Abstract
Despite a growing body of literature focused on racial/ethnic disparities in Covid-19 mortality, few previous studies have examined the pandemic's impact on 2020 cause-specific mortality by race and ethnicity. This paper documents changes in mortality by underlying cause of death and race/ethnicity between 2019 and 2020. Using age-standardized death rates, we attribute changes for Black, Hispanic, and White populations to various underlying causes of death and show how these racial and ethnic patterns vary by age and sex. We find that although Covid-19 death rates in 2020 were highest in the Hispanic community, Black individuals faced the largest increase in all-cause mortality between 2019 and 2020. Exceptionally large increases in mortality from heart disease, diabetes, and external causes of death accounted for the adverse trend in all-cause mortality within the Black population. Within Black and White populations, percentage increases in all-cause mortality were similar for men and women, as well as for ages 25–64 and 65+. Among the Hispanic population, however, percentage increases in mortality were greatest for working-aged men. These findings reveal that the overall impact of the pandemic on racial/ethnic disparities in mortality was much larger than that captured by official Covid-19 death counts alone.
Keywords: Covid-19, Mortality, Race/ethnicity, Public health, Inequality
1. Introduction
The onset of the Covid-19 pandemic in 2020 led to a sharp rise in mortality in the United States, with Black and Hispanic communities absorbing a disproportionate share of the impact (Alsan et al., 2021; Andrasfay & Goldman, 2021; Woolf, Chapman, et al., 2021). Recent research suggests that the 2020 life expectancy drop eliminated much of the progress made in the past decade in narrowing the Black-White life expectancy gap and nearly erased the Hispanic life expectancy advantage (Andrasfay & Goldman, 2021; Woolf, Chapman, et al., 2021).
These emerging disparities highlight underlying systems of structural racism in the United States that have long shaped unequitable treatment and access to health care among marginalized racial/ethnic groups (Bailey et al., 2021; McClure et al., 2020). Previous research has recognized racism as a fundamental cause of health disparities, which works to constrain access to health-promoting resources and opportunities, unequally distribute health-related risks and exposures, and drive weathering processes that impose a greater health burden on racialized groups (Garcia et al., 2021; Geronimus, 1992; Phelan & Link, 2015). The racialized impact of the pandemic has increasingly drawn public and scholarly attention to these structural inequities which place Black and Hispanic populations at a higher risk of Covid-19 infection and mortality. These factors include disproportionate representation in frontline jobs with minimal workplace protections, denser living conditions, a higher prevalence of comorbid conditions, and unequal access to adequate health care (Lopez et al., 2021; Macias Gil et al., 2020; Woolf, Chapman, et al., 2021).
Although the disparities in Covid-19 deaths are well-documented, studies that only consider deaths directly attributable to Covid-19 may obscure the overall magnitude of racial/ethnic disparities in the impact of Covid-19 on mortality for several reasons. First, Covid-19 death counts do not capture the indirect impact of the pandemic on mortality, driven by increased economic and housing hardship, worsened mental health, and reductions in healthcare access (Anderson et al., 2021; Cantor et al., 2020; Stokes, Lundberg, Bor, Elo, et al., 2021). Second, official Covid-19 death counts fail to capture Covid-19 deaths that were misclassified to other causes of death. Such deaths inappropriately ascribed to other causes may be especially prevalent among racial/ethnic groups who have historically received less adequate medical attention (Wrigley-Field et al., 2020).
We build on previous work that has attempted to capture the total mortality impact of the Covid-19 pandemic on racial/ethnic mortality disparities by examining changes in several non-Covid-19 underlying causes of death during the pandemic in 2020 (Arias et al., 2021; Cronin & Evans, 2021; Shiels, Almeida, et al., 2021). Using age-standardized death rates for Non-Hispanic White, Non-Hispanic Black, and Hispanic individuals (hereafter referred to as White, Black, and Hispanic), we examine patterns of mortality change between 2019 and 2020 by underlying cause of death, age, and sex and identify the causes of death with the greatest impact on changes in racial/ethnic mortality differentials.
2. Methods
2.1. Data sources
All analyses were conducted using a combination of publicly available datasets from the National Center for Health Statistics (NCHS) and the United States Census Bureau. Provisional monthly death counts for January–December 2019 and 2020, were obtained for the US population aged 25+ by available underlying causes of death, 10-year age groups (25–34, 35–44, … 75–85, 85+), sex, and single-race coded categories for race/ethnicity (NCHS, 2021). Mid-year (July 1st) population estimates by age, sex, and race/ethnicity were obtained from the Census Bureau's monthly national-level population estimates (US Census Bureau, 2020).
2.2. Causes of death
Covid-19 deaths were restricted to deaths in which Covid-19 was assigned as the underlying cause, an approach employed in prior studies (Ahmad & Anderson, 2021; Glei, 2021; Shiels, Haque, et al., 2021). By doing so, we were able to examine a mutually exclusive and exhaustive set of 13 underlying causes of death, including: Covid-19; Alzheimer's disease; cerebrovascular diseases; chronic lower respiratory disease (CLRD); diabetes mellitus; heart diseases; external causes; influenza and pneumonia; malignant neoplasms; nephritis, nephrotic syndrome, and nephrosis; other respiratory diseases; septicemia; signs and symptoms not elsewhere classified; and a residual all other cause-of-death category. Our use of these 13 causes of death expands upon a previous study of racial/ethnic differences that investigated only Covid-19 deaths and those from all other causes combined (Cronin & Evans, 2021). Another study included a list of seven causes of death that did not include the major category of external causes, which was grouped into a residual category (Shiels, Haque, et al., 2021).
The inclusion of Covid-19 deaths not assigned as an underlying cause would have raised 2020 Covid-19 deaths for the population aged 25+ by 8.8%. We conducted supplementary tests to investigate how features of cause-of-death assignment may affect the findings presented here. In these analyses, we explore variation in the assignment of Covid-19 as an underlying cause by age and race/ethnicity. We also identify differences in cause-of-death patterns between early and later stages of the pandemic to investigate whether coding practices may have changed over the course of the 2020 pandemic year [Appendix B].
2.3. Procedures
Crude death rates were age-standardized using the mid-year 2020 national age distribution for population aged 25+ as well as for ages 25–64 and 65+. All-cause and cause-specific age-standardized death rates (ASDR) were derived by sex and by race/ethnicity for White, Black, and Hispanic populations. We start at age 25 because the number of Covid-19 deaths in 2020 below age 25 was likely small given that all-cause deaths below age 25 in 2020 were 2% below the average for 2015-19 (Rossen, 2020). We use age-standardized rates to avoid spurious changes in numbers of deaths or crude death rates resulting from population growth and/or aging (Shiels, Almeida, et al., 2021). We examine changes in both absolute and relative (percent change) differences in mortality by cause of death, though we primarily feature the absolute change in this paper as the most direct measure of the change in the frequency of death per person.
We assume that the difference in age-standardized all-cause mortality rates between 2019 and 2020 reflects the effect of the Covid-19 pandemic on mortality, aligning with previous descriptive work on excess mortality in 2020 (Ahmad & Anderson, 2021). Alternative approaches have compared 2020 mortality to mortality projected in 2020 on the basis of mortality rates in years prior to 2020 (Weinberger et al., 2020; Woolf, Chapman, et al., 2021). The absence of single-race death counts before 2018, and the absence of bridged-race data in 2020, prevents us from using the time-series approach (NCHS, 2020a). Single-race coding reflects categories in which non-Hispanic White and non-Hispanic Black correspond to those who selected White and Black only, excluding multiple race selections, whereas a bridged-race schema allots and reclassifies those multiple-race selections into single-race categories. However, to investigate the sensitivity of the primary results to this methodological choice, we used bridged-race deaths to investigate how results would change if, instead of using 2019 rates for comparison to 2020 rates, we had used predicted 2020 rates based on a time series fitted to 2015–2019 observations [Appendix B3]. These analyses were conducted for all-cause mortality and for those underlying causes of death that were the key contributors for the increase in all cause-mortality (external causes, heart disease, and diabetes).
3. Results
For the entire United States, the number of deaths at ages 25+ rose by 19.0% between 2019 and 2020 and the age-standardized death rate at ages 25+ rose by 17.0% [Table 1 ]. The age-standardized percentage varied sharply among racial/ethnic groups, increasing by only 13.0% among the White population compared to 27.2% and 39.3% among the Black and Hispanic population, respectively.
Table 1.
All-cause deaths, population, and age-standardized death rates (ages 25+) by race/ethnicity and sex.
| Total Population |
Non-Hispanic White |
Non-Hispanic Black |
Hispanic |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change |
Change |
Change |
Change |
|||||||||||||
| 2019 | 2020 | (#) | (%) | 2019 | 2020 | (#) | (%) | 2019 | 2020 | (#) | (%) | 2019 | 2020 | (#) | (%) | |
| Deaths (thousands) | ||||||||||||||||
| Male | 1435 | 1731 | 296 | 20.7 | 1098 | 1262 | 164 | 14.9 | 171 | 226 | 55.0 | 32.1 | 109 | 167 | 57.9 | 52.9 |
| Female | 1360 | 1594 | 234 | 17.2 | 1058 | 1196 | 138 | 13.0 | 160 | 206 | 46.1 | 28.8 | 90 | 126 | 35.8 | 39.6 |
| Total | 2795 | 3325 | 530 | 19.0 | 2157 | 2458 | 302 | 14.0 | 331 | 432 | 101.1 | 30.5 | 200 | 293 | 93.7 | 46.9 |
| Population (thousands) | ||||||||||||||||
| Male | 108,907 | 109,726 | 819 | 0.8 | 70,293 | 70,348 | 55 | 0.1 | 12,453 | 12,613 | 160 | 1.3 | 17,492 | 17,891 | 399 | 2.3 |
| Female | 116,100 | 116,909 | 810 | 0.7 | 74,356 | 74,384 | 28 | 0.0 | 14,437 | 14,600 | 164 | 1.1 | 17,462 | 17,868 | 406 | 2.3 |
| Total | 225,006 | 226,635 | 1629 | 0.7 | 144,649 | 144,732 | 83 | 0.1 | 26,889 | 27,213 | 324 | 1.2 | 34,954 | 35,758 | 804 | 2.3 |
| ASDR(per 100,000) | ||||||||||||||||
| Male | 1479 | 1747 | 267 | 18.1 | 1521 | 1727 | 206 | 13.5 | 1877 | 2411 | 534 | 28.4 | 1106 | 1592 | 487 | 44.0 |
| Female | 1064 | 1230 | 166 | 15.6 | 1109 | 1245 | 136 | 12.3 | 1258 | 1581 | 323 | 25.7 | 762 | 1016 | 254 | 33.4 |
| Total | 1254 | 1467 | 213 | 17.0 | 1300 | 1469 | 169 | 13.0 | 1521 | 1935 | 413 | 27.2 | 918 | 1279 | 361 | 39.3 |
Note: ASDR refers to age-standardized death rate (per 100,000).
Table 2 shows the ordering of the mortality change by racial/ethnic group depends on whether we focus on the absolute or the percentage change in the age-standardized death rate. While Hispanic individuals suffered the greatest percentage increase in age-standardized mortality, the Black population had the largest absolute increase (413/100,000) compared to the Hispanic (361/100,000) and White population (169/100,000).
Table 2.
Change in age-standardized death rates (ages 25+) by cause of death and race/ethnicity, both sexes.
| Total Population |
Non-Hispanic White |
Non-Hispanic Black |
Hispanic |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASDR |
Change |
ASDR |
Change |
ASDR |
Change |
ASDR |
Change |
|||||||||
| 2019 | 2020 | (#) | (%) | 2019 | 2020 | (#) | (%) | 2019 | 2020 | (#) | (%) | 2019 | 2020 | (#) | (%) | |
| All Cause |
1253.7 |
1467.2 |
213.4 |
17.0 |
1299.8 |
1468.9 |
169.1 |
13.0 |
1521.4 |
1934.8 |
413.3 |
27.2 |
918.2 |
1278.9 |
360.7 |
39.3 |
| Covid-19 | – | 154.8 | 154.8 | – | – | 121.9 | 121.9 | – | – | 259.2 | 259.2 | – | – | 285.8 | 285.8 | – |
| Non-Covid-19 |
1253.7 |
1312.4 |
58.7 |
4.7 |
1299.8 |
1347.0 |
47.2 |
3.6 |
1521.4 |
1675.6 |
154.2 |
10.1 |
918.2 |
993.1 |
74.9 |
8.2 |
| Alzheimer disease | 54.5 | 59.2 | 4.8 | 8.7 | 57.6 | 62.1 | 4.6 | 7.9 | 50.5 | 57.6 | 7.1 | 14.1 | 46.5 | 53.0 | 6.5 | 13.9 |
| Cerebrovascular diseases | 67.2 | 70.6 | 3.5 | 5.2 | 64.9 | 67.8 | 2.8 | 4.3 | 96.5 | 104.7 | 8.2 | 8.5 | 59.7 | 63.6 | 3.9 | 6.5 |
| CLRD | 70.5 | 67.2 | −3.3 | −4.7 | 80.9 | 76.7 | −4.2 | −5.2 | 53.4 | 55.8 | 2.5 | 4.7 | 29.5 | 29.1 | −0.4 | −1.2 |
| Diabetes mellitus | 39.2 | 45.0 | 5.7 | 14.6 | 34.7 | 38.4 | 3.7 | 10.8 | 69.9 | 85.3 | 15.4 | 22.0 | 47.3 | 56.8 | 9.5 | 20.2 |
| Diseases of heart | 295.0 | 307.5 | 12.5 | 4.2 | 303.8 | 312.0 | 8.2 | 2.7 | 377.7 | 420.3 | 42.6 | 11.3 | 204.4 | 225.6 | 21.2 | 10.4 |
| External Causes | 99.0 | 110.8 | 11.8 | 11.9 | 108.9 | 119.1 | 10.2 | 9.4 | 111.3 | 140.3 | 29.0 | 26.1 | 65.3 | 74.7 | 9.4 | 14.3 |
| Influenza and pneumonia | 22.1 | 23.5 | 1.4 | 6.3 | 22.4 | 22.9 | 0.5 | 2.0 | 24.7 | 30.8 | 6.1 | 24.9 | 17.8 | 22.0 | 4.1 | 23.1 |
| Malignant neoplasms | 268.4 | 265.0 | −3.4 | −1.3 | 279.0 | 276.5 | −2.4 | −0.9 | 319.6 | 312.5 | −7.0 | −2.2 | 193.3 | 189.2 | −4.1 | −2.1 |
| Nephritis | 23.1 | 23.2 | 0.0 | 0.2 | 20.8 | 20.5 | −0.3 | −1.3 | 46.0 | 48.1 | 2.1 | 4.6 | 21.6 | 21.5 | −0.2 | −0.9 |
| Other respiratory diseases | 19.6 | 19.7 | 0.1 | 0.7 | 20.6 | 20.4 | −0.2 | −1.1 | 18.5 | 21.7 | 3.2 | 17.4 | 16.7 | 17.2 | 0.5 | 3.1 |
| Septicemia | 17.1 | 17.6 | 0.5 | 3.1 | 16.8 | 17.2 | 0.4 | 2.4 | 28.9 | 30.4 | 1.5 | 5.1 | 12.3 | 13.1 | 0.8 | 6.4 |
| Signs not elsewhere classified | 13.0 | 13.6 | 0.6 | 4.4 | 13.9 | 14.0 | 0.1 | 1.0 | 15.4 | 18.0 | 2.6 | 16.6 | 6.9 | 7.8 | 1.0 | 14.1 |
| All Other Causes | 265.0 | 289.4 | 24.4 | 9.2 | 275.6 | 299.3 | 23.7 | 8.6 | 309.1 | 350.0 | 40.8 | 13.2 | 196.9 | 219.5 | 22.6 | 11.5 |
Note: ASDR refers to age-standardized death rate (per 100,000). CLRD refers to chronic lower respiratory diseases.
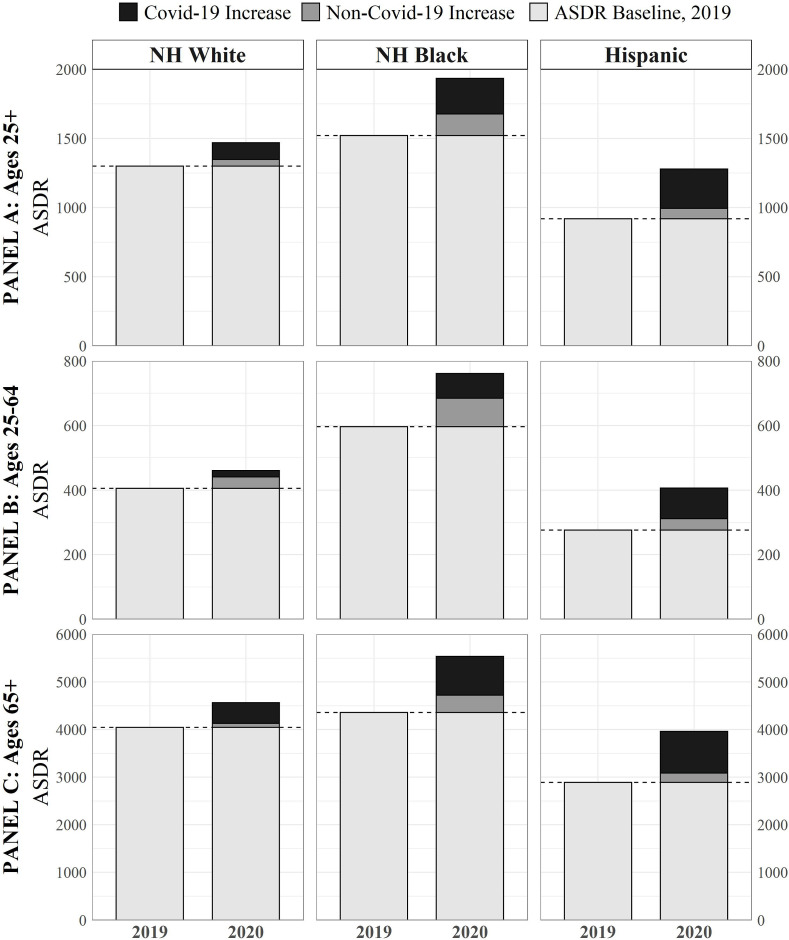
Fig. 1 illustrates the contribution of Covid-19 and causes other than Covid-19 to changes in all-cause mortality between 2019 and 2020. Although the Black population had the largest increase, the reason was not that Black individuals had the highest Covid-19 death rates. Instead, the Hispanic population aged 25+ saw the highest Covid-19 death rate in 2020 (286/100,000), compared to 259/100,000 for the Black population and 122/100,000 for the White population.
Fig. 1.
Age-standardized death rates (ASDR) by race/ethnicity, 2019–2020
Note: ASDR refers to age-standardized death rate (per 100,000). Figure shows All-Cause ASDR by race/ethnicity (both sexes) in 2019 and 2020, decomposing the 2020 increase attributable to Covid-19 and non-Covid-19. Y-axis scales change between age group panels.
The figure also reveals that mortality from underlying causes of death other than Covid-19 rose for all three groups. The Black population aged 25+ saw the largest increase in mortality from causes other than Covid-19, with an increase of 154/100,000, followed by the Hispanic population (75/100,000) and the White population (47/100,000) [Table 2]. Of the total increase in mortality between 2019 and 2020, Covid-19 deaths accounted for 62.7% of the increase among Black, 72.1% among White, and 79.2% among Hispanic individuals [Table 3 ].
Table 3.
Decomposition of All-Cause and Non-Covid-19 Mortality Change by Cause
| Total Population |
Non-Hispanic White |
Non-Hispanic Black |
Hispanic |
|||||
|---|---|---|---|---|---|---|---|---|
| All-Cause (%) | Non-Covid-19 (%) | All-Cause (%) | Non-Covid-19 (%) | All-Cause (%) | Non-Covid-19 (%) | All-Cause (%) | Non-Covid-19 (%) | |
| All Cause |
100.0 |
– |
100.0 |
– |
100.0 |
– |
100.0 |
– |
| Covid-19 | 72.5 | – | 72.1 | – | 62.7 | – | 79.2 | – |
| Non-Covid-19 |
27.5 |
100.0 |
27.9 |
100.0 |
37.3 |
100.0 |
20.8 |
100.0 |
| Alzheimer disease | 2.2 | 8.1 | 2.7 | 9.7 | 1.7 | 4.6 | 1.8 | 8.6 |
| Cerebrovascular diseases | 1.6 | 6.0 | 1.7 | 6.0 | 2.0 | 5.3 | 1.1 | 5.2 |
| CLRD | −1.5 | −5.6 | −2.5 | −8.9 | 0.6 | 1.6 | −0.1 | −0.5 |
| Diabetes mellitus | 2.7 | 9.8 | 2.2 | 7.9 | 3.7 | 10.0 | 2.6 | 12.7 |
| Diseases of heart | 5.9 | 21.3 | 4.8 | 17.4 | 10.3 | 27.6 | 5.9 | 28.3 |
| External Causes | 5.5 | 20.2 | 6.0 | 21.7 | 7.0 | 18.8 | 2.6 | 12.5 |
| Influenza and pneumonia | 0.7 | 2.4 | 0.3 | 1.0 | 1.5 | 4.0 | 1.1 | 5.5 |
| Malignant neoplasms | −1.6 | −5.8 | −1.4 | −5.1 | −1.7 | −4.5 | −1.1 | −5.4 |
| Nephritis | 0.0 | 0.1 | −0.2 | −0.6 | 0.5 | 1.4 | −0.1 | −0.2 |
| Other respiratory diseases | 0.1 | 0.2 | −0.1 | −0.5 | 0.8 | 2.1 | 0.1 | 0.7 |
| Septicemia | 0.3 | 0.9 | 0.2 | 0.8 | 0.4 | 1.0 | 0.2 | 1.1 |
| Signs not elsewhere classified | 0.3 | 1.0 | 8.1 | 0.3 | 0.6 | 1.7 | 0.3 | 1.3 |
| All Other Causes | 11.4 | 41.5 | 14.0 | 50.3 | 9.9 | 26.5 | 6.3 | 30.2 |
Note: Table presents the percent of the change in All-Cause and Non-Covid-19 age-standardized death rate (ASDR) between 2019 and 2020 attributable to various causes of death.
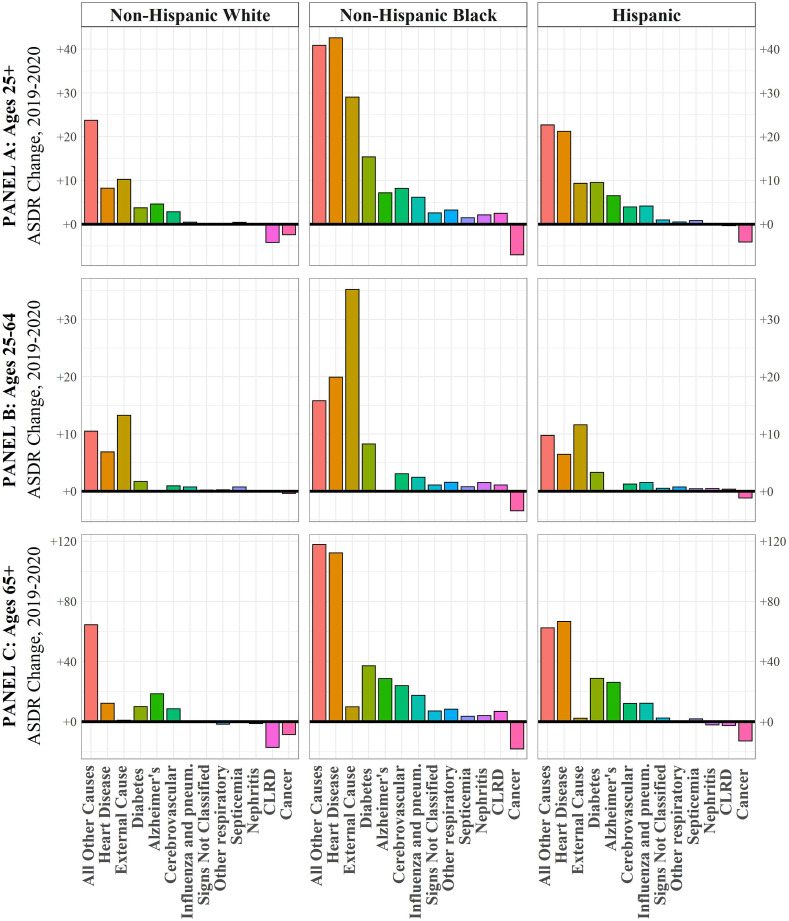
Other non-Covid-19 causes of death contributing to the mortality increase between 2019 and 2020 are shown in Table 3 and in Fig. 2 . Apart from Covid-19 and the residual category, the three largest increases in mortality for Black and Hispanic individuals were from heart disease, diabetes, and external causes of death. These were three of the four largest increases among White populations as well, along with Alzheimer's disease. However, the magnitude of the increases was markedly different; Black individuals experienced the greatest increase from all three causes, ranging from 11% to over 26%. In fact, for all causes of death except malignant neoplasms, where mortality fell, Black populations suffered from larger mortality increases than White or Hispanic populations.
Fig. 2.
Change in Cause-Specific Age-Standardized Death Rates other than Covid-19 by Race/Ethnicity, 2019–2020
Note: ASDR refers to age-standardized death rate (per 100,000). Figure shows absolute ASDR change by race/ethnicity (both sexes) for all non-Covid-19 causes of death in 2020, relative to 2019. Y-axis scales change between age group panels. All other causes refers to the constructed residual category. CLRD = Chronic Lower Respiratory Disease.
The same four cause-of-death categories dominate racial/ethnic mortality disparities [Table A1]. Fifty-six percent of the increase in age-standardized Black mortality relative to White mortality was attributable to Covid-19, while 14.1% was attributable to heart disease, 7.7% to external causes, and 4.8% to diabetes. The change in the Hispanic and White mortality gap was overwhelmingly attributable to Covid-19, which accounted for 85.5% of the relative rise in Hispanic mortality. Greater increases for Black mortality relative to Hispanic mortality from heart disease, external causes, and diabetes more than offset the greater increase from Covid-19 in the Hispanic population.
Relative increases in mortality by age reveal differential age-patterns by race/ethnicity [Table A2]. Within the White population, percentage change in mortality was the same across age groups, increasing 13% among both working aged (25–64) and older aged (65+) White populations. Though over double the White increase, Black working age and older age populations also experienced the same percentage increase in all-cause mortality in both age groups, 27%. Hispanic age-specific mortality, however, told a different story, with the percent increase in mortality at working ages, 47%, substantially higher than the percent increase at ages 65+, 37%.
Since the age-pattern of mortality from Covid-19, like that of all causes of death combined, is skewed towards older individuals, cause-specific mortality changes for ages 25+ closely reflect those that occurred at ages 65+. The story when focused on working ages (25–64) is quite different. Covid-19 accounted for most of the all-cause mortality increase for the Hispanic working-age population (72.9%), whereas it was responsible for only 36.5% of the increase among White and 46.9% among Black working-age individuals. For all three racial/ethnic groups, the cause of death contributing the most to increases in mortality between 2019 and 2020 at ages 25–64, apart from Covid-19, was external causes of death. The rise in external-cause mortality for the Black working-age population was 2.7–3.0 times the increase for the other two groups. Increases in mortality from heart disease and diabetes were the third and fourth largest contributors to all-cause mortality increases at age 25–64 for all three groups.
The pattern of relative change in mortality between 2019 and 2020 was similar for men and women [Tables A3 and A4] with the largest increases documented for Hispanic men (44.0% increase) and women (33.4% increase). This difference was particularly exaggerated at working-ages with working-age Hispanic men facing by far the sharpest percentage increase in mortality, 51.9%, of any age-sex-race/ethnicity group.
Although there were few sex differences in the contribution of Covid-19 to mortality change, one specific cause of death showed a sharp differentiation between the sexes. For all three groups, mortality from external causes increased much more in 2020 for men than for women. This distinction was especially pronounced in the working ages, where the rise in mortality was 19.4/100,00 for males vs. 3.5 for females among Hispanic, 19.2 vs. 7.2 among White, and 57.1 vs. 15.0 among Black populations.
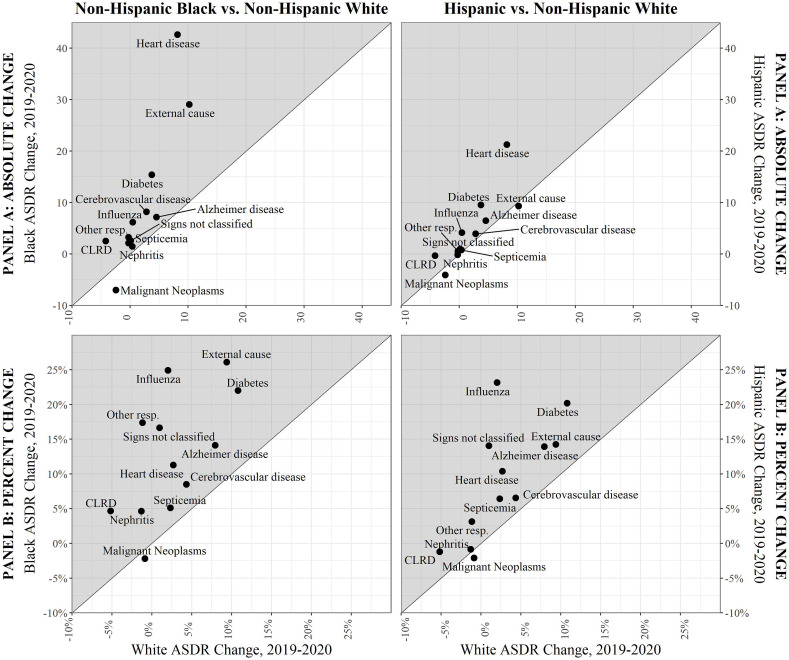
Our discussion has largely focused on absolute changes in mortality among the different racial/ethnic groups. Fig. 3 illustrates the contrast between absolute and relative changes. The Figure presents scatter diagrams of both absolute (Panel A) and percentage changes (Panel B) in mortality at ages 25+ for different causes of death for White individuals on the x-axis and either Black or Hispanic individuals on the y-axis. Points above the 45-degree line indicate causes of death for which Black or Hispanic populations had a higher absolute or percentage increase (or smaller decline) than the White population. Nearly all points are above the 45-degree lines. In absolute terms, Panel A shows that Black populations faced clear and strikingly larger increases in heart disease, external cause, and diabetes mortality compared to the White population. In percentage or relative terms, the story is more varied. For both Black and Hispanic communities, the highest percentage increase relative to White communities pertains to influenza and pneumonia, a category with symptoms similar to those of Covid-19. Percentage increases in mortality from a variety of other causes, including diabetes, heart disease, Alzheimer's, chronic lower respiratory diseases, external causes, other respiratory diseases, and signs and symptoms not elsewhere classified, are also higher for both Hispanic and Black populations compared to the White population [Table 2]. Although a clear White mortality advantage persists across both panels, this figure demonstrates how the cause-specific interpretation of that advantage may vary when considering absolute versus relative disparities.
Fig. 3.
Racial/ethnic comparisons of non-Covid-19 age-standardized death rate change (both sexes, ages 25+), 2019–2020.
Note: ASDR refers to age-standardized death rate (per 100,000). Figure shows racial/ethnic comparisons of ASDR change (both sexes) for all non-Covid-19 causes of death in 2020, relative to 2019, with Panel A presenting ABSOLUTE change and Panel B presenting PERCENT change. Shaded area indicates where increase was greater for Black (Panel A) and Hispanic (Panel B) individuals relative to White individuals. CLRD = Chronic Lower Respiratory Disease, Influenza = Influenza and pneumonia, Other resp = Other respiratory diseases. The constructed residual category is not included.
4. Discussion
Although all-cause mortality rose sharply in the United States between 2019 and 2020, the extent and nature of that increase varied greatly for White, Black, and Hispanic individuals. The largest all-cause mortality increase was recorded for the Black population, but the reason was not the number of deaths assigned to Covid-19 as an underlying cause of death. Instead, Black individuals had by far the largest increase in death rates from other causes of death, nearly double that among Hispanic individuals and more than triple that among White individuals. Meanwhile, Hispanic populations experienced the largest absolute increase in Covid-19 mortality, with particularly remarkable increases over pre-pandemic levels among Hispanic working-age men.
4.1. High Covid-19 mortality among Hispanic communities
The Hispanic Covid-19 death rate in 2020 was around 1.1 times higher than the Black death rate and 2.3 times higher than the White death rate. These findings are consistent with other evidence that has emerged surrounding the particularly adverse impact of the pandemic on Hispanic mortality (Riley et al., 2021; Rodriguez-Diaz et al., 2020; Simon et al., 2021).
The high mortality of Hispanic individuals from Covid-19 appears to be primarily attributable to a high incidence of infection and secondarily to a high case-fatality rate. A study of Covid-19 incidence among 50 million health system enrollees revealed a per capita infection rate of 143/1000,00 for Hispanic individuals, relative to 107 and 46 for Black and White individuals, respectively (Rubin-Miller et al., 2020). The relative rate ratios of infection are even higher than the respective ratios of Covid-19 mortality [Table 2], suggesting that infection rates are driving mortality differentials (Zelner et al., 2020).
In particular, we show that all-cause and Covid-19 mortality was particularly inflated among the Hispanic working-aged populations, strikingly so for Hispanic working-age men, underscoring the saliency of unequal structural contexts (e.g. occupational, residential, socioeconomic) that have shaped a distinct Covid-19 mortality disadvantage for the Hispanic community. A large body of research has shown how structural and systemic racism during the pandemic has routinely disadvantaged communities of color by placing these communities at heightened risk of Covid-19 incidence (Bailey et al., 2021; Garcia et al., 2021; McClure et al., 2020). Hispanic individuals are disproportionately represented in essential occupations with high-exposure to Covid-19 and limited workplace protections (Rodriguez-Diaz et al., 2020; Simon et al., 2021). Additionally, Hispanic populations are more likely to live in denser, multigenerational households, magnifying the effect of occupational exposure (Macias Gil et al., 2020; Riley et al., 2021). These factors may be particularly influential within the immigrant community, where an even more pronounced mortality disadvantage during the pandemic has been found (Riley et al., 2021).
Reduced access to adequate health care also likely contributes towards higher Covid-19 case-fatality rates among Hispanic individuals. Hispanic communities have the lowest rate of health insurance coverage of any racial/ethnic group in the United States, with nearly 20% uninsured, compared to just 5% of the White population (Macias Gil et al., 2020). Language barriers, distrust and fear of healthcare institutions driven by broader anti-immigrant rhetoric and policy, and underlying financial hardship faced by Hispanic individuals, particularly those in the immigrant community, have all been linked to worse healthcare access and quality, potentially amplifying the impact of Covid-19 on mortality outcomes (Macias Gil et al., 2020). These health care barriers, coupled with a higher prevalence of comorbid conditions, such as diabetes and heart disease, may worsen Covid-19 outcomes once infection occurs (Simon et al., 2021).
The alarming impact of the Covid-19 pandemic on Hispanic working-age mortality calls attention to the need for policy interventions targeting the domains of employment, housing, and healthcare. These could include expanding worker protections and improving workplace safety regulations, especially in high-risk occupations like meat processing; providing more comprehensive financial relief to low-income families; broadening the availability of no cost testing; and ensuring universal access to health care regardless of immigration status.
4.2. High mortality from non-Covid-19 causes of death among Black individuals
Despite having levels of Covid-19 incidence and mortality below those of Hispanic individuals, Black individuals saw the largest absolute increase in all-cause mortality, a pattern consistent with previous work (Price-Haywood et al., 2020; Rossen, 2021; Stokes, Lundberg, Bor, Elo, et al., 2021). In addition to Covid-19, this increase is substantially attributable to causes other than Covid-19, highlighting the ways that the Covid-19 pandemic may have indirectly shaped mortality among Black communities.
Increases in heart disease and diabetes mortality for Black individuals were more than four times and 1.6–2.0 times higher than for White and Hispanic individuals, respectively. One explanation offered for the large increases in non-Covid-19 mortality is that the pandemic disrupted access to personal support networks and health care in ways that hindered disease management for people with these chronic diseases (Ahmad & Anderson, 2021; Glei, 2021). Fear of infection, loss of health insurance, reductions in visits to physicians and in elective procedures have been noted as indirect effects of the pandemic (Cantor et al., 2020). These factors are more salient among Black individuals for whom the pre-pandemic prevalence of serious heart disease, hypertension and diabetes exceeded that among White individuals (Kim et al. 2021). Research has increasingly pointed to the role of structural racism in producing a higher prevalence of chronic conditions among communities of color (Bleich & Ard, 2021; Golden, 2021), highlighting another way in which the Covid-19 crisis has exposed the human costs of continued racial injustice.
The possible role of forgone care for these conditions during the pandemic (Anderson et al., 2021) underscores the important of reinforcing continuity of care for chronic conditions during public health emergencies, especially among those with limited or no health insurance. Such care includes ensuring universal health care coverage, access to high quality primary care, including diabetes screening and support services, and providing affordable medications, including life-saving therapies like oral glycemic agents and insulin.
Mortality from external causes of death also rose sharply among Black individuals. This increase was nearly three times greater for the Black population than for the White or Hispanic population, a distinction most pronounced among working-age males. Unfortunately, the data do not currently permit us to distinguish among external causes. Previous research has shown that the principal increase in mortality within this category between 2019 and 2020 pertains to drug-related mortality (Ahmad & Anderson, 2021; Glei, 2021), as well as increases in homicides (Faust et al., 2021), and there are indications that this rise may be more pronounced among Black and Hispanic communities (Friedman et al., 2021). Growth in external-cause mortality draws attention to the ways in which social isolation, economic instability, and treatment disruption may have exacerbated “deaths of despair” among working-age Americans (Elo et al., 2019; Shiels et al., 2020). Health systems may be implicated through pandemic-related interruptions in emergency response and shortages of drug overdose response medication such as Naloxone. This possibility warrants particular concern for the Black and Hispanic communities who have absorbed a disproportionate share of these forms of disadvantage during the pandemic.
4.3. Possible errors in diagnosis and coding of underlying cause of death
Another explanation of changing death rates in 2020 relates to the process by which underlying cause of death is assigned on death certificates. Some jurisdictions across the U.S., especially early in the pandemic, required a positive test result for a death to be assigned to Covid-19 and thus an absence of testing may have led to a death being assigned to a comorbid chronic condition such as diabetes or heart disease (Stokes, Lundberg, Bor, Elo, et al., 2021). Accurate cause of death assignment is also complicated by the large number of home deaths, especially among racial/ethnic minority populations (Pathak et al., 2021). Deaths occurring at home are more likely to be certified by a local coroner, who may lack medical training and has limited resources for performing post-mortem testing or autopsies (Stokes, Lundberg, Bor, & Bibbins-Domingo, 2021).
In Appendix B, we assess the extent to which differences in diagnostic or coding practices may be reflected in our results. We find that, among Hispanics, 94.5% of deaths in which Covid-19 appears anywhere on the death certificate are assigned to Covid-19 as an underlying cause of death, in contrast to 91.9% among Black and 89.9% among White individuals [Table B1]. Thus, a small portion of the higher death rates from Covid-19 among Hispanics may reflect differences in diagnostic or coding practices, including a greater tendency to assign Covid-19 as an underlying cause, or a weaker tendency to assign it as a contributing cause, among Hispanic deaths.
Table B2 presents evidence on the timing of mortality associated with the pandemic during 2020. One might anticipate that, during its early stages, limitations of testing and unfamiliarity with the disease might have resulted in many deaths that should have been attributable to Covid-19 being assigned to other causes. In this case, the ratio of non-Covid-19 mortality increases to Covid-19 increases should be inflated, particularly for the Black population who saw the largest increases in non-Covid-19 mortality. Table B2 shows that the ratio of non-Covid-19 mortality increases (excluding those from external causes) to Covid-19 increases among the Black population was very similar in the first half of 2020 (0.490) to that in the second half (0.476). In the Hispanic population, the comparable ratios were 0.247 and 0.221 and in the White population, 0.240 and 0.329. These comparisons provide scant evidence that faulty cause-of-death assignments in the early stages of the pandemic played a major role in inflating the number of deaths from causes other than Covid-19. The same conclusion applies to the working age population (25–64) in Table B2.
Increases in mortality from influenza/pneumonia and other respiratory diseases fell in the later stage of 2020 relative to the earlier stage for all three groups. While this change could represent over-coding of these entities early in the pandemic, as suggested by Weinberger et al. (2020), it is also likely that mortality from these causes declined as social distancing and masking behaviors improved. The much higher values of mortality from these causes for the Black and Hispanic populations (Fig. 3) is consistent with a greater tendency for Covid-19 deaths to be assigned to them than among the White population, although other explanations are also possible.
These findings suggest an urgent need to improve mortality surveillance systems in the United States to ensure the accuracy and timeliness of data for tracking the effects of the current pandemics and future public health emergencies on racial/ethnic health disparities. Future research should fully investigate the nature and extent of misclassification, particularly racial/ethnic variation in misclassification, which would have urgent implications for pandemic response policies and interventions.
4.4. Limitations
Our analysis had several limitations. First, deaths included in this analysis were available from the NCHS through August 3, 2021 and it is possible that delays in registration will result in additional deaths being reported for 2020. Such delays are especially likely for external causes of death for which certification often involves multiple authorities.
Second, the present paper was limited to Black, Hispanic, and White adults, as data quality was greatest in these groups and the populations were sufficiently large to generate stable mortality rates by age, sex, and cause of death. Future research should incorporate analyses of American Indian and Alaskan Natives and other racial/ethnic groups that experienced significant adverse mortality trends during the Covid-19 pandemic (Rossen, 2021).
A third limitation involves uncertainty about how deaths attributable to the Covid-19 pandemic should be estimated. Alternative methods of estimating what mortality would have been in 2020 in the absence of the Covid-19 pandemic will produce different estimates of the pandemic's impact. The present analysis employed direct comparisons of mortality between 2019 and 2020 in order to maintain consistency in single-race coding across years (Ahmad & Anderson, 2021). In Appendix Table B3 we compare 2019 death rates at ages 25+ and 65+ from all-causes, heart disease and diabetes to predicted 2020 mortality levels using a linear modeling approach based on bridged-race deaths between 2015 and 2019. The two sets of predictions of 2020 death rates are very consistent. In contrast, estimates of changes in mortality from external causes are sensitive to whether prior mortality trends are incorporated into estimates of expected deaths in 2020. This sensitivity is likely the result from the rising drug overdose mortality already evident between 2015 and 2019, a trend that may have continued into 2020 (Glei, 2021).
Finally, as noted earlier, our study is based on data in which Covid-19 is listed as the underlying cause of death and detailed cause of death information available in the publicly released NCHS data is limited to 13 select causes of death (NCHS, 2020b). Thus, our residual cause-of-death category comprised a small but not an insignificant portion of the increase in all-cause mortality at ages 25+ (6.3% for Hispanic, 9.7% for Black, and 13.9% for White populations). Future research should further explore how varying time-series approaches and more detailed cause-of death information may affect the estimates presented here.
Despite these limitations, this research provides a rich and comprehensive view of the United States mortality landscape throughout the 2020 Covid-19 pandemic, expanding the current conversation surrounding the pandemic's mortality impact to the intersection of race/ethnicity, age, sex, and cause of death.
5. Conclusion
Our findings suggest that the overall effect of the Covid-19 pandemic on racial/ethnic disparities was much larger than that captured by official Covid-19 death tallies alone. This study captures additional evidence of a distressing Covid-19 mortality disadvantage absorbed by the Hispanic population, with Hispanic working-age men experiencing the largest percentage increases in all-cause mortality. Black individuals, on the other hand, in addition to the sizable contribution of Covid-19 to a mortality increase in 2020, had exceptionally large increases in non-Covid-19 causes of death during the pandemic, including from heart disease, diabetes, and external causes, reinforcing the importance of assessing these deaths to fully account the pandemic's disparate impacts on population health.
Ethical statement
This secondary data analysis relied on publicly available, de-identified data from the National Center for Health Statistics and the Census Bureau. Thus, there was no need to obtain ethics approval. Analytical code is publicly available in a replication repository (https://github.com/annelieseluck/Covid-19-Racial-Ethnic-Disparities-by-Cause-of-Death).
Authorship contribution statement
All Authors: Conceptualization, Writing, Review & Editing. A. Luck: Formal analysis.
Declaration of competing interest
A. Stokes reported receiving grants from Swiss Re and Johnson and Johnson, Inc outside the submitted work. No other authors reported conflicts of interest.
Acknowledgements
The authors acknowledge funding from the Robert Wood Johnson Foundation (#77521), the National Institute on Aging (#R01-AG060115-04 and #R01-AG060115-04S1), and National Institute of Child Health and Human Development (#T32 HD007242). The authors thank Robert N. Anderson and Farida B. Ahmad from the National Center for Health Statistics, Kevin Barragan from the U.S. Census Bureau and Katherine Hempstead from the Robert Wood Johnson Foundation. We are also grateful for comments by Dana Glei.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.101012.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ahmad F.B., Anderson R.N. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829–1830. doi: 10.1001/jama.2021.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsan M., Chandra A., Simon K.I. National Bureau of Economic Research; 2021. The great unequalizer: Initial health Effects of COVID-19 in the United States (working paper No. 28958; working paper series) [DOI] [Google Scholar]
- Anderson K.E., McGinty E.E., Presskreischer R., Barry C.L. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Network Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.34882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrasfay T., Goldman N. Association of the COVID-19 pandemic with estimated life expectancy by race/ethnicity in the United States, 2020. JAMA Network Open. 2021;4(6) doi: 10.1001/jamanetworkopen.2021.14520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias E., Betzaida T.-V., Ahmad F., Kochanek K. National Center for Health Statistics (U.S.; 2021. Provisional life expectancy estimates for 2020. [DOI] [Google Scholar]
- Bailey Z.D., Feldman J.M., Bassett M.T. How structural racism works—racist policies as a root cause of U.S. Racial health inequities. New England Journal of Medicine. 2021;384(8):768–773. doi: 10.1056/NEJMms2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich S.N., Ard J.D. COVID-19, obesity, and structural racism: Understanding the past and identifying solutions for the future. Cell Metabolism. 2021;33(2):234–241. doi: 10.1016/j.cmet.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor J.H., Sood N., Bravata D., Pera M., Whaley C.M. National Bureau of Economic Research; 2020. The impact of the COVID-19 pandemic and policy response on health care utilization: Evidence from county-level medical claims and cellphone data (working paper No. 28131; working paper series) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronin C.J., Evans W.N. Excess mortality from COVID and non-COVID causes in minority populations. Proceedings of the National Academy of Sciences. 2021;118(39) doi: 10.1073/pnas.2101386118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo I.T., Hendi A.S., Ho J.Y., Vierboom Y.C., Preston S.H. Trends in non-hispanic white mortality in the United States by metropolitan-nonmetropolitan status and region, 1990–2016. Population and Development Review. 2019;45(3):549–583. doi: 10.1111/padr.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faust J.S., Du C., Mayes K.D., Li S.-X., Lin Z., Barnett M.L., Krumholz H.M. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic. JAMA. 2021;326(1):84–86. doi: 10.1001/jama.2021.8012. March-August 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J., Mann N.C., Hansen H., Bourgois P., Braslow J., Bui A.A.T., Beletsky L., Schriger D.L. Racial/ethnic, social, and geographic trends in overdose-associated cardiac arrests observed by US emergency medical services during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(8):886–895. doi: 10.1001/jamapsychiatry.2021.0967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M.A., Homan P.A., García C., Brown T.H. The color of COVID-19: Structural racism and the disproportionate impact of the pandemic on older Black and latinx adults. Journal of Gerontology: Series B. 2021;76(3):e75–e80. doi: 10.1093/geronb/gbaa114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T. The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity & Disease. 1992;2(3):207–221. [PubMed] [Google Scholar]
- Glei D.A. 2021. The us midlife mortality crisis continues: Increased death rates from causes other than covid-19 during 2020. 2021.05.17.21257241. [DOI] [Google Scholar]
- Golden S.H. The contribution of structural racism to metabolic health disparities in the USA. Lancet Diabetes & Endocrinology. 2021;9(8):478–480. doi: 10.1016/S2213-8587(21)00144-3. [DOI] [PubMed] [Google Scholar]
- Kim C., Stierman B., Hales C.M., Ogden C.L. Race and Hispanic-origin Disparities in Underlying Medical Conditions Associated With Severe COVID-19 Illness: U.S. Adults, 2015-2018. National Health Statistics Reports. 2021:154. [Google Scholar]
- Lopez L., Hart L.H., Katz M.H. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(8):719. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- Macias Gil R., Marcelin J.R., Zuniga-Blanco B., Marquez C., Mathew T., Piggott D.A. COVID-19 pandemic: Disparate health impact on the hispanic/latinx population in the United States. The Journal of Infectious Diseases. 2020;222(10):1592–1595. doi: 10.1093/infdis/jiaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure E.S., Vasudevan P., Bailey Z., Patel S., Robinson W.R. Racial capitalism within public health-how occupational settings drive COVID-19 disparities. American Journal of Epidemiology. 2020;189(11):1244–1253. doi: 10.1093/aje/kwaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS . 2020. Underlying cause of death by single race 2018-2019.https://wonder.cdc.gov/wonder/help/ucd-expanded.html [Google Scholar]
- NCHS . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2020. Guidance for certifying deaths due to coronavirus disease 2019.https://asprtracie.hhs.gov/technical-resources/resource/8174/guidance-for-certifying-deaths-due-to-coronavirus-disease-2019-covid-19 [Google Scholar]
- NCHS . 2021. AH monthly provisional counts of deaths for select causes of death by sex, age, and race and hispanic origin | data | centers for disease control and prevention.https://data.cdc.gov/NCHS/AH-Monthly-Provisional-Counts-of-Deaths-for-Select/65mz-jvh5 [Google Scholar]
- Pathak E.B., Garcia R.B., Menard J.M., Salemi J.L. Out-of-Hospital COVID-19 deaths: Consequences for quality of medical care and accuracy of cause of death coding. American Journal of Public Health. 2021;111(S2):S101–S106. doi: 10.2105/AJPH.2021.306428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annual Review of Sociology. 2015;41:311–330. [Google Scholar]
- Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among Black patients and white patients with covid-19 | NEJM. New England Journal of Medicine. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley A.R., Chen Y.-H., Matthay E.C., Glymour M.M., Torres J.M., Fernandez A., Bibbins-Domingo K. The Preprint Server for Health Sciences; MedRxiv: 2021. (Excess death among Latino people in California during the COVID-19 pandemic). 2020.12.18.20248434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Diaz C.E., Guilamo-Ramos V., Mena L., Hall E., Honermann B., Crowley J.S., Baral S., Prado G.J., Marzan-Rodriguez M., Beyrer C., Sullivan P.S., Millett G.A. Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics. Annals of Epidemiology. 2020;52:46–53. doi: 10.1016/j.annepidem.2020.07.007. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen L.M. 2020. Excess deaths associated with COVID-19, by age and race and ethnicity—United States. January 26–October 3, 2020. MMWR. Morbidity and Mortality Weekly Report, 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen L.M. 2021. Disparities in excess mortality associated with COVID-19—United States. 2020. MMWR. Morbidity and Mortality Weekly Report, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin-Miller L., Alban C. COVID-19 racial disparities in testing, infection, hospitalization, and death: Analysis of epic patient data. 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-racial-disparities-testing-infection-hospitalization-death-analysis-epic-patient-data/ Sep 16, S. S. P., & 2020. September 16KFF.
- Shiels M.S., Almeida J.S., García-Closas M., Albert P.S., Freedman N.D., Berrington de González A. Impact of population growth and aging on estimates of excess U.S. Deaths during the COVID-19 pandemic. Annals of Internal Medicine. 2021;174(4):437–443. doi: 10.7326/M20-7385. March to August 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiels M.S., Haque A.T., Haozous E.A., Albert P.S., Almeida J.S., García-Closas M., Nápoles A.M., Pérez-Stable E.J., Freedman N.D., de González A.B. Racial and ethnic disparities in excess deaths during the COVID-19 pandemic, march to December 2020. Annals of Internal Medicine. 2021;M21–2134 doi: 10.7326/M21-2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiels M.S., Tatalovich Z., Chen Y., Haozous E.A., Hartge P., Nápoles A.M., Pérez-Stable E.J., Rodriquez E.J., Spillane S., Thomas D.A., Withrow D.R., Berrington de González A., Freedman N.D. Trends in mortality from drug poisonings, suicide, and alcohol-induced deaths in the United States from 2000 to 2017. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.16217. e2016217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon P., Ho A., Shah M.D., Shetgiri R. Trends in mortality from COVID-19 and other leading causes of death among latino vs white individuals in Los Angeles county. 2011-2020. JAMA. 2021 doi: 10.1001/jama.2021.11945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes A.C., Lundberg D.J., Bor J., Bibbins-Domingo K. Excess deaths during the COVID-19 pandemic: Implications for US death investigation systems. American Journal of Public Health. 2021;111(S2):S53–S54. doi: 10.2105/AJPH.2021.306331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes A.C., Lundberg D.J., Bor J., Elo I.T., Hempstead K., Preston S.H. Association of health care factors with excess deaths not assigned to COVID-19 in the US. JAMA Network Open. 2021;4(9) doi: 10.1001/jamanetworkopen.2021.25287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau National Population by Characteristics: 2010-2020. Vintage 2020 Population Estimates. https://www.census.gov/programs-surveys/popest/technical-documentation/research/evaluation-estimates/2020-evaluation-estimates/2010s-national-detail.html
- Weinberger D.M., Chen J., Cohen T., Crawford F.W., Mostashari F., Olson D., Pitzer V.E., Reich N.G., Russi M., Simonsen L., Watkins A., Viboud C. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, march to may 2020. JAMA Internal Medicine. 2020;180(10):1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S.H., Chapman D.A., Sabo R.T., Zimmerman E.B. Excess deaths from COVID-19 and other causes in the US, march 1, 2020, to January 2, 2021. JAMA. 2021;325(17):1786–1789. doi: 10.1001/jama.2021.5199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S.H., Masters R.K., Aron L.Y. Effect of the covid-19 pandemic in 2020 on life expectancy across populations in the USA and other high income countries: Simulations of provisional mortality data. BMJ. 2021;373:n1343. doi: 10.1136/bmj.n1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrigley-Field E., Garcia S., Leider J.P., Robertson C., Wurtz R. Racial disparities in COVID-19 and excess mortality in Minnesota. Socius. 2020;6 doi: 10.1177/2378023120980918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelner J., Trangucci R., Naraharisetti R., Cao A., Malosh R.E., Broen K., Masters N., Delamater P.V. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America; 2020. Racial disparities in COVID-19 mortality are driven by unequal infection risks. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.