Abstract
Background:
Treatment of ankle fractures in patients with diabetes is associated with increased complication rates. Ankle arthrodesis is considered a salvage procedure after failed ankle fracture fixation, yet primary ankle arthrodesis has been proposed as a treatment option for patients with significant diabetes-related complications. To date, the characteristics of patients who undergo primary ankle arthrodesis and the associated outcomes have not been described.
Methods:
A retrospective review was performed of 13 patients with diabetes who underwent primary arthrodesis for traumatic ankle fracture. Patient demographics were characterized in addition to their diabetes complications, Adelaide Fracture in the Diabetic Ankle (AFDA) score, and fracture type. Outcomes assessed included reoperation rates, infection rates, wound complications, nonunion/malunion, amputation, and development of Charcot arthropathy postoperatively.
Results:
Patients who underwent primary arthrodesis had high rates of diabetes complications, average AFDA scores of 6.4, and high rates of severe injuries, including 38.5% open fractures and 69.2% fracture dislocations. The overall complication rate for primary arthrodesis of ankle fractures in diabetes patients was more than 75% in this cohort. Complications included a 38.5% reoperation rate, 38.5% infection rate, 53.8% wound complication rate, and 23.1% amputation rate. Despite a high nonunion rate at the attempted fusion sites, 89.9% of fractures healed and patients had a stable extremity.
Conclusion:
This review is the first to characterize the epidemiology and complications of diabetes patients undergoing primary ankle arthrodesis for ankle fractures. In this cohort, patients with multiple diabetic complications and severe injuries underwent primary arthrodesis, which led to an overall high complication rate. Further research is needed to determine the appropriate treatment option for these high-risk patients, and tibiotalocalcaneal stabilization without arthrodesis may be beneficial.
Level of Evidence:
Level IV, retrospective case series.
Keywords: diabetes, trauma, ankle fracture, ankle arthrodesis
Introduction
Managing ankle fractures in patients with diabetes presents a significant challenge for both the patient and treating surgeon. Diabetes is a well-known risk factor for complications following ankle fracture fixation. 26 Diabetes patients who sustain ankle fractures that require operative fixation have a complication rate of approximately 40%, nearly 3-fold higher than patients without diabetes. 4 These complications include wound breakdown, deep infection, nonunion, hardware failure, and Charcot arthropathy, which often requires repeat operations and can lead to amputation. 31 Accordingly, diabetes patients have extended hospitalizations, and the cost of treating ankle fractures in diabetes patients is approximately $2000-$7000, depending on the number of comorbidities, which is higher than in patients without diabetes. 12,24 In previous studies, peripheral neuropathy and peripheral vascular disease appear to be the most significant risk factors for complications. 8 The current incidence of ankle fractures is approximately 179 fractures annually per 100,000 persons, 18 and the prevalence of diabetes in the United States is approximately 9.4%, affecting 23 million people. 5 The incidence of diabetes and ankle fractures also appears to be increasing across the population; thus, determining an appropriate treatment protocol to limit complications and repeat procedures for this difficult problem is important. 19,22
Current recommendations for operative treatment of ankle fractures in patients with diabetes consist of increased rigid fixation and prolonged periods of non–weight bearing. 7 Described techniques include multiple quadricortical syndesmotic screws, 10,25 stiffer plates, 23 and fixation augmentation with transarticular Steinmann pins 16 or intramedullary fibular Kirschner wires. 20 Recently, Yee et al 32 described a treatment algorithm for ankle fractures in diabetes patients based on the extent of their diabetic complications, Adelaide Fracture in the Diabetic Ankle (AFDA) score, and suggest that primary ankle arthrodesis may be an option in severe situations. One potential limitation to the outlined algorithm is failure to include fracture characteristics/classification, that is, open/closed, isolated lateral malleolar, bimalleolar, trimalleolar, or fracture/dislocations that would have varying degrees of soft tissue damage, instability, and associated complications. 6,11,15
Ankle arthrodesis has been primarily described as a salvage procedure for Charcot arthropathy or failed fracture fixation. 3,9,17,28 Described methods for ankle arthrodesis include tibiotalocalcaneal (TTC) hindfoot nails, ringed external fixators, and tibiotalar arthrodesis with crossed screws or plating. Although primary arthrodesis has been described for the management of severe pilon fractures, 1,14 there is a paucity of literature describing its role in acute diabetic ankle fractures without concomitant Charcot arthropathy. Here, we present a case series of 13 diabetic ankle fractures that underwent primary arthrodesis following an ankle fracture with a focus on patient and injury characteristics and operative outcomes/complications. The goal was to characterize patient profiles to begin to understand if acute fusion/rigid stabilization limits the serious and often catastrophic complications of diabetic ankle fractures.
Methods
A retrospective analysis was performed of patients with diabetes and surgically treated ankle fractures at a level 1 trauma center from January 1, 2010, to December 31, 2018. This study was approved by the institutional review board. Data were gathered from the Healthcare Enterprise Repository for Ontological Narration (Heron) research data repository. 29 Inclusion criteria consisted of patients >18 years of age, a diagnosis of diabetes, and an operatively managed ankle fracture with hindfoot arthrodesis/stabilization. Patients indicated for primary arthrodesis were deemed poor candidates for traditional fixation methods based on their degree of injury and comorbidities by the treating surgeon. However, there was no formal protocol or method for determining which patients would undergo primary arthrodesis. Exclusion criteria included prior ipsilateral ankle fracture fixation, concurrent ipsilateral hindfoot fractures, pilon fractures, arthrodesis performed as a salvage procedure, or for Charcot arthropathy.
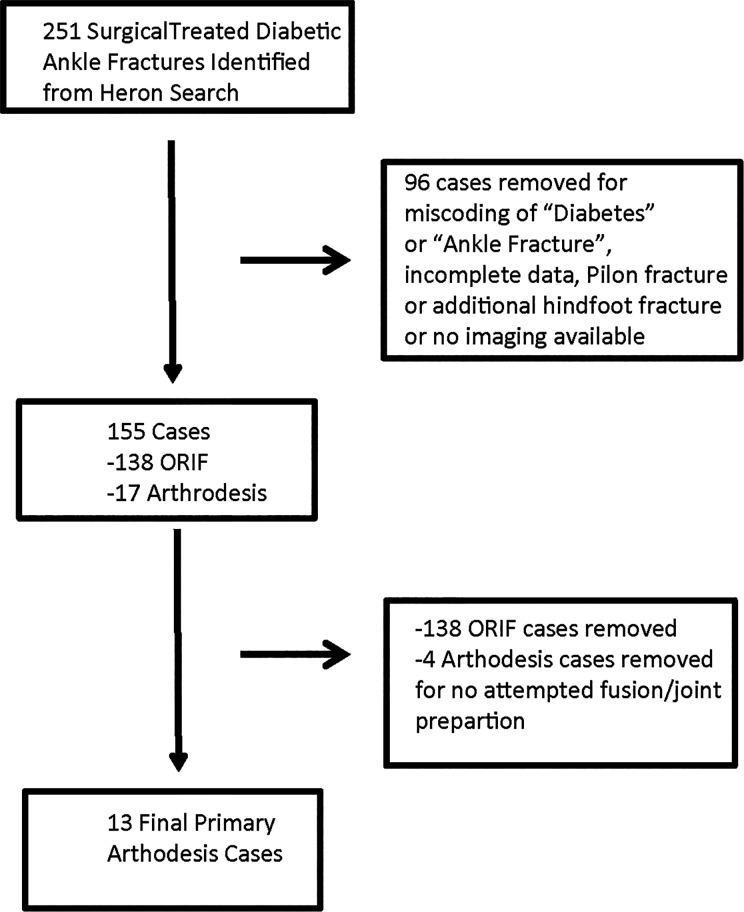
Two hundred fifty-one cases (249 patients) were reviewed and 13 were included in the final analysis (Figure 1). Demographic variables including age, sex, body mass index, smoking status, and American Society of Anesthesiologists (ASA) classification were gathered. Diabetes characteristics including insulin dependence, complications (neuropathy, nephropathy, retinopathy, peripheral neuropathy, peripheral vascular disease), and glycated hemoglobin (HbA1c) were also recorded. AFDA scores were also calculated as previously described 32 (Table 1); however, “years of diabetes” and “patient compliance” were not reliably recorded and of limited benefit. Fractures were classified by laterality, mechanism of injury, open vs closed, and pattern (lateral malleolar, medial malleolar, bimalleolar, trimalleolar, or fracture dislocation) based on radiographic review. Complication rates including reoperation, infection, wound complications, malunion, nonunion, amputation, and postoperative Charcot arthropathy were all documented.
Figure 1.
Study flowchart. Heron search was performed for ICD9/ICD10 codes of “diabetes” and “ankle fracture” with CPT codes of “ORIF” and “arthrodesis.” Chart and imaging review excluded 96 cases based on timing of diabetes and ankle fracture, miscoding of diabetes (ie, family history, or gestational diabetes, etc), miscoding of ankle fracture (ie, Charcot neuropathy, hindfoot fracture, etc), pilon fractures, associated hindfoot/midfoot fractures, or incomplete data/imaging. ORIF cases were removed (138) and an additional 4 arthrodesis case were removed as there was no attempted fusion. CPT, Combined Procedural Terminology; ICD9, International Classification of Diseases, Ninth Revision; ICD10, International Classification of Diseases, Tenth Revision; ORIF, open reduction internal fixation.
Table 1.
Adelaide Fracture in the Diabetic Ankle (AFDA) Scoring System.a
| Two Points Each | One Point Each |
|---|---|
| (i) Peripheral neuropathy/loss of protective sensation | (i) Diabetic history of greater than 20 years |
| (ii) Presence of vasculopathy | (ii) Presence of diabetic nephropathy or retinopathy |
| (iii) Insulin dependence with poor compliance | (iii) Obesity |
| (iv) Previous or coinciding history of Charcot's arthropathy in any joint | (iv) Poor patient compliance |
aAFDA scoring system reprinted from Yee et. al. 32
Thirteen patients were identified with ankle fractures that were treated with primary arthrodesis following acute ankle fracture and a focused review of these cases was performed. Categorical variables were summarized as a percentage and continuous variables are presented as mean ± SD.
Results
Case Series of Primary Arthrodesis
Patient characteristics
Overall, there were 13 diabetes patients who underwent primary arthrodesis for acute ankle fracture in our cohort. Demographic data are listed in Table 2. The average follow-up was 297 days, average age of patients was 67.1 years, and 46% of patients were male. Average body mass index was 35.8, 23.07% of patients were smokers, and the average American Society of Anesthesiologists (ASA) score was 3.1. One of the indications for the treating surgeons to pursue primary arthrodesis was multiple diabetic complications. As such, this population demonstrated high levels of end organ damage from diabetes, including 69% nephropathy, 46% retinopathy, 82% neuropathy, 62% peripheral vascular disease, and 15% prior Charcot arthropathy in a contralateral joint. Twelve of the 13 patients had type 2 diabetes and 77% were insulin dependent. Patients averaged 2.8 diabetic complications and AFDA scores of 6.4, which is above the stated threshold of 5 as suggested by Yee et al 32 to consider primary arthrodesis. However, 3 patients were below 5 with scores of 0, 2, and 3. Two of these patients were frail and elderly and 1 had pre-existing tibiotalar arthritis.
Table 2.
Patient Characteristics.
| Number of cases | 13 |
| Follow-up length, d, mean (SD) | 296.8 (358.3) |
| Age, y, mean (SD) | 67.1 (5.3) |
| Sex, % male | 46.2 |
| HbA1c, mean (SD) | 7.5 (1.6) |
| ASA, mean (SD) | 3.1 (0.3) |
| BMI, mean (SD) | 35.8 (6.5) |
| Smoking, % | 23.1 |
| Insulin dependence, % | 76.9 |
| Nephropathy, % | 69.2 |
| Retinopathy, % | 46.2 |
| Neuropathy, % | 81.8 |
| PVD, % | 61.5 |
| Charcot arthropathy, % | 15.4 |
| No. of diabetic complications, mean (SD) | 2.8 (1.5) |
| AFDA score, mean (SD) | 6.4 (2.9) |
Abbreviations: AFDA, Adelaide Fracture in the Diabetic Ankle; ASA, American Society of Anesthesiologists; BMI, body mass index; HbA1c, glycated hemoglobin; PVD, peripheral vascular disease
Injury characteristics
Patients indicated for primary arthrodesis in this cohort had more severe injuries as shown in Table 3. Nearly 70% of the injuries were fracture dislocations, and just less than 40% of injuries were open. These results are expected, as one of the current indications for primary arthrodesis at our institution is severity of injury in the setting of multiple diabetic complications. Falls from standing height accounted for all injuries in this study.
Table 3.
Fracture Characteristics.
| Percentage | |
|---|---|
| Medial malleolus | 0.0 |
| Lateral malleolus | 0.0 |
| Bimalleolar | 7.7 |
| Trimalleolar | 23.1 |
| Fracture/dislocation | 69.2 |
| Open fracture | 38.5 |
Operative treatment
All patients underwent TTC fusion with a hindfoot nail, except for 1 that was an isolated tibiotalar fusion with a cannulated screw construct. The subtalar joint was only formally prepared in 54% of cases, whereas the tibiotalar joint was prepared in all cases. Two approaches were primarily used, transfibular 54% of the time and an anteromedial approach through the open wound 40% of the time; 1 medial approach with medial malleolar osteotomy was performed. Five patients were initially managed with external fixators; all patients with open injuries had formal irrigation and debridement and all but 2 patients had definitive fixation placed at that time. Radiographs demonstrating a patient managed with TTC primary arthrodesis are shown in Figure 2.
Figure 2.

Primary arthrodesis for ankle fracture in diabetic patient. (A) Injury radiographs with left ankle fracture/dislocation. (B) 1-month postoperative primary tibiotalocalcaneal arthrodesis with hindfoot nail. (C) 8 month postoperation.
Postoperative complications
There was an overall high complication rate in our cohort (Table 4), and approximately 77% of patients experienced at least 1 complication; however, it is recognized that this is a high-risk population secondary to the patients selected for attempted primary arthrodesis. Five patients required repeat operation (38%), all for infection. The initial reoperation occurred approximately 1 month after the initial surgery, and there was an average of 2.6 repeat procedures in patients who required reoperation. Three patients required below-the-knee amputation, all for uncontrollable deep infection and all had initially been managed with an external fixator. Wound complications were common and occurred in 53% of patients. Charcot arthropathy was seen in 1 patient postoperatively. One patient died in the acute postoperative period after cardiac arrest.
Table 4.
Postoperative Complications.
| Percentage | |
|---|---|
| Overall complication | 76.9 |
| Reoperation | 38.5 |
| Infection | 38.5 |
| Wound complication | 53.8 |
| Hardware failure | 30.8 |
| Arthrodesis nonunion | 77.8 |
| Fracture nonunion | 11.1 |
| Malunion | 0.0 |
| Amputation | 23.1 |
| Charcot arthropathy | 7.7 |
Only 2 patients had complete consolidation of both the tibiotalar and subtalar joints in this study, but all nonunions were asymptomatic, and for the 10 fractures that did not lead to amputation, all except for 1 healed (89% union rate) despite nonunion at the proposed arthrodesis site. Of note, patients with less than 3 months’ follow-up or those who underwent amputation prior to 3 months (n = 4) were not included in the analysis of union rates. Of the arthrodesis nonunions, 4 were isolated subtalar nonunions (only 1 joint had been formally prepared) and 3 were combined tibiotalar and subtalar nonunions (1 of which did not have the subtalar joint formally prepared).
Discussion
The operative treatment and postoperative management of acute ankle fractures in the diabetes patient population is a difficult problem given the high rate of complications and need for reoperations. 26 Several strategies exist to help minimize fixation failure and stability including syndesmotic ladders, increased rigid fixation, and prolonged time to weight bearing. However, these strategies have not completely solved the dilemma on how to adequately and optimally treat patients with what can be a devastating and limb-threatening injury. Recently, it has been suggested that acute primary arthrodesis in patients with poorly controlled diabetes could be considered 32 and that early arthrodesis of diabetes patients who develop Charcot arthropathy after ankle fractures can produce satisfactory results. 30 To date, there has been relatively little data regarding demographics and complication rates in diabetes patients who undergo primary arthrodesis for acute ankle fractures. This is the first case series to analyze this patient population. This study demonstrates an overall high complication rate for diabetes patients undergoing primary arthrodesis for unstable ankle fractures, and that more research is needed.
Our results demonstrate that patients who underwent primary arthrodesis had high rates of diabetic complications and more severe injuries. Overall, primary arthrodesis had high rates of postoperative complications. The treatment of ankle fractures in patients with poorly controlled diabetes remains a difficult problem, and patients should be counseled appropriately on the significant rate of serious complications associated with operative management.
Patient selection could be a major factor contributing to the high complication rate in this study. At our institution, patients selected for primary arthrodesis were deemed poor candidates for traditional fixation methods based on their degree of injury and comorbidities. However, there is no official protocol to determine the best stabilization method for each patient. This represents selection bias for a high-risk patient population. This is a crucial area for further research to identify the most appropriate fixation method for the right patient in this at-risk population.
AFDA scoring was previously described to help guide operative decision making 32 and remains the only description of primary arthrodesis for diabetic ankle fractures in the literature. AFDA scores ≥5 were suggested as a cut-off to consider primary arthrodesis. The average AFDA score in this study was 6.4. The AFDA score gives a summary of the patients’ overall level of diabetic complications but does not account for severity of injury and fracture characteristics. Adding fracture/injury characteristics to the AFDA score is a potential modification that could improve the application of the treatment algorithm; furthermore, future studies could stratify these scores into a risk calculator that could potentially be used to educate patients on the risk of complications and outcomes.
The overall high complication rate associated with primary arthrodesis in our study suggests that attempting fusion in patients with ankle fractures and multiple diabetic complications should be done on a limited basis. Principles of diabetic ankle fracture fixation include “super constructs” with increased mechanical properties and strength, carefully planned incisions with limited soft tissue dissection, and fixation beyond the zone of injury. 21 One potential fixation option that could apply all aspects of these principles and build from the results of this study is the use of TTC hindfoot nails as an “internal fixator” without attempted fusion. This has been described for elderly patients with fragility ankle fractures, and recent results from both retrospective studies 2,27 and prospective randomized controlled trials 13 show promising results. Our data support this stabilization method; most fractures healed and patients had a stable extremity, despite a high rate of nonunion at the arthrodesis site.
The strengths of this study are that this is the first case series reported for diabetes patients undergoing primary arthrodesis of acute ankle fracture and the descriptive characteristics and associated complications. Weaknesses included the small sample size of patients who were treated with primary arthrodesis. Second, this was a retrospective review, and multiple variables were dependent on appropriate documentation by medical providers in the chart, and clinical/functional outcomes were unable to be assessed. Another weakness is that 3 different orthopedic surgeons were involved in the management of patients throughout the study time frame. Each surgeon has his own operative technique, training, soft tissue management, and bias in treatment strategies that may have affected treatment decisions, operative outcomes, and complications.
In conclusion, this study provides an important addition to the literature on primary arthrodesis for the management of ankle fracture in diabetes patients. Although primary arthrodesis may be considered, the optimal patient and injury type is not clearly defined, and further research is needed. Certainly, more research is needed on this topic, and a prospective randomized trial in diabetes patients with unstable ankle fractures would be an important next step in evaluating the optimal treatment strategy for this difficult problem.
Supplemental Material
Supplemental Material, FAO908841-ICMJE for Primary Arthrodesis for Diabetic Ankle Fractures by Caleb W. Grote, William Tucker, Kelly Stumpff, Mitchell C. Birt and Greg A. Horton in Foot & Ankle Orthopaedics
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Caleb W. Grote, MD, PhD,  https://orcid.org/0000-0002-9071-7202
https://orcid.org/0000-0002-9071-7202
William Tucker, MD,  https://orcid.org/0000-0001-6774-909X
https://orcid.org/0000-0001-6774-909X
References
- 1. Al-Ashhab ME. Primary ankle arthrodesis for severely comminuted tibial pilon fractures. Orthopedics. 2017;40(2):e378–e381. [DOI] [PubMed] [Google Scholar]
- 2. Al-Nammari SS, Dawson-Bowling S, Amin A, Nielsen D. Fragility fractures of the ankle in the frail elderly patient: treatment with a long calcaneotalotibial nail. Bone Joint J. 2014;96-B(6):817–822. [DOI] [PubMed] [Google Scholar]
- 3. Ayoub MA. Ankle fractures in diabetic neuropathic arthropathy: can tibiotalar arthrodesis salvage the limb? J Bone Joint Surg Br. 2008;90(7):906–914. [DOI] [PubMed] [Google Scholar]
- 4. Blotter RH, Connolly E, Wasan A, Chapman MW. Acute complications in the operative treatment of isolated ankle fractures in patients with diabetes mellitus. Foot Ankle Int. 1999;20(11):687–694. [DOI] [PubMed] [Google Scholar]
- 5. Bullard KM, Cowie CC, Lessem SE, et al. Prevalence of diagnosed diabetes in adults by diabetes type—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):359–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carragee EJ, Csongradi JJ, Bleck EE. Early complications in the operative treatment of ankle fractures. Influence of delay before operation. J Bone Joint Surg Br. 1991;73(1):79–82. [DOI] [PubMed] [Google Scholar]
- 7. Chaudhary SB, Liporace FA, Gandhi A, et al. Complications of ankle fracture in patients with diabetes. J Am Acad Orthop Surg. 2008;16(3):159–170. [DOI] [PubMed] [Google Scholar]
- 8. Costigan W, Thordarson DB, Debnath UK. Operative management of ankle fractures in patients with diabetes mellitus. Foot Ankle Int. 2007;28(1):32–37. [DOI] [PubMed] [Google Scholar]
- 9. Dalla Paola L, Volpe A, Varotto D, et al. Use of a retrograde nail for ankle arthrodesis in Charcot neuroarthropathy: a limb salvage procedure. Foot Ankle Int. 2007;28(9):967–970. [DOI] [PubMed] [Google Scholar]
- 10. Dunn WR, Easley ME, Parks BG, et al. An augmented fixation method for distal fibular fractures in elderly patients: a biomechanical evaluation. Foot Ankle Int. 2004;25(3):128–131. [DOI] [PubMed] [Google Scholar]
- 11. Ebraheim NA, Mekhail AO, Gargasz SS. Ankle fractures involving the fibula proximal to the distal tibiofibular syndesmosis. Foot Ankle Int. 1997;18(8):513–521. [DOI] [PubMed] [Google Scholar]
- 12. Ganesh SP, Pietrobon R, Cecilio WA, et al. The impact of diabetes on patient outcomes after ankle fracture. J Bone Joint Surg Am. 2005;87(8):1712–1718. [DOI] [PubMed] [Google Scholar]
- 13. Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: open reduction and internal fixation versus tibio-talo-calcaneal nailing: short-term results of a prospective randomized-controlled study. Injury. 2017;48(2):519–524. [DOI] [PubMed] [Google Scholar]
- 14. Ho B, Ketz J. Primary arthrodesis for tibial pilon fractures. Foot Ankle Clin. 2017;22(1):147–161. [DOI] [PubMed] [Google Scholar]
- 15. Hoiness P, Stromsoe K. Early complications of surgically managed ankle fractures related to the AO classification. A review of 118 ankle fractures treated with open reduction and internal fixation. Arch Orthop Trauma Surg. 1999;119(5-6):276–279. [DOI] [PubMed] [Google Scholar]
- 16. Jani MM, Ricci WM, Borrelli J, Jr, et al. A protocol for treatment of unstable ankle fractures using transarticular fixation in patients with diabetes mellitus and loss of protective sensibility. Foot Ankle Int. 2003;24(11):838–844. [DOI] [PubMed] [Google Scholar]
- 17. Johnson AR, Yoon P. Limb salvage in an unstable ankle fracture of a diabetic patient with Charcot arthropathy. Foot Ankle Spec. 2010;3(4):184–189. [DOI] [PubMed] [Google Scholar]
- 18. Juto H, Nilsson H, Morberg P. Epidemiology of adult ankle fractures: 1756 cases identified in Norrbotten County during 2009-2013 and classified according to AO/OTA. BMC Musculoskelet Disord. 2018;19(1):441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kannus P, Palvanen M, Niemi S, et al. Increasing number and incidence of low-trauma ankle fractures in elderly people: Finnish statistics during 1970-2000 and projections for the future. Bone. 2002;31(3):430–433. [DOI] [PubMed] [Google Scholar]
- 20. Koval KJ, Petraco DM, Kummer FJ, Bharam S. A new technique for complex fibula fracture fixation in the elderly: a clinical and biomechanical evaluation. J Orthop Trauma. 1997;11(1):28–33. [DOI] [PubMed] [Google Scholar]
- 21. Manway JM, Blazek CD, Burns PR. Special considerations in the management of diabetic ankle fractures. Curr Rev Musculoskelet Med. 2018;11(3):445–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79. [DOI] [PubMed] [Google Scholar]
- 23. Perry MD, Taranow WS, Manoli A, 2nd, Carr JB. Salvage of failed neuropathic ankle fractures: use of large-fragment fibular plating and multiple syndesmotic screws. J Surg Orthop Adv. 2005;14(2):85–91. [PubMed] [Google Scholar]
- 24. Regan DK, Manoli A, 3rd, Hutzler L, et al. Impact of diabetes mellitus on surgical quality measures after ankle fracture surgery: implications for “value-based” compensation and “pay for performance.” J Orthop Trauma. 2015;29(12):e483–486. [DOI] [PubMed] [Google Scholar]
- 25. Schon LC, Marks RM. The management of neuroarthropathic fracture-dislocations in the diabetic patient. Orthop Clin North Am. 1995;26(2):375–392. [PubMed] [Google Scholar]
- 26. SooHoo NF, Krenek L, Eagan MJ, et al. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am. 2009;91(5):1042–1049. [DOI] [PubMed] [Google Scholar]
- 27. Taylor BC, Hansen DC, Harrison R, et al. Primary retrograde tibiotalocalcaneal nailing for fragility ankle fractures. Iowa Orthop J. 2016;36:75–78. [PMC free article] [PubMed] [Google Scholar]
- 28. Vaudreuil NJ, Fourman MS, Wukich DK. Limb salvage after failed initial operative management of bimalleolar ankle fractures in diabetic neuropathy. Foot Ankle Int. 2017;38(3):248–254. [DOI] [PubMed] [Google Scholar]
- 29. Waitman LR, Warren JJ, Manos EL, Connolly DW. Expressing observations from electronic medical record flowsheets in an i2b2 based clinical data repository to support research and quality improvement. AMIA Annu Symp Proc. 2011;2011:1454–1463. [PMC free article] [PubMed] [Google Scholar]
- 30. Wallace SJ, Liskutin TE, Schiff AP, Pinzur MS. Ankle fusion following failed initial treatment of complex ankle fractures in neuropathic diabetics. Foot Ankle Surg. 2020;26(2):189–192. [DOI] [PubMed] [Google Scholar]
- 31. Wukich DK, Kline AJ. The management of ankle fractures in patients with diabetes. J Bone Joint Surg Am. 2008;90(7):1570–1578. [DOI] [PubMed] [Google Scholar]
- 32. Yee J, Pillai A, Ferris L. Diabetic ankle fractures: a review of the literature and an introduction to the Adelaide fracture in the diabetic ankle algorithm and score. Biomed Res Int. 2014;2014:153146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO908841-ICMJE for Primary Arthrodesis for Diabetic Ankle Fractures by Caleb W. Grote, William Tucker, Kelly Stumpff, Mitchell C. Birt and Greg A. Horton in Foot & Ankle Orthopaedics