Level of Evidence:
Level V, expert opinion.
Keywords: conservative treatment, posterior process fracture, posterior process of talus, subtalar dislocation, talus
Introduction
Isolated fracture of the posterior process of the talus (PPT) is rare, 7,10,12,13 with PPT fracture with concomitant subtalar dislocation being even more rare 1,3,8,11,14 ; thus, the mechanism of injury, appropriate treatment, and prognosis are unclear. 1,11,12,14 Subtalar dislocation accounts for 1% to 2% of all dislocations. 1,6,8,14 Talus fracture incidence is 0.1% to 0.85% of all fractures. 4,15 There are only 5 case reports of subtalar dislocation with fracture of the PPT previously reported in the literature. 1,3,8,11,14 Furthermore, each of the previous case reports elected to treat the PPT fracture with various methods of open reduction and internal fixation (ORIF) after closed reduction of the subtalar dislocation. Because of incidence, it is difficult to evaluate outcomes and determine treatment guidelines for this injury. There have been no published case reports of nonoperative treatment of this injury. We present a case of fracture of the entire PPT with subtalar dislocation that was recognized early and successfully treated nonoperatively.
Case Report
A 53-year-old man was brought to our emergency department after falling approximately 3 feet off a ladder. He described the left foot being plantarflexed and sustaining a strong inversion force upon landing on the pavement. He presented with severe pain, swelling, and gross deformity of the foot and ankle region, with the midfoot locked medially. The skin was intact, and there was no neurovascular compromise.
The patient had poorly controlled hypertension and smoked ½ to 1 pack of cigarettes per day for 35 years. He otherwise had no other known comorbidities. Anteroposterior (AP), mortise, and lateral radiographs of the ankle as well as AP, oblique, and lateral radiographs of the foot showed a medial subtalar dislocation with a large PPT fracture fragment sitting superior to the calcaneus and posterior to the distal tibia and talus (Figure 1). Under conscious sedation in the emergency department, a closed reduction of the subtalar joint was performed with manual traction and direct pressure over the head of the talus. Under fluoroscopy, the subtalar joint was grossly unstable and required splinting in dorsiflexion and eversion to maintain reduction. Postreduction radiographs were obtained, as well as computed tomography (CT), to further evaluate the fracture fragment, displacement, and articular involvement. CT showed a fracture of the entire PPT with maximum displacement of 3 mm at the mid-coronal body portion of the fracture. Both the tibiotalar and subtalar joints revealed only 1 to 2 mm of displacement at the proximal and distal ends of the fracture (Figures 2 and 3).
Figure 1.
(A) Lateral, (B) mortise, and (C) anteroposterior ankle radiographs at the time of injury showing deformity and a fracture fragment posterior to the talus. (E, F) Foot radiographs showing medial subtalar joint dislocation. (D, G, H) Radiographs taken after closed reduction and splinting of the subtalar dislocation. Reduction of the posterior process of the talus fracture is difficult to accurately assess on plain films.
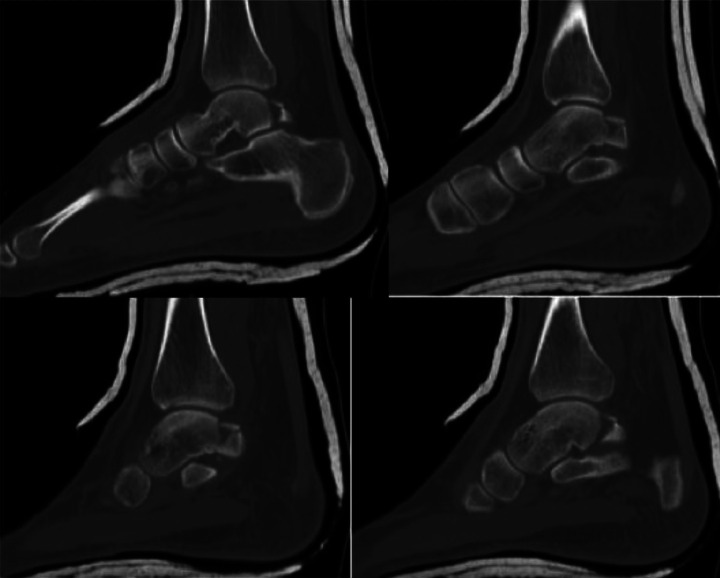
Figure 2.
Progression of sagittal computed tomography scan images visualizing the posterior process of the talus fracture post-reduction.
Figure 3.
Axial computed tomographic views of the posterior process of the talus fracture: (A) Proximal articular involvement at the ankle joint with minimal displacement. (B) The middle portion of the PPT fracture where the greatest displacement is noted. (C) The distal articular involvement of the subtalar joint with minimal displacement.
Because of swelling, the patient’s tobacco use, and patient preference, it was decided to attempt nonoperative treatment. The patient was made strictly nonweightbearing on the injured leg and remained splinted. Eleven days from injury, the patent was found to have extensive serous and hemorrhagic fracture blisters on the dorsal aspect of the foot and forefoot with some serous drainage, but no clinical signs of infection. The patient was prophylactically placed on a short course of oral antibiotics and treated locally by cleaning and placement of Xeroform gauze over the blisters. Eighteen days after the injury, radiographs were obtained outside of the splint showing a well-reduced subtalar joint with no further displacement of the PPT fracture. The fracture blisters were noted to extend up the medial and lateral ankle (Figure 4), which healed without sequela. The patient was placed into a short leg cast and remained nonweightbearing. At 6 weeks, the patient was transitioned into a removable fracture boot, but kept nonweightbearing for an additional 3 weeks. At 9 weeks, the patient was allowed to transition to full weightbearing. Radiographs at that time showed continued interval healing, no evidence of avascular necrosis of the talus, with some disuse osteopenia. At 14 weeks from injury, the patient was able to full weight-bear and reported 1/10 pain in the foot and ankle. Weightbearing films showed resolution of the osteopenia and healed posterior process of the talus fracture and a stable subtalar joint without signs of post-traumatic arthrosis of the tibiotalar or subtalar joints (Figures 5 to 7). The patient was transitioned into a normal shoe at that time. At 11 months from injury, the patient had returned to his employment full-time and resumed all activities without pain, impairment, or noticeable deficits in range of motion or stability. Via phone interview, the patient completed the American Orthopaedic Foot & Ankle Society (AOFAS) 9 Ankle-Hindfoot Scale assessment with a score of 100.
Figure 4.
Post-traumatic fracture blisters that developed within the first few days of injury. Care must be taken with regard to operative planning and timing as this can potentially create operative wound and healing complications.
Figure 5.

Follow-up lateral radiographs 14 weeks after injury
Figure 6.
Follow-up anteroposterior and oblique radiographs of foot 14 weeks after injury.
Figure 7.

Mortise view of ankle 10 weeks out from injury.
Discussion
The posterior process of the talus articulates with both the tibiotalar and subtalar joints. It is made up of 2 tubercles, medial and lateral, and separated by a groove for the flexor hallucis longus (FHL) tendon. The lateral tubercle, also known as the Steida process, is larger, more posterior, and is an attachment site of the posterior talofibular ligament. It develops from a separate ossification center, which if it fails to fuse to the rest of the talus, is known as the os trigonum. The os trigonum can be an accessory bone commonly located in this area. The eponym for a fracture of the lateral process of the talus is “Shepherd’s fracture.” These fractures can be initially missed 40% to 50% of the time. 1,3,4,12,13 Fractures of the medial tubercle of the posterior process are much less common and occur from an avulsion of the posterior portion of the deltoid ligament. 12 Historically, a fracture of either the lateral or medial posterior tubercles in isolation is not uncommon, but have been referred to as a PPT fracture, which is not a proper description. A posterior process fracture of the talus involves the entire posterior process where both the lateral and medial tubercles are present on the posterior fracture fragment, which is much less common. 1,3,7,12
Prior to Nasser and Manoli’s case report in 1990, 12 PPT fracture had only been described once. 5 Even less common is PPT fracture with concomitant subtalar dislocation. The first case report of medial subtalar dislocation combined with PPT fracture was in 1994 by Ebraheim et al. 3 To our knowledge, there have been only 4 additional cases reported since that time, 1,8,11,14 limiting information about the mechanism of injury, treatment approach, and long-term outcomes. Our case report supports a possible mechanism of injury and the importance of early recognition and treatment, while presenting a treatment approach that has not been reported.
Nasser and Manoli 12 postulated that the mechanism of injury of an entire PPT fracture occurs after maximum plantarflexion of the ankle, causing compression of the posterior talus between the posterior lip of the tibia and calcaneus. Medial subtalar dislocation has shown to be caused by forceful inversion of the foot. 1,6 As pointed out by Park and Park, 14 it is believed that forced plantarflexion with inversion causes fracture of the posterior process of the talus with concomitant subtalar dislocation. Comparing the mechanism of injury of the 5 previously reported cases (Table 1), 2 resulted from high-energy motor vehicle accidents, 1,3 1 a fall on a plantarflexed foot, 11 and 2 describe a forceful plantarflexion with inversion at the time of injury. 8,14 Our patient also fell in maximum plantarflexion while sustaining a strong inversion force on contacting the pavement, thus supporting previous descriptions of the mechanism of injury.
Table 1.
Comparison of Case Reports.
| Case Report | Patient | Mechanism | Operative Approach | Fixation | Postoperative Protocol | Follow-up/Outcomes | Final Imaging |
|---|---|---|---|---|---|---|---|
| Ebraheim, 1994 | 27 y old, male | High-energy MVA | Posteromedial | 2 cannulated Herbert screws in lateral tubercle | Postop splint transitioned to SLC, NWB × 6 wk | 1-y f/u: minimal discomfort | Healed on radiograph, intact hardware |
| Naranja, 1996* | 26 y old, male | Fall from 15 feet on plantarflexed foot | Posterolateral | 4.0-mm cannulated screw | Splint, NWB (amount of time not specified) | 8-mo f/u: no pain with ambulation. Decreased subtalar ROM | Healed on radiograph with no evidence of arthrosis |
| Chen, 1996 | 52 y old, female | Motorcycle accident | Approach not specified | "miniscrew’ in medial tubercle | SLC NWB × 3 wk, then dynamic ankle brace and partial weightbearing for 3 wk with aggressive postoperative ROM | 32-mo f/u: full ROM | Radiograph showed successful healing |
| Liu, 2012 | 17 y old, male | Plantarflexion and strong inversion playing basketball | Posteromedial | 3 absorbable screws (two 2.7-mm, one 3.5-mm) | SLC NWB × 6 wk | 1-y f/u: No clinical outcomes mentioned | MRI: No AVN or post-traumatic arthrosis (fracture healing not mentioned) |
| Park, 2016 | 50 y old, male | Fall from 10 feet forced plantarflexion and inversion | Posteromedial | 2 headless 3.0-mm compression screws | SLC NWB × 6 wk | 13-mo f/u: return to sports and work at preinjury level | Satisfactory bone healing on CT scan and radiograph at 6 mo Radiographs at 13 mo: No signs of arthrosis or FHL tendinosis |
Abbreviations: AVN, avascular necrosis; CT, computed tomography; FHL, flexor hallucis longus; f/u, follow-up; MRI, magnetic resonance imaging; MVA, motor vehicle accident; NWB, nonweightbearing; ROM, range of motion; SLC, short leg cast.
* Open medial subtalar dislocation.
Early recognition is imperative for a successful outcome of this injury. Although a subtalar dislocation will be apparent, the associated PPT fracture can be difficult to identify. 1,7,8,14 After reduction of the subtalar dislocation, a CT scan should be obtained to evaluate for fracture and amount of displacement at the tibiotalar and subtalar joints. CT helps confirm the diagnosis and guide treatment. 1,3,7,13,14 Although operative vs nonoperative treatment is unclear, early treatment is key to success regardless of method. Delay in operative treatment showed bone resorption of fracture fragments, making them irreparable. 3 Delay in conservative treatment also led to poor outcomes in a case series where PPT fractures were initially missed and improperly addressed. 13 In our case, the articular surface displacement of the PPT fracture was less than 3 mm, allowing us to justify an attempt at nonoperative treatment.
Proper treatment of the PPT fracture remains unclear. These fractures involve both the tibiotalar and subtalar joints; therefore, fracture malunion could lead to early arthritis. It is also believed that comminution or malunion in the groove for the FHL tendon could cause tendonitis, or heterotrophic ossification could cause tethering of the FHL tendon. 12,14 Naranja et al 11 noted that the FHL was a significant deforming force that externally rotates the PPT fragment. Some argue that because of the articular nature of the PPT fracture through weightbearing joints, anatomic reduction and stabilization is indicated. 7,11 -13 In contrast, others agree that operative intervention depends on the degree of joint involvement and displacement of the PPT fragment, pointing out that closed reduction and immobilization may be sufficient in fractures with up to 3 mm of displacement. In articular fractures displaced more than 3 mm, open reduction and internal fixation is recommended. 3,8,10,14 Chen et al 1 argued for operative fixation to facilitate early active and passive range of motion and weightbearing to avoid stiffness and tethering of the FHL tendon.
Arguments against nonoperative management of PPT fractures may stem from a case series reported by Nyska et al 13 of 4 patients with PPT fractures that were missed on initial presentation. Treatment varied and outcomes were poor, with malunions and early degenerative changes. They concluded that “conservative treatments” of either early range of motion or cast immobilization both led to poor results. This article was later cited by Iyakutty et al 7 and used as a strong argument against nonoperative measures and in favor of ORIF. After review of the cases reported, our conclusions differ from those drawn by Nyska and Iyakutty. 7,13 Two of their cases were found to have comminution into the talar body on CT, which are known to have worse outcomes. Regardless, the first case was treated with nonweightbearing for 6 weeks but early range of motion. Case 2 was treated with physiotherapy and nonweightbearing for only 3 weeks and did not specify immobilization. Case 3 was treated with only 3 weeks of cast immobilization followed by physiotherapy and did not specify weightbearing status during the period of immobilization. Case 4 was treated with cast immobilization followed by physiotherapy and did not provide duration of immobilization or weightbearing status. Of the 4 cases, the longest period of immobilization was 3 weeks. The longest period of nonweightbearing was 6 weeks, but was treated with early range of motion, with no immobilization of the injury. Therefore, based on what we feel were improper conservative treatments of these injuries, we could not draw similar conclusions against conservative treatment. In those cases, the fractures were initially missed, and none of them were treated with the appropriate restrictions, which include nonweightbearing and immobilization for appropriate length of time. Nevertheless, these reports remain valuable as they stress the importance of early recognition and treatment.
Our criteria for what we consider appropriate nonoperative treatment includes both immobilization and nonweightbearing due to fracture involvement of articular surfaces of 2 weightbearing joints. Additionally, with the attachments of the posterior one-third of the deltoid ligament and posterior talofibular ligament on the medial and lateral tubercles of the PPT, respectively, we feel that nonweightbearing alone is not sufficient treatment. Fracture motion and displacement may occur with early range of motion without sufficient fixation. For this reason, we believe that this fracture is not properly treated conservatively if either range of motion or weightbearing is allowed prematurely. Further research is needed regarding time required for immobilization and nonweightbearing; however, we strongly recommend a minimum of 8 weeks. We allowed our patient to transition to full weightbearing in a fracture boot at 9 weeks and transitioned him into a normal shoe by 14 weeks with an excellent outcome.
Based on the current literature in conjunction with our case, appropriate approach to these injuries involves immediate closed reduction of the subtalar dislocation with further evaluation with a postreduction CT scan. Based on the fracture characteristics on CT, treatment of the PPT fracture could be as follows:
With >3 mm of articular displacement, the surgeon should consider ORIF if the patient is a reasonable operative candidate. 1,3,7,8,10 -12,14
For fractures with 1 to 2 mm of articular displacement, nonoperative treatment is acceptable. ORIF is also reasonable in order to facilitate early active and passive range of motion and eventual weightbearing to avoid stiffness and tethering of the FHL tendon. 1 This is an option for healthier, active patients with few comorbidities. Surgery should be avoided in patients with risk factors (smoking, diabetes, peripheral neuropathy, vascular disease, and noncompliance) that increase the likelihood of operative site problems and healing issues.
For patients with >3 mm of articular displacement where early operative intervention is not possible or the injury is initially missed, excision of the posterior part of the talus or subtalar fusion have been suggested as salvage procedures. 13
Both operative and nonoperative treatments have potential complications. Although overall short-term operative results of ORIF of PPT fractures with subtalar dislocations seem satisfactory in the literature, 1,3,8,11,14 surgery comes with inherent risk. Higher-energy trauma and postinjury swelling often accompany this injury pattern, which may lead to soft tissue, operative wound, and healing complications (Figure 4). The operative approaches required can be difficult as they are less common with close approximation to the joint surfaces, neurovascular bundle, and FHL tendon. 3,8,11,14 Additional operative intervention can possibly compromise the talar blood supply. 3,12 In one case of isolated PPT fracture, limited ankle and subtalar motion resulted because of impingement from hardware. This patient also had decreased great toe dorsiflexion, which was thought to be from tethering of the FHL tendon behind the ankle joint. 12
Patient factors such as smoking, diabetes, neuropathy, noncompliance, or osteoporosis may have negative impacts regardless of treatment choice. With conservative treatment, complications can include loss of reduction and fracture displacement from premature motion or weightbearing. This could lead to nonunion, fracture resorption, or early arthritis, which may lead to delay in return to work or full activities. Prolonged immobilization and nonweightbearing can also lead to stiffness and osteopenia. In our case, we noticed osteopenia, which fully resolved after initiation of weightbearing.
Limitations in knowledge of mechanism, treatment, and outcomes in PPT fractures with subtalar dislocation are a result of the overall rarity of this injury. Although there are some descriptions of these injuries since at least 1977, 2 reports are rare and knowledge has only been derived from case reports. As in other case reports, ours is limited by a lack of long-term follow-up as well as subjective evaluation. Long-term data would be helpful in determining prognosis. Follow-up CT would have been desirable to evaluate fracture healing and joint surfaces; however, the patient declined this study.
In conclusion, fracture of the entire PPT with concomitant subtalar dislocation is rare. This injury can be missed; thus, a high index of suspicion with early recognition and proper treatment is essential to achieve successful outcomes. Mechanism, treatment, and prognosis have been unclear. Our study supports a mechanism of forced plantarflexion with a strong inversion force of the foot to create this combined injury pattern. We propose treatment guidelines, providing evidence for nonoperative treatment, which has not been reported in the literature. Short-term results of ORIF and proper nonoperative treatment are promising; however, long-term prognosis of both operative and nonoperative treatment is unknown, requiring further research and long-term follow-up.
Supplemental Material
Supplemental Material, FAO918570-ICMJE for Nonoperative Treatment of Fracture of the Entire Posterior Process of the Talus With Subtalar Dislocation: Case Report by Jordan S. McCoy, Amy L. Meyers and Matthew Marquart in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Amy L. Meyers, DO,  https://orcid.org/0000-0001-8019-2812
https://orcid.org/0000-0001-8019-2812
References
- 1. Chen Y, Hsu R, Shih H, Huang T. Fracture of the entire posterior process of the talus associated with subtalar dislocation: a case report. Foot Ankle Int. 1996;17(4):226–229. [DOI] [PubMed] [Google Scholar]
- 2. Christensen SB, Lorentzen JE, Krogsoe O, Sneppen O. Subtalar dislocation. Acta Orthop Scand. 1977;48(6):707–711. [DOI] [PubMed] [Google Scholar]
- 3. Ebraheim NA, Skie MC, Podeszwa DA. Medial subtalar dislocation associated with fracture of the posterior process of the talus: a case report. Clin Orthop Relat Res. 1994;303:226–230. [PubMed] [Google Scholar]
- 4. Fortin PT, Balazsy JE. Talus fractures: evaluation and treatment. J Am Acad Orthop Surg. 2001;9:114–127. [DOI] [PubMed] [Google Scholar]
- 5. Heckman JD. Fractures in adults. In: Rockwood CA, Green DP, eds. Philadelphia, PA: JB Lippincott Co; 1984, Chapter 19, pp. 1749–1751. [Google Scholar]
- 6. Heppenstall RB, Farahvar H, Balderstron R, Lotke P. Evaluation and management of subtalar dislocations. J Trauma. 1980;20:494-497. [DOI] [PubMed] [Google Scholar]
- 7. Iyakutty PP, Singaravadivelu V. Fracture of the entire posterior process of the talus: a case report. J Foot Ankle Surg. 2000;39:198–201. [DOI] [PubMed] [Google Scholar]
- 8. Liu Z, Zhao Q, Zhang L. Medial subtalar dislocation associated with fracture of the posterior process of the talus. J Pediatr Orthop. 2012;21:439–442. [DOI] [PubMed] [Google Scholar]
- 9. Madeley NJ, Wing KJ, Topliss C, Penner M, Glazebrook MA, Younger ASE. . Responsiveness and validity of the SF-36, Ankle Osteoarthritis Scale, AOFAS Ankle Hindfoot Score, and Foot Function Index in End Stage Ankle Arthritis. Foot Ankle Int. 2012;33(1):57–63. [DOI] [PubMed] [Google Scholar]
- 10. Mehrpour SR, Aghamirsalim MR, Sheshvan MK, Sorbi R. Entire posterior process talus fracture: a report of two cases. J Foot Ankle Surg. 2012;51:326–329. [DOI] [PubMed] [Google Scholar]
- 11. Naranja R, Monaghan B, Okereke E, Williams G. Case report: open medial subtalar dislocation associated with fracture of the posterior process of the talus. J Orthop Trauma. 1996;10(2):142–144. [DOI] [PubMed] [Google Scholar]
- 12. Nasser S, Manoli A II. Fracture of the entire posterior process of the talus: a case report. Foot Ankle. 1990;10(4):235–238. [DOI] [PubMed] [Google Scholar]
- 13. Nyska M, Howard CB, Matan Y, et al. Fracture of the posterior body of the talus—the hidden fracture. Arch Orthop Trauma Surg. 1998;117:114–117. [DOI] [PubMed] [Google Scholar]
- 14. Park CH, Park KH. Fracture of the posterior process of the talus with concomitant subtalar dislocation. J Foot Ankle Surg. 2016;55:193–197. [DOI] [PubMed] [Google Scholar]
- 15. Santavirta S, Seitsalo S, Kiviluoto O, Myllynen P. Fractures of the Talus. J Trauma. 1984;24:986–989. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO918570-ICMJE for Nonoperative Treatment of Fracture of the Entire Posterior Process of the Talus With Subtalar Dislocation: Case Report by Jordan S. McCoy, Amy L. Meyers and Matthew Marquart in Foot & Ankle Orthopaedics