Abstract
Background:
The most frequent complication after Weil osteotomies is a floating toe deformity, but there are no reports about its effect on the patient. In this study, we analyzed the consequences of floating toe deformities after the performance of a modified Weil osteotomy (MWO) or a modified Weil osteotomy with interphalangeal fixation (MWOIF).
Methods:
We performed a retrospective review with a prospective follow-up of 50 patients (98% women, 120 rays) who underwent MWO (65 rays) or MWOIF (55 rays), with a mean age of 54 ± 12 years and a minimum follow-up of 4 years (mean of 6 years). We analyzed the presence of floating toe deformity in MWO and MWOIF and the outcomes measured by the subjective satisfaction, Lower Extremity Functional Scale (LEFS), American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot score, and quality of prehension force between patients with or without floating toe deformity.
Results:
The mean floating toe incidence was of 57%, with no significant difference between operative techniques (48% MWO, 67% MWOIF; P = .053). Our analysis did not show differences in satisfaction, LEFS and AOFAS scores, or grip strength between the group of patients with or without floating toes.
Conclusion:
The presence of a floating toe deformity was more frequent than generally believed but did not have a meaningful impact on the patient’s satisfaction or functional outcomes measured by the AOFAS and LEFS scales. There was no clear correlation between operative technique, floating toe, and quality of prehension force.
Level of Evidence:
Level III, retrospective comparative series.
Keywords: floating toe, satisfaction, modified Weil osteotomy, interphalangeal fixation
Introduction
Metatarsalgia with or without lesser toe deformities remains one of the most challenging problems in foot and ankle pathology. In cases of metatarsalgia with unstable joints, Weil osteotomy can achieve an excellent outcome, 12 but complications such as floating toe, transfer metatarsalgia, or problems during the stages of bone healing (delayed union, non-union, and malunion) frequently occur, with overall incidences ranging from 15% to 68%. 9,12,16,22 Floating toe is the most frequently described complication, with studies addressing possible explanations for its occurrence, but no study has examined the impact on the patient overall function and satisfaction, with only expert opinions stating that floating toe would have limited effect. 17,18
Because of this lack of evidence, this study’s objective was to analyze if the presence of floating toe influenced patient’s satisfaction and functional outcomes. We hypothesized that floating toe deformity would have no impact on the patient self-reported satisfaction, Lower Extremity Functional Scale (LEFS) or American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot score at a minimum follow-up of 4 years after the operation.
Methods
After approval from the ethical and institutional review board, patients who underwent modified Weil osteotomy (MWO) or modified Weil osteotomy with DuVries arthroplasty and interphalangeal fixation (MWOIF) between January 2010 and November 2013 at a single private local hospital were selected for a prospective analysis based on the following criteria: patients aged ≥18 years and available for a physical evaluation. We excluded patients with incomplete data (n = 5) and those who did not agree to give informed consent (n = 0). Patients were identified using the institution’s operative techniques codes from the hospital-wide database. We included 50 patients in the analysis (98% women). The main indication for MWO was metatarsalgia and for MWOIF, they were metatarsalgia and a rigid hammertoe that had failed conservative treatment for 6 months. Table 1 shows the epidemiologic information.
Table 1.
Participant Characteristics at Baseline, by Group.a
| Characteristics | FT– (n = 16) |
FT+ (n = 34) |
|---|---|---|
| Age, y | 54.2 (11.7) | 53.7 (12.9) |
| Women | 16 (100) | 33 (97.1) |
| BMI | 24.4 (3.6) | 24.8 (3.1) |
| Hallux valgas | 16 (100) | 31 (91.2) |
Abbreviations: BMI, body mass index; FT–, no floating toe; FT+, at least incomplete floating toe.
a Data are shown as n (%) or mean (SD). Number of surgeries are calculated per patient. The presence of hallux valgus is controlled by foot. Mann-Whitney U test or t test used for all between-group comparisons, all 2 tailed probabilities are P >.05.
An author who was not aware of the procedure contacted the patients to perform a clinical evaluation and obtain the outcomes assessments tools (Modified Kenneth scale, AOFAS, and LEFS). During the physical evaluation, the physician recorded the patient’s characteristics such as age, sex, body mass index, the presence of hallux valgus, the operative procedure indication, the presence of floating toe, and the grip strength of the involved toe.
For this study, we defined a floating toe as a toe that was not in complete contact with the floor under weightbearing conditions, 8 and classified it into 3 categories: Complete Floating Toe (CFT), Incomplete Floating Toe (PFT), or No Floating Toe (NFT) (Table 2). Our primary outcomes were the incidence of floating toe deformity and the difference in self-reported patient subjective satisfaction, LEFS, and AOFAS scores between the different operative procedures (MWO or MWOIF) depending on the presence or absence of floating toe. The minimum follow-up period was 4 years. The measurement of patient satisfaction was through the Kenneth scale modified by Stamatis et al. 20 This is a subjective system that classifies patients as completely satisfied, satisfied with minor reservations, satisfied with major reservations, or dissatisfied (Table 2). The AOFAS score range from 0 to 100 and is calculated for each foot, while the LEFS system range is per patient with a score ranging from 0 to 80. In both systems, lower scores indicate more disability related to the intervention. 2,4,6,13,14,19 The minimal clinically important difference for LEFS and AOFAS was determined from previous studies and prespecified as 9 and 8.4 points, respectively. 2,5
Table 2.
Description of Floating Toe, Satisfaction, and Grip Strength Classifications.a
| Description | |
|---|---|
| Floating toe | |
| Complete | A toe with no contact with the floor |
| Incomplete | A toe with partial contact with the floor |
| No | A toe with full contact with the floor |
| Satisfaction | |
| Completely satisfied | No restrictions of activity, footwear, or pain |
| Satisfied, with minor reservations | Mild restriction of activity, footwear, or pain |
| Satisfied, with major reservations | Moderate restriction of activity, footwear, or pain |
| Dissatisfied | Severe restriction of activity, footwear, or pain |
| Toe grip strength | |
| Full strength | Can hold paper on floor with involved toe |
| Mild strength | Can touch paper with toe, but not hold |
| No strength | Cannot touch paper with toe |
The secondary outcomes compared the toe grip strength and the incidence of floating toe to the operative technique. Assessment of the toe grip strength was with the “paper pullout test” as described by Bouche and Heit. 3 We classified toe grip strength as full strength, mild strength, or no strength (Table 2).
Regarding the operative techniques, after fluoroscopic confirmation, we performed the MWOIF through the implantation of a resorbable pin (Trim-It drill Pin; Arthrex, Naples, FL) and fixed the Weil osteotomy with a noncannulated 2.0-mm cortical screw (DePuy Synthes, Johnson & Johnson, Malvern, PA). 15,21 All the surgeons routinely performed both operations tested in the study; each of the participating surgeons form part of the foot and ankle staff with at least 10 years of experience.
Statistical Analysis
Independent sample t test was conducted to compare intergroup baseline characteristics for continuous variables, shown as means and standard deviations (SD); for categorical variables, the Fisher exact test or chi-square test was used, presented as numbers and percentages. For the analysis of the primary outcome, we dichotomized floating toe as existing (FT+) or absent (FT–) among all the patients who had a follow-up assessment. To determine the impact of floating toe on personal satisfaction, AOFAS, and LEFS score, we used the Mann-Whitney U test and the independent sample t test, respectively. To compare the difference in grip strength and floating toe degree depending on the operative technique, we used the Mann-Whitney U test. Presentation of values is as mean ± standard deviation for parametric tests and medians for nonparametric tests. P <.05 was considered statistically significant. Performance of all analyses was with IBM SPSS Statistics for Macintosh, version 25.0 (IBM Corp, Armonk, NY).
Results
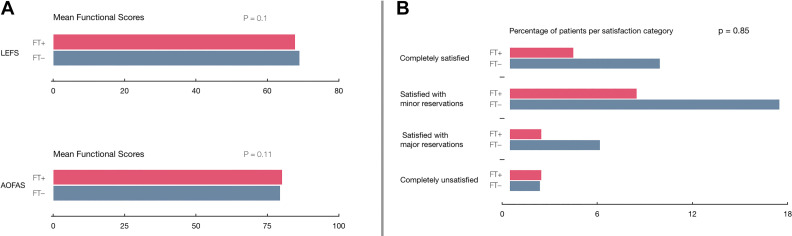
A total of 120 operated rays represented by 50 patients (98% women) with a mean age of 54 years fulfilled the inclusion criteria for this study. Their floating toe incidence was 57% (68/120 rays) (34/50 patients). Table 1 shows the baseline characteristics of patients with and without a floating toe. No difference was found in terms of LEFS, AOFAS, and patient satisfaction if floating toe was present or absent (Figure 1). Confidence interval for LEFS was 0.892 to 1.062 and for AOFAS, it was 0.926-1.125. As both confidence intervals cross 1, no difference between scores was found, depending on floating toe results.
Figure 1.
Outcomes of patients according to the presence of floating toe. There was no statistical difference between the presence or absence of floating toe in terms of AOFAS, LEFS, and subjective satisfaction. Abbreviations: FT–, no floating toe; FT+, present floating toe; LEFS, Lower Extremity Functional Scale; AOFAS, American Orthopaedic Foot & Ankle Society ankle-hindfoot score. (A) In these rating scales, lower values represent more disability. (B) The patient’s satisfaction was measured using the Kenneth scale, modified by Stamatis et al. 19
The toe grip strength between operative techniques (MWO and MWOIF) alone was not significantly different when analyzed independently (P = .86), or when controlling for floating toe (P = .63) (Table 3). Forty-eight percent of the patients who underwent an MWO and 67% of those who underwent an MWOIF had some degree of floating toe (P = .053).
Table 3.
Outcomes of the Rays According to the Operative Procedure.a
| Operative Procedure | MWO (n = 65) |
MWOIF (n = 55) |
|---|---|---|
| Floating toe | ||
| Complete | 18 (27.7) | 21 (38.2) |
| Incomplete | 13 (20) | 16 (29.1) |
| No | 34 (52.3) | 18 (32.7) |
| Toe grip strength | ||
| Full strength | 22 (34.3) | 22 (40.4) |
| Mild strength | 36 (55.2) | 21 (38.6) |
| No strength | 7 (10.4) | 12 (21.1) |
Abbreviations: MWO, modified Weil osteotomy; MWOIF, modified Weil osteotomy with interphalangeal fixation.
a Data are shown as n (%). Mann-Whitney U test used for all between-group comparisons, all 2-tailed probabilities are P >.05. Toe grip strength was defined by the “paper pullout test.”
Discussion
The Weil osteotomy was originally indicated exclusively for long metatarsals with an abnormal parabola, 23 but the procedure and indications have evolved. Now it is a preferred procedure for metatarsalgia and digital deformities associated with metatarsophalangeal subluxation or dislocation. 1,7,18 Consequently, the complications found have also evolved, which include floating toes, transfer metatarsalgia and recurrence of deformities being the most common. Despite the relatively high frequency of these complications, they seem not to influence patient satisfaction. However, no study has specifically evaluated this aspect.
Results from this prospective study of a retrospective database of 50 patients with a minimum follow-up of 56 months found that the frequency of floating toe deformity (57%) after an MWO was higher than generally believed. Previous theoretical studies have suggested that modifying the Weil osteotomy by removing a slice of bone would avoid or at least decrease the floating toe incidence because metatarsal head depression would be avoided (no change in center of rotation would happen if a bone slice was removed). 9,18 Our study, nevertheless, showed that removing a slice of bone did not avoid floating toe occurence. 10 This research has a relatively long follow-up, longer than the average of those in the literature (71 vs 25.8 months). 11 Hofstaetter et al has the only study with a similar follow-up time (84 months) and a higher floating toe incidence (68%). 12
Regarding patients’ functional outcomes, there was no significant difference found if floating toe was present or absent. Regarding patient satisfaction, in comparison with the literature, 12,16,21 our study showed a higher percentage of patients satisfied with minor reservations (50%) and around half as completely satisfied (27%). The presence of different pathologies in our patients such as hallux valgus, Morton neuroma, and exostosis may explain the high percentage of minor reservations, as personal satisfaction is inextricable from global function.
In conclusion, floating toe deformity was more frequent than generally believed. We found that the presence of a floating toe deformity did not have a meaningful impact on patient satisfaction or functional outcomes with the scores used in this study.
Supplemental Material
Supplemental Material, FAO891956-ICMJE for Incidence of and Functional Significance of Floating Toe After Weil Osteotomy by Emilio Wagner, Luis A. O’Connell, Ruben Radkievich, Nathaly Caicedo, Pablo Mococain and Pablo Wagner in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Luis A. O’Connell, MD,  https://orcid.org/0000-0001-6827-2342
https://orcid.org/0000-0001-6827-2342
Ruben Radkievich, MD,  https://orcid.org/0000-0002-7024-4786
https://orcid.org/0000-0002-7024-4786
Pablo Wagner, MD,  https://orcid.org/0000-0003-4896-4434
https://orcid.org/0000-0003-4896-4434
References
- 1. Bevernage BD, Deleu PA, Leemrijse T. The translating Weil osteotomy in the treatment of an overriding second toe: a report of 25 cases. Foot Ankle Surg. 2010;16(4):153–158. [DOI] [PubMed] [Google Scholar]
- 2. Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–383. [PubMed] [Google Scholar]
- 3. Bouche RT, Heit EJ. Combined plantar plate and hammertoe repair with flexor digitorum longus tendon transfer for chronic, severe sagittal plane instability of the lesser metatarsophalangeal joints: preliminary observations. J Foot Ankle Surg. 2008;47(2):125–137. [DOI] [PubMed] [Google Scholar]
- 4. Ceccarelli F, Calderazzi F, Pedrazzi G. Is there a relation between AOFAS ankle-hindfoot score and SF-36 in evaluation of Achilles ruptures treated by percutaneous technique? J Foot Ankle Surg. 2014;53(1):16–21. [DOI] [PubMed] [Google Scholar]
- 5. Chan HY, Chen JY, Zainul-Abidin S, Ying H, Koo K, Rikhraj IS. Minimal clinically important differences for American Orthopaedic Foot & Ankle Society Score in Hallux Valgus Surgery. Foot Ankle Int. 2017;38(5):551–557. [DOI] [PubMed] [Google Scholar]
- 6. Dingemans SA, Kleipool SC, Mulders MAM, et al. Normative data for the Lower Extremity Functional Scale (LEFS). Acta Orthop. 2017;88(4):422–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Downey MS, McGlamry MC, Spizzirri SA. Transverse plane digital deformities. Compr Textb Foot Ankle Surg. 2001:354–371. [Google Scholar]
- 8. Fukuyama K, Maruyama H. Occurrence of floating toe from the viewpoint of the structure of foot arch. J Phys Ther Sci. 2011;23(1):33–36. doi:10.1589/jpts.23.33. [Google Scholar]
- 9. Garg R, Thordarson DB, Schrumpf M, Castaneda D. Sliding oblique versus segmental resection osteotomies for lesser metatarsophalangeal joint pathology. Foot Ankle Int. 2008;29(10):1009–1014. [DOI] [PubMed] [Google Scholar]
- 10. Grimes J, Coughlin M. Geometric analysis of the Weil osteotomy. Foot Ankle Int. 2006;27(11):985–992. [DOI] [PubMed] [Google Scholar]
- 11. Highlander P, VonHerbulis E, Gonzalez A, Britt J, Buchman J. Complications of the Weil osteotomy. Foot Ankle Spec. 2011;4(3):165–170. [DOI] [PubMed] [Google Scholar]
- 12. Hofstaetter SG, Hofstaetter JG, Petroutsas JA, Gruber F, Ritschl P, Trnka HJ. The Weil osteotomy: a seven-year follow-up. J Bone Joint Surg Br. 2005;87(11):1507–1511. [DOI] [PubMed] [Google Scholar]
- 13. Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007;46(2):65–74. [DOI] [PubMed] [Google Scholar]
- 14. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. [DOI] [PubMed] [Google Scholar]
- 15. Maceira E, Monteagudo M. Transfer metatarsalgia post hallux valgus surgery. Foot Ankle Clin. 2014;19(2):285–307. [DOI] [PubMed] [Google Scholar]
- 16. Migues A, Slullitel G, Bilbao F, Carrasco M, Solari G. Floating-toe deformity as a complication of the Weil osteotomy. Foot Ankle Int. 2004;25(9):609–613. [DOI] [PubMed] [Google Scholar]
- 17. Phisitkul P. Managing complications of lesser toe and metatarsophalangeal joint surgery. Foot Ankle Clin. 2018;23(1):145–156. [DOI] [PubMed] [Google Scholar]
- 18. Reddy VB. Metatarsal osteotomies: complications. Foot Ankle Clin. 2018;23(1):47–55. [DOI] [PubMed] [Google Scholar]
- 19. SooHoo NF, Vyas R, Samimi D. Responsiveness of the foot function index, AOFAS clinical rating systems, and SF-36 after foot and ankle surgery. Foot Ankle Int. 2006;27(11):930–934. [DOI] [PubMed] [Google Scholar]
- 20. Stamatis ED, Myerson MS. Treatment of recurrence of symptoms after excision of an interdigital neuroma. A retrospective review. J Bone Joint Surg Br. 2004;86(1):48–53. [PubMed] [Google Scholar]
- 21. Trnka HJ, Gebhard C, Muhlbauer M, Ivanic G, Ritschl P. The Weil osteotomy for treatment of dislocated lesser metatarsophalangeal joints: good outcome in 21 patients with 42 osteotomies. Acta Orthop Scand. 2002;73(2):190–194. [DOI] [PubMed] [Google Scholar]
- 22. Vandeputte G, Dereymaeker G, Steenwerckx A, Peeraer L. The Weil osteotomy of the lesser metatarsals: a clinical and pedobarographic follow-up study. Foot Ankle Int. 2000;21(5):370–374. [DOI] [PubMed] [Google Scholar]
- 23. Zirm RJ. The Weil lesser metatarsal osteotomy. In: McGlamry’s Comprehensive Textbook of Foot and Ankle Surgery. 4th ed. Philadelphia, PA: Wolters Kluwer Health; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO891956-ICMJE for Incidence of and Functional Significance of Floating Toe After Weil Osteotomy by Emilio Wagner, Luis A. O’Connell, Ruben Radkievich, Nathaly Caicedo, Pablo Mococain and Pablo Wagner in Foot & Ankle Orthopaedics