Abstract
Background:
Traditionally, a lengthy period of nonweightbearing is required following arthrodesis of the first tarsometatarsal (TMT) joint in order to provide a stable healing environment for the bones. The goal of this research was to determine the resistance to plantar gapping of 2 locked intramedullary devices and a medial plate with crossing screw, all specifically designed for hallux valgus correction, and compare them to traditional 2–crossing screw fixation under a cyclic testing protocol. We hypothesized the locked intramedullary devices and the medial plate with crossing screw would better resist plantar gapping.
Methods:
Forty cadaver specimens received 1 of 4 operative treatments: a locked intramedullary device with 2 points of fixation in the cuneiform, a locked intramedullary device with 1 point of fixation in the cuneiform, a medial plate with crossing screw, or 2 crossing screws. We applied dorsiflexion bending forces to the first TMT joint using a cadaveric fatigue model for 20 000 cycles. The plantar gap between the metatarsal and cuneiform was measured at the beginning and end of cyclic testing. Thirty-six specimens were included in the final data set.
Results:
Both locked intramedullary device groups and the medial plate with crossing screw group exhibited significantly less gap widening compared to the 2–crossing screw group (vs 3-hole intramedullary device, P = .014; vs 4-hole intramedullary device, P = .010; and vs medial plate with crossing screw, P = .044). The intramedullary device groups were the most stable during the cyclic fatigue test, exhibiting the smallest gap widening. The medial plate with crossing screw fixation was also more stable than crossing screws in the cyclic fatigue model.
Conclusions:
The locked intramedullary devices and medial plate with crossing screw resisted plantar gapping better than 2 crossing screws when used for first TMT arthrodesis.
Clinical Relevance:
These results indicate that locked intramedullary devices and medial plates with crossing screws may promote superior bone healing and may better tolerate early weightbearing compared with 2 crossing screws.
Keywords: hallux valgus, arthrodesis, biomechanics, intramedullary nail, medial locking plate, crossing screws, tarsometatarsal, bunion, Lapidus procedure
Introduction
Historically, standard postoperative care following first tarsometatarsal (TMT) arthrodesis generally involved a prolonged period of nonweightbearing of approximately 6-8 weeks. 2,13 Lengthy periods of nonweightbearing are commonly associated with postoperative complications. 14 However, there are encouraging reports that early weightbearing can be achieved following first TMT arthrodesis. 2,3,14 Stable constructs will be crucial in order for early weightbearing to become the new standard of care.
Bone healing requires a sufficient blood supply and mechanical stability. 6 By increasing stability across a fracture site, revascularization and new bone formation can occur. 6,16 Direct fracture healing occurs under the conditions of fracture stability coupled with anatomic alignment. 12 Contact healing can take place if the gap between the bone fragments is small (less than 0.01 mm) whereas gap healing will take place if the gap is slightly larger (less than 1 mm). 12 Indirect fracture healing occurs when there is interfragmentary motion or lack of contact that stimulates the formation of a callus. 12,16 An excessive gap or too much interfragmentary motion can lead to delayed union or nonunion. 7,12 Compression across the fusion site can promote direct bone healing by reducing the interfragmentary gap and motion. 8 This may lessen the amount of tissue required to bridge the bone fragments, which may lead to faster healing. 9
Given that interfragmentary gap and interfragmentary motion can be harmful to the healing process of bone, the goal of this research was to determine the resistance to plantar gapping of 3 modern hallux valgus fixation constructs and compare them to traditional crossing screw fixation under a lengthy cyclic testing protocol. We hypothesized the locked intramedullary devices and the medial plate with crossing screw would better resist plantar gapping.
Methods
Forty fresh-frozen, unmatched cadaver below-knee extremities were obtained via an accredited AATB donation program and were evenly assigned to 1 of 4 groups:
Four-hole locked intramedullary device with 2 points of fixation in the medial cuneiform (4-Hole Phantom Intramedullary Nail; Paragon 28, Englewood, CO; Figure 1A).
Three-hole locked intramedullary device with 1 point of fixation in the medial cuneiform (3-Hole Phantom Intramedullary Nail; Paragon 28; Figure 1B).
Medial plate with crossing screw (Gorilla Lapidus Plate; Paragon 28; Figure 1C).
Two crossing screws (Mini-Monster cannulated screws; Paragon 28: Figure 1D).
Figure 1.
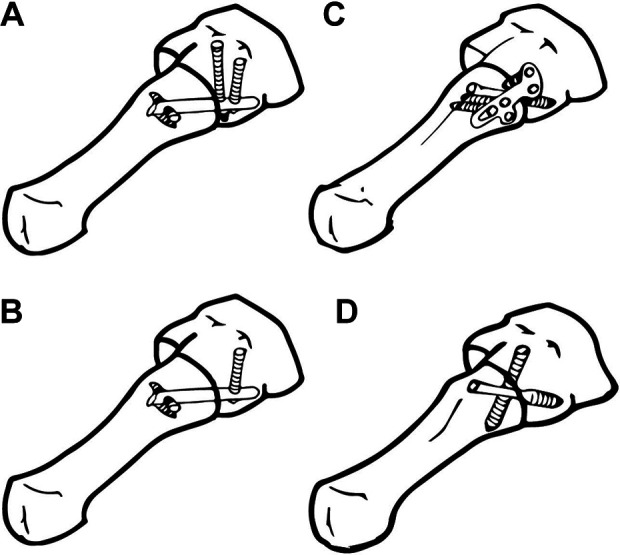
Illustrations of the 4 fixation groups: (A) 4-hole intramedullary device, (B) 3-hole intramedullary device, (C) medial plate with crossing screw, and (D) crossing screws.
Only right feet, age 65 years or younger at the time of death, were eligible for the experiment. Specimens were allocated to testing groups solely based on the order of arrival from the tissue bank with no prior knowledge of the characteristics of the specimens, outside of the eligibility requirements. Existing hallux valgus was not a requirement for inclusion into the experiment. Two of the 40 specimens were excluded after implantation because of poor bone quality. The data files from another 2 specimens became corrupt and unusable after testing was complete. Thus, 36 specimens successfully completed the experiment and are reported on in this article.
Relative bone quality for each specimen was assessed by measuring the average cortical bone hardness of the medial malleolus using an indentation technique. 17 A trocar tip was attached to a handheld force gauge and firmly pressed into bone until the cortex was breached (M5-500 Force Gauge; Mark-10, Long Island, NY). The peak force required to puncture the cortex was recorded. This was repeated 3 times per specimen.
Each fixation group contained both male and female specimens with no significant difference found between the gender composition of the groups (P = .752). Additionally, no other significant differences were found in the characteristics of the specimens when divided by fixation type (Table 1).
Table 1.
Specimen Characteristics at Time of Death by Fixation Group.a
| 4-Hole IM Device (n = 8) |
3-Hole IM Device (n = 9) |
Medial Plate With Crossing Screw (n = 10) |
Crossing Screws (n = 9) |
P Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Age, y | 52.0 | 17.2 | 60.3 | 4.2 | 60.7 | 3.5 | 55.0 | 10.7 | .223 |
| Height, cm | 170.8 | 9.2 | 166.5 | 9.4 | 173.0 | 10.9 | 173.0 | 7.7 | .422 |
| Weight, kg | 69.2 | 18.0 | 62.3 | 18.3 | 80.4 | 21.1 | 76.3 | 18.2 | .201 |
| Body mass index | 23.9 | 5.1 | 22.3 | 6.0 | 26.7 | 5.5 | 26.0 | 8.4 | .447 |
| Bone hardness, N | 136.8 | 65.2 | 127.1 | 51.0 | 146.7 | 110.3 | 139.7 | 62.7 | .957 |
| Moment arm, mm | 56.5 | 6.2 | 52.8 | 3.2 | 53.2 | 2.8 | 54.0 | 4.2 | .289 |
| Joint height, mm | 28.2 | 5.4 | 27.8 | 4.8 | 32.3 | 2.4 | 29.8 | 3.3 | .081 |
| Preoperative IMA, degrees | 8.0 | 1.0 | 8.5 | 1.8 | 7.8 | 3.8 | 7.8 | 2.1 | .913 |
Abbreviations: IM, intramedullary; IMA, intermetatarsal angle.
a The number of specimens for each group included in the analysis is in parentheses.
Operative Technique
All specimens were implanted by a surgeon (L.B.) familiar with the study devices and associated operative techniques. Hardware was sized to each specific specimen, where applicable.
For all specimens, a 4-cm dorsomedial incision was made across the first TMT. Small variations in incision size were necessary, both because of specimen size and type of fixation being employed. Commercially available cutting guides specifically designed for the Lapidus procedure were used to ensure consistent joint resection via a sagittal saw (Lapidus Cut Guide System; Paragon 28). Because of anatomic variation, some specimens required additional free-hand saw cuts to complete joint resection. The joint was provisionally fixed with a K-wire passed distal-medial-plantar to proximal-lateral-dorsal. Group-specific operative techniques are detailed in the following paragraphs.
Four-Hole Locked Intramedullary Device
After provisional fixation, a guidewire for device positioning was determined by a jig system that targets the proximal-plantar aspect of the medial cuneiform from a start point set approximately 23 mm distal to the TMT joint just lateral to the midline. After the guidewire placement and length measurement, a drill was used to cut a tunnel for device insertion. Two threaded pegs were inserted through the proximal-medial and proximal-lateral aspects of the medial cuneiform and advanced through the proximal holes of the device. All intramedullary devices were compressed to 100 N through a torque indicating driver. A single threaded peg was inserted through the medial aspect of the metatarsal into the distal hole of the device. A single locking screw was inserted through the distal end of the device, at an oblique angle, and advanced to the plantar aspect of the first metatarsal.
Three-Hole Locked Intramedullary Device
The procedure for the specimens that received the 3-hole locked intramedullary device was similar to those specimens that received the 4-hole locked intramedullary device, with the exception that only a single threaded peg, which matched the proximal-medial hole of the 4-hole device, was inserted into the cuneiform.
Medial Plate With Crossing Screw
Once provisional fixation was in place, the plate was positioned along the first ray and temporarily held with olive wires. A partially threaded lag screw was inserted from the dorsal metatarsal into the medial cuneiform using a jig to achieve consistent position. Two locking screws were placed on each side of the joint and a nonlocking screw was placed in the first metatarsal (Figure 2).
Figure 2.

Final placement of a medial plate with crossing screw.
Crossing Screws
After provisional fixation, a guidewire for a partially threaded 4.0-mm cannulated screw was placed across the first TMT joint from dorsal-distal to plantar-proximal at the lateral aspect of the joint. Countersinking, measurement, and drilling were performed prior to placing a partially threaded screw. The provisional fixation was removed prior to seating the partially threaded screw. A fully threaded 4.0-mm cannulated screw was placed from dorsal-proximal to plantar-distal on the medial side of the joint using the steps outlined above for the first screw.
Biomechanical Testing
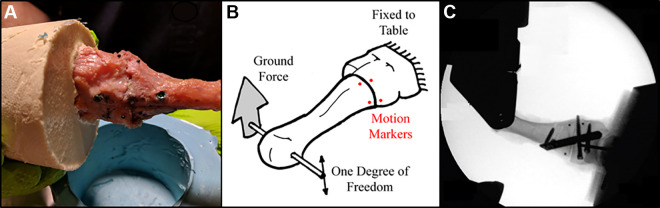
The first ray was dissected en bloc along with the intermediate cuneiform. All dissections were performed carefully as to not disrupt the soft tissue attachments between the first metatarsal, medial cuneiform, intermediate cuneiform, and navicular. Trocar pins were placed through the navicular and through the intermediate cuneiform, thus keeping the medial cuneiform and the naviculocuneiform joint free from mounting hardware. The specimen was cast in a silicone mold with a urethane resin for adaption to the test frame (InstaCast; Douglas & Sturgess, San Francisco, CA). The construct was installed on a test frame with a custom-designed test fixture to apply cantilever bending forces at the head of the metatarsal as displayed in Figure 3. The resin potting surrounding the navicular was rigidly fixed to the table. The metatarsal was angled 15 degrees from horizontal to simulate the declination angle during stance. A hard steel axle was placed through the metatarsal head and attached to rotational bearings, to ensure that the specimens were loaded in a consistent manner. This axle constrained the motion of the metatarsal to a single plane of freedom. The motion of the cuneiform was left unconstrained. Force was applied by the test frame actuator (858 Mini Bionix II; MTS System Corporation, Eden Prairie, MN). Radiopaque beads were used as motion markers and placed on each side of the first TMT joint. 5
Figure 3.
(A) Potted specimen with motion marker beads. (B) Schematic illustration of the biomechanical model. The model included a ground force applied through a steel axle at the metatarsal head and rigid fixation of the navicular to the table. The motion of the cuneiform was unconstrained. (C) Fluoroscopic image of specimen and test frame during the setup process.
Dorsiflexion cantilever bending was performed in a nondestructive cyclic fatigue profile. Loading from 10 to 40 N at 1 Hz was performed for 20 000 cycles. These loading parameters were primarily based on previous work and used to simulate a postoperative patient partially weightbearing in a healing shoe. 4 Fluoroscopic images of marker positions were collected at the start and end of each cyclic trial (OEC 9800; GE, Salt Lake City, UT; Figure 4). Dorsiflexion force and displacement of the metatarsal head was recorded by the test frame actuator and software at an acquisition rate of 20 Hz.
Figure 4.
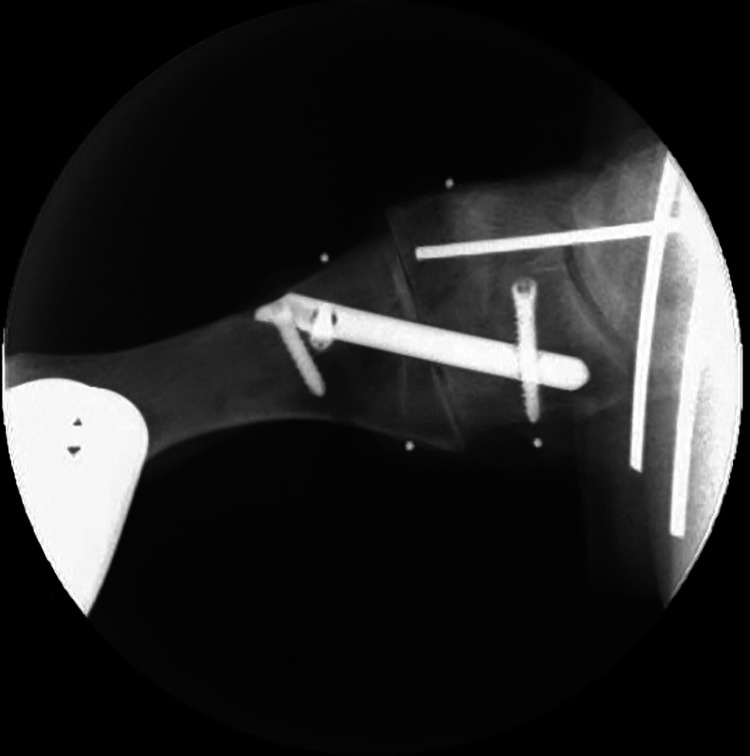
Fluoroscopic image of a specimen with a 3-hole intramedullary device during cyclic testing.
Outcome Measures and Statistical Analysis
Cyclic fatigue measures included initial plantar gap, final plantar gap, and gap widening. Initial gap was defined as the space between plantar aspects of the metatarsal and the medial cuneiform before cyclic fatigue. Gap widening was defined as the change in distance between the motion markers over the fatigue trial. Final gap was calculated as the initial plantar gap plus gap widening. These separation distances were collected from the fluoroscopic imaging under zero dorsiflexion loading. ImageJ (National Institute of Health) was used to measure each fluoroscopic image of interest. A scaling factor was used to convert image pixels to millimeters. A test was performed to determine the accuracy of the methods described above. A foam block with motion markers was attached to the test frame, and the test frame was moved in incremental amounts. Our accuracy was calculated as the average difference between distances calculated by our method and displacement measured by the test frame. The accuracy of our study methods was determined to be 0.05 mm.
Statistical analysis was performed using RStudio (v1.2.1335, Boston, MA). Means and standard deviations were calculated for each of the 4 fixation groups. Ninety-five percent confidence intervals were calculated, where appropriate. Statistical significance was set at alpha equal to .05. Regression models were used to test the effects of age, height, weight, body mass index, bone hardness, moment arm, joint height, preoperative intermetatarsal angle, and gender on the gap measures. Fisher exact test was used for count data. Group means were analyzed with analysis of variance. The reported P values from the subsequent pairwise comparisons were adjusted with Tukey honestly significant difference correction for multiple comparisons. An a priori power analysis was not conducted for this study.
Results
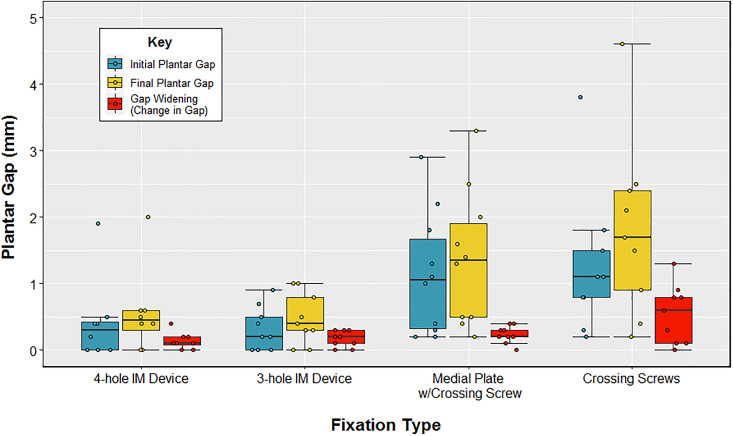
The results from our cyclic fatigue trials are displayed in Figure 5 and Tables 2 and 3. We were unable to find any differences in moment arm length between groups (Table 1), ensuring the specimens were loaded in a consistent manner. We were unable to show significant differences between the fixation groups for initial gap (P > .05 for all pairs; Table 3). Final gap was significantly smaller for both intramedullary device groups compared with crossing screws (vs 3-hole, P = .022, and vs 4-hole, P = .043). Final gap was not significantly different between either intramedullary device group and the medial plate with crossing screw group (vs 3-hole, P = .176, and vs 4-hole, P = .274). We were unable to detect a significant difference for final gap between the 3-hole intramedullary device and 4-hole intramedullary device groups either (P = .998). Gap widening, or change in gap over the 20 000-cycle fatigue test, was significantly larger for the crossing screw group compared to all other groups (vs 3-hole intramedullary device, P = .014; vs 4-hole intramedullary device, P = .010; and vs medial plate with crossing screw, P = .044). We were unable to detect significant differences in gap widening between the medial plate with crossing screw and 3-hole intramedullary device (P = .944) or 4-hole intramedullary device (P = .859).
Figure 5.
Boxplot for each fixation group for initial plantar gap, final plantar gap and gap widening. IM, intramedullary.
Table 2.
Results of Cyclic Testing.a
| 4-Hole IM Device | 3-Hole IM Device | Medial Plate With Crossing Screw |
Crossing Screws | |
|---|---|---|---|---|
| Initial gap, mm | 0.43 | 0.32 | 1.14 | 1.27 |
| (–0.10 to 0.95) | (0.07 to 0.57) | (0.48 to 1.80) | (0.44 to 2.10) | |
| Final gap, mm | 0.56 | 0.48 | 1.37 | 1.81 |
| (0.04 to 1.09) | (0.18 to 0.77) | (0.64 to 2.10) | (0.79 to 2.84) | |
| Gap widening, mm | 0.14 | 0.17 | 0.23 | 0.54 |
| (0.03 to 0.25) | (0.07 to 0.26) | (0.14 to 0.32) | (0.20 to 0.89) |
Abbreviation: IM, intramedullary.
aAll data are represented as mean with upper and lower 95% confidence interval (CI) within parentheses.
Table 3.
Pairwise Comparisons for Initial Plantar Gap, Final Plantar Gap, and Gap Widening for All Fixation Group Combinations.a
| Initial Gap | Final Gap | Gap Widening | ||||
|---|---|---|---|---|---|---|
| Pairwise Difference, mm | P Value | Pairwise Difference, mm | P Value | Pairwise Difference, mm | P Value | |
| 4-hole IM device vs 3-hole IM device | 0.10 | .993 | 0.08 | .998 | –0.03 | .995 |
| 4-hole IM device vs medial plate | –0.72 | .259 | –0.81 | .274 | –0.09 | .860 |
| 4-hole IM device vs crossing screws | –0.84 | .158 | –1.25 | .043b | –0.41 | .010b |
| 3-hole IM device vs medial plate | –0.82 | .141 | –0.89 | .176 | –0.06 | .944 |
| 3-hole IM device vs crossing screws | –0.94 | .080 | –1.33 | .022b | –0.38 | .014b |
| Crossing screws vs medial plate | 0.13 | .986 | 0.44 | .729 | 0.31 | .044b |
Abbreviation: IM, intramedullary.
a All P values have been adjusted for multiple comparisons.
b Statistically significant differences.
Regression analysis determined that specimen age at the time of death had a significant effect on widening of the first TMT (P = .015). After controlling for age, the 4-hole intramedullary device, 3-hole intramedullary device, and the medial plate with crossing screw were estimated to have 0.38, 0.43, and 0.37 mm less plantar gap widening than crossing screw fixation, respectively. No other analyzed characteristic had a significant effect on gap widening.
Discussion
The experiment presented here documents the ability of 2 locked intramedullary devices and a medial plate with crossing screw to resist widening of the first TMT better than a 2–crossing screw construct during cyclic testing. The final gap for both intramedullary device groups was smaller than that of the crossing screw group. The intramedullary device groups were more stable than crossing screws during the cyclic fatigue test, exhibiting less gap widening. The medial plate with crossing screw fixation was also more stable than crossing screws in the cyclic fatigue model. We were unable to detect a significant difference in gap widening between the 3 modern fixation methods.
Our results are corroborated by previous investigations for a variety of devices. 1,4,10,11,15 Baxter et al 1 investigated plantar gapping in a cyclic fatigue model and reported a 1.1-mm gap for crossing screws and 3.2-mm gap for dorsomedial plates after 1000 cycles, with the plate group experiencing a 2.1-mm increase over the trial whereas the screw group remained relatively unchanged. These results are in contrast to the results from the current study, where medial plates outperformed crossing screw fixation. These differing results may be due to the geometric differences in the plate designs, the lack of or inclusion of a crossing screw with the plate, or the differences in testing protocols. Baxter et al 1 also reported initial gap measurements that are in line with our results for the medial plate with crossing screw and crossing screw groups. Similar to Baxter, we were unable to show significant differences in the initial gap. However, it should be noted that the initial gap for the 3-hole intramedullary device approached statistical significance compared with crossed screw fixation (P = .080).
Our hypothesis on why the locked intramedullary devices and medial plates demonstrated better resistance to plantar gapping in our study is that the devices tested produce a more rigid construct than traditional 2-screw fixation by engaging more cortical bone. The crossing screw construct tested in this study penetrated the cortex in 4 locations whereas the intramedullary constructs engaged the cortex in 6 (3-hole device) or 8 (4-hole device) locations. Similarly, the medial plate with crossing screw construct tested in this study can engage the cortex in 12 locations. Furthermore, because of the aforementioned inline compression of the 3- and 4-hole intramedullary devices, it is possible that greater bone apposition could have been achieved when compared to an uncompressed construct or a construct that relies on off-axis compression. This may lead to less “windshield wiper”–type motion, thus preserving the integrity of the bone-hardware interface.
The results presented here indicate that both locked intramedullary devices and medial plates with crossing screw may provide a better osseous healing environment compared with screw fixation by limiting interfragmentary motion. This may allow for faster healing time and the ability to bear weight earlier than the traditional standard of care following first TMT arthrodesis. Future clinical investigations are needed to prove this hypothesis. Although this study outlines biomechanical advantages of intramedullary nailing for arthrodesis of the first TMT, clinical drawbacks may exist. Given the novelty of these devices, surgeons may need to familiarize themselves with the operative technique before mastering the procedure. This may result in increased operative times and increased use of intraoperative fluoroscopy until proficiency is achieved. Similarly, the biomechanical advantages of medial plating may be offset by increased soft tissue exposure and the periosteal stripping associated with plating.
Furthermore, this study does not take into account the potential cost differences associated with the various constructs that were tested, as this was outside the scope of the study. Given that we do not fully understand how construct stability relates to clinical outcomes, it is possible that the cost of intramedullary devices and plate with screw constructs outweigh the clinical benefits gained by the reduction in gap. Further cost-benefit analysis on specific hallux valgus hardware is needed.
Strengths of our study include using cadaver tissue of similar demographic makeup within a controlled laboratory setting. All devices were implanted by a single surgeon to avoid variation in technique and skill. We quantified plantar gap for 36 specimens, which to our knowledge, is the largest cadaveric, biomechanical study conducted on arthrodesis of the first TMT. At 20 000 cycles, our cadaver fatigue model is the longest published, to date. The next longest fatigue study ran for just over 12 000 cycles for only a few of their trials. 15
Our experiment is not without limitations. We used a cortical hardness measurement that might not be as sensitive to osteopenia or osteoporosis as other modalities. Study specimens were not matched, which may have introduced variability in biologic and biomechanical properties. An a priori power analysis was not conducted for this study. This may have led to clinically relevant differences between groups to go undetected. Our fixture design constrained the metatarsal to a single plane of motion. This constraint is not physiologic but was consistently applied to all our specimens and is common in biomechanical evaluations of this joint. 1,4,10,11,15 Furthermore, it is possible that this constraint may have had an uneven effect on our outcomes, depending on fixation type. Our motion tracking system only measured motion in a single plane; thus, we were unable to quantify medial-lateral motion. The study is also inherently limited by the devices included in the investigation. Devices not tested in the study may have better or worse performance characteristics than those tested. Continued biomechanical testing of other fixation methods is needed. Nonetheless, we have been able to capture fixation performance for initial, final, and gap widening, which speaks directly to the aims of our experiment.
Conclusion
The current study provides evidence to suggest that locked intramedullary devices and medial plates with crossing screws can provide more stable fixation of the first TMT joint while resisting changes to joint gap during robust biomechanical testing compared with a 2–crossing screw technique. No difference in change in gap over the cyclic trial could be detected between the 3 modern hallux valgus devices. Crossing screw fixation demonstrated the largest increase in gap. Constructs that reduce interfragmentary gap and prevent excessive interfragmentary motion may be more conducive to bone healing than those that do not.
Supplemental Material
Supplemental Material, FAO892240-ICMJE for Biomechanical Comparison of First Tarsometatarsal Arthrodesis Constructs Over Prolonged Cyclic Testing by Cynthia Prieto-Diaz, Mathew R. Anderle, Laura Zagrocki Brinker, Randall Allard and Jeremi Leasure in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors report grants from Paragon 28, during the conduct of the study. Mathew R. Anderle, MPH, Laura Zagrocki Brinker, DPM, and Randall Allard, MS, report other from Paragon 28, Inc., outside the submitted work. ICMJE forms for all authors are available online.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Paragon 28, Inc.
ORCID iD: Mathew R. Anderle, MPH,  https://orcid.org/0000-0002-8887-3804
https://orcid.org/0000-0002-8887-3804
References
- 1. Baxter JR, Mani SB, Chan JY, Vulcano E, Ellis SJ. Crossed-screws provide greater tarsometatarsal fusion stability compared to compression plates. Foot Ankle Spec. 2015;8(2):95–100. [DOI] [PubMed] [Google Scholar]
- 2. Blitz NM, Lee T, Williams K, Barkan H, DiDimenico LA. Early weight bearing after modified lapidus arthodesis: a multicenter review of 80 cases. J Foot Ankle Surg. 2010;49(4):357–362. [DOI] [PubMed] [Google Scholar]
- 3. Bohay DR, Hooper JM, Anderson JG, et al. Early weight bearing following first TMT arthrodesis. Foot Ankle Orthop. 2016;1(1). doi:10.1177/2473011416S00106. [Google Scholar]
- 4. Burchard R, Massa R, Soost C, et al. Biomechanics of common fixation devices for first tarsometatarsal joint fusion—a comparative study with synthetic bones. J Orthop Surg Res. 2018;13(1):176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Campbell B, Schimoler P, Belagaje S, Miller MC, Conti SF. Weight-bearing recommendations after first metatarsophalangeal joint arthrodesis fixation: a biomechanical comparison. J Orthop Surg Res. 2017;12(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Claes L, Eckert-Hubner K, Augat P. The effect of mechanical stability on local vascularization and tissue differentiation in callus healing. J Orthop Res. 2002;20(5):1099–1105. [DOI] [PubMed] [Google Scholar]
- 7. Claes L, Eckert-Hubner K, Augat P. The fracture gap size influences the local vascularization and tissue differentiation in callus healing. Langenbeck’s Arch Surg. 2003;388(5):316–322. [DOI] [PubMed] [Google Scholar]
- 8. Claes L, Recknagel S, Ignatius A. Fracture healing under healthy and inflammatory conditions. Nat Rev Rheumatol. 2012;8(3):133–143. [DOI] [PubMed] [Google Scholar]
- 9. Claes LE, Heigele CA, Neidlinger-Wilke C, et al. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res. 1998;355(suppl):S132–S147. [DOI] [PubMed] [Google Scholar]
- 10. Cohen DA, Parks BG, Schon LC. Screw fixation compared to H-locking plate fixation for first metatarsocuneiform arthrodesis: a biomechanical study. Foot Ankle Int. 2005;26(11):984–989. [DOI] [PubMed] [Google Scholar]
- 11. Gruber F, Sinkov VS, Bae S-Y, Parks BG, Schon LC. Crossed screws versus dorsomedial locking plate with compression screw for first metatarsocuneiform arthrodesis: a cadaver study. Foot Ankle Int. 2008;29(9):927–930. [DOI] [PubMed] [Google Scholar]
- 12. Marsell R, Einhorn TA. The biology of fracture healing. Injury. 2011;42(6):551–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Patel S, Ford LA, Etcheverry J, Rush SM, Hamilton GA. Modified lapidus arthrodesis: rate of nonunion in 227 cases. J Foot Ankle Surg. 2004;43(1):37–42. [DOI] [PubMed] [Google Scholar]
- 14. Prissel MA, Hyer CF, Grambart ST, et al. A multicenter, retrospective study of early weightbearing for modified lapidus arthrodesis. J Foot Ankle Surg. 2016;55(2):226–229. [DOI] [PubMed] [Google Scholar]
- 15. Roth KE, Peters J, Schmidtmann I, Maus U, Stephan D, Augat P. Intraosseous fixation compared to plantar plate fixation for first metatarsocuneiform arthrodesis: a cadaveric biomechanical analysis. Foot Ankle Int. 2014;35(11):1209–1216. [DOI] [PubMed] [Google Scholar]
- 16. Sathyendra V, Darowish M. Basic science of bone healing. Hand Clin. 2013;29(4):473–481. [DOI] [PubMed] [Google Scholar]
- 17. Zysset PK. Indentation of bone tissue: a short review. Osteoporos Int. 2009;20(6):1049–1055. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO892240-ICMJE for Biomechanical Comparison of First Tarsometatarsal Arthrodesis Constructs Over Prolonged Cyclic Testing by Cynthia Prieto-Diaz, Mathew R. Anderle, Laura Zagrocki Brinker, Randall Allard and Jeremi Leasure in Foot & Ankle Orthopaedics