Abstract
Talar osteonecrosis is a well-described phenomenon following talar neck fracture, but is a rarely described complication after procedures about the foot and ankle. Here we describe the clinical course of 5 cases of talar osteonecrosis following injection of calcium phosphate into the talus (subchondroplasty) with or without acute lateral ligament repair after acute lateral ankle ligament injuries performed at an outside institution. Practitioners should be aware of this potentially devastating complication. Future research is indicated to determine the safety and efficacy of subchondroplasty for the talus.
Level of Evidence:
Level V, case series.
Keywords: talus, osteonecrosis, avascular necrosis, subchondroplasty
Introduction
Nonoperative treatment is regarded as the standard of care for the management of acute, uncomplicated lateral ankle sprains. Although the evidence comparing early operative intervention (with lateral ligament repair) vs functional rehabilitation in the setting of acute ankle inversion injuries is of poor quality owing to heterogeneity of nonoperative treatment modalities and lack of randomized controlled studies, the available literature and historical standard of care supports conservative management irrespective of age or athletic demands. 6
As diagnostic and treatment options evolve, there is intermittently renewed interest in early operative treatment of these acute injuries. Wider availability of magnetic resonance imaging (MRI) in particular has made advanced imaging of acute ankle sprains more commonplace, and frequently demonstrates pathology that to some may be a target for operative intervention. One such entity commonly seen on MRI is the “bone marrow lesion” (BML), variably described as “bone marrow edema,” “osteochondral lesion,” or “subchondral fracture.” These lesions, which are best described in the orthopedic sports literature with respect to the knee after anterior cruciate ligament injury, can also occur at the tibiotalar joint. 4 After an acute ankle instability episode, the tibia and talus can make abnormal contact because of sudden coronal plane or rotational forces, leading to microfracture and hematoma. 7,10 On MR imaging, this can be detected as increased signal change or “bony edema.” 7,10,13 Common locations to see bone marrow signal changes after ankle sprains include the medial talar dome and the talar neck/head. 7 These lesions are considered to represent focal bony contusions that typically resolve without intervention and are of no long-term clinical consequence. 7,10,13 Occasionally, BMLs can be related to chronic conditions such as osteochondral lesions of the talus or os trigonum syndrome. 10
Recently, a procedure termed “subchondroplasty” (Zimmer, Warsaw, IN) has been developed to address bone marrow lesions. 4 This technology utilizes a highly porous synthetic calcium phosphate bone graft substitute placed under fluoroscopic guidance in regions of assumed symptomatic bony defects or edema. Conceptually, this bone graft substitute is meant to provide pain relief by creating temporary structural support and also providing a scaffold for bony healing to occur. More recently, there have been several case reports and series of this procedure being performed for lesions in the foot and ankle. 2,8,12
We present a series of 5 cases in which patients developed rapid osteonecrosis, and in 2 cases collapse of their tali after undergoing acute lateral ligament reconstruction with talar subchondroplasty. These cases highlight a potential devastating complication that surgeons should be aware of when considering subchondroplasty for BMLs of the talus in the setting of acute lateral ligament injury.
Case Series
We performed a retrospective chart review of 5 patients who had undergone a subchondroplasty procedure in the setting of acute lateral ligament injury. All of these patients were initially taken care of by outside providers at 2 different institutions and later referred to our clinics after initial treatment (Table 1). The average age of the patients was 23 (range 16-31). In all cases, patients were otherwise healthy and had no known risk factors for osteonecrosis of the talus. In all cases, the patients had an inversion ankle sprain injury. When they presented to the outside providers, radiographs and MRIs were obtained in all cases (Figures 1 and 2). Outside radiologists reported “talar bone marrow edema,” and injury to the lateral ligamentous structures including the anterior talofibular ligament. Review of these MRIs by the authors of this study was performed, and in all cases demonstrate signal change within the anterior talofibular ligament consistent with sprain, as well as T2-weighted signal changes within the lateral talar body consistent with bony contusion. In none of the preoperative MRIs is there evidence of talar fracture or osteochondral lesion of the talus. In each case, the outside provider diagnosed these patients with “lateral ligament ankle sprain” and in 3 cases “talar body fracture.”
Table 1.
Patient Data and Demographics.
| Patient Number | Age | Comorbidities | Preoperative Diagnosis by outside Provider | Preoperative MRI findings | Time from Injury to Index Procedure | Index Procedure | Postoperative MRI Findings | Secondary Procedures |
|---|---|---|---|---|---|---|---|---|
| 1 | 16 | None | ATFL tear | ATFL signal change, talar bone edema | 3 wk | Open Broström, subchondroplasty | Talar osteonecrosis with collapse | Considering arthrodesis |
| 2 | 31 | None | ATFL tear, “talar body fracture” | ATFL signal change, talar bone edema | 4 wk | Subchondroplasty | Talar osteonecrosis | Arthroscopy, debridement and microfracture |
| 3 | 17 | None | Ankle sprain, “talar body fracture” | ATFL tear, talar bone edema | 2 wk | Subchondroplasty | Talar osteonecrosis | Arthroscopy, debridement, and retrograde drilling |
| 4 | 27 | None | Ankle sprain, “talar edema” | ATFL tear, talar bone edema | 4 wk | Subchondroplasty | Talar osteonecrosis | Total ankle replacement |
| 5 | 25 | None | ATFL tear, “talar body fracture” | ATFL signal change, talar bone edema | 2 wk | Open Broström, Subchondroplasty | Talar osteonecrosis with collapse | Considering ankle arthrodesis |
Abbreviations: ATFL, anterior talofibular ligament; MRI, magnetic resonance imaging.
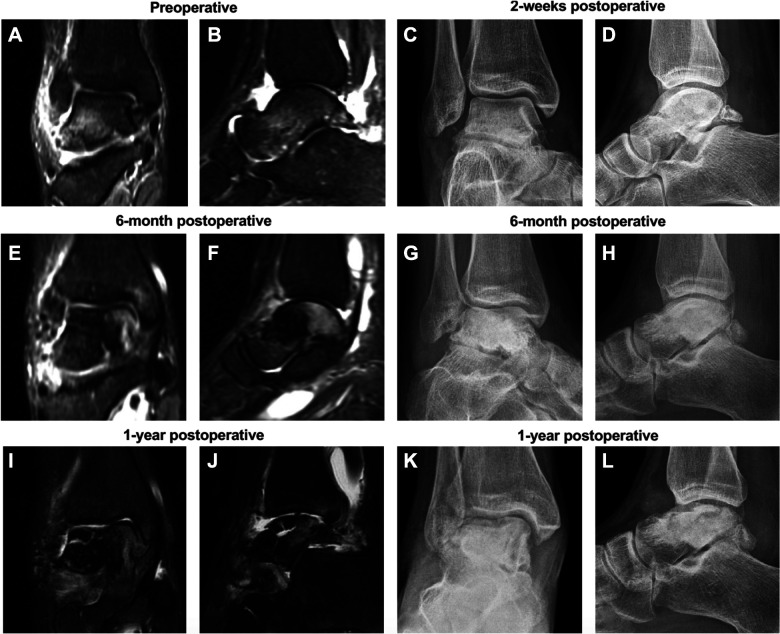
Figure 1.
Coronal and sagittal magnetic resonance images of a 25-year-old woman before (A, B) and 6 months and 1 year after undergoing a talar subchondroplasty and open Broström procedure 2 weeks after the date of injury. Corresponding anteroposterior and lateral radiographs are shown at time points of (C, D) 2 weeks, (E-H) 6 months, and (I-L) 1 year after the same procedure. Postoperatively there is evolution from talar bone marrow edema and sclerosis to collapse and fragmentation.
Figure 2.
Lateral radiograph, T1-weighted sagittal magnetic resonance imaging, and coronal and sagittal computed tomographic images of a 16-year-old woman showing severe talar osteonecrosis with collapse and fragmentation 8 months status post subchondroplasty procedure and open Broström performed 3 weeks after the initial injury.
In all cases, the patients were brought to the operating room by their outside provider within 4 weeks of the injury date. In 3 of 5 cases, the patients underwent the isolated subchondroplasty procedure, which the outside provider called “open reduction and internal fixation of talus fracture.” One patient underwent an open Broström procedure with subchondroplasty, and in the final case, the patient underwent ankle arthroscopy, open Broström procedure, and subchondroplasty. In 1 case, the patient also underwent a calcaneal subchondroplasty procedure.
In the operative reports of these patients, the outside providers describe inserting a cannula for the subchondroplasty from medial to lateral across the talar body and then injecting the calcium phosphate bone substitute under fluoroscopic guidance into the area of presumed “fracture.” In Figure 1, at the “2-week postoperative” section, the cannula track at the medial talar body can be seen on the anteroposterior radiograph and at the anterior talus on the lateral radiograph. The patients were immobilized for several weeks and then underwent physical therapy, which provided initial relief. In all cases, within the 6 months following surgery, the patients developed progressively worsening pain in their ankles. They then presented to our clinic for a second opinion.
Normally after subchondroplasty, expected radiographic findings include a focal region of increased density within the region of the injected calcium phosphate. 1 On MR imaging, normal expected findings include the presence of a focal hypointense region in the region of injected calcium phosphate on T1- and T2-weighted imaging in the region of previous bone marrow edema, sometimes with a fine hyperintense surrounding border the first 6 months after the procedure. 1 In each case presented here, radiographs and MR imaging indicated osteonecrosis of the talus. In 3 of the 5 cases, this included diffuse (rather than focal) talar sclerosis involving the body, neck, and head of the talus on radiographs. Similarly, on MRI there was widespread increased bone marrow signal within the head, neck, and body of the talus surrounding the focal hypointense region corresponding to the region of calcium phosphate injection. In 2 of the 5 cases, radiographs and MRI scan additionally demonstrate subchondral collapse and talar dome fracture (Figures 1 and 2). Figure 1 demonstrates the pre- and postoperative images of the patient who underwent ankle arthroscopy with open Broström procedure and subchondroplasty. At 1 year, there was fracture and collapse of the medial talar dome. Figure 2 demonstrates similar findings in a patient 8 months after open Broström procedure and subchondroplasty, demonstrating similar fracture and collapse, in this case of the lateral talar dome.
At the time of this writing, 2 of the patients without collapse have subsequently undergone ankle arthroscopy with bone marrow stimulation procedures. The third patient without collapse underwent total ankle replacement at an outside institution. The 2 patients with collapse are considering ankle arthrodesis at the time of this writing (Table 1).
Discussion
Talar osteonecrosis is a well-described phenomenon after high-energy injuries of the talus such as talar neck fractures and associated subtalar dislocations. However, reports of iatrogenic talar osteonecrosis after lateral ligament repair are exceedingly rare and are not traditionally considered a risk with this procedure. The authors could only find a single case report of osteonecrosis in connection with the Broström procedure, in which talar osteonecrosis developed after use of an internal brace implant within the talus following a modified Broström procedure performed for chronic ankle instability. 11 The authors of that report hypothesized that there was disruption of talar blood supply by the implant, leading to osteonecrosis.
We present 5 cases in which subchondroplasty was performed for young patients with lateral ankle sprains and associated talar bone marrow edema. In all cases, rapid (within 6 months of surgery) symptomatic osteonecrosis and bony collapse of the dome of the talus ensued, resulting in an indication for salvage procedures. It is not clear what caused osteonecrosis in these cases, and cause and effect between the procedures performed and talar osteonecrosis cannot be concluded. However, the rarity of this complication and the association in all cases with a subchondroplasty procedure is alarming. The primary blood supply to the talar body originates from the arteries of the tarsal canal and tarsal sinus and the deltoid artery. 5,9 The artery of the tarsal canal, which originates as a branch off the posterior tibial artery, supplies the lateral two-thirds of the talar body and lateral posterior facet, whereas the artery of the tarsal sinus, which variably arises as a branch of the dorsalis pedis or from one of the peroneal artery branches, supplies the lateral anterior talar body and the remainder of the posterior facet. The deltoid artery supplies the medial body. These arteries create an intraosseous anastamotic network (Figure 3). Notably, in all presented cases, subhcondroplasty was performed by inserting a cannula from medial to lateral across the talar body. It is possible that this technique damaged the extraosseous blood supply or disrupted the intraosseous network. The subsequent bone graft substitute itself may also have damaged or displaced the delicate intraosseous network, preventing revascularization.
Figure 3.
Artist’s rendering of talar blood supply. (A) Sagittal section through the midtalus demonstrating the distribution of the 3 major arteries supplying the talus. (B) Coronal section through the posterior midtalus demonstrating the distribution of the deltoid and tarsal canal branches.
Subchondroplasty is a relatively new procedure and has been primarily described for chronic bone marrow lesions about the knee. The marketed indication is for patients with chronic bone marrow lesions demonstrated on fat-suppressed MRI that have not improved with a trial of conservative management. Within this indication, there have been conflicting reports in terms of outcomes. More recently, a few cases have reported subchondroplasty performed about the foot and ankle. 2,3,8,12 In the largest case series of 10 patients, subchondroplasty was performed for osteochondral lesions of the talus that had been refractory to nonoperative management with reportedly good results and no complications. 3 This series does not report on how long bone marrow lesions had been present or how long conservative management was attempted prior to subchondroplasty. Additionally, in this series, the cannula was inserted from anterior to posterior across the subchondral bone.
Further research, both clinical and anatomic, is indicated to determine what role subchondroplasty may have to play in talar BMLs. Should providers perform subchondroplasty for talar lesions in the future, validated longitudinal clinical outcome scoring should be performed. Basic science research should define how subchondroplasty may affect talar bone supply. Regardless, bone marrow contusions after acute trauma, which can be expected to resolve without treatment, are not an indication for this procedure. Additional research regarding indications for acute lateral ligament reconstruction remain unresolved.
Conclusion
Talar subchondroplasty performed in the setting of acute lateral ligament injury may lead to talar osteonecrosis and collapse. Surgeons should be aware of this potential devastating complication when indicating patients for this procedure.
Supplemental Material
Supplemental Material, FAO907072-ICMJE for Talar Osteonecrosis After Subchondroplasty for Acute Lateral Ligament Injuries: Case Series by Ian M. Foran, Daniel D. Bohl, Anand M. Vora, Nasima Mehraban, Kamran S. Hamid and Simon Lee in Foot & Ankle Orthopaedics
Footnotes
Editor’s Note: This case series is unusual in that it appears patients should not have undergone surgery. However, the procedures they underwent were complicated by devastating complications. It would have been useful to know how much of the material had been injected as it is distinctly possible that too much of the calcium phosphate cement had been injected, thus leading to this devastating complication.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ian M. Foran, MD,  https://orcid.org/0000-0002-6805-2275
https://orcid.org/0000-0002-6805-2275
Daniel D. Bohl, MD,  https://orcid.org/0000-0002-7599-4244
https://orcid.org/0000-0002-7599-4244
References
- 1. Agten C, Kaplan D, Jazrawi L, Burke C. Subchondroplasty: what the radiologist needs to know. Am J Radiol. 2016;207:1257–1262. [DOI] [PubMed] [Google Scholar]
- 2. Barp E, Hall J, Reese E, Smith H. Subchondroplasty of the foot: two case reports. J Foot Ankle Surg. 2018;58(5):989–994. [DOI] [PubMed] [Google Scholar]
- 3. Chan J, Guzman J, Vargas L, Myerson L, Chan J, Vulcano E. Safety and effectiveness of talus subchondroplasty and bone marrow aspirate concentrate for the treatment of osteochondral defects of the talus. Orthopedics. 2018;41(5):e734–e737. [DOI] [PubMed] [Google Scholar]
- 4. Cohen SB, Sharkey PF. Subchondroplasty for treating bone marrow lesions. J Knee Surg. 2016;29(7):555–563. [DOI] [PubMed] [Google Scholar]
- 5. Kelikian A. Sarrafian’s Anatomy of the Foot and Ankle. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 6. Kerkhoffs GJ, Handoll HG, de Bie R, Rowe BH, Struijs PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2007;2:CD000380. [DOI] [PubMed] [Google Scholar]
- 7. Labovitz J, Schweitzer M. Occult osseous injuries after ankle sprains: incidence, location, pattern, and age. Foot Ankle Int. 1998;19(10):661–667. [DOI] [PubMed] [Google Scholar]
- 8. Miller J, Dunn K. Subchondroplasty of the ankle. Foot Ankle Online J. 2015;8(1):7. [Google Scholar]
- 9. Mulfinger GL, Trueta J. The blood supply of the talus. J Bone Joint Surg Br. 1970;52(1):160–167. [PubMed] [Google Scholar]
- 10. Rios A, Rosenberg ZS, Bencardino JT, Rodrigo SP, Theran SG. Bone marrow edema patterns in the ankle and hindfoot: distinguishing MRI features. AJR Am J Roentgenol. 2011;197(4):W720–W729. [DOI] [PubMed] [Google Scholar]
- 11. Sawley W, Guerrero E, Parekh S. Iatrogenic talar avascular necrosis secondary to lateral ligament reconstruction suture anchor placement requiring total talar replacement. Duke Orthop J. 2018;8(1):7–10. [Google Scholar]
- 12. Vulcano E, Chan J. Safety and efficacy of talus subchondroplasty and bone marrow aspirate concentrate for treatment of osteochondral lesions of the talus. Foot Ankle Orthop. 2018; 3(3). [DOI] [PubMed] [Google Scholar]
- 13. Weishaupt D, Schweitzer M. MR imaging of the foot and ankle: patterns of bone marrow signal abnormalities. Eur Radiol. 2002;12:416–426. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO907072-ICMJE for Talar Osteonecrosis After Subchondroplasty for Acute Lateral Ligament Injuries: Case Series by Ian M. Foran, Daniel D. Bohl, Anand M. Vora, Nasima Mehraban, Kamran S. Hamid and Simon Lee in Foot & Ankle Orthopaedics