Abstract
Peroneal tendon tears are a common but under-recognized source of ankle pain and dysfunction. Recognition of the characteristic symptoms, physical findings, and imaging results of peroneal tendon tears is essential for accurate diagnosis and appropriate treatment. Acute, limited tears of a single peroneal tendon may be debrided and repaired. However, by the time operative treatment is undertaken, many tears of a single tendon are sufficiently advanced that the surgeon may need to consider excision of the nonviable segment and tenodesis of the damged tendon to the to the adjacent peroneal tendon. Irreparable tearing of both peroneal tendons may be treated with flexor tendon transfer and/or allograft reconstruction. This review article focuses on diagnosis and operative treatment of peroneal tendon tears, including the treatment algorithms, operative technique, and published outcomes.
Keywords: peroneal tendon tears, operative treatment, peroneus brevis, peroneus longus, tendon disorders, sports, tenodesis, tendon reconstruction
Introduction
For the patient who presents with lateral ankle pain, the differential diagnosis includes ankle sprain, lateral ligament instability, subfibular impingement, occult fracture of lateral process of the talus or anterior process of the calcaneus, osteochondral lesions of the lateral talar dome, peroneal tendonitis or subluxation, or peroneal tendon tears. These pathologies may coexist because they are frequently related to injury in inversion. Insidious onset of symptoms may delay presentation, and the wide array of possible causes may delay diagnosis.
The frequency of peroneal tendon tears has been reported by Sammarco and DiRaimondo. Of 47 patients with lateral ankle complaints, 36% were found to have attrition of the peroneus brevis tendon. 43 Although peroneal tendon tears are common, they are an under-recognized contributor to lateral ankle pain and dysfunction. A survey of 40 patients with peroneal tendon disorders found that only 60% of those were diagnosed at presentation. 10
Once the diagnosis is made, the clinician must weigh treatment options. Conservative management may be successful, depending on severity, chronicity, and the patient’s activity level. However, for the patient whose symptoms are not acceptably alleviated by a regimen of rest, anti-inflammatory medications, physical therapy, and bracing, operative treatment is often necessary. Recommendations and operative strategies have evolved to reflect our refined understanding of pathologies of the peroneal tendons as well as the evidence-based outcomes.
Pathophysiology
Peroneal tendon tears may be acute but the majority are chronic. 22 Although 20% to 60% of patients in the literature have been reported to have a sentinel event that precipitated their lateral ankle pain, the event is often remote, and the tears occur over an extended interval prior to the time of presentation. 3,22,39
Observational studies have shown tendon tears to occur at the tip of the fibula or at bony prominences where there is pressure against them (Figure 1A), 3,7,22,30,51 suggesting that the tears are mechanical in origin. Attenuation of the blood supply may also contribute to peroneal tendon tears. These same regions of mechanical stress are regions of hypovascularity, 35 which can deprive the tendon of nutrition, contributing to tear occurrence and propagation.
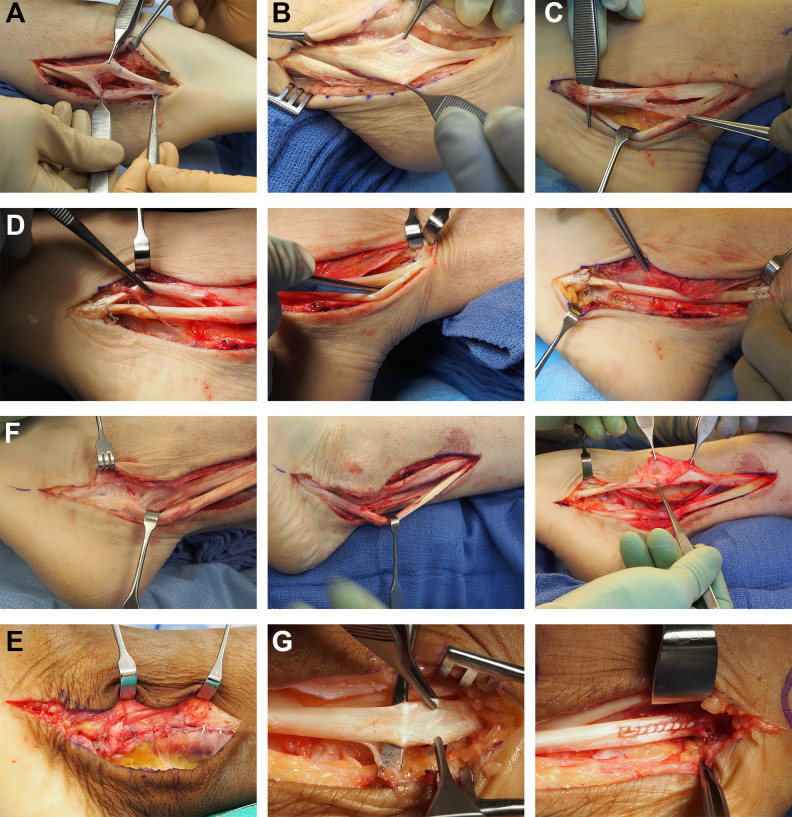
Figure 1.
Operative illustrations—peroneus brevis tears: (A) Example of a split tear of peroneus brevis due to subluxation over lateral malleolus. (B) Example of shredded fibers of peroneus brevis causing splaying of the tendon. (C, D) Unsalvageable brevis, proximal and distal tenodeses. (E) Retinacular reconstruction. (F) Failed tendon repair. This patient would have been better served by a tenodesis. (G) Mild peroneus tear, debrided and repaired.
Peroneus Brevis
For the peroneus brevis, the most common pattern of tendon tear is longitudinal and centered at the level of the tip of the fibula (Figure 1B). 3 At this location, the tendon acutely changes direction, increasing the mechanical stress on the tendon. In addition, compression of the brevis between the peroneus longus tendon and the fibula also increases the mechanical stress on the tendon. 21,22,29,47 Such mechanical stress can lead to fraying or longitudinal splitting, in this characteristic location (Figures 2). 22,37
Figure 2.

Pathophysiology: Splayed and scarred peroneus brevis due to subluxation.
The superior peroneal retinaculum may be a source of pathology even without frank tearing of the tendon. The retinacular tissue may become attenuated following inversion injuries of the ankle 5,22,43 and separation of the retinaculum from the lateral surface of the fibula, resulting in intra-sheath or frank subluxation of the tendons (Video IA). 37 This attenuation may also result from overstuffing due to intratendinous fibrosis, a low-lying peroneus brevis muscle, or a peroneus quartus muscle and tendon. 17,25 Tendinoscopic techniques have been advocated for cases of tendon instability without tendon tears. 56
Immunohistochemical staining of the vascular network of the peroneus brevis tendon has shown a nearly avascular region of the tendon at the level of the fibular groove, 35 suggesting a vascular contribution to tendon pathology.
Less common and less consistently symptomatic are the multiple small splits of the peroneus brevis just proximal to its insertion on the base of the fifth metatarsal, which are degenerative rather than mechanical. 5,47
Peroneus Longus
Tears of the peroneus longus are much less common than tears of the peroneus brevis. 16,41 They occur most often between the peroneal tubercle of the calcaneus and the cuboid tunnel, a zone of both mechanical stress and relative hypovascularity. 35,55 The common peroneal tendon sheath divides into separate sheaths at the peroneal tubercle. The longus is especially vulnerable to damage from enlargement or irregularity of the tubercle, though either tendon may be affected (Figure 3C). 5 -7,30,52 As the peroneus longus tendon courses distally to the plantar base of the first metatarsal, it makes an acute turn under the cuboid, increasing the mechanical stress on the tendon. Frequently, the peroneus longus tendon has an embedded os peroneum (Figure 3A), which is located at the cuboid tunnel and sometimes slightly proximal to it; it serves as a mechanical fulcrum, similar to other sesamoid bones in the body. Disorders of the os peroneum including fracture, osteophytes, or degenerative enlargement, sometimes called POPS (Painful Os Peroneum Syndrome) are an additional source of pathology for the peroneus longus tendon (Figure 3B). 3,42,51
Figure 3.
Longus tear: (A) Example of tear of the peroneus longus at the os peroneum. (B) Tear of the peroneus longus with fracture of the os peroneum. (C) Tear of the peroneus longus at the peroneal tubercle.
Diagnosis
Physical Examination
Since both peroneal tendons cross the ankle joint posteriorly, they are best examined with the ankle in plantarflexion. The position of both tendons lateral to the subtalar joint results in hindfoot eversion with muscle contraction. The insertion of the peroneus brevis on the base of the fifth metatarsal 12 makes it the strongest abductor of the forefoot. The peroneus longus inserts plantarly at the base of the first metatarsal 12 leading to plantarflexion of that ray and, to a lesser extent, abduction of the forefoot.
On exam, there may be enlargement of the tendon. This finding is present in 90% of patients with tears and more easily observed in brevis than in longus tears. 8,22 , 27 Swelling proximal to and at the lateral malleolus usually denotes a brevis tear, while swelling at and distal to the peroneal tubercle sometimes indicates a longus tear. 5
Pain with resisted eversion and tenderness to palpation are common but may also present with tendinitis. 8,22 Passive inversion of the hindfoot may provoke pain as well. Though subluxation of the tendons within their sheath is difficult to elicit in clinic, subluxation of the peroneal tendons over the posterior border of the fibula may be demonstrated on physical examination.
Peroneus brevis pathology may be distinguished from longus pathology by tenderness to palpation where the tendons diverge at the peroneal tubercle. The course of the longus is inferior to the brevis and it is palpable where it turns medially in the cuboid groove. The brevis, whose insertion is eccentric and dorsal on the fifth metatarsal base, is easily palpated as well. In this distal zone, each tendon can be palpated distinctly.
A thorough physical examination is essential because coexisting cavus deformity, ankle instability, or subfibular impingement may need to be operatively addressed at the same time as peroneal reconstruction. Sural neuritis or pain related to the Achilles tendon can mimic peroneal tendon symptoms. The clinical assessment is critical to identify the source of pain and contributing factors.
Imaging
Radiographs of the foot and ankle (weightbearing anteroposterior, lateral, and oblique views) can be useful to assess deformity and related osseous pathology. The diagnosis of a peroneus longus rupture can sometimes be made on radiographs, based on the position of the os peroneum, when present. 51 Approximately 20% of the population has an ossified os peroneum, visible on internal rotation oblique foot radiographs at the level of the calcaneocuboid joint. 1 Under physiologic conditions, the os peroneum should not appear proximal to the calcaneocuboid joint. 1 Migration of the os proximal to the calcaneocuboid joint is indicative of a tear of the peroneus longus tendon distal to the os peroneum. 53 If the tendon tear is associated with fragmentation of the os, the telltale fragment distraction can also be visualized on radiographs. 1,4,53
When peroneal tendon pathology is suspected and nonoperative treatment has not resulted in satisfactory results, magnetic resonance (MR) imaging is indicated (Figure 4D). Although the early literature reported inaccuracies of imaging, 3,22,39 MR imaging is currently a useful diagnostic aid, despite conflicting results regarding the reliability of this method. 9,31 -33 There is a consensus, however, that the utility is increased with better understanding of the “magic angle effect,” a phenomenon in MR imaging in which there is a factitious appearance of heterogeneity and increased signal in a tendon when it intersects the main magnetic vector at an angle of 55° (Figure 4B). 11,15,36 The peroneal tendons are susceptible to this artifact, especially at the tip of the lateral malleolus. Thus, it is essential that MR imaging of the peroneals include sections formatted in a parasagittal oblique plane that is perpendicular to the tendons where they turn at the lateral malleolus. Peroneus brevis tears will be diagnosed most easily in this plane (Figure 4A and B). Imaging the ankle in 20° of plantarflexion can also increase the accuracy of the study by separating the peroneal tendons in the sheath and decreasing the magic angle effect. 15,18,53,58
Figure 4.
Imaging of peroneal tendon tears. (A) Oblique coronal showing brevis tear. (B) Sagittal with plane of oblique coronal marked. (C) Peroneus longus tear on axial distal to malleolus. (D) MRI of tears of both longus and brevis.
Tears of the peroneus longus are seen well on axial images (Figure 4C). Additionally, it can be helpful to include sections in the oblique coronal plane perpendicular to the axis of the metatarsals to better visualize the extent of peroneus longus tendon tears in the midfoot. 36,58 A recent study by Res et al observed increased fatty infiltration of the muscle on MRI in cases of peroneus brevis tendon tears. 40 The clinical implications of this observation remain to be determined.
Despite the increasing sensitivity of MR imaging, the importance of correlation with a careful physical examination cannot be overstated. Tears found incidentally on imaging that are asymptomatic do not require treatment. 56
Ultrasound imaging for diagnosis of peroneal tendon pathology can be useful and accurate. 13,23,26 In a study of 30 patients (60 peroneal tendons) who underwent both dynamic ultrasound assessment and operative exploration, the sensitivity of ultrasonography in predicting a tendon tear was 100%. 13 The specificity was 85%, and the accuracy was 90%. 13 A practical limitation is that the technique is operator dependent and less readily available than MRI in many centers.
Treatment
Nonoperative
For most patients, nonoperative strategies are a reasonable first step in treatment. These may include a 4- to 8-week period of immobilization in a boot or brace, activity modification, physical therapy, lightweight ankle support brace, or a course of anti-inflammatory medications. Should those interventions fail to produce an acceptable improvement in symptoms, treatment may progress to operative intervention.
Tendonoscopy
In patients whose clinical presentation is convincing for a peroneal tendon tear but who have negative imaging, immobilization, activity modification, physical therapy, and anti-inflammatory medications are the first step. If those conservative therapies fail, however, the provider might consider operative intervention. The recent consensus statement by the Ankle and Foot Associates of the European Society of Sports traumatology, Knee surgery, and Arthroscopy (ESSKA-AFAS) advocates and reserves tendoscopy for these cases. 56
Algorithms to Guide Operative Intervention
Krause and Brodsky proposed a classification system and treatment algorithm. This was described based both on their experience with chronic peroneus brevis tendon tears and the increased mechanical load borne by the remaining tendon when more than half the original tendon is removed. Tears are divided into grades 1 and 2, depending on the extent of damage to the tendon’s cross-sectional area, observed intraoperatively, with a threshold of 50%. For grade 1 tears (less than 50% of the cross-sectional area), they advocated debridement and repair by tubularization (Figure 1G). For grade 2 tears (greater than 50% of the cross-sectional area), they advocate resection of the affected segment and tenodesis to the adjacent peroneus longus. 22 The rationale for excision and tenodesis has been reinforced by the authors’ observation that repaired brevis tendons are likely to later scar to the longus, causing pain because of restriction of tendon excursion.
Redfern and Myerson 39 expanded this algorithm to include peroneus longus tears and concomitant tears of both tendons. For tendons that are grossly intact, they recommended repair (analogous to Krause and Brodsky grade 1, though Redfern and Myerson did not specify a threshold of tendon integrity). If one tendon is completely torn and the other is functional with intact excursion, they recommended tenodesis of the tendon proximal to the tear. When there is limited muscle excursion of the intact peroneal due to scarring or when both tendons are torn, they recommended a tendon graft or tendon transfer. 39
Repair
Tendon repair consists of excision of the frayed and degenerated tissue and tubularization of the remaining tendon (Figure 1G). Krause and Brodsky 22 and Squires et al 47 advocate the use of absorbable suture to prevent persistent irritation from the sutures within the tendon sheath. Other authors promote nonabsorbable sutures for strength and durability. 39,41 Steel and DeOrio did not find the use of absorbable or nonabsorbable suture to influence patient outcomes. 49
It is essential to address underlying tendon instability and subluxation at the time of the procedure to prevent recurrence. 22 In every case, careful attention is paid to reconstruct the volume and tightness of the superior peroneal retinaculum so that the tendons are neither compressed nor able to subluxate. Use of a pants-over-vest repair allows the surgeon to progressively adjust the tension of the imbrication intraoperatively, rather than a figure-of-8 stitch, where the tension is set by the distance the stitch is positioned from the edge of the suture.
In a study of 20 patients with tears of the peroneus brevis, Krause and Brodsky reported 82% of patients undergoing debridement and repair were satisfied without reservations, compared with 66% of patients undergoing tenodesis. 22 However, overall satisfaction rate for both groups was greater than 90%. 22 They also reported favorable functional outcomes; patients in this series had an average American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot score of 85 postoperatively. 22 Similar satisfaction rates were shown in a study of 17 patients by Grasset et al, 14 13 of whom were treated with repair. Demetracopoulos et al 8 corroborated these promising results in a more recent study of 18 patients undergoing debridement and primary repair. There was a significant improvement in VAS pain scores at follow-up, and 94% returned to full sporting activity. 8 Steel and DeOrio looked specifically at return to sport in an assessment of 30 patients undergoing operative treatment of peroneal tendon tears, 29 of whom had debridement or repair the torn tendon. They found that only 46% were able to return to at least some sporting activity, whereas 42% were only able to perform ADLs. 49 The remaining 12% were not active in sports either before or after the surgery. They also reported that 54% continued to experience lateral ankle swelling and 31% had pain at rest. 49 A retrospective case series of 71 patients after peroneus brevis repair by Steginsky et al 50 showed 76% returning to preinjury activities, with 62% performing at their preinjury levels. Functional scores improved, and 85% of patients reported that they were satisfied and 91% would choose to have the procedure again. 50
Tenodesis
When the degenerated zone of the tendon exceeds or even approaches 50% of the tendon cross-sectional area, and/or is complex or very long, debridement and repair is more likely to produce a poor result. 22 The main reason for this is that a large area of tendon repair usually results in scarring and adhesion of the tendon to the sheath and the adjacent tendon. Once the tendon or tendons are scarred and immobile, the patient will have persistent pain. Debridement that results in extensive reduction of the tendon diameter also weakens it mechanically (Figure 1F). 20,51
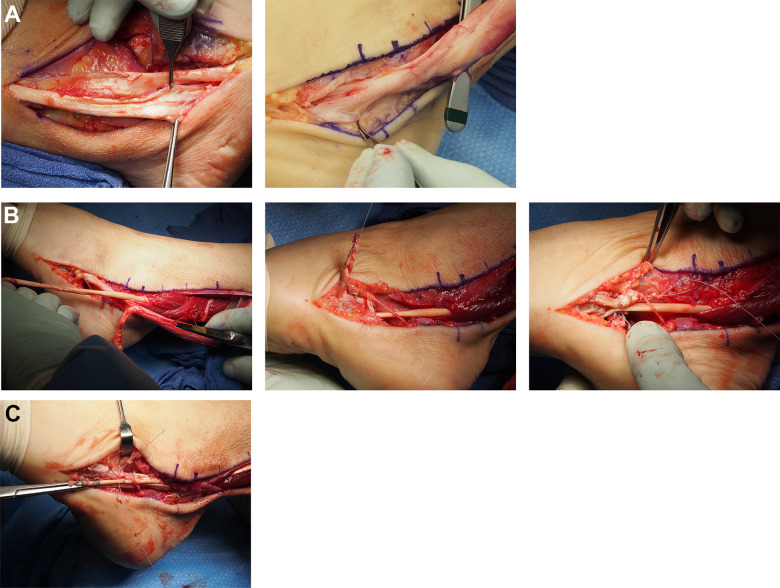
Tenodesis of the torn peroneal tendon to the intact one is the favored, and most common, solution because of the use of native tissue, rather than cadaver tissue, and the relative ease of the technique (Figures 1C and D). Once tenodesis is elected, the operative technique proceeds according to several key steps. At the sites of tenodesis, the adjacent tendon surfaces must be thoroughly debrided of synovium, and then gently roughened with the edge of the scalpel for improved adherence. For a torn peroneus brevis tendon, the proximal tenodesis transfers or attaches the brevis to the longus sufficiently proximal to the superior peroneal retinaculum such that the combined tendons at the tenodesis will not pass through the narrow zone of the retinaculum even in maximum inversion. Then the distal tenodesis is performed, to attach the longus tendon to the distal brevis near its insertion on the fifth metatarsal base (Figure 5A). Distal tenodesis at or near the brevis insertion maximizes postoperative eversion strength by combining the force of the 2 tendons to act through the insertion of the brevis on the fifth metatarsal base. Suturing the injured tendon both proximal and distal to the resected segment improves the power of eversion as well as the load-to-failure of the repair construct.
Figure 5.

Sural nerve. Preservation crossing branch of sural nerve (note distal tenodesis).
Tensioning of the tendons is important and is guided by the effect of ankle and hindfoot position, with the ankle in neutral and the hindfoot everted. The proximal end of the torn tendon can be slightly pulled distally, to stretch the musculotendinous unit and the distal end pulled proximally while suturing to offset possible stretching at the repair. Once both tenodeses are completed, the damaged section of the brevis is excised. Suture material should be nonabsorbable, preferably 2-0 in size, but not larger than -0. A complex running suture has been shown to be strongest for early motion 57 ; thus, this is our preferred suture pattern. We recommend placing the knots internally in the tenodesis, between the tendons, to prevent knot prominence, and using a suture that is a variant of a running mattress so that the suture does not loop over the tendons, in order to reduce pressure on the tendons because it is a relatively avascular zone of the tendons.
Retinacular reconstruction can be performed either after or between the first and second tenodesis (Figure 1E). We use pants-over-vest stitches of 2-0 nonabsorbable sutures, beginning on the posterior flap of the superior peroneal retinaculum, placing them under the subcutaneous tissue so that they are not palpable. The distance from the edge of the flap of the pants-over-vest sutures determines the volume and tightness of the retinaculum, and must be judged by the surgeon.
Our postoperative protocol following tenodesis includes splinting for 10-14 days, followed by cast immobilization for 6-10 weeks, then transition to a walking boot. Formal physical therapy begins after 3 months, but the patient is instructed in specific ROM exercises for the peroneal tendons.
Krause and Brodsky found favorable functional outcomes after operative treatment in a series of 20 patients, 9 of whom underwent tenodesis. 22 Forty-four percent of their patients returned to unlimited activities and 67% returned to work without restriction. 22
In partial or complete tears of the peroneus longus, the operative technique is almost the same as described for chronic tears of the brevis, with the exception of a distal tenodesis. Distal to the cuboid groove, the peroneus longus tendon is inaccessible and, therefore, not addressed operatively. It is best to position the tenodesis of the longus to the brevis proximal to the SPR. In Stockton and Brodsky’s series of patients with pathology of the os peroneum associated with tears of peroneus longus, the patients were treated with excision of the os and of the longus tendon containing it, with proximal tenodesis to the peroneus brevis. 51 AOFAS scores increased from an average of 61 preoperatively to 91.7 postoperatively. 51 SF-36 scores increased and VAS scores decreased as well.
Unreconstructable Tears of Both Peroneus Brevis and Peroneus Longus Tendons
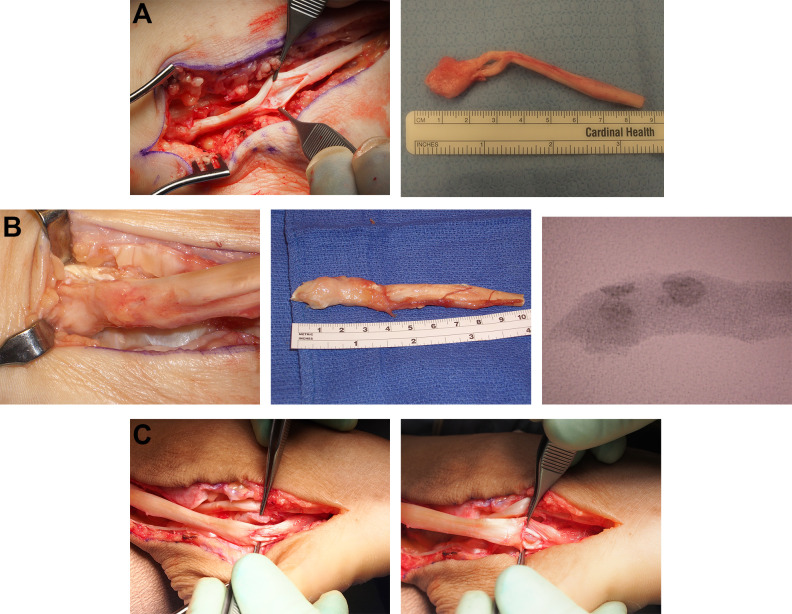
There are cases where the tendons are not amenable to reconstruction. In these instances, the tendons are grossly destroyed, enlarged from degeneration, and/or status-post prior surgery in which the remaining tendon is severely scarred or irreparably shredded (Figure 6A). Transfer of the flexor hallucis longus (FHL) or flexor digitorum longus (FDL) is a reconstructive option when both peroneal tendons are irreparably torn (Figure 6B). This technique involves harvest of the donor tendon at the level of the knot of Henry, passing it proximal and then posteriorly around the tibia and fibula, and attaching it distally to the remaining brevis tendon fibers and/or through a bone tunnel directly to the base of the fifth metatarsal with suture to itself in a loop or with a bio-interference screw.
Figure 6.
Concomitant tears of both peroneus longus and brevis. (A) Appearance of tears of both peroneus longus and peroneus brevis. (B) FHL transfer. (C) Allograft reconstruction.
Jockel and Brodsky reported a series of FHL or FDL tendon transfer for 8 patients who had severe concomitant tears of the peroneus longus and brevis that were not reconstructable. AOFAS scores increased from 64 to 86 after the surgery, with 7 of the 8 patients returning to their preoperative activity levels and reporting good or excellent results. 20 One patient developed a transient (<3-month) peroneal nerve palsy. 20 The authors noted their preference of FHL over FDL for the donor tendon. Another study of 9 patients found loss of approximately 25% of eversion strength and range of motion in patients after FHL or FDL transfer for concomitant tears. 45 Anatomic studies have shown FHL tendon length to be preferable to FDL for transfer. 44 Jeng et al 19 assessed the relative muscle strength and found FHL volume to be greater than FDL. Similarly, Silver et al 46 reported favorable strength of FHL over FDL transfer with comparable excursion between the two. Seybold et al 45 did not find differences in power, balance, or motion between the 2 groups after transfer.
Although FHL/FDL transfer has the advantage of using autologous tissue, the muscles may not be strong enough to be a durable and functional substitute for the peroneals, based on the physiologic principle that muscle power is proportional to the cross-sectional area of the muscle belly. As with tendon transfers for the tibialis posterior tendon, the use of the FHL or FDL is best considered an intercalary tendon bridge, rather than as a true transfer, and hence a proximal attachment of the native muscle-tendon unit to the recruited tendon. The FDL or FHL can bridge the gap between the proximal peroneal muscle-tendon unit, and the insertion on the fifth metatarsal base, in the case of unreconstructable and distal tears of both brevis and longus tendons. FHL and FDL transfers that do not include anastomosis to the proximal peroneal musculotendinous unit will be functionally weak for sustained repetitive eversion, that is, extended distances of walking. However, there are times when the proximal muscle has no excursion at all intraoperatively and it may not be beneficial to tenodese it.
Allograft Reconstruction
Cadaver allografts can be used to span the intercalary segment following excision of the torn native tendon (Figure 6C). Allograft reconstruction has been advocated over tendon transfer for patients who demonstrated intact proximal muscle excursion. This technique has been advocated to improve biomechanics, and reduce scarring leading to decreased range of motion. 28 In a clinical study of 14 patients who underwent peroneal or semitendinosus allograft reconstruction for irreparable tendon tears, Mook et al 28 found that patients returned to their preinjury activity levels, including professional dancing, running 5-km races, and cycling more than 25 miles. With an average follow-up of 17 months, there was a statistically significant improvement in pain, eversion strength, and function on the 12-item Short Form Health Survey and the Lower Extremity Functional Scale. It should be noted that only half had tears of both tendons, whereas half of these patients had isolated tears of the peroneus brevis. Thus, the groups were small, and the analysis was of heterogeneous groups. More than 25% of patients in the study experienced numbness in the sural nerve distribution (half of which were permanent). 28
A cadaver laboratory study concluded that allograft reconstruction restored tension in the distal segment of the tendon under physiologic loads. The allografts performed superiorly to tenodesis, which did not restore peroneal tendon tension, but there is no clinical correlation or corroboration at this time. 34
Patients with longstanding dysfunction or those who have previously undergone attempts at repair and reconstruction may have extensive scarring in this area. In these instances, staging the reconstruction with a silicone rod for bed preparation had been proposed to facilitate tendon gliding at final reconstruction. 39,48,59 Wapner et al 59 reported on 7 female patients with tears of both peroneal tendons who had been treated with at least 2 previous operative procedures before undergoing staged reconstruction with a Hunter rod, followed by FHL transfer. This technique was also reported by Raikin et al 38 to stimulate formation of a secondary tendon sheath to receive the FHL graft in the setting of extensive scarring. However, Redfern and Myerson 39 qualitatively noted unanticipated scarring even with the staged procedure. For this reason, staged procedures have lost their popularity and are not commonly performed.
Concomitant Procedures for Associated Pathologies
Numerous authors have advocated correction of underlying varus deformities at the time of peroneal tendon tear reconstruction. 21,49 -51 The association of a cavovarus deformity of the hindfoot and peroneal tendon tear is well-recognized, but there are currently no established criteria for severity or type of cavus or cavovarus deformity that warrant concomitant surgery, nor are there agreed on standards for that surgery. Some authors express concern regarding adhesion of reconstructed peroneal tendons to concomitant calcaneal osteotomy. 2,3,24,39,45
Other pathologies, such as lateral ankle instability, peroneal tubercle hypertrophy, osteochondral lesions of the ankle, and soft tissue ankle impingement, 6,22,41 , 47,50,52 may warrant operative repair at the time of peroneal reconstruction.
Complications
The most common complication following peroneal tendon surgery is skin numbness on the anterior side of the distal incision, due to unavoidable transection of small branches of the sural nerve (Figure 5). Skin healing issues are possible because of the thin skin and relative absence of subcutaneous tissue over the ankle and lateral hindfoot. Complications of the tendons themselves include scarring, recurrent tears, or degeneration of the remaining tendon, any of which may require revision surgery, often with allograft substitution of the nonviable segment.
Postoperative Rehabilitation Following Reconstruction of Peroneal Tendon Tears
There is a range of postoperative rehabilitation protocols described in the literature, but most authors have kept their patients nonweightbearing for a period between 2 and 6 weeks, depending on the extent of the procedure. Subsequently, weightbearing with immobilization in a cast or walking brace was begun. 8,22,50 In a meta-analysis of 49 studies of operative treatment of peroneal tendon tears, the median immobilization period ranged from 6 to 8 weeks across all treatment options. 54 Timing of physical therapy was highly variable. 8,22,50 There is not a significant difference in duration of immobilization or commencement of range of motion among operative treatment types. 54
Conclusion
Peroneal tendon injuries represent an under-recognized cause of lateral ankle pain and dysfunction. Assessment of peroneal tendon injuries reveals a wide breadth of injuries which are usually chronic but can have acute or subacute components. The range of pathology includes tears of one or both tendons, partial or complete tears, recurrent tears, and tears associated with concomitant pathologies. Treatment algorithms should account for the variety of disorders affecting the peroneal tendons. Further investigations will be required to better define indications for the variety of reconstructive options as well as the long-term functional outcomes.
Supplemental Material
Supplemental Material, FAO910407-ICMJE for Diagnosis and Operative Treatment of Peroneal Tendon Tears by Natalie R. Danna and James W. Brodsky in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: A supplemental video for this article is available online.
References
- 1. Bianchi S, Bortolotto C, Draghi F. Os peroneum imaging: normal appearance and pathological findings. Insights Imaging. 2017;8(1):59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bonnin M, Tavernier T, Bouysset M. Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am J Sports Med. 1997;25(5):699–703. [DOI] [PubMed] [Google Scholar]
- 3. Brandes CB, Smith RW. Characterization of patients with primary peroneus longus tendinopathy: a review of twenty-two cases. Foot Ankle Int. 2000;21(6):462–468. [DOI] [PubMed] [Google Scholar]
- 4. Brigido MK, Fessell DP, Jacobson JA, et al. Radiography and US of os peroneum fractures and associated peroneal tendon injuries: initial experience. Radiology. 2005;237(1):235–241. [DOI] [PubMed] [Google Scholar]
- 5. Brodsky JW, Toppins A. Postsurgical imaging of the peroneal tendons. Semin Musculoskelet Radiol. 2012;16(3):233–240. [DOI] [PubMed] [Google Scholar]
- 6. Bruce WD, Christofersen MR, Phillips DL. Stenosing tenosynovitis and impingement of the peroneal tendons associated with hypertrophy of the peroneal tubercle. Foot Ankle Int. 1999;20(7):464–467. [DOI] [PubMed] [Google Scholar]
- 7. Celikyay F, Yuksekkaya R, Almus F, Bilgic E. Tenosynovitis of the peroneal tendons associated with a hypertrophic peroneal tubercle: radiography and MRI findings. BMJ Case Rep. 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Demetracopoulos CA, Vineyard JC, Kiesau CD, Nunley JA. Long-term results of debridement and primary repair of peroneal tendon tears. Foot Ankle Int. 2014;35(3):252–257. [DOI] [PubMed] [Google Scholar]
- 9. DiGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000;21(10):809–815. [DOI] [PubMed] [Google Scholar]
- 10. Dombek MF, Lamm BM, Saltrick K, Mendicino RW, Catanzariti AR. Peroneal tendon tears: a retrospective review. J Foot Ankle Surg. 2003;42(5):250–258. [DOI] [PubMed] [Google Scholar]
- 11. Erickson SJ, Cox IH, Hyde JS, Carrera GF, Strandt JA, Estkowski LD. Effect of tendon orientation on MR imaging signal intensity: a manifestation of the “magic angle” phenomenon. Radiology. 1991;181(2):389–392. [DOI] [PubMed] [Google Scholar]
- 12. Gomes MDR, Pinto AP, Fabián AA, Gomes TJM, Navarro A, Oliva XM. Insertional anatomy of peroneal brevis and longus tendon—a cadaveric study. Foot Ankle Surg. 2019;25(5):636–639. [DOI] [PubMed] [Google Scholar]
- 13. Grant TH, Kelikian AS, Jereb SE, McCarthy RJ. Ultrasound diagnosis of peroneal tendon tears: a surgical correlation. J Bone Joint Surg Am. 2005;87(8):1788–1794. [DOI] [PubMed] [Google Scholar]
- 14. Grasset W, Mercier N, Chaussard C, Carpentier E, Aldridge S, Saragaglia D. The surgical treatment of peroneal tendinopathy (excluding subluxations): a series of 17 patients. J Foot Ankle Surg. 2012;51(1):13–19. [DOI] [PubMed] [Google Scholar]
- 15. Gyftopoulos S, Bencardino JT. Normal variants and pitfalls in MR imaging of the ankle and foot. Magn Reson Imaging Clin N Am. 2010;18(4):691–705. [DOI] [PubMed] [Google Scholar]
- 16. Heckman DS, Reddy S, Pedowitz D, Wapner KL, Parekh SG. Operative treatment for peroneal tendon disorders. J Bone Joint Surg Am. 2008;90(2):404–418. [DOI] [PubMed] [Google Scholar]
- 17. Highlander P, Pearson KT, Burns P. Magnetic resonance imaging analysis of peroneal tendon pathology associated with low-lying peroneus Brevis muscle belly: a case-control study. Foot Ankle Spec. 2015;8(5):347–353. [DOI] [PubMed] [Google Scholar]
- 18. Horn DB, Meyers S, Astor W. True pathologic abnormality versus artifact. J Am Podiatr Med Assoc. 2015;105(5):443–450. [DOI] [PubMed] [Google Scholar]
- 19. Jeng CL, Thawait GK, Kwon JY, et al. Relative strengths of the calf muscles based on MRI volume measurements. Foot Ankle Int. 2012;33(5):394–399. [DOI] [PubMed] [Google Scholar]
- 20. Jockel JR, Brodsky JW. Single-stage flexor tendon transfer for the treatment of severe concomitant peroneus longus and brevis tendon tears. Foot Ankle Int. 2013;34(6):666–672. [DOI] [PubMed] [Google Scholar]
- 21. Karlsson J, Wiger P. Longitudinal split of the peroneus brevis tendon and lateral ankle instability: treatment of concomitant lesions. J Athl Train. 2002;37(4):463–466. [PMC free article] [PubMed] [Google Scholar]
- 22. Krause JO, Brodsky JW. Peroneus brevis tendon tears: pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int. 1998;19(5):271–279. [DOI] [PubMed] [Google Scholar]
- 23. Lee SJ, Jacobson JA, Kim SM, et al. Ultrasound and MRI of the peroneal tendons and associated pathology. Skeletal Radiol. 2013;42(9):1191–1200. [DOI] [PubMed] [Google Scholar]
- 24. Manoli A, Graham B. The subtle cavus foot, “the underpronator,” a review. Foot Ankle Int. 2005;26(3):256–263. [DOI] [PubMed] [Google Scholar]
- 25. Mirmiran R, Squire C, Wassell D. Prevalence and role of a low-lying peroneus brevis muscle belly in patients with peroneal tendon pathologic features: a potential source of tendon subluxation. J Foot Ankle Surg. 2015;54(5):872–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Molini L, Bianchi S. US in peroneal tendon tear. J Ultrasound. 2014;17(2):125–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Molloy R, Tisdel C. Failed treatment of peroneal tendon injuries. Foot Ankle Clin. 2003;8(1):115–129. [DOI] [PubMed] [Google Scholar]
- 28. Mook WR, Parekh SG, Nunley JA. Allograft reconstruction of peroneal tendons: operative technique and clinical outcomes. Foot Ankle Int. 2013;34(9):1212–1220. [DOI] [PubMed] [Google Scholar]
- 29. Munk RL, Davis PH. Longitudinal rupture of the peroneus brevis tendon. J Trauma. 1976;16(10):803–806. [DOI] [PubMed] [Google Scholar]
- 30. Ochoa LM, Banerjee R. Recurrent hypertrophic peroneal tubercle associated with peroneus brevis tendon tear. J Foot Ankle Surg. 2007;46(5):403–408. [DOI] [PubMed] [Google Scholar]
- 31. O’Neill PJ, Van Aman SE, Guyton GP. Is MRI adequate to detect lesions in patients with ankle instability? Clin Orthop Relat Res. 2010;468(4):1115–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Park HJ, Cha SD, Kim HS, et al. Reliability of MRI findings of peroneal tendinopathy in patients with lateral chronic ankle instability. Clin Orthop Surg. 2010;2(4):237–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Park HJ, Lee SY, Park NH, Rho MH, Chung EC, Kwag HJ. Accuracy of MR findings in characterizing peroneal tendons disorders in comparison with surgery. Acta Radiol. 2012;53(7):795–801. [DOI] [PubMed] [Google Scholar]
- 34. Pellegrini MJ, Glisson RR, Matsumoto T, et al. Effectiveness of allograft reconstruction vs tenodesis for irreparable peroneus brevis tears: a cadaveric model. Foot Ankle Int. 2016;37(8):803–808. [DOI] [PubMed] [Google Scholar]
- 35. Petersen W, Bobka T, Stein V, Tillmann B. Blood supply of the peroneal tendons: injection and immunohistochemical studies of cadaver tendons. Acta Orthop Scand. 2000;71(2):168–174. [DOI] [PubMed] [Google Scholar]
- 36. Rademaker J, Rosenberg ZS, Delfaut EM, et al. Tear of the peroneus longus tendon: MR imaging features in nine patients. Radiology. 2000;214(3):700–704. [DOI] [PubMed] [Google Scholar]
- 37. Raikin SM, Elias I, Nazarian LN. Intrasheath subluxation of the peroneal tendons. J Bone Joint Surg Am. 2008;90(5):992–999. [DOI] [PubMed] [Google Scholar]
- 38. Raikin SM, Schick FA, Karanjia HN. Use of a hunter rod for staged reconstruction of peroneal tendons. J Foot Ankle Surg. 2016;55(1):198–200. [DOI] [PubMed] [Google Scholar]
- 39. Redfern D, Myerson M. The management of concomitant tears of the peroneus longus and brevis tendons. Foot Ankle Int. 2004;25(10):695–707. [DOI] [PubMed] [Google Scholar]
- 40. Res LCS, Dixon T, Lubberts B, et al. Peroneal tendon tears: we should consider looking at the muscle instead. J Am Acad Orthop Surg. 2018;26(22):809–815. [DOI] [PubMed] [Google Scholar]
- 41. Roster B, Michelier P, Giza E. Peroneal tendon disorders. Clin Sports Med. 2015;34(4):625–641. [DOI] [PubMed] [Google Scholar]
- 42. Sammarco GJ. Peroneus longus tendon tears: acute and chronic. Foot Ankle Int. 1995;16(5):245–253. [DOI] [PubMed] [Google Scholar]
- 43. Sammarco GJ, Diraimondo CV. Chronic peroneus brevis tendon lesions. Foot Ankle Int. 1989;9(4):163–170. [DOI] [PubMed] [Google Scholar]
- 44. Seybold JD, Campbell JT, Jeng CL, Myerson MS. Anatomic comparison of lateral transfer of the long flexors for concomitant peroneal tears. Foot Ankle Int. 2013;34(12):1718–1723. [DOI] [PubMed] [Google Scholar]
- 45. Seybold JD, Campbell JT, Jeng CL, Short KW, Myerson MS. Outcome of lateral transfer of the FHL or FDL for concomitant peroneal tendon tears. Foot Ankle Int. 2016;37(6):576–581. [DOI] [PubMed] [Google Scholar]
- 46. Silver RL, de la Garza J, Rang M. The myth of muscle balance. A study of relative strengths and excursions of normal muscles about the foot and ankle. J Bone Joint Surg Br. 1985;67(3):432–437. [DOI] [PubMed] [Google Scholar]
- 47. Squires N, Myerson MS, Gamba C. Surgical treatment of peroneal tendon tears. Foot Ankle Clin. 2007;12(4):675–695, vii. [DOI] [PubMed] [Google Scholar]
- 48. Stamatis ED, Karaoglanis GC. Salvage options for peroneal tendon ruptures. Foot Ankle Clin. 2014;19(1):87–95. [DOI] [PubMed] [Google Scholar]
- 49. Steel MW, DeOrio JK. Peroneal tendon tears: return to sports after operative treatment. Foot Ankle Int. 2007;28(1):49–54. [DOI] [PubMed] [Google Scholar]
- 50. Steginsky B, Riley A, Lucas DE, Philbin TM, Berlet GC. Patient-reported outcomes and return to activity after peroneus brevis repair. Foot Ankle Int. 2016;37(2):178–185. [DOI] [PubMed] [Google Scholar]
- 51. Stockton KG, Brodsky JW. Peroneus longus tears associated with pathology of the os peroneum. Foot Ankle Int. 2014;35(4):346–352. [DOI] [PubMed] [Google Scholar]
- 52. Taki K, Yamazaki S, Majima T, Ohura H, Minami A. Bilateral stenosing tenosynovitis of the peroneus longus tendon associated with hypertrophied peroneal tubercle in a junior soccer player: a case report. Foot Ankle Int. 2007;28(1):129–132. [DOI] [PubMed] [Google Scholar]
- 53. Taljanovic MS, Alcala JN, Gimber LH, Rieke JD, Chilvers MM, Latt LD. High-resolution US and MR imaging of peroneal tendon injuries—erratum. RadioGraphics. 2015;35(2):651. [DOI] [PubMed] [Google Scholar]
- 54. van Dijk PA, Lubberts B, Verheul C, DiGiovanni CW, Kerkhoffs GMMJ. Rehabilitation after surgical treatment of peroneal tendon tears and ruptures. Knee Surg Sport Traumatol Arthrosc. 2016;24(4):1165–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. van Dijk PA, Madirolas FX, Carrera A, Kerkhoffs GMMJ, Reina F. Peroneal tendons well vascularized: results from a cadaveric study. Knee Surg Sport Traumatol Arthrosc. 2016;24(4):1140–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. van Dijk PA, Miller D, Calder J, et al. The ESSKA-AFAS international consensus statement on peroneal tendon pathologies. Knee Surg Sport Traumatol Arthrosc. 2018;26(1):3096–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wagner E, Ortiz C, Wagner P, Guzmán-Venegas R. Biomechanical evaluation of various suture configurations in side-to-side tenorrhaphy. J Bone Joint Surg Am. 2014;96(3):232–236. [DOI] [PubMed] [Google Scholar]
- 58. Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. RadioGraphics. 2005;25(3):587–602. [DOI] [PubMed] [Google Scholar]
- 59. Wapner KL, Taras JS, Lin SS, Chao W. Staged reconstruction for chronic rupture of both peroneal tendons using hunter rod and flexor hallucis longus tendon transfer: a long-term followup study. Foot Ankle Int. 2006;27(8):591–597. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO910407-ICMJE for Diagnosis and Operative Treatment of Peroneal Tendon Tears by Natalie R. Danna and James W. Brodsky in Foot & Ankle Orthopaedics