20 degrees. Finally, type 4 involves increased HVA and IMA with or without first metatarsal pronation, in addition to degenerative joint disease of the first MTP joint (Table 2, Figure 4). 82 Validation studies for this new classification system are under way.
Table 2.
Triplane Hallux Valgus Classification and Treatment (Anatomic Based).
| Classification | Anatomic Findings | MTP Joint Status | Author’s Preferred Treatment |
|---|---|---|---|
| Type 1 | Increased HVA and IMA No first metatarsal pronation on radiographs Sesamoids may be subluxed |
No clinical or radiographic evidence of DJD | Transverse plane corrective procedure ± distal soft tissue procedures |
| Type 2a | Increased HVA and IMA First metatarsal pronation on AP and sesamoid radiographs No sesamoid subluxation |
No clinical or radiographic evidence of DJD | Triplane first tarsometatarsal (TMT) arthrodesis ± distal soft tissue procedures |
| Type 2b | Increased HVA and IMA First metatarsal pronation on AP and sesamoid radiographs With sesamoid subluxation |
No clinical or radiographic evidence of DJD | Triplane first TMT arthrodesis + lateral release ± Akin’s osteotomy |
| Type 3 | Increased HVA and IMA >20 degrees metatarsus adductus angle |
No clinical or radiographic evidence of DJD | Triplane first TMT arthrodesis + second and third metatarsal transverse plane correction |
| Type 4 | Increased HVA and IMA ± first metatarsal pronation |
Clinical and/or radiographic evidence of DJD | First MTP arthrodesis |
Abbreviations: DJD, degenerative joint disease; HVA, hallux valgus angle; IMA, intermetatarsal angle; MTP, metatarsophalangeal.
Figure 4.
New anatomical-based hallux valgus classification. Type 1 depicted in panels A and B involves increased hallux valgus angle (HVA) and intermetatarsal angle (IMA), no metatarsal pronation, and no sesamoid subluxation. Type 2 involves the addition of metatarsal pronation either without sesamoid subluxation as in panels C and D or with sesamoid subluxation as in panels E and F. Type 3 incorporates metatarsus adductus > 20 degrees as in panels G and H. Type 4 incorporates degenerative changes at the first metatarsophalangeal (MTP) joint as in panels I and J.
Treatment
Nonoperative Management
Nonoperative treatment of hallux valgus consists of symptomatic management with the goal of decreasing irritation of the medial eminence. Patients should be educated on proper footwear and including comfortable shoes with a wide toe box to help decrease pain, blistering, and inflammation of the bursa. 15 Toe spacers and cushions can also help to further mitigate pain. Patients should be counseled that although shoe and activity modifications may reduce the symptoms, they do not correct the underlying pathology and thus will not reduce the deformity.
Operative Management
Surgical intervention should be reserved for those individuals who have failed nonoperative treatment due either to persistent problems with shoe wear or pain. The appearance of the foot in the absence of other symptoms is not an indication for surgery.
The choice of surgical procedure has traditionally been based on the severity of the deformity determined using HVA and IMA measured on the weight bearing AP radiograph (Table 1). 19,76,88 There are more than 100 procedures described for treatment of hallux valgus; most often, they include a combination of soft tissue–balancing procedures, bony osteotomies, and fusions (Figure 5). The recent growth in the use of 3-dimensional weight-bearing CT has drawn attention to the rotational and sagittal plane components of the hallux valgus deformity and has led to the development of new surgical techniques that address the 3-dimensional nature of the deformity. 44,45
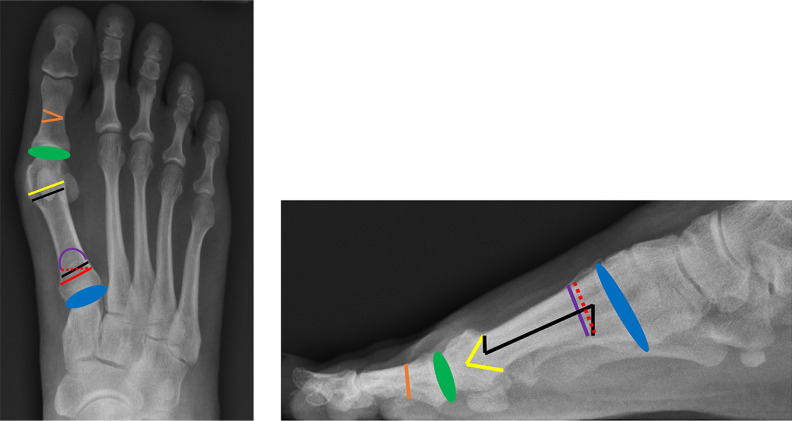
Figure 5.
Anteroposterior (AP) and lateral view demonstrating various surgical options to correct hallux valgus. Shown is Akin osteotomy (orange), metatarsophalangeal (MTP) fusion (green), distal chevron osteotomy (yellow), scarf osteotomy (black), proximal opening wedge osteotomy (red), proximal crescentic osteotomy (purple), and a tarsometatarsal (TMT) fusion (Lapidus; blue).
Soft-tissue procedures
The modified McBride procedure is a distal soft tissue procedure mostly used as an adjunct with other hallux valgus corrective surgeries such as proximal osteotomies and Lapidus procedure. This procedure involves release of the adductor hallucis and lateral sesamoid suspensory ligament. Completion of the procedure typically involves shaving the medial eminence and plication of the medial capsule. Two surgical approaches have been described: one technique involving a medial trans-articular approach and the other involving an incision at the dorsal first webspace. The most common approach is through the first dorsal webspace due to better visualization and easier access to the lateral soft tissues. In moderate to severe deformities, the modified McBride may be used as an adjunct to metatarsal osteotomies. Excellent patient satisfaction scores and significant improvements in AOFAS scores have been reported when the modified McBride is combined with a distal chevron osteotomy. However, the modified McBride should not be used in isolation to treat hallux valgus, as evidence shows inferior results and high recurrence rates when used in isolation compared to distal metatarsal osteotomies. 7,41,48,98
Akin osteotomy
The Akin osteotomy is a medial-based closing wedge osteotomy of the first proximal phalanx. An Akin osteotomy is typically performed as an adjunct to other procedures, such as a distal Chevron osteotomy, if the hallux valgus interphalangeus (HVI) angle is >10 degrees. A longitudinal, medial incision is made along the first proximal phalanx, and a small wedge of bone is removed. It is important to keep the lateral cortex integrity intact; otherwise, there is a risk of destabilization of the osteotomy. 25
Distal metatarsal osteotomies
Distal chevron osteotomy
The distal chevron osteotomy is indicated in mild to moderate hallux valgus deformity. This procedure is performed creating a V-shaped cut into the distal metatarsal head/neck with lateral displacement of the distal fragment. The benefits of this procedure are the inherent stability to dorsiflexion and the minimal amount of metatarsal shortening. Favorable outcomes have been reported in the literature utilizing the distal chevron osteotomy, specifically for mild deformity. 59,92 Recent Level IV evidence showed improved Foot and Ankle Outcome Scores (FAOS) in a large cohort of patients with mild to moderate hallux valgus after distal chevron osteotomy (n=250). 93
Long arm chevron osteotomy
The long arm chevron osteotomy allows for correction of greater deformities by extending the plantar limb of the osteotomy. 51 The concept is to improve the contact between the distal fragment and the proximal fragment to increase the stability of the correction and allow for greater correction of the deformity. A recent Level I study compared the long arm chevron osteotomy to the scarf osteotomy and found that both techniques had comparable results in correcting moderate to severe hallux valgus. However, the long arm distal chevron was superior to the scarf osteotomy in regard to magnitude of IMA correction (9.1 vs 7.1 degrees, P = .007). 51 The long arm distal chevron osteotomy is generally considered a less technically challenging option for moderate to severe hallux valgus. At this time, both the scarf osteotomy and the long arm chevron osteotomy appear to be viable options to correct moderate to severe hallux valgus.
Biplanar chevron osteotomy
The biplanar chevron osteotomy allows simultaneous correction of mild hallux valgus and reduction of the DMAA. Cuts are made similar to a standard distal chevron osteotomy; however, more bone is removed from the dorsomedial and plantar medial limbs. Additionally, an oblique medial wedge is excised. This allows lateral translation of the metatarsal head as well as restoration of MTP joint congruency. 29,20 Evidence to support this procedure is limited though patient satisfaction and functional outcomes are favorable. 8,59
Diaphyseal metatarsal osteotomies
Scarf osteotomy
The scarf osteotomy is typically used to treat moderate to severe hallux valgus. The procedure is performed with 3 separate osteotomy cuts. The first cut involves creating a longitudinal, plantar sloping cut of the proximal and distal metatarsal diaphysis. Chevron osteotomies are then performed distally in the dorsal cortex and proximally in the plantar cortex with the head fragment being translated laterally. Good to excellent outcomes have been shown using the scarf osteotomy. 1,5 A recent Level IV study showed that, at an average follow-up of 10 years, patients who received a scarf osteotomy with lateral release had an improvement in AOFAS scores from 57 points preoperatively to 95 points postoperatively (P < .05). They also showed significant (P < .05) improvement of the HVA, IMA, and DMAA; however, there was a recurrence (HVA >20 degrees) rate of 30% at 10-year follow-up. 5 A potential downside is that the scarf osteotomy has been described as being technically challenging. Complication rates have been described from 6% up to 47%. 11,87 The most common complication is troughing, which involves the cortices wedging into the cancellous bone resulting in elevation of the first ray. Techniques to potentially avoid troughing include avoiding cutting into cancellous bone, using a noncompressing screw, limiting the depth of the distal and proximal cuts, and ensuring the distal cut is as distal as possible because the metaphyseal bone has better support. 10,12
Proximal metatarsal osteotomies
The proximal metatarsal osteotomies are typically reserved for patients with moderate to severe hallux valgus. The most common proximal osteotomies include the proximal chevron, the proximal opening or closing wedge, and the proximal crescentic. A distal soft-tissue procedure such as the modified McBride is generally used as an adjunct to the proximal osteotomies.
Proximal chevron osteotomy
This procedure involves a medial approach to create a v-shaped cut in the proximal metatarsal with lateral rotation of the metatarsal shaft. The proximal chevron is considered more inherently stable and less technically challenging than the other proximal metatarsal osteotomies. 27,79 A Level I study of 75 patients with moderate to severe hallux valgus comparing the proximal opening wedge osteotomy to the proximal chevron osteotomy found no significant differences in radiographic outcomes or operative times. Similar clinical outcomes for pain, satisfaction, and function were also noted for both procedures. The study found that the proximal chevron osteotomy shortened the first metatarsal, whereas the proximal opening wedge osteotomy lengthened the first metatarsal. 32
Proximal opening or closing wedge osteotomy
The proximal opening wedge osteotomy is a powerful technique to reduce the IMA and also increase the length of the first metatarsal. 61 Depending on the size of the wedge, the first metatarsal can be lengthened by 2 to 3 mm. Because of this lengthening, the opening wedge osteotomy may result in tightening of the medial soft tissues and predispose to stiffness. 61,86 Recent attention has shifted to the use of opening wedge plates because of their lower profile. 36,89 The proximal closing base wedge osteotomy has lost popularity as a result of concerns about high recurrence rates, metatarsal shortening, instability of the osteotomy, and dorsal malunion. 81,91
Proximal crescentic osteotomy
This osteotomy involves the creation of a crescentic bone cut 1 cm distal to the first TMT joint using a crescentic saw blade, and the distal fragment is then rotated laterally and secured with screws, Kirschner wires, or dorsal plates. High patient satisfaction and excellent results have been reported with significant improvements of the HVA and IMA in patients with severe hallux valgus. 53,94 Difficulties of this procedure relate to achieving stable fixation of the osteotomy site, as instability may lead to dorsal malunion. A Level I study comparing the proximal crescentic osteotomy to the proximal chevron in moderate to severe hallux valgus found no significant differences in IMA correction or functional outcomes between the 2 techniques. A shorter healing time was noted with the proximal chevron osteotomy. In that study, the proximal crescentic osteotomy led to greater metatarsal shortening and more dorsal malunion. 27
First tarsometatarsal (TMT) arthrodesis (modified Lapidus)
The modified Lapidus procedure has traditionally been used to treat moderate to severe hallux valgus deformity in patients with hypermobility of the first ray, in addition to hallux valgus deformity with concomitant pes planus or first TMT arthritis. This procedure involves fusion of the first TMT joint with angular correction and is normally combined with a distal soft tissue procedure. Patients normally remain nonweightbearing for several weeks to prevent elevation of the first ray and nonunion, which has been regarded as a weakness of the procedure. Recently, a large multicenter study presenting Level III evidence comparing early weightbearing to delayed weightbearing with the modified Lapidus procedure showed no difference in nonunion rates (P = .663). 74 Another Level IV study showed low nonunion rates when meticulous joint preparation and joint compression were achieved using rigid screw fixation. 52
The authors prefer a triplanar TMT arthrodesis (modified Lapidus) with immediate weight-bearing for moderate to severe hallux valgus deformity with hypermobility of the first ray. The triplanar technique utilizes a 90-90 biplanar plating to achieve correction of the deformity at the apex of the deformity or center of rotation of angulation (Figure 6). Correction of the deformity is achieved via derotation of the first metatarsal to achieve neutral frontal plane rotation, while also achieving correction in the transverse and sagittal planes. This construct allows for physiological micromotion to promote healing at the osteotomy site. 71 The triplanar TMT arthrodesis seeks to achieve correction in all 3 planes while minimizing bony resection. Studies to investigate early clinical and radiographic outcomes for patients treated with this technique are currently under way.
Figure 6.

Preoperative and 12-month postoperative radiographs demonstrating the triplanar first tarsometatarsal (TMT) corrective arthrodesis technique with biplanar miniplate construct at 90-degree angles to each other.
First metatarsophalangeal joint arthrodesis
First metatarsophalangeal (MTP) joint fusion is indicated for hallux valgus in patients who have degenerative changes at the first MTP joint, in addition to patients with rheumatoid arthritis as part of a forefoot reconstruction. A first MTP joint fusion is also a powerful corrective option for the elderly patient with hallux valgus or as a salvage procedure for a failed previous hallux valgus surgery. 34 An isolated fusion of the first MTP joint has proven capable to restore a normal IMA and HVA, as a Level IV study found an improvement in the HVA of 33.0 to 10.4 degrees (P < .001) and IMA of 13.1 to 8.6 degrees (P < .001) postoperatively. 75 For the elderly patient, those with prior failed surgical correction, patients with arthrosis of the first MTP joint, and certain rheumatoid patients, a first MTP joint arthrodesis to treat hallux valgus results in excellent outcomes, high satisfaction rates, and low risks of recurrence. 9,18,30
Double osteotomy
The double osteotomy uses both a proximal and distal metatarsal osteotomy to treat moderate to severe hallux valgus deformity with an associated increased DMAA. With this technique, there is a significant risk of shortening the first metatarsal, which may result in transfer metatarsalgia. Avascular necrosis (AVN) of the metatarsal head is also a concern with the double osteotomy. A recent Level III study comparing the double osteotomy to proximal chevron osteotomy in hallux valgus patients with an increased DMAA found no significant difference in AOFAS scores or radiographic measures between groups. The double osteotomy group had greater shortening of the first metatarsal and higher rates of both transfer metatarsalgia and AVN of the metatarsal head. 67,68
Rotational osteotomy
Recent attention has been given to techniques that address the 3-dimensional nature of hallux valgus deformity, particularly frontal plane rotation (pronation/supination). A variety of rotational osteotomies have been described, including rotational scarf, Ludlow, and proximal opening wedge osteotomies. A recent Level V case series described a new rotational osteotomy technique for hallux valgus. 95 The proximal rotational metatarsal osteotomy involves a single oblique osteotomy through the proximal metatarsal. After rotational correction is achieved in the frontal plane, a lag screw and medial locking plate are placed to secure the osteotomy. Early clinical and radiographic results of a series of 6 patients at 7 months after surgery are encouraging, but longer-term and larger studies are needed to validate this technique. 95
Minimally invasive surgery
Percutaneous and minimally invasive surgery (MIS) techniques have emerged over the last decade because of potential advantages of less soft tissue trauma, reduced operative times, and quicker recoveries. Percutaneous techniques are typically used in patients with mild hallux valgus. Several techniques have been described such as the minimally invasive chevron and Akin procedures, arthroscopic techniques, a subcapital osteotomy technique, and the simple, effective, rapid, and inexpensive (SERI) technique. The SERI technique involves fixation of the osteotomy with a Kirschner wire. 6,31,46,50 Although early clinical and radiographic results with MIS are promising, most studies present low levels of evidence, and further long-term comparative studies are needed.
Complications
There are numerous complications associated with hallux valgus surgery. Recurrence is the most common complication, with rates ranging from as low as 8% to as high as 78%. 5,38,43,64,69 The causes are multifactorial, and is associated with skeletal immaturity, increased DMAA, hypermobility, hyperlaxity syndromes, neuromuscular conditions, undercorrection, surgeon technical ability, and noncompliance. 11,16,65,80 Avascular necrosis (AVN) is an uncommon but devastating complication. AVN is associated with distal metatarsal osteotomies that disrupt the blood supply of the metatarsal head. 26,37 It is thought that the chances of AVN can be decreased by avoiding disruption to the lateral vessels through the second lateral incision (used to release the adductor tendon) and instead release the lateral capsule through the joint itself. 41,73
Transfer metatarsalgia, most commonly to the second metatarsal, can be a result of metatarsal shortening or dorsal malunion. Shortening can occur with any type of metatarsal osteotomy; however, the Mitchell osteotomy (double cut through the metatarsal neck) tends to be associated with the greatest amount of shortening, with some studies showing an average shortening of 7 mm. 55 Proximal crescentic osteotomies have traditionally been associated with dorsal malunion, although some studies question this outcome and relate it to surgeon technique, patient compliance, and loss of fixation. 42 Surgeons should also be aware of hallux varus complication. Hallux varus is relatively rare. It is associated with technical errors including over-resection of the medial aspect of the metatarsal head, overtightening of the medial capsule, excessive lateral capsule release, overcorrection of the first IMA, and excision of the lateral sesamoid. 24,57
Conclusions
There is considerable variability in surgical treatment to correct hallux valgus, with numerous procedures described. Soft tissue balancing procedures and distal metatarsal osteotomies have traditionally been used to treat mild hallux valgus deformity. For moderate deformity, more proximal metatarsal osteotomies are typically employed. Proximal osteotomies or a first TMT arthrodesis are used for severe hallux valgus deformity. In the presence of first MTP arthritis or inadequate soft tissues, a fusion of the first MTP joint may be performed. Newer techniques such as the triplanar TMT corrective arthrodesis are emerging and hold promise, but long-term follow-up studies are needed to compare them to traditional corrective procedures.
Supplemental Material
Supplemental Material, FAO838500-ICMJE for Hallux Valgus by Justin J. Ray, Andrew J. Friedmann, Andrew E. Hanselman, Justin Vaida, Paul D. Dayton, Daniel J. Hatch, Bret Smith and Robert D. Santrock in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Paul D. Dayton, DPM, MS, Daniel J. Hatch, DPM, Bret Smith, DO, MS, and Robert D. Santrock, MD, are paid consults for Treace Medical Concepts, Inc. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Adam SP, Choung SC, Gu Y, O’Malley MJ. Outcomes after scarf osteotomy for treatment of adult hallux valgus deformity. Clin Orthop Relat Res. 2011;469:854–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aiyer A, Shub J, Shariff R, Ying L, Myerson M. Radiographic recurrence of deformity after hallux valgus surgery in patients with metatarsus adductus. Foot Ankle Int. 2016;37(2):165–171. [DOI] [PubMed] [Google Scholar]
- 3. Aiyer AA, Shariff R, Ying L, Shub J, Myerson MS. Prevalence of metatarsus adductus in patients undergoing hallux valgus surgery. Foot Ankle Int. 2014;35(12):1292–1297. [DOI] [PubMed] [Google Scholar]
- 4. Bierman RA, Christensen JC, Johnson CH. Biomechanics of the first ray. Part III. Consequences of Lapidus arthrodesis on peroneus longus function: a three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2001;40:125–131. [DOI] [PubMed] [Google Scholar]
- 5. Bock P, Kluger R, Kristen KH, Mittlbock M, Schuh R, Trnka HJ. The scarf osteotomy with minimally invasive lateral release for treatment of hallux valgus deformity: intermediate and long-term results. J Bone Joint Surg Am. 2015;97:1238–1245. [DOI] [PubMed] [Google Scholar]
- 6. Bosch P, Wanke S, Legenstein R. Hallux valgus correction by the method of Bosch: a new technique with a seven-to-ten-year follow-up. Foot Ankle Clin. 2000;5:485–498, v–vi. [PubMed] [Google Scholar]
- 7. Choi GW, Kim HJ, Kim TS, et al. Comparison of the modified McBride procedure and the distal chevron osteotomy for mild to moderate hallux valgus. J Foot Ankle Surg. 2016;55:808–811. [DOI] [PubMed] [Google Scholar]
- 8. Chou LB, Mann RA, Casillas MM. Biplanar chevron osteotomy. Foot Ankle Int. 1998;19(9):579–584. [DOI] [PubMed] [Google Scholar]
- 9. Chraim M, Bock P, Alrabai HM, Trnka HJ. Long-term outcome of first metatarsophalangeal joint fusion in the treatment of severe hallux rigidus. Int Orthop. 2016;40:2401–2408. [DOI] [PubMed] [Google Scholar]
- 10. Coetzee JC. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int. 2003;24(1):29–33. [DOI] [PubMed] [Google Scholar]
- 11. Coetzee JC, Resig SG, Kuskowski M, Saleh KJ. The Lapidus procedure as salvage after failed surgical treatment of hallux valgus: a prospective cohort study. J Bone Joint Surg Am. 2003;85:60–65. [DOI] [PubMed] [Google Scholar]
- 12. Coetzee JC, Rippstein P. Surgical strategies: scarf osteotomy for hallux valgus. Foot Ankle Int. 2007;28(4):529–535. [DOI] [PubMed] [Google Scholar]
- 13. Condon F, Kaliszer M, Conhyea D, O’Donnell T, Shaju A, Masterson E. The first intermetatarsal angle in hallux valgus: an analysis of measurement reliability and the error involved. Foot Ankle Int. 2002;23(8):717–721. [DOI] [PubMed] [Google Scholar]
- 14. Corrigan JP, Moore DP, Stephens MM. Effect of heel height on forefoot loading. Foot Ankle. 1993;14:148–152. [DOI] [PubMed] [Google Scholar]
- 15. Coughlin MJ. Hallux valgus. Instr Course Lect. 1997;46:357–391. [PubMed] [Google Scholar]
- 16. Coughlin MJ. Roger A. Mann Award. Juvenile hallux valgus: etiology and treatment. Foot Ankle Int. 1995;16(11):682–697. [DOI] [PubMed] [Google Scholar]
- 17. Coughlin MJ, Freund E. Roger A. Mann Award. The reliability of angular measurements in hallux valgus deformities. Foot Ankle Int. 2001;22(5):369–379. [DOI] [PubMed] [Google Scholar]
- 18. Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: intermediate results. Foot Ankle Int. 2005;26(10):783–792. [DOI] [PubMed] [Google Scholar]
- 19. Coughlin MJ, Jones CP. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007;28(7):759–777. [DOI] [PubMed] [Google Scholar]
- 20. Coughlin MJ, Mann RA, Saltzman CL. Hallux Valgus. Surgery of the Foot and Ankle. 8th ed. Philadelphia, PA: Mosby Elsevier;2007:265–267. [Google Scholar]
- 21. Dayton P, Feilmeier M, Kauwe M, Holmes C, McArdle A, Coleman N. Observed changes in radiographic measurements of the first ray after frontal and transverse plane rotation of the hallux: does the hallux drive the metatarsal in a bunion deformity? J Foot Ankle Surg. 2014;53:584–587. [DOI] [PubMed] [Google Scholar]
- 22. Dayton P, Kauwe M, Feilmeier M. Is our current paradigm for evaluation and management of the bunion deformity flawed? A discussion of procedure philosophy relative to anatomy. J Foot Ankle Surg. 2015;54:102–111. [DOI] [PubMed] [Google Scholar]
- 23. DiGiovanni CW, Kuo R, Tejwani N, et al. Isolated gastrocnemius tightness. J Bone Joint Surg Am. 2002;84:962–970. [DOI] [PubMed] [Google Scholar]
- 24. Donley BG. Acquired hallux varus. Foot Ankle Int. 1997;18(9):586–592. [DOI] [PubMed] [Google Scholar]
- 25. Douthett SM, Plaskey NK, Fallat LM, Kish J. Retrospective analysis of the akin osteotomy. J Foot Ankle Surg. 2018;57:38–43. [DOI] [PubMed] [Google Scholar]
- 26. Easley ME, Kelly IP. Avascular necrosis of the hallux metatarsal head. Foot Ankle Clin. 2000;5:591–608. [PubMed] [Google Scholar]
- 27. Easley ME, Kiebzak GM, Davis WH, Anderson RB. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Foot Ankle Int. 1996;17(6):307–316. [DOI] [PubMed] [Google Scholar]
- 28. Easley ME, Trnka HJ. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int. 2007;28(5):654–659. [DOI] [PubMed] [Google Scholar]
- 29. Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007;28(6):748–758. [DOI] [PubMed] [Google Scholar]
- 30. Feilmeier M, Dayton P, Wienke JC, Jr. Reduction of intermetatarsal angle after first metatarsophalangeal joint arthrodesis in patients with hallux valgus. J Foot Ankle Surg. 2014;53:29–31. [DOI] [PubMed] [Google Scholar]
- 31. Giannini S, Faldini C, Nanni M, Di Martino A, Luciani D, Vannini F. A minimally invasive technique for surgical treatment of hallux valgus: simple, effective, rapid, inexpensive (SERI). Int Orthop. 2013;37:1805–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Glazebrook M, Copithorne P, Boyd G, et al. Proximal opening wedge osteotomy with wedge-plate fixation compared with proximal chevron osteotomy for the treatment of hallux valgus: a prospective, randomized study. J Bone Joint Surg Am. 2014;96:1585–1592. [DOI] [PubMed] [Google Scholar]
- 33. Gribbin CK, Ellis SJ, Nguyen J, Williamson E, Cody EA. Relationship of radiographic and clinical parameters with hallux valgus and second ray pathology. Foot Ankle Int. 2017;38(1):14–19. [DOI] [PubMed] [Google Scholar]
- 34. Grimes JS, Coughlin MJ. First metatarsophalangeal joint arthrodesis as a treatment for failed hallux valgus surgery. Foot Ankle Int. 2006;27(11):887–893. [DOI] [PubMed] [Google Scholar]
- 35. Hatch DJ. Radiographic assessment. In: Dayton PD, ed. Evidence-Based Bunion Surgery: A Critical Examination of Current and Emerging Concepts and Techniques. Cham, Switzerland: Springer International Publishing; 2017:61–72. [Google Scholar]
- 36. Iyer S, Demetracopoulos CA, Sofka CM, Ellis SJ. High rate of recurrence following proximal medial opening wedge osteotomy for correction of moderate hallux valgus. Foot Ankle Int. 2015;36(7):756–763. [DOI] [PubMed] [Google Scholar]
- 37. Jahss MH. Hallux valgus: further considerations—the first metatarsal head. Foot Ankle. 1981;2:1–4. [DOI] [PubMed] [Google Scholar]
- 38. Jeuken RM, Schotanus MG, Kort NP, Deenik A, Jong B, Hendrickx RP. Long-term follow-up of a randomized controlled trial comparing scarf to chevron osteotomy in hallux valgus correction. Foot Ankle Int. 2016;37(7):687–695. [DOI] [PubMed] [Google Scholar]
- 39. Johnson CH, Christensen JC. Biomechanics of the first ray, part V: the effect of equinus deformity. A 3-dimensional kinematic study on a cadaver model. J Foot Ankle Surg. 2005;44:114–120. [DOI] [PubMed] [Google Scholar]
- 40. Johnson CH, Christensen JC. Biomechanics of the first ray. Part I. The effects of peroneus longus function: a three-dimensional kinematic study on a cadaver model. J Foot Ankle Surg. 1999;38:313–321. [DOI] [PubMed] [Google Scholar]
- 41. Johnson JE, Clanton TO, Baxter DE, Gottlieb MS. Comparison of Chevron osteotomy and modified McBride bunionectomy for correction of mild to moderate hallux valgus deformity. Foot Ankle. 1991;12:61–68. [DOI] [PubMed] [Google Scholar]
- 42. Jones C, Coughlin M, Villadot R, Golano P. Proximal crescentic metatarsal osteotomy: the effect of saw blade orientation on first ray elevation. Foot Ankle Int. 2005;26(2):152–157. [DOI] [PubMed] [Google Scholar]
- 43. Kilmartin TE, O’Kane C. Combined rotation scarf and Akin osteotomies for hallux valgus: a patient focussed 9 year follow up of 50 patients. J Foot Ankle Res. 2010;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kim Y, Kim JS, Young KW, Naraghi R, Cho HK, Lee SY. A new measure of tibial sesamoid position in hallux valgus in relation to the coronal rotation of the first metatarsal in CT scans. Foot Ankle Int. 2015;36(8):944–952. [DOI] [PubMed] [Google Scholar]
- 45. Kimura T, Kubota M, Taguchi T, Suzuki N, Hattori A, Marumo K. Evaluation of first-ray mobility in patients with hallux valgus using weight-bearing CT and a 3-D analysis system: a comparison with normal feet. J Bone Joint Surg Am. 2017;99:247–255. [DOI] [PubMed] [Google Scholar]
- 46. Lai MC, Rikhraj IS, Woo YL, Yeo W, Ng YCS, Koo K. Clinical and radiological outcomes comparing percutaneous chevron-akin osteotomies vs open scarf-akin osteotomies for hallux valgus. Foot Ankle Int. 2018;39(3):311–317. [DOI] [PubMed] [Google Scholar]
- 47. LaPorta GA, Nasser EM, Mulhern JL, Malay DS. The mechanical axis of the first ray: a radiographic assessment in hallux abducto valgus evaluation. J Foot Ankle Surg. 2016;55:28–34. [DOI] [PubMed] [Google Scholar]
- 48. Lee HJ, Chung JW, Chu IT, Kim YC. Comparison of distal chevron osteotomy with and without lateral soft tissue release for the treatment of hallux valgus. Foot Ankle Int. 2010;31(4):291–295. [DOI] [PubMed] [Google Scholar]
- 49. Lee KM, Ahn S, Chung CY, Sung KH, Park MS. Reliability and relationship of radiographic measurements in hallux valgus. Clin Orthop Relat Res. 2012;470(9):2613–2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Magnan B, Bortolazzi R, Samaila E, Pezze L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. Surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1, pt 1):135–148. [DOI] [PubMed] [Google Scholar]
- 51. Mahadevan D, Lines S, Hepple S, Winson I, Harries W. Extended plantar limb (modified) chevron osteotomy versus scarf osteotomy for hallux valgus correction: a randomised controlled trial. Foot Ankle Surg. 2016;22:109–113. [DOI] [PubMed] [Google Scholar]
- 52. Mani SB, Lloyd EW, MacMahon A, Roberts MM, Levine DS, Ellis SJ. Modified Lapidus procedure with joint compression, meticulous surface preparation, and shear-strain-relieved bone graft yields low nonunion rate. HSS J. 2015;11:243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mann RA, Rudicel S, Graves SC. Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy. A long-term follow-up. J Bone Joint Surg Am. 1992;74:124–129. [PubMed] [Google Scholar]
- 54. Menz HB, Roddy E, Marshall M, et al. Epidemiology of shoe wearing patterns over time in older women: associations with foot pain and hallux valgus. J Gerontol A Biol Sci Med Sci. 2016;71:1682–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Merkel KD, Katoh Y, Johnson EW, Jr, Chao EY. Mitchell osteotomy for hallux valgus: long-term follow-up and gait analysis. Foot Ankle. 1983;3:189–196. [DOI] [PubMed] [Google Scholar]
- 56. Meyr AJ. The etiology of hallux abductovalgus described in six pieces. In: Dayton PD, ed. Evidence-Based Bunion Surgery: A Critical Examination of Current and Emerging Concepts and Techniques. Cham, Switzerland: Springer International Publishing; 2017:23–41. [Google Scholar]
- 57. Miller JW. Acquired hallux varus: a preventable and correctable disorder. J Bone Joint Surg Am. 1975;57:183–188. [PubMed] [Google Scholar]
- 58. Munteanu SE, Menz HB, Wark JD, et al. Hallux valgus, by nature or nurture? A twin study. Arthritis Care Res (Hoboken). 2017;69:1421–1428. [DOI] [PubMed] [Google Scholar]
- 59. Nery C, Barroco R, Ressio C. Biplanar chevron osteotomy. Foot Ankle Int. 2002;23(9):792–798. [DOI] [PubMed] [Google Scholar]
- 60. Nery C, Coughlin MJ, Baumfeld D, Ballerini FJ, Kobata S. Hallux valgus in males—part 1: demographics, etiology, and comparative radiology. Foot Ankle Int. 2013;34(5):629–635. [DOI] [PubMed] [Google Scholar]
- 61. Nery C, Ressio C, de Azevedo Santa Cruz G, de Oliveira RS, Chertman C. Proximal opening-wedge osteotomy of the first metatarsal for moderate and severe hallux valgus using low profile plates. Foot Ankle Surg. 2013;19:276–282. [DOI] [PubMed] [Google Scholar]
- 62. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2007;89:2163–2172. [DOI] [PubMed] [Google Scholar]
- 64. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Shima H, Takamura M. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J Orthop Sci. 2011;16:760–764. [DOI] [PubMed] [Google Scholar]
- 65. Osterhoff G, Boni T, Berli M. Recurrence of acute Charcot neuropathic osteoarthropathy after conservative treatment. Foot Ankle Int. 2013;34:359–64. [DOI] [PubMed] [Google Scholar]
- 66. Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 67. Park CH, Cho JH, Moon JJ, Lee WC. Can double osteotomy be a solution for adult hallux valgus deformity with an increased distal metatarsal articular angle? J Foot Ankle Surg. 2016;55:188–192. [DOI] [PubMed] [Google Scholar]
- 68. Park CH, Lee WC. Is double metatarsal osteotomy superior to proximal chevron osteotomy in treatment of hallux valgus with increased distal metatarsal articular angle? J Foot Ankle Surg. 2018;57:241–246. [DOI] [PubMed] [Google Scholar]
- 69. Pentikainen I, Ojala R, Ohtonen P, Piippo J, Leppilahti J. Preoperative radiological factors correlated to long-term recurrence of hallux valgus following distal chevron osteotomy. Foot Ankle Int. 2014;35(12):1262–1267. [DOI] [PubMed] [Google Scholar]
- 70. Perera AM, Mason L, Stephens MM. The pathogenesis of hallux valgus. J Bone Joint Surg Am. 2011;93:1650–1661. [DOI] [PubMed] [Google Scholar]
- 71. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093–1110. [DOI] [PubMed] [Google Scholar]
- 72. Pique-Vidal C, Sole MT, Antich J. Hallux valgus inheritance: pedigree research in 350 patients with bunion deformity. J Foot Ankle Surg. 2007;46:149–154. [DOI] [PubMed] [Google Scholar]
- 73. Pochatko DJ, Schlehr FJ, Murphey MD, Hamilton JJ. Distal chevron osteotomy with lateral release for treatment of hallux valgus deformity. Foot Ankle Int. 1994;15(9):457–461. [DOI] [PubMed] [Google Scholar]
- 74. Prissel MA, Hyer CF, Grambart ST, et al. A multicenter, retrospective study of early weightbearing for modified Lapidus arthrodesis. J Foot Ankle Surg. 2016;55:226–229. [DOI] [PubMed] [Google Scholar]
- 75. Pydah SK, Toh EM, Sirikonda SP, Walker CR. Intermetatarsal angular change following fusion of the first metatarsophalangeal joint. Foot Ankle Int. 2009;30(5):415–418. [DOI] [PubMed] [Google Scholar]
- 76. Robinson AH, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br. 2005;87:1038–1045. [DOI] [PubMed] [Google Scholar]
- 77. Roling BA, Christensen JC, Johnson CH. Biomechanics of the first ray. Part IV: the effect of selected medial column arthrodeses. A three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2002;41:278–285. [DOI] [PubMed] [Google Scholar]
- 78. Rush SM, Christensen JC, Johnson CH. Biomechanics of the first ray. Part II: Metatarsus primus varus as a cause of hypermobility. A three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2000;39:68–77. [DOI] [PubMed] [Google Scholar]
- 79. Sammarco GJ, Brainard BJ, Sammarco VJ. Bunion correction using proximal chevron osteotomy. Foot Ankle. 1993;14:8–14. [DOI] [PubMed] [Google Scholar]
- 80. Sammarco VJ. Management of soft tissue deficiency of the hallux: salvage in trauma, diabetes, and following surgical complications. Foot Ankle Clin. 2005;10:55–74. [DOI] [PubMed] [Google Scholar]
- 81. Sammarco VJ, Acevedo J. Stability and fixation techniques in first metatarsal osteotomies. Foot Ankle Clin. 2001;6:409–432, v–vi. [DOI] [PubMed] [Google Scholar]
- 82. Santrock RD, Smith B, Hatch DJ, Dayton PD. Anatomic triplane hallux abducto valgus classification: PVB Working Group Recommendations. 2017. [DOI] [PubMed]
- 83. Scott G, Menz HB, Newcombe L. Age-related differences in foot structure and function. Gait Posture. 2007;26:68–75. [DOI] [PubMed] [Google Scholar]
- 84. Sharma J, Aydogan U. Algorithm for severe hallux valgus associated with metatarsus adductus. Foot Ankle Int. 2015;36(12):1499–503. [DOI] [PubMed] [Google Scholar]
- 85. Shibuya N, Kitterman RT, LaFontaine J, Jupiter DC. Demographic, physical, and radiographic factors associated with functional flatfoot deformity. J Foot Ankle Surg. 2014;53:168–172. [DOI] [PubMed] [Google Scholar]
- 86. Shurnas PS, Watson TS, Crislip TW. Proximal first metatarsal opening wedge osteotomy with a low profile plate. Foot Ankle Int. 2009;30(9):865–872. [DOI] [PubMed] [Google Scholar]
- 87. Smith AM, Alwan T, Davies MS. Perioperative complications of the Scarf osteotomy. Foot Ankle Int. 2003;24(3):222–227. [DOI] [PubMed] [Google Scholar]
- 88. Smith JT, Bluman EM. Hallux valgus and hallux varus. In: Orthopaedic Knowledge Update: Foot and Ankle. 5th ed. Rosemont: American Academy of Orthopaedic Surgeons; 2014:183–191. [Google Scholar]
- 89. Smith WB, Hyer CF, DeCarbo WT, Berlet GC, Lee TH. Opening wedge osteotomies for correction of hallux valgus: a review of wedge plate fixation. Foot Ankle Spec. 2009;2:277–282. [DOI] [PubMed] [Google Scholar]
- 90. Tanaka Y, Takakura Y, Kumai T, Samoto N, Tamai S. Radiographic analysis of hallux valgus. A two-dimensional coordinate system. J Bone Joint Surg Am. 1995;77:205–213. [DOI] [PubMed] [Google Scholar]
- 91. Trnka HJ, Muhlbauer M, Zembsch A, Hungerford M, Ritschl P, Salzer M. Basal closing wedge osteotomy for correction of hallux valgus and metatarsus primus varus: 10- to 22-year follow-up. Foot Ankle Int. 1999;20(3):171–177. [DOI] [PubMed] [Google Scholar]
- 92. Trnka HJ, Zembsch A, Wiesauer H, Hungerford M, Salzer M, Ritschl P. Modified Austin procedure for correction of hallux valgus. Foot Ankle Int. 1997;18(3):119–127. [DOI] [PubMed] [Google Scholar]
- 93. van Groningen B, van der Steen MC, Reijman M, Bos J, Hendriks JG. Outcomes in chevron osteotomy for hallux valgus in a large cohort. Foot (Edinb). 2016;29:18–24. [DOI] [PubMed] [Google Scholar]
- 94. Veri JP, Pirani SP, Claridge R. Crescentic proximal metatarsal osteotomy for moderate to severe hallux valgus: a mean 12.2 year follow-up study. Foot Ankle Int. 2001;22(10):817–822. [DOI] [PubMed] [Google Scholar]
- 95. Wagner P, Ortiz C, Wagner E. Rotational osteotomy for hallux valgus: a new technique for primary and revision cases. Tech Foot Ankle Surg. 2017;16:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Wulker N, Mittag F. The treatment of hallux valgus. Dtsch Arztebl Int. 2012;109:857–867; quiz 868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Yu GV, Johng B, Freireich R. Surgical management of metatarsus adductus deformity. Clin Podiatr Med Surg. 1987;4:207–232. [PubMed] [Google Scholar]
- 98. Yucel I, Tenekecioglu Y, Ogut T, Kesmezacar H. Treatment of hallux valgus by modified McBride procedure: a 6-year follow-up. J Orthop Traumatol. 2010;11:89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO838500-ICMJE for Hallux Valgus by Justin J. Ray, Andrew J. Friedmann, Andrew E. Hanselman, Justin Vaida, Paul D. Dayton, Daniel J. Hatch, Bret Smith and Robert D. Santrock in Foot & Ankle Orthopaedics