Abstract
Background
CapsoCam Plus is a capsule endoscopy (CE) system that utilizes four cameras to capture a panoramic view. This has theoretical advantage over conventional forward-viewing CE with limited field of view. Its ease of administration without requiring any additional equipment during the recording also provides a unique opportunity for patients to self-administer the test. We aimed to evaluate real-life experience using this novel system and to determine feasibility of a remote access program.
Methods
Retrospective chart review was conducted for consecutive adult outpatients who underwent CE using CapsoCam Plus. Patients with significant challenges for in-person procedures were selected for remote access through mail courier services. Gastric transit time, small bowel transit time, completion rate, diagnostic yield and adverse events were compared between remote access versus usual practice.
Results
Ninety-four patients (52.1% male) were included, with 28 in remote access program. Most common indication was gastrointestinal bleeding (85.1%). Complete examination was achieved in 87 patients. Five (5.3%) patients’ capsule remained in stomach during the recording, while two (2.1%) patients missed capsule retrieval. Median small bowel and gastric transit times were 231.9 (interquartile range [IQR] 169.5–308.2) and 27.6 (IQR 13.8–63.5) minutes, respectively. Diagnostic yield was 23.4%. There was no difference in completion rate or transit times between two groups, but diagnostic yield was higher in remote access group (odds ratio 3.80, 95% confidence interval 1.28–11.31). One patient required elective endoscopic retrieval of capsule.
Conclusion
CapsoCam Plus can be safely administered remotely with a high degree of success, which may facilitate timely investigations while limiting nonessential physical interactions during pandemic.
Introduction
Capsule endoscopy (CE) is a noninvasive diagnostic tool for patients with suspected or established small bowel (SB) diseases that are otherwise inaccessible by conventional endoscopies. In most centers, CE is primarily used to investigate obscure gastrointestinal bleeding (OGIB), but its use has also expanded to other indications including inflammatory bowel disease (IBD), celiac disease and surveillance of inherited polyposis syndrome (1). CE and radiological studies are often complementary in the evaluation of OGIB and IBD, but given CE’s ability to directly visualize the mucosa and detect subtle abnormalities, it generally has an increased diagnostic yield (2,3).
Most CE models implement a forward-facing camera in which the light source and image sensor move in a singular direction. The limited field of view potentially limits SB visualization (4,5). Panoramic view has been suggested to improve overall SB visualization and potentially improve diagnostic yield by minimizing ‘miss rates’ (6). The CapsoCam Plus (CapsoVision, Inc. Saratoga, USA) is a novel CE system that utilizes four lateral-viewing 90-degree cameras in its mid-section to achieve a 360-degree panoramic perspective (5). This CE system has operating time exceeding 15 hours and is able to capture images at variable rates between three and five frames per second per camera, depending on its transit speed. Despite the theoretical advantages of panoramic CE, few studies to-date have demonstrated similar diagnostic yield as forward-facing CE (7–10).
A more distinctive feature of CapsoCam Plus is the mode of data storage. Unlike other SB CE systems that wirelessly transmit images to an external wearable recorder during the study, CapsoCam Plus stores images internally within the capsule. As a result, the capsules must be retrieved and returned upon excretion in order to download and review the images. Without requiring an external recorder, this design can improve patient comfort during the study and limit maintenance expenses (5,6). More importantly, the simple set-up with internal image storage creates a unique opportunity for patients to administer the CE independently at home.
We aimed to evaluate real-life experience using CapsoCam Plus for patients living in rural areas and to determine feasibility (as measured by return rates of capsule) of a remote access program for patients who are unable to attend in-person visits.
Methods
Study Design and Patients
This study is a retrospective chart review of consecutive outpatient SB CE conducted using CapsoCam Plus (CapsoVision, Inc.) between January 1, 2016 and May 31, 2020 at a university-affiliated outpatient gastroenterology clinic in Vancouver, Canada. Patients were selected for CapsoCam Plus if they were unable to either attend clinic visit in-person or stay in Vancouver to return equipment the next day. Data extracted include: basic demographics (i.e., age and gender), indication, extent of examination, gastric transit time (time between first duodenal image and first gastric image), small bowel transit time (time between first cecal image and first duodenal image), capsule finding, adverse events, capsule retention (retained capsule after 14 days), capsule recovery rates and recommendations. The study was approved by University of British Columbia Research Ethics Board.
Procedure
All patients had previous endoscopic exams including colonoscopy and endoscopy at least once; patients with previous surgery were not excluded. Patients with obstructive symptoms all had CT scans to exclude strictures.
All patients started clear liquid diet at 12 PM the day before procedure until 2 hoursbefore capsule intake. Bowel preparation was administered in the form of 2L polyethylene glycol plus electrolytes solution the evening before procedure. Patients could resume clear liquids and light meal 2 and 5 hours after capsule ingestion, respectively. Essential medications could be taken until 2 hours before, or 2 hours after capsule ingestion. Bisacodyl 10mg was administered orally at 12 hours.
CapsoRetrieve (CapsoVision, Inc.), a capsule retrieval kit, was provided to every patient along with the capsule endoscope. The retrieval kit contains single-use accessories for the collection, storage and transportation of the excreted capsule endoscope. Patients were provided verbal and written instructions on how to activate and retrieve the capsule. Clinicians were available to answer questions during and after the procedure.
Patients were instructed to record the time and date of capsule ingestion and excretion. Retrieved capsules were returned via courier service to the clinic, where they were cleaned and disinfected as per manufacturer’s cleaning process (11) before image download to a workstation for review by a single experienced endoscopist.
Remote Access Patients
All patients were assessed during initial consultation either in-person or via telehealth. A pilot program of remote access CE via mail courier was initiated for patients in rural areas who had significant challenges attending an in-person visit for CE. Patients were selected based on not only geographical location, but also pretest probability based on clinical history and anticipated adherence to medical instructions; otherwise, patients were encouraged to attend clinical visit in person as per usual practice.
Statistical Analysis
Baseline characteristics were summarized using descriptive statistics: categorical variables were described in frequency and percentage, while continuous variables were expressed as mean and standard deviation (SD), as well as median and interquartile range (IQR). Comparisons of baseline characteristics between the two groups were conducted using Wilcoxon rank sum test, chi-square test or Fisher’s exact test, as appropriate. GTT/SBTT and CR were compared using Cox regression model and logistic regression model, respectively (with and without adjusting for potential confounders including age, gender and indication). A P value < 0.05 was considered statistically significant. All statistical analyses performed using STATA 15 (STATA Corp., College Station, TX).
Results
Subject Demographics
Ninety-four patients, including 49 (52.1%) male, were included. Median age was 63.5 (IQR 53–73) years (Table 1). Gastrointestinal bleeding was the most common indication (n = 80, 85.1%). Sixty-six (70.2%) patients completed CE following an in-person clinic visit (Group A), while 28 (29.8%) patients completed CE remotely (Group B), with the majority of the remote CE (n = 21, 75%) performed during COVID19 pandemic.
Table 1.
Basic demographics
| All | Group A (Usual) | Group B (Remote) | P-value | |
|---|---|---|---|---|
| Sample size | 94 | 66 | 28 | |
| Age, years | ||||
| Median (IQR) | 63.5 (53–73) | 62 (52–74) | 65 (53–73) | 0.9703 |
| Mean ± SD | 62.3 ± 14.4 | 62.7 ± 13.4 | 62.2 ± 14.8 | |
| Male, n (%) | 49 (52.1%) | 36 (54.6%) | 13 (46.4%) | 0.471 |
| Indication, (%) | ||||
| GI bleeding | 80 (85.1%) | 55 (83.3%) | 25 (89.3%) | 0.823 |
| IBD | 1 (1.1%) | 1 (1.5%) | 0 (0%) | |
| Other* | 13 (13.8%) | 10 (15.2%) | 3 (10.7%) |
*Diarrhea (3), polyp surveillance (2), abdominal discomfort (8).
GI, Gastrointestinal; IBD, Inflammatory bowel disease; IQR, Interquartile range; SD, Standard deviation.
Completion Rate
Of 94 CEs performed, 87 (92.3%) were completed and reviewed. The concern for ‘capsule’ loss in our patient group was only 2%. In both cases, the patients forgot to use the retrieval kit outside of home setting. Reasons for incomplete study included gastric retention for the duration of recording (n = 5, 5.3%) and missed retrieval (n = 2, 2.1%, both from group A). One of the patients experienced prolonged gastric retention and required endoscopic retrieval of capsule in setting of previous pyloric stenosis and vertical band gastroplasty; the others excreted the capsule spontaneously within 48 hours. There was no significant difference between the two groups in CR (Odds ratio [OR] 1.07, 95% confidence interval [CI] 0.19–5.85, P = 0.942), even after adjusting for potential confounders (OR 1.09, 95%CI 0.20–6.03, P = 0.92).
Transit Times
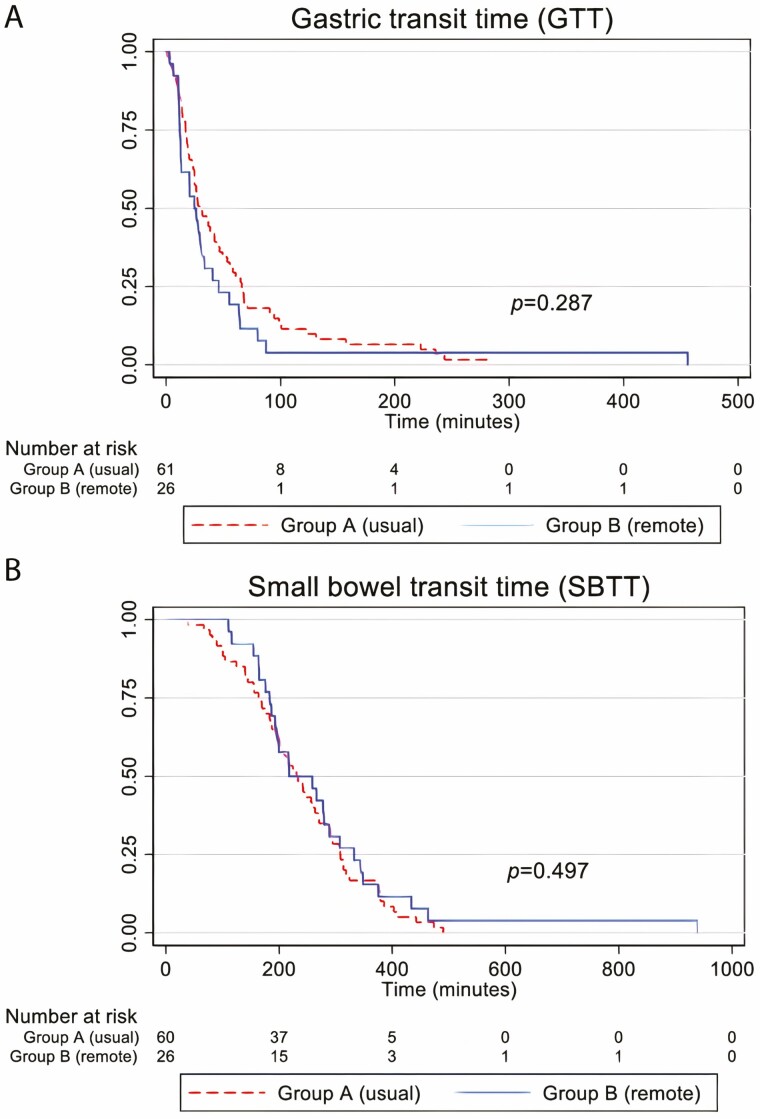
Patients whose capsule remained in stomach for the duration of recording were excluded. Median GTT was 27.6 (IQR 13.8–63.5) minutes. There was no significant difference in GTT between the two groups (hazard ratio [HR] 1.29, 95%CI 0.81–2.07, P = 0.287), and after adjusting for potential confounders (HR 1.16, 95%CI 0.71–1.89, P = 0.545; Figure 1a).
Figure 1.
Kaplan Meier curves of standard and remote access patients undergoing capsule endoscopy.
One additional patient in Group A was excluded from calculation of SBTT given history of prior small bowel surgery. Median SBTT was 231.9 (IQR 169.5–308.2) minutes. There was no significant difference in SBTT between the two groups (HR 0.85, 95%CI 0.53–1.36, P = 0.497), and after adjusting for potential confounders (HR 0.81, 95%CI 0.50–1.31, P = 0.393; Figure 1b).
Capsule Endoscopy Findings
Overall diagnostic yield was 23.4% (n = 22), with 11 patients from each group having positive yield. Mucosal changes, such as ulceration/erosions and blunted/coarsened villi, in the small bowel (n = 11) and stomach (n = 1) were the most frequent findings, followed by vascular lesions/fresh blood (n = 7) (Table 2). Group B had a higher diagnostic yield compared to that of Group A (OR 3.33, 95%CI 1.21–9.20, P = 0.020) on univariate analysis, which remained significant after adjusting for potential confounders (OR 3.80, 95%CI 1.28–11.31, P = 0.016).
Table 2.
Capsule endoscopy findings
| All, n (%) | Group A, n (%) | Group B, n (%) | |
|---|---|---|---|
| Normal | 65 (69.1) | 50 (75.8) | 15 (53.6) |
| Fresh blood | 2 (2.1) | 1 (1.5) | 1 (3.6) |
| Vascular lesion | 5 (5.3) | 1 (1.5) | 4 (14.3) |
| Erosion, ulcer, or blunted villi | 12 (12.8) | 9 (13.6) | 3 (10.7) |
| Polyp/mass | 3 (3.2) | 0 (0) | 3 (10.7) |
| Not retrieved | 2 (2.1) | 2 (3.0) | 0 (0) |
| Did not exit stomach | 5 (5.3) | 3 (4.5) | 2 (7.1 |
Adverse Events
No adverse events occurred except for one case of gastric retention described above. For the four patients whose capsule remained in stomach for the duration of the recording, capsules were excreted and retrieved after mean duration of 30.9 ± 10.6 hours (range 22.6–46.5 hours).
Discussion
This study confirms that with appropriate patient selection (all patients had consults- either in person or via telehealth), there is a very high completion rate of these studies. One of the major concerns for using CapsoCam Plus in the past has been the fact that patients must recover it. Not only did we demonstrate that virtually all patients in this study recover the capsule appropriately, we also demonstrated that this could be done remotely with high rates of success and no difference in performance characteristics of the capsules (i.e., completion rate and transit times). In both instances of capsule loss (2%), the patients forgot to use the retrieval kit outside of the home. Otherwise, image acquisition was appropriate in the entire group of patients. The advantage of accessing patients remotely includes significant cost savings to patients living in rural areas in terms of travel expenses. In addition, this mode of examination limits physical interaction between care providers and patients where possible, which has become critical during the COVID-19 crisis.
Previous studies utilizing panoramic CE demonstrated diagnostic yields between 40% and 60% depending on the indication (6,7,9,10). In our study, the overall diagnostic yield was modest at 23.4%. The yield for CE depends highly on patient selection, and in this study, patients were carefully selected to ensure capsule recovery. Therefore, patients with severe and acute bleeding were not entered as commonly as those with chronic anemia and occult bleeding subsequently resulting in a lower yield due to selection bias. Traditionally, CE has been limited to tertiary care centers as it is relatively more expensive. However, as time and experience evolved, it has become clear that the cost difference between repeating conventional endoscopic procedures (i.e., esophagogastroduodenoscopy, colonoscopy and push enteroscopy) versus CE has become marginal. Therefore, we presently promote consultation and access to CE at an earlier stage to try to exclude significant disease and adopt supportive management earlier in the process (i.e., iron supplementation and/or clinical monitoring).
Capsule retention is defined as persistent presence of capsule within the digestive tract after a minimum of 2 weeks and required directed intervention for its removal (12). Previously reported capsule retention rates varied between 2.1% and 8.2% depending on the indication for CE, with the highest rate among patients with established diagnosis of IBD (13). In this study, five capsules (5.3%) remained in stomach for the duration of the recording. Four patients’ capsules passed spontaneously within 2 days and underwent repeat CE with forward-viewing capsules without issues. One patient with remote history of pyloric stenosis and vertical band gastroplasty, but no other upper GI symptoms, required endoscopic retrieval of retained capsule after 76 days. The actual capsule retention rate (1/94 = 1.1%) was very low in this group of patients given that majority of the patients underwent CE for GI bleeding. Even though CapsoCam Plus (31 mm × 11 mm) (14) is slightly larger in size compared to other forward-viewing capsules, capsule size has not been shown to correlate with risk of capsule retention (15).
There are a few limitations in this study, the first of which is the retrospective design. We attempted to address potential confounding through statistical analyses, but residual confounding remains possible. Selection bias also exists given that patients in remote access (Group B) were selected based on characteristics deemed to make them more likely successful candidates for the program, which could explain the higher DY in this group. Moreover, small sample size may not be adequate to detect the difference in completion/retrieval rates between the two groups. The power of the study is limited by the number of patients we have performed this capsule on. However, the goal of this study was to assess feasibility, not outcomes. Additionally, some patients do not have capacity to follow all the necessary steps to collect the capsule and those patients were moved to a different capsule procedure. Although CapsoCam Plus can be performed remotely, this specific indication has not yet received approval in most countries.
We have shown that remote access CE can be done safely with high capsule recovery rate. Remote access patients can be managed via telehealth and the capsule can be sent by courier thereby saving the patient the travel to a different location. This offers both patients and physicians a unique alternative for investigations that will advance patient care; particularly during crisis times like COVID-19, where physical interaction needs to be limited.
Funding
No funding source was utilized as this was a retrospective study.
Conflict of Interest: The authors declare no conflict of interest.
References
- 1. Enns RA, Hookey L, Armstrong D, et al. Clinical practice guidelines for the use of video capsule endoscopy. Gastroenterology 2017;152(3):497–514. [DOI] [PubMed] [Google Scholar]
- 2. Kopylov U, Yung DE, Engel T, et al. Diagnostic yield of capsule endoscopy versus magnetic resonance enterography and small bowel contrast ultrasound in the evaluation of small bowel Crohn’s disease: Systematic review and meta-analysis. Dig Liver Dis 2017;49(8):854–63. [DOI] [PubMed] [Google Scholar]
- 3. Wang Z, Chen JQ, Liu JL, et al. CT enterography in obscure gastrointestinal bleeding: A systematic review and meta-analysis. J Med Imaging Radiat Oncol 2013;57(3):263–73. [DOI] [PubMed] [Google Scholar]
- 4. Friedrich K, Gehrke S, Stremmel W, et al. First clinical trial of a newly developed capsule endoscope with panoramic side view for small bowel: A pilot study. J Gastroenterol Hepatol 2013;28(9):1496–501. [DOI] [PubMed] [Google Scholar]
- 5. Koulaouzidis A, Dabos KJ. Looking forwards: Not necessarily the best in capsule endoscopy? Ann Gastroenterol 2013;26(4):365–7. [PMC free article] [PubMed] [Google Scholar]
- 6. Tontini GE, Wiedbrauck F, Cavallaro F, et al. Small-bowel capsule endoscopy with panoramic view: Results of the first multicenter, observational study (with videos). Gastrointest Endosc 2017;85(2):401–8.e2. [DOI] [PubMed] [Google Scholar]
- 7. Branchi F, Ferretti F, Orlando S, et al. Small-bowel capsule endoscopy in patients with celiac disease, axial versus lateral/panoramic view: Results from a prospective randomized trial. Dig Endosc 2020;32(5):778–84. [DOI] [PubMed] [Google Scholar]
- 8. Chetcuti Zammit S, McAlindon ME, Sidhu R. Panoramic versus axial small bowel capsule endoscopy in overt obscure gastrointestinal bleeding. Dig Endosc 2020;32(5):823. [DOI] [PubMed] [Google Scholar]
- 9. Zwinger LL, Siegmund B, Stroux A, et al. CapsoCam SV-1 Versus PillCam SB 3 in the detection of obscure gastrointestinal bleeding: Results of a prospective randomized comparative multicenter study. J Clin Gastroenterol 2019;53(3):e101–6. [DOI] [PubMed] [Google Scholar]
- 10. Pioche M, Vanbiervliet G, Jacob P, et al. ; French Society of Digestive Endoscopy (SFED) . Prospective randomized comparison between axial- and lateral-viewing capsule endoscopy systems in patients with obscure digestive bleeding. Endoscopy 2014;46(6):479–84. [DOI] [PubMed] [Google Scholar]
- 11. CapsoVision. Instruction for use CapsoCam Plus (IFU-2796 Rev: C). https://capsovision.com/wp-content/uploads/2019/10/IFU-2796C_CapsoCam-Plus.pdf. Published 2019. Accessed June 29, 2020.
- 12. Cave D, Legnani P, de Franchis R, et al. ; ICCE . ICCE consensus for capsule retention. Endoscopy 2005;37(10):1065–7. [DOI] [PubMed] [Google Scholar]
- 13. Rezapour M, Amadi C, Gerson LB. Retention associated with video capsule endoscopy: Systematic review and meta-analysis. Gastrointest Endosc 2017;85(6):1157–68.e2. [DOI] [PubMed] [Google Scholar]
- 14. CapsoVision. CapsoCam Plus Specifications - CapsoVision US. https://capsovision.com/physician-resources/capsocam-plus-specifications/. Published 2020. Accessed June 27, 2020.
- 15. Rondonotti E. Capsule retention: Prevention, diagnosis and management. Ann Transl Med 2017;5(9):198. [DOI] [PMC free article] [PubMed] [Google Scholar]