Background: Hispanic persons with limited English proficiency (LEP) have low rates of COVID-19 testing and high rates of COVID-19 infection and death (1). About 8% of Medicare enrollees have LEP, and the Centers for Medicare & Medicaid Services has identified improving their care as a priority (2). Anecdotal reports suggest that LEP may pose a barrier to COVID-19 vaccination (3, 4), a safe and effective preventive measure, but little is known about the willingness of older persons with LEP to be vaccinated or about factors that might impede vaccination acceptance.
Objective: To assess language-based differences in concerns about and willingness to receive COVID-19 vaccination among Medicare enrollees and differences in COVID-19 testing, symptom severity, whether medical care has been sought, and perceptions regarding COVID-19's contagiousness and lethality.
Methods and Findings: We analyzed data from the Medicare Current Beneficiary Survey COVID-19 Fall Supplement, a nationally representative, cross-sectional telephone survey of Medicare beneficiaries. We classified respondents taking the survey in Spanish as LEP and those taking the survey in English as English proficient (EP). On the basis of self-reported ethnicity, we compared Hispanic beneficiaries with LEP to both Hispanic and non-Hispanic beneficiaries with EP. The survey, which was conducted before the roll-out of COVID-19 vaccines, asked respondents how likely they were to get vaccinated when vaccination became available. We categorized respondents answering “definitely” or “probably” as likely and those answering “probably not,” “definitely not,” or “not sure” as hesitant. Among vaccine-hesitant respondents, we report the prevalence of the 2 most common concerns about the vaccine.
Testing for COVID-19 was self-reported. Among respondents who tested positive, we report severity of symptoms (moderate/severe vs. none/mild), and whether medical care was sought (yes/no). Respondents were considered to agree that COVID-19 is more contagious or deadly than influenza (referred to as “the flu” in the survey) if they answered “agree” or “strongly agree” and to disagree if they answered otherwise. We assessed COVID-19 precautions on the basis of responses to questions about 2 precautions that are the most practicable, effective, and widely advocated by public health experts. For all of these variables, we categorized “don't know,” “refused,” or “inapplicable” responses as missing.
We used logistic regression with marginal standardization to compare Hispanic respondents with LEP with both comparison groups and report unadjusted risk differences (RDs) and RDs adjusted for sex, income, census region, Medicare–Medicaid dual eligibility, and Medicare Advantage enrollment. We used Stata/MP V16.1 (StataCorp), procedures that account for the complex sample design and weights to generate national estimates. Cambridge Health Alliance's Institutional Review Board exempted this study from review.
Results: The sample included 438 Hispanic adults with LEP, 533 Hispanic adults with EP, and 8713 non-Hispanic adults with EP. Hispanic adults with LEP were more often female, older (≥75 years), lower-income, residents of the South or West, enrolled in Medicare Advantage, and lacking a source of care (Table 1).
Table 1.
Characteristics of Medicare Beneficiaries With and Without LEP, by Hispanic Ethnicity, Fall 2020

Hispanic Medicare enrollees with LEP were less likely to anticipate getting vaccinated (unadjusted RD, −12.6% [95% CI, −19.4 to −5.9]) than non-Hispanic adults with EP (Table 2), a difference that was attenuated in the adjusted analysis (RD, −5.8 [CI, −13.6 to 2.0]), primarily due to income differences. Among vaccine-hesitant older respondents, those who were Hispanic with LEP were more likely to be worried about vaccine side effects than non-Hispanic adults with EP (62.6% vs. 41.2%; adjusted RD, 22.4 [CI, 7.7 to 37.1]).
Table 2.
COVID-19 Care Among Medicare Beneficiaries With and Without LEP, by Hispanic Ethnicity, Fall 2020
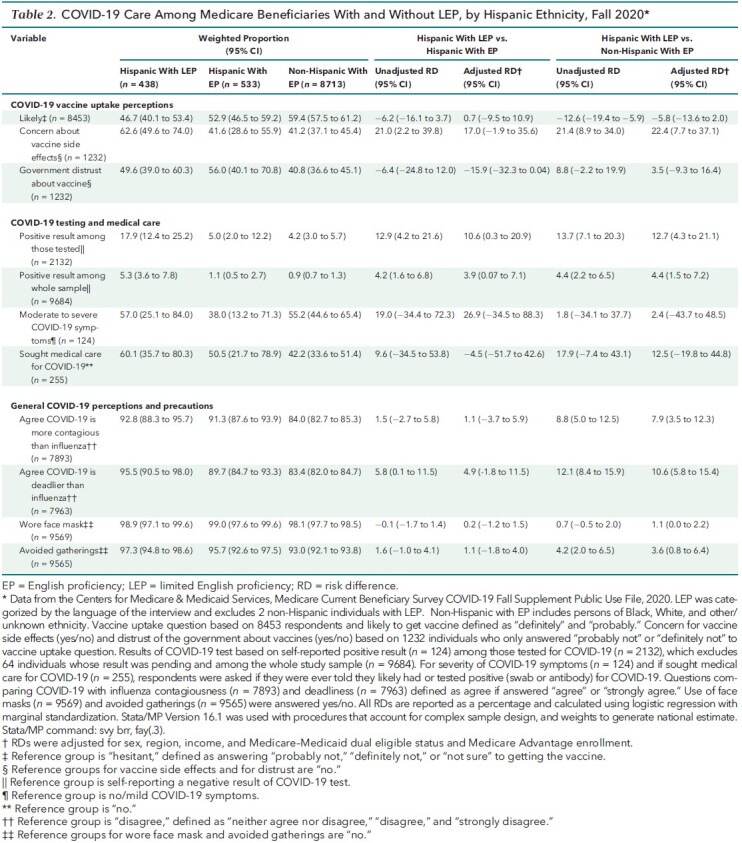
Hispanic adults with LEP reported high rates of COVID-19 test positivity (17.9% of those tested [CI, 12.4% to 25.2%] and 5.3% overall [CI, 3.6% to 7.8%]) and, in adjusted analyses, were more likely than non-Hispanic adults with EP to recognize that COVID-19 is more contagious and deadly than influenza and to report avoiding large gatherings (Table 2).
Discussion: Among Medicare enrollees, persons with LEP were less likely to intend to get vaccinated, despite being insured and having higher test positivity rates and knowledge of the seriousness of COVID-19. Concern about side effects was a major driver of vaccine hesitancy. Although reduced health literacy, which is more common among persons with LEP, may influence vaccine hesitancy, we lacked data to explore this. Adjustment for sociodemographic differences (most importantly, income) attenuated the language-based disparity in vaccine hesitancy, suggesting that lower income among adults with LEP (which LEP may cause) explains at least some of this disparity.
Our findings support efforts by Medicare and Medicare Advantage plans to communicate the risks and benefits of COVID-19 vaccines to this high-risk group through linguistically and culturally appropriate outreach and engagement in care (5). Clinicians, public health officials, and Spanish-language news media also have roles to play in overcoming vaccine hesitancy in the older population with LEP.
Footnotes
This article was published at Annals.org on 26 October 2021.
References
- 1. Reitsma MB , Claypool AL , Vargo J , et al. Racial/Ethnic disparities in COVID-19 exposure risk, testing, and cases at the subcounty level in California. Health Aff (Millwood). 2021;40:870-878. [PMID: ] doi: 10.1377/hlthaff.2021.00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The CMS Equity Plan for Improving Quality in Medicare. Centers for Medicare & Medicaid Services Office of Minority Health; 2015:19. Accessed at www.cms.gov/about-cms/agency-information/omh/omh_dwnld-cms_equityplanformedicare_090615.pdf on 7 September 2021.
- 3.Salame R. Limited English skills can mean limited access to the COVID-19 vaccine. Slate. 30 April 2021. Accessed at https://slate.com/news-and-politics/2021/04/covid-19-vaccine-for-non-english-speakers.html on 7 September 2021.
- 4. Fuchs JR , Fuchs JW , Tietz SE , et al. Older adults with limited English proficiency need equitable COVID-19 vaccine access. J Am Geriatr Soc. 2021;69:888-891. [PMID: ] doi: 10.1111/jgs.17069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandez A. We need to get more Latinx people vaccinated. Here's how. AAMC. 11 February 2021. Accessed at www.aamc.org/news-insights/we-need-get-more-latinx-people-vaccinated-heres-how on 7 September 2021.


