Abstract
Background:
Measuring ankle range of motion (ROM) following injury or intervention is necessary for monitoring recovery as well as for calculating permanent impairment ratings in workers’ compensation cases. In recent years, smartphone application developers have created applications (apps) that emulate ROM measurement tools like the universal goniometer. This study assessed the correlation between smartphone ROM measurements and universal goniometer measurements, as well as the reliability and usability of these apps in clinical practice.
Methods:
Three raters used the Goniometer app (Gonio), Clinometer app (Clino), DrGoniometer app (DrG), and a universal goniometer (UG) to assess the ankle ROM in plantarflexion and dorsiflexion of 24 patients with ankle pathology. Each patient completed a survey on the usability of the apps.
Results:
Lin’s concordance correlation coefficient test showed moderate correlation between the smartphone and UG measurements (Lin‘s correlation coefficient [rLC] = 0.931, 95% confidence interval [CI] = 0.911-0.946 for UG-Gonio; rLC = 0.908, 95% CI = 0.881-0.929 for UG-Clino; rLC = 0.935, 95% CI = 0.915-0.950 for UG-DrG). A 2-way mixed model showed good to excellent interrater reliability for each app for plantarflexion and dorsiflexion (ICCp = 0.836, ICCd = 0.912, P < .001 for Gonio; ICCp = 0.788, ICCd = 0.893, P < .001 for Clino; ICCp = 0.777, ICCd = 0.897, P < .001 for DrG). Most participants surveyed were very comfortable with having their ankle ROM measured by a smartphone.
Conclusion:
Smartphone apps may be a more convenient way to measure ankle ROM than UG. Physicians can use these apps to measure a patient’s ROM in clinic, a patient could send a picture of his or her dorsiflexed or plantarflexed ankle to the physician to remotely track ROM, or a patient could measure his or her own ROM at home using a personal smartphone.
Level of Evidence:
Level IV, case series.
Keywords: ankle joint, range of motion, ROM, smartphone, smartphone applications, workers’ compensation, ankle rehabilitation
The ankle joint is one of the most commonly injured joints, and ankle range of motion (ROM) is an important criterion for postinjury assessment in the general population as well as in special groups like the elderly or athletes undergoing physical therapy. 20 In the lateral ankle sprain, an ankle joint dysfunction that makes up 80% of all ankle injuries, limitation of ROM dorsiflexion has been shown to be a key parameter used for evaluation. 13 In addition, ankle ROM measurements are needed to calculate permanent impairment ratings in workers’ compensation cases, making ROM financially important for many patients. In many states, ankle ROM is the primary factor used to determine a patient’s permanent impairment rating following a work-related injury. 3
Many methods of measuring ROM—from simple visual estimation to high-speed cinematography, to the more widely used universal goniometer—have been used and evaluated over the past 60 years to increase measurement accuracy and reduce potential sources of error. 19 The universal goniometer (UG) has become the clinical standard for measuring joint ROM, particularly for measuring ankle plantarflexion and dorsiflexion. 20 The UG is the single most commonly used device to measure ROM in clinical practice and works by aligning the arms of the device with reference points on the patient’s joint. While this type of goniometry is easy to use and low cost, studies have shown a lack of reproducibility with goniometric measurements by different examiners. 17 Despite this drawback, the UG remains the clinical standard for measuring ROM. 6
With the growth of smartphone applications (apps) built to transform smartphones into medical devices, many smartphone app developers have created apps to measure ROM across various joints. As a result, it has become increasingly important to identify and reduce sources of measurement error that stem from the specific measurement device used to calculate ROM. 17 In 2015, 1 study reported that searching both Apple and Samsung smartphone app stores for “Gonio” and “ROM” yielded 16 unique apps for measuring joint ROM. 12 That number has likely increased substantially in the past 4 years since the study was published. It is necessary to consider the usability of smartphone apps in clinical practice, as there is often both patient and physician opposition to unproven technologies introduced into the health care space. 7 It is thus important to gauge both patient and physician sentiments regarding using smartphone apps in clinic.
Previous studies have reported the accuracy, validity, and reliability of various smartphone apps that measure joint ROM, particularly in the knee, shoulder, and wrist. 5,9,15,16 These studies have assessed individual apps, but to the authors’ knowledge, no study has categorically compared the ability of apps that use fundamentally different methods to measure ankle ROM. Moreover, no previous study has surveyed patient sentiments about having their ankle ROM measured using smartphone apps in clinic. The main purpose of this study was to determine if the Goniometer Pro (Gonio), Dr. Goniometer (DrG), and Clinometer (Clino) iPhone apps measure ankle ROM as accurately as the clinical standard UG, by determining the correlations between UG measurements and measurements from the 3 smartphone apps. In addition, this study assessed the interrater reliability of the smartphone apps and surveyed the patients’ comfortability with having their ankle ROM measured by an iPhone app. We hypothesized that there would be a strong correlation between ankle ROM measurements of all 3 apps and the UG measurements and that all 3 apps would have excellent interrater reliability. We also hypothesized that the participants surveyed would be comfortable with having their ankle ROM measured in clinic using iPhone apps.
Methods
Participants
The pathologic ankles of 24 patients who presented to the senior authors’ foot and ankle clinics were measured. The study included all patients 18 years old or older and excluded patients who underwent an ankle arthrodesis, had an acute fracture, or otherwise exhibited severely limited ROM. Human subjects approval was granted, and a written informed consent was obtained from all participants before any measurements were taken. The participants had an average age of 52 years. Twenty-one of the 24 patients had prior ankle surgery. The average time elapsed between a participant’s surgery and our measurements in clinic was 146 (range, 20-624) days.
Examiners
All goniometric measurements were performed by 3 independent examiners—an attending orthopaedic surgeon (A.T.S.), an orthopaedic surgery resident physician (S.H.H.), and a medical student (K.Y.W.). Although the examiners have varying degrees of experience with goniometry, all examiners were trained in measurement and interpretation of the UG and all 3 apps prior to collecting data. To effectively blind the measurements, while 1 examiner was doing a measurement, a separate examiner recorded the values of the measurement.
Instrumentation
A plastic BLUEJAY (Los Angeles, CA) universal goniometer with a 360-degree face and 8-inch movable arms was used for all UG measurements. To prevent the examiner from being biased by seeing the measurement figures on the UG, examiner blinding was accomplished by covering 1 surface of the UG face by a cutout piece of paper during measurements. All 3 apps were downloaded onto a single iPhone SE unit (Apple, Cupertino, CA), which was used for measurements by all examiners. Prior to the measurements, all cases and covers were removed from the iPhone SE unit. Examiners taking measurements with the iPhone were blinded using a cutout piece of paper that covered the face of the device. A separate examiner removed the blinding paper to document the measurements after each measurement was completed.
The goal of investigating different types of apps was to determine if the method by which an app took measurements would significantly influence the correlation between app measurements and UG measurements. Existing apps that measure ROM could be broadly categorized by 2 features. The first feature was how the app was designed to measure angles: there were (1) picture-based apps (ie, DrG), which used a smartphone’s built-in camera to capture a picture of the joint and subsequently calculate the angle from the picture, and (2) accelerometer-based apps (ie, Gonio), which used the smartphone’s internal accelerometer to sense a smartphone’s spatial position and measure angles. A 2015 study that assessed goniometer apps in hand surgery termed this stratification a “functional” categorization of goniometric apps. 12 The second feature that could be used to categorize apps that measure angles was whether these apps were designed to either (1) be used specifically in a medical context (ie, Gonio, DrG) or (2) be used as a general-level app to assess angles for various purposes, like making sure a picture frame was level (ie, Clino). Cross-classification by these 2 features created 4 categories of apps: picture-based medical apps, accelerometer-based medical apps, picture-based nonmedical apps, and accelerometer-based nonmedical apps. There were no apps in the Apple App Store as of 2018 that fall into the category of picture-based nonmedical apps, so this study used the highest-rated app in each of the 3 other categories as representative of that category of app. Thus, the 3 apps investigated were the highest-rated app in each of the following categories: (1) picture-based medical apps (DrG), (2) accelerometer-based medical apps (Gonio), and (3) accelerometer-based nonmedical apps (Clino).
Procedure
All participants were patients presenting to the senior authors’ foot and ankle clinics. Patients who met the study’s inclusion and exclusion criteria were introduced to the study after their clinic appointments. If they provided written informed consent, then ROM measurements were completed in a separate examination room during their office visit.
For each specific measurement protocol detailed below, the participant’s pant leg on the side of the pathologic ankle was rolled up to expose the participant’s leg and foot. Knee position was standardized such that each participant’s knee joint was flexed at a 90-degree angle during the measurement process. To eliminate bias due to patient fatigue, the order in which measurements were taken using the 3 apps was randomized for each patient. After all measurements were completed for a participant, the participant was asked to complete the survey.
Universal Goniometer Protocol
Examiners positioned themselves lateral to the pathologic ankle of each participant. The UG was positioned such that the goniometer axis was lateral to the participant’s lateral malleolus, with the stationary arm extending toward the fibular head and the mobile arm parallel to the longitudinal axis of the fifth metatarsal (Figure 1). After the examiner adjusted the mobile arm and was satisfied with the measurement, the recorder documented the measured angle in the neutral position and in the plantarflexed or dorsiflexed position in whole degrees from the nonblinded side of the UG.
Figure 1.
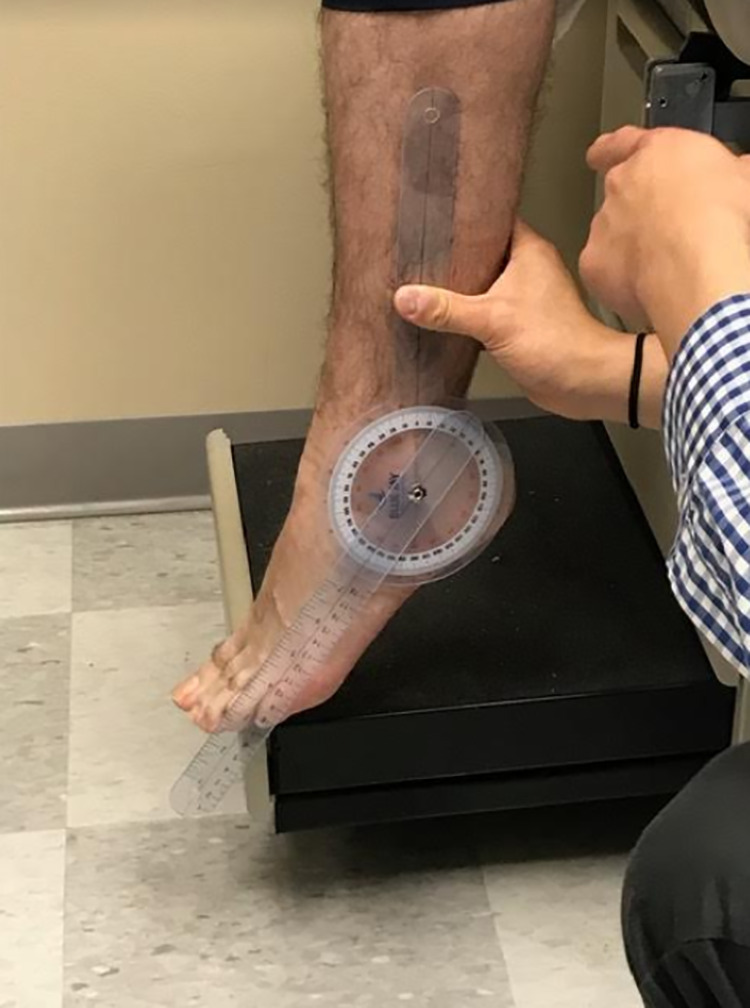
The universal goniometer was positioned such that the goniometer axis was lateral to the participant’s lateral malleolus, with the stationary arm extending toward the fibular head and the mobile arm parallel to the longitudinal axis of the fifth metatarsal.
Gonio Protocol
The examiner was positioned lateral to the participant’s pathologic ankle. The phone was positioned such that the bottom corner (toward the home button) of the phone was centered on the participant’s lateral malleolus with the side edge of the phone parallel to the longitudinal axis of the participant’s fifth metatarsal (Figure 2). Once neutral position was attained, the examiner selected the “Start” button on the app, which recorded the angle of this neutral position. Then, as the participant plantarflexed or dorsiflexed, the examiner rotated the phone’s position such that the side edge of the phone was repositioned to be parallel to the longitudinal axis of the participant’s fifth metatarsal, with the bottom corner of the phone still centered on the participant’s lateral malleolus. At this point, the examiner selected the “End” button, and the recorder documented the measured angle of plantarflexion and dorsiflexion displayed on the screen (Figure 3).
Figure 2.
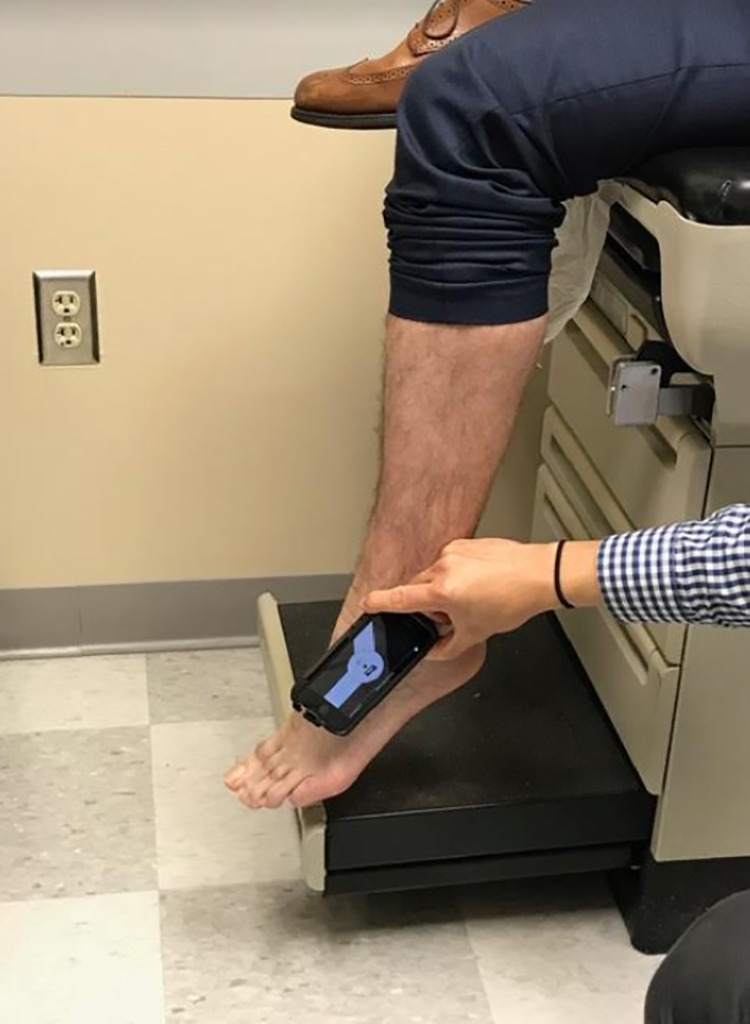
For the Gonio and Clino measurements, the phone was positioned such that the bottom corner (toward the home button) of the phone was centered on the participant’s lateral malleolus with the side edge of the phone parallel to the longitudinal axis of the participant’s fifth metatarsal.
Figure 3.
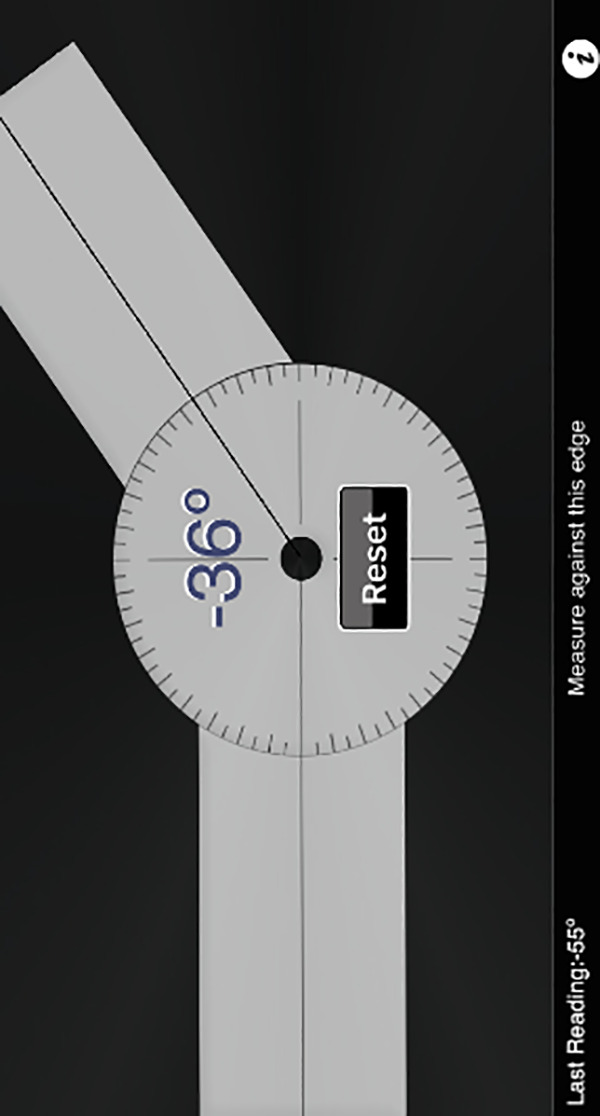
For the Gonio measurements, measured angles were documented by the recorder as displayed on the screen.
Clino Protocol
Both the examiner and participant were positioned in the same way as for the Gonio protocol, and measurements were taken in the same fashion (Figure 2). After the examiner completed the measurement, the recorder documented the measured angle after plantarflexion and dorsiflexion as displayed on the screen (Figure 4).
Figure 4.

For the Clino measurements, measured angles were documented by the recorder as displayed on the screen.
DrG Protocol
The examiner was positioned lateral to the participant’s pathologic ankle, 3 feet from the participant’s ankle. The examiner held the phone vertically at the level of the participant’s ankle and used the app to take a picture, with the participant’s foot, ankle, and leg in the frame (Figure 5). Once this picture was saved, the examiner placed the 3 movable markers on the participant’s fibular head, lateral malleolus, and just above the fifth toe such that the line between the markers of the lateral malleolus and fifth toe was parallel to the longitudinal axis of the fifth metatarsal (Figure 6). The recorder documented the angle displayed on the screen.
Figure 5.

For the DrG measurements, the examiner held the phone in a vertical position at the same level as the participant’s ankle, using the app’s intrinsic tilt feature to ensure that the phone was level with the participant’s ankle before taking a picture of the participant’s leg.
Figure 6.

For the DrG measurements, after a picture was taken with the participant’s leg, foot, and ankle in the frame, the examiner placed the 3 movable red markers on the participant’s fibular head, lateral malleolus, and just above the fifth toe such that the line between the markers of the lateral malleolus and fifth toe was parallel to the longitudinal axis of the participant’s fifth metatarsal. The angle of plantarflexion or dorsiflexion was documented as displayed on the bottom of the screen after marker placement.
Survey
After all measurements were completed, each participant was given a survey with 5 questions:
How comfortable are you having your ankle range of motion measured with a smartphone? (Choices: very comfortable, comfortable, neither comfortable nor uncomfortable, uncomfortable, very uncomfortable)
Would you be willing to send photos of your ankle to your surgeon to monitor your ankle recovery? (Choices: yes, no)
If recommended by your surgeon or physical therapist, would you use your smartphone to measure your ankle range of motion at home to track your progress? (Choices: yes, sometimes, no)
Would seeing consistent improvement in your ankle range of motion motivate you to do more simple ankle exercises at home? (Choices: yes, possibly, no)
Would you measure your ankle range of motion more of less frequently at home if you could easily do it yourself? (Choices: more frequently, same amount, less frequently)
While participants completed the survey, all examiners were outside of the exam room. All 24 participants completed each question of the survey.
Statistical Analysis
All measurements were tabulated and recorded in an Excel document spreadsheet. Lin’s concordance analysis was conducted to assess reliability of Gonio, Clino, and DrG measurements relative to the UG. Lin’s concordance analysis was deliberately chosen for this study instead of the more commonly used Pearson’s correlation analysis. The Pearson’s correlation coefficient is a measure of linear covariation between 2 sets of values, without specifying any degree of correspondence between the 2 sets of values. On the other hand, Lin’s concordance analysis provides a measure of reliability based on both covariation and correspondence, making it a more appropriate analysis for comparing a set of experimental values to a set of standard values. 11 Interpretations of Lin’s concordance coefficients were made based on the 2005 article by McBride et al, 14 “A Proposal for Strength-of-Agreement Criteria for Lin’s Concordance Correlation Coefficient,” which suggests that a coefficient of >0.99 indicates “almost perfect” correlation, 0.95 to 0.99 indicates “substantial” correlation, 0.90 to 0.95 indicates “moderate” correlation, and <0.90 indicates “poor” correlation. Interrater reliability was assessed using an intraclass correlation (ICC) analysis with a 2-way mixed model. Interpretations of ICC values were adopted from Cicchetti: values less than 0.40, between 0.40 and 0.59, between 0.60 and 0.74, and greater than 0.75 are indicative of poor, fair, good, and excellent reliability, respectively. 2 A P value of .05 was deemed the threshold for statistical significance. All statistical analyses were conducted using R statistical package version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
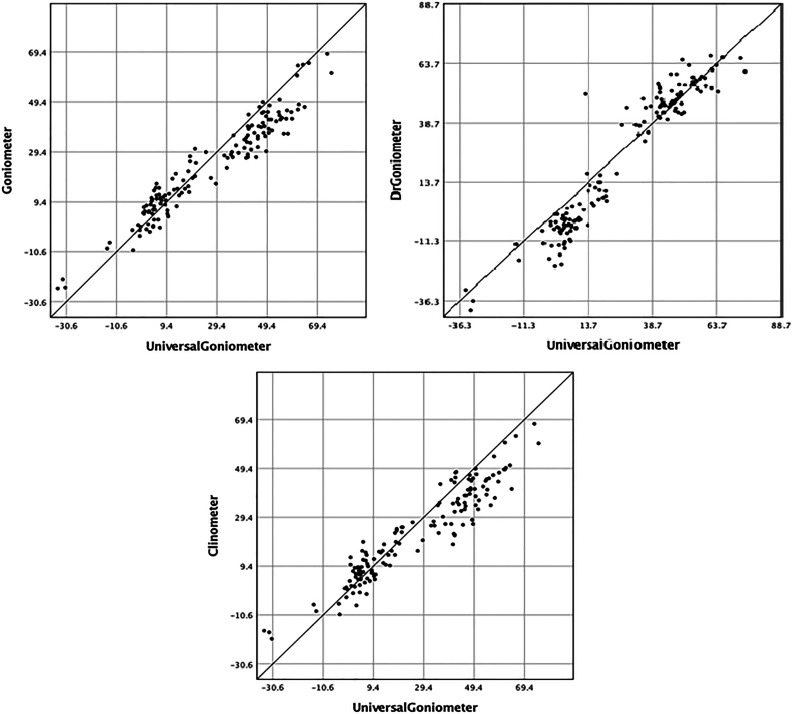
Lin’s concordance correlation coefficient test showed moderate correlation between the smartphone measurements and the UG measurements, suggesting that all 3 apps recorded measurements that were in agreement with those recorded by UG (Figure 7 and Table 1; Lin’s correlation coefficient [rLC] = 0.931, 95% confidence interval [CI] = 0.911-0.946 for UG-Gonio; rLC = 0.908, 95% CI = 0.881-0.929 for UG-Clino; rLC = 0.935, 95% CI = 0.915-0.950 for UG-DrG). The picture-based medical app, DrG, showed the highest correlation, while the accelerometer-based medical app, Clino, showed the lowest correlation, but the difference between the two was not statistically significant with the numbers available. A 2-way mixed model for each of the apps showed good to excellent interrater reliability for each of the apps for plantarflexion and dorsiflexion (Table 2; ICCp = 0.836, ICCd = 0.912, P < .001 for Gonio; ICCp = 0.788, ICCd = 0.893, P < .001 for Clino; ICCp = 0.777, ICCd = 0.897, P < .001 for DrG). Survey results are displayed in Table 3.
Figure 7.
Lin’s concordance correlation coefficient test showed moderate correlation between all the smartphone-based measurements and the measurements taken by the universal goniometer (Lin’s correlation coefficient [rLC] = 0.931, 95% CI = 0.911-0.946 for UG-Gonio; rLC = 0.908, 95% CI = 0.881-0.929 for UG-Clino; rLC = 0.935, 95% CI = 0.915-0.950 for UG-DrG).
Table 1.
Lin’s Correlation Coefficients Between the Universal Goniometer and Smartphone Apps.
| Characteristic | Lin’s Correlation | CI | P Value |
|---|---|---|---|
| UG-Gonio | 0.931 | 0.911-0.946 | <.001 |
| UG-Clino | 0.908 | 0.881-0.929 | <.001 |
| UG-DrG | 0.935 | 0.915-0.950 | <.001 |
Abbreviations: CI, confidence interval; UG, universal goniometer.
Table 2.
Interrater Reliability of Smartphone Apps.
| Characteristic | Reliability | P Value |
|---|---|---|
| Gonio | ||
| Plantarflexion | 0.836 | <.001 |
| Dorsiflexion | 0.912 | <.001 |
| Clino | ||
| Plantarflexion | 0.788 | <.001 |
| Dorsiflexion | 0.893 | <.001 |
| DrG | ||
| Plantarflexion | 0.777 | <.001 |
| Dorsiflexion | 0.897 | <.001 |
Table 3.
Survey Questions and Results.
| Characteristic | Very Comfortable | Comfortable | Neither Comfortable nor Uncomfortable | Uncomfortable | Very Uncomfortable |
|---|---|---|---|---|---|
| How comfortable are you having your ankle range of motion measured with a smartphone? | 15 | 7 | 2 | 0 | 0 |
| Yes | No | ||||
| Would you be willing to send photos of your ankle to your surgeon to monitor your ankle recovery? | 21 | 3 | |||
| Yes | Sometimes | No | |||
| If recommended by your surgeon or physical therapist, would you use your smartphone to measure your ankle range of motion at home to track your progress? | 15 | 6 | 3 | ||
| Yes | Possibly | No | |||
| Would seeing consistent improvement in your ankle range of motion motivate you to do more simple ankle exercises at home? | 19 | 5 | 0 | ||
| More Frequently | Same Amount | Less frequently | |||
| Would you measure your ankle range of motion more of less frequently at home if you could easily do it yourself? | 15 | 7 | 2 |
Discussion
To the authors’ knowledge, this is the first study to investigate the correlation between the clinical standard UG and 3 distinct types of apps (Gonio, DrG, Clino) for measuring ankle ROM in plantarflexion and dorsiflexion in a clinical setting. Furthermore, to the authors’ knowledge, this is the first study to survey patient sentiment about these ROM-measuring apps in the clinical setting. We found moderate correlation between all the smartphone measurements and the measurements taken by the UG, in addition to good to excellent interrater reliability for each of the apps for measuring plantarflexion and dorsiflexion. These results agree with previous studies that have also reported moderate to strong correlations between smartphone app measurements and UG measurements in various joints. 5,9,15,16,18 For the ankle joint specifically, Vohralik et al 21 reported a Pearson correlation of r = 1 (P < .01) between another app called iHandy Level and an inclinometer for measuring ankle dorsiflexion. In a separate study, Cox et al 4 reported a Pearson correlation of r = .92, (P < .001) between the Clinometer app and the UG for ankle plantarflexion.
There are a few potential reasons why this present study demonstrated slightly lower correlations than a few past studies like those of Cox et al 4 and Vohralik et al. 21 First, our study measured pathologic ankles and incorporated a different way of standardizing the ankle measurements compared to previous studies. In Vohralik et al, 21 only healthy participants were included, and measurements were taken with the participants’ ankles dorsiflexed against a wall. In Cox et al, 4 the health statuses of participants were not determined, and a thin bolster was used to standardize the participants’ ankles for measurements. Although some ankle stabilization is important for producing reliable measurements, taking time to overstabilize the ankle is not always practical in clinical practice when caregivers need to measure ankle ROM quickly. Our study measured patients’ pathologic ankles in a clinical setting, so our study naturally found slightly less correlation and higher variability. Even so, the results of our study add to current literature by affirming the ability to use smartphone apps to measure ankle ROM in clinic, in addition to controlled research settings as previous studies have shown. To be sure, some minimal standardization process is required for measuring ankle ROM accurately. Our investigation established this minimal standardization as flexing the knee joint at 90 degrees while the participant sat upright with legs hanging over the table, which was maintained throughout the measurement process for each participant. The authors maintain that this method of standardization is reproducible enough to be consistently used in clinic.
A second potential reason for the slight deviations of this study’s results from those of previous studies is that no previous study assessing ankle ROM has used Lin’s concordance analysis. Lin’s concordance analysis has been shown to be a superior method for comparing a set of values to a standard set of values, as done in this present study. 11 However, there is not yet an established conversion system between Lin’s concordance coefficient and other correlation coefficients, preventing a direct comparison between Lin’s coefficient and correlation coefficients commonly used in other studies like Pearson’s coefficient. Regardless, values for Lin’s coefficient tend to be lower than for Pearson’s coefficient due to the fact that Lin’s coefficient accounts for both covariation and correspondence. 11 In terms of interrater reliability, Alawna et al 1 reported excellent interrater reliability between smartphone measurements and UG measurements in both dorsiflexion (ICC = 0.91) and plantarflexion (ICC = 0.82). The good to excellent interrater reliability of smartphone measurements that we found in our study supports findings by Alawna et al. 1
With the numbers available, this study suggests that there is no significant difference between the measurements from the 3 types of apps that were used in this investigation. This conclusion should give providers and patients confidence to choose an app based on personal preference. Moreover, clinicians should also feel comfortable using any of these 3 app types to measure ankle ROM for determining workers’ compensation and impairment ratings.
Although the 3 apps yielded similar measurements, they operate in different ways. Clino and Gonio are similar apps in how they measure angles, but Gonio is designed and marketed for medical purposes, whereas Clino is not. However, this study still demonstrated the accuracy of Clino relative to the clinical standard UG. Of the 3 apps, DrG is the only one that can store picture-based measurements. This may be important, as most participants surveyed in this study indicated that they would be willing to send pictures of their ankle to their surgeons to remotely assess ROM (21/24 yes; 3/24 no).
The concept of biofeedback has been explored in other fields such as poststroke motor recovery, but only a few studies have been conducted on the efficacy of biofeedback for improving joint ROM. 8 A patient being encouraged to continue working on increasing ROM after seeing numerical evidence of improvement is an application of biofeedback. If this principle is as effective in increasing ROM as it is in other scenarios, then an app with the ability to document and display ROM measurement and progress over time could potentially prove useful in rehabilitation from joint injuries. Of the participants surveyed in this investigation, a heavy majority responded that seeing consistent improvement in ankle ROM motion would motivate them to do more simple ankle exercises at home (19 yes; 5 possibly; 0 no). Further studies would be necessary to determine whether the principle of biofeedback can indeed be applied effectively to ROM.
Smartphone apps could allow patients to more frequently measure ankle ROM in nonclinical settings like their own home, since most patients now own smartphones and can download ROM-measuring apps that are substantially cheaper than a UG. 10 Most patients surveyed in this study reported that they would measure their ankle range of motion more frequently at home if they could easily do it themselves (15 more frequently; 7 same amount; 2 less frequently). Introducing mobile apps into the medical sector generally comes with a level of uncertainty about whether patients and providers will buy into and ultimately trust these technologies. 7 In this investigation, most participants were very comfortable having their ankle ROM measured by a smartphone (15/24 very comfortable; 7/24 comfortable; 2/24 neither comfortable nor uncomfortable). Furthermore, most participants reported that they would use their smartphones to measure their ROM if recommended by their surgeon (15/24 yes; 6/24 sometimes; 3/24 no). Overall, since most patients represented by this study’s survey held favorable opinions about using apps to measure ankle ROM, this study found no reason for health care providers to expect pushback from patients against using apps to measure ankle ROM in clinic.
This study is not without limitations. Both the survey and ROM measurements in this study are limited by sample size. By using the fifth metatarsal as a landmark for measurement, as opposed to using the plantar aspect of the heel, the dorsiflexion and plantarflexion measurements likely obtained a component of midfoot and forefoot motion. Participant leg positions were not as strictly standardized as in some other studies, which may have contributed to the slightly lower correlations in our measurements. Participant fatigue may have also added slight variability in the results, as participants were instructed to plantarflex and dorsiflex their ankles numerous times for multiple examiners; the order of app usage was randomized to try to limit bias due to this fatigue.
There are many directions in which the present study can be expanded upon. Since many new apps are developed yearly, further studies must assess newer ROM apps on the market. Currently, none of the apps currently in the Apple App Store allow patients to conveniently measure their own ankle ROM without the help of a caregiver. This is primarily due to the distal location of the ankle joint relative to other commonly measured joints like the elbow or knee, which makes it nearly impossible for a patient to measure ankle ROM independently using present apps. An attempt was made in this study to have participants self-measure ankle ROM by strapping the smartphone to their feet, but the participants had too much difficulty maneuvering the smartphone at the level of the ankle. Further studies should be done on any newer apps that may give patients this ability of pure self-measurement of ankle ROM, which would increase accessibility of such apps for patients living on their own. Apps allowing patients to measure their own ankle ROM would also open more possibilities for studying biofeedback applied to ankle rehabilitation.
Supplemental Material
Supplemental Material, FAO874779-ICMJE for Smartphone Applications for Assessing Ankle Range of Motion in Clinical Practice by Kevin Y. Wang, S. Hanif Hussaini, Robert D. Teasdall, Chukwuweike U. Gwam and Aaron T. Scott in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kevin Y. Wang, BA,  https://orcid.org/0000-0001-9641-6462
https://orcid.org/0000-0001-9641-6462
References
- 1. Alawna MA, Unver BH, Yuksel EO. The reliability of a smartphone goniometer application compared with a traditional goniometer for measuring ankle joint range of motion. J Am Podiatr Med Assoc. 2019;109(1):22–29. [DOI] [PubMed] [Google Scholar]
- 2. Cicchetti DV. Guidelines, Criteria, and Rules of Thumb for Evaluating Normed and Standardized Assessment Instruments in Psychology. Psychol Assess. 1994;(4):284–290. [Google Scholar]
- 3. Commission NCI, Guide N.C. Industrial commission rating. http://www.ic.nc.gov/ncic/pages/ratinggd.htm. Published 2000. Accessed February 19, 2019.
- 4. Cox RW, Martinez RE, Baker RT, Warren L. Validity of a smartphone application for measuring ankle plantar flexion. J Sport Rehabil. 2017;27(3):2017–2019. [DOI] [PubMed] [Google Scholar]
- 5. Ebrahimi Takamjani I, Rajabzadeh F, Sarrafzadeh J, et al. Reliability and concurrent validity of a new iPhone goniometric application for measuring active wrist range of motion: a cross-sectional study in asymptomatic subjects. J Anat. 2016;230(3):484–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jonson LSR, Gross MT. Intraexaminer reliability, interexaminer reliability, and mean values for nine lower extremity skeletal measures in healthy naval midshipmen. J Orthop Sport Phys Ther. 2013;25(4):253–263. [DOI] [PubMed] [Google Scholar]
- 7. Kao CK, Liebovitz DM. Consumer mobile health apps: current state, barriers, and future directions. PM R. 2017;9(5):S106–S115. [DOI] [PubMed] [Google Scholar]
- 8. Kim S, Cho H, Kim K, Lee S. Effects of ankle biofeedback training on strength, balance, and gait in patients with stroke. J Phys Ther Sci. 2016;28(9):2596–2600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim TS, Park DDH, Lee YB, et al. A study on the measurement of wrist motion range using the iPhone 4 gyroscope application. Ann Plast Surg. 2014;73(2):215–218. [DOI] [PubMed] [Google Scholar]
- 10. Lee J. Future of the smartphone for patients and healthcare providers. Healthc Inform Res. 2016;22(1):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lin L. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45(1):255–268. [PubMed] [Google Scholar]
- 12. Lumenta DB, Tuca A, Kuegler P, et al. Goniometer-apps in hand surgery and their applicability in daily clinical practice. Saf Heal. 2015;1(1):1–7. [Google Scholar]
- 13. Lynch SA, Renstrom PAFH. Treatment of acute lateral ankle ligament rupture in the athlete. Sport Med. 2006;27(1):61–71. [DOI] [PubMed] [Google Scholar]
- 14. McBride G, Bland JM, Altman DG, Lin LI. A proposal for strength-of-agreement criteria for Lin’s concordance correlation coefficient. NIWA Client Rep. 2005;45(1):307–310. [Google Scholar]
- 15. McCormack S, O’Sullivan W, Buettner P, et al. Reliability and concurrent validity of knee angle measurement: smart phone app versus universal goniometer used by experienced and novice clinicians. Man Ther. 2014;19(6):569–574. [DOI] [PubMed] [Google Scholar]
- 16. Milani P, Coccetta CA, Rabini A, Sciarra T, Massazza G, Ferriero G. Mobile smartphone applications for body position measurement in rehabilitation: a review of goniometric tools. PM R. 2014;6(11):1038–1043. [DOI] [PubMed] [Google Scholar]
- 17. Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting: elbow and knee measurements. Phys Ther. 1983;63(10):1611–1615. [DOI] [PubMed] [Google Scholar]
- 18. Santos C, Pauchard N, Guilloteau A. Reliability assessment of measuring active wrist pronation and supination range of motion with a smartphone. Hand Surg Rehabil. 2017;36(5):338–345. [DOI] [PubMed] [Google Scholar]
- 19. Smith D. Measurement of joint range—an overview. Clin Rheum Dis. 1982;8:523–531. [PubMed] [Google Scholar]
- 20. Venturni C, André A, Aguilar BP, Giacomelli B. Reliability of two evaluation methods of active range of motion in the ankle of healthy individuals. Acta Fisiatr. 2006;13(1):39–43. [Google Scholar]
- 21. Vohralik SL, Bowen AR, Burns J, Hiller CE, Nightingale EJ. Reliability and validity of a smartphone app to measure joint range. Am J Phys Med Rehabil. 2015;94(4):325–330. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO874779-ICMJE for Smartphone Applications for Assessing Ankle Range of Motion in Clinical Practice by Kevin Y. Wang, S. Hanif Hussaini, Robert D. Teasdall, Chukwuweike U. Gwam and Aaron T. Scott in Foot & Ankle Orthopaedics