Abstract
The COVID-19 pandemic created an opportunity to incorporate nurse-led virtual home care visits into heart failure patients’ plan of care. As a supplemental nurse visit to traditional in-person home visits, the Virtual Nurse Visit (VNV) service was deployed using Zoom teleconferencing technology enabling telehealth nurses to remotely communicate, assess, and educate their patients. This mixed methods study explored heart failure patients’ abilities, experience, and satisfaction to use and adopt a virtual nurse visit. Sociodemographic, semi-structured interview questions, and the System Usability Scale data were collected. Thirty-four participants completed the study. Over half of participants perceived the VNV usable and four qualitative themes emerged: perceived safety during COVID-19, preferences for care delivery, user experiences and challenges, and satisfaction with the VNV service. Findings from this study builds the science around telehealth that will inform future studies examining this type of nurse-led virtual visit and subsequent patient outcomes.
Keywords: Virtual care, home health, nursing, telehealth
Introduction
Heart failure (HF) is a chronic condition that affects approximately 6.9 million Americans (Urbich et al., 2020) with an estimated 900,000 new cases diagnosed annually (American Heart Association (AHA), 2020). HF alone contributes to nearly one million hospitalizations and 11 million primary care visits (Emory Healthcare, 2019) costing approximately 43.6 USD billion per year (Urbich et al., 2020). HF continues to rank among the highest healthcare expenditure in the U.S with continued expected growth over the next decade, creating an economic burden on healthcare systems (Urbich et al., 2020).
Common comorbidities contributing to this economic burden include hypertension, diabetes, coronary artery disease, and chronic obstructive pulmonary disease (AHA, 2020). These chronic conditions often require complex, multi-faceted care to maintain optimal health and to prevent rehospitalizations (Bauce, Fahs, Batten, & Whittemore, 2018; Idris et al., 2015). This care necessitates adherence to a variety of treatment regimens, self-management of physical health, and recognition of symptoms that require interventions (Bauce et al., 2018) that may be difficult for patients and their caregivers to manage on their own. Therefore, HF patients discharged from inpatient settings are often referred to home health care (HHC) services to decrease the risk of rehospitalization (Jones, Bowles, Richard, Boxer, & Masoudi, 2017). In the home setting, HHC nurses help HF patients manage their chronic conditions and bridge the gap between hospital and self-care (Bauce et al., 2018). HHC nurses’ primary roles during the post-hospitalization period include being a clinician, teacher, nutritionist, and coach for comprehensively managing patients’ care (Ong et al., 2016). Their efforts make the complicated work of HF management feasible for patients and their caregivers while preventing rehospitalization.
Heart failure management in HHC during COVID-19
In March 2020, the World Health Organization (WHO) (2020a) declared the COVID-19 virus a global pandemic. In the United States, this resulted in 42 states and territories issuing mandatory stay-at-home orders to slow the spread of the COVID-19 virus (Centers for Disease Control and Prevention [CDC], 2020). COVID-19 is an infectious virus causing mild to moderate respiratory illness; however, vulnerable individuals may experience serious illness (WHO, 2020b). HF patients are considered to be vulnerable and at increased risk for complications during the post hospitalization period. Because of their vulnerability, continuity of care must be preserved regardless of the COVID-19 pandemic. Continuity of care could be maintained with telehealth services, which are defined as the use of electronic information and telecommunications to support remote clinical health care (The Office of the National Coordinator for Health Information Technology [ONC], 2019). Use of telehealth may support patients at multiple points of care providing opportunities for nurses to implement novel approaches to care for patients in their homes (Bauce et al., 2018), especially for heart failure patients who are at high risk of hospital readmission.
Virtual nurse visit using zoom teleconferencing technology
To minimize the risks of COVID-19 exposures through direct in-person contact and to sustain HF patients’ continuity of HHC services, the Virtual Nurse Visit (VNV) using Zoom teleconferencing technology was implemented by a large suburban healthcare system in Delaware as a supplement to in-person home nurse visits. Zoom provided secure bi-directional high-definition video and audio meetings (Zoom, 2020). Additional layers of security were added by prohibiting e-mail or texting of links, requiring the use of passcodes, and the utilization of Zoom’s waiting room before admittance.
The VNV centered around telehealth nurses educating patients and often their caregivers about their chronic disease management, prevention of HF exacerbations, and rehospitalization avoidance through Zoom communication. These virtual visits typically occurred on days when an in-person home nursing appointment was not scheduled. Patients used their smartphones, iPads/tablets, or computers to interact with their telehealth nurses. In addition to Zoom teleconferencing, telehealth nurses used a telemonitoring system to assess daily vital signs and weight for significant changes. During the 20–30-minute visit, telehealth nurses discussed and addressed patients’ current state of health, concerns, and questions. Most often, the telehealth nurses discussed new or worsening symptoms common to HF patients, management of those symptoms, medication and possible side effects, and reviewed vital signs, and dietary choices. If patients had other chronic conditions, such as diabetes or wounds, the telehealth nurses addressed those issues and concerns. Additionally, telehealth nurses reminded patients of upcoming appointments and when to contact their primary care office.
The VNV is an innovative approach for nurses to care for their patients remotely. However, much is still unknown about patients’ ability and willingness to adopt a new care delivery modality and the extent to which this new encounter will impact patients’ care experiences and satisfaction. Gaining a better understanding of patients’ barriers to technology use and adoption is critically important. Therefore, the purpose of this study was to 1) explore the facilitators and challenges of HF patients’ ability to use and potentially adopt the VNV, and to 2) assess their satisfaction and experiences using the VNV in conjunction with traditional in-person homecare nursing visits.
Materials and methods
Theoretical framework
Diffusion of Innovation (DOI) theory served as a guide to understanding decision-making processes involved in the adoption of the VNV innovation (Rogers, 2003). The DOI theory consists of four constructs: communication, time, social systems, and innovation. Innovation, defined as an idea, practice, or object considered new (Rogers, 2003), was the construct of interest in this study. According to DOI theory, the following five factors explain the rate of adoption of an innovation: relative advantage, compatibility, complexity, trialability, and observability (Rogers, 2003). Relative advantage, compatibility, complexity and trialability characteristics guided this study. Relative advantage, defined as the degree to which an innovation is perceived as being better than what is currently in place and trialability refers to the degree to which an innovation is perceived as relatively difficult to understand and use (Rogers, 2003). Compatibility is defined as the degree to which an innovation is perceived as consistent with the existing values, past experiences, and needs of potential adopters (Rogers, 2003). Finally, complexity refers to the extent to which the environment is ready for a technological innovation. (Rogers, 2003).
Design
A mixed method convergent parallel design (QUAL + QUAN) was used to describe and explore the complexity and contextual factors associated with adopting the VNV service delivered via Zoom to an at-risk HF population during a pandemic. Coupling quantitative and qualitative data and encouraging investigators to compare complementary data sets illuminated and deepened understanding of research findings and context not captured by a singular approach (Creswell & Plano Clark, 2018). Qualitative data were collected using semi-structured interview questions about the fear of COVID-19 transmission, trialability and complexity of the VNV service, compatibility with existing values, and relative advantage of the VNV. Quantitative data were collected to assess participant sociodemographic characteristics, measure perceived usability from the System Usability Scale (SUS) and satisfaction from Likert scales. All study protocols and tools were reviewed and approved by the ChristianaCare Institutional Review Board.
Study population and setting
Adult HF patients at risk of rehospitalization who were receiving HHC in their home or assisted living residence were recruited using convenience sampling. Participation was open to HF patients who consented to and enrolled in the VNV service, were receiving HHC services and would complete at least three VNVs with the ability to read, write, and speak English. HF patients on the HHC service were ineligible to participate if they had visual and/or auditory deficits, were disoriented to person, place, or time, had short-term memory impairment or significant physical impairment, and were only schedule for one HHC appointment. Participants who did not own a smart device were loaned an iPad for the duration of their home care episodes.
Data collection procedure
Prior to recruitment, study team members screened adult HF patients admitted to the HHC service for eligibility. Eligible patients were introduced to the study at the end of their first VNV. Eligible, interested patients received the informed consent via e-mail link to review with a study team member. At the end of the third VNV, a study team member administered all measures (i.e., demographic and SUS questionnaires and semi-structured interview questions). Responses were recorded verbatim and directly entered into the study’s REDCap database.
Sociodemographic data were abstracted from electronic medical record prior to the third VNV. At the third VNV, a study team member displayed and read participants the 11 semi-structured interview questions about COVID-19 fears, trialability, compatibility, complexity, and relative advantage of the VNV. Trialability of the VNV was also measured using the SUS, a reliable tool for measuring perceived usability of a wide variety of products and services (U.S. Health and Human Services [HHS], 2020). The SUS consists of 10 questions measured by five Likert options from strongly disagree to strongly agree (HHS, 2020). Satisfaction questions were measured on a 5-point Likert scale (strongly disagree to strongly agree). To ensure confidentiality, participants’ informed consent and data were collected in the secure REDCap web application with access limited to study team members.
Data analysis
Descriptive statistics (mean, standard deviation, frequency, and percentage) were calculated for sociodemographic characteristics and SUS measures using Statistical Package for Social Sciences (SPSS) version 25 software. Individual SUS survey questions for each participant were recalculated using the SUS scoring sheet (HHS, 2020). Qualitative analyses were conducted for the 11 semi-structured qualitative interview questions. Microsoft Excel and Word were used to structure codes, document emerging themes, and select and document illustrative quotes. Interview questions were first analyzed manually to examine the context of each participants’ experiences as well as to determine similarities and differences among these experiences (Creswell & Plano Clark, 2018). Traditional coding methods were used to generate scientific themes using an inductive approach by five study team members that included two qualitative experts. Integration of qualitative and quantitative data occurred during the final analytic step. Using a convergent approach (Creswell & Plano Clark, 2018), merged data sets were compared to provided deeper insight into the facilitators and barriers to VNV adoption.
Results
One hundred eighty-eight patients were screened for eligibility to participate in the study and 65 met the inclusion criteria (Figure 1). Thirty-four participants enrolled into this study. Participant sociodemographic characteristics are summarized in Table 1. Almost equal numbers of males (n = 16, 47%) and females (n = 18, 53%) participated. The mean age was 75 years (SD±11), ranging from 59 to 98 years. Participants were either white (n = 27, 79%) or black/African American (n = 7, 21%). Most participants were alert and oriented (n = 23, 68%), had no confusion (n = 24, 71%), and lived with another person (n = 27, 79%) around the clock (n = 28, 82%) with a moderate (n = 13, 38%) to high risk (n = 19, 56%) of rehospitalization.
Figure 1.
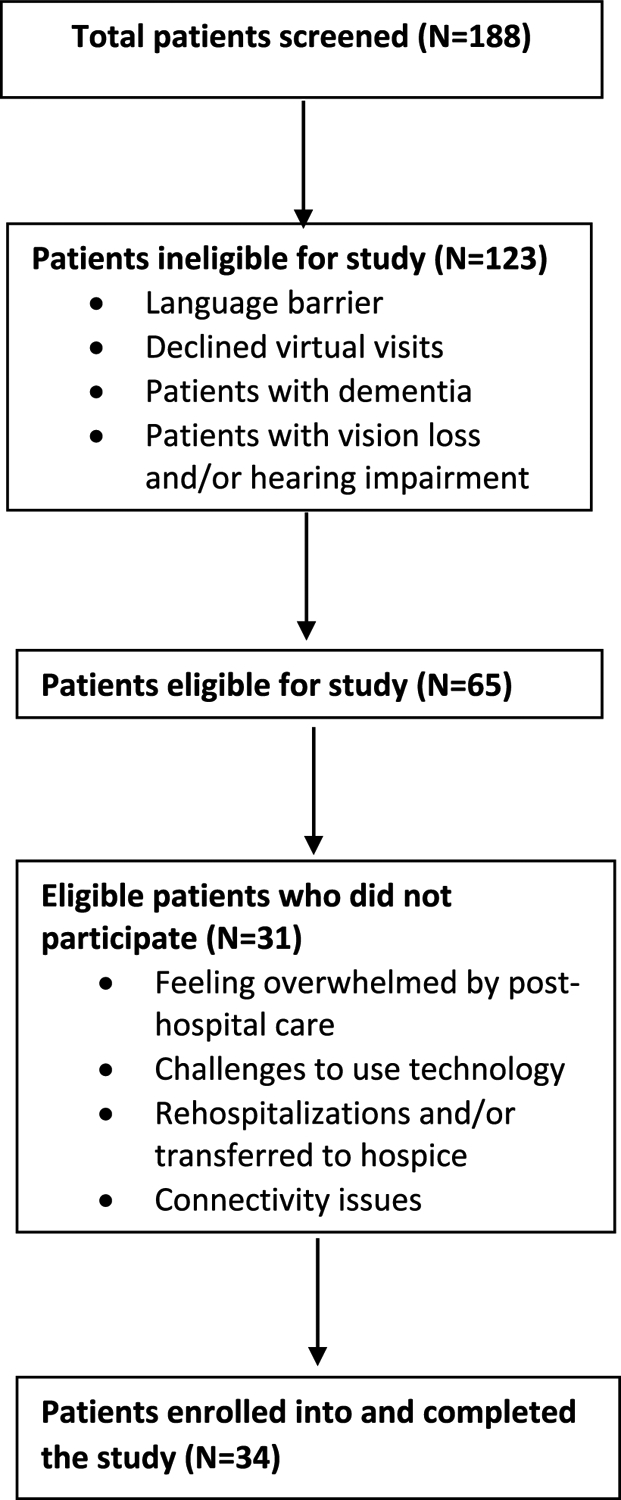
Patient screening and enrollment flow diagram.
Table 1.
Participant sociodemographic characteristics (N = 34).
| Age, years | mean (SD) |
|---|---|
| 75 (11) | |
| Gender | n (%) |
| Male | 16 (47%) |
| Female | 18 (53%) |
| Marital Status | n (%) |
| Single | 6 (18%) |
| Married | 14 (41%) |
| Widowed | 11 (32%) |
| Divorced | 3 (9%) |
| Race | n (%) |
| White | 27 (79%) |
| Black | 7 (21%) |
| Hispanic | 0 (0%) |
| Asian | 0 (0%) |
| Education * | n (%) |
| Some high school | 3 (9%) |
| High school graduate | 15 (44%) |
| Some college | 12 (35%) |
| Trade/technical school | 1 (3%) |
| Associate degree | 2 (6%) |
| Risk of hospitalization | n (%) |
| Low | 1 (3%) |
| Moderate | 13 (38%) |
| High | 19 (56%) |
| Very high | 1 (3%) |
| Living arrangement | n (%) |
| Patient lives alone | 7 (21%) |
| Patient lives at home with another person | 27 (79%) |
| Patient lives in congregate situation | 0 (0%) |
| Caregiver presence | n (%) |
| Around the clock | 28 (82%) |
| Regular daytime | 0 (0%) |
| Regular nighttime | 0 (0%) |
| Occasional/short term assistance | 5 (15%) |
| No assistance available | 1 (3%) |
| Neurological status | n (%) |
| Alert and oriented | 23 (68%) |
| Required prompting | 10 (29%) |
| Requires assistance and some directions in specific situations | 1 (3%) |
| Requires considerable assistance in routine situations | 0 (0%) |
| Totally dependent | 0 (0%) |
| Confusion | n (%) |
| Never | 24 (71%) |
| In new or complex situations only | 9 (27%) |
| On awakening or at night only | 1 (3%) |
| During the day or evening, but not constantly | 0 (0%) |
| Constantly | 0 (0%) |
| Nonresponsive | 0 (0%) |
| Supervisions and safety | n (%) |
| No assistance is needed – independent | 15 (44%) |
| Non-agency caregivers providing assistance | 13 (38%) |
| Non agency caregivers need training/support | 5 (15%) |
| Non-agency caregivers not providing assistance or unclear | 1 (3%) |
| Assistance needed, no non-agency caregivers available | 0 (0%) |
1 missing response
Thirty-four patients responded to the semi-structured interview questions. Four themes emerged from the qualitative data: 1) perceived safety during COVID-19, 2) preferences for delivery of care, 3) user experiences and challenges with the VNV service, and 4) satisfaction with VNV. Table 2 provides themes with illustrative examples.
Table 2.
VNV qualitative themes.
| Perceived Safety | Preferences for Delivery |
|
|
| User Experience | Satisfaction |
|
|
Relative advantage
Theme 1: perceived safety during COVID-19
Participants perceived the VNV to be advantageous compared to traditional in-person home nursing visits. Almost half of the participants (n = 16, 47.1%,) stated they felt safer with the VNV while a minority of patients (n = 7, 20.6%,) had COVID-19-related concerns or fears. Most participants reported they were not afraid of COVID-19 because their nurse wore personal protective equipment (PPE) upon entering their residence. Participants trusted that their nurses would not place them at risk of contracting the virus, “everyone is good about wearing their protective gear and sanitizing”. Some participants felt safe because they had negative COVID-19 results, did not believe the pandemic was real, or were relieved the nurse is “not in the house with me”.
Theme 2: preference for delivery of care
Half of participants (n = 17, 50%) considered the VNV to be comparable to in-home nursing visits. One participant stated the VNV was “Just as good but not better. Just as good.” while others felt “it’s not that different. It doesn’t matter which one I have.” Other participants expressed a strong preference for the VNV stating “I understand that nurses have to come to the house … and that is okay. I just like this [VNV] better.” One participant also perceived an increased length of visit with the VNV, stating “You cover a lot of ground. You can do more talking about things this way. There is more time.”
Those who did not prefer the VNV to in-person visits mentioned difficulties using technology, taking their own vitals, feeling like it was hard to hear during the VNV, or an overall preference for in-person encounters. While these participants were willing to participate in VNVs out of necessity, they preferred the nurse to be face-to-face and would like to continue using VNVs only as a supplement to in-person care in the future. Participants expressed concern over the telehealth nurse’s inability to complete physical and environmental assessments that are typically done during in-person visits. For example, “When the nurse comes in the house, she can see for herself what is going on. I don’t have to worry about making sure I am telling the right thing and remembering things.” Several participants also mentioned feeling more secure when nurses were in-person. For example, “When the nurse comes, she can check his vitals and listen to his lungs. That makes us [sic] feel better.”
Trialability, complexity, and compatibility
Several qualitative themes had overlapping meaning with trialability, complexity, and compatibility. To explore trialability at the third VNV, participants answered the System Usability Scale (SUS) to measure their perception of VNV’s usability. The mean SUS score was 66 (SD±17) with a range of 20–98. In our study, the 50th percentile score was 68. Using the SUS’ benchmarked general usability score of 68 or above (HHS, 2020), more than half of the participants scored the VNV at 68 or higher (n = 18, 53%). Individual questions (Table 3) revealed most participants agreed (n = 24, 71%) or strongly agreed (n = 5, 15%) the VNV was easy to use, yet there appeared to be a learning curve associated with using the technology, which may have contributed to the lower SUS mean score.
Table 3.
System usability scale (SUS) results.
| 1. I think I would use this system frequently. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 0 (0%) | 2 (6%) | 3 (9%) | 22 (65%) | 7 (21%) |
| 2. I found the system unnecessarily complex. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 5 (15%) | 21 (62%) | 2 (6%) | 6 (18%) | 0 (0%) |
| 3. I thought the system was easy to use. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 0 (0%) | 2 (6%) | 3 (9%) | 24 (71%) | 5 (15%) |
| 4. I think that I would need the support of a technical person to be able to use this system. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 4 (12%) | 12 (35%) | 0 (0%) | 13 (38%) | 5 (15%) |
| 5. I found the various functions in this system well integrated. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 0 (0%) | 2 (6%) | 9 (27%) | 19 (56%) | 4 (12%) |
| 6. I thought there was too much inconsistency with this system. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 6 (18%) | 21 (62%) | 4 (12%) | 2 (6%) | 1 (3%) |
| 7. I would imagine that most people would learn to use this system very quickly. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 1 (3%) | 2 (6%) | 8 (24%) | 21 (62%) | 2 (6%) |
| 8. I found the system very cumbersome to use. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 3 (9%) | 23 (68%) | 0 (0%) | 4 (12%) | 4 (12%) |
| 9. I felt very confident to use this system. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 1 (3%) | 2 (6%) | 2 (6%) | 23 (68%) | 6 (18%) |
| 10. I need to learn a lot of thinqs before I could qet qoinq with this system. | ||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| 4 (12%) | 12 (35%) | 2 (6%) | 12 (35%) | 4 (12%) |
Theme 3: user experiences and challenges with the VNV service
Fewer than half of the participants (n = 14, 41%) reported previous experience with telehealth visits or virtual communication tools, such as Zoom or FaceTime. All participants reported having a positive experience with the VNV and many preferred to see their nurse on their smart device, rather than just hearing them on a phone call. As noted by one participant, “It is nice to have a face and voice contact. This is a more secure feeling then just over the phone.” Other benefits of the VNV included the convenience of not having to leave the house or clean the house prior to a VNV. One participant mention, “nicer than having to get ready for someone to come here or having to go out” noted two participants.
Participants also reported various challenges with accessing their Zoom session due to the requirement of inputting numerical passcodes to enter the secured VNV. Participants new to using technology experienced a learning curve with using this software; however, the telehealth nurse provided education during each VNV. For example, one participant stated, “I don’t think I really had any challenges. Once the nurse showed me how to use Zoom, it was easy.” Additional assistance was often required by family members to set up the VNV; however, most participants (n = 27, 79%) lived with another person. Almost a third of participants (n = 10, 20%) needed a family member to connect or initiate the VNV for them.
The unfamiliarity with technology posed additional challenges. One participant stated, “I find it very stressful. My son showed me how to do it, but I prefer just the old-fashioned way. It’s something I worry I won’t be able to do when I need to.” Participants cited issues with poor internet connectivity, difficulties navigating the software, and forgetting how to access the visit. Participants with limited physical abilities expressed additional challenges. A quarter of participants did not provide recommendations for improvement because a family member managed the VNV for them. A common challenge noted by participants was the absence of a one click hyperlink sent via text message or e-mail to avoid the difficulty of inputting numerical passwords to easily access the VNV.
Theme 4: satisfaction with VNV
At the participants’ third VNV, they were asked a series of satisfaction questions (see Table 4). All participants (100%, n = 34) expressed that they were satisfied (agreed or strongly agreed) with the ability to see and talk to their nurse during the VNV. Most participants agreed (n = 19, 56%) or strongly agreed (n = 10, 29%) they were satisfied with the education they received to use the Zoom technology. Lastly, most participants agreed or strongly agreed they would recommend the VNV to other patients like them and they would like to see the VNV used more often in their plan of care.
Table 4.
Satisfaction scores.
| I was satisfied with the ability to see and talk to my nurse through this virtual nurse visit. | ||||
| Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 0 | 0 | 0 | 15 (44%) | 19 (56%) |
| I was satisfied with the education I received on how to use Zoom for this virtual nurse visit. | ||||
| Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 0 | 0 | 5 (15%) | 19 (56%) | 10 (29%) |
| I would recommend this virtual nurse visit to other patients like me. | ||||
| Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 0 | 2 (6%) | 2 (6%) | 9 (27%) | 21 (62%) |
| I would like to see the virtual nurse visit used more often in my plan of care. | ||||
| Strongly disagree | Disagree | Undecided | Agree | Strongly agree |
| 0 | 5 (15%) | 6 (18%) | 12 (35%) | 11 (32%) |
Qualitative satisfaction results were aligned with the quantitative satisfaction scores. All participants expressed some degree of satisfaction with VNV. Participants emphasized that they liked being able to see the nurse and perceived greater accessibility regarding scheduling visits. As one participant stated, “I like that I can call someone and see them. I don’t feel alone. This is easier than waiting for a nurse to come.” Another area of satisfaction among participants was the ability to discuss their concerns with their telehealth nurse. The consistency of having the same telehealth nurse at each VNV was also appreciated and many participants responded that they would not change anything about their VNV experience. Those who felt that the experience could be improved mentioned that it would be helpful if the complexity of connecting to the virtual platform and WiFi connectivity issues could be resolved.
Discussion
The VNV was conceptualized, planned, and implemented to address increased cancellations of in-person HHC visits at the start of the COVID-19 pandemic. HF patients benefit from intensive monitoring and symptom management offered during in-person HHC visits (Jones et al., 2017), yet the pandemic created unique challenges to maintain a safe and appropriate level of in-person care. Quickly optimizing the VNV supplemented in-person HHC visits with the intention of reducing potential COVID-19 exposure while simultaneously delivering consistent, high-quality care. However, barriers to use and adoption exist as many elderly patients are not digital natives and may struggle with the usability of and learning curve associated with adopting a virtual care service (Huang, Lu, Alizadeh, & Mostaghimi, 2016). Therefore, this study was a critical first step to understanding the facilitators and barriers influencing the use and adoption of the VNV.
The study sample consisted of an almost even enrollment of male and female participants of whom were mostly white, older/elderly adults (mean age = 75 years) living with family members around the clock. Most participants had a moderate to high risk of rehospitalization. Some black/African American participants (n = 7, 21%) enrolled in the study, but no other races were represented in this sample. This lack of diversity could be related to the inability to read, speak, and understand English, in addition to possible limited access to digital platforms, all of which may have precluded individuals from participating in this study. Mitchell, Chebli, Ruggiero, & Muramatsu’s (2019) study found minority populations were less likely to use technology for health-related purposes. Additionally, Nouri, Khoong, Lyles, and Karliner (2020) reported that digital barriers are commonly found in racial minorities and those of low socioeconomic status, limited English proficiency and low health literacy. Together, these findings suggest that future studies assessing a VNV type of service may benefit from offering the study in additional languages and recruiting from various minority populations. Further, exploring socioeconomic factors and other determinants of technology use and health literacy may further enhance understanding.
Study investigators, guided by the innovation construct of the DOI theory, identified several facilitators and challenges experienced by older adult HF patients when engaging with the VNV using Zoom technology. Based on the trialability characteristic, more than half of the participants perceived the VNV usable measured by the total SUS score, yet more customization is needed to create an easier process to log in and to navigate the system. This was evident when participants first began logging into the VNV, most participants were unable to use the hardware or software independently without the help of another tech savvy caregiver, in addition to the reinforcement education delivered by the telehealth nurses. Based on the qualitative data, inputting Zoom numbers and turning on the video were initial challenges. Sometimes, the telehealth nurses had to use a regular telephone for audio and Zoom for video because participants could not figure out how to turn up the audio on their smart phone or tablet. This finding is supported by Delello and McWhorter’s (2015) mixed-method study in which they found older adults do not have the manual dexterity nor the foundational skills to use smart technology adeptly and thus, needed additional help to use technology. Interestingly, because the pandemic created a situation in which many grand-children were learning remotely at home, they were available to help participants troubleshoot any issues. Once participants learned how to connect to Zoom and to navigate the screens, they appeared to be capable of using the hardware and software without difficulty.
To have increased VNV adoption, especially as the pandemic continues, the hardware and/or software cannot be too complex to use and should be compatible with current needs and past experiences. Many successful VNVs involved either having personal experience using technology such as through shopping or playing games online or having a technology savvy person available to facilitate log in. Conversely, for some participants who lived alone, much of the VNV was spent reviewing and reinforcing how to navigate the system. These findings are supported in Huang et al. (2016) qualitative descriptive study highlighting the degree of familiarity and perceived ability to learn a new technology was influenced by attitudes toward telehealth care. Having a baseline comfort level with different types of technology created positive attitudes to adopt telehealth services (Huang et al., 2016).
For the VNV to be considered to have a relative advantage to in-person HHC visits, the VNV must be viewed as having a clear benefit in addition to the in-person HHC visits. One distinct advantage of the VNV was the reduced feeling of pressure to prepare oneself or one’s house for an in-person visit. Another benefit to the VNV is the impossibility of transmitting the COVID-19 virus. One participant stated, “Yeah, I’m not worried about you. You can’t breathe on me.” Many participants appreciated connecting with their telehealth nurse on days when they did not have an in-person HHC visit. Additionally, participants perceived their VNV lasted longer, even though in-person and VNV typically last up to 30 minutes. This finding may be related to the consistency of having the same telehealth nurse for each VNV, which avoided re-explaining their course of illness and allowed for additional time to thoroughly review and educate participants about effectively managing their chronic condition. This finding is similar to conclusions drawn by Russell, Rosati, Rosenfeld, and Marren (2011) suggesting that consistent use of nursing personnel in HHC visits was linked to improved patient outcomes. Further, the VNV offered scheduling flexibility that is not always available with in-person visits (Gorodeski et al., 2020).
Overall, participants were satisfied using the VNV to supplement their in-person HHC visits. All participants agreed or strongly agreed being satisfied with seeing and speaking to their telehealth nurse. Based on qualitative data, the consistency of the telehealth nurses appears to be the basis of their satisfaction, as they enjoyed connecting with them on their smartphone or tablet. Most participants stated they would recommend the VNV to other HF patients. Although participants expressed overall satisfaction with the VNV service, some participants did report concerns about the lack of physical, hands-on assessment that is typically completed during in-person visits. Despite this limitation in virtual care delivery, participants were satisfied with the VNV service and suggested continued use as a supplement to their plan of care.
Limitations
Several limitations were present in this study. Biases may have been present in our study related to lack of racial diversity, socioeconomic factors, caregiver involvement needed to operate the hardware and software, and self-selection to participate. Further, this study was a pilot and therefore had a relatively small sample. The VNV was deployed in the older adult/elderly HF population at risk for rehospitalization; thus, potentially limiting the generalizability of our findings to other patient populations of varying ages receiving virtual home care services. Only Zoom technology was used to virtually connect with participants during their VNV, therefore, our findings are limited to this technology. Using a different video-conference platform may result in different outcomes.
Conclusion
VNVs present a promising new approach for remote patient care requiring additional research to maximize its functionality and effectiveness. In our study, HF participants identified facilitators and challenges to using Zoom technology during their VNV. Although participants were satisfied overall with their VNV experience, further refinement of this service is needed. This virtual care approach provided telehealth nurses with the opportunity to provide high quality care without the possibility of a potential COVID-19 exposure. Future studies should include family caregivers’ perspectives, especially family members caring for the elderly population, as they are not digital natives. This pandemic has shifted the caring burden to them as a result of the sudden decrease in outside visitors and caregivers. Virtual visits may provide reassurance and confidence to caregivers that they are adequately caring for their loved ones (Chang, Lee, & Mills, 2017).
Acknowledgments
ChristianaCare HomeHealth Leadership team: Ann Painter, MSN, RN; Rita Elentrio, MSN, RN; Lori Davis-Palmer, MSN, RN, COS-C; Leslie Kaczmarczyk, RN, BS, COS-C
Funding
This work was supported by the Delaware Accelerating Clinical and Translation Research (ACCEL), and Institutional Development Aware (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number U54-GM104941, with additional support from the State of Delaware.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- American Heart Association (AHA). (2020). Causes and risks for heart failure. Retrieved from https://www.heart.org/en/health-topics/heart-failure/causes-and-risks-for-heart-failure
- Bauce K, Fahs DB, Batten J, & Whittemore R (2018). Videoconferencing for management of heart failure: An integrative review. Journal of Gerontological Nursing, 44(4), 45–52. doi: 10.3928/00989134-20180207-01 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Morbidity and Mortality Weekly Report: MMWR. (2020, September). Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement — United States, March 1–May 31, 2020. Retrieved from https://www.cdc.gov/mmwr/volumes/69/wr/mm6935a2.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CP, Lee TT, & Mills ME (2017). Experience of home telehealth technology in older patients with diabetes. CIN, 35(10), 530–537. doi: 10.1097/CIN.0000000000000341 [DOI] [PubMed] [Google Scholar]
- Creswell JW, & Plano Clark VL (2018). Designing and conducting mixed methods research (3rd ed.). Thousand Oaks, CA: SAGE. [Google Scholar]
- Delello JA, & McWhorter RR (2015). Reducing the digital divide: Connecting older adults to iPad technology. Journal of Gerontology, 36(1), 328. doi: 10.1177/0733464815589985 [DOI] [PubMed] [Google Scholar]
- Emory Healthcare. (2019). Heart failure statistics. Retrieved from https://www.emoryhealthcare.org/heart-vascular/wellness/heart-failure-statistics.html
- Gorodeski EZ, Goyal P, Cox ZL, Thibodeau JT, Reay RE, Rasmusson K, … Starling RC (2020). Virtual visits for care of patients with heart failure in the era of COVID-19: A statement from the heart failure society of America. Journal of Cardiac Failure, 26(6), 448–456. doi: 10.1016/j.cardfail.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang KTL, Lu TJ, Alizadeh F, & Mostaghimi A (2016). Homebound patients’ perspectives on technology and telemedicine: A qualitative analysis. Home Health Care Services Quarterly, 35(3–4), 172–181. doi: 10.1080/01621424.2016.1264341 [DOI] [PubMed] [Google Scholar]
- Idris S, Degheim G, Ghalayini W, Larsen TR, Nejad D, & David S (2015). Home telemedicine in heart failure: A pilot study of integrated telemonitoring and virtual provider appointments. Reviews in Cardiovascular Medicine, 16(2), 156–162. [DOI] [PubMed] [Google Scholar]
- Jones CD, Bowles KH, Richard A, Boxer RS, & Masoudi FA (2017, May). High-value home health care for patients with heart failure. Circulation: Cardiovascular Quality and Outcomes, 5(10). doi: 10.1161/CIRCOUTCOMES.117.003676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell UA, Chebli PG, Ruggiero L, & Muramatsu N (2019). The digital divide in health-related technology use: The significance of race/ethnicity. The Gerontologist, 59(1), 6–14. doi: 10.1093/geront/gny138 [DOI] [PubMed] [Google Scholar]
- Nouri S, Khoong EC, Lyles CR, & Karliner L (2020, May). Addressing equity in telemedicine for chronic disease management during the COVID-19 pandemic. Retrieved from https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123
- Office of the National Coordinator for Health Information Technology (ONC). (2019). What is telehealth? How is telehealth different from telemedicine? Retrieved from https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine
- Ong M, Roman PS, Edgington S, Aronow HU, Auerbach AD, Black JT, … Fonarow G (2016). Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: The better effectiveness after transition–heart failure (BEAT-HF) randomized clinical trial. AJAMA Internal Medicine, 176(3), 310–318. doi: 10.1001/jamainternmed.2015.7712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM (2003). Diffusion of innovations (5th ed.). New York: Free Press. [Google Scholar]
- Russell D, Rosati R, Rosenfeld P, & Marren J (2011). Continuity in home health care: Is consistency in nursing personnel associated with better patient outcomes? Journal for Healthcare Quality, 33(6), 33–39. doi: 10.1111/j.1945-1474.2011.00131.x [DOI] [PubMed] [Google Scholar]
- U.S. Health and Human Services [HHS]. (2020). System usability scale (SUS). Retrieved from https://www.usability.gov/how-to-and-tools/methods/system-usability-scale.html
- Urbich M, Globe G, Pantiri K, Heisen M, Bennison C, Wirtz H, & DiTanna GL (2020). A systematic review of medical costs associated with heart failure in the USA (2014–2020). PharmacoEconomics, 38(11), 1219–1236. doi: 10.1007/s40273-020-00952-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2020a). Coronavirus. Retrieved from https://www.who.int/health-topics/coronavirus#tab=tab_1
- World Health Organization (WHO). (2020b). Archived: WHO COVID-19 timeline. Retrieved from https://www.who.int/news/item/27-04-2020-who-timeline—covid-19
- Zoom. (2020, July). Video conferencing, web conferencing, webinars, screen sharing. Retrieved from https://zoom.us/meetings


