Abstract
Background:
The transfer of flexor-to-extensor is widely used to correct lesser toe deformity and joint instability. The flexor digitorum longus tendon (FDLT) is percutaneously transected at the distal end and then routed dorsally to the proximal phalanx. The transected tendon must have enough mobility and length for the transfer. The purpose of this study was to dissect the distal end of FDLT and identify the optimal technique to percutaneously release FDLT.
Methods:
Eight fresh adult forefoot specimens were dissected to describe the relationship between the tendon and the neurovascular bundle and measure the width and length of the distal end of FDLT. Another 7 specimens were used to create the percutaneous release model and test the strength required to pull out FDLT proximally. The tendons were randomly released at the base of the distal phalanx (BDP), the space of the distal interphalangeal joint (SDIP), and the neck of the middle phalanx (NMP).
Results:
At the distal interphalangeal (DIP) joint, the neurovascular bundle begins to migrate toward the center of the toe and branches off toward the center of the toe belly. The distal end of FDLT can be divided into 3 parts: the distal phalanx part (DPP), the capsule part (CP), and the middle phalanx part (MPP). There was a significant difference in width and length among the 3 parts. The strength required to pull out FDLT proximally was about 168, 96, and 20 N, respectively, for BDP, SDIP, and NMP.
Conclusion:
The distal end of FDLT can be anatomically described at 3 locations: DPP, CP, and MPP. The tight vinculum brevis and the distal capsule are strong enough to resist proximal retraction. Percutaneous release at NMP can be performed safely and effectively.
Clinical Relevance:
Percutaneous release at NMP can be performed safely and effectively during flexor-to-extensor transfer.
Keywords: FDLT, vinculum brevis, plantar capsule, BDP, NMP
Introduction
Taylor reported the treatment of claw toes by multiple transfers of flexor into extensor tendons in 1951. 15 The transfer of flexor-to-extensor is widely used to correct lesser toe deformity and stabilize the metatarsophalangeal joint. It was originally designed to treat flexible claw toes. 6 Now, this process is often combined with plantar plate repair, proximal interphalangeal arthrodesis, or Weil osteotomy to treat more complicated lesser toe deformities. 2 -4,7,9 In addition to flexible claw toes, the indications of the procedure include the hammer toe, the crossover toe, and the metatarsophalangeal (MTP) joint instability, even some of the lesser toe deformities in rheumatoid conditions, stroke, and spinal cord injury. 11
In order to ensure that the tendon to be transferred will be of appropriate length, some authors feel that the flexor tendon should be cut as far distally as possible. 1,11 Most authors advocate that flexor digitorum longus tendon (FDLT) should be transected percutaneously at its insertion into the base of the distal phalanx. 2,4,7,8 For effective transfer, it is necessary for the tendon to have sufficient mobility and length.
The purpose of this study was to assess the anatomy and determine the most effective way of releasing FDLT for flexor-to-extensor transfer.
Materials and Methods
Fifteen fresh-frozen adult forefoot specimens were used for this study, including 8 left and 7 right, nine male and six female. Red latex perfusion was used in 8 specimens, and no latex perfusion was used in 7 feet. The experiments were performed on the second, third, and fourth toes of each foot. The fresh human tissue lab at Duke University supplied the specimens. None of the specimens had any obvious lesser toe deformity. All specimens were thawed for 24 hours at room temperature prior to dissection.
The 8 feet, which were perfused with red latex through the dorsal pedis artery, were used for gross anatomy. Plantar skin and superficial soft tissue were removed, exposing the tendon sheath and the bilateral neurovascular bundles. The space between the distal end of the FDLT and the proper digital nerve and artery was observed in each specimen.
The vascular nerve bundles and superficial soft tissue were removed, exposing the tendon and its insertion distally. The distal end of the FDLT was divided into 3 components: the distal part (distal bone insertion), the middle part (capsule of the distal interphalangeal joint), and the proximal part (the soft vinculum brevis). The length and width of the 3 parts were measured using electronic digital calipers.
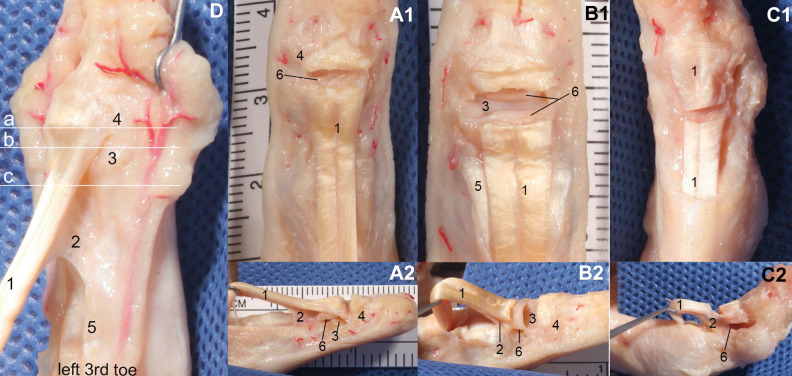
Toe specimens from another 7 feet without red latex perfusion were cut off at the base of the metatarsal bone. The plantar flexor tendon sheath, FDLT, MTP, distal interphalangeal (DIP) joint, and proximal interphalangeal (PIP) joint were kept intact. The flexor tendon sheath was opened to A1 pulley. The distal end of FDLT was exposed clearly, so it could be cut accurately for the experiment. Twenty-one toes from 7 feet were randomly divided into 3 groups according to the random numbers produced by the Excel form (Figure 1D). The tendons in group A were cut at the base of distal phalanx (BDP) (Figure 1A); group B were cut at the distal interphalangeal joint space (SDIP) (Figure 1B); those in group C were cut in the neck of the middle phalanx (NMP) (Figure 1C). The toe was then fixed on the test bench, the metatarsophalangeal joint and the interphalangeal joints were kept at the 0-degree position. The proximal end of the FDLT was also fixed on the test bench without any tension. The INSTRON (model 1321, from the orthopedic biomechanics laboratory at Duke University) was used to test the force required to pull out the distal end of the FDLT (Figure 2).
Figure 1.
Model of cutting off the distal end of flexor digitorum longus tendon (FDLT) at different levels. Cutting at base of the distal phalanx (BDP): (A1) anteroposterior view; (A2) lateral view. Cutting at space of the distal interphalangeal joint (SDIP): (B1) anteroposterior view; (B2) lateral view. Cutting at neck of the middle phalanx (NMP): (C1) anteroposterior view; (C2) lateral view. (D) Relationships among the 3 cutting levels: 1, FDLT; 2, proximal part of the vinculum brevis; 3, head of the middle phalanx; 4, BDP; 5, flexor digital brevis tendon; 6, capsule. Line a: BDP; line b: SDIP; line c: NMP.
Figure 2.
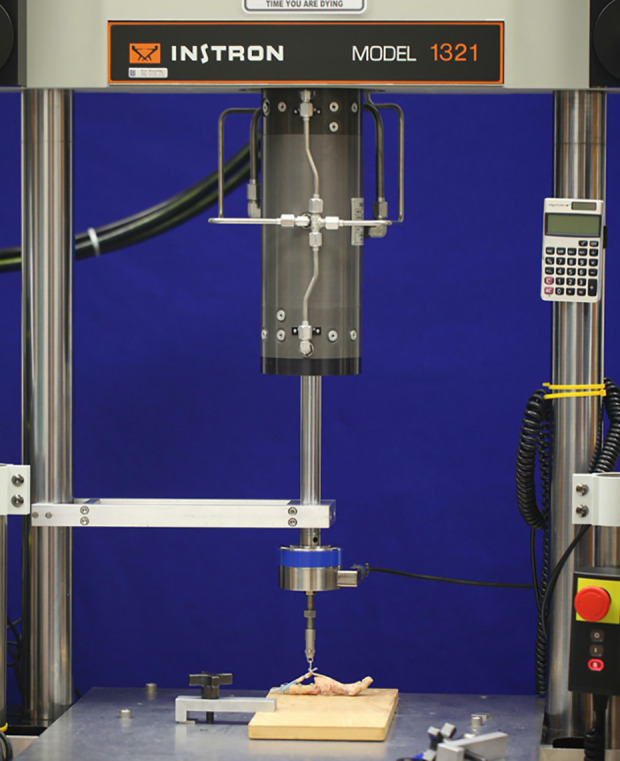
Method, establishment, and equipment used in the biomechanical test.
Sample size was conducted via PASS 14.0 (NCSS, LLC, Kaysville, UT). Experimental plan was to release the tendon at 3 different levels and hypothesized an SD of 50 N. The significance level was set to alpha=0.05. The result of sample size was 18. An additional specimen was reserved for each group in order to allow for potential damage during the test. All continuous variables are reported as means ± SDs. Normal distribution in continuous variable was verified with the Kolmogorov-Smirnov test. One-way analysis of variance was performed for continuous variables between the different levels of toes, depending on the normality of the data distribution. Statistical significance was defined as P <.05. SPSS software (version 18.0; SPSS, Inc, an IBM Company, Chicago, IL) was used for all statistical analyses.
Results
Tendon Anatomy
The neurovascular bundles, which arise from the plantar intermetatarsal nerve and artery, located on both sides of the tendon sheath, travel distally along the tendon sheath. The plantar digital nerves lay plantar to the plantar digital arteries. The neurovascular bundles migrate medially as they travel distally. The artery migrates centrally and forms an anastomosis with the contralateral artery, forming the arterial arch at the base of the distal phalanx. The arterial arch gives off several branches toward the toe tip (Figure 3). The neurovascular bundle and the arterial arch overlapped the tendon in the base of the distal phalanx. The nerve also migrates centrally a little and gives off branches to the toe tip.
Figure 3.

Relationship between the neurovascular bundle and the distal end of flexor digitorum longus tendon (FDLT) (the left second toe). 1, fat pad; 2, pulp artery; 3, distal transverse arch; 4, proper plantar digital artery; 5, distal end of the FDLT; 6, pulley; and 7, proper plantar digital nerve.
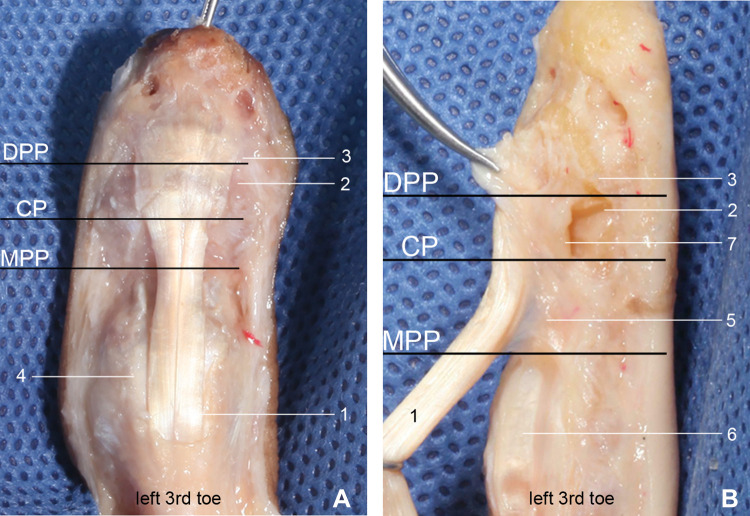
FDLT leaves the tendon sheath distally and widens gradually, finally attaching to the distal phalanx. The distal end of FDLT can be divided into 3 parts: the distal phalanx part (DPP), the capsular part (CP), and the middle phalanx part (MPP) (Figure 4). The DPP lies in the plantar side of the distal phalanx, also called the bony insertion. The CP lies in the space of the DIP, connected to the capsular (plantar plate) through the tight vinculum brevis. The MPP is connected to the middle phalanx through the loose vinculum brevis. The lengths of the 3 parts are shown in Table 1, and the widths in Table 2.
Figure 4.
Division of the distal part of flexor digitorum longus tendon (FDLT) (left third toe): (A) anteroposterior view; (B) Lateral view. 1, FDLT; 2, distal interphalangeal joint (DIP); 3, base of the distal phalanx (BDP); 4, proximal interphalangeal joint (PIP); 5, proximal part of the vinculum brevis; 6, FDLT; 7, capsule of the DIP. Abbreviations: DPP, distal phalanx part; CP, capsule part; MPP, middle phalanx part.
Table 1.
Length of the Distal End of FDLT.
| Second Toe, mm (Mean ± SD) | Third Toe, mm (Mean ± SD) |
Fourth Toe, mm (Mean ± SD) |
P Value | |
|---|---|---|---|---|
| DPP | 7.7 ± 1.3 | 7.3 ± 1.4 | 6.3 ± 1.2 | .121 |
| CP | 4.5 ± 1.2 | 4.1 ± 1.0 | 3.5 ± 0.8 | .200 |
| MPP | 5.0 ± 1.7 | 4.1 ± 1.5 | 3.4 ± 1.0 | .090 |
Abbreviations: CP, capsular part; DPP, distal phalanx part; MPP, middle phalanx part.
Table 2.
Width of the Distal End of FDLT.
| DPP, mm (Mean ± SD) |
CP, mm (Mean ± SD) |
MPP, mm (Mean ± SD) |
P Value | |
|---|---|---|---|---|
| Second toe | 7.9 ± 0.8 | 5.5 ± 0.8 | 4.4 ± 0.3 | <.001 |
| Third toe | 7.4 ± 1.3 | 5.5 ± 1.1 | 4.3 ± 0.7 | <.001 |
| Fourth toe | 6.8 ± 1.0 | 4.8 ± 0.7 | 4.0 ± 0.6 | <.001 |
Abbreviations: CP, capsular part; DPP, distal phalanx part; MPP, middle phalanx part.
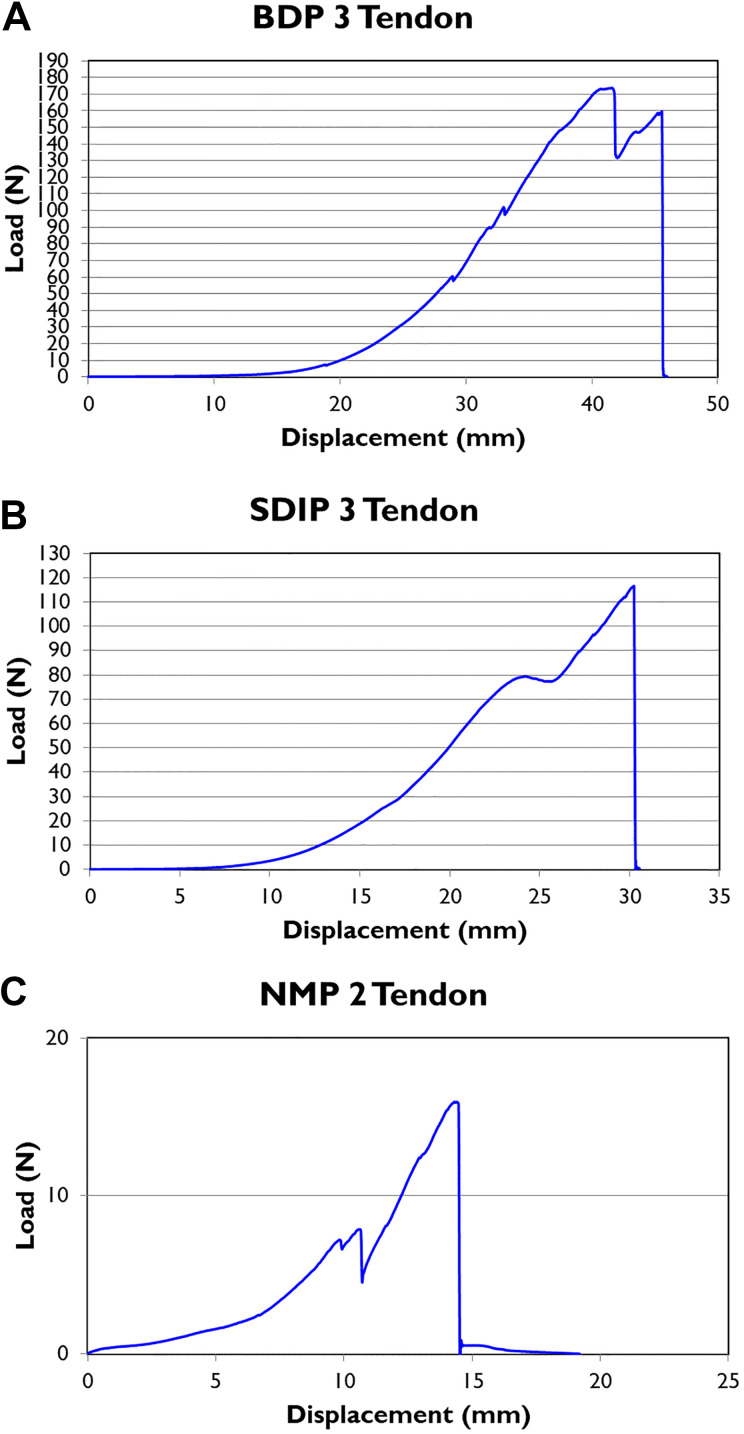
Biomechanical Strength Needed to Pull Out the Tendon
The distal end of the FDLT was transected at the BDP, SDIP, and NMP and then the force required to pull out the FDLT proximally was tested. The results of the 3 groups are shown in Table 3. The tendons in group A were cut at the BDP, and FDLT was connected to the middle and distal phalanx through the soft vinculum brevis, capsule, and vinculum longus. The force required to pull out FDLT proximally was quite high (Figure 5A). In 2 cases, we failed to pull it out. In group B, tendons were cut at the SDIP, and the FDLT was connected to the middle phalanx through the soft vinculum brevis, part of the capsule, and vinculum longus. Moderate force was required to pull the FDLT out proximally, less than in group A, but still very high (Figure 5B). In group C, tendons were cut at the NMP, and the FDLT was connected to the middle phalanx through the soft vinculum brevis and vinculum longus alone. For this reason, the FDLT was easily pulled out through the proximal incision (Figure 5C).
Table 3.
Strength Required to Pull Out the FDLT Proximally.
| n | Strength, N (Mean ± SD) |
95% CI | P Value | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Group A | 5 | 168.2 ± 13.5 | 151.4 | 185.0 | <.001 |
| Group B | 7 | 96.3 ± 15.8 | 81.7 | 111.0 | |
| Group C | 7 | 20.5 ± 9.9 | 11.4 | 29.6 | |
Abbreviation: CI, confidence interval; FDLT, flexor digitorum longus tendon.
Figure 5.
(A) Cutting at the base of the distal phalanx (BDP). (B) Cutting at the space of the distal interphalangeal joint (SDIP). (C) Cutting at the neck of the middle phalanx (NMP).
Discussion
From the anatomic dissection, the neurovascular bundles travel along the flexor tendon sheath. They moved toward the center of the toe in the distal phalanx, then formed a transverse arch and gave rise to several branches into the belly of the toe. The bony insertion of FDLT is fan-shaped and located on the plantar side of the distal phalanx. The tendon in the distal phalanx is closely related to the neurovascular bundle and its branches. With percutaneous release of FDLT, the more distal the cutting plane is, the greater the risk of damage to the neurovascular bundle. FDLT is still wide at the BDP, so percutaneous release is more difficult and it becomes more likely that the tendon needs to be cut repeatedly. FDLT becomes narrow proximally and then enters the flexor tendon sheath. In the NMP, FDLT is narrow and limited in the flexor tendon sheath, so percutaneous cutting is easier and safer with respect to the neurovascular bundle.
The plantar capsule of the DIP is thickened significantly. FDLT is connected to the plantar capsule through the tight vinculum brevis. The test results show that the intact vinculum brevis and capsule can resist strong tension. As a result, it can be very difficult to pull out the tendon proximally, as shown with the pullout force reaching 168 N, and the cases in which it was not possible to pull it out. Sasaki reported 2 cases in which full flexion of the PIP was produced by the intact short vinculum after complete division of both flexor tendons. 13 The vinculum brevis of the flexor digitorum profundus tendon was found to apply traction to the volar plate on flexion of the DIP. 5
Percutaneous release at the SDIP, although part of the capsule and the tight vinculum brevis will be cut, often leaves part of the capsule and the tight vinculum brevis connected, and so leaves the tendon capable of resisting the strong extension force. The force needed to pull out the FDLT proximally can reach about 96 N. With regard to percutaneous release at the NMP, only the loose vinculum brevis and longus connect the FDLT to the phalanx. The force required to pull out FDLT proximally is only 20 N. At that level, there is very little connection of the tendon to the bone or soft tissues. Many previous works mention that the FDLT should be transected at its insertion into the BDP. 2,4,7,8 The length of the CP is about 4.0 mm; percutaneous release at the NMP will not increase the tension of the tendon after transposition.
Kwon reported that through a small transverse “stab” incision made at the level of the distal plantar flexion crease (under the DIP), the FDLT is percutaneously released from the BDP using a No. 11 blade. 8 The flexor digitorum longus is released distally through a stab incision just distal to the distal interphalangeal flexion crease, with care taken not to enter the DIP. 3 A technique for percutaneous tenotomy and the capsule release at the level of the DIP has been described. 7 If the capsule is completely transected, it can easily render the plantar of DIP unstable.
Taylor brought the FDLT around the lateral aspect of the proximal phalanx and sutured to the extensor expansion. 15 In Parrish’s modification, the long flexor is divided longitudinally. Each half is brought out on each side of the proximal phalanx and sutured to itself and then to dorsal expansions of the extensor tendon. 12 Many authors advocate that the FDLT be transferred to the proximal dorsal side, sutured end to end, or sutured with the central part of the extensor tendon. 14 Myerson sutured the transferred tendon stump through a knot under the tension with the MTP in approximately 30 degrees of dorsiflexion and the ankle in neutral dorsiflexion. 10 Optimizing tendon length and excursion may render these techniques more feasible.
Because of the limitations of the specimens, this study had only 15 specimens, from both men and women. It is inevitable that there will be differences in tendons from feet of different sizes. This is only a single-center study. A multicenter clinical study is needed in the future. Future research will have greater numbers of specimens, and note the size of each foot.
Conclusion
The distal end of FDLT can be anatomically described at 3 distinct locations: DPP, CP, and MPP. Based on this study, the vinculum brevis and the distal capsule resist proximal retraction; therefore, percutaneous release at NMP can be performed safely and is most effective. The neurovascular bundle begins to migrate toward the center of the toe at the distal interphalangeal joint.
Supplemental Material
Supplemental Material, FAO884274-ICMJE for Anatomy of the Distal End of Flexor Digitorum Longus Tendon and Percutaneous Release Technique: A Cadaveric Study by Baofu Wei, Ruoyu Yao and Annunziato Amendola in Foot & Ankle Orthopaedics
Acknowledgments
We would like to sincerely thank Professor Richard Glisson of Duke University for the biomechanical test. HFTL of Duke University provided the fresh foot specimens.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Baofu Wei, MD,  https://orcid.org/0000-0001-6979-1718
https://orcid.org/0000-0001-6979-1718
References
- 1. Arbab D, Frank D, Bouillon B, Lüring C. Behandlung flexibler leinzehenfeh- lstellungen: transfer der flexor-digitorum-longus-sehne [Correction of flexible lesser toe deformity : Transfer of the flexor digitorum longus tendon]. Oper Orthop Traumatol. 2017;29(5):452–458. [DOI] [PubMed] [Google Scholar]
- 2. Bouché RT, Heit EJ. Combined plantar plate and hammertoe repair with flexor digitorum longus tendon transfer for chronic, severe sagittal plane instability of the lesser metatarsophalangeal joints: preliminary observations. J Foot Ankle Surg. 2008;47(2):125–137. [DOI] [PubMed] [Google Scholar]
- 3. Boyer ML, DeOrio JK. Transfer of the flexor digitorum longus for the correction of lesser-toe deformities. Foot Ankle Int. 2016;28(4):422–430. [DOI] [PubMed] [Google Scholar]
- 4. Butterworth M. Tendon transfers for management of digital and lesser metatarsophalangeal joint deformities. Clin Podiatr Med Surg. 2016;33(1):71–84. [DOI] [PubMed] [Google Scholar]
- 5. Flindall E, Mcgrouther DA. Accessory roles of the vinculum breve of the flexor digitorum profundus and Check-Rein ligaments at the distal interphalangeal joint. J Hand Surg Br. 1991;16(3):305–310. [DOI] [PubMed] [Google Scholar]
- 6. Frey-Ollivier S, Catena F, Hélix-Giordanino M, Piclet-Legré B. Treatment of flexible lesser toe deformities. Foot Ankle Clin. 2018;23(1):69–90. [DOI] [PubMed] [Google Scholar]
- 7. Haddad SL, Sabbagh RC, Resch S, Myerson B, Myerson MS. Results of flexor-to-extensor and extensor brevis tendon transfer for correction of the crossover second toe deformity. Foot Ankle Int. 1999;20(12):781–788. [DOI] [PubMed] [Google Scholar]
- 8. Kwon JY, De Asla RJ. The use of flexor to extensor transfers for the correction of the flexible hammer toe deformity. Foot Ankle Clin. 2011;16(4):573–582. [DOI] [PubMed] [Google Scholar]
- 9. Myers SH, Schon LC. Forefoot tendon transfers. Foot Ankle Clin. 2011;16(3):471–488. [DOI] [PubMed] [Google Scholar]
- 10. Myerson MS, Jung HG. The role of toe flexor-to-extensor transfer in correcting metatarsophalangeal joint instability of the second toe. Foot Ankle Int. 2005;26(9):675–679. [DOI] [PubMed] [Google Scholar]
- 11. Ozdolop S, Mathew KM, McClelland M, Ravichandran G. Modified Girdlestones-Taylor procedure for claw toes in spinal cord injury. Spinal Cord. 2006;44(12):787–790. [DOI] [PubMed] [Google Scholar]
- 12. Parrish TF. Dynamic correction of claw toes. Orthop Clin North Am. 1973;4:97–102. [PubMed] [Google Scholar]
- 13. Sasaki Y, Nomura S. An unusual role of the vinculum after complete laceration of the flexor tendons. J Hand Surg Br. 1987;12(1):105–108. [DOI] [PubMed] [Google Scholar]
- 14. Shirzad K, Kiesau CD, DeOrio JK, Parekh SG. Lesser toe deformities. J Am Acad Orthop Surg. 2011;19(8):505–514. [DOI] [PubMed] [Google Scholar]
- 15. Taylor RG. The treatment of claw toes by multiple transfers of flexor into extensor tendons. J Bone Joint Surg. 1951;33-B(4):539–542. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO884274-ICMJE for Anatomy of the Distal End of Flexor Digitorum Longus Tendon and Percutaneous Release Technique: A Cadaveric Study by Baofu Wei, Ruoyu Yao and Annunziato Amendola in Foot & Ankle Orthopaedics