Abstract
Background:
Knee scooters (“scooters”) are a commonly used device to facilitate postoperative adherence to weightbearing restrictions. Although high rates of falls have been reported, little is known about injuries related to scooter use.
Methods:
We analyzed survey responses from 316 of 2046 members (15%) of the American Orthopaedic Foot & Ankle Society in May-June 2019 describing (1) frequency of scooter recommendation; (2) indications for which they recommended scooters; (3) characteristics of patients for whom they recommended scooters; (4) prevalence, anatomic locations, mechanisms, and sequelae of scooter-related injuries; and (5) characteristics of patients with scooter-related injuries. Descriptive statistics and χ2 goodness-of-fit tests were performed (alpha = .05).
Results:
Mean frequency with which respondents recommended scooters in particular was 69%. Respondents most often recommended scooters after hindfoot arthrodesis (97% [305/316]), ankle arthrodesis (96% [302/316]), and for total nonweightbearing (64% [202/316]) and to patients who were overweight (vs obese) or aged 45-75 years. Mean prevalence of scooter-related injuries was 2.5%. The most common injury mechanism was making a sharp turn (reported by 62% [103/166]). Thirty-four percent (56/166) of respondents with injured patients said patients underwent surgery to treat scooter-related injuries. Patients with scooter-related injuries were more often women, >44 years old, obese, and sedentary.
Conclusion:
Scooters were commonly recommended postoperatively, most often for total nonweightbearing after hindfoot or ankle arthrodesis, and most often in overweight adults or those aged 45-75 years. Mean reported prevalence of scooter-related injuries was 2.5%. Female sex, older age, obesity, and sedentary lifestyle were associated with scooter-related injury.
Level of Evidence:
Level IV, retrospective case series.
Keywords: knee scooter, nonweightbearing, orthopedic scooter, partial weightbearing, scooter-related injury, survey
Introduction
Various assistive devices are used to facilitate weightbearing restriction after lower extremity injury or surgery, including axillary and elbow crutches, walking frames, rolling walkers, wheelchairs, and knee scooters (“scooters”). 7,8 Scooters, also described as “orthopedic scooters,” “knee coasters,” or “knee walkers,” consist of a steering handle and a raised, wheeled platform that supports the affected lower extremity at the flexed knee while the user propels the device with the unaffected leg. 6 In healthy volunteers, the use of a scooter on a flat surface requires less energy expenditure, 5,7 results in lower perceived exertion, 4,7 and yields faster self-selected walking velocity 4 compared with the use of crutches. Although high rates of patient satisfaction 9 and preference 4 have been reported for scooters, little is known regarding their safety. Yeoh et al 9 reported that more than 40% of patients (32/73) patients who responded to a survey about postoperative scooter use after foot and ankle surgery experienced falls while using the scooter. We are unaware of any other studies reporting the prevalence, locations, mechanisms, or sequelae of these injuries.
Because of the lack of information about injuries incurred during postoperative knee scooter use, as well as the high rate of falls reported in a previous study, we aimed to characterize postoperative knee scooter–associated injuries. Specifically, we surveyed foot and ankle surgeons regarding the (1) frequency with which they recommended scooters; (2) indications for which they recommended scooters; (3) characteristics of patients for whom they recommended scooters; (4) prevalence, anatomic locations, mechanisms, and sequelae of scooter-related injuries; and (5) characteristics of patients with scooter-related injuries. Our goal is that our findings will help surgeons make evidence-based recommendations for postoperative knee scooter use when counseling patients.
Methods
We developed a 19-item survey (Appendix A) in a secure, web-based platform (REDCap version 9.1.20, Vanderbilt University Medical Center, Nashville, TN) and emailed it to surgeon members of the American Orthopaedic Foot & Ankle Society (AOFAS). Responses were collected between May 2 and June 2, 2019. An e-mail reminder was sent on May 27, 2019. We included all respondents who had an active lower extremity surgery practice and were able to complete an English-language, web-based survey. Because various terms are used to describe scooters, we included with the survey an illustration of a scooter to clarify the intended subject (Figure 1).
Figure 1.

Illustration of a knee scooter shown to survey respondents to clarify the intended subject of study because various terms are used to describe knee scooters. Courtesy Michelle Seu.
Respondent and Practice Characteristics
Respondents were asked about themselves and their practices: their gender, their type of fellowship training, their practice location, their number of years in practice, and whether they currently perform lower extremity surgeries. Respondents who indicated that they currently perform lower extremity surgeries were asked how many they perform in a typical month.
Scooter Recommendations
The next questions related to respondents’ recommendations for the use of scooters: the number of patients per month for whom they recommend any device to support weightbearing restrictions (eg, crutches, rolling walkers, scooters); the number of patients per month for whom they recommend scooters specifically; the types of operative procedures after which they are likely to recommend a scooter; the type of weightbearing restrictions for which they more commonly recommend scooters (ie, partial weightbearing, nonweightbearing, both, or neither); the patient characteristics that influence them to recommend a scooter; and the patient characteristics that dissuade them from recommending a scooter. Multiple responses were allowed for the questions about operative procedure types and patient characteristics.
Scooter-Related Injuries
Respondents were then asked whether any of their patients had experienced scooter-related injuries. Respondents who answered affirmatively were asked about the patients and their injuries, including: the percentage of patients for whom they recommended scooters who subsequently experienced scooter-related injuries; the characteristics the respondents identified as common among patients who experienced such injuries; the types and locations of scooter-related injuries seen by respondents; whether patients underwent operative treatment of their scooter-related injuries; which sequelae of scooter-related injuries they have treated; and which mechanisms caused the scooter-related injuries in their patients. Multiple responses were allowed for questions about patient characteristics, injury types and locations, injury mechanisms, and injury sequelae.
Survey Respondents
Survey responses were received from 333 AOFAS members. Seventeen responses were excluded: 10 were incomplete, and 7 were from members without an active lower extremity surgery practice. Of the 316 included respondents, 272 (86%) were men, 260 (82%) were practicing in North America, and 269 (94%) had completed foot and ankle fellowship training, including 27 (8.5%) who had also completed trauma fellowship training. Respondents reported having a mean (±SD) of 14 ± 10 years in practice and performing a mean of 29 ± 15 lower extremity surgeries in a typical month (Table 1).
Table 1.
Characteristics of 316 Members of the American Orthopaedic Foot & Ankle Society Who Responded to a Survey About Knee Scooters.
| Characteristics | No. (%) of Respondents |
|---|---|
| Gender | |
| Male | 272 (86) |
| Female | 44 (14) |
| Years in practice | 14 ± 10 a |
| Location of practice | |
| North America | 260 (82) |
| South America | 16 (5.1) |
| Other | 16 (5.1) |
| Europe | 13 (4.1) |
| Asia | 10 (3.2) |
| Africa | 1 (0.32) |
| Type of fellowship training | |
| Foot and ankle | 269 (85) |
| Trauma and foot and ankle | 27 (8.5) |
| None | 11 (3.5) |
| Other | 6 (1.9) |
| Orthopedic trauma | 3 (0.95) |
| Lower extremity surgeries performed monthly | 29 ± 15 a |
a Presented as mean ± SD.
Statistical Analysis
An a priori sample size calculation based on the target population of 2046 AOFAS members, a 95% confidence level, and a 5% margin of error indicated that 324 survey responses were needed.
For survey items to which multiple responses were allowed, the percentages of respondents who selected each response are reported. The mean reported prevalence of scooter-related injuries was calculated by assigning a “zero” response for respondents who reported recommending scooters but not having patients with scooter-related injuries. Responses to the following survey items were analyzed using the χ2 goodness-of-fit test: scooter-related injury locations, mechanisms, and sequelae; type of operative procedure, weightbearing status, and patient characteristics for which respondents would be more or less likely to recommend scooter use; and characteristics identified by respondents as common among patients injured. For these analyses, responses of “other” or “none of the above” were excluded, and degrees of freedom were equal to 1 less than the number of the remaining response options. The null hypothesis was equal distribution of responses among the remaining answer choices. We used α = .05.
We used Bonferroni adjustment for multiple comparisons 2 for questions about the following: (1) patient characteristics that would influence respondents to recommend scooters; (2) patient characteristics that would dissuade respondents from recommending scooters; and (3) patient characteristics identified by respondents as common among those who were injured. A maximum experiment-wise error rate (MEER) α = .05 was used for each question. The 4 patient characteristics tested (gender, age group, body mass index [BMI] category, and active/sedentary lifestyle) were treated as independent hypotheses. Each test result was considered statistically significant if P values <MEER α / 4, or .0125. Data were stored on REDCap and analyzed using Stata, version 15.1 (StataCorp LLC, College Station, TX) and Microsoft Excel, version 15 (Microsoft Corporation, Redmond, WA).
Results
Frequency of Scooter Recommendations
In a typical month, respondents reported recommending any lower extremity partial or nonweightbearing device (eg, crutches, scooters, other devices) to a mean (±SD) 21 ± 12 patients and recommending scooters specifically to a mean 15 ± 11 patients. The mean percentage of patients for whom scooters were recommended (of the total number of patients for whom assistive devices were recommended in a typical month by each respondent) was 69% (SD, 33%).
Indications for Scooters
The largest proportions of respondents said they commonly recommend scooters after hindfoot arthrodesis (97%), ankle arthrodesis (96%), and lower extremity fracture fixation (92%) (Table 2). Of the 6 indications about which respondents were asked, the smallest proportion of respondents (76%) said they commonly recommend scooters after Achilles tendon repair (P = .04).
Table 2.
Factors Describing Knee Scooter Recommendations of 316 Members of the American Orthopaedic Foot & Ankle Society.
| Factors | No. (%) of Respondents | P |
|---|---|---|
| No. of total/partial nonweightbearing devices recommended per month | ||
| All devices | 21 ± 12a | |
| Knee scooters | 15 ± 11a | |
| Procedures after which respondent commonly recommends scooterb | ||
| Hindfoot arthrodesis | 305 (97) | .04c |
| Ankle arthrodesis | 302 (96) | |
| Lower extremity fracture fixation | 292 (92) | |
| Forefoot/midfoot arthrodesis | 267 (85) | |
| Lower extremity osteotomy | 264 (84) | |
| Achilles tendon repair | 241 (76) | |
| Other | 38 (12) | |
| Would not recommend after any surgery | 6 (1.9) | |
| Weightbearing restrictions for which respondent commonly recommends scooter | ||
| Total nonweightbearing | 202 (64) | <.001 |
| Both total and partial nonweightbearing | 99 (31) | |
| Neither total nor partial nonweightbearing | 13 (4.1) | |
| Partial nonweightbearing | 2 (0.63) |
a Presented as mean ± SD.
b Respondents were able to select >1 answer for this question.
c Based on χ2 goodness-of-fit test, with null hypothesis expecting equal distribution of observations among answer choices, excluding “Other” and “Would not recommend after any surgery.”
Patient Characteristics and Scooters Recommendations
The largest proportion of respondents (64%) said they more commonly recommend scooters for patients with total nonweightbearing restrictions (Table 2). Only 2 respondents (<1%) said they more commonly recommend scooters for patients with partial nonweightbearing restrictions. Approximately one-third of respondents (31%) said they commonly recommended scooters for both total and partial nonweightbearing restrictions.
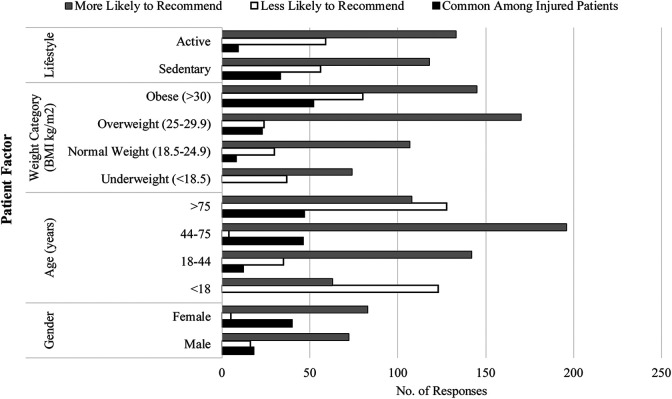
We found no significant differences in how likely respondents were to recommend scooters to male vs female patients and to patients with active vs sedentary lifestyles (Figure 2). More respondents said they were more likely to recommend scooters to patients aged 44-75 years (196 respondents, 62%) compared with patients who were older than 75 years (128 respondents, 41%) or younger than 18 years (123 respondents, 39%) (P < .001). More respondents also reported that they were more likely to recommend scooters to overweight patients (170 respondents, 54%) than to obese patients (80 respondents, 25%) (P < .001).
Figure 2.
Patient characteristics that 316 foot and ankle surgeons report would make them more or less likely to recommend postoperative knee scooter use, and common characteristics in patients with knee scooter–related injuries.
Scooter-Related Injuries
Prevalence
One hundred sixty-six respondents (53%) reported that at least 1 of their patients had sustained a scooter-related injury (Table 3). On average, those respondents reported that 4.5% of their scooter-using patients sustained scooter-related injuries. When including the 130 respondents who reported recommending scooters and having no patients with scooter-related injuries, we calculated a mean reported prevalence of scooter-related injury of 2.5%.
Table 3.
Patient Characteristics by Likelihood of 316 Foot and Ankle Surgeons to Recommend Postoperative Knee Scooter Use and by Scooter-Related Injury.
| Patient Characteristicsa | How Respondents Said the Characteristic Influences Their Likelihood of Recommending Scooter | Respondents Reporting Injured Patients With These Characteristics (n = 166) | ||||
|---|---|---|---|---|---|---|
| More Likely, n (%)b | P Value | Less Likely, n (%)c | P Value | n (%) | P Valued | |
| Gender | .38 | .02 | <.01 | |||
| Female | 83 (26) | 5 (1.6) | 40 (24) | |||
| Male | 72 (23) | 16 (5.1) | 18 (11) | |||
| Age group, y | <.001 | <.001 | <.001 | |||
| <18 | 63 (20) | 123 (39) | 0 (0.0) | |||
| 18-44 | 142 (45) | 35 (11) | 12 (7.2) | |||
| 44-75 | 196 (62) | 4 (1.3) | 46 (28) | |||
| >75 | 108 (34) | 128 (41) | 47 (28) | |||
| BMI category | <.001 | <.001 | <.001 | |||
| <18.5 (underweight) | 74 (23) | 37 (12) | 0 (0.0) | |||
| 18.5-24.9 (normal weight) | 107 (34) | 30 (9.5) | 8 (4.8) | |||
| 25-29.9 (overweight) | 170 (54) | 24 (7.6) | 23 (14) | |||
| >30 (obese) | 145 (46) | 80 (25) | 52 (31) | |||
| Lifestyle | .34 | .78 | <.001 | |||
| Active | 133 (42) | 59 (19) | 9 (5.4) | |||
| Sedentary | 118 (37) | 56 (18) | 33 (20) | |||
| None of the above | 40 (24) | |||||
Abbreviation: BMI, body mass index.
a Respondents were able to select >1 patient characteristic within each category.
b When considering all patient characteristics listed, 43 respondents (14%) said that none of the characteristics would make them more likely to recommend scooter use.
c When considering all patient characteristics listed, 66 respondents (21%) said that none of the characteristics would make them less likely to recommend scooter use.
d From χ2 goodness-of-fit test, with null hypothesis expecting equal distribution of observations among patient characteristics within each category. Degrees of freedom = number of patient characteristics within the category − 1. Applying Bonferroni adjustment, maximum experiment-wise error rate (MEER) α = .05 was used for each question with 4 hypotheses tested per question. Each test was considered statistically significant if P < MEER α / by 4, or .0125
Anatomic Locations of Injury
Scooter-related injuries were reported more frequently in the lower extremity (30% of 329 responses) than in the upper extremity (60% of 329 responses) (P < .001). Among both upper and lower extremity injuries, those ipsilateral to the operative site (54%) were reported more commonly than those contralateral (37%) (P <.01). Although lower extremity injuries were more common overall, the most commonly reported specific injury location was the ipsilateral upper extremity (reported by 34% [56/166] of respondents, P < .001) (Table 4, Figure 3).
Table 4.
Prevalence, Patterns, and Sequelae of Knee Scooter–Related Injuries as Reported by 166 Survey Respondents (Foot and Ankle Surgeons) With Patients Who Experienced Such Injuries.
| Variable | No. (%) of Respondents | P Valuea |
|---|---|---|
| Respondent’s patients who experienced knee scooter–related injury, % | 4.5 ± 4.9b | |
| Injury types experience by respondent’s patientsc | <.001 | |
| Ipsilateral upper extremity trauma | 56 (34) | |
| Contralateral upper extremity trauma | 44 (27) | |
| Ipsilateral ankle trauma | 34 (21) | |
| Ipsilateral other lower extremity trauma | 34 (21) | |
| Ipsilateral knee trauma | 32 (19) | |
| Contralateral ankle trauma | 27 (16) | |
| Contralateral knee trauma | 27 (16) | |
| Contralateral other lower extremity trauma | 23 (14) | |
| Operative wound complication | 21 (13) | |
| Other | 31 (19) | |
| Mechanism of injury of respondent’s patientsc | <.001 | |
| Making a sharp turn | 103 (62) | |
| Loss of balance while stationary on scooter | 76 (46) | |
| Hitting an obstacle | 68 (41) | |
| Moving too fast | 58 (35) | |
| Moving downhill | 20 (12) | |
| Other | 10 (6.0) | |
| Unsure | 10 (6.0) | |
| Operative treatment required for at least one of respondent’s injured patients | <.01 | |
| Yes | 57 (34) | |
| No | 104 (63) | |
| Unsure | 5 (3.0) | |
| Sequelae of respondent’s patients’ scooter-related injuriesc | <.001 | |
| Additional mobility deficit (treated nonoperatively) | 84 (51) | |
| Other | 47 (28) | |
| New injury (treated operatively) | 33 (20) | |
| Operative revision of index procedure | 23 (14) |
a From χ2 goodness-of-fit test, with null hypothesis expecting equal distribution of observations among answer choices, excluding “Other” and/or “Unsure.”
b Expressed as mean ± SD.
c Respondents were able to select >1 answer choice.
Figure 3.

Anatomic locations of patients’ postoperative knee scooter–related injuries reported by 166 surgeon members of the American Orthopaedic Foot & Ankle Society. Numbers indicate the number of surgeons who reported the anatomic location as an injury site in at least 1 of their patients.
Mechanisms of Injury
The most commonly reported mechanism of injury was making a sharp turn on the scooter (reported by 103 respondents [62%]), followed by loss of balance while stationary on scooter (reported by 76 respondents [46%]) (P < .001; Table 4).
Injury Sequelae
The most commonly reported scooter-related injury sequela was an additional mobility deficit treated nonoperatively (reported by 81 respondents [51%] (P < .001; Table 4). Operative treatment of a scooter-related injury was reported by 57 (34%) of the 166 respondents who reported having patients with such injuries.
Characteristics of Injured Patients
Of the 166 respondents who reported having patients with scooter-related injuries, more said that their injured patients were female (40 respondents; 24%) than male (18 respondents; 11%) (P < .01). More respondents reported that their patients with scooter-related injuries were aged 44-75 (46 respondents, 28%) or >75 years (47 respondents, 28%) than aged 18-44 (12 respondents, 7.2%) or <18 years (0 respondents) (P < .001). By BMI category, more respondents reported that their patients with scooter-related injuries were obese (52 respondents, 31%) or overweight (23 respondents, 14%) than normal weight (8 respondents, 4.8%) (P < .001). Finally, 33 respondents (20%) said that their patients with scooter-related injuries had a sedentary lifestyle, and 9 (5.4%) said their injured patients had an active lifestyle (P < .001).
Discussion
In this survey of 316 lower extremity surgeon members of the AOFAS, we estimated the prevalence of postoperative knee scooter–related injuries to be 2.5%. Although we assessed injuries overall and not falls specifically, our number is much lower than the >40% rate of falls reported by Yeoh et al. 9 It is possible that minor injuries were not reported to surgeons, suggesting that during postoperative follow-up, surgeons should ask patients directly if they are experiencing falls or minor injuries while using scooters. Injuries were most commonly reported to occur in the lower extremity. Among respondents who reported patients with scooter-related injuries, 34% (57/166) said the injuries were treated operatively. As far as we know, such findings have not been previously reported. Injuries were reported to occur most commonly when patients were making sharp turns on the scooter or when they lost balance while stationary on the scooter. It may be prudent to warn patients of the risk of injury via these mechanisms. This is an important finding in understanding scooter-related injuries because researchers who have assessed individual exertion on scooters have studied only forward motion and did not include turning. 1,4
We identified female gender, age >44 years, obesity, and sedentary activity level as potential risk factors for scooter-related injuries. When comparing the characteristics of patients for whom respondents said they commonly recommended scooters with the characteristics of patients who sustained scooter-related injuries, we found important differences. Although scooter-related injuries were reported to occur more than twice as often in female patients than in male patients, respondents did not identify patient gender as affecting their likelihood of recommending scooter use. Lower peak bone mineral density and the marked decline of bone mineral density after menopause in female patients may place them at higher risk of fracture after a scooter-related fall than men. 3 Similarly, most respondents indicated that they commonly recommend scooters to patients aged 44–75 years; however, injuries were reported most commonly in both this age group and in patients older than 75. Again, this may be attributable to the decline in bone mineral density starting as early as age 25 years in both men and women. 3 Many respondents commonly recommended scooters for patients who are obese, and obesity was identified as a common characteristic among injured patients. Obese individuals might be injured more commonly because they are more likely to have scooters recommended. Alternatively, higher BMI may predispose them to injury, perhaps because of greater weightbearing support required from the scooters or different weight distributions on the scooter itself. These explanations would warrant reevaluation of recommendation practices, and the latter would warrant innovation in scooter design.
These findings contradict those of Yeoh et al, 9 who found no significant associations between gender, age, or BMI and scooter-related injuries, suggesting that more rigorous research is necessary to explore these questions directly. Finally, although respondents indicated that a patient’s lifestyle (sedentary vs active) does not influence their likelihood of recommending scooters, sedentary lifestyle was a more commonly reported characteristic among injured patients. Physical activity improves bone mineral density, 3 and those with higher activity levels at baseline may be less susceptible to fractures from scooter-related falls. It is also possible that those with a more active lifestyle at baseline have better physical agility, allowing them to avoid situations on scooters that could result in injury. We are unaware of other studies that have evaluated the relationship between patient activity level and scooter-related injuries.
No respondents identified age <18 years as a common characteristic among their patients with scooter-related injuries. It is unknown whether this finding is related to a lower frequency of scooter recommendation or a lower rate of scooter-related injury relative to older patients. We did not ask why surgeons are less likely to recommend scooters to this age group. We believe it may have been because of concerns about risk of injury or because younger patients tolerate axillary crutches better than older patients.
Respondents recommended scooters for patients 69% of the time when recommending devices to facilitate weightbearing restrictions after surgery. Respondents more commonly recommended scooters to patients with total nonweightbearing restrictions and to those who underwent hindfoot or ankle arthrodesis. We are unaware of other studies that report the frequency of or indications for scooter recommendation. An interesting finding was that 6 respondents (1.9%) indicated that they would not recommend scooter use for any operative indication, and 13 respondents (4.1%) indicated they would not recommend scooters for either partial nonweightbearing or total nonweightbearing. One might expect these percentages to be more similar. This discrepancy may relate to the wording of the survey question. Whereas the first question asks after which surgeries the respondent would be more likely to recommend a scooter, the second question asks whether the respondent more commonly recommends scooters for partial or total nonweightbearing. The first question may assess how the respondent might, in theoretical scenarios, recommend a scooter, whereas the second question may more closely reflect the respondent’s current practice.
This study has several limitations. Our 15% response rate resulted in 8 fewer respondents than the 324 that our a priori sample size calculation indicated were needed. We attempted to restrict our survey to only practicing AOFAS lower extremity surgeons, but several respondents did not meet this inclusion criterion. Thus, the target population on which the sample size calculation was based included some ineligible individuals, and the needed sample size may actually have been met. The 15% response rate is also likely an underestimation of our true response rate among practicing surgeons. Nonetheless, our results may be subject to response bias, with surgeons who have had more experience with scooter-related injuries being more likely to respond. This bias limits confidence in our estimate of the prevalence of scooter-related injuries. Recall bias may affect the reporting of common characteristics of injured patients. Future prospective studies could minimize recall bias. Our survey was open for a period of 1 month, and it is possible that a longer survey period may have increased the response rate. However, more than 60% of responses were received during the first week after the survey was distributed, with a substantial drop until a survey reminder approximately 1 week before survey closure resulted in approximately 30% of responses received during the final week. This pattern suggests that opening the survey for a longer period would not have substantially increased the response rate because most responses were received during the weeks after survey distribution or reminder.
An additional limitation of survey studies is the lack of answers to explain survey findings, such as the reasons for falls among patients with certain characteristics. In our questions regarding mechanism of scooter-related injury, we did not include “backing up while on the scooter” as a response option. Respondents attempting to report this option would likely have selected the “other” response choice. However, this may be a common mechanism of injury that cannot be analyzed with our survey findings and could be explored further in future studies. Finally, this study was not designed to compare injuries associated with scooters vs other assistive devices and did not investigate all adverse events potentially associated with scooter use.
Conclusion
Surgeon members of the AOFAS said they recommend scooters to most patients who have total or partial weightbearing restrictions after lower extremity surgery. The mean reported prevalence of postoperative scooter-related injury was 2.5%. The most common mechanism of injury was making a sharp turn on the scooter. Factors associated with scooter-related injury were female gender, age >44 years, obesity, and sedentary lifestyle. Surgeons and physical therapists may consider these findings when educating patients about the use of assistive devices.
Supplemental Material
Supplemental Material, FAO914561-ICMJE for Knee Scooter–Related Injuries: A Survey of Foot and Ankle Orthopedic Surgeons by Rafa Rahman, Brett A. Shannon and James R. Ficke in Foot & Ankle Orthopaedics
Acknowledgments
We thank Michelle Seu, research fellow at the Johns Hopkins University School of Medicine, Department of Plastic and Reconstructive Surgery, for her contribution in producing the figure of the knee scooter (Figure 1). We also thank Carrie Price, informationist at the Johns Hopkins University Welch Medical Library, for her assistance with literature review on the topic of knee scooters.
Requests for supporting data may be directed to James R. Ficke, MD, at jficke1@jhmi.edu
Appendix A
Survey distributed to members of the American Orthopaedic Foot & Ankle Society in May-June 2019 regarding postoperative use of knee scooters.
-
Location of practice
North America
South America
Europe
Asia
Africa
Other
-
Gender
Male
Female
Other
-
Type of fellowship training
Foot and ankle
Orthopedic trauma
Trauma and foot and ankle
Other
None
Number of years in practice?
-
Do you currently perform lower extremity surgeries?
Yes
No
The following questions were asked only of respondents who answered “Yes” to question 5.
Number of lower extremity surgeries performed in a typical month?
-
For which of the following surgeries would you be likely to recommend orthopedic scooter use at any point during the non- or partial weightbearing postoperative period? (You may select more than 1 option.)
Forefoot/midfoot arthrodesis
Hindfoot arthrodesis
Ankle arthrodesis
Lower extremity osteotomy
Lower extremity fracture fixation
Achilles tendon repair
Other
Would not recommend for any surgery
In an average month, for how many surgical patients do you recommend use of a lower extremity partial or nonweightbearing device (eg, crutches, orthopedic scooters, etc.)?
For how many of these surgical patients, in an average month, do you recommend use of an orthopedic scooter?
-
Do you more commonly recommend orthopedic scooters for partial or nonweightbearing, or both?
Partial weightbearing
Nonweightbearing
Both
Neither
-
Which patient factors would make you MORE LIKELY to recommend use of an orthopedic scooter for an individual patient? (You may select more than 1 option.)
Male gender
Female gender
<18 years old
18-44 years old
44-75 years old
75 years old
Underweight (BMI < 18.5)
Normal weight (BMI 18.5-24.9)
Overweight (BMI 25-29.9)
Obese (BMI > 30)
Sedentary lifestyle
Active lifestyle
None of the above
-
Which patient factors would make you LESS LIKELY to recommend use of an orthopedic scooter for an individual patient? (You may select more than 1 option.)
Male gender
Female gender
<18 years old
18-44 years old
44-75 years old
75 years old
Underweight (BMI < 18.5)
Normal weight (BMI 18.5-24.9)
Overweight (BMI 25-29.9)
Obese (BMI > 30)
Sedentary lifestyle
Active lifestyle
None of the above
-
Have you had any patients suffer injuries in relationship to their orthopedic scooter use following a surgery?
Yes
No
Unsure
The following questions were asked to only those who answered “yes” to question number 13.
Approximately what percentage of patients for whom you have recommended orthopedic scooter use have suffered an injury related to their orthopedic scooter use? (Please enter a percentage between 0% and 100%.)
-
Of your patients who have suffered injuries associated with orthopedic scooter use, which of the following were common factors among these patients?
Male gender
Female gender
<18 years old
18-44 years old
44-75 years old
75 years old
Underweight (BMI <18.5)
Normal weight (BMI 18.5-24.9)
Overweight (BMI 25-29.9)
Obese (BMI > 30)
Sedentary lifestyle
Active lifestyle
None of the above
-
What types of injuries have you seen related to orthopedic scooter use following a surgery? (You may select more than 1 option.)
Ipsilateral upper extremity trauma
Contralateral upper extremity trauma
Ipsilateral ankle trauma
Contralateral ankle trauma
Ipsilateral knee trauma
Contralateral knee trauma
Ipsilateral other lower extremity trauma
Contralateral other lower extremity trauma
Surgical wound complication
Other
-
Have any of your surgical patients with an injury related to orthopedic scooter use required additional surgery?
Yes
No
Unsure
-
Which of the following sequelae from orthopedic scooter-related injuries have you treated? (You may select more than 1 option.)
Surgical treatment of a new injury
Surgical revision of index procedure
Nonsurgical treatment of an injury that resulted in additional mobility deficit
Other
-
Which of the following mechanisms have caused injury related to orthopedic scooter use among your surgical patients? (You may select more than 1 option.)
Moving downhill while on the orthopedic scooter
Making a sharp turn while on the orthopedic scooter
Moving too fast while on the orthopedic scooter
Hitting an obstacle while on the orthopedic scooter
Loss of balance while non-motile on the orthopedic scooter
Other
Unsure
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: James R. Ficke, MD,  https://orcid.org/0000-0002-0275-4223
https://orcid.org/0000-0002-0275-4223
References
- 1. American Thoracic Society Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. [DOI] [PubMed] [Google Scholar]
- 2. Bender R, Lange S. Adjusting for multiple testing—when and how? J Clin Epidemiol. 2001;54(4):343–349. [DOI] [PubMed] [Google Scholar]
- 3. Herbert AJ, Williams AG, Hennis PJ, et al. The interactions of physical activity, exercise and genetics and their associations with bone mineral density: implications for injury risk in elite athletes. Eur J Appl Physiol. 2019;119(1):29–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kocher BK, Chalupa RL, Lopez DM, Kirk KL. Comparative study of assisted ambulation and perceived exertion with the wheeled knee walker and axillary crutches in healthy subjects. Foot Ankle Int. 2016;37(11):1232–1237. [DOI] [PubMed] [Google Scholar]
- 5. Patel N, Batten T, Roberton A, et al. A comparison of energy consumption between the use of a walking frame, crutches and a Stride-on rehabilitation scooter. Foot (Edinb). 2016;28:7–11. [DOI] [PubMed] [Google Scholar]
- 6. Reid M. Personal paper: orthopaedic scooter. Br Med J (Clin Res Ed). 1986;292(6528):1121–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roberts P, Carnes S. The orthopaedic scooter. An energy-saving aid for assisted ambulation. J Bone Joint Surg Br. 1990;72(4):620–621. [DOI] [PubMed] [Google Scholar]
- 8. Salminen AL, Brandt A, Samuelsson K, et al. Mobility devices to promote activity and participation: a systematic review. J Rehabil Med. 2009;41(9):697–706. [DOI] [PubMed] [Google Scholar]
- 9. Yeoh J, Ruta D, Murphy GA, et al. Post-operative use of the knee walker after foot and ankle surgery, a retrospective study. Foot Ankle Orthop. 2017;2(3). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO914561-ICMJE for Knee Scooter–Related Injuries: A Survey of Foot and Ankle Orthopedic Surgeons by Rafa Rahman, Brett A. Shannon and James R. Ficke in Foot & Ankle Orthopaedics