Abstract
Background:
The os trigonum (OT)—the most common accessory bone of the foot—although usually asymptomatic, may cause posterior ankle impingement syndrome (PAIS), which may be a severely debilitating problem for recreational or competitive athletes. The aim of the present study was to evaluate effectiveness of posterior ankle arthroscopy and to assess the outcome in the treatment of PAIS secondary to OT impingement or OT fractures within a group of young athletes and their return to previous sports level.
Methods:
From 2011 to 2018, a retrospective review of 81 recreational athletes of mean age 27.8 years was performed. All patients were diagnosed with PAIS due to OT pathology and were operated on endoscopically with resection of the OT. Pre- and postoperative clinical evaluation were performed at 3 months, 1 year, and 2 years based on visual analog scale (VAS), ankle range of motion (ROM), American Orthopaedic Foot & Ankle Society (AOFAS) hindfoot score, and the Foot & Ankle Disability Index (FADI) scores, in a follow-up of at least 2 years.
Results:
VAS score was significantly improved from an average of 7.5 (5-9) preoperatively to 1.9 (1-3) at 3 months postoperatively and to 0.6 (0-2) and 0.3 (0 -1) at 1 and 2 years postoperatively. Ankle ROM was significantly improved from an average of 24.8 (10-35) preoperatively to 58.0 (50-65) at 3 months postoperatively and to 64.0 (50-65) at 1 year and 64.7 (60-65) at 2 years postoperatively. AOFAS and FADI scores were significantly improved from 39.4 (18-55) and 49.7 (42.3-62.5) preoperatively to 85.2 (74-89) and 87.3 (81.7-88.5) postoperatively at 3 months to 97.7 (85-100) and 97.9 (93.3-100) postoperatively at 1 year, respectively (P < .001). Only 5 patients dropped to a lower activity level. There were 5 complications (4 transient).
Conclusion:
Endoscopic treatment of PAIS due to OT pathology demonstrated excellent results. Posterior ankle arthroscopy was an effective treatment and allowed for a prompt return to a high activity level of their athletic performance.
Level of Evidence:
Level IV, therapeutic study / retrospective case series.
Keywords: os trigonum, posterior ankle syndrome, posterior impingement, posterior arthroscopy, hindfoot arthroscopy
Introduction
Over the last 2 decades, posterior arthroscopy (PA) of the ankle improved considerably and became an excellent procedure, as a safe and reliable treatment option for different pathologies of the ankle and hindfoot. 13 The indications for ankle PA has extended to include both intra- and extra-articular pathologies and may involve: (1) bone (hypertrophic posterior talar process, os trigonum [OT], loose bodies, ossicles, post-traumatic ossifications, avulsion fragments, posterior facet talocalcaneal coalition, Haglund’s deformity, osteophytes, posterior tibial, talar or calcaneal fractures, or Cedell fracture); (2) cartilage (posterior talar, tibial, or calcaneal osteochondral defects, arthritis, chondromatosis, talar cystic lesions, intraosseous talar ganglia); or (3) soft tissues (flexor hallucis longus tendinopathy, symptomatic inflammation of the retrocalcaneal bursa, posttraumatic synovitis, villonodular synovitis, and soft-tissue impingement). 9,13,19,25,34,37,38,43,44,48 Most of these conditions (excluding fractures) should initially be treated conservatively; but should these measures fail, or if dealing with high performance young athletes, operative treatment should be considered. 13 It is especially important for the orthopedic surgeon to assess preoperatively in which of these 3 categories the patient belongs, in order to properly treat the problem.
One of the main etiologies for posterior ankle impingement syndrome (PAIS) pain is OT pathology, often due to an acute or chronic fracture. The OT is an inconsistently present accessory bone of the foot situated at the posterolateral aspect of the talus. 24 OT syndrome is the result of an overuse injury of the posterior ankle caused by repetitive plantarflexion stress. It is predominantly seen in ballet dancers and soccer and basketball players and is primarily a clinical diagnosis of exacerbated posterior ankle pain while dancing en pointe or demi-pointe or while doing push-off maneuvers. 27,36
Open and arthroscopic techniques have been used as effective methods in the treatment of PAIS and hindfoot. Advantages of arthroscopic intervention when compared to open procedures have been described in multiple joints and include decreased morbidity, reduced scarring and trauma to the surrounding tissues, and early rehabilitation, recovery, and return to daily and sporting activities. 8,16,39
Accordingly, the purpose of the present study was to evaluate the efficiency and the effectiveness of ankle PA in the treatment of OT pathology in a large number of young athletes. The study was designed to assess the level of function, outcome measures and physical examination parameters in these athletes. The current study would give readers an overview of clinical results after performing a posterior ankle arthroscopy and could help them in managing expectations of their patients, as it offers earlier recovery with less pain, significant improvement in function and restoration of ankle motion with limited complications.
Methods
We retrospectively reviewed the medical records and radiographs of 81 young adult athletes (mean age, 27.4 years; range, 17-46 years; 27 females and 54 males; Table 1) who underwent PA of the ankle for OT fractures (29/81) [acute (11/81); chronic (18/81)] or os trigonum syndrome (52/81) between January 2011 to January 2018. Among the 81 patients, 18 were ballet dancers, 15 dancers, 15 soccer players, 13 basketball players, 4 volleyball players, 5 polo-players, 5 cyclists, 4 marathon runners, and 2 sprinters (Table 1).
Table 1.
Patient Demographics.
| Variable | |
| Age, mean (range); SD | 27.4 (17-46); 8.08 |
| Gender, n | |
| Male | 54 |
| Female | 27 |
| BMI, mean (range); SD | 20.8 (15.9-27.7); 5.86 |
| Etiology, n | |
| OT fracture acute | 11 |
| OT fracture chronic | 18 |
| OT impingement | 52 |
| Sport, n | |
| Ballet-dancers | 18 |
| Dancers | 15 |
| Soccer players | 15 |
| Basketball players | 13 |
| Volleyball players | 04 |
| Polo-players | 05 |
| Cyclists | 05 |
| Marathon runners | 04 |
| Sprinters | 02 |
Abbreviations: BMI, body mass index; OT, os trigonum.
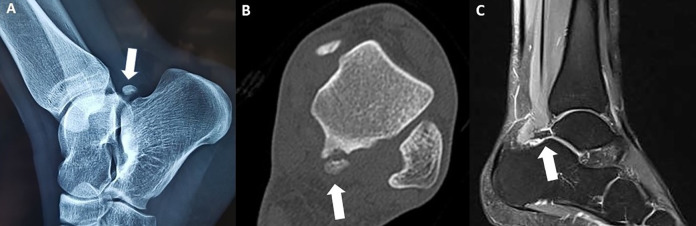
The diagnosis of PAIS was based primarily on a history of posterior ankle and hindfoot pain and the physical examination. Clinical symptoms included deep posterior ankle pain, especially during forced plantarflexion of the ankle (the so-called nutcracker sign), weakness, persistent swelling, locking and catching, or stiffness and limited range of motion on weight bearing. On physical examination, there was tenderness to palpation of the posterior aspect of the talus. The posterior talar process could best be palpated posterolateral, between the peroneal tendons and the Achilles tendon. The passive forced plantarflexion was positive in all the patients. Afterwards, ankle radiographs (anteroposterior and lateral) (Figure 1A), CT (Figure 1B), and magnetic resonance imaging (MRI) scan (Figure 1C) were performed in all cases. CT scanning is the imaging method of choice in cases when posterior talus structure fractures, including an OT fracture, are suspected (Figure 1B). 3,20,24 All patients completed a conservative therapy period of a minimum of 3 months, which included rest, anti-inflammatory medication, controlled ankle motion boot, and physical therapy.
Figure 1.
(A) Preoperative ankle radiograph (lateral view) showing the os trigonum (OT) in the posterior talus area, as indicated by an arrow. (B) Preoperative ankle computed tomographic scan showing the fractured OT after ankle injury. (C) Preoperative ankle magnetic resonance imaging (MRI) showing the OT pathology of the patient.
Patients were athletes with posterior bony impingement due to OT pathology. In order to avoid selection bias as well as a successful group homogeneity, the following groups were excluded from the study: (1) patients with PAIS but not recreational athletes, (2) patients with PAIS due to cartilage or soft tissue pathology, (3) pathology of the anterior and posterior compartments of the ankle that required combined anterior and posterior arthroscopies, (4) patients with PAIS and ankle instability (positive anteroposterior drawer and radiographically >10 degrees of talar tilt or >10 mm of anterior displacement), (5) patients with ankle active infection, and (6) patients with restricted foot and ankle blood supply (>50% lower limb arterial stenosis on ultrasound).
Outcome Measures
Clinical evaluation was performed preoperatively and then at 12 months and at 2 years postoperatively. The outcome measures included the pain visual analog scale (VAS), the ankle range of motion (ROM) using a goniometer (and compared to the contralateral extremity), the American Orthopaedic Foot & Ankle Society (AOFAS) hindfoot score, and the Foot & Ankle Disability Index (FADI) score. The scores were measured in the clinic by 2 orthopedic surgeons for better reliability (the same in each scheduled evaluation): 1 interobserver (the orthopedic surgeon who performed the operation) and 1 extra observer (orthopedic surgeon of the Orthopaedic Research Institute for Education and Training). An AOFAS score greater than 90 was defined as excellent, 84 to 90 as good, 65 to 83 as fair, and less than 65 as poor. Any complications were noted, including numbness, subjective sensation of Achilles tightness, infection, etc. The study also reported when the athletes and dancers returned to their activity and if they had reached the prior level of activity or if it was diminished. Lastly, we conducted longer follow-ups at 2-5 years.
Operative Technique
All patients underwent an endoscopic approach in the treatment of OT PAIS, based on the technique described in detail by van Dijk. 42,44,46 The procedure was performed under general or regional anesthesia, epidural block. The patient was placed in a prone position, with a tourniquet to be applied around the upper leg (thigh) and a small support under the lower leg, making it possible to move the ankle freely (Figure 2). Arthroscopically, the os trigonum was removed and the flexor hallucis longus was released in all the cases. A 4.0-mm 30-degree arthroscope was routinely used from a posterolateral and a posteromedial portal (Figure 3). After removal of the Kager fat pad, fibrous tissue, and the thin joint capsule, the ankle joint was accessed and inspected. Removal of a symptomatic os trigonum or treatment of a nonunion of a posterior talar process fracture, or a fractured OT-involved partial detachment of the posterior talofibular ligament, release of the flexor retinaculum, and release of the posterior talocalcaneal ligament (Figure 3). The os trigonum was lifted from the subtalar joint by means of a small-sized bone elevator and removed finally with a grasper. At the end of the procedure, bleeding was controlled by radiofrequency electrocautery, and the skin was closed with nonabsorable sutures. A sterile compression dressing was applied. Average total operative time was 50 minutes (SD 12 minutes).
Figure 2.
(A) The posterolateral portal is the first portal to be made, in front of the Achilles tendon is a line from the tip of the lateral malleolus to the Achilles tendon, parallel to the sole of the foot. (B) The posteromedial portal is the second portal be made at the same level as posterolateral. (C) The position of the 30-degree arthroscope and the shaver during the posterior arthroscopic operation.
Figure 3.
Operative arthroscopic images of different cases: (A) Os trigonum (OT). (B) Removing with arthroscopic grasp the OT. (C) Release of flexor hallucis longus tendon with flexor retinaculum. (D) Large OT removal with arthroscopic grasp. (E) Large OT. (F) Detaching OT from the posterior talus area.
Postoperative Care
The postoperative regimen was a functional one that consisted of a 3-week period of partial weightbearing on crutches, followed by full weight bearing. All patients were placed in a well-padded splint or soft tissue dressing and controlled ankle motion walking orthotic boot with the ankle maintained in neutral position. The patients were advised to begin range of motion exercises as soon as possible after surgery. At approximately 3 weeks postoperatively, ankle strengthening was initiated, whereas transition to sports or activity-specific rehabilitation was performed as symptoms dictated, generally 5-6 weeks postoperatively.
Statistical Analysis
Statistical analysis was performed using SPSS, version 25.0 (IBM Corp, Armonk, NY). Friedman analysis of variance and Wilcoxon signed-rank test were conducted for the evaluation of changes in AOFAS, FADI, and VAS score and ROM parameters. A P value of less than .05 was considered statistically significant.
Ethical Approval
The local ethics committee of the Central Clinic of Athens (Orthopaedic Research Institute for Education and Training) approved the study, which was carried out according to the World Medical Association Declaration of Helsinki. Institutional review board approval and written consent from all patients were obtained. 11
Results
The VAS score was statistically significantly improved from an average of 7.5 (5-9) preoperatively to 1.9 (1-3) at 3 months postoperation and to 0.6 (0-2) at 1 year postoperation and 0.3 (0-1) at 2 years postoperation (P < .001) (Table 2). Also, the ankle ROM was statistically significantly improved from 24.8 (10-35) preoperation to 58.0 degrees (50-65) at 3 months postoperation and to 64.0 (50-65) at 1 year postoperation and 64.7 (60-65) at 2 years postoperation (P < .001) (Table 3). The VAS score had significantly improvement between the preoperative and 3-month postoperative time points, but also between 3 months and 1 year postoperation and between 1 and 2 years postoperation. In ankle ROM, there were significantly improvements between the preoperative and the 3-month postoperative time points, and between 3 months and 1 year postoperation, but there was no statistical significance between 1 and 2 years postoperation.
Table 2.
VAS Score Results and Statistics.
| Mean (Range) | SD | Wholea | 3 mo Postop – Preopb | 1 y Postop – Preopb | 1 y Postop – 3 mo Postopb | 2 y Postop – 1 y Postopb | |
|---|---|---|---|---|---|---|---|
| Preop | 7.5 (5-9) | 1.2 | P < .001 | P < .001 | P < .001 | P < .001 | P < .001 |
| Postop 3 mo | 1.9 (1-3) | 0.7 | χ2(3) = 225.296 | z = –7.879 | z = –7.877 | z = –7.439 | z = –4.512 |
| Postop 1 y | 0.6 (0-2) | 0.6 | |||||
| Postop 2 y | 0.3 (0-1) | 0.4 |
Abbreviations: Postop, postoperative; Preop, preoperative; VAS, visual analog scale.
a Friedman analysis of variance.
b Wilcoxon signed-rank test.
Table 3.
ROM Results and Statistics.
| Mean (Range) | SD | Wholea | 3 mo Postop – Preopb | 1 y Postop – Preopb | 1 y Postop – 3 mo Postopb | 2 y Postop – 1 y Postopb | |
|---|---|---|---|---|---|---|---|
| Preop | 24.8 (10-35) | 6.3 | P < .001 | P < .001 | P < .001 | P < .001 | P < .001 |
| Postop 3 mo | 58.0 (50-65) | 4.9 | χ2(3) = 220.661 | z = –7.863 | z = –7.872 | z = –6.949 | z = –2.935 |
| Postop 1 y | 64.0 (50-65) | 2.4 | |||||
| Postop 2 y | 64.7 (60-65) | 1.0 |
Abbreviations: Postop, postoperative; Preop, preoperative; ROM, range of motion.
a Friedman analysis of variance.
b Wilcoxon signed-rank test.
Furthermore, the AOFAS and FADI scores were statistically significant improved from 39.4 (18-55) and 49.7 (42.3-62.5) preoperatively to 85.2 (74-89) and 87.3 (81.7-88.5) postoperatively at 3 months, and to 97.7 (85-100) and 97.9 (93.3-100) 1 year postoperation, respectively (P < .001) (Tables 3 and 4). There was also improvement in AOFAS and FADI scores from 1 to 2 years (Tables 3 and 4).
Table 4.
AOFAS Score Results and Statistics.
| Mean (Range) | SD | Wholea | 3 mo Postop – Preopb | 1 y Postop – Preopb | 1 y Postop – 3 mo Postopb | 2 y Postop – 1 y Postopb | |
|---|---|---|---|---|---|---|---|
| Preop | 39.4 (18-55) | 9.5 | P < .001 | P < .001 | P < .001 | P < .001 | P < .001 |
| Postop 3 mo | 85.2 (74-89) | 4 | χ2(3) = 233.407 | z = –7.820 | z = –7.821b | z = –7.796 | z = –5.474 |
| Postop 1 y | 97.7 (85-100) | 2.4 | |||||
| Postop 2 y | 99.0 (87-100) | 1.8 |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; Postop, postoperative; Preop, preoperative.
a Friedman analysis of variance.
b Wilcoxon signed-rank test.
At the time of the last follow-up, there were 76 patients (93.8%) with excellent and very good results and 5 (6.2%) with good results based on the AOFAS score. Seventy-six patients were active at the same level as that prior to PAIS, whereas 5 dropped to a lower activity level. The patients began a return to their activity after a minimum of 8 weeks, and all of them were back within a maximum of 12 weeks (mean 9.1 weeks). The 5 athletes (3 ballet dancers, 1 dancer, and 1 soccer player) that dropped to a lower activity level consisted of cases with multiple previous ankle sprains and OT fracture or pathology. Also, in all cases, the patients had received conservative therapy for a period of 4-6 months and had received at least 1 local injection of steroids. When they were operated on, there was an existing copathology of cartilage defects and primary posterior ankle arthritis, as detected on MRIs.
Furthermore, with regard to operative complications, there were 4 transient complications: 1 woman with 2 months of drainage at the medial portal due to fat pad atrophy and skin healing issues after 2 local injections of cortisone the last 4 months before operation and 3 additional transient sural nerve neurapraxia. There was also 1 more serious and rare complication. A 21-year-old male ballet dancer, whose pain decreased significantly postoperatively but the ROM had a limitation of 5 degrees in plantarflexion and less than 5 degrees in dorsiflexion. That limitation began after the first postoperative month and took a turn for the worse by the third month. A new MRI showed arthrofibrosis, mainly on the posterior part of the ankle joint and less so on the anterior part. Physical therapy, nonsteroidal anti-inflammatory medication, and corticosteroid injection were administered without significant improvement. After the sixth postoperative month, the patient underwent removal of the scar tissue via anterior and posterior arthroscopy. The result was finally positive with nearly full ankle ROM (limitation of only 3 degrees in dorsiflexion) and an AOFAS and FADI score of 97 and 98, respectively, at the last follow-up (Table 5). For the remaining 76 patients, there were no complications.
Table 5.
FADI Score Results and Statistics.
| Mean (Range) | SD | Wholea | 3 mo Postop – Preopb | 1 y Postop – Preopb | 1 y Postop – 3 mo Postopb | 2 y Postop – 1 y Postopb | |
|---|---|---|---|---|---|---|---|
| Preop | 49.7 (42.3-62.5) | 6.2 | P < .001 | P < .001 | P < .001 | P < .001 | P < .001 |
| Postop 3 mo | 87.3 (81.7-88.5) | 1.5 | χ2(3) = 237.650 | z = –7.824 | z = –7.824 | z = –7.837 | z = –6.558 |
| Postop 1 y | 97.9 (93.3-100) | 1.8 | |||||
| Postop 2 y | 99.3 (95.2-100) | 0.8 |
Abbreviations: FADI, Foot & Ankle Disability Index; Postop, postoperative; Preop, preoperative.
a Friedman analysis of variance.
b Wilcoxon signed-rank test.
Discussion
The present study evaluated the endoscopic treatment of PAIS due to OT pathology in athletes and showed good to excellent results. The posterior ankle arthroscopy was minimally invasive, safe, and effective for treatment of bony PAIS, offering a quick recovery and allowing for a prompt return to a preinjury activity. They had good clinical scores from the first 3 postoperative months after endoscopic treatment and consecutive improvement up until the first postoperative year. The athletes in our study returned to preinjury level of athletic performance on an average of 9.1 ± 1.3 weeks (range 7-12). The current results in terms of patients’ prompt return to sports after surgery are comparable to the mean time of 47 days (6.7 weeks) of López Valerio et al 22 and the 41 days of Calder et al 7 (Table 6).
Table 6.
Outcome and Complications of Studies: Arthroscopic Procedure of PAIS.
| Study | Year of Publication | No. of Patients | Age (y) | Athletes | Follow-up (Mean) |
VAS Score | AOFAS Score | ROM | Complications | Return to Sport |
|---|---|---|---|---|---|---|---|---|---|---|
| Carreira et al 8 | 2016 | 20 | 21 | 19 | 38.2 mo | Sign. | Sign. | Nonsign. Exception plantarflexion |
15% neuritis | NR |
| López Valeiro et al 22 | 2015 | 20 | 24.8 | 20 (soccer players) |
7 y | Sign. | NR | NR | None | 46.9 d |
| van Dijk et al 43 | 2009 /2008 | 55 | 29 | General Population | 36 mo | NR | Sign. | NR | 1 temporary loss of sensation of the posteromedial aspect of the heel | 8 wk |
| Galla and Lobenhoffer 12 | 2011 | 36 | 46 | General population (not professionals) | 9.7 mo | Sign. | NR | NR | 3.3% superficial infection 3.3% deep wound infection 6.6% sensitivity of sural nerve 6.6% required resurgery |
NR |
| Ogut et al 30 | 2011 | 59 | 36.9 | NR | 26.7 mo | NR | Sign |
NR | 2/59 sural nerve | 8 wk |
| Calder et al 7 | 2010 | 27 | 25 | 27 | 23 mo | NR | NR | NR | 1/27 leakage 1/27 3 mo post- pain |
41 d |
| Nickisch 28 | 2012 | 186 34 PAIS |
37.1 | NR | 17 ±13 mo | NR | NR | NR | 4 tibial nerve neurapraxia (1 permanent) 3 sural nerve neurapraxia 4 tightness of the Achilles tendon 2 complex regional pain syndrome 2 infections 1 cyst at the posteromedial portal |
NR |
| Park et al 32 | 2013 | 23 | NR | 20 11 soccer 6 basketball 1 baseball 1 gymnast 1 taekwondo |
18 mo | Sign. | Sign. | Sign. | None | 6.7 wk |
| Noguchi et al 29 | 2010 | 12 | 21.4 | 12 7 soccer 1 ballet 1 baseball 1 rugby 1 kendo 1 volleyball |
33.8 mo | Sign. | NR | 1 transient sural nerve neurapraxia | 5.9 wk | |
| Ahn et al 2 | 2013 | 28 | 29.8 | 28 (amateur athletes and dancers) |
30 | Sign. | Sign. | Sign. | 1 transient sural nerve neurapraxia (each group) | 8 wk (endoscopy) 7.5 wk (arthroscopy) |
| Willits et al 47 | 2008 | 23 (15 in last follow-up) |
25 | 23 | 32 | NR | Sign. | Sign. | 5 temporary numbness (scar region) 1 temporary ankle stiffness |
5.8 mo |
| Nikolopoulos et al (this study) | 2020 | 81 | 27.8 | 81 | 2 y (2-5) | Sign. | Sign. | Sign. | 1 leakage 3 transient sural nerve neurapraxia 1 scar tissue posteriorly (ankle stiffness) |
9.1 wk |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; BMI, body mass index; NR, nonreferred; Nonsign., no statistically significant improvement; OT, os trigonum; PAIS, posterior ankle impingement syndrome; ROM, range of motion; Sign., statistically significant improvement; VAS, visual analog score
It is well known that the OT is one of the largest and most common accessory ossicles in the ankle and foot region, with an estimated prevalence of 1% to 25% and in some cases it can be fragmented or bipartite. 1,3,6,21,24 In ballet dancers, it has a reported prevalence of 30%, which may be attributed to repetitive forced plantarflexion in ballet training during the skeletal maturation phase of development that precedes the closure of the ossification center. 26,33,45 Apart from ballet dancers, other sports with an inherent risk of OT syndrome include soccer, cricket, downhill running or walking, running or sprinting, swimming, and sports involving kicking. 15,36,40 Ankle overuse or acute trauma can lead to a fracture of the Stieda process (posterior process fracture of the talus), 5 cartilaginous synchondrosis disruption, os trigonum fracture, or an avulsion injury of the posterior talofibular ligament.
Symptoms typically diminish initially with rest from the triggering activity. In young athletes, symptomatic OT syndrome decreases range of motion in plantarflexion, as observed also in the current study. Physical examination reveals posterolateral tenderness on palpation, typically between the Achilles and peroneal tendons. 5,36 Passive maximal plantarflexion may reproduce the patient’s symptoms. Os trigonum syndrome often coexists with FHL tenosynovitis in the same patient population. Repetitive plantarflexion leads to constant pressure exerted on the os trigonum by the FHL tendon, leading to tenosynovitis. 41 In the setting of concomitant FHL tenosynovitis, patients may report episodes of the ankle giving way, triggering of the hallux, pain on palpation of the posteromedial ankle between the Achilles tendon and the medial malleolus, or pain over the FHL tendon at the level of the ankle/hindfoot with active contraction or passive stretching. 41
Routine ankle radiographs may suggest posterior osteophytes, a large Stieda process, or os trigonum. In cases of ankle trauma, to diagnose a Stieda process or an OT acute fracture, a CT scan can be helpful to look for multiple fragments and hidden posterior pathology. 49 MRI is also helpful and can depict fluid with edema in the posterior talar region. MRI has the added advantage of showing injuries of the articular surfaces, ligaments, and tendons; other entities in the differential diagnosis; and to assist in deciding the most likely cause of the patient’s symptoms. 10,17,31,39 Local anesthetic injection can also help confirm the diagnosis and can combined with a corticosteroid for treatment purposes. 39 Consequently, the combination of clinical examination, CT and MRI scans and local anesthetic injection are all helpful for the final diagnosis of PAIS; for these reasons, they were performed on all 81 athletes in our study.
The differential diagnosis of OT syndrome is particularly important; in order to decide the best therapeutic option, especially in young athletes. PAIS can be associated with accessory muscles 4,16 or by an accessory ligament, such as the posterior intermalleolar ligament or by scar tissue that typically forms in the gutter of the posteromedial ankle after multiple ankle sprains. 15 In acute trauma, the differential diagnosis includes the Shepherd fracture, the OT fracture, and synchondrosis disruption. Nevertheless, other conditions that require diagnosis include Achilles tendinitis, FHL tenosynovitis, tarsal tunnel syndrome, sural nerve entrapment, osteoid osteoma, calcaneal apophysitis, retrocalcaneal bursitis, osteochondritis dissecans, subtalar coalition, stress fracture, and osteoarthritis. With the current roster of patients, the differential diagnosis was especially important in the study’s inclusion criteria as only bony PAIS was accepted (homogeneity of the group).
Conservative treatment ranging from 6 weeks to 3 months was required of all our patients (rest, cessation of activity, technique modification, nonsteroidal anti-inflammatory agents, ice, physical therapy, injections, and immobilization). If no clinical improvement was noted, an arthroscopic excision of OT was suggested. Arthroscopic excision shows equally good results as the older open techniques, 14,18,35 with the advantage of smaller incisions, minimal operative morbidity, and shorter recovery time. 23,25,34,42,43 Contraindication would be simultaneous posterior tarsal tunnel nerve entrapment, which would also require a medial incision. 39
In 2000, van Dijk et al 42 described the use of posterior hindfoot endoscopy with posteromedial and posterolateral portals for OT resection with minimal complications with hastened return to sports. Since then, a small number of studies have been published mainly on arthroscopic resection of OT in athletes (Table 6.) In 2009 van Dijk et al, 43 and in 2008 Scholten et al 38 presented their experience with 55 patients with PAIS who were treated with an endoscopic removal of bone fragments and/or scar tissue. The symptoms were caused by trauma (65%) or overuse (35%). The median AOFAS hindfoot score increased from 75 points preoperatively to 90 points at the time of final follow-up. The median time to return to work and sports activities were 2 and 8 weeks, respectively. At the time of follow-up, patients in the overuse group were more satisfied than those in the post-traumatic group, and the AOFAS hindfoot scores were higher in patients in the overuse group (median, 100 points) compared with patients in the posttraumatic group (median, 90 points). 38,42 In our cases, we have not observed any difference in the scores between the 2 groups (OT fracture vs overuse) (Table 6). Furthermore, Carreira et al presented the results of 20 patients who underwent arthroscopic treatment for OT, tibial exostosis, talar exostosis, loose body or fracture nonunion, and ganglion cyst removal, and were followed up with prospectively at a mean of 38.2 months. Nineteen of 20 patients were competitive athletes. At the final follow-up, VAS pain and AOFAS hindfoot scores showed significant improvement (P < .01) pre- to postoperatively. Fifteen percent of patients reported postoperative neuritis (Table 6). 8 López Valerio et al also presented in 2015, 20 soccer players with significant improvement of pain after the endoscopy; whereas the mean time to return to previous level of sports was 46.9 days, reaching the same pre-lesion Tegner level. 22 Similar results were reported by Galla and Lobenhoffer 12 and Ogut et al, 30 whereas in Calder et al’s study 7 of 28 professional soccer players treated for soft-tissue or bony PAIS, the players returned to training and competition in 34 and 41 days, respectively. The complications, reported in Table 6, were, however, nonserious. Many complications after posterior ankle and hindfoot arthroscopies were reported by Nickisch et al 28 on 186 patients (only 34 of all for PAIS) where OT excision were performed with/without FHL tenolysis. Willits et al also presented the results of 23 patients who underwent 24 posterior ankle arthroscopies at a mean follow-up time of 32 months. The average time to return to work was 1 month (range, 0-3) and to sports, 5.8 months (range, 1-24). Fourteen patients returned to their preinjury level of athletics. 47 Park et al noted significant improvement after arthroscopy for OT syndrome as the result of a traumatic ankle injury, in a study of 23 patients (20 athletes). Park et al used 3 arthroscopic portals and performed the procedures in the lateral decubitus position. The mean time to return to sport was 6.7 weeks, and no major complications were reported (Table 6). 32 Similarly, Noguchi et al reported subtalar arthroscopic resection of bony impingement in the lateral decubitus position, on 12 young athletes, with statistically significant improvement of AOFAS score and ROM. The average time to return to sport was 5.9 weeks. 29 Lastly, Ahn et al compared the outcomes in 28 patients (amateur athletes and dancers) treated with excision of the OT either by an arthroscopic (16 patients) or endoscopic (12 patients) technique. Both groups had substantially improved VAS and AOFAS scores postoperatively, with no significant difference between the groups. In addition, the mean operative time and the time to return to sport were similar for both groups. Transient sural nerve dysesthesia was reported in 2 patients. The authors concluded that both techniques are safe and effective, but that subtalar arthroscopy is more challenging. They recommend the use of posterior endoscopy for patients with an OS >135 mm2 and for those with concomitant FHL tendinitis or other posterior ankle conditions. In patients with concomitant talar osteochondritis dissecans, anterior ankle impingement, or sinus tarsi syndrome, the arthroscopic technique is the technique of choice (Table 6). 2
Comparing the aforementioned studies with ours, it is important to mention that we had the advantage of analyzing in detail the results of a great number of athletes (81 patients) with PAIS due to bony impingement pathology from acute or chronic OT fractures and OT syndrome (homogeneity in the group). In many of the previous published studies, there were some limitations. First, there was a limited sample size; second, there was heterogeneity within the patient sample (different categories of general population and athletes); and third, they performed posterior or hindfoot arthroscopy for different indications, including both intra- and extra-articular pathologies (cartilage, soft tissue, bony, arthritis). The present study treated solely bony pathology in accordance with FHL pathology, which in our experience was simple synovectomy and debridement (release). Lastly, in all of our cases, we analyzed detailed results of clinical and functional scores (VAS, AFAS, FADI scores, ankle ROM, return to sport); whereas in many of the previous studies, there were no outcome measures of higher level functioning which quantitatively demonstrated restoration of motion, with the exception of Carreira et al. 8
Conclusion
Hindfoot or PA arthroscopy has become the primary method for treating OT fractures and PAIS in young athletes. In the current study, use of the arthroscopic approach demonstrated a significant increase in postoperative AOFAS, FADI, VAS scores, and ankle ROM from preoperative levels, with only minimal complications among patients. With PA, we have succeeded in maintaining or restoring anatomic ankle and hindfoot ROM, ability to return to a previous level of activity, as well as improvement in objective assessment of pain relief and an overall marked level of functionality.
Supplemental Material
Supplemental Material, FAO945330-ICMJE for Endoscopic Treatment of Posterior Ankle Impingement Secondary to Os Trigonum in Recreational Athletes by Dimitrios Nikolopoulos, George Safos, Konstantinos Moustakas, Neoptolemos Sergides, Petros Safos, Athanasios Siderakis, Dimitrios Kalpaxis and Andreas Moutsios-Rentzos in Foot & Ankle Orthopaedics
Footnotes
Ethics Approval: Ethical approval for this study was obtained from the Orthopaedic Research Institute for Education and Training in Athens, Greece (No 05 / 11.01.2011).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Dimitrios Nikolopoulos, MD, PhD,  https://orcid.org/0000-0003-1083-5039
https://orcid.org/0000-0003-1083-5039
References
- 1. Abramowitz Y, Wollstein R, Barzilay Y, et al. Outcome of resection of a symptomatic os trigonum. J Bone Joint Surg Am. 2003;85:1051–1057. [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Kim YC, Kim HY. Arthroscopic versus posterior endoscopic excision of a symptomatic os trigonum: a retrospective cohort study. Am J Sports Med. 2013;41(5):1082–1089. [DOI] [PubMed] [Google Scholar]
- 3. Anwar R, Nicholl JE. Non-union of a fractured os trigonum. Injury. 2005;36:267–270. [Google Scholar]
- 4. Best A, Giza E, Linklater J, Sullivan M. Posterior impingement of the ankle caused by anomalous muscles: a report of four cases. J Bone Joint Surg Am. 2005; 87(9):2075–2079. [DOI] [PubMed] [Google Scholar]
- 5. Brodsky AE, Khalil MA. Talar compression syndrome. Am J Sports Med. 1986;14(6):472–476. [DOI] [PubMed] [Google Scholar]
- 6. Bureau NJ, Cardinal E, Hobden R, Aubin B. Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology. 2000;215:497–503. [DOI] [PubMed] [Google Scholar]
- 7. Calder JD, Sexton SA, Pearce CJ. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38(1):120–124. [DOI] [PubMed] [Google Scholar]
- 8. Carreira DS, Vora AM, Hearne KL, Kozy J. Outcome of arthroscopic treatment of posterior impingement of the ankle. Foot Ankle Int. 2016;37(4):394–400. [DOI] [PubMed] [Google Scholar]
- 9. de Leeuw PAJ, van Sterkenburg MN, van Dijk CN. Arthroscopy and endoscopy of the ankle and hindfoot. Sports Med Arthrosc Rev. 2009;17:175–184. [DOI] [PubMed] [Google Scholar]
- 10. Donovan A, Rosenberg ZS. MRI of ankle and lateral hindfoot impingement syndromes. AJR Am J Roentgenol. 2010;195(3):595–604. [DOI] [PubMed] [Google Scholar]
- 11. Fuson RL, Sherman M, Van Vleet J, Wendt T. The conduct of orthopaedic clinical trials. J Bone Joint Surg Am. 1997;79:1098. [DOI] [PubMed] [Google Scholar]
- 12. Galla M, Lobenhoffer P. Technique and results of arthroscopic treatment of posterior ankle impingement. Foot Ankle Surg. 2011;17(2):79–84. [DOI] [PubMed] [Google Scholar]
- 13. Gasparetto F, Collo G, Pisanu G, et al. Posterior ankle and subtalar arthroscopy: indications, technique, and results. Curr Rev Musculoskelet Med 2012;5(2):164–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Georgiannos D, Bisbinas I. Endoscopic versus open excision of os trigonum for the treatment of posterior ankle impingement syndrome in an athletic population: a randomized controlled study with 5-year follow-up. Am J Sports Med. 2017;45(6):1388–1394. [DOI] [PubMed] [Google Scholar]
- 15. Giannini S, Buda R, Mosca M, et al. Posterior ankle impingement. Foot Ankle Int. 2013;34:459–465. [DOI] [PubMed] [Google Scholar]
- 16. Hamilton WG, Geppert MJ, Thompson FM. Pain in the posterior aspect of the ankle in dancers: differential diagnosis and operative treatment. J Bone Joint Surg Am. 1996;78(10):1491–1500. [DOI] [PubMed] [Google Scholar]
- 17. Hayashi D, Roemer FW, D’Hooghe P, Guermazi A. Posterior ankle impingement in athletes: pathogenesis, imaging features and differential diagnoses. Eur J Radiol. 2015;84(11):2231–2241. [DOI] [PubMed] [Google Scholar]
- 18. Heyer JH, Rose DJ. Os trigonum excision in dancers via an open posteromedial approach. Foot Ankle Int. 2017;38(1):27–35. [DOI] [PubMed] [Google Scholar]
- 19. Keeling JJ, Guyton GP. Endoscopic flexor hallucis longus decompression: a cadaver study. Foot Ankle Int. 2007;28:810–814. [DOI] [PubMed] [Google Scholar]
- 20. Kose O, Okan AN, Durakbasa MO, et al. Fracture of the os trigonum: a case report. J Orthop Surg. 2006;14(3):354–356. [DOI] [PubMed] [Google Scholar]
- 21. Lawson JP. Symptomatic radiographic variants in extremities. Radiology. 1985;157(3):625–631. [DOI] [PubMed] [Google Scholar]
- 22. López Valerio V, Seijas R, Alvarez P, et al. Endoscopic repair of posterior ankle impingement syndrome due to os trigonum in soccer players. Foot Ankle Int. 2015;36(1):70–74. [DOI] [PubMed] [Google Scholar]
- 23. Marumoto JM, Ferkel RD. Arthroscopic excision of the os trigonum: a new technique with preliminary clinical results. Foot Ankle Int. 1997;18(12):777–784. [DOI] [PubMed] [Google Scholar]
- 24. Mellado JM, Ramos A, Salvado E, et al. Accessory ossicles and sesamoid bones of the ankle and foot: imaging findings, clinical significance and differential diagnosis. Eur Radiol. 2003;13(suppl 4):L164–L177. [DOI] [PubMed] [Google Scholar]
- 25. Morag G, Maman E, Arbel R. Endoscopic treatment of hindfoot pathology. Arthroscopy. 2003;19:E13. [DOI] [PubMed] [Google Scholar]
- 26. Moser BR. Posterior ankle impingement in the dancer. Curr Sports Med Rep. 2011;10(6):371–377. [DOI] [PubMed] [Google Scholar]
- 27. Nault ML, Kocher MS, Micheli LJ. Os trigonum syndrome. J Am Acad Orthop Surg. 2014;22(9):545–553. [DOI] [PubMed] [Google Scholar]
- 28. Nickisch F, Barg A, Saltzman CL, et al. Postoperative complications of posterior ankle and hindfoot arthroscopy. J Bone Joint Surg Am. 2012;94(5):439–446. [DOI] [PubMed] [Google Scholar]
- 29. Noguchi H, Ishii Y, Takeda M. Arthroscopic excision of posterior ankle bony impingement for early return to the field: short-term results. Foot Ankle Int. 2010;31(5):398–403. [DOI] [PubMed] [Google Scholar]
- 30. Ogut T, Ayhan E, Irgit K, Sarikaya AI. Endoscopic treatment of posterior ankle pain. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1355–1361. [DOI] [PubMed] [Google Scholar]
- 31. Özer M, Yıldırım A. Evaluation of the prevalence of os trigonum and talus osteochondral lesions in ankle magnetic resonance imaging of patients with ankle impingement Syndrome. J Foot Ankle Surg. 2019;58(2):273–277. [DOI] [PubMed] [Google Scholar]
- 32. Park CH, Kim SY, Kim JR, Lee WC. Arthroscopic excision of a symptomatic os trigonum in a lateral decubitus position. Foot Ankle Int. 2013;34(7):990–994. [DOI] [PubMed] [Google Scholar]
- 33. Peace KA, Hillier JC, Hulme A, Healy JC. MRI features of posterior ankle impingement syndrome in ballet dancers: a review of 25 cases. Clin Radiol. 2004;59(11):1025–1033. [DOI] [PubMed] [Google Scholar]
- 34. Ribbans WJ, Ribbans HA, Cruickshank JA, Wood EV. The management of posterior ankle impingement syndrome in sport: a review. Foot Ankle Surg. 2015; 21(1):1–10. [DOI] [PubMed] [Google Scholar]
- 35. Rietveld ABMB, Hagemans FMT. Operative treatment of posterior ankle impingement syndrome and flexor hallucis longus tendinopathy in dancers open versus endoscopic approach. J Dance Med Sci. 2018;22(1):11–18. [DOI] [PubMed] [Google Scholar]
- 36. Russell JA, Kruse DW, Koutedakis Y, et al. Pathoanatomy of posterior ankle impingement in ballet dancers. Clin Anat. 2010;23(6):613–621. [DOI] [PubMed] [Google Scholar]
- 37. Scholten PE, Altena MC, Krips R, van Dijk CN. Treatment of a large intraosseous talar ganglion by means of hindfoot endoscopy. Arthroscopy. 2003;19:96–100. [DOI] [PubMed] [Google Scholar]
- 38. Scholten PE, Sierevelt IN, van Dijk CN. Hindfoot endoscopy for posterior ankle impingement. J Bone Joint Surg Am. 2008;90(12):2665–2672. [DOI] [PubMed] [Google Scholar]
- 39. Stone JW, Ferkel RD. Osteophytes, loose bodies, posttraumatic problems, and foreign bodies. In: Ferkel RD, ed. Foot and Ankle Arthroscopy 2017. 2nd ed. Philadelphia, PA: Wolters Kluwer; 245–246. [Google Scholar]
- 40. Tol JL, Slim E, van Soest AJ, et al. The relationship of the kicking action in soccer and anterior ankle impingement syndrome. A biomechanical analysis. Am J Sports Med. 2002;30:45–50. [DOI] [PubMed] [Google Scholar]
- 41. Uzel M, Cetinus E, Bilgic E, Karaoguz A, Kanber Y. Bilateral os trigonum syndrome associated with bilateral tenosynovitis of the flexor hallucis longus muscle. Foot Ankle Int. 2005;26(10):894–898. [DOI] [PubMed] [Google Scholar]
- 42. van Dijk CN. Ankle arthroscopy. Techniques Developed by the Amsterdam Foot and Ankle School. Cham, Switzerland: Springer; 2014. [Google Scholar]
- 43. van Dijk CN, de Leeuw PAJ, Scholten PE. Hindfoot endoscopy for posterior ankle impingement. Surgical technique. J Bone Joint Surg Am. 2009;91:287–298. [DOI] [PubMed] [Google Scholar]
- 44. van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871–876. [DOI] [PubMed] [Google Scholar]
- 45. Watkins CA Dogas DC. The os trigonum: a discussion and case report. Arch Pod Med Surg. 1976;3:17–26. [Google Scholar]
- 46. Wiegerinck JI, Vroemen JC, van Dongen TH, et al. The posterior impingement view: an alternative conventional projection to detect bony posterior ankle impingement. Arthroscopy. 2014;30(10):1311–1316. [DOI] [PubMed] [Google Scholar]
- 47. Willits K, Sonneveld H, Amendola A, et al. Outcome of posterior ankle arthroscopy for hindfoot impingement. Arthroscopy. 2008;24(2):196–202. [DOI] [PubMed] [Google Scholar]
- 48. Yilmaz C, Eskandari MM. Arthroscopic excision of the Talar Stieda’s process. Arthroscopy. 2006;22:225.e1–225.e3. [DOI] [PubMed] [Google Scholar]
- 49. Zwiers R, Baltes TPA, Opdam KTM, et al. Prevalence of os trigonum on CT imaging. Foot Ankle Int. 2018;39(3):338–342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO945330-ICMJE for Endoscopic Treatment of Posterior Ankle Impingement Secondary to Os Trigonum in Recreational Athletes by Dimitrios Nikolopoulos, George Safos, Konstantinos Moustakas, Neoptolemos Sergides, Petros Safos, Athanasios Siderakis, Dimitrios Kalpaxis and Andreas Moutsios-Rentzos in Foot & Ankle Orthopaedics