Abstract
Background:
Hallux valgus can alter load bearing in the foot leading to abnormal forces on the second toe. The purpose of this study was to determine demographic and radiographic factors associated with second ray hammertoes in hallux valgus using 3-dimensional weightbearing CT scans.
Methods:
Seventy-one patients who underwent a modified Lapidus procedure for hallux valgus with preoperative weightbearing CT scans were separated into 2 groups: (1) hallux valgus only (47 feet) and (2) hallux valgus with second ray hammertoe (29 feet). Preoperative age, body mass index (BMI), sex, hallux valgus angle (HVA), intermetatarsal angle (IMA), absolute and effective metatarsal (MT) lengths, ratios between metatarsal lengths, Meary angle, metatarsus adductus angle (MAA), and pronation were measured. Mean values of continuous variables were compared and both simple and multivariable logistic regression models were used to evaluate associations between variables and hammertoe occurrence.
Results:
Patients in the hammertoe group were found to be significantly older and have higher BMIs, HVAs, effective second MT lengths, IMAs, and more apex plantar Meary angles (all P < .05). The multivariable analysis demonstrated that a higher IMA and a more apex plantar Meary angle were the only significant predictors of second ray hammertoe risk (P = .03 and P = .01, respectively) once corrected for age and BMI.
Conclusion:
Significant associations were found between older age, higher BMI, and more severe deformity and the occurrence of hammertoe in hallux valgus patients. These results may help clinicians counsel hallux valgus patients about the risk of developing an advanced hammertoe deformity.
Level of Evidence:
Level III, retrospective comparative series
Keywords: hallux valgus, bunion, hammertoe, second ray, weightbearing CT
Introduction
In hallux valgus, the great toe of the foot deviates laterally while the first metatarsal shifts medially, causing malalignment at the first metatarsophalangeal (MTP) joint. 10,14,15,30 This common pathology affects 23% of people between 18 and 65 years old and 36% of people more than 65 years old. 14,27 Left untreated, hallux valgus can contribute to gait impairment, loss of balance, disabling foot pain, and an increased fall risk. 10,27 Hallux valgus results in progressive deformity as the first metatarsal moves medially and pronates, resulting in unbalanced forces on the proximal phalanx of the great toe and sesamoids. 3 Altered mechanics at the first MTP joint may induce secondary pathologies such as hammertoes and tarsometatarsal arthritis. 13 Altered loading of the first ray transfers increased pressure to the lesser metatarsals, 38 which can overload the joints and cause MTP joint hyperextension and proximal interphalangeal joint plantarflexion as seen in hammertoe deformity. 14,17 The second ray of the foot is highly susceptible to this increased loading pressure and overcrowding because of its proximity to the first metatarsal. 17,30,34 Hammertoes may be more painful and symptomatic than the inciting hallux valgus, leading to poorer outcomes. 9,17,21
Treatment of hallux valgus typically begins with nonoperative management, including wider shoes, shoe inserts, and bunion shields. These options seek to control symptoms rather than addressing the underlying deformity, and consequently, may not slow the progression of secondary pathologies. 15 As the main indication for operative correction is pain and disability, 8 patients may develop concomitant second ray complications before reaching the clinical threshold for surgery.
Operative treatment has been shown to successfully correct hallux valgus and concomitant second ray pathology 38 to improve patient function. 35 However, surgeries that address second ray pathologies in addition to hallux valgus are more complex than hallux valgus correction alone, and there are higher rates of decreased range of motion and increased postoperative complications. 13 Specifically, it has been found that surgeries to correct hammertoe deformities in conjunction with hallux valgus have a lower rate of patient satisfaction 4 as well as less favorable correction outcomes than when either deformity is treated separately. 5 Therefore, early intervention may theoretically prevent progression to associated second ray pathologies and improve clinical outcomes. Few studies, however, have investigated the association between second ray pathology and hallux valgus. 13
Conventional evaluation of hallux valgus has focused on weightbearing plain radiographs, 2,3 but hallux valgus is a triplanar deformity and includes a pronation component not well visualized on 2-dimensional imaging. 1 Standard weightbearing radiographs may be inadequate 2,22 because of their inability to capture axial rotation of the first ray, the presence of superimposed bones, and its reliance on proper foot orientation and beam projection. 23,31 Weightbearing CT scans overcome the limitations of weightbearing plain radiographs as they can evaluate the foot in 3 dimensions and do not require calibration. 2,31 This relatively new imaging modality could be used to identify characteristics of patients with hallux valgus that are associated with second ray pathologies such as hammertoe.
Previous research has shown that hallux valgus occurs more frequently in patients who are female, older, have a family history, 28 have abnormal metatarsal ratios, 24 or have a lower body mass index (BMI). 11 Other research found that hallux valgus, neuromuscular dysfunction, metatarsus adductus, pes planus, abnormal metatarsal lengths, 34 higher BMI, and lower intermetatarsal angle (IMA) 19 are risk factors for developing hammertoe. Despite the association of hallux valgus and hammertoes, little research has been conducted on the variables associated with hammertoe deformities in the setting of hallux valgus.
Previous radiographic studies have shown that increased age, hallux valgus angle (HVA), 13 and IMA 17,32 are associated with the development of hammertoe. These studies were limited by uncalibrated measurements and the 2-dimensional nature of radiographs. Therefore, the primary aim of this article was to assess hallux valgus via weightbearing computed tomography, which did not require calibration of measurements, to determine if there was an association between radiographic parameters and patient characteristics and hammertoe deformities in hallux valgus patients indicated for surgical intervention. We expect that patients who have risk factors that may transfer or increase load on the second metatarsal such as BMI, HVA, and IMA would be associated with hammertoe deformities. We also hypothesized that pronation and abnormal effective metatarsal lengths, additional parameters that alter mechanics of the foot, may be correlated with hammertoe deformities.
Methods
Data for this retrospective study of hallux valgus patients indicated for surgical intervention was obtained from an institutional review board–approved foot and ankle registry following permission from the registry steering committee. Consecutive patients who had a first tarsometatarsal fusion for hallux valgus between 2017 and 2019 as well as a preoperative weightbearing CT scan were eligible for inclusion in this study. Patients were found through 2 registry database searches. The first for hallux valgus, International Classification of Diseases, Tenth Revision (ICD-10) code M20.1, Lapidus corrective surgery, Current Procedural Terminology (CPT) code 28297 or 28740, and preoperative weightbearing CT scan noted on their intake form. This database search yielded 43 eligible patients (45 feet). As the option to specify if a patient had a preoperative weightbearing CT scan was new, a second search in the registry was done for all other patients who had hallux valgus and Lapidus surgery between 2017 and 2019. This database search yielded 302 unique eligible patients (316 feet). A total of 251 patients (261 feet) were then excluded overall who were missing preoperative weightbearing CT scans. An additional 18 patients (19 feet) were excluded due to a previous first or second ray surgery, one patient was excluded for rheumatoid arthritis, and 4 patients were excluded due to midfoot osteoarthritis. This left a total of 71 patients (76 feet) for analysis.
These patients were divided into 2 groups based on intraoperative findings: (1) concomitant advanced hammertoe (HT) group and (2) hallux valgus (HV) only group. In order to create a more homogenous group of hammertoe patients as there is a wide variation in the severity of hammertoes, patients who underwent second ray MTP joint release and proximal interphalangeal joint resection were considered to have advanced hammertoe deformities to be treated operatively and were placed in the concomitant advanced HT group. The rest were considered HV-only patients. Within the HV group, there was a subset (n = 8) who had undergone second ray MTP joint release only, indicating a hammertoe too mild to classify as part of the advanced HT group. Within the HT group, there was a subset (n = 5) with second toe dislocation who also underwent concomitant second metatarsal shortening during surgery. This subgroup was considered to have severe hammertoe and was included in the HT group. The HV-only group consisted of 43 patients (47 feet) and was made up of 4 men and 39 women with an average age of 49 (range, 24-68) years. The concomitant advanced HT group had 28 patients (29 feet) including 2 men and 26 women with an average age of 59 (range, 46-68) years.
Patient body mass index (BMI) was recorded for all patients from their preoperative electronic medical records. BMI was analyzed as a continuous variable as well as a categorical variable that included obese and nonobese groups. Obese BMI was considered as 30 or more, and the remaining patients were classified as nonobese.
Radiographic Measurements
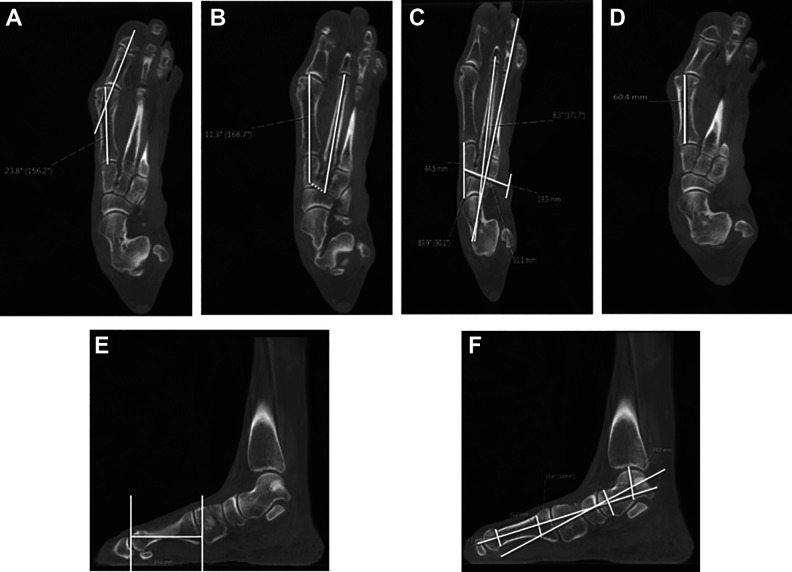
Radiographic parameters were measured from preoperative weightbearing CT scans, which did not require calibration, using picture archiving and communication system (PACS) software Sectra IDs7. These parameters included HVA; IMA; metatarsus adductus angle (MAA); absolute and effective first, second, and third metatarsal lengths, the ratios between the metatarsal lengths; Meary angle; and pronation. HVA and IMA measurements (Figure 1A and B) were taken following protocol used to measure these angles on plain radiographs. 15 HVA was divided into categories based on severity. The mild group consisted of values less than 30 degrees, the moderate group had values between 30 and 40 degrees, and the severe group included values equal to or greater than 40 degrees. MAA (Figure 1C) was measured from axial weightbearing CT slices using Sgarlato’s method. 29 Absolute MT measurements (Figure 1D) were determined on the axial weightbearing CT slices that demonstrated the longest length between the ends of each MT. Effective MT measurements (Figure 1E) were made on sagittal weightbearing CT scans on the slice with the longest distance between 2 vertical lines marking the ends of each MT. Ratios of MT lengths were calculated for the absolute second MT to absolute first MT and the effective second MT to effective first MT. Meary angle (Figure 1F) was measured from sagittal weightbearing CT scans as the angle between a line bisecting the talus and a second line bisecting the first MT. 36 Apex dorsal measurements where the line bisecting the talus was found superior to the line bisecting the first MT were considered negative angles. Pronation of the first metatarsal was determined from preoperative weightbearing CT scans in relation to the second metatarsal as a reference as described previously by Campbell et al. 1 Because pronation was determined by an outside institution using proprietary 3-dimensional computer-aided design, pronation of the first ray was only available for 27 patients of which 19 were in in the HV-only group and 8 were in the advanced HT group.
Figure 1.
Sample radiographic measurements from weightbearing CT scans. (A) Hallux valgus angle measured from axial weightbearing CT slices as the angle between the hallux and first metatarsal. (B) Intermetatarsal angle measured from axial weightbearing CT slices as the angle between the first and second metatarsals. (C) Metatarsus adductus angle was measured from axial weightbearing CT slices as the angle between the second metatarsal and a line perpendicular to a line bisecting the navicular and cuboid bones. (D) Absolute first MT measured on an axial weightbearing CT slice as the length from one end of the metatarsal bone to the other. (E) Effective first MT length was measured from sagittal weightbearing CT scans as the length between 2 lines projected down from each end of the bone to account for the angle of the metatarsal in the foot. (F) Meary angle was measured from sagittal weightbearing CT slices as the angle between a line bisecting the talus and another bisecting the first metatarsal. CT, computed tomographic; MT, metatarsal angle.
Statistical Methodology
Normality was determined for continuous variables through Shapiro-Wilk test. For variables that fit this assumption of normality, 1-way analysis of variance was conducted to compare the mean values across the different outcome groups. For variables that did not meet the assumption of normality, mean differences were compared through nonparametric Kruskal-Wallis test (including age, BMI, absolute and effective ratio of first to second MT lengths, Meary angle, and preoperative pronation). Associations between demographic and radiographic parameters and advanced second ray hammertoe were evaluated using simple logistic regressions. Sensitivity analyses were conducted using 3 different foot outcome variable encodings to account for the subgroups of mild and severe hammertoe: (1) modeling the odds of advanced hammertoe vs hallux valgus only (n = 76 feet), (2) a model in which feet with mild hammertoe (requiring only an MTPJ release) who did not meet the criteria for the HT group were treated as missing values (n = 68 feet), and (3) a model in which feet with severe hammertoe (requiring a concomitant second metatarsal shortening) were treated as missing values (n = 71 feet).
Additionally, multivariable logistic regression models were generated to adjust risk scores for age and continuous BMI. Separate multivariable logistic regression models were fit for HVA, IMA, MAA, absolute first and second MT lengths, effective first and second MT lengths, and Meary angle. All odds ratios are reported with 95% confidence interval and correspond to the presence of advanced hammertoe compared to the presence of hallux valgus only. Statistical significance of model coefficients was evaluated at the .05 alpha level using Wald tests. Preoperative pronation data was evaluated through Mann-Whitney U test to assess for differences between outcome groups. All analyses were conducted in R, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) using the following packages: dplyr, 37 purrr, 16 and broom. 33
Results
The average HVA in the HV-only group was 34.4 degrees (SD, 7.0 degrees; range, 18.4-53.4). The mean HVA in the concomitant advanced HT group was significantly higher at 38.7 degrees (SD, 8.9 degrees; range, 21.8-61.5, P = .02). The average IMA in the HV-only group was 14.7 degrees (SD, 2.8 degrees; range, 7.8-20.1). The mean IMA in the concomitant advanced HT group was significantly higher at 17.4 degrees (SD, 3.6 degrees; range, 10.9-25.1, P = .0004). The average BMI in the HV-only group was 24.5 (SD, 4.07; range, 18.6-36.2). The mean BMI in the concomitant advanced HT group was significantly higher at 28.2 (SD, 4.63; range, 19.1-43.3, P = .006).
In the HV-only group, the average effective second MT length was 71.3 mm (SD, 4.4 mm; range, 62.2-81.3), whereas the mean effective second MT length in the concomitant advanced HT group was significantly larger at 74.7 mm (SD, 5.1 mm; range, 67.0-85.5, P = .003). The average Meary angle in the HV-only group was 1.4 degrees apex plantar (SD, 6.2 degrees; range, –11.1 to 12.5). The mean Meary angle in the concomitant advanced HT group was significantly higher at 5.6 degrees apex plantar (SD, 6.4 degrees; range, –6.4 to 16.0, P = .01). These differences in mean BMI, HVA, IMA, effective second MT length, and Meary angle were found to be statistically significant (Table 1).
Table 1.
Foot Characteristics Stratified by Advanced Hammertoe Status.a
| Characteristic | Hallux Valgus Only (n = 47) |
Advanced Hammertoe (n = 29) |
P Value |
|---|---|---|---|
| Age | 49 (12.56) | 59 (5.90) | .0005 |
| BMI | 24.54 (4.07) | 28.21 (4.63) | .006 |
| HVA | 34.4 (7.02) | 38.7 (8.92) | .02 |
| Absolute first MT | 60.6 (3) | 61.4 (3.48) | .26 |
| Absolute second MT | 72.8 (3.41) | 74.3 (4.42) | .11 |
| Absolute MT ratio 2:1 | 1.2 (0.03) | 1.21 (0.04) | .48 |
| Effective first MT | 64.4 (3.92) | 65.7 (4.03) | .14 |
| Effective second MT | 71.3 (4.43) | 74.7 (5.14) | .003 |
| Effective MT ratio 2:1 | 1.11 (0.06) | 1.14 (0.06) | .06 |
| IMA | 14.7 (2.76) | 17.4 (3.63) | .0004 |
| MAA | 15.2 (4.26) | 17.5 (5.83) | .06 |
| Meary angle | 1.4 (6.16) | 5.6 (6.44) | .01 |
| Pronation (preop) | 30.5 (9.62) | 25.3 (6.92) | .18 |
Abbreviations: BMI, body mass index; HVA, hallux valgus angle; IMA, intermetatarsal angle; MAA, metatarsus adductus angle; MT, metatarsal; Preop, preoperative.
a Presented as mean (SD) for each characteristic. Comparison of variables across outcome groups (hallux valgus only or hallux valgus and advanced second ray hammertoe). Bold values are statistically significant (P < .05).
Age was also found to be statistically higher by an average of 10 years in the concomitant advanced HT group (P = .0005) than in the HV-only group (Table 1). Additionally, there was a trend toward a higher ratio of second to first effective MT length and MAA measurements in the concomitant advanced HT group compared to the HV-only group (P = .06 for both). No significant difference was found between outcome groups for the mean absolute MT lengths or ratios, effective first MT, or pronation results (all P values > .05).
The simple logistic regression model showed that categorical BMI, where odds of an advanced hammertoe were compared for obese vs nonobese patients, and categorical HVA, where odds of hammertoe were compared for severe vs mild HVA values, were found to be significant predictors of advanced hammertoe risk (Table 2). Every unit increase in BMI increased patient risk of an advanced hammertoe by 15%, and obese patients were 5.66 times more at risk than nonobese patients. Additionally, for every degree increase in HVA, patient risk of an advanced hammertoe increased by 7% overall whereas patients with severe HVA over 40 degrees were 4.5 times more likely than patients with mild HVA measurements of less than 30 degrees to develop an advanced hammertoe. A significant association was also found between the odds of developing an advanced second ray hammertoe and increased age, IMA, MAA, effective second MT length, and a more apex plantar Meary angle through simple logistic regression analyses (Table 2).
Table 2.
Results of Simple Logistic Regression Using Different Hammertoe Groupings.a
| Variable | Advanced Hammertoe Only, OR (95% CI) |
Mild Hammertoe Removed, OR (95% CI) |
Severe Hammertoe Removed, OR (95% CI) |
|---|---|---|---|
| Age | 1.12 (1.05, 1.2) | 1.15 (1.07, 1.25) | 1.12 (1.05, 1.21) |
| BMI (continuous) | 1.15 (1.05, 1.29) | 1.17 (1.05, 1.32) | 1.12 (1.02, 1.26) |
| BMI (obese vs nonobese) | 5.66 (1.67, 22.79) | 6.32 (1.7, 30.76) | 5.37 (1.48, 22.52) |
| HVA | 1.07 (1.01, 1.15) | 1.09 (1.02, 1.18) | 1.08 (1, 1.16) |
| HVA (moderate vs mild) | 1.44 (0.41, 5.95) | 1.55 (0.43, 6.51) | 2.67 (0.6, 18.86) |
| HVA (severe vs mild) | 4.5 (1.13, 21.06) | 6.6 (1.5, 34.76) | 7.5 (1.49, 57.99) |
| IMA | 1.33 (1.13, 1.61) | 1.35 (1.14, 1.66) | 1.37 (1.15, 1.7) |
| MAA | 1.1 (1, 1.22) | 1.35 (1.14, 1.66) | 1.09 (0.99, 1.21) |
| Absolute first MT | 1.09 (0.94, 1.27) | 1.1 (0.95, 1.3) | 1.12 (0.96, 1.32) |
| Absolute second MT | 1.11 (0.98, 1.26) | 1.13 (0.99, 1.29) | 1.11 (0.98, 1.27) |
| Absolute MT ratio 2:1 | 146.68 (0, 214141488.1) | 2259.46 (0, 6109746048.53) | 1.79 (0, 7250286.13) |
| Effective first MT | 1.1 (0.97, 1.25) | 1.11 (0.98, 1.27) | 1.09 (0.97, 1.25) |
| Effective second MT | 1.16 (1.05, 1.31) | 1.2 (1.07, 1.37) | 1.18 (1.06, 1.33) |
| Effective MT ratio 2:1 | 3662.8 (1.22, 20842529.75) | 10350.79 (3.18, 69984346.58) | 24700.29 (4.26, 371731259.85) |
| Meary angle | 1.11 (1.03, 1.21) | 1.11 (1.03, 1.21) | 1.14 (1.04, 1.25) |
Abbreviations: BMI, body mass index; CI, confidence interval; HVA, hallux valgus angle; IMA, intermetatarsal angle; MAA, metatarsus adductus angle; MT, metatarsal; OR, odds ratio.
a This table demonstrates the ORs of a second ray hammertoe occurring based on how a hammertoe is defined. Advanced hammertoes included those patients who underwent a proximal interphalangeal resection and MTPJ capsular release. Mild hammertoes were patients who had an MTPJ capsular release only. Severe hammertoes were patients who required a second metatarsal shortening osteotomy. Bold values are statistically significant (P < .05).
The simple logistic regression models removing the mild and severe hammertoe groups demonstrated findings that were consistent with our original model (Table 2). For the model that removed mild hammertoe patients, a significant association remained between age, BMI, HVA, IMA, MAA, effective second MT length, and Meary angle. When compared to the advanced hammertoe outcome model, odds ratios demonstrated an equal or greater risk of developing moderate to severe hammertoe with every unit increase in these variables. For the model that removed severe hammertoe patients, a significant association remained between age, BMI, HVA, IMA, effective second MT length, and Meary angle while there was no longer a significant association between MAA and the risk of hammertoe. When compared to the advanced hammertoe outcome model, odds ratios demonstrated an equal or greater risk of developing mild to moderate hammertoe with every unit increase in these variables except for BMI. Therefore, sensitivity analysis illustrated that, although the variables associated with the overall risk of developing an advanced hammertoe and the risk of developing a more severe hammertoe remained the same, MAA and BMI were less significant predictors of more mild hammertoe development.
The multivariable logistic regression model demonstrated that only a higher IMA and a more apex plantar Meary angle remained significant predictors of risk of having an advanced hammertoe once the results were adjusted for patient age and BMI (Table 3). For every degree increase in the IMA, the odds of having an advanced hammertoe increased by 22% (P = .03), and for every degree increase apex plantar in Meary angle, the odds of having an advanced hammertoe increased by 13% (P = .01). The trend toward a higher ratio of second to first effective MT length also remained once results were adjusted for patient age and BMI (P = .07). The regression models suggest that the most significant predictors of advanced hammertoe development were increased BMI, IMA, and Meary angle.
Table 3.
Results of Multivariable Logistic Regression on the Odds of Developing an Advanced Hammertoe.a
| Variable | OR (95% CI) | P Value |
|---|---|---|
| HVA | 1.04 (0.97, 1.12) | .28 |
| IMA | 1.22 (1.02, 1.49) | .03 |
| MAA | 1.05 (0.93, 1.18) | .46 |
| Absolute first MT | 1.04 (0.88, 1.24) | .64 |
| Absolute second MT | 1.08 (0.94, 1.25) | .29 |
| Effective first MT | 1.05 (0.9, 1.22) | .54 |
| Effective second MT | 1.12 (0.99, 1.27) | .07 |
| Meary angle | 1.13 (1.03, 1.25) | .01 |
Abbreviations: BMI, body mass index; CI, confidence interval; HVA, hallux valgus angle; IMA, intermetatarsal angle; MAA, metatarsus adductus angle; MT, metatarsal; OR, odds ratio.
a This table shows the OR of certain radiographic parameters on the risk of having an advanced hammertoe after controlling for patient age and BMI. The OR correspond to the presence of an advanced hammertoe compared to presence of hallux valgus only for a 1-unit increase in the independent variable adjusting for age and BMI. Bold values are statistically significant (P < .05).
Discussion
Second ray hammertoe often occurs concomitantly with hallux valgus and has been found to negatively affect patient outcomes by increasing pain and decreasing physical function. 9,17,21 However, few studies have examined which patient characteristics, demographic or anatomical, may increase a patient’s risk of developing this deformity. Previous works that have examined the relationship between hallux valgus and hammertoe used plain radiographs, which are not calibrated and have inherent limitations when analyzing 3-dimensional foot pathologies. 23,31 By using weightbearing CT scans to examine hammertoe in the setting of hallux valgus, we were able to re-evaluate radiographic variables previously determined to be associated with either pathology while also exploring new variables, including first metatarsal pronation and effective MT lengths that were previously difficult to measure on 2-dimensional images. Our study demonstrated an association between the presence of a hammertoe deformity in patients with hallux valgus and increased age, BMI, HVA, IMA, effective second MT length, and apex plantar Meary angle. 13
Variables that act as predictors of an advanced hammertoe deformity can be divided into 2 main groups: (1) those that increase pressure on the second metatarsal directly such as patient BMI and effective second MT length and (2) those that result in worsening deformity at the first MTP joint including age, HVA, IMA, and Meary angle, thereby increasing the likelihood of progression to an advanced second ray hammertoe.
The strong association between hammertoe and higher BMI may be explained by increased force secondary to the patient’s weight on the second ray of the foot, which has been shown to increase the risk of developing a hammertoe regardless of other foot deformities. 7,19 Although BMI has been found to have an inverse relationship with the development of hallux valgus on its own, 11 this elevated pressure from patient BMI coupled with the already increased load on the lesser metatarsals from the hallux valgus 38 may accelerate the development of a hammertoe deformity.
The association between increased effective second MT length and advanced hammertoe may be multifactorial. Greater load bearing with a longer second MT may increase pressure on the second ray and result in the development of a hammertoe. Additionally, a longer second MT can predispose patients to plantar plate tears, which in turn causes MTP joint instability leading to a hammertoe deformity. 6,25 Although statistically significant in univariable analysis, there was only a trend toward statistical significance in the multivariable regression analysis (P = .07) when controlling for BMI. This may suggest that BMI more directly affects the load on the second MT and the development of a hammertoe deformity.
Age was also strongly associated with advanced hammertoe deformities in patients with hallux valgus. Because our study was not population based and only included patients who were indicated for surgical intervention, we hypothesized that age may represent the duration of hallux valgus. Therefore, longstanding disease may result in chronic, repetitive abnormal loading of the second ray and lead to the development of an advanced hammertoe.
Supporting this hypothesis is that the magnitude of the hallux valgus deformity as measured by HVA and IMA was associated with the risk of an advanced hammertoe. In univariable analyses, both increased HVA and IMA were predictors of risk of an advanced hammertoe. HVA has been found to be inversely related to hallux loading and hallux plantarflexion strength. 26 This reduction in loading and flexion strength in hallux valgus results in increased pressure on the lesser MT, 20 which in turn can contribute to a hammertoe deformity. Because IMA has been found to increase in conjunction with HVA, 13 it is reasonable that the same association between hammertoe risk and HVA and IMA was found. After multivariable analysis, however, only IMA remained associated with advanced hammertoe risk. IMA, and not HVA, may better represent the severity of hallux valgus and the transfer of load to the second MT leading to a hammertoe.
A similar conclusion may be drawn from the association between the development of a hammertoe and Meary angle, which represents a sagittal plane deformity. The association between Meary angle and the risk of having an advanced hammertoe remained after multivariable regression analysis (odds ratio 1.13, P = .01). In fact, in the multivariable regression analysis, Meary angle had the second largest effect size after IMA, suggesting sagittal plane deformity plays an important role in the risk of developing an advanced hammertoe. For each 1-degree apex plantar increase in the Meary angle, the risk of having an advanced hammertoe deformity increased 13%. Similar to IMA, this association may be explained by worsening first MTP joint deformity inducing second ray pathology. Meary angle measures the extent of plantarflexion of the first MT in relation to the talar axis and has been found to increase with pes planus. 12 Therefore, more apex plantar Meary angle values suggest a flatter medial longitudinal arch, which may result in increased joint instability and rotation under loading and contribute to hammertoe development. 18
Although no other studies have examined the association of radiographic and demographic parameters and hammertoe risk in the setting of hallux valgus through weightbearing CT, comparison to the study by Gribbin et al 13 demonstrated similar findings where patients who were older and had a higher BMI and HVA had a larger risk of hammertoe development. However, there were some differences in terms of predictive significance. Specifically, our results found Meary angle and IMA to be more predictive of hammertoe development than HVA, a major predictor in the prior paper. This difference could be due to our use of weightbearing CT rather than plain radiographs. As this 3-dimensional modality allowed us to better examine multiplanar variables, it is possible that we could more accurately determine the association between sagittal instability and hammertoe development than was possible on AP radiographs alone. The greater significance of IMA in our study could be due to the role that instability at the first tarsometatarsal joint plays in transferring load to the second metatarsal. Increased HVA may also be associated with a higher BMI or older age, and this may explain why HVA was not a significant predictor once corrected for BMI and age in our study. These variables were not controlled for in the prior study.
There are numerous limitations of this study. The main limitation of this study was its small sample size. The sample was derived from a cohort of patients who were indicated for surgical intervention for hallux valgus and had a preoperative weightbearing CT scan. At our institution, only patients who are indicated for surgical intervention undergo a weightbearing CT scan for preoperative planning purposes. Consequently, the results of this study are applicable only to patients who are indicated for surgical intervention based on their symptoms. Patients treated nonoperatively were excluded from this cohort. Additionally, this was a sample of convenience; therefore, a power analysis was not performed. Variables not associated with advanced hammertoe such as absolute first or second metatarsal length were at risk of having a type II error. Because pronation data were only available for 27 patients, this subanalysis was at particular risk of having inadequate statistical power.
In conclusion, this study used weightbearing CT scans, which do not require calibration, in order to determine radiographic and demographic risk factors associated with the development of significant hammertoe deformities in patients planning to undergo surgical management of their hallux valgus. In hallux valgus patients indicated for surgical intervention, an increased IMA, apex plantar Meary angle (flatter medial longitudinal arch), older age, and higher BMI were observed to be associated with having hammertoe deformities requiring more than a simple MTPJ capsular release. These results may help clinicians counsel hallux valgus patients about the risk of developing an advanced hammertoe deformity.
Supplemental Material
Supplemental Material, FAO909088-ICMJE for Relationship Between Demographic and Radiographic Characteristics and Second Ray Pathology in Hallux Valgus Patients by Samantha Cronin, Matthew Conti, Nicholas Williams and Scott J. Ellis in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Samantha Cronin, BA,  https://orcid.org/0000-0002-7406-4870
https://orcid.org/0000-0002-7406-4870
Matthew Conti, MD,  https://orcid.org/0000-0003-3313-2520
https://orcid.org/0000-0003-3313-2520
Scott J. Ellis, MD,  https://orcid.org/0000-0002-4304-7445
https://orcid.org/0000-0002-4304-7445
References
- 1. Campbell B, Miller MC, Williams L, Conti SF. Pilot study of a 3-dimensional method for analysis of pronation of the first metatarsal of hallux valgus patients. Foot Ankle Int. 2018;39(12):1449–1456. [DOI] [PubMed] [Google Scholar]
- 2. Collan L, Kankare JA, Mattila K. The biomechanics of the first metatarsal bone in hallux valgus: a preliminary study utilizing a weight bearing extremity CT. Foot Ankle Surg. 2013;19(3):155–161. [DOI] [PubMed] [Google Scholar]
- 3. Coughlin MJ. Instructional course lectures, The American Academy of Orthopaedic Surgeons—hallux valgus. J Bone Joint Surg. 1996;78(6):932–966. [PubMed] [Google Scholar]
- 4. Coughlin MJ, Dorris J, Polk E. Operative repair of the fixed hammertoe deformity. Foot Ankle Int. 2000;21(2):94–104. [DOI] [PubMed] [Google Scholar]
- 5. Cracchiolo A, Kitaoka HB, Leventen EO. Silicone implant arthroplasty for second metatarsophalangeal joint disorders with and without hallux valgus deformities. Foot Ankle. 1988;9(1):10–18. [DOI] [PubMed] [Google Scholar]
- 6. Dinoá V, von Ranke F, Costa F, Marchiori E. Evaluation of lesser metatarsophalangeal joint plantar plate tears with contrast-enhanced and fat-suppressed MRI. Skeletal Radiol. 2016;45(5):635–644. [DOI] [PubMed] [Google Scholar]
- 7. Dufour AB, Losina E, Menz HB, LaValley MP, Hannan MT. Obesity, foot pain and foot disorders in older men and women. Obes Res Clin Pract. 2017;11(4):445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Giannoudis PV, Xypnitos FN. Hallux valgus correction. In: Giannoudis P, ed. Procedures in Elective Orthopaedic Surgery. London: Springer; 2011:293–302. [Google Scholar]
- 9. Gines-Cespedosa A, Alentorn-Geli E, Sanchez JF, et al. Influence of common associated forefoot disorders on preoperative quality of life in patients with hallux valgus. Foot Ankle Int. 2013;34(12):1634–1637. [DOI] [PubMed] [Google Scholar]
- 10. Glasoe WM. Treatment of progressive first metatarsophalangeal hallux valgus deformity: a biomechanically based muscle-strengthening approach. J Orthop Sports Phys Ther. 2016;46(7):596–605. [DOI] [PubMed] [Google Scholar]
- 11. Golightly YM, Hannan MT, Dufour AB, Renner JB, Jordan JM. Factors associated with hallux valgus in a community-based cross-sectional study of adults with and without osteoarthritis. Arthritis Care Res. 2015;67(6):791–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gould N. Graphing the adult foot and ankle. Foot Ankle. 1982;2(4):213–219. [DOI] [PubMed] [Google Scholar]
- 13. Gribbin CK, Ellis SJ, Nguyen J, Williamson E, Cody EA. Relationship of radiographic and clinical parameters with hallux valgus and second ray pathology. Foot Ankle Int. 2017;38(1):14–19. [DOI] [PubMed] [Google Scholar]
- 14. Hannan MT, Menz HB, Jordan JM, Cupples LA, Cheng CH, Hsu YH. High heritability of hallux valgus and lesser toe deformities in adult men and women. Arthritis Care Res. 2013;65(9):1515–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hecht PJ, Lin TJ. Hallux valgus. Med Clin North Am. 2014;98(2):227–232. [DOI] [PubMed] [Google Scholar]
- 16. Henry L, Wickham H. Purrr: functional programming tools. R Package version 032. https://cran.r-project.org/web/packages/purrr/index.html. Published 2019.
- 17. Kaz AJ, Coughlin MJ. Crossover second toe: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007;28(12):1223–1237. [DOI] [PubMed] [Google Scholar]
- 18. Kido M, Ikoma K, Imai K, Tokunaga D, Inoue N, Kubo T. Load response of the medial longitudinal arch in patients with flatfoot deformity: in vivo 3D study. Clin Biomech. 2013;28(5):568–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kokubo T, Hashimoto T, Suda Y, Waseda A, Ikezawa H. Radiographic shape of foot with second metatarsophalangeal joint dislocation associated with hallux valgus. Foot Ankle Int. 2017;38(12):1374–1379. [DOI] [PubMed] [Google Scholar]
- 20. Koller U, Willegger M, Windhager R, Wanivenhaus A, Trnka HJ, Schuh R. Plantar pressure characteristics in hallux valgus feet. J Orthop Res. 2014;32(12):1688–1693. [DOI] [PubMed] [Google Scholar]
- 21. Kramer WC, Parman M, Marks RM. Hammertoe correction with K-wire fixation. Foot Ankle Int. 2015;36(5):494–502. [DOI] [PubMed] [Google Scholar]
- 22. Lee KM, Ahn S, Chung CY, Sung KH, Park MS. Reliability and relationship of radiographic measurements in hallux valgus foot and ankle. Clin Orthop Relat Res. 2012;470(9):2613–2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lintz FCesar Netto C, de, Barg A, Burssens A, Richter M; Weight Bearing CT International Study Group. Weight-bearing cone beam CT scans in the foot and ankle. EFORT Open Rev. 2018;395):278–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Munuera PV, Polo J, Rebollo J. Length of the first metatarsal and hallux in hallux valgus in the initial stage. Int Orthop. 2008;32(4):489–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nery C, Baumfeld D, Umans H, Yamada AF. MR imaging of the plantar plate. Magn Reson Imaging Clin N Am. 2017;25(1):127–144. [DOI] [PubMed] [Google Scholar]
- 26. Nishimura A, Ito N, Nakazora S, Kato K, Ogura T, Sudo A. Does hallux valgus impair physical function? BMC Musculoskelet Disord. 2018;19(1):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Okuda H, Juman S, Ueda A, Miki T, Shima M. Factors related to prevalence of hallux valgus in female university students: a cross-sectional study. J Epidemiol. 2014;24(3):200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Park CH, Chun Lee W, Rae Kim J, Whan Lim S. Characteristics of severe hallux valgus deformity with moderate intermetatarsal angle. J Korean Foot Ankle Soc. 2014;18(4):173–177. [Google Scholar]
- 30. Ray JJ, Freidmann AJ, Hanselman AE, et al. Hallux valgus. Foot Ankle Orthop. 2019;4(2):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Richter M, Seidl B, Zech S, Hahn S. PedCAT for 3D-imaging in standing position allows for more accurate bone position (angle) measurement than radiographs or CT. Foot Ankle Surg. 2014;20(3):201–207. [DOI] [PubMed] [Google Scholar]
- 32. Roan LY, Tanaka Y, Taniguchi A, Tomiwa K, Kumai T, Cheng YM. Why do lesser toes deviate laterally in hallux valgus? A radiographic study. Foot Ankle Int . 2015;36(6):664–672. [DOI] [PubMed] [Google Scholar]
- 33. Robinson D, Hayes A. broom: Convert statistical analysis objects into tidy tibbles. R Package version 052. https://cran.r-project.org/package=broom%0A. Published 2019.
- 34. Schuberth JM. Hammer toe syndrome. J Foot Ankle Surg. 1999;38(2):166–178. [PubMed] [Google Scholar]
- 35. Thordarson D, Ebramzadeh E, Moorthy M, Lee J, Rudicel S. Correlation of hallux valgus surgical outcome with AOFAS forefoot score and radiological parameters. Foot Ankle Int. 2005;26(2):122–127. [DOI] [PubMed] [Google Scholar]
- 36. Usuelli FG, Di Silvestri CA, D’Ambrosi R, Maccario C, Tan EW. Return to sport activities after medial displacement calcaneal osteotomy and flexor digitorum longus transfer. Knee Surg Sport Traumatol Arthrosc. 2018;26(3):892–896. [DOI] [PubMed] [Google Scholar]
- 37. Wickham H, Francois R, Henry L, Müller K. ‘dplyr’. A grammar of data manipulation. R Package version 083. https://cran.r-project.org/package=dplyr%0A . Published 2019.
- 38. Young KW, Lee HS, Park KC. Outcome of second-ray pathologies following Weil osteotomy in patients treated for hallux valgus. Foot Ankle Spec. 2019;12(5):452–457. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO909088-ICMJE for Relationship Between Demographic and Radiographic Characteristics and Second Ray Pathology in Hallux Valgus Patients by Samantha Cronin, Matthew Conti, Nicholas Williams and Scott J. Ellis in Foot & Ankle Orthopaedics