Abstract
This study analyzes global health consequences of the new coronavirus disease by focusing on the roles of normative beliefs on social distancing and country-level factors, i.e., mobility estimate and globalization index. We fitted mixed effects models to examine the associations between two outcome measures, depression and self-rated health, and their multilevel determinants using a subset of Global Behaviors and Perceptions in the COVID-19 Pandemic, an online survey consisting of more than 100,000 participants from 67 nations. Results show that both personal beliefs and general beliefs significantly predict depression and poor health. There is also a contextual effect of globalization on depression. In addition, the relationship between general beliefs and depression is stronger in countries with lower rates of mobility. With respect to poor health, the effect of general beliefs similarly varies inversely with the level of globalization. Our study indicates that one's own beliefs and the perception of others' regarding social distancing, along with contextual factors (measures of mobility and globalization), critically shape mental and physical health. Subjective and objective factors should be considered, in other words, in properly understanding the differential impact of COVID-19 across the world.
Keywords: COVID-19, Depression, Self-rated health, Social distancing, Normative beliefs
Highlights
-
•
Personal normative beliefs on social distancing positively predicts depression.
-
•
General normative beliefs positively predicts depression and poor self-rated health.
-
•
Globalization has a negative contextual effect on depression.
-
•
Mobility estimate and globalization index moderate the impact of general normative beliefs on health outcomes.
1. Introduction
Since the initial outbreak in December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), or COVID-19, has swept across every continent adversely affecting public health in just about every country (Fiorillo and Gorwood, 2020; Pfefferbaum and North, 2020; World Health Organization, 2020). Despite the indiscriminate spread of COVID-19, its impact has not been felt equally across individuals and nations (Harlem and Lynn, 2020; Mamluk and Jones, 2020; Raisi-Estabragh et al., 2020; Wright et al., 2020). Because of the government mandate on physical distancing to contain the virus, albeit in varying degrees, people everywhere have endured limited mobility and incurred psychological and emotional costs associated with self-isolation (Brooks et al., 2020; Kim and Laurence, 2020; Giallonardo et al., 2020; Tull et al., 2020; Vindegaard and Benros, 2020). A growing body of research also reveals that COVID-19 has clearly exacerbated existing inequality. The “collateral damages” of COVID-19 are in fact unevenly distributed across the globe (Cénat et al., 2020), as socially marginalized groups bear the brunt of the disease (Oxfam International, 2020; Przeworski, 2020).
In the present study, while recognizing the critical issue of the social gradient underlying the impact of COVID-19, we turn our attention to a novel topic: normative attitudes toward social distancing. How individuals personally feel and think about quarantine (stay-at-home) measures are central to understanding their physical and mental wellbeing. Studies show that lay perceptions on social distancing mandates vary across socioeconomic strata (Ölcer et al., 2020; Pederson and Favero, 2020) and that individual willingness to comply with them significantly influences levels of coronavirus-induced anxiety and stress (Williams et al., 2020). Personal beliefs concerning how one “ought to behave” in times of a highly contagious virus are certainly important. But perhaps just as important are beliefs about others' (general) normative beliefs (Fetzer et al., 2020; Jachimowicz et al., 2018; for a formal modeling approach, see Tesar, 2020). In fact, the so-called “Social Norms Approach” (Dempsey et al., 2018) has been widely applied as an intervention strategy to curb negative, as well as promote positive, health-related and other behaviors (Reynolds, 2018; for a recent review, see Legros and Cislaghi, 2020).
An interesting question is: adjusting for one's personal beliefs, how is the subjective perception of general beliefs with respect to social distancing related to one's health outcomes? In addition to addressing this question, we investigate the potential associations with two contextual or country-level measures that are shown to be critical: globalization (international flows of people, goods and services) and domestic mobility (intranational movements of citizens). Our empirical analysis is further informed by the following queries: 1) how is the country's globalization level related to health outcomes? 2) And how is the country's measure of (post-COVID-19) physical mobility or lack of social distancing associated with health outcomes? 3) Lastly, is the hypothesized connection between social distancing-related normative beliefs and (physical and mental) health moderated by these two country characteristics (border openness and human mobility)? According to a recent study based on a U.S. sample, perception that the virus was a major threat to the national economy significantly raised the level of psychological distress (Holingue et al., 2020). We complement and extend the existing scholarship by probing the role of “perception” cross-nationally in explaining differential mental and physical (self-rated) health outcomes during the current pandemic.
2. Methods
2.1. Study sample
Data are drawn from Global Behaviors and Perceptions in the COVID-19 Pandemic (hereafter “GB&P COVID-19”), which was launched globally on March 20th and continued until April 5th of 2020, by which time the vast majority (over 85%) of sampled countries with more than 1000 confirmed cases had adopted various measures to limit mobility and mandate social distancing. An overview of the study design and methodological details are described in a National Bureau of Economic Research Working Paper (Fetzer et al., 2020). Micro data files and documentations are available at an open source repository (Banik et al., 2020; https://osf.io/3sn2k/). Details on the study design and sampling procedure are available at doi:10.31234/osf.io/3kfmh. The Principal Investigators obtained exempt IRB review E-2065 from MIT (Massachusetts Institute of Technology). We apply case weights provided to convert the data to be representative of age, gender, education, and income between survey respondents and the general population in each country, based on data from the United Nations statistical agency and the Gallup World Poll. Excluding countries with less than 100 respondents and listwise deletion of cases with missing values, our initial analytic sample contains 109,922 individuals across 67 countries.
2.2. Outcome measures
There are two outcome measures: Depression and SRH (self-rated health). The former is gauged using a modified version of the Patient Health Questionnaire (PHQ-9), excluding the item concerning suicidality (Cronbach's α = 0.86), as available in the dataset. Answers are summed and standardized as z-scores, with a higher score indicating a greater level of depression. The latter is based on the standard question about personal health status originally coded on a 4-point scale. Given the skewed distribution of data, responses are dichotomized such that poor and fair categories receive the value of 1 and 0 otherwise. Statistical models presented below, therefore, estimate worse mental and physical (self-rated) health.
2.3. Main predictors
At the individual level, the main predictors concern one's own normative views on social distancing (Personal Beliefs) and subjective understanding of what others believe (General Beliefs). Personal Beliefs, ranging in value from 1 to 4, is measured based on four survey items concerning what “people in your country” should do during the current pandemic (e.g., cancel meetings, not shake others' hands). General Beliefs, on the other hand, assesses the respondents' views on “how many of 100 people in your country” would think about the same four survey items, answers to which vary from 0 to 100 (for detail, see Table 1 ). At the contextual level, Globalization Index comes from the KOF Swiss Economic Institute (Gygli et al., 2019). Mobility Estimate are based on the COVID-19 community mobility reports provided by Google (2020).
Table 1.
Descriptive statistics, variable definitions, and coding procedures.
| Mean/proportion | S.D. | Min. | Max. | |
|---|---|---|---|---|
| Outcome measures | ||||
|
Depression “How often have you been bothered by the following over the past 2 weeks?” 1. Little interest or pleasure in doing things; 2. Feeling down, depressed or hopeless; 3. Trouble falling or staying asleep; 4. Feeling tired or having little energy; 5. Poor appetite or overeating; 6. Feeling bad about yourself or that you are a failure or have let yourself or your family down; 7. Trouble concentrating on things such as reading the newspaper or watching television; 8. Moving or speaking so slowly that other people could have noticed or so fidgety or restless that you have been moving a lot more than usual (not at all = 1; several days = 2; more than half the days = 3; nearly every day = 4). Summed responses converted to z-scores with the mean of 0 and standard deviation of 1 |
0 | 1 | −1.11 | 3.63 |
|
SRH (self-rated health) “How healthy are you?” Answers dichotomized so that “poor/fair” = 1 and “good/excellent” = 0. |
20% | — | 0 | 1 |
| Individual level (L1) covariates | ||||
| Male (ref.: female) | 44% | __ | 0 | 1 |
| Age (years) | 38.91 | 13.02 | 18 | 110 |
| Partner (ref.: living alone) | 56% | __ | 0 | 1 |
| Education (total years of schooling) | 16.36 | 4.67 | 0 | 25 |
| Household Income (pre-tax monthly earnings log transformed) | 9.36 | 3.01 | 0 | 21.89 |
|
Comorbidities “Please consider the following list of health conditions: A. cardiovascular diseases; B. diabetes; C. hepatitis; D. chronic obstructive pulmonary disease; E. chronic kidney disease; F. and cancer. How many of these conditions do you have?” Dichotomized due to right-tailed skewed distribution (coded 1 if experienced at least one of the symptoms; 0 otherwise) |
14% | __ | 0 | 1 |
|
Insufficiency “Do you think the reaction of your country's government to the current coronavirus outbreak is appropriate, too extreme, or not sufficient?” (The reaction is much too extreme = 1; the reaction is somewhat too extreme = 2; the reaction is appropriate = 3; the reaction is somewhat insufficient = 4; the reaction is not at all sufficient = 5). Less than 5% answered the reaction is “much too extreme” or “somewhat too extreme.” Recoded as 1 the last two choices (“somewhat insufficient” and “not at all sufficient”); 0 otherwise. |
60% | — | 0 | 1 |
|
Personal Beliefs “What do you think: should people in your country 1) cancel their participation at social gatherings 2) should people in your country not shake other people's hands 3) should all shops in your country other than particular important ones, such as supermarkets, pharmacies, post offices, and gas stations, be closed; 4) should there be a general curfew in your country (with the exception of grocery shopping, necessary family trips and the commute to work) because of the coronavirus right now? Binary responses (yes/no) summed across the four items. |
3.47 | 0.8 | 1 | 4 |
|
General Beliefs “How many of 100 people in your country do you think believe that 1) participation at social gatherings should be cancelled; 2) one should not shake other people's hands; 3) all shops other than particularly important ones should be closed; 4) and there should be a general curfew because of the coronavirus right now? Original answers combined and standardized. |
0 | 1 | −3.38 | 1.95 |
| Country level (L2) covariates | ||||
|
Stringency Measure Based on the Oxford COVID-19 Government Response Tracker (OxCGRT) created by a cross-disciplinary team of researchers at the University of Oxford (https://covidtracker.bsg.ox.ac.uk/), which records the strictness of government policies restricting people's behaviors or physical mobility during the COVID-19 pandemic. |
0 | 1 | −3.02 | 1.51 |
|
Mobility Estimate Based on Google Community Mobility Reports (https://www.google.com/covid19/mobility/) on how visitors to (or time spent in) categorized places change compared to the baseline days, which are represented by a series of “normal” values for that day of the week prior to the coronavirus outbreak (i.e., median value from the 5-week period between January 3rd and February 6th, 2020). For each country, the scores for 5 categories (retail, grocery, parks, transit, work) are averaged for the period during which the online survey had been conducted. |
0 | 1 | −1.71 | 2.13 |
|
Globalization Index Based on the multidimensional globalization index maintained by the KOF Swiss Economic Institute, which combines a host of measures of cross-border interconnectedness (e.g., volumes of trade, foreign direct investments, number of embassies, and proportion of immigrants). A higher index score, ranging from 0 to 100, means more globalized (https://kof.ethz.ch/en/). |
0 | 1 | −2.72 | 1.46 |
|
Infected Cases Natural log-transformed numbers of coronavirus infections for each country averaged across the duration of the survey (retrieved from COVID-19 Data Repository maintained by the Center for Systems Science and Engineering at Johns Hopkins University). |
6.39 | 2.65 | 2.82 | 11.31 |
Data source: Global Behaviors and Perceptions in the COVID-19 Pandemic.
Note: Stringency Measure, Mobility Estimate and Globalization Index are standardized with the mean of 0 and the standard deviation of 1). L1 = Individual level; L2 = Country level.
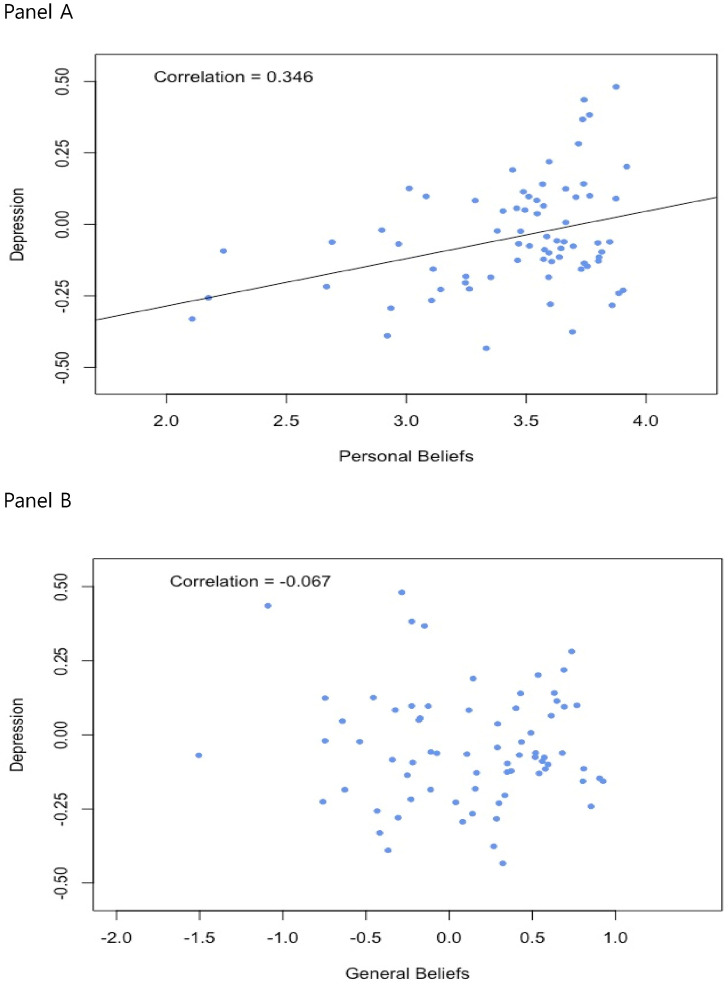
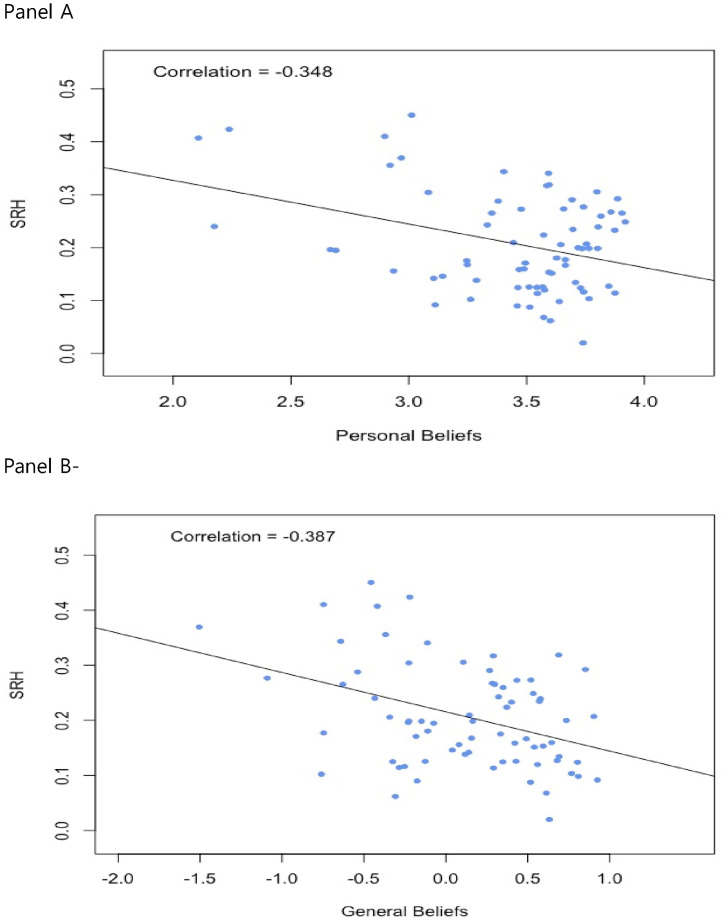
2.4. Confounders
Our models adjust for the following demographic and socioeconomic variables: age (in years), gender (ref.: female), education (coded on an ordinal scale), household income (in quintiles), and marital/partner status (ref.: solo). We also control for comorbidities (number of preexisting physical conditions) and the public perception of inadequateness of the government's handling of the COVID-19 pandemic. Variable definitions, coding procedures, and descriptive statistics are given in Table 1. Table 2 summarizes aggregate-level values for the outcome variables and the two predictors measuring beliefs concerning social distancing. We illustrate their relationships graphically in Fig. 1 (for Depression) and Fig. 2 (for SRH).
Table 2.
Description of the outcome measures and main predictors across 67 countries.
| Country | Sample size | Depression | SRH | Personal Beliefs | General Beliefs |
|---|---|---|---|---|---|
| Albania | 706 | 0.14 | 0.02 | 3.74 | 0.63 |
| Argentina | 1096 | −0.12 | 0.22 | 3.57 | 0.37 |
| Australia | 1026 | 0.05 | 0.17 | 3.49 | −0.18 |
| Austria | 1138 | −0.11 | 0.10 | 3.64 | 0.81 |
| Bangladesh | 132 | 0.44 | 0.28 | 3.74 | −1.09 |
| Belarus | 3729 | −0.02 | 0.41 | 2.90 | −0.75 |
| Belgium | 625 | −0.09 | 0.12 | 3.58 | 0.56 |
| Bolivia | 193 | −0.18 | 0.34 | 3.59 | −0.11 |
| Brazil | 11,738 | 0.38 | 0.20 | 3.76 | −0.23 |
| Bulgaria | 381 | 0.13 | 0.45 | 3.01 | −0.46 |
| Canada | 3098 | 0.04 | 0.11 | 3.55 | 0.29 |
| Chile | 566 | −0.06 | 0.27 | 3.66 | 0.52 |
| China | 488 | −0.16 | 0.09 | 3.11 | 0.93 |
| Colombia | 1902 | −0.10 | 0.26 | 3.82 | 0.35 |
| Czech Republic | 278 | −0.08 | 0.09 | 3.51 | 0.52 |
| Denmark | 534 | −0.20 | 0.18 | 3.25 | 0.33 |
| Dominican Republic | 562 | −0.23 | 0.27 | 3.90 | 0.30 |
| Ecuador | 317 | −0.28 | 0.27 | 3.86 | 0.28 |
| Egypt | 135 | 0.37 | 0.20 | 3.74 | −0.15 |
| Estonia | 166 | −0.18 | 0.17 | 3.25 | 0.16 |
| Ethiopia | 142 | −0.23 | 0.10 | 3.26 | −0.76 |
| Finland | 821 | −0.29 | 0.16 | 2.94 | 0.08 |
| France | 2993 | −0.06 | 0.13 | 3.85 | 0.68 |
| Germany | 11,350 | −0.07 | 0.16 | 3.47 | 0.42 |
| Greece | 374 | 0.06 | 0.07 | 3.57 | 0.61 |
| Guatemala | 151 | −0.06 | 0.31 | 3.80 | 0.11 |
| Hong Kong | 127 | −0.06 | 0.19 | 2.69 | −0.07 |
| Hungary | 635 | 0.10 | 0.13 | 3.51 | −0.13 |
| India | 1086 | −0.13 | 0.20 | 3.80 | 0.16 |
| Indonesia | 1642 | 0.05 | 0.34 | 3.40 | −0.64 |
| Ireland | 751 | −0.10 | 0.15 | 3.59 | 0.59 |
| Israel | 433 | −0.02 | 0.27 | 3.48 | 0.43 |
| Italy | 1974 | 0.10 | 0.10 | 3.76 | 0.77 |
| Japan | 621 | −0.39 | 0.36 | 2.92 | −0.37 |
| Kenya | 411 | 0.06 | 0.09 | 3.46 | −0.18 |
| Latvia | 690 | 0.10 | 0.30 | 3.08 | −0.23 |
| Lithuania | 105 | 0.08 | 0.14 | 3.29 | 0.12 |
| Luxembourg | 108 | 0.10 | 0.13 | 3.71 | 0.69 |
| Malaysia | 578 | −0.08 | 0.23 | 3.70 | 0.57 |
| Mexico | 3444 | −0.19 | 0.27 | 3.35 | −0.63 |
| Morocco | 398 | 0.20 | 0.25 | 3.92 | 0.53 |
| Netherlands | 1490 | −0.23 | 0.15 | 3.14 | 0.04 |
| New Zealand | 406 | −0.13 | 0.15 | 3.61 | 0.54 |
| Nigeria | 278 | −0.28 | 0.06 | 3.60 | −0.31 |
| Norway | 317 | −0.27 | 0.14 | 3.11 | 0.14 |
| Pakistan | 174 | 0.12 | 0.18 | 3.66 | −0.75 |
| Panama | 118 | −0.12 | 0.24 | 3.80 | 0.58 |
| Peru | 2092 | −0.24 | 0.29 | 3.89 | 0.85 |
| Philippines | 799 | 0.22 | 0.32 | 3.60 | 0.69 |
| Poland | 605 | 0.19 | 0.21 | 3.44 | 0.14 |
| Portugal | 592 | 0.01 | 0.17 | 3.66 | 0.49 |
| Qatar | 1296 | 0.28 | 0.20 | 3.72 | 0.74 |
| Romania | 855 | −0.14 | 0.12 | 3.74 | −0.25 |
| Russia | 3449 | −0.07 | 0.37 | 2.97 | −1.51 |
| Saudi Arabia | 112 | 0.09 | 0.23 | 3.87 | 0.40 |
| Singapore | 443 | −0.22 | 0.20 | 2.67 | −0.23 |
| Slovakia | 624 | −0.13 | 0.12 | 3.46 | 0.35 |
| South Africa | 608 | −0.08 | 0.21 | 3.64 | −0.34 |
| South Korea | 310 | −0.09 | 0.42 | 2.24 | −0.22 |
| Spain | 2491 | −0.15 | 0.21 | 3.75 | 0.90 |
| Sweden | 6060 | −0.26 | 0.24 | 2.17 | −0.43 |
| Switzerland | 4243 | −0.16 | 0.12 | 3.73 | 0.80 |
| Taiwan | 146 | −0.33 | 0.41 | 2.11 | −0.42 |
| Thailand | 339 | −0.04 | 0.32 | 3.59 | 0.29 |
| Turkey | 2926 | 0.48 | 0.11 | 3.87 | −0.28 |
| Ukraine | 1472 | −0.02 | 0.29 | 3.38 | −0.54 |
| United Arab Emirates | 205 | 0.14 | 0.13 | 3.57 | 0.43 |
| United Kingdom | 11,665 | −0.06 | 0.18 | 3.63 | −0.11 |
| United States | 12,379 | 0.08 | 0.12 | 3.54 | −0.32 |
| Uruguay | 248 | −0.43 | 0.24 | 3.33 | 0.32 |
| Venezuela | 665 | −0.38 | 0.29 | 3.69 | 0.27 |
| Vietnam | 867 | 0.11 | 0.16 | 3.49 | 0.65 |
Data source: Global Behaviors and Perceptions in the COVID-19 Pandemic.
Fig. 1.
Bivariate correlation between social distancing attitudes and depression.
Fig. 2.
Bivariate correlation between social distancing attitudes and self-rated health.
2.5. Analysis
We fitted mixed-effects models to examine the associations between the dependent variables and their individual- (L1) and country-level (L2) predictors. For Depression, we estimated multilevel linear regression models. SRH is coded as a binary variable. However, because log-odds ratios reflect the degree of unobserved heterogeneity and cannot be compared across models with different covariates (Mood, 2010), we used linear probability models for SRH. To investigate contextual effects of country-level predictors (Globalization Index and Mobility Estimate), we grand mean centered all L1 variables (Brincks et al., 2017). We ran cross-level interactions with both fixed and, as a robustness check, random slopes for the lower-level term (General Beliefs), as recommended (Heisig and Schaffer, 2019).
3. Results
3.1. Models predicting Depression
According to the null model (Model 1) in Table 3 , the intraclass correlation (ICC) is 0.044, i.e., 4.4% of the variance in people's mental health is due to country-level factors. According to Model 2, Personal Beliefs is positively related (β = 0.071, SE = 0.028, p < .05), while General Beliefs is negatively related (β = −0.151, SE = 0.02, p < .001). Model 3 introduces the background controls, according to which men, older persons, and those living with a spouse or partner are less depressed. By contrast, existing physical conditions (Comorbidities) and negative assessment of the government's handling of the new coronavirus (Insufficiency) are both positively associated with depression. As Model 4 indicates, net of controls, the two main predictors are consistently significant. In the final model (Model 5), Globalization Index (but not Mobility Estimate) emerges as a contextual predictor (β = -0.099, SE = 0.022, p < .001). Even with the inclusion of country-level covariates, the coefficients for Personal Beliefs and General Beliefs remain robust.
Table 3.
Results from mixed-effects models predicting mental health across 67 countries.
| DV = Depression | Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | |
| Intercept | 0.100⁎ | 0.0410 | 0.1268⁎⁎ | 0.0402 | 0.0395 | 0.0291 | 0.0529 | 0.0302 | 0.0500 | 0.0335 |
| (Individual level) | ||||||||||
| Male | −0.2708⁎⁎⁎ | 0.0340 | −0.2784⁎⁎⁎ | 0.0332 | −0.2829⁎⁎⁎ | 0.0356 | ||||
| Age | −0.0154⁎⁎⁎ | 0.0013 | −0.0148⁎⁎⁎ | 0.0013 | −0.0144⁎⁎⁎ | 0.0013 | ||||
| Partner | −0.1801⁎⁎⁎ | 0.0321 | −0.1710⁎⁎⁎ | 0.0317 | −0.1681⁎⁎⁎ | 0.0346 | ||||
| Education | 0.0019 | 0.0045 | 0.0016 | 0.0044 | 0.0004 | 0.0046 | ||||
| Household Income | −0.0032 | 0.0040 | −0.0025 | 0.0040 | −0.0076 | 0.0040 | ||||
| Comorbidities | 0.2875⁎⁎⁎ | 0.0436 | 0.2883⁎⁎⁎ | 0.0433 | 0.2861⁎⁎⁎ | 0.0457 | ||||
| Insufficiency | 0.1260⁎⁎ | 0.0413 | 0.0708 | 0.0436 | 0.0730 | 0.0433 | ||||
| Personal Beliefs | 0.0708⁎ | 0.0278 | 0.0725⁎⁎ | 0.0265 | 0.0817⁎⁎ | 0.0278 | ||||
| General Beliefs | −0.1513⁎⁎⁎ | 0.0202 | −0.1169⁎⁎⁎ | 0.0195 | −0.1367⁎⁎⁎ | 0.0205 | ||||
| (Country level) | ||||||||||
| Mobility Estimate | 0.0249 | 0.0239 | ||||||||
| Stringency Measure | 0.0154 | 0.0256 | ||||||||
| Globalization Index | −0.099⁎⁎⁎ | 0.0220 | ||||||||
| Infected Cases | 0.0360⁎⁎ | 0.0121 | ||||||||
| L1 variance (σ2) | 1.09937 | 1.0795 | 0.9560 | 0.9435 | 0.8729 | |||||
| L2 variance (τ) | 0.0495*** | 0.0463*** | 0.0040*** | 0.0056*** | 0.0001*** | |||||
| Deviance | 320,677.0605 | 307,454.4826 | 305,982.9586 | 297,137.8201 | ||||||
| L1/L2 N | 109,922/67 | 109,922/67 | 108,953/67 | 108,953/67 | 98,313/67 | |||||
Data: Global Behaviors and Perceptions in the COVID-19 Pandemic.
Note: SE = standard errors. DV = dependent variable. L1 = Individual level; L2 = Country level. Estimates are from using the restricted maximum likelihood (REML) estimator.
p* < 0.05, p ** < 0.01, p *** < 0.001 (two-tailed tests).
3.2. Models predicting SRH
Moving onto SRH, according to Model 1 in Tables 4 , 6.6% of the variance in people's physical health occurs between, as opposed to within, countries. Findings in Model 2 show, once again, that Personal Beliefs is positively associated with worse physical health (ß = 0.03, SE = 0.012, p < .01), while General Beliefs is negatively associated (ß = −0.017, SE = 0.008, p < .05). However, in contrast to the previous finding regarding mental health, according to Model 4, Personal Beliefs is not a significant predictor when adjusted for controls, whereas General Beliefs continues to be negatively associated (ß = −0.021, SE = 0.008, p < .01). Also, adding country variables hardly alters the strength of this latter association (Model 5). And no significant contextual effects are found.
Table 4.
Results from mixed-effects models predicting subjective physical health across 67 countries.
| DV = SRH | Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | |
| Intercept | 0.2669⁎⁎⁎ | 0.0189 | 0.2716⁎⁎⁎ | 0.0188 | 0.2586⁎⁎⁎ | 0.0185 | 0.2601⁎⁎⁎ | 0.0183 | 0.2644⁎⁎⁎ | 0.0187 |
| (Individual level) | ||||||||||
| Male | −0.0232 | 0.0139 | −0.0243 | 0.0137 | −0.0235 | 0.0137 | ||||
| Age | 0.0011⁎ | 0.0005 | 0.0012⁎ | 0.0005 | 0.0010 | 0.0005 | ||||
| Partner | −0.0454⁎⁎⁎ | 0.0131 | −0.0438⁎⁎⁎ | 0.0130 | −0.0460⁎⁎⁎ | 0.0131 | ||||
| Education | 0.0014 | 0.0018 | 0.0013 | 0.0018 | 0.0010 | 0.0018 | ||||
| Household Income | −0.0025 | 0.0017 | −0.0025 | 0.0017 | −0.0018 | 0.0017 | ||||
| Comorbidities | 0.3453⁎⁎⁎ | 0.0180 | 0.3455⁎⁎⁎ | 0.0179 | 0.3420⁎⁎⁎ | 0.0185 | ||||
| Insufficiency | 0.0588⁎⁎⁎ | 0.0173 | 0.0471⁎⁎ | 0.0182 | 0.0421⁎ | 0.0182 | ||||
| Personal Beliefs | 0.0295⁎⁎ | 0.0115 | 0.0171 | 0.0110 | 0.0211 | 0.0118 | ||||
| General Beliefs | −0.0174⁎ | 0.0084 | −0.0213⁎⁎ | 0.0081 | −0.0244⁎⁎ | 0.0083 | ||||
| (Country level) | ||||||||||
| Mobility Estimate | 0.0225 | 0.0189 | ||||||||
| Stringency Measure | 0.0080 | 0.0173 | ||||||||
| Globalization Index | −0.0239 | 0.0278 | ||||||||
| Infected Cases | −0.0165 | 0.0139 | ||||||||
| L1 variance (σ2) | 0.1854 | 0.1848 | 0.1615 | 0.1611 | 0.1440 | |||||
| L2 variance (τ) | 0.0134*** | 0.0132*** | 0.0114*** | 0.011*** | 0.0083*** | |||||
| Deviance | 126,690.3675 | 111,872.9676 | 111,588.7418 | 99,217.6990 | ||||||
| L1/L2 N | 109,922/67 | 109,922/67 | 108,953/67 | 108,953/67 | 98,313/67 | |||||
Data: Global Behaviors and Perceptions in the COVID-19 Pandemic.
Note: SE = standard errors. DV = dependent variable. L1 = Individual level; L2 = Country level. Estimates are from using the restricted maximum likelihood (REML) estimator.
p* < 0.05, p ** < 0.01, p *** < 0.001 (two-tailed tests).
3.3. Interaction effects with General Beliefs
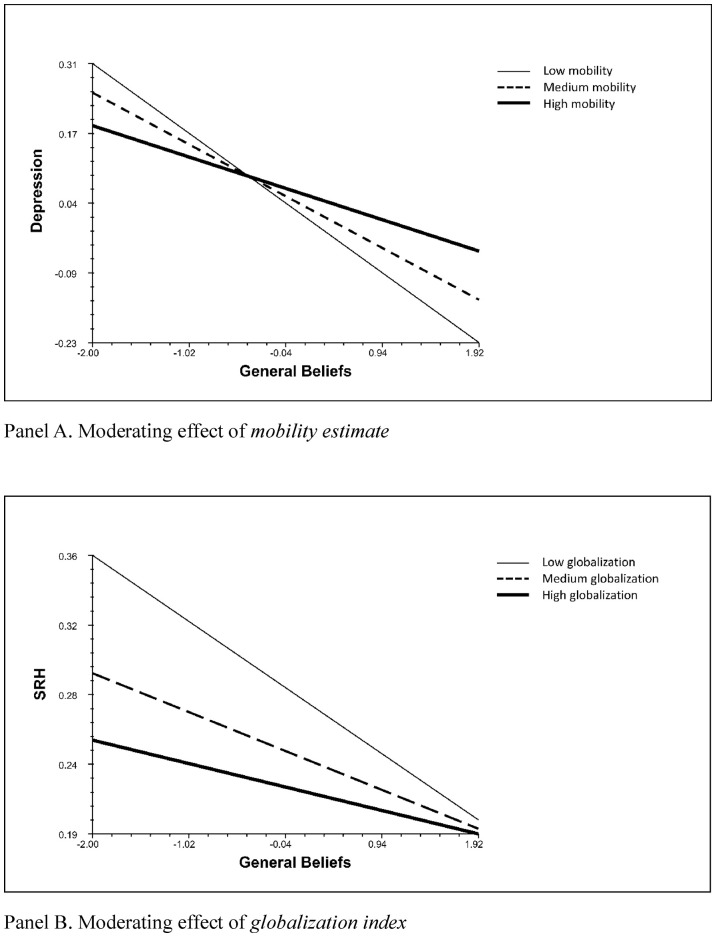
As the cross-level interaction term (ß = 0.062, SE = 0.022, p < .01) in Model 1 in Table 5 shows, the negative association between General Beliefs and Depression becomes less pronounced in countries with greater internal mobility, i.e., lower rates of self-isolation. In Model 2, we allow the slopes for General Beliefs to vary across countries for a more stringent test (Heisig and Schaffer, 2019). The multiplicative term (General Beliefs x Mobility Estimate) in this random coefficient model is also significant (ß = 0.054, SE = 0.026, p < .05), providing additional support. In Fig. 3 (Panel A based on Model 2 from Table 5), we demonstrate this contingent relationship across three distinct levels of mobility estimate: high (75th percentile), medium (50th percentile) and low (25th percentile).
Table 5.
Results from estimating cross-level interactions for the two health outcomes.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||
|---|---|---|---|---|---|---|---|---|
| (DV = Depression) |
(DV = Depression) |
(DV = SRH) |
(DV = SRH) |
|||||
| Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | Coef. | (SE) | |
| Intercept | 0.0674⁎ | 0.0330 | 0.0453 | 0.0350 | 0.2647⁎⁎⁎ | 0.0186 | 0.2575⁎⁎⁎ | 0.0195 |
| (Individual level) | ||||||||
| Personal Beliefs | 0.0745⁎⁎ | 0.0278 | 0.0716⁎ | 0.0285 | 0.0204 | 0.0117 | 0.0198 | 0.0118 |
| General Beliefs | −0.1424⁎⁎⁎ | 0.0209 | −0.0949⁎⁎⁎ | 0.0275 | −0.0272⁎⁎ | 0.0091 | −0.0288⁎ | 0.0114 |
| (Country level) | ||||||||
| Mobility Estimate | 0.0006 | 0.0246 | 0.0224 | 0.0290 | 0.0227 | 0.0187 | 0.0236 | 0.0339 |
| Stringency Measure | 0.0128 | 0.0255 | 0.0376 | 0.0306 | 0.0079 | 0.0171 | 0.0192 | 0.0429 |
| Globalization Index | −0.0975⁎⁎⁎ | 0.0209 | −0.0545 | 0.0288 | −0.0254 | 0.0276 | −0.0372 | 0.0336 |
| Infected Cases | 0.0361⁎⁎ | 0.0116 | 0.0239 | 0.0149 | −0.0168 | 0.0138 | −0.0042 | 0.0210 |
| (Interaction effects) | ||||||||
| General Beliefs x | Mobility Estimate | Mobility Estimate | Globalization Index | Globalization Index | ||||
| 0.0623⁎⁎ | 0.0217 | 0.0539⁎ | 0.0253 | 0.0124 | 0.0066 | 0.0166⁎ | 0.0075 | |
| L1 variance (σ2) | 0.8727 | 0.8511 | 0.1439 | 0.1438 | ||||
| L2 variance (τ) | 0.0000*** | 0.0062⁎⁎⁎ | 0.0080⁎⁎⁎ | 0.0086⁎⁎⁎ | ||||
| Varying slopes | 0.0075⁎⁎⁎ | 0.0003⁎⁎⁎ | ||||||
| L1/L2 N | 98,313/67 | 98,313/67 | 98,313/67 | 98,313/67 | ||||
Data: Global Behaviors and Perceptions in the COVID-19 Pandemic.
Note: All models adjust for the individual-level covariates shown in Table 2, Table 3. SE = standard errors. DV = dependent variable. L1 = Individual level; L2 = Country level. Estimates are from using the restricted maximum likelihood (REML) estimator.
p* < 0.05, p ** < 0.01, p *** < 0.001 (two-tailed tests).
Fig. 3.
Contingent relationships between general beliefs and health outcomes.
The last two models in Table 4 predict SRH, according to which the positive association between the perception of what others believe concerning COVID-19 and worse physical health similarly decreases as a function of globalization, as confirmed by the interaction term in Model 4 with varying slopes (ß = 0.017, SE = 0.008, p < .05). Panel B in Fig. 3 (based on this last model) reflects the shifting trend, as shown by the separate lines referring to distinct levels on the score index (low, medium, and high). That the darkest line (a subgroup of most globalized countries) has the flattest slope indicates that globalization weakens the relationship between the two variables under consideration. In models not shown, we estimated cross-level interactions with Personal Beliefs. Results were not significant.
4. Discussion
This study investigated how and the extent to which normative beliefs concerning coronavirus-induced social distancing behaviors are related to health outcomes in a cross-national context. In so doing, it also probed contextual and moderation effects of two country-level variables, aggregate estimate of physical mobility and level of globalization. Our main finding is that individuals who are personally more worried about the coronavirus (i.e., believe in canceling social gatherings, maintaining physical distancing closing non-essential stores, and imposing a general curfew) experience higher levels of depression. Notably, our analysis shows that mental health is also associated with the perception of others' attitudes on anti-coronavirus measures. Given the highly contagious nature of COVID-19, believing that a greater number of compatriots endorse social distancing, including complete lockdown, would provide some emotional relief, all things equal. According to our findings, concerning depression, both personal and general normative beliefs emerge as significant predictors, while adjusting for a host of controls at individual and country levels. With respect to self-rated health, when we check the sensitivity of our results to potential confounders, the net effect of personal beliefs becomes fully mediated, whereas that of general beliefs remains robustly significant. In short, the attitudes of generalized others matter when it comes to the impact of COVID-19 on mental and physical health.
The present study indicates that the associations between normative beliefs of others and the two health outcomes are not constant but vary cross-nationally partly as a function of mobility (internal movements of people) and globalization (cross-border economic, social and political inflows). Specifically, the negative association between others' beliefs about social distancing and depression is stronger for the residents of countries with lower mobility rates, i.e., relatively limited physical movements of citizens since the COVID-19 outbreak. If you believe that more people are willing to adhere to anti-coronavirus measures, then you are less depressed (knowing that others are being careful about spreading the disease or being infected by it). However, this protective effect becomes diminished in the context of higher mobility. That is, the objective reality of human movements (unwillingness to comply with social distancing mandates) undermines the health-promoting role of subjective perception of others' normative views. A major public health implication is to recognize the interconnected and intersubjective nature of social distancing and its impact on mental wellbeing. As such, it is critical to raise public awareness concerning the dual importance of social distancing: not only does it prevent the spread of the virus but it also creates positive ripple effects. That is, perception that others are being responsible can help improve the mental health status of the perceivers.
Moreover, with respect to physical health, the impact of general beliefs is greater in less globalized countries. As mentioned above, contextual or independent effect of globalization is significant: net of compositional factors, residents of more globalized countries are mentally healthier (less depressed). This may be the case because more globalized countries are on average more developed economically (as GDP is a key variable in calculating the index), more likely to have better global access to information about public health safety, have more connections with foreign governments and international organizations for collaboration in tackling pandemics, and are consequently better able to deal with the current coronavirus pandemic. That is, globalization is a proxy for protection against depression. As a result, general normative beliefs would matter less for the citizens in more globalized (i.e., “better protected”) countries. Believing that others believe in behaving appropriately to fight against COVID-19, therefore, becomes more salient in less globalized (i.e., “more vulnerable”) parts of the world. In our sample, Switzerland and the Netherlands rank number one and two in terms of globalization, respectively. At the other end, Ethiopia occupies the lowest position, followed by Bangladesh. Panel B in Fig. 3 contains three lines (groups of countries) according to varying levels of globalization, with the darkest line (with the flattest slope) referring to the most globalized subgroup of nations including Switzerland and Netherlands and the lightest one (with the steepest slope) corresponding to the most insulated or least globally connected countries such as Ethiopia and Bangladesh. Another implication, this time, for global public health is that to reduce worsening health inequality during the current pandemic, it is imperative to foster general normative beliefs especially in countries that are economically less developed.
Contrary to some expectations, COVID-19 has not been a great “equalizer” in indiscriminately affecting all people across all nations (Mein, 2020). Rather, the infection and the associated burdens of the coronavirus disease have fallen disproportionately on the socially marginalized and the financially precarious (Przeworski, 2020). One of the main tasks for researchers is to clarify the differential ways in which the current pandemic has had its impact globally. Why are some individuals more susceptible than others to the novel coronavirus and face higher costs? What are the key socioeconomic, demographic, and other factors that contribute to unequal health consequences? And how does the country of residence possibly play a role in all of this? The present study sought to shed light on these critical questions by using large-scale micro data containing rare information about the attitudes, beliefs, and behaviors of people in times of a pandemic across multiple countries. Given the cross-sectional nature of the data used in this study, findings regarding the focal measures should be interpreted with caution. For a more causal analysis, longitudinal data are needed. No doubt, cross-national panel data are costly and time-consuming. Given what is at stake, designing longitudinal studies would prove valuable in not only better understanding the current situation but perhaps better dealing with the health consequences of future pandemics.
Declaration of Competing Interest
None.
References
- Banik A., Nag T., Chowdhury S.R., Chatterjee R. Why do COVID-19 fatality rates differ across countries? An explorative cross-country study based on select indicators. Glob. Bus. Rev. 2020;21(3):607–625. doi: 10.1177/0972150920929897. [DOI] [Google Scholar]
- Brincks A.M., Enders C.K., Llabre M.M., Bulotsky-Shearer R.J., Prado G., Feaster D.J. Centering predictor variables in three-level contextual models. Multivar. Behav. Res. 2017;52(2):149–163. doi: 10.1080/00273171.2016.1256753. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Dalexis R.D., Kokou-Kpolou C.K., Mukunzi J.N., Rousseau C. Social inequalities and collateral damages of the COVID-19 pandemic: when basic needs challenge mental health care. Int. J. Public Health. 2020;65:717–718. doi: 10.1007/s00038-020-01426-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey R.C., McAlaney J., Bewick B.M. A critical appraisal of the Social Norms Approach as an interventional strategy for health-related behavior and attitude change. Front. Psychol. 2018;9:2180. doi: 10.3389/fpsyg.2018.02180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fetzer T.R., Witte M., Hensel L., Jachimowicz J., Haushofer J., Ivchenko A., Caria S., Reutskaja E., Roth C.P., Fiorin S., Gomez M., Kraft-Todd G., Gotz F.M., Yoeli E. National Bureau of Economic Research; 2020. Global Behaviors and Perceptions at the Onset of the COVID-19 pandemic.http://www.nber.org/papers/w27082 Working Paper 27082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63(1):e32. doi: 10.1192/j.eurpsy.2020.35. 1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giallonardo V., Sampogna G., Del Vecchio V., Luciano M., Albert U., Carmassi C., Carrà G., Cirulli F., Dell’Osso B., Nanni M.G., Pompili M., Sani G., Tortorella A., Volpe U., Fiorillo A. The impact of quarantine and physical distancing following COVID-19 on mental health: study protocol of a multicentric Italian population trial. Front. Psychiatry. 2020;11(533) doi: 10.3389/fpsyt.2020.00533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Google COVID-19 Community Mobility Reports: See How Your Community is Moving Around Differently due to COVID-19. 2020. https://www.google.com/covid19/mobility/
- Gygli S., Haelg F., Sturm J.-E., Potrafke N. The KOF globalisation index – revisited. Rev. Int. Organ. 2019;14(3):543–574. (doi:10.1007/s11558- 019-09344-2) [Google Scholar]
- Harlem G., Lynn M. Descriptive analysis of social determinant factors in urban communities affected by COVID-19. J. Public Health. 2020;42(3):466–469. doi: 10.1093/pubmed/fdaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heisig J.P., Schaffer M. Why you should always include a random slope for the lower-level variable involved in a cross-level interaction. Eur. Sociol. Rev. 2019;35(2):258–279. doi: 10.1093/esr/jcy053. [DOI] [Google Scholar]
- Holingue C., Badillo-Goicoechea E., Riehm K.E., Veldhuis C.B., Thrul J., Johnson R.M., Fallin M.D., Kreuter F., Stuart E.A., Kalb L.G. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: findings from American trend panel survey. Prev. Med. 2020;139(106231) doi: 10.1016/j.ypmed.2020.106231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jachimowicz J.M., Hauser O.P., O’Brien J.D., Sherman E., Galinsky A.D. The critical role of second-order normative beliefs in predicting energy conservation. Nat. Hum. Behav. 2018;2(10):757–764. doi: 10.1038/s41562-018-0434-0. [DOI] [PubMed] [Google Scholar]
- Kim H., Laurence J. COVID-19 restrictions and mental distress among American adults: evidence from Corona Impact Survey (W1 & W2) J. Public Health. 2020 doi: 10.1093/pubmed/fdaa148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legros S., Cislaghi B. Mapping the social-norms literature: an overview of reviews. Perspect. Psychol. Sci. 2020;15(1):62–80. doi: 10.1177/1745691619866455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamluk L., Jones T. National Institute for Health Research; 2020. The Impact of COVID-19 on Black, Asian and Minority Ethnic Communities.https://arc-w.nihr.ac.uk/research-and-implementation/covid-19-response/reports/the-impact-of-covid-19-on-black-asian-and-minority-ethnic-communities/ [Google Scholar]
- Mein S.A. COVID-19 and health disparities: the reality of “the Great Equalizer”. J. Gen. Intern. Med. 2020;35(8):2439–2444. doi: 10.1007/s11606-020-05880-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mood C. Logistic regression: why we cannot do what we think we can do, and what we can do about it. Eur. Sociol. Rev. 2010;26(1):67–82. doi: 10.1093/esr/jcp006. [DOI] [Google Scholar]
- Ölcer S., Yilmaz-Aslan Y., Brzoska P. Lay perspectives on social distancing and other official recommendations and regulations in the time of COVID-19: a qualitative study of social media posts. BMC Public Health. 2020;20(963) doi: 10.1186/s12889-020-09079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxfam International How the Coronavirus Pandemic Exploits the Worst Aspects of Extreme Inequality. 2020. https://www.oxfam.org/en/how-coronavirus-pandemic-exploits-worst-aspects-extreme-inequality
- Pederson M.J., Favero N. Social distancing during the COVID-19 pandemic: who are the present and future noncompliers? Public Adm. Rev. 2020 doi: 10.1111/puar.13240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Przeworski A. COVID-19: A Magnifier of Social Inequality. 2020. https://graduateinstitute.ch/coronavirus-information-our-community-and-visitors/covid-19-magnifier-social-inequality
- Raisi-Estabragh Z., McCracken C., Bethell M.S., Cooper J., Cooper C., Caulfield M.J., Munroe P.B., Harvey N.C., Petersen S.E. Greater risk of severe COVID-19 in black, Asian and minority ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank. J. Public Health. 2020;42(3):451–460. doi: 10.1093/pubmed/fdaa095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds K. Social norms and how they impact human behaviour. Nat. Hum. Behav. 2018;3:14–15. doi: 10.1038/s41562-018-0498-x. Published online: 17 December 2018. [DOI] [PubMed] [Google Scholar]
- Tesar J. How do social norms and expectations about others influence individual behavior? Found. Sci. 2020;25:135–150. doi: 10.1007/s10699-019-09582-y. [DOI] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289(113098) doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams S.N., Armitage C.J., Tampe T., Dienes K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: a UK-based focus group study. BMJ Open. 2020;10(e039334) doi: 10.1136/bmjopen-2020-039334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Mental Health and Psychosocial Considerations During the COVID-19 Outbreak. 2020. https://www.who.int/teams/mental-health-and-substance-use/covid-19
- Wright L., Steptoe A., Fancourt D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J. Epidemiol. Community Health. 2020;0:1–6. doi: 10.1136/jech-2020-214475. [DOI] [PMC free article] [PubMed] [Google Scholar]