Abstract
Degenerative disorders of the Achilles tendon are common, affecting up to 18% of the adult population. A thorough evaluation including a focused history, physical examination, and diagnostic studies helps in choosing the appropriate treatment. Initial treatment is usually nonoperative, consisting of activity modification, bracing, and physical therapy. Patents who fail nonoperative management may be treated operatively with a wide range of procedures from endoscopic surgery to open debridement and tendon transfer. Understanding a patient’s expectations and educating patients about potential treatments and their outcomes enables informed collaborative decision making. This article will review the evaluation and management Achilles tendinopathy and associated disorders.
Keywords: tendon disorders, Achilles, tendon, tendinosis, tendonitis, Haglund, chronic
Introduction
Disorders of the Achilles tendon affect a substantial portion of the population with an annual incidence of 6% to 18% in the United States. 9,28,34 Research in recent years has increased, with the number of PubMed searchable articles on the topic increasing 5- to 8-fold in the last 15 years (21 in 2000 vs 147 in 2016). Although Achilles tendonitis or tendinopathy occur commonly in the middle-aged (45-65 years old) weekend warrior, this problem can affect any age group. 28 Patients will present with a variety of symptoms involving the posterior heel and will have a range of clinical morbidity from acute, mild, intermittent heel pain to rupture of the Achilles tendon. This review will focus on the evaluation as well as nonoperative and operative treatment of tendinopathy of the Achilles tendon.
Achilles Tendinopathy
Despite the pervasive use of the term tendinitis, there is a lack of histologic evidence of inflammation taken from intraoperative specimens. 18 The term tendinopathy is a more accurate descriptor. 36 Achilles tendinopathy encompasses a wide array of symptoms, including pain, swelling, and impaired performance. 49 This disease process can be separated into 3 categories, based on anatomy and affected structures: peritendinitis meaning inflammation isolated to the peritendinous sheath; peritendinitis with tendinopathy, encompassing intrasubstance changes of the tendon with inflammation of the peritenon; isolated tendinopathy with no peritenon inflammation. 52 Of the 3 disease processes, peritendinitis has the best prognosis and is usually successfully treated with nonoperative measures. 52 Conversely, isolated tendinopathy is the most likely to progress to surgical intervention. 13
The chronicity of the tendinopathy can be defined as acute (symptom duration ≤2 weeks), subacute (symptom duration between 3 and 6 weeks), and chronic (symptom duration ≥6 weeks). 52,63 It is also possible to further describe Achilles pathology using specific anatomic location to more accurately identify the source of the posterior heel pain, such as insertional versus midsubstance, using location of pain as the distinguishing factor. 36
Evaluation
Patients often report an insidious onset of symptoms, and there is often a delay in seeking medical care. It is important to elicit a detailed history of the disease, including types of activities that cause symptoms, intensity of activity, duration of symptoms, and location of pain. Use of fluoroquinolones and statins should be noted as these are known to cause tendinopathy. 28 It is also important to note if a patient is diabetic, on chronic corticosteroids, or a nicotine user, as these factors are associated with delayed wound healing following Achilles tendon repair and may impair tendon healing as well. 5,7 These conditions are also known to be associated with ruptures, but not necessarily with tendinosis, of the Achilles. 5,45,62 Lastly, the use of inhaled high-dose corticosteroids has been shown in case reports to increase patient susceptibility to Achilles tendonitis in patients undergoing treatment for long-standing chronic obstructive pulmonary disease. 59
Physical Examination
A well-executed physical examination is highly specific for Achilles tendinosis. The examination should include evaluation of areas of tendon enlargement at the midsubstance or insertion, presence of muscular atrophy, and sensation (presence of neuropathy may impact decisions regarding surgery). A standing examination allows for assessment of alignment of the foot and ankle in the functional position, noting calcaneal varus or valgus and allowing comparison to the contralateral side. It is also easier to assess atrophy in the standing position. Swelling, crepitus, erythema, warmth, and palpable tendon nodules or defects should be noted. Palpation of the calcaneal tuberosity, and a calcaneal squeeze test can help differentiate insertional Achilles tendinopathy from a calcaneal stress reaction. Positive dynamic tests include pain with forced dorsiflexion, resisted plantarflexion, and single heel raise. The knee should be examined, paying special attention to muscular contractures that may affect gait. For example, quadriceps weakness can lead to the development of an Achilles contracture and tendinopathy secondary to knee flexion contracture. Additionally, it is important to note biomechanical factors that may be associated with tendinopathy, including leg length discrepancy, planovalgus, cavovarus deformity, and ankle instability. 35,66
Examination of the Achilles may reveal thickening at the tendon insertion (bursitis), fusiform thickening (noninsertional tendinopathy), or a prominence at the calcaneal tuberosity (insertional tendinopathy). Patients may have intratendinous nodules or thickening that is painful with ankle motion (painful arc sign). 54 Patients with insertional tendinopathy will have tenderness at the calcaneal tuberosity while those with noninsertional tendinopathy will have tenderness about 3 to 4 cm proximal to the insertion of the tendon in the area of fusiform enlargement of the tendon. 66 Patients with peritendinitis exhibit focal tenderness independent of ankle position, whereas patients with tendinopathy have pain that migrates with movement of the ankle. 66 The patient may have pain with range of motion and/or limited dorsiflexion. Achilles contracture should be differentiated from gastrocnemius contracture, via the Silversköld test, as this helps to guide both nonsurgical and surgical treatment.
Imaging
Radiographs of the hindfoot are important in the initial evaluation of Achilles tendinopathy. X-rays can reveal calcific changes of the tendon or a Haglund deformity (a prominence of the posterior superior calcaneal tuberosity) in up to 60% of cases. 28 Haglund deformities (Figure 1) apply pressure on the retrocalcaneal bursa or on the tendon, causing irritation. They can be quantified radiographically by deformity height and mean deformity peak angle. 9 None of the radiographic parameters used to describe a Haglund deformity (eg, Fowler’s angle, parallel pitch line) have shown significant clinical correlation, and thus are not critical for clinical practice. 8,29
Figure 1.

Lateral view of an ankle radiograph showing a pronounced Haglund deformity with calcification of the distal Achilles at its insertion point on the calcaneus.
Supplemental imaging such as magnetic resonance imaging (MRI) or ultrasonography can be helpful in differentiating ambiguous presentations and in determining the extent and location of chronic tendinopathy (Figure 2). 54 Ultrasonography demonstrates different patterns in acute and chronic tendinopathy (Figure 3). In the acute setting, fluid can be seen surrounding the tendon (Figure 4). 54 Whereas, in chronic tendinopathy, tendinous adhesions are seen as thickening of the paratenon with poorly defined borders. 54 Unlike normal tendon, which demonstrates little signal on MRI, increased signal within the tendon represents lesions associated with edema or hemorrhage (Figure 5, Figure 6). 32 MRI studies exhibiting partial tears can be differentiated from tendinopathy based on sagittal diameter. Partial tears have a diameter 10 to 18 mm larger than tendinopathy. 1
Figure 2.

Sagittal image from a T1 series magnetic resonance image demonstrating insertional Achilles tendinosis. Please note the interstitial tearing shown by increased signal in the tendon, Haglund deformity that impinges on the tendon, enthesopathy, and calcification at insertion of the tendon into the calcaneus.
Figure 3.
Cross-sectional ultrasonograph showing Achilles tendon with tendinosis and partial tear. Note the hyperechoic paratenon and irregular orientation of the fibers of the tendon, demonstrated by fusiform thickening and loss of the normal architecture.
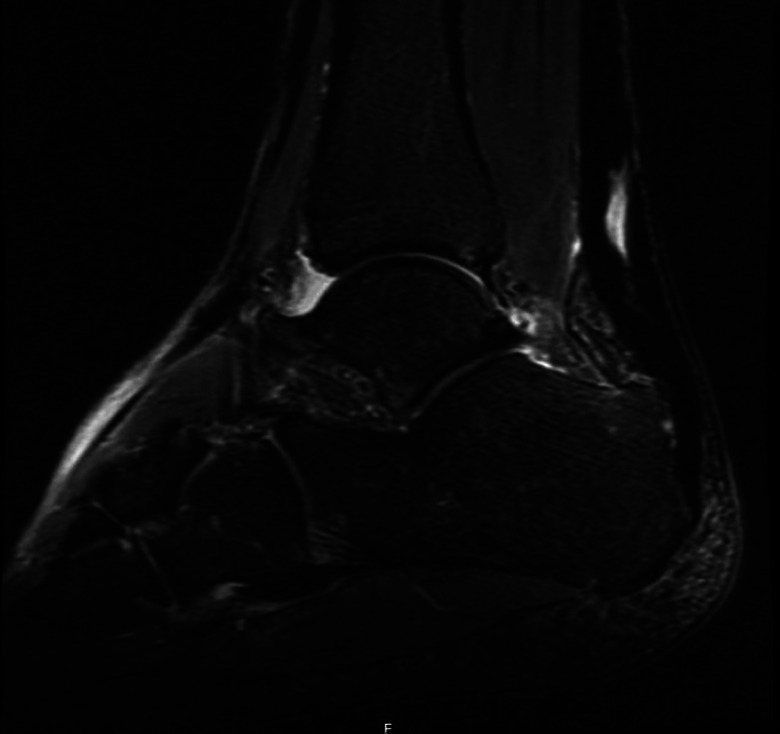
Figure 4.

Sagittal image from a T2 series magnetic resonance image demonstrating insertional Achilles tendinosis. Note the interstitial tearing of tendon, bone edema in Haglund deformity, and edema within Kager fat pad. In addition to the damage within the tendon, the edema in surrounding structures gives the physician an indication of chronic (>3-6 months) inflammation present in the area.
Figure 5.

Sagittal image from a T1 series magnetic resonance image demonstrating midsubstance Achilles tendinosis. There is also a significant Haglund deformity of the calcaneus noted with direct impingement on the Achilles tendon. Kager fat pad is appreciated directly anterior to the tendon.
Figure 6.
Sagittal image from a T2 series magnetic resonance image demonstrating midsubstance Achilles tendinosis. There is also an appreciable inflammation of Kager fat pad noted directly anterior to the tendon. Additionally, there is the Haglund deformity noted in Figure 5, with edematous changes noted in the bone about the distal Achilles tendon just proximal to its insertion.
Specimens demonstrating micropathologic chronic tendinopathy have been analyzed using ultrasonography and MRI, and it was found that MRI was positive in 96% of cases whereas ultrasonography was positive in only 78% of cases. 10,18,19 MRI and ultrasonography can both provide excellent information; however, the sensitivities of these modalities may not exactly correlate with symptoms or physical examination as there are overlapping imaging appearances between “normal” and “abnormal.” 31 MRI may also provide insight into the percentage of tendon thickness involved and reactive changes in the calcaneus or the anterior Achilles bursa, which can aid in surgical planning. 18,19 Presence of inflammation isolated to the anterior bursa is a potential indication for endoscopic bursal debridement. 19
Nonoperative Treatment
Initial Treatment
Initial treatment of Achilles tendinopathy consists of nonsteroidal anti-inflammatory drugs (NSAIDs), rest, ice, and either immobilization or physical therapy depending on the amount of pain and duration of symptoms. For patients with more severe tenderness and pain, a period of immobilization is indicated prior to physical therapy interventions. Once the acute pain is under control, therapy may begin. The therapy may be either self-directed or performed under the guidance of a physical therapist. Patients should be counseled to modify their exercise and daily activities during the treatment phase to avoid further damage to the tendon.
Eccentric therapy has been shown effective for midsubstance tendinopathy. 61 Microtrauma of the tendon occurs with eccentric loading secondary to high-frequency oscillations. 60,61 This can be attributed to the increased force transmitted through the tendon with eccentric loading. 60 Eccentric rehabilitation promotes remodeling of the tendon, which eventually allows the tendon to withstand the type of loads that initially caused the damage. 60 A daily home stretching regimen in conjunction with supervised physical therapy has been shown to cause statistically significant improvement in upwards of 88% of patients. 3,35 Recent literature has also shown positive results with heavy, slow resistance protocols. 3 Patients should be trained to stretch with the foot internally rotated to lock the transverse tarsal joint in order to ensure that the gastrocnemius-soleus complex is engaged as opposed to having motion occurring through the mid- and hindfoot.
Physical therapy treatment may be supplemented by an in-shoe heel lift or cushion to alleviate some of the mechanical strain on the Achilles. Some patients find symptomatic relief with commercial compression supports, some of which have gel pads to cushion the Achilles tendon. When patients are in severe pain, or have failed heel lifts previously, it is necessary to relieve the stress on the tendon for a period of time to allow for pain relief and better healing potential before formal therapy is initiated. This is often accomplished using immobilization with a controlled ankle motion (CAM) boot, but it is our practice to utilize a brace such as a custom-molded ankle-foot orthosis (MAFO) (Figure 7) to immobilize the ankle joint. This removes the repetitive stress associated with contraction of the gastrocnemius-soleus complex but is much more functional and better tolerated than the CAM boot as it minimally affects leg length and causes less knee, hip, and back discomfort while allowing patients to wear more normal footwear. The MAFO is also an effective definitive treatment in patients who do not wish to undergo operative intervention for either health or personal reasons. 27 Cost is a factor in choice of orthotic. A CAM (cost $257.85; Komfort & Kare, Philadelphia, PA) is significantly less expensive than a MAFO ($863.51, Komfort & Kare). Despite the increased cost, a MAFO is significantly more durable and can be used with a regular shoe without creating a leg length discrepancy concern. A CAM boot causes a 1- to 3-cm leg length difference, although this can be offset by using a shoe balancer ($24.69, Amazon.com).
Figure 7.

Custom Molded Ankle Foot Orthosis (MAFO).
Minimally Invasive Treatment
If the initial nonoperative treatment fails, the patient can be offered additional therapeutic options prior to surgical intervention. These can include shock-wave therapy, injections, and topical treatments.
Low-energy shock-wave therapy is a treatment modality which has moderate support in the literature. Shock-wave therapy appears to stimulate soft tissue healing and inhibits pain receptors. Results are somewhat controversial. It is generally agreed that low-energy shock-wave therapy alone does not appear beneficial; however, when added to eccentric stretching, it demonstrates positive results. 61 A randomized controlled study compared addition of low-energy shock-wave therapy to eccentric exercise versus eccentric exercise alone and found improved outcomes with the combination therapy. 56
Platelet-rich plasma (PRP) injections are becoming more common in the treatment of chronic tendinopathies, with some favorable evidence. 22 Ultrasonography-guided PRP injections have shown pain relief in 88% patients after 2 months; however, at 12 months, only 44% continued to report complete pain resolution. 30 Another study with a 4½-year follow-up had 83% return to sport and 93% were satisfied with the results and which remained stable at final follow-up. 13 However, they discovered that delay in treatment resulted in slower return to sport. 16
Corticosteroid injections (CSI) are generally contraindicated in the treatment of chronic Achilles tendinopathy because of the high rate of tendon rupture (occurring in 8.4% of cases). Other common documented side effects include postinjection pain, subcutaneous fat and skin atrophy, and skin pigmentation changes. 21,25,26,46,58 It has been suggested that the volume and mode of delivery are more important factors than the steroid itself. 39 It may be safer to deliver steroids via iontophoresis than direct injection into the tendon sheath, as that may not significantly alter the structural or biomechanical characteristics of the tendon. 39
Topical glyceryl trinitrate has been investigated for treatment of chronic non-insertional Achilles tendinopathy with favorable results. A randomized, double-blind, placebo-controlled study using continuous topical glyceryl trinitrate through a transdermal patch found a significant reduction in pain and improved functional outcomes compared with physical therapy alone. 51
Use of brisement to treat peritendinitis in the younger, more active patient with palpable or audible crepitus on ambulation has been documented in literature. The brisement procedure involves injecting slowly into the peritenon sheath approximately 5 to 10 mL of a diluted local anesthetic, such as lidocaine, or saline solution under pressure. If available, ultrasonographic guidance can be used to ensure correct and proper needle placement. Two or 3 injections can reduce symptoms approximately half of the time. Multiple published studies have described brisement’s clinical efficacy, but there are not any comparative studies currently available in literature looking at brisement’s efficacy compared to other conservative options. 6,38 It is important to note that only a local anesthetic be used and not a corticosteroid/anesthetic mixture to prevent unintended damage to the tendon itself, which could potentially result in a rupture. 24
Operative Treatment
Operative treatment is indicated when 6 months of nonoperative measures have failed to improve symptoms. The amount of tendon, bone, and bursal involvement determined from imaging can assist in preoperative planning. In patients with contracture, a gastrocnemius recession may be considered. For active patients with noninsertional pathology, simple debridement may be augmented with PRP or other biologics. 16,17 For patients with greater involvement, more aggressive debridement and potentially tendon transfer is indicated. Calcific changes at the tendon insertion and Haglund deformity should be removed at the time of surgery. This may require complete detachment of the Achilles, followed by subsequent reattachment. 33 In select subsets of the population, less invasive surgical options including endoscopic calcaneoplasty and calcaneal osteotomies may be appropriate.
Gastrocnemius Recession
Gastrocnemius recession has been explored with favorable outcomes and minimal complication rates for treatment of noninsertional Achilles tendinopathy resistant to conservative measures. 11 It has also been examined for cases of insertional tendinosis, but the results are less favorable. 64 Patients who underwent the procedure reported significant improvements in their pain and functional status with activities of daily living, but did show slight power and endurance deficits in the surgical leg. 11,42 -44 Recent literature has examined both the open Strayer procedure and proximal medial gastrocnemius recession, and both techniques demonstrated excellent patient-reported outcomes. 23,64
Achilles Tendon Debridement and Repair
Debridement of pathologic tissue is an essential element of surgical treatment. In noninsertional pathology, this debridement may be done in an intralesional fashion (Figure 8) followed by local tendon repair. When there is significant pathology at the calcaneal insertional site of the Achilles tendons, it may be necessary to detach a portion or even the entire tendon from the calcaneus to remove all diseased tendon and calcified prominences. Several authors have described the utilization of suture anchor fixation to assist with reattachment of the tendon to its native bed. 2,15,55 The suture anchor provides strong biomechanical fixation, especially when applied in a double-row technique that allows for tendon compression to bone. 2 Good to excellent patient-reported outcomes following double-row fixation techniques for patients with insertional Achilles tendinosis in 2 separate case series with more than 40 patients. 15,55
Figure 8.
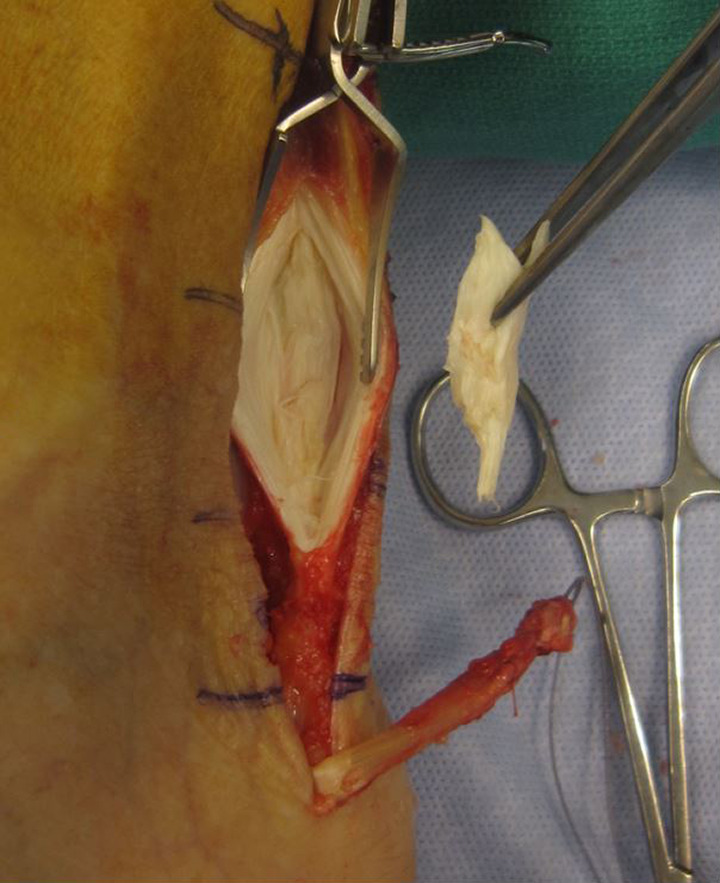
Intraoperative image showing excised portion of pathologic Achilles tendon. Note the yellow discoloration. Additionally, the long harvest FHL, which has already been passed through a bone tunnel in the calcaneus (not visible) is seen at the bottom of the incision with the blue suture attached to it.
Flexor Hallucis Longus Tendon Transfer
An FHL transfer is often incorporated as part of the surgical treatment (Figure 9) if more than 50% of the tendon is thickened and damaged, although this amount is based solely on expert opinion and not scientific evaluation of tendon strength. 54 FHL tendon transfer and incorporation can be used for both insertional and noninsertional tendinosis that has failed to improve with conservative measures after 6 or more months.
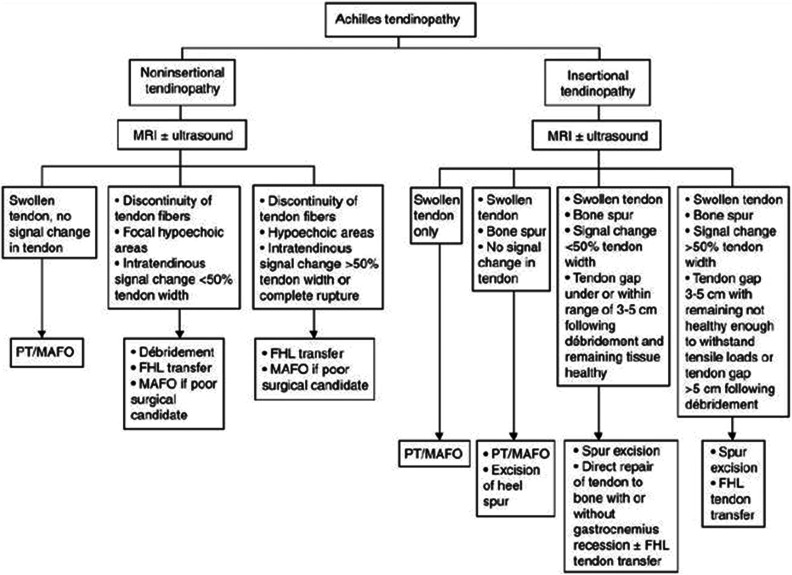
Figure 9.
Achilles tendinopathy treatment algorithm (courtesy of Wapner, KL). FHL, flexor hallucis longus tendon; MAFO, molded ankle-foot orthosis; MRI, magnetic resonance imaging; PT, physical therapy.
When choosing to perform an FHL transfer, the decision must be made between short and long harvest. During a short harvest, the tendon is transected at the posterior talus, and using the same incision, the tendon is secured to the calcaneus using either a bio-interference screw or suture anchor(s). 53 A long FHL harvest involves approaching the distal tendon through a separate incision at the medial midfoot (Figure 10) and securing the tendon through a bone tunnel and retrograde Pulvertaft weave and suture fixation.
Figure 10.
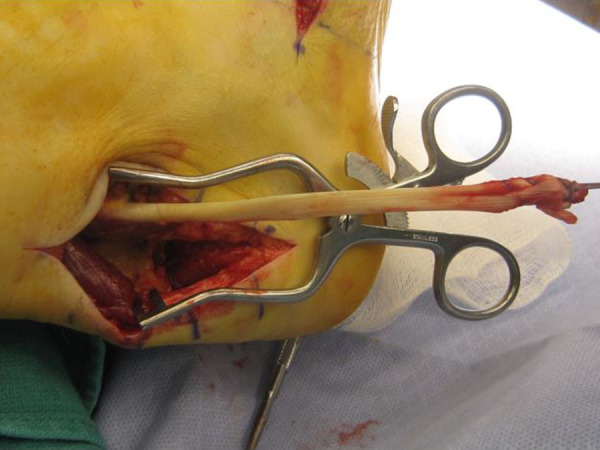
Intraoperative of a long FHL harvest as viewed from the posterior incision (small portion of the midfoot incision is visible at the top of the image). This is done in preparation for an FHL transfer in the setting of chronic Achilles tendinosis.
Both techniques have been reported to be equal from a strength and stability standpoint in cadaveric studies. 18 In either technique, some great toe flexion is maintained by the interconnections between the FHL and flexor digitorum longus (FDL) at the master knot of Henry and is supplemented by the flexor hallucis brevis (FHB). Regardless of method used, patients may report great toe flexion weakness and decreased push-off strength during gait. When performing a long harvest, we recommend anastomosing the distal FHL tendon to the FDL tendon in the midfoot to allow maintenance of great toe flexion motion and strength. Failure to do so may result in deficit of great toe interphalangeal joint flexion strength. 67
The decision to perform short or long harvest is often dictated by surgeon preference. One way of approaching this decision is to consider the extent of damaged tissue, and if it is felt that the Achilles would benefit from incorporation of healthy tendon tissue then perform a long harvest, but if the goal is primarily mechanical assist and the degenerative change is limited at the very distal insertion then a short harvest may be appropriate. One rationale is that the disease process has revealed the tendon is failing under normal physiologic load and tendon transfer reduces the load borne by the Achilles, making it less susceptible to recurrent failure. Current literature does not provide definitive guidance on the usage of long vs short harvest technique, so surgeon comfort and preference should be the driving factor.
Additional Considerations
A potential disadvantage of FHL tendon augmentation is loss of great toe plantarflexion force; however, the decreased force does not appear to significantly affect function. 24,40 It is for this reason we make a practice of performing the FHL to FDL anastomosis during a long FHL harvest to maintain great toe flexion strength. It is also our practice is to perform an open tendon debridement with possible FHL augmentation, depending on the extent of tendon involvement identified at the time of surgery in younger patients. If diseased tendon is noted to be greater than 50% thickness in the young patient, an FHL transfer is performed. We perform FHL transfer on most patients older than 55 years of age. A long or short FHL harvest may be used depending on physician preference, which allows for continued in-phase pull of the FHL. 67
Endoscopic Calcaneoplasty
Another surgical technique to consider for patients desiring a minimally invasive option or where concerns about wound healing or incisional pain may be an issue is endoscopy. Endoscopic techniques for both debridement of the Achilles tendon and paratenon and for removal of Haglund deformities have been described. Two case series resulted in no wound issues and high patient function and satisfaction. 64,65 It is also possible to use a percutaneous technique to apply a suture anchor in the setting of bony resection to mitigate risk of iatrogenic Achilles rupture. 64 Similarly successful results with endoscopic paratenon debridement and release of the plantaris tendon have been noted. In a series of 45 Achilles debridements, good to excellent results and function were reported by all patients and the only complication noted was repeat surgery for return of symptoms, which subsequently resolved. 47
Calcaneal Osteotomies
In higher demand patients who would be more cognizant of a residual FHL deficit, such as athletes, an isolated calcaneal osteotomy may be a successful operative treatment. Using a lateral approach, a dorsal closing wedge osteotomy of the calcaneus using 2 staples for fixation can alleviate adequate tension on the tendon and allow return to competition without noticeable deficits. The procedure decreases tension on the tendon and utilizes bony healing. A study reviewing 52 athletes (64 feet) who had failed 6 months of conservative treatment found that 50 of 52 reported excellent (38) or good (12) results, with the other 2 reporting fair outcomes over 3 years of follow-up. Patients were also able to return to athletics sooner. 20
Surgical Approach and Closure
The surgical approach may be performed with the patient prone or supine and utilizes an incision either directly posterior or medial of the midline posteriorly. Placing the incision medial to the posterior midline serves to minimize risk of injury to the sural nerve and creates a scar that is not in contact with the posterior aspect of footwear. 14 A direct midline incision may also be employed as it may make tendon visualization easier, and it better aligns with the posterior ankle angiosomes, but it has been associated with a painful scar that can be irritated by footwear. 4,37 The peritenon is incised and is often scarred to the underlying Achilles tendon. Depending on the location, the tendon may be directly debrided or split longitudinally to access more central tears or degenerative change. In the setting of long-standing Achilles tendinopathy, the tendon may appear thick, soft, and yellowish. 54
A helpful technique to assist with closure of the posterior investing tissues is to perform a longitudinal incision in the deep anterior portion of the fascia to allow for accommodation of excess tissue within the tendon sheath. The increased sheath volume allows for the accommodation of the increased tissue mass and assists with a tension-free closure. Care must be taken to not penetrate the deep sheath too far, as the neurovascular bundle lies deep in this structure. The authors’ preferred technique is to place all intratendinous surgical knots on the anterior portion of the tendon to minimize skin irritation and prevent breakdown.
Patient Age Considerations
Older patients have less consistent results with operative treatment compared with younger patients. This discrepancy may be secondary to reduced blood flow and healing capacity or more severe tendinopathy, or less capacity for rehabilitation. 58,67 In patients younger than 50 years, Achilles tendon decompression and debridement alone is appropriate. 40,58,67 There was noted good to excellent results in 70% to 90% of patients younger than 50 years. 41 Conversely, longer persistent pain and slower return to function was noted in the population older than 50 years. 41 Younger patients typically have more focal involvement, which allows for less dissection and tendon excision, and in turn permits for more aggressive rehabilitation and a better ultimate outcome. 41 Patients older than 50 years may benefit from tendon augmentation in addition to debridement and decompression. 40,41,67 There are reported success rates of 86% in patients older than 50 years with FHL augmentation. 40 Patients older than 55 years will eventually obtain good to excellent results with an FHL augmentation, but experience both longer persistent pain and longer return to function. 12 It has been shown that augmentation improves overall patient results when compared to debridement alone. Satisfaction rates increased to 87% with the addition of an FHL transfer in patients older than 50 years, and the addition of the FHL transfer improved plantar flexion strength. 12,24,40
Postoperative Care
There is variation in recommendations for postoperative management for Achilles tendinopathy. Protocols vary for range of motion, weight bearing, and immobilization. Most recommend range of motion and stretching to begin postoperative week 2, with gradual return to sports once strength has returned. 49
The authors’ preferred postoperative protocol includes non–weight bearing immediately postoperatively in a well-padded splint in resting plantar flexion. Care is taken not to apply additional dorsiflexion, aside from that which occurs by gravity, to the ankle while the splint hardens. At the 2-week follow-up, sutures are removed, and patients are either casted for an additional 2 weeks (if there are concerns about tissue integrity) or transitioned to a CAM boot with heel lifts and early motion allowed. Physical therapy is initiated with a protocol similar to the Willits protocol for Achilles tendon rupture repair. 68 This consists of graduated weight bearing in the boot with heel lifts beginning at week 4 postoperatively and full weight-bearing around 6 weeks. At 10 to 12 weeks, transition to a sneaker is allowed with a heel lift as needed. Therapy is focused on range of motion initially followed by progressive strengthening. Return to sport without restrictions is usually around 6 months as long as the patient has achieved adequate strength and flexibility similar to the contralateral side. Patients are counseled preoperatively that full recovery may take up to a year or more.
Complications
Studies examining operative treatment in patients with chronic Achilles tendinopathy found 11% to 19% developed complication rates. 48,50 Major complications included skin edge necrosis and wound or infection issues, partial rupture, and deep vein thrombosis. Careful trimming of adhesions and preserving as much of the peritenon as possible can mitigate risk. 48,50 Suture reaction and delayed granuloma formation are also a concern, noted as high as 2.7%. To counteract this, we recommended using nonabsorbable suture for deep repair as the lack of fat to hydrolyze absorbable sutures likely play a role in increased reaction. 57 Patients who underwent tendon augmentation in addition to decompression and debridement did not exhibit a statistically significant rate of increased complications. 24,40
Conclusion
Achilles tendinopathy is a common condition. Accurate diagnosis is essential to guide the choice of treatment. Conservative treatment is almost always indicated at initial presentation. This may involve a period of immobilization with a MAFO or CAM walker boot followed by physical therapy. Conservative measures are generally employed for a minimum of 6 months before surgical intervention is considered. Supplemental imaging in the form of ultrasonography or MRI may assist the surgeon in creating an operative plan. The principal factors to consider are the duration of symptoms and extent and location of tendon involvement. Surgical treatment generally involves tendon and bony debridement with consideration of tendon transfer. Patient education on appropriate expectations about duration of recovery, and the usually gradual nature of symptom improvement, are crucial to successful recovery.
Supplemental Material
Supplemental Material, FAO838294-ICMJE for Achilles Tendinopathy and Associated Disorders by Adam Ferguson, Christy Christophersen, Osama Elattar and Daniel C. Farber in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Daniel C. Farber, MD,  https://orcid.org/0000-0002-4999-7038
https://orcid.org/0000-0002-4999-7038
References
- 1. Åström M, Gentz CF, Westlin N, et al. Imaging in chronic Achilles tendinopathy: a comparison of ultrasonography, magnetic resonance imaging and surgical findings in 27 histologically verified cases. Skeletal Radiol. 1996;25(7):615–620. [DOI] [PubMed] [Google Scholar]
- 2. Beitzel K, Mazzocca AD, Obopilwe E, et al. Biomechanical properties of double- and single-row suture anchor repair for surgical treatment of insertional Achilles tendinopathy. Am J Sports Med. 2013;41(7):1642–1648. [DOI] [PubMed] [Google Scholar]
- 3. Beyer R, Kongsgaard M, Hougs Kjær B, et al. Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy: a randomized controlled trial. Am J Sports Med. 2015;43(7):1704–1711. [DOI] [PubMed] [Google Scholar]
- 4. Bosanquet DC, Glasbey JD, Williams IM. Systematic review and meta-analysis of direct versus indirect angiosomal revascularisation of infrapopliteal arteries. Eur J Vasc Endovasc Surg. 2014;48(1):88e97. [DOI] [PubMed] [Google Scholar]
- 5. Bruggeman NB, Turner NS, Dahm DL, et al. Wound complications after open Achilles tendon repair: an analysis of risk factors. Clin Orthop Relat Res. 2004;427:63–66. [DOI] [PubMed] [Google Scholar]
- 6. Chan O, O’Dowd D, Padhiar N, et al. High volume image guided injections in chronic Achilles tendinopathy. Disabil Rehabil. 2008;30:1697–1708. [DOI] [PubMed] [Google Scholar]
- 7. Cheema AN, Newton JB, Boorman-Padgett JF, et al. Nicotine impairs intra-substance tendon healing after full thickness injury in a rat model. J Orthop Res. 2019;37(1):94–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cheng-Chang L, Yu-Min F, Yin-Chih T, et al. Angle analysis of Haglund syndrome and its relationship with osseous variations and Achilles tendon calcification. Foot Ankle Int. 2007;28(2):181–185. [DOI] [PubMed] [Google Scholar]
- 9. Clancy WG, Jr, Neidhart D, Brand RL. Achilles tendonitis in runners: a report of five cases. Am J Sports Med. 1976;4:46–57. [DOI] [PubMed] [Google Scholar]
- 10. Clanton TC. Haglund deformity and insertional Achilles tendon disease. Paper presented at: IFFAS Symposium—Achilles Tendon, September 20, 2014.
- 11. Cychosz CC, Phisitkul P, Belatti DA, Glazebrook MA, DiGiovanni CW. Gastrocnemius recession for foot and ankle conditions in adults: evidence-based recommendations. Foot Ankle Surg. 2015;21(2):77–85. [DOI] [PubMed] [Google Scholar]
- 12. Den Hartog BD. Flexor hallucis longus transfer for chronic Achilles tendinosis. Foot Ankle Int. 2003;24(3):233–237. [DOI] [PubMed] [Google Scholar]
- 13. Drakos MC, Gott M, Karnovsky SC, et al. Biomechanical analysis of suture anchor vs tenodesis screw for FHL transfer. Foot Ankle Int. 2017;38(7):797–801. [DOI] [PubMed] [Google Scholar]
- 14. Easley ME, Wiesel SW. Operative Techniques in Foot and Ankle Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2016. [Google Scholar]
- 15. Ettinger S, Razzaq R, Waizy H, et al. Operative treatment of the insertional Achilles tendinopathy through a transtendinous approach. Foot Ankle Int. 2016;37(3):288–293. [DOI] [PubMed] [Google Scholar]
- 16. Filardo G, Kon E, Di Matteo B, et al. Platelet-rich plasma injections for the treatment of refractory Achilles tendinopathy: results at 4 years. Blood Transfus. 2014;12(4):533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Filardo G, Presti ML, Kon E, Marcacci M. Nonoperative biological treatment approach for partial Achilles tendon lesion. Orthopedics. 2010;33(2):120–123. [DOI] [PubMed] [Google Scholar]
- 18. Fornage BD. Achilles tendon: US examination. Radiology. 1986;159(3):759–764. [DOI] [PubMed] [Google Scholar]
- 19. Garras DN, Raikin SM, Bhat SB, Taweel N, Karanjia H. MRI is unnecessary for diagnosing acute Achilles tendon ruptures: clinical diagnostic criteria. Clin Orthop Relat Res. 2012;470(8):2268–2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Georgiannos D, Lampridis V, Vasiliadis A, Bisbinas I. Treatment of insertional Achilles pathology with dorsal wedge calcaneal osteotomy in athletes. Foot Ankle Int. 2017;38(4):381–387. [DOI] [PubMed] [Google Scholar]
- 21. Gidumal R, Evanski P. Calcaneal osteomyelitis following steroid injection: a case report. Foot Ankle Int. 1985;6(1):44–46. [DOI] [PubMed] [Google Scholar]
- 22. Gross CE, Hsu AR, Chahal J, Holmes GB, Jr. Injectable treatments for noninsertional Achilles tendinosis: a systematic review. Foot Ankle Int. 2013;34(5):619–628. [DOI] [PubMed] [Google Scholar]
- 23. Gurdezi S, Kohls-Gatzoulis J, Solan MC. Results of proximal medial gastrocnemius release for Achilles tendinopathy. Foot Ankle Int. 2013;34(10):1364–1369. [DOI] [PubMed] [Google Scholar]
- 24. Hunt KJ, Cohen BE, Davis WH, Anderson RB, Jones CP. Surgical treatment of insertional Achilles tendinopathy with or without flexor hallucis longus tendon transfer: a prospective, randomized study. Foot Ankle Int. 2015;36(9):998–1005. [DOI] [PubMed] [Google Scholar]
- 25. Johnson E, Scranton P, Jr, Pfeffer GB. Chronic disorders of the Achilles tendon: results of conservative and surgical treatments. Foot Ankle Int. 1997;18(9):570–574. [DOI] [PubMed] [Google Scholar]
- 26. Johnson JE, Klein SE, Putnam RM. Corticosteroid injections in the treatment of foot & ankle disorders: an AOFAS survey. Foot Ankle Int. 2011;32(4):394–399. [DOI] [PubMed] [Google Scholar]
- 27. Johnson M, Alvarez RG. Nonoperative management of retrocalcaneal pain with AFO and stretching regimen. Foot Ankle Int. 2012;33(7):571–581. [DOI] [PubMed] [Google Scholar]
- 28. Kälebo P, Goksör LA, Swärd L, Peterson L. Soft-tissue radiography, computed tomography, and ultrasonography of partial Achilles tendon ruptures. Acta Radiologica. 1990;31(6):565–570. [PubMed] [Google Scholar]
- 29. Kang S, Thordarson DB, Charlton TP. Insertional Achilles tendinitis and Haglund’s deformity. Foot Ankle Int. 2012;33(6):487–491. [DOI] [PubMed] [Google Scholar]
- 30. Kaux JF, Drion P, Croisier JL, Crielaard JM. Tendinopathies and platelet-rich plasma (PRP): from pre-clinical experiments to therapeutic use. J Stem Cells Regen Med. 2015;11(1):7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Khan KM, Forster BB, Robinson J, et al. Are ultrasound and magnetic resonance imaging of value in assessment of Achilles tendon disorders? A two-year prospective study. Br J Sports Med. 2003;37(2):149–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Koblik PD, Freeman DM. Short echo time magnetic resonance imaging of tendon. Investig Radiol. 1993;28(12):1095–1100. [DOI] [PubMed] [Google Scholar]
- 33. Kolodziej P, Glisson RR, Nunley JA. Risk of avulsion of the Achilles tendon after partial excision for treatment of insertional tendonitis and Haglund’s deformity: a biomechanical study. Foot Ankle Int. 1999;20(7):433–437. [DOI] [PubMed] [Google Scholar]
- 34. Kujala UM, Sarna S, Kaprio J. Cumulative incidence of Achilles tendon rupture and tendinopathy in male former athletes. Clin J Sports Med. 2005;15(3):133–135. [DOI] [PubMed] [Google Scholar]
- 35. Li HYun, Hua YH. Achilles tendinopathy: current concepts about the basic science and clinical treatments. Biomed Res Int. 2016;2016:6492597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Maffulli N, Khan KM, Puddu G. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy. 1998;14:840–843. [DOI] [PubMed] [Google Scholar]
- 37. Maffulli N, Longo UG, Gougoulias N, Denaro V. Ipsilateral free semitendinosus tendon graft transfer for reconstruction of chronic tears of the Achilles tendon. BMC Musculoskelet Disord. 2008;9(1):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Maffulli N, Longo UG, Spiezia F, Denaro V. Minimally invasive surgery for Achilles tendon pathologies. Open Access J Sports Med. 2010;1:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Martin DF, Carlson CS, Berry J, Reboussin BA, Gordon ES, Smith BP. Effect of injected versus iontophoretic corticosteroid on the rabbit tendon. South Med J. 1999;92(6):600–608. [DOI] [PubMed] [Google Scholar]
- 40. Martin RL, Manning CM, Carcia CR, Conti SF. An outcome study of chronic Achilles tendinosis after excision of the Achilles tendon and flexor hallucis longus tendon transfer. Foot Ankle Int. 2005;26(9):691–697. [DOI] [PubMed] [Google Scholar]
- 41. McGarvey WC, Palumbo RC, Baxter DE, Leibman BD. Insertional Achilles tendinosis: surgical treatment through a central tendon splitting approach. Foot Ankle Int. 2002;23(1):19–25. [DOI] [PubMed] [Google Scholar]
- 42. Molund M, Lapinskas SR, Nilsen FA, Hvaal KH. Clinical and functional outcomes of gastrocnemius recession for chronic Achilles tendinopathy. Foot Ankle Int. 2016;37(10):1091–1097. [DOI] [PubMed] [Google Scholar]
- 43. Nawoczenski DA, Barske H, Tome J, Dawson LK, Zlotnicki JP, DiGiovanni BF. Isolated gastrocnemius recession for Achilles tendinopathy: strength and functional outcomes. J Bone Joint Surg Am. 2015;97(2):99–105. [DOI] [PubMed] [Google Scholar]
- 44. Nawoczenski DA, DiLiberto FE, Cantor MS, Tome JM, DiGiovanni BF. Ankle power and endurance outcomes following isolated gastrocnemius recession for Achilles tendinopathy. Foot Ankle Int. 2016;37(7):766–775. [DOI] [PubMed] [Google Scholar]
- 45. Newnham DM, Douglas JG, Friend JAR, et al. Achilles tendon rupture: an underrated complication of corticosteroid treatment. Thorax. 1991;46:853–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Nichols AW. Complications associated with the use of corticosteroids in the treatment of athletic injuries. Clin J Sport Med. 2005;15(5):E370. [DOI] [PubMed] [Google Scholar]
- 47. Opdam KT, Baltes TP, Zwiers R, Wiegerinck JJ, van Dijk CN. Endoscopic treatment of mid-portion Achilles tendinopathy: a retrospective case series of patient satisfaction and functional outcome at a 2- to 8-year follow-up. Arthroscopy. 2018;34(1):264–269. [DOI] [PubMed] [Google Scholar]
- 48. Paavola M, Orava S, Leppilahti J, Kannus P, Järvinen M. Chronic Achilles tendon overuse injury: complications after surgical treatment. Am J Sports Med. 2000;28(1):77–82. [DOI] [PubMed] [Google Scholar]
- 49. Paavola M, Kannus P, Järvinen TA, Khan K, Józsa L, Järvinen M. Achilles tendinopathy. J Bone Joint Surg Am. 2002;84(11):2062–2076. [DOI] [PubMed] [Google Scholar]
- 50. Paavola M, Kannus P, Orava S, Pasanen M, Järvinen M. Surgical treatment for chronic Achilles tendinopathy: a prospective seven month follow up study. Br J Sports Med. 2002;36(3):178–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Paoloni JA, Appleyard RC, Nelson J, Murrell GA. Topical glyceryl trinitrate treatment of chronic noninsertional Achilles tendinopathy: a randomized, double-blind, placebo-controlled trial. J Bone Joint Surg Am. 2004;86(5):916–922. [DOI] [PubMed] [Google Scholar]
- 52. Puddu G, Ippolito E, Postachini F. A classification of Achilles tendon disease. Am J Sports Med 1976;4(4):145–150. [DOI] [PubMed] [Google Scholar]
- 53. Ralston EL, Schmidt ER. Repair of the ruptured Achilles tendon. J Trauma. 1971;11(1):15–21. [DOI] [PubMed] [Google Scholar]
- 54. Reddy SS, Wapner KL. Surgical treatment for chronic disease and disorders of the Achilles tendon. J Am Acad Orthop Surg. 2009;17(1):3–14. [DOI] [PubMed] [Google Scholar]
- 55. Rigby RB, Cottom JM, Vora A. Early weightbearing using Achilles suture bridge technique for insertional Achilles tendinosis: a review of 43 patients. J Foot Ankle Surg. 2013;52(5):575–579. [DOI] [PubMed] [Google Scholar]
- 56. Rompe JD, Furia J, Maffulli N. Eccentric loading versus eccentric loading plus shock-wave treatment for midportion Achilles tendinopathy. Am J Sports Med. 2009;37(3):463–470. [DOI] [PubMed] [Google Scholar]
- 57. Saxena A, Maffulli N, Nguyen A, Li A. Wound complications from surgeries pertaining to the Achilles tendon: an analysis of 219 surgeries. J Am Podiatr Med Assoc. 2008;98(2):95–101. [PubMed] [Google Scholar]
- 58. Shapiro PS, Rohde RS, Froimson MI, Lash RH, Postak P, Greenwald AS. The effect of local corticosteroid or ketorolac exposure on histologic and biomechanical properties of rabbit tendon and cartilage. Hand. 2007;2(4):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Singh D, Pandit D, Doherty M. High dose inhaled corticosteroids can cause Achilles tendonitis. Respir Med CME. 2009;2:15–17. [Google Scholar]
- 60. Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res. 1986;208:65–68. [PubMed] [Google Scholar]
- 61. Sussmilch-Leitch SP, Collins NJ, Bialocerkowski AE, Warden SJ, Crossley KM. Physical therapies for Achilles tendinopathy: systematic review and meta-analysis. J Foot Ankle Res. 2012;5(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Van Der Linden PD, Sturkenboom MC, Stricker BH, et al. Increased risk of Achilles tendon rupture with quinolone antibacterial use, especially in elderly patients taking oral corticosteroids. Arch Intern Med. 2003;163(15):1801–1807. [DOI] [PubMed] [Google Scholar]
- 63. Van Dijk CN, van Sterkenburg MN. Terminology for Achilles tendon related disorders. Knee Surg Sports Traumatol Arthrosc. 2011;19:835–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Vega J, Baduell A, Malagelada F, Allmendinger J, Dalmau-Pastor M. Endoscopic Achilles tendon augmentation with suture anchors after calcaneal exostectomy in Haglund syndrome. Foot Ankle Int. 2018;39(5):551–559. [DOI] [PubMed] [Google Scholar]
- 65. Vega J, Cabestany JM, Golanó P, Pérez-Carro L. Endoscopic treatment for chronic Achilles tendinopathy. Foot Ankle Surg. 2008;14(4):204–210. [DOI] [PubMed] [Google Scholar]
- 66. Waldecker U, Hofmann G, Drewitz S. Epidemiologic investigation of 1394 feet: coincidence of hindfoot malalignment and Achilles tendon disorders. Foot Ankle Surg. 2012;18(2):119–123. [DOI] [PubMed] [Google Scholar]
- 67. Wapner KL, Pavlock GS, Hecht PJ, Naselli F, Walther R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle. 1993;14(8):443–449. [DOI] [PubMed] [Google Scholar]
- 68. Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92:2767–2775. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO838294-ICMJE for Achilles Tendinopathy and Associated Disorders by Adam Ferguson, Christy Christophersen, Osama Elattar and Daniel C. Farber in Foot & Ankle Orthopaedics