Abstract
Background:
Hammertoe deformities can seriously affect activity level and footwear. The use of prescription, mood-altering medications is very common, with some estimates as high as 25% of the population. Mood disorders, especially depression, negatively affect the results of medical and operative treatments. This study assessed the relationship of mood-altering medication use with the outcomes and complications of operative reconstruction of hammertoes.
Methods:
Data were prospectively collected from 116 patients who underwent hammertoe reconstruction, including demographic information, medical history, the use of mood-altering psychotropic medications (antidepressants, anxiolytics, hypnotics, and mood stabilizers), and postoperative complications. Preoperative patient-reported outcomes were measured using the visual analog scale (VAS) for pain and Short Form Health Survey (SF-36), which were repeated at 1-year follow-up.
Results:
A total of 36.2% of patients were taking psychotropic medications. Medication and nonmedication groups had similar pain VAS and SF-36 Physical Component Summary (PCS) scores before and after surgery. Compared with nonmedication patients, patients on psychotropic medications had significantly lower SF-36 Mental Component Summary (MCS) scores preoperatively (P = .001) and postoperatively ( P = .006), but no significant difference in the change in MCS (ΔMCS) from preoperative to postoperative. Psychotropic medication use was associated with superficial wound infections (P = .048), but not other complications.
Conclusions:
Patients taking psychotropic medications were equally likely to benefit from forefoot reconstruction as nonmedication patients. Preoperative and postoperative PCS and VAS were not significantly different between medication and nonmedication groups. Although the medication group had lower absolute MCS, they reported the same magnitude of improvement in MCS (ΔMCS) as the nonmedication group.
Level of Evidence:
Level II, prospective cohort study.
Keywords: hammertoe, psychiatry, outcomes, complications, forefoot disorders, depression, psychotropic medications
Introduction
Psychiatric disorders are increasingly understood to have important clinical implications in orthopedic surgery owing to the impact on pain perception. Depression has been found to be the strongest predictor of health status and has been associated with heightened pain perception and stress. 28 Because of the prevalence of anxiety (29%) and depression (17%) in the population, 14 and the expectation that these numbers may double in the next 20 years, 2,24 orthopedic surgeons have increasingly taken interest in the effect of psychiatric disorders on orthopedic conditions, their treatments, and their outcomes. 4,13,25,30
Current literature documents that psychiatric conditions can lead to more difficult treatment courses, including longer hospital stays, increased demand on resources, generally poorer outcomes, and overall increased incidence of disease. 3,10 -12,17,24,26,31 There is also an association with decreased access to care and difficulty in expressing somatic symptoms, which can lead to delayed diagnosis and treatment. 17 These patients are more likely to experience side effects from medicine or anesthesia and have a higher rate of comorbid conditions such as hypertension, diabetes, obesity, and hyperlipidemia, which can lead to procedures and postoperative care that is more complicated. 8 Despite these findings, there have been few studies examining the effect of psychiatric and mood disorders in patients with foot and ankle conditions, a group that has reported to have increased rates of psychiatric comorbidity. 28
Hammertoe deformities may be associated with mood disorders or psychiatric conditions because of the link to chronic pain. 28 Malaligned toes and metatarsophalangeal joints can cause pain due to synovitis, swelling, and pressure lesions. In a sensate patient, pressure of the deformities may cause plantar callus, dorsal corns, and overlapping digits. In patients with neuropathy, the patient is at risk for ulcer formation. These problems can cause issues with footwear, ability to exercise, and even restrict activities of daily living, and as a result, like many musculoskeletal conditions, may influence emotional health. When nonoperative measures fail to resolve the pain, 7 operative correction may be pursued to improve physical pain and function. Although operative correction of these deformities has proven successful in relieving pain, 29 there is a relatively high complication rate reported in the literature, ranging from 20% to 55%. 1,6,9,21,29 The purpose of this study was to explore the possible association of psychotropic medication use in patients with hammertoe deformities, on the demographics, comorbidities, patient-reported outcomes, including the perception of pain, and complications related to operative reconstruction of hammertoe deformities.
Methods
A prospective cohort study was conducted on all patients who underwent operative correction of hammertoe deformity of 1 or more toes at 2 institutions between January 1, 2015, and September 1, 2018. Patients who underwent concomitant procedures for other deformities were excluded. Demographic data, including age, sex, and affected toes, were collected at each patient’s preoperative clinic visit. The use of psychotropic medications, specifically antidepressants and others (anxiolytics, hypnotics, and mood stabilizers), was also documented at this time. Informed consent was received from all participants. Patients were surveyed regarding their past medical history, and the following comorbidities were recorded: smoking history, blood thinner use (including aspirin, warfarin, and antiplatelet agents), rheumatoid arthritis, diabetes mellitus, peripheral arterial disease, chronic obstructive pulmonary disease, coronary artery disease, and osteoporosis. A preoperative visual analog scale (VAS) to assess pain and Short Form-36 Health Survey (SF-36) Physical and Mental Component Summary scores to assess function (PCS and MCS, respectively) were recorded for all patients.
Surgical Technique
Two foot and ankle fellowship–trained orthopedic surgeons performed the surgeries. For patients who had failed an adequate trial of nonoperative management of their hammertoe deformity, reconstruction always included proximal interphalangeal (PIP) arthroplasty, resecting both sides of the PIP joint with an electric micro-saw, and flexor tenotomy at the level of the resection. The PIP joint was stabilized with smooth 0.045 and 0.035 wires. Persistent extension of the MTP joint was addressed first with extensor tendon lengthening, followed by extensive MTP capsulotomy as needed. For severe deformities, additional procedures were performed commensurate to the required correction, including a modified Weil distal metatarsal osteotomy, reconstructions of the plantar plate, collateral ligaments and capsular repair, and, if needed, flexor digitorum longus tendon transfer to the extensor hood on the side of the residual deformity. Performed procedures were collected. Following surgery, patients were allowed progressive weightbearing in a postoperative shoe. Sutures were removed at 2 weeks. At 6 weeks, the Kirschner wires were removed, and patients were instructed to continue full weightbearing in the surgical shoe another 2 weeks prior to gradually transitioning to wide or open-toed shoes.
Patients were followed at regular intervals to assess for postoperative complications, including wound infections requiring antibiotics, deep vein thrombosis, recurrence of the deformity, and the need for revision surgery (any reoperation performed on the deformity, excluding incision and drainage for infection). All patients were followed at 1 year postoperatively and were readministered the VAS pain scale, and the SF-36 PCS and MCS scores. At least 1 year of patient-reported survey data were collected on 107 of 116 patients (92.2% response rate). Change in patient-reported outcome (Δ) metrics were calculated by subtracting preoperative results from postoperative results. Patients were divided into groups based on whether they were preoperatively taking 1 or more psychotropic medications (MED) or not (NON-MED).
A total of 116 patients were identified who underwent surgery for hammertoe deformity and enrolled in this study. Comparison of demographics and comorbidities between the medication group and the nonmedication group are presented in Table 1. The average age of patients in the study was 63.2 ± 11.5, and 85.3% were female. Patients in the MED group were more likely to be concurrently taking blood thinners than patients in the NON-MED group (P = .040). No other significant associations were found between psychotropic medication use and the other baseline characteristics. A comparison of type of procedure performed (operative techniques noted in Methods) also detected no differences between groups.
Table 1.
Baseline and Procedural Characteristics.a
| Psychotropic Medication Use | P Value | |||
|---|---|---|---|---|
| Total | NON-MED (n = 74) | MED (n = 42) |
||
| Female | 99 (85.3) | 65 (87.8) | 34 (81.0) | .41 |
| Age, mean ± SD | 63.2 ± 11.5 | 62.2 ± 12.9 | 65.0 ± 8.3 | .16 |
| Number of toes operated | .30 | |||
| 1 | 36 (31.0) | 19 (25.7) | 17 (40.5) | |
| 2 | 33 (28.5) | 23 (31.1) | 10 (23.8) | |
| 3 | 14 (12.1) | 11 (14.9) | 3 (7.1) | |
| 4 | 23 (19.8) | 16 (21.6) | 7 (16.7) | |
| 5 or more | 10 (8.6) | 5 (6.8) | 5 (11.9) | |
| Smoker | .30 | |||
| Current | 4 (3.5) | 2 (2.7) | 2 (4.8) | |
| Former | 13 (11.2) | 6 (8.1) | 7 (16.7) | |
| Never | 99 (85.3) | 66 (89.2) | 33 (78.6) | |
| Blood thinners | 26 (22.4) | 12 (16.2) | 14 (33.3) | .040* |
| RA | 16 (13.8) | 7 (9.5) | 9 (21.4) | .09 |
| Diabetes | 9 (7.8) | 6 (8.1) | 3 (7.1) | .53 |
| Peripheral arterial disease | 2 (1.7) | 2 (2.7) | 0 (0.0) | .534 |
| COPD | 8 (6.9) | 3 (4.1) | 5 (11.9) | .14 |
| Coronary artery disease | 11 (9.5) | 5 (6.8) | 6 (14.3) | .20 |
| Osteoporosis | 18 (15.5) | 9 (12.2) | 9 (21.4) | .20 |
| Procedural characteristics | ||||
| PIP arthroplasty | 108 (145.9) | 69 (93.2) | 39 (92.9) | >.99 |
| Flexor to extensor transfer | 30 (40.5) | 18 (24.3) | 12 (28.6) | .62 |
| Extensor transfer | 13 (17.6) | 8 (10.8) | 5 (11.9) | >.99 |
| Extensor lengthening | 78 (105.4) | 52 (70.3) | 26 (61.9) | .36 |
| Flexor transfer | 45 (60.8) | 27 (36.5) | 18 (42.9) | .50 |
| Flexor tenotomy | 24 (32.4) | 16 (21.6) | 8 (19.0) | .74 |
| Weil osteotomy | 43 (58.1) | 32 (43.2) | 11 (26.2) | .07 |
| Plantar plate repair | 29 (39.2) | 21 (28.4) | 8 (19.0) | .27 |
| MTP joint capsulotomy | 85 (114.9) | 56 (75.7) | 29 (69.0) | .44 |
Abbreviations: COPD, chronic obstructive pulmonary disease; MTP, metatarsophalangeal; PIP, proximal interphalangeal; RA, rheumatoid arthritis.
a Unless otherwise noted, values are n (%).
* Statistical significance (P < .05).
Statistical Analysis
Data were summarized by the psychiatric medication use. Continuous variables were presented as mean, with standard deviations. Categorical data were presented as frequency and percentage. The Shapiro-Wilk test was used to assess normality. Demographics, baseline clinical measurements and outcomes were compared between the groups using Student t test to compare the means of the continuous variables and Fisher exact test / Pearson chi-square test to compare the rates of the categorical variables. We inferred statistical significance if the computed 2-sided P value is <.05. Data analysis was performed using JMP, version 14.3 (SAS Institute Inc, Cary, NC).
Results
Patient-reported outcome measures are presented in Table 2, comparing the preoperative scores, the postoperative scores, and the change from preoperative to postoperative between the medication (MED) and nonmedication (NON-MED) groups. When comparing the preoperative VAS scores, the postoperative VAS scores, or the change in the VAS scores (Δ VAS) from preoperative to postoperative, no significant differences were found between the 2 patient groups. When comparing the preoperative PCS scores, the postoperative PCS scores, or the change in the PCS scores (Δ PCS) from preoperative to postoperative, no significant differences were found between the 2 patient groups.
Table 2.
Outcomes.
| Psychotropic Medication Use | P Value | |||
|---|---|---|---|---|
| Total, Mean ± SD | NON-MED, Mean ± SD (n = 74) |
MED, Mean ± SD (n = 42) |
||
| VAS | ||||
| Preoperative | 4.4 ± 2.8 | 4.3 ± 2.9 | 4.6 ± 2.6 | .53 |
| Postoperative | 1.6 ± 2.2 | 1.5 ± 2.1 | 1.8 ± 2.3 | .53 |
| Δ VAS | –2.8 ± 3.0 | –2.8 ± 2.9 | –2.6 ± 3.1 | .76 |
| PCS | ||||
| Preoperative | 59.6 ± 23.4 | 62.5 ± 23.2 | 54.6 ± 23.2 | .08 |
| Postoperative | 70.4 ± 22.9 | 73.1 ± 21.5 | 65.4 ± 24.9 | .12 |
| Δ PCS | 10.8 ± 21.1 | 10.7 ± 19.0 | 11.1 ± 24.8 | .93 |
| MCS | ||||
| Preoperative | 80.9 ± 16.6 | 85.5 ± 13.1 | 72.9 ± 19.0 | .001* |
| Postoperative | 84.3 ± 14.9 | 87.5 ± 11.8 | 78.1 ± 18.2 | .006* |
| Δ MCS | 3.1 ± 13.7 | 2.0 ± 12.8 | 5.3 ± 15.2 | .25 |
Abbreviations: MCS, Mental Component Summary; PCS, Physical Component Summary; VAS, visual analog scale.
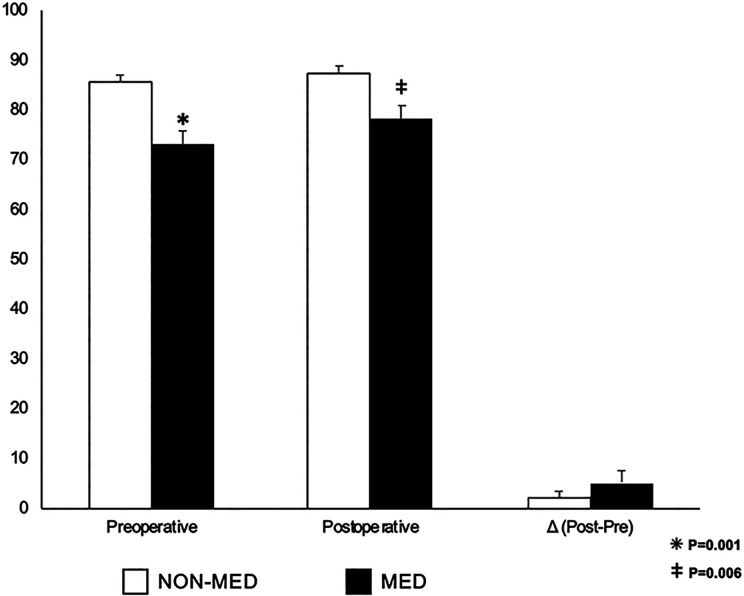
Significant differences were found between the 2 patient groups in the preoperative and postoperative MCS scores (Figure 1). The preoperative MCS of the MED group was 72.9 ± 19.0, which was lower than the MCS of 85.5 ± 13.1 in the NON-MED group (P = .001). The 1-year postoperative MCS was also lower in the MED group (MED: 78.1 ± 18.2 vs. NON-MED: 87.5 ± 11.8; P = .006). However, no significant difference was found in the change (improvement) in the MCS score (Δ MCS) from preoperative to postoperative between the 2 groups (MED: 5.3 ± 15.2 vs. NON-MED: 2.0 ± 12.8; P = .25).
Figure 1.
A comparison of preoperative, postoperative, and Δ (calculated as postoperative minus preoperative) MCS values between patients taking psychotropic medications (MED) and those who are not (NON-MED).
The occurrence of postoperative complications is presented in Table 3. One or more complications occurred in 33.6% of patients, with the most prevalent being recurrent deformity in 14.7%. Superficial wound infections were more common in the MED group (21.4%) compared to the NON-MED group (8.1%; P = .048). No other statistically significant differences were found between the medication and nonmedication groups and other postoperative complications of deep vein thrombosis, recurrent deformity, or revision surgery.
Table 3.
Postoperative Complications.
| Psychotropic Medication Use | P Value | |||
|---|---|---|---|---|
| Total | NON-MED (n = 74) |
MED (n = 42) |
||
| Superficial wound infection | 15 (12.9) | 6 (8.1) | 9 (21.4) | .048* |
| Deep vein thrombosis | 3 (2.6) | 2 (2.7) | 1 (2.4) | .99 |
| Deformity recurrence | 17 (14.7) | 12 (16.2) | 5 (11.9) | .60 |
| Revision surgery | 11 (9.5) | 7 (9.5) | 4 (9.5) | .99 |
*P < .05.
Discussion
This study investigated the possible associations of mood-altering drug use (and presumably the underlying mood disorders for which they were prescribed) on the demographics, comorbidities, patient-reported outcomes, and complications of operative correction of hammertoe deformities. We found that patients in the psychotropic medication group had statistically significant lower patient-reported mental component SF-46 (MCS) scores as well as a higher rate of superficial wound infections.
In our study, the prevalence of patients being treated with any type of psychotropic medications at the time of their preoperative appointment was 36.2%. More specifically, 25.9% of our sample population was using antidepressant pharmacotherapy and 19.0% were using other psychotropic medications, with some patients taking both. These findings are substantially higher than the results of a National Center for Health Statistics study, which found that 12.7% of the US population over the age of 12 years take antidepressants and 19.1% over the age of 60 (more similar to our study’s average age of 63.2 years). 23 Because operative correction of hammertoes is pursued when nonoperative measures fail to treat patients’ subjective pain and people with depression are more likely to report bothersome foot and ankle–related symptoms, one explanation for this discrepancy in prevalence may be that patients taking psychotropic medications seek operative management of symptomatic hammertoe more readily. 7,27
The percentage of patients in this study who were taking antidepressants was higher than rates of depression found in previous studies investigating the relationship between mental health and other foot and ankle operative outcomes. Based on Short Form-12 Mental Component Summary scores that were correlated with Patient Health Questionnaire–9 results, Shakked et al 27 reported that 15% of patients who underwent operative correction for hallux valgus were depressed. Among all patients who visited a foot and ankle clinic for chronic diseases, Nakagawa et al 20 found 27% of patients had depression and 30% had anxiety, which was determined using the Hospital Anxiety and Depression Scale. It is important to note that we only assessed whether patients were taking psychotropic medications, whereas the 2 aforementioned studies used patient questionnaires to identify study participants with depression, whether treated or not. One possible explanation for this difference is that patients who have a history of mood disorders and depression may not have necessarily been detectable by preoperative questionnaires, especially if on treatment.
Our data showed that patients using psychotropic medications reported significantly lower MCS scores than the nonmedication group, both preoperatively and postoperatively. This finding was noted on subgroup analysis to be true for antidepressants (and for other psychotropic medications preoperatively). This result concurs with previous studies, which have demonstrated that foot and ankle patients exhibit a higher degree of anxious and depressive behavior and thoughts, both of which have been associated with heightened perception of pain intensity, chronicity of pain, and resulting disability. 28
On the other hand, it is interesting that the absolute improvement in MCS scores (Δ MCS) was comparable between the medication and nonmedication groups at 1 year postoperatively. Although patients in the medication group achieved the same amount of improvement in the MCS scores, they still had lower absolute MCS scores, before and after surgery, than the nonmedication group.
While the data did not detect any significant differences in VAS pain scale and physical function scale (PCS) data between the medication and nonmedication groups, there was a nonsignificant trend for higher PCS values in the nonmedication group, which may be a function of the difference in the number of patients in the groups. Future studies with larger populations may show this distinction in PCS to be significant. By contrast, the VAS pain values in the 2 groups were equivalent. Although depression and anxiety are associated with magnified perception of pain, this was not borne out in this patient population.
In this study, a significant association was found between psychotropic medication use and the development of superficial wound infections requiring antibiotic treatment. Although past studies have analyzed operative technique and patient age for their relationship with complications, psychotropic medication use has never been assessed. 7,15,19,29 Overall, 12.9% of the patients in the study group received antibiotics for superficial wound infections. No differences in prescribing rates were detected between the surgeons who performed the operations. This is higher than a rate of 5% reported by Catena et al 5 and 3% by O’Kane and Kilmartin. 21 An explanation for this finding is that superficial infection was determined by clinical history and physical examination; we did not culture wounds nor measure serum markers of infection when making a diagnosis of possible superficial infection, and we erred on the side of aggressively prescribing antibiotics. The higher rates in the psychotropic medication group may be because patients with psychiatric illness view their wounds differently 28 and, as such, are more likely to initiate conversations about antibiotics at postoperative visits.
Our study has strengths, including a sample population of 116 patients undergoing hammertoe surgery, which is one of the largest to date. 5,21,22,29 Our study population also had a high response rate to the postoperative patient-reported outcomes questionnaires. The patients in this study were demographically comparable to the populations examined in previous studies of hammertoe reconstruction with regard to gender and age, suggesting that our patients are likely a representative sample of patients who undergo hammertoe corrective surgery. 5,16,21,22,29 We also used validated questionnaires to determine the subjective assessment of pain and function (the VAS and SF-36 survey), allowing accurate comparison of the changes from preoperative to postoperative results. 18 To our knowledge, this is the first study to report pharmacotherapy data on patients undergoing hammertoe correction surgery.
As a prospective cohort study, there are inherent limitations. Our study was conducted by 2 different attendings surgeons at 2 separate institutions. Although this may increase the generalizability of our study, it may also add subtle or undetected variability in patient selection, operative technique, and postoperative protocols. Additional future studies may reveal greater differences based on larger sample sizes.
Conclusion
In this study, patients on psychotropic medications were equally likely to have satisfactory outcomes from forefoot reconstruction as nonmedication patients as judged by validated outcome measure of physical function and pain. Although this group had a lower absolute MCS score than the nonmedication group, they had comparable improvements in the MCS scores. Future studies may further elaborate on these results in larger groups of patients undergoing this and other reconstructive foot surgeries.
Supplemental Material
Supplemental Material, FAO944133-ICMJE for Effect of Psychotropic Medications on Hammertoe Reconstruction Outcomes by Samuel D. Maidman, Amalie E. Nash, Amanda Fantry, Shay Tenenbaum, Yahya Daoud, James Brodsky and Jason T. Bariteau in Foot & Ankle Orthopaedics
Footnotes
Ethics Approval: Ethical approval for this study was obtained from Emory University Institutional Review Board (ID: STUDY00000652).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Samuel D. Maidman, BA,  https://orcid.org/0000-0002-1376-5526
https://orcid.org/0000-0002-1376-5526
Amalie E. Nash, MD,  https://orcid.org/0000-0003-3205-7194
https://orcid.org/0000-0003-3205-7194
James Brodsky, MD,  https://orcid.org/0000-0002-2759-9418
https://orcid.org/0000-0002-2759-9418
References
- 1. Angirasa AK, Barrett MJ, Silvester D. SmartToe(R) implant compared with Kirschner wire fixation for hammer digit corrective surgery: a review of 28 patients. J Foot Ankle Surg. 2012;51(6):711–713. [DOI] [PubMed] [Google Scholar]
- 2. Bot AG, Menendez ME, Neuhaus V, Ring D. The influence of psychiatric comorbidity on perioperative outcomes after shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(4):519–527. [DOI] [PubMed] [Google Scholar]
- 3. Bressi SK, Marcus SC, Solomon PL. The impact of psychiatric comorbidity on general hospital length of stay. Psychiatr Q. 2006;77(3):203–209. [DOI] [PubMed] [Google Scholar]
- 4. Carstensen TB. The influence of psychosocial factors on recovery following acute whiplash trauma. Dan Med J. 2012;59(12):B4560. [PubMed] [Google Scholar]
- 5. Catena F, Doty JF, Jastifer J, Coughlin MJ, Stevens F. Prospective study of hammertoe correction with an intramedullary implant. Foot Ankle Int. 2014;35(4):319–325. [DOI] [PubMed] [Google Scholar]
- 6. Coughlin MJ. Lesser toe abnormalities. Instr Course Lect. 2003;52:421–444. [PubMed] [Google Scholar]
- 7. Coughlin MJ, Dorris J, Polk E. Operative repair of the fixed hammertoe deformity. Foot Ankle Int. 2000;21(2):94–104. [DOI] [PubMed] [Google Scholar]
- 8. Douzenis A, Seretis D, Nika S, et al. Factors affecting hospital stay in psychiatric patients: the role of active comorbidity. BMC Health Serv Res. 2012;12:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ellington JK, Anderson RB, Davis WH, Cohen BE, Jones CP. Radiographic analysis of proximal interphalangeal joint arthrodesis with an intramedullary fusion device for lesser toe deformities. Foot Ankle Int. 2010;31(5):372–376. [DOI] [PubMed] [Google Scholar]
- 10. Graven LJ, Grant J. The impact of social support on depressive symptoms in individuals with heart failure: update and review. J Cardiovasc Nurs. 2013;28(5):429–443. [DOI] [PubMed] [Google Scholar]
- 11. Hill J, Fillit H, Shah SN, del Valle MC, Futterman R. Patterns of healthcare utilization and costs for vascular dementia in a community-dwelling population. J Alzheimers Dis. 2005;8(1):43–50. [DOI] [PubMed] [Google Scholar]
- 12. Kagal UA, Torgal SS, Patil NM, Malleshappa A. Prevalence of the metabolic syndrome in schizophrenic patients receiving second-generation antipsychotic agents--a cross-sectional study. J Pharm Pract. 2012;25(3):368–373. [DOI] [PubMed] [Google Scholar]
- 13. Kennedy SA, Vranceanu AM, Nunez F, Ring D. Association between psychosocial factors and pain in patients with trigger finger. J Hand Microsurg. 2010;2(1):18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 15. Kramer WC, Parman M, Marks RM. Hammertoe correction with K-wire fixation. Foot Ankle Int. 2015;36(5):494–502. [DOI] [PubMed] [Google Scholar]
- 16. Kwon JY, De Asla RJ. The use of flexor to extensor transfers for the correction of the flexible hammer toe deformity. Foot Ankle Clin. 2011;16(4):573–582. [DOI] [PubMed] [Google Scholar]
- 17. Maeda T, Babazono A, Nishi T, Tamaki K. Influence of psychiatric disorders on surgical outcomes and care resource use in Japan. Gen Hosp Psychiatry 2014;36(5):523–527. [DOI] [PubMed] [Google Scholar]
- 18. Martin RL, Irrgang JJ, Lalonde KA, Conti S. Current concepts review: foot and ankle outcome instruments. Foot Ankle Int. 2006;27(5):383–390. [DOI] [PubMed] [Google Scholar]
- 19. Mueller CM, Boden SA, Boden AL, et al. Complication rates and short-term outcomes after operative hammertoe correction in older patients. Foot Ankle Int. 2018;39(6):681–688. [DOI] [PubMed] [Google Scholar]
- 20. Nakagawa R, Yamaguchi S, Kimura S, et al. Association of anxiety and depression with pain and quality of life in patients with chronic foot and ankle diseases. Foot Ankle Int. 2017;38(11):1192–1198. [DOI] [PubMed] [Google Scholar]
- 21. O’Kane C, Kilmartin T. Review of proximal interphalangeal joint excisional arthroplasty for the correction of second hammer toe deformity in 100 cases. Foot Ankle Int. 2005;26(4):320–325. [DOI] [PubMed] [Google Scholar]
- 22. Obrador C, Losa-Iglesias M, Becerro-de-Bengoa-Vallejo R, Kabbash CA. Comparative study of intramedullary hammertoe fixation. Foot Ankle Int. 2018;39(4):415–425. [DOI] [PubMed] [Google Scholar]
- 23. Pratt LA, Brody DJ, Gu Q. Antidepressant use among persons aged 12 and over: United States, 2011-2014. NCHS Data Brief. 2017(283):1–8. [PubMed] [Google Scholar]
- 24. Reynolds CF, 3rd, Cuijpers P, Patel V, et al. Early intervention to reduce the global health and economic burden of major depression in older adults. Annu Rev Public Health. 2012;33:123–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ring D, Kadzielski J, Fabian L, Zurakowski D, Malhotra LR, Jupiter JB. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006;88(9):1983–1988. [DOI] [PubMed] [Google Scholar]
- 26. Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA 2003;290(2):215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shakked R, McDonald E, Sutton R, Lynch MK, Nicholson K, Raikin SM. Influence of depressive symptoms on hallux valgus surgical outcomes. Foot Ankle Int. 2018;39(7):795–800. [DOI] [PubMed] [Google Scholar]
- 28. Shivarathre DG, Howard N, Krishna S, Cowan C, Platt SR. Psychological factors and personality traits associated with patients in chronic foot and ankle pain. Foot Ankle Int. 2014;35(11):1103–1107. [DOI] [PubMed] [Google Scholar]
- 29. Sung W, Weil L, Jr, Weil LS, Sr. Retrospective comparative study of operative repair of hammertoe deformity. Foot Ankle Spec. 2014;7(3):185–192. [DOI] [PubMed] [Google Scholar]
- 30. Vranceanu AM, Barsky A, Ring D. Psychosocial aspects of disabling musculoskeletal pain. J Bone Joint Surg Am. 2009;91(8):2014–2018. [DOI] [PubMed] [Google Scholar]
- 31. Zhao Y, Kuo TC, Weir S, Kramer MS, Ash AS. Healthcare costs and utilization for Medicare beneficiaries with Alzheimer’s. BMC Health Serv Res. 2008;8:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO944133-ICMJE for Effect of Psychotropic Medications on Hammertoe Reconstruction Outcomes by Samuel D. Maidman, Amalie E. Nash, Amanda Fantry, Shay Tenenbaum, Yahya Daoud, James Brodsky and Jason T. Bariteau in Foot & Ankle Orthopaedics