Abstract
The COVID-19 pandemic response has had a significant impact on the general population’s ability to participate in their communities. Individuals with disabilities, an already socially disadvantaged population, are more vulnerable to and have likely been disproportionately impacted by COVID-19 response conditions. Yet, the extent to which the daily community living activities of people with disabilities have been impacted is unknown. Thus, this study assesses their travel behavior and community living during the COVID-19 pandemic conditions compared with those of the general population.
A web survey was conducted using Qualtrics’s online panel data (respondents included 161 people with any type of disability and 232 people without a disability). Regression models found that people with disabilities reduced their daily travel to a greater extent but at varying degrees, depending on the destination types and travel modes. Reductions in taxi rides (including ride-hailing services) were most significant among people with cognitive and sensory (e.g., vision and hearing) disabilities. By place type, cognitive disability was associated with a trip reduction for multiple destination types—grocery, restaurants, outdoor recreation, indoor recreation, and healthcare providers. Findings from this study could contribute to decision- and policy-making in planning, transportation, and community services during the remainder of the COVID-19 pandemic, in future major public health crises, and post-COVID, because the adjustments in travel behavior and community living might be longer-term.
Keywords: Individuals with disabilities, Disabled people, Activities of daily community living, Pandemic
1. Introduction
Community participation is vital to health, well-being, self-determination, and quality of life (Christensen and Byrne, 2014, White and Summers, 2017). COVID-19 has negatively impacted individuals’ ability to participate in their communities, especially those who are physically and mentally vulnerable (Pfefferbaum & North, 2020). In addition to the challenges faced during COVID-19, people with disabilities are simultaneously dealing with existing social disadvantages. This combination can heighten vulnerability and lead to disproportionate effects (Armitage and Nellums, 2020, Constantino et al., 2020, Pineda and Corburn, 2020). Yet, there is limited evidence documenting the extent to which activities of daily community living (ADCL) for people with disabilities have been impacted. Consequently, there is a lack of evidence-based decision-making about interventions to address challenges related to employment, housing, community services, planning/transportation, recreation, social engagement, and education.
The purpose of this exploratory empirical study is to assess ADCL of people with disabilities during COVID-19 pandemic conditions, compared to the general population during the same period. For these comparisons, we conducted a web survey using Qualtrics’s online panel data (respondents included 161 people with any type of disability and 232 people without a disability) and analyzed differences using descriptive and inferential statistics. Survey development was based on a proposition that people with disabilities would have experienced a greater impact on travel compared with the general population. For example, public transit use for people with disabilities would decrease due to a higher association of medical conditions such as vulnerability to infection, increased risk of COVID spread on public transportation, and decrease in service of publicly available transportation services (Penfold et al., 2008, Jansuwan et al., 2013). The expected result would have been a higher reduction in daily travel and a greater modal shift than for people without disabilities. In general, we expect to find that moderating for the effects of socio-demographics, COVID-19 impacts will be more negative among people with disabilities, an already disadvantaged population.
We believe that the findings of this study will contribute to evidence-based decision- and policy-making during the remainder of the COVID-19 pandemic. Even more importantly, the practical implications of our findings are relevant post-COVID because pandemic-related adjustments in travel behavior and community living patterns may well manifest for the longer term, and this difficult period may result in greater attention to the long-standing disadvantages faced by those with disabilities.
2. Literature review
Given the importance of participation in one’s community for health and well-being, self-determination, and quality of life (Christensen and Byrne, 2014, White and Summers, 2017), the very nature of the response to the COVID-19 pandemic has had a significant impact on the general population. The pandemic response’s protective measures have altered the general population’s activities of daily community living, including basic activities necessary for an individual to live independently in their community, thus contributing to isolation (Palgi et al., 2020, Probst et al., 2020), high psychological distress (Wang et al., 2020, Park et al., 2020), financial stress (Chakraborty & Chatterjee, 2020), and depression and anxiety (Madani et al., 2020). These conditions have long been disproportionately experienced by people with disabilities. This is due to greater barriers to community participation, self-determination, and well-being. Other authors suggest that people with disabilities have experienced such effects of the COVID-19 pandemic as ‘everyday emergencies’ long before the pandemic struck (Pineda & Corburn, 2020). With COVID-19, these everyday emergencies have only been exacerbated.
People with disabilities may experience double jeopardy as pandemic responses impact their ADCLs, resulting in more severe COVID-19 outcomes than those brought on by their disability and health conditions alone (Abedi et al., 2021, Armitage and Nellums, 2020, Constantino et al., 2020, Pineda and Corburn, 2020, WHO., 2020). Often people with disabilities are already at increased risk for contracting COVID-19 because of their disability and/or underlying medical conditions, with many experiencing more severe outcomes for the same reasons (Karaye and Horney, 2020, Landes et al., 2020, Turk et al., 2020). Additionally, many people with disabilities are dependent upon direct personal services and support, such as personal care providers, thereby increasing potential exposure, especially when compared with the general population. Drum et al. (2020) suggest that nearly one-quarter of people with disabilities have reduced access to these personal services and supports because of the pandemic response. In addition, congregate care settings, such as residential group homes or day habilitation programs, also increase vulnerability as they are less able to practice protective physical distancing, both from other residents and personal care providers (Landes et al., 2020, Sabatello et al., 2020). Furthermore, access to public awareness and education for people with hearing, visual, and cognitive disabilities is more limited (Pineda & Corburn, 2020), increasing their reliance on healthcare providers and systems for guidance (Drum et al., 2020). Compared with the general population, people with disabilities have, on average, less education, more economic, food, housing, and employment insecurity, and less internet access (Krahn et al., 2015), all of which are associated with increased pandemic response impacts on activities of daily community living. COVID-19 pandemic response measures have reduced access to continuity of care and social supports (e.g., food, housing, healthcare, and transportation) among people with disabilities, conditions which should not be viewed as an individual challenge but rather as a failure of land use and infrastructure planning (such as transportation planning) (Pineda & Corburn, 2020).
Transportation, which is both an ADCL and acts as a support for other ADCLs, is of particular concern among populations with disabilities. Travel is fundamental in order for people with disabilities to engage with their community for employment, goods and services, health, education, and social interaction (Christensen & Byrne, 2014). People with disabilities with increased access to travel report greater quality of life and lower levels of social isolation (Cvitkovich & Wister, 2001). Yet a key COVID-19 pandemic protective measure has been community mitigation through reduced interactions due to travel restrictions.
2.1. COVID-19 impacts on travel behavior
COVID-19 triggered unprecedented travel behavior change worldwide, including significant reduction of trips and modal shifts (Brough et al., 2020, Hamidi and Zandiatashbar, 2021, Hotle et al., 2020, Molloy et al., 2020). The early months of the pandemic caused a nearly 38 percent reduction in trips for both essential and non-essential trips (Hamidi & Zandiatashbar, 2021). Such decreases were not the same across all destination types; for instance, the reduction in park trips was substantially lower than essential trips (e.g., grocery and pharmacy trips). The difference in these behaviors may be due to perceived risks. Shamshiripour et al. (2020) showed that visiting hospitals and gyms/fitness centers had the highest perception of risk, whereas visits to family/friend homes or parks had the lowest risk perception. As a direct impact of the pandemic on travel behavior, participation in social and physical activities has been lowered, negatively impacting individuals’ well-being (Brooks et al., 2020, De Vos, 2020).
Other communicable respiratory disease outbreaks, such as SARS, H1N1, and MERS, changed travel behavior for the general public (Wen et al., 2005, Liu et al., 2011, Fenichel et al., 2013, Kim et al., 2017). Wen et al. (2005) reported that SARS influenced travel preferences and patterns by increasing outdoor activities and migration to suburbs and countryside. Related to H1N1 swine flu, Fenichel et al. (2013) showed that people are not only willing to pay for infection-free trips but also that their behavior shifts can be triggered by perceived risks, types of accessible transportation, and jurisdictional policies (e.g., stay-at-home orders). Kim et al. (2017) confirmed these factors after the MERS outbreak showed that fear of travel can result in a sharp decline in public transit.
Regardless of the kind of disease outbreak, perceived risk has also influenced mode choice. Troko et al. (2011) illustrated that using public buses and trams is considered an individual risk factor that significantly contributes to acquiring acute respiratory infections. Moreover, studies have shown that the perceived risks of traveling via transit and pooled ride-hailing are the highest among all modes of travel (Shamshiripour et al., 2020, Yıldırım and Güler, 2020). On the other hand, the perceived risks of traveling with personal vehicles, on foot, or on private bikes are the lowest (Shamshiripour et al., 2020). These findings signal substantial changes in individuals’ mode choice decision making, pushing them away from public transportation and toward more private modes.
While risk perception plays a critical role in travel behavior, geographic and demographic factors can also influence travel patterns. Hamidi & Zandiatashbar (2021) demonstrated higher trip reductions to grocery stores/pharmacies and transit stations in compact urban areas more than other locations, partially due to better home-delivery services. Moreover, the percentage of seniors who are more vulnerable to infections than younger people positively contributes to the trip reduction in trips to transit stations (Hamidi & Zandiatashbar, 2021). An inability to reduce reliance on public transportation is associated with lower-income employees who are also less capable of working remotely, whereas individuals with higher education could more easily substitute modes of transportation (Brough et al., 2020). This dichotomy suggests that public transport capacity cannot be unreasonably decreased because some captive riders lack alternative modes other than public transit, and thus, must have access to safe public transport for travel during the pandemic (Beimborn et al., 2003, De Vos, 2020).
The pandemic has had an even greater impact on individuals with travel-related disabilities. The occurrence of the pandemic may worsen the accessibility issues for people with disabilities (Eskytė et al., 2020). This could be the result of people with disabilities not being able to access required physical, occupational, speech, or other rehabilitation programs, interventions, and therapies as a direct consequence of the pandemic (Milicevic, 2020).
2.2. Conceptual framework and research questions
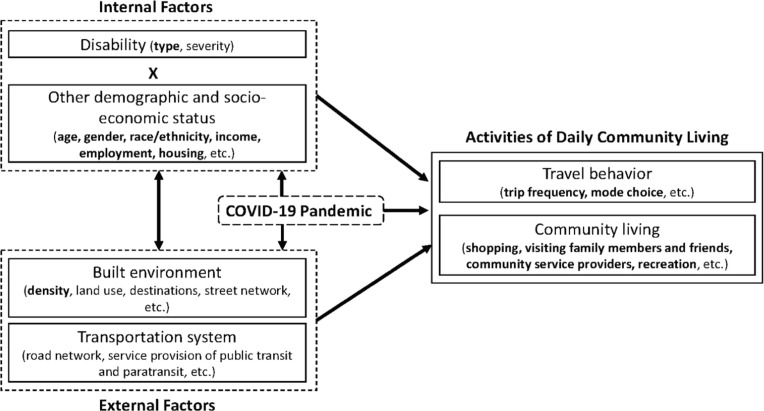
To the best of the authors’ knowledge, there is no empirical study exploring the impact of the COVID-19 pandemic on travel behaviors and community living of people with disabilities directly. Considering this gap and the expectation that this may not be the last of such events, we have developed a conceptual framework to facilitate our broad understanding of how internal and external factors have influenced travel behavior amid the pandemic (Fig. 1 ). As an exogenous, confounding factor, the pandemic and related conditions affect both the explanatory variables (internal and external factors) and the outcomes (travel behaviors and community living), or the lived experience of people with disabilities. For example, the pandemic simultaneously and directly impacted the demand of people with disabilities to travel as a result of the perception of increased risks to exposure to COVID-19 due to age, disability, etc. Reduced demand for traveling by people with disabilities may also have been due to changes in employment from pandemic-related reductions in service industry employment and/or a greater shift to remote employment (Internal Factor). In addition, reductions in public transit availability as a fixed-route service increased demand for paratransit service, thereby reducing some individuals’ ability to travel (External Factor), and imposed stay-at-home responses directly reduced the opportunity to physically visit family members and friends, in effect reducing the number of travel destinations available to people with disabilities (ADCL).
Fig. 1.
Conceptual framework of COVID-19 pandemic impacts on activities of daily community living of people with disabilities (note: factors in bold are included in this study).
Internal factors include demographics and socioeconomic status (e.g., age, gender, race/ethnicity, income and employment status, and housing type). Disability status and type (e.g., mobility, sensory, cognitive) are key internal factors of interest in this study. Disability is a complex social phenomenon that involves the interaction of individuals with specific functional competencies (perhaps due to a physical impairment) with their identity, their physical and social surroundings, and cultural and normative systems (Altman, 2001). As a result, disability can only be defined empirically when reduced to focus on a specific aspect of experience (Altman, 2001). Differences in how these experiences are defined and associated with the phenomena of disability as a heterogeneous group make it difficult to effectively collect data that are representative (Fujiura & Rutkowski-Kmitta, 2001). For these reasons, data on disabilities are difficult to collect and understand (Blaser & Ladner, 2020). In this study, we define disability as self-reported limitations in functional abilities related to one or more of the broad disability categories used in the American Community Survey and U.S. Census research: hearing difficulty, vision difficulty, cognitive difficulty, ambulatory difficulty, self-care difficulty, and independent living difficulty (US Census Bureau, 2020b).
In our framework, external factors include the built environment and COVID-19-related travel restrictions (e.g., travel bans, stay-at-home orders, limited availability of public transportation services). The impacts of the built environment on travel behavior are well-documented in the literature, often being referred to as “D variables,” such as development density, land use diversity, street network design, distance to transit, and destination accessibility (Boarnet, 2011, Ewing and Cervero, 2010). In this study, we explore the impacts of a few select external factors, such as using population density at a zip code level. Urban communities with higher density levels provide better access to public transit and healthcare facilities. Travel restriction policies and other built environment characteristics are not included in this study due to the limited national data availability and the cross-sectional nature of the research design. Studies have shown differences in COVID-19 case counts and severity between urban and rural communities (CDC, 2020).
Our conceptual framework guides the three exploratory questions in this study. First, have people with disabilities reduced their daily travel to a greater extent during COVID-19 than people without disabilities (Q1)? Second, if trip reductions have occurred due to COVID-19, have people with disabilities made a more significant shift on certain modes (Q2)? Third, are the changes in travel behavior and community living different between people with and without disabilities by destination type (Q3)?
3. Data and methods
With the global reach of COVID-19, our data collection was intended to reach a national audience. We adopted the Qualtrics survey platform as (1) their panels have consistently proven to be one of the better demographic representations (Boas et al., 2020) and (2) our institution has previously contracted with Qualtrics, ensuring a more rapid contractual process for securing data for this study during the pandemic.
The recruitment panel was set up to facilitate quotas on three distinct demographic variables: First, the representation of people with and without disabilities (between 50/50 and 60/40, respectively). The type of disability was not restricted (e.g., cognitive, motor, auditory, vision). Second, an age quota with no less than 20% over the age of 65, as the current census identifies this group as covering roughly 16% of the population (US Census Bureau, 2020a). Third, we aimed for a gender balance between those identifying as female or male (between 50/50 and 60/40, respectively). We did not establish quotas for the race, community type (urban/rural), or geographic region in order to expedite the survey and get results in a timely manner. A pilot survey was conducted in late October 2020 (with about 200 participants), with minor changes augmenting the survey eventually used for this study.
The data presented in this study were collected from November 30 to December 08, 2020. The survey was open nationally, with no geographic limitations. Geographic data were collected by asking a zip code of primary residence. These data were cross-referenced with socio-demographic census data from the National Historical Geographic Information System (Manson et al., 2020), as well as zip code, state and region, and urban area data (US Census Bureau, 2020d).
After screening for inconsistent responses, our final sample from Qualtrics’s online panel data consisted of 161 people with any type of disability and 232 people without a disability. Respondents reside in 48 different states with the following regional distribution: Northeast (17%), Midwest (22%), South (43%), West (18%), aligning with the 2019 Census Region population of 17%, 21%, 38%, and 24%, respectively (US Census Bureau, 2020e). Among these participants, 64% live in a Census-designated urban area. A chi-squared test of independence of region with disability/non-disability status shows no statistical significance ( = 2.76, df = 3, p = .43).
We expected that our 60-question survey would take about 15 min to complete, and indeed, the average time of completion was 14 min. The survey was divided into five sections: eligibility, demographics, internet use, travel behavior, and social relationships. This paper focuses primarily on results from the eligibility, demographics, and travel behavior sections. Eligibility and demographics questions included collecting age, type of disability, race, gender, income, and employment status. For these variables (including disability types), we drew from the American Community Survey 2014–2018 Questionnaire (US Census Bureau, 2020c), with inspiration on employment status provided from Critical Care Nutrition (Critical Care Nutrition, 2020). For travel behavior questions, we collected data on the frequency of weekday trips, frequency of modes, and places visited. Each participant was asked to identify or estimate their activities “pre-COVID,” “during COVID,” and “post-COVID,” where 2019 represents “pre-COVID,” 2020 after the COVID-19 outbreak represents “during COVID,” and the time when COVID-19 is no longer a concern in the U.S. represents “post-COVID.” We incorporated feedback from our advisory board (consisting of eight people with a variety of disabilities). All survey data collection was approved by Utah State University’s Institutional Review Board #11509.
As noted in our conceptual framework, collecting representative data of people with disabilities can be challenging (Blaser and Ladner, 2020, Fujiura and Rutkowski-Kmitta, 2001). Because of these challenges, we ensured that our sample provided an adequate representation of the two focus populations (people with and without disabilities). In our pilot study, we intentionally chose not to include a screener or Instructional Manipulation Check (Oppenheimer et al., 2009) because these may induce bias (Clifford and Jerit, 2015, Anduiza and Galais, 2017). But our pilot data of about 200 individuals (half with a disability) demonstrated significant anomalies for those identifying as having a disability. Therefore, we instituted a validation check at the end of the survey, which required individuals to confirm their disability using the same eligibility screener question as at the beginning of the survey. To address potential biases where individuals may have made an inconsistent response, we reduced the consistency to a 50% accuracy of responses. For instance, this eliminates individuals who indicated a vision disability in the eligibility question, but then hearing disability in the validation question. With this validation completed, we discovered that about a quarter of participants indicating they had disability were inconsistent with what kind of disability they identified. While we may have eliminated some individuals who had a genuine disability, we believe most of those eliminations were due to individuals who may have been straight-lining (Vannette & Krosnick, 2014) or did not actually possess a disability. We are confident that our technique, which merely asks an individual to confirm their condition, provides a means to ensure more accurate data collection and representation of those disabilities.
Data collected were used to generate descriptive statistics as a first step. We calculate changes in daily trip frequency between two time periods (pre-COVID vs. during COVID) and compare it between people with and without disabilities (Q1). Such differences are compared for each travel mode (Q2) and place type (Q3). We ran bivariate inferential statistics, such as t-tests, for continuous variables (e.g., daily trip frequency between the two groups) and Chi-square tests of independence for categorical variables (e.g., educational attainment between the two groups) to see if the mean differences are statistically significant.
For the next analysis phase, multiple regression models were developed to answer different questions following the conceptual framework that estimates travel behavior outcomes by internal and external factors. The first set of models estimates daily trip frequency in a certain period (e.g., during COVID) after controlling for the same measure in a previous period (e.g., pre-COVID), so that the model outcome shows changes between the two (Q1). Independent variables include both internal factors (e.g., disability status and type, gender, age, race/ethnicity, employment status, household characteristics) and external factors (e.g., population density of a zip code area, urban area status). We also model trip frequency change by place type (Q2) and travel model (Q3). Given a relatively small sample and many independent variables, we selected a set of variables for each model after an exhaustive search. After checking every possible model, the final model was chosen with the lowest Akaike Information Criterion (AIC) value. We used the regsubsets function in the R package leaps (Lumley, 2020). We tested for multicollinearity for each model. The highest variance inflation factor (VIF) values across all models were lower than 2.0 below the standard ceiling value for multicollinearity of 5.0 (Daoud, 2017).
4. Results
4.1. Descriptive statistics
In our final sample of 393 respondents, 41.0% (n = 161) indicated at least one type of disability, which was categorized into a major disability type (sensory, cognitive, mobility, and others). Our two groups—people with and without a disability—were not demographically different except for their age, gender, and race/ethnicity (more older adults, male, and non-Hispanic Whites among the respondents with disabilities) at the statistical significance level (p<.05). Other characteristics (employment/student status, household income, housing type, etc.) were similar between the two groups. Table 1 shows mean value comparisons.
Table 1.
Mean values of variables between people with and without disabilities (n = 393; standard deviation in parenthesis for continuous variables). Note that those with disabilities may have multiple disability types.
| Variables | Total | No disability | With disability1 |
|---|---|---|---|
| Disability status dummy (1 = yes) | 41.0% | – | 100.0% |
| Disability type: Sensory | – | – | 43.5% |
| Disability type: Cognitive | – | – | 39.1% |
| Disability type: Mobility | – | – | 28.6% |
| Disability type: Others (e.g., self-care, independent living) | – | – | 37.3% |
| Most impactful disability type (1 = Sensory) | – | – | 31.1% |
| Most impactful disability type (1 = Cognitive) | – | – | 21.1% |
| Most impactful disability type (1 = Mobility) | – | – | 24.8% |
| Most impactful disability type (1 = Others) | – | – | 23.0% |
| Age (years)* | 41.8 (16.9) | 40.0 (15.9) | 44.5 (18.0) |
| Age dummy (1 = 65 years or older)* | 14.2% | 10.3% | 19.9% |
| Female dummy (1 = yes)** | 61.3% | 67.2% | 52.8% |
| Non-Hispanic White dummy (1 = yes)* | 65.9% | 61.6% | 72.0% |
| Worker status dummy (1 = full-time or part-time) | 50.4% | 52.2% | 47.8% |
| Educational attainment dummy (1 = bachelor’s degree or higher) | 32.6% | 31.5% | 34.2% |
| Household income (past 12 months) | |||
| Less than $10,000 | 13.0% | 13.8% | 11.8% |
| $10,000 to $14,999 | 4.3% | 4.7% | 3.7% |
| $15,000 to $24,999 | 13.5% | 11.6% | 16.1% |
| $25,000 to $34,999 | 11.2% | 10.3% | 12.4% |
| $35,000 to $49,999 | 13.7% | 12.5% | 15.5% |
| $50,000 to $74,999 | 13.0% | 13.8% | 11.8% |
| $75,000 to $99,999 | 8.9% | 9.9% | 7.5% |
| $100,000 to $149,000 | 8.4% | 8.2% | 8.7% |
| $150,000 to $199,999 | 3.6% | 2.2% | 5.6% |
| $200,000 or more | 3.6% | 4.7% | 1.9% |
| Don’t know | 6.9% | 8.2% | 5.0% |
| Category 1: poverty (1 = less than $25 K)2 | 30.8% | 30.2% | 31.7% |
| Category 2: low (1 = between $25 K and $50 K)2 | 24.9% | 22.8% | 28.0% |
| Household size | 2.9 (1.4) | 3.0 (1.5) | 2.8 (1.4) |
| Number of children | 0.6 (0.9) | 0.7 (0.9) | 0.6 (0.9) |
| Marital status dummy (1 = married or living with a partner) | 52.7% | 52.6% | 52.8% |
| Driver status dummy (1 = driver) | 82.7% | 81.0% | 85.1% |
| Student status dummy (1 = student) | 16.3% | 16.4% | 16.1% |
| Home ownership status dummy (1 = owner) | 51.7% | 51.3% | 52.2% |
| Housing type dummy (1 = single-family housing) | 63.6% | 66.8% | 59.0% |
| Population density (1000 people/square mile; zip code) | 6.3 (14.9) | 5.6 (13.4) | 7.3 (16.9) |
| Urban area dummy (1 = Census-designated urban area) | 64.9% | 64.5% | 65.6% |
. **: p < .01, *: p < .05, ^: p < .1 from an independent samples t-test for continuous variables and a chi-squared test for dummy variables.
. Income category thresholds were selected from the U.S. 2020 poverty guideline for a four-person household ($25,701) for the “poverty” group and the U.S. Department of Housing and Urban Development’s guideline of the low-income limits (80% of the area median family income) for the “low-income” group.
4.2. Daily trip frequency change between people with and without disabilities by mode
Our respondents reduced their weekday travels from 4.02 per day in 2019 (pre-COVID) to 2.96 per day in 2020 (during COVID) (Table 2 ). As a reference, the average numbers of daily trips from the 2017 National Household Travel Survey (pre-COVID) were 3.6 for non-disabled and 2.6 for disabled (Brumbaugh, 2018), which are slightly lower than our survey results. Differences might be due to outliers, particularly in our disabled group (the median trip frequency in our sample is 4 for non-disabled and 3 for disabled, which is closer to the national data), and potential errors regarding the retrospective survey. Regarding travel mode, the respondents reduced their uses of all modes of transportation (except for wheelchair uses among respondents with disabilities) at the p < .05 significance level.
Table 2.
Average trip frequency pre-COVID and during COVID-19 and changes between the two periods by travel mode (n = 393).
| Variables | Total | t-statistic (pre vs. during COVID)1 |
Non-disabled | Disabled | t-statistic (Non-disabled vs. Disabled)2 |
|---|---|---|---|---|---|
| Average daily trip frequency pre-COVID | 4.02 | – | 4.08 | 3.94 | 0.48 |
| Average daily trip frequency during COVID | 2.96 | – | 3.05 | 2.83 | 0.83 |
| Change in daily trip frequency | −1.06 | −8.46** | −1.03 | −1.11 | 0.30 |
| Change in automobile trip frequency | −0.51 | −7.11** | −0.37 | −0.71 | 2.42^ |
| Change in public transit trip frequency | −0.35 | −5.88** | −0.29 | −0.43 | 1.15 |
| Change in taxi (Uber/Lyft) trip frequency | −0.27 | −5.87** | −0.10 | −0.52 | 4.19** |
| Change in walking frequency | −0.27 | −3.53** | −0.13 | −0.47 | 2.24^ |
| Change in paratransit trip frequency3 | −0.14 | −2.30* | – | – | – |
| Change in wheelchair trip frequency3 | −0.01 | −0.20 | – | – | – |
: **: p < .01, *: p < .05, ^: p < .1 (paired samples t-tests).
: **: p < .01, *: p < .05, ^: p < .1 (independent samples t-tests).
. Changes in paratransit trips and wheelchair trips were only calculated for respondents with disabilities.
In general, there were no statistically significant differences in daily trip frequency between people with and without disabilities (p < .05), either pre- or during COVID. With respect to changes in trip frequency by travel mode, however, t-test results show that trip reduction was significantly different between the two groups for taxi trips (including ride-hailing services such as Uber and Lyft). COVID-19 also affected automobile trips and walking more negatively among people with disabilities, but only at a marginally significant level (p < .1). The use of paratransit services among people with disabilities was significantly reduced, shown in a one-sample t-test.
Regression models of trip frequency change during COVID-19 show additional trip reductions among the specific type of disabilities (Table 3 ). In the model, a positive coefficient value for a given mode means trip frequency increases during the pandemic for that mode. After controlling for other personal characteristics, people with cognitive disability decreased their paratransit uses and taxi trips (including Uber/Lyft rides) during the pandemic more than other groups at p < .05 significance level. Those with mobility disabilities reduced the overall daily trip frequency, automobile uses, and walking to a greater extent, but only at the marginal significance level (p < .1). Sensory disability (e.g., vision, hearing) is also marginally related to additional reduction in taxi/Uber/Lyft rides (p < .05) and walking (p < .1).
Table 3.
| Overall | Auto | Public transit | Para-transit2 | Taxi (Uber/Lyft) | Walk | |
|---|---|---|---|---|---|---|
| (Intercept) | −0.62 | 0.66* | 0.38** | 0.04 | 0.35** | 0.03 |
| Daily trip frequency (pre-COVID) | 0.48** | 0.69** | 0.50** | 0.63** | 0.64** | 0.73** |
| Disability (cognitive) | – | – | – | −0.29* | −0.41** | |
| Disability (mobility) | −0.64^ | −0.40^ | – | – | – | −0.43^ |
| Disability (sensory) | – | – | – | – | −0.24* | −0.38^ |
| Disability (others) | – | – | – | −0.17 | −0.20 | |
| Age (years) | 0.03** | −0.01^ | – | – | – | 0.01* |
| Age: over 65 (yes/no) | −0.90* | – | – | – | – | |
| Female (yes/no) | – | – | – | 0.21^ | – | – |
| Household income: low (yes/no) | – | 0.28^ | – | – | – | |
| Household size | 0.15* | – | – | – | – | |
| Number of children | – | – | – | −0.11* | −0.06 | |
| Driver status (yes/no) | – | 0.41* | −0.21^ | – | – | |
| Non-Hispanic White (yes/no) | – | – | −0.26** | – | −0.16* | |
| Worker status (yes/no) | 0.38 | – | – | – | – | 0.21 |
| Student status (yes/no) | 0.48 | −0.42* | 0.22^ | 0.28^ | −0.15 | |
| Bachelor’s degree or higher (yes/no) | −0.29 | – | – | – | – | |
| Single-family housing (yes/no) | – | 0.28^ | – | – | – | |
| Homeowner (yes/no) | – | – | – | – | −0.15* | −0.36* |
| Population density (1000 people/sq.mi.) | – | – | – | – | – | 0.01 |
| Urban area (yes/no) | – | −0.26^ | – | – | – | |
| Model fit statistics | ||||||
| - R-squared | 0.36 | 0.55 | 0.47 | 0.59 | 0.54 | 0.54 |
| - Adjusted R-squared | 0.34 | 0.54 | 0.47 | 0.57 | 0.53 | 0.53 |
| - AIC | 561.55 | 228.53 | −87.69 | −133.04 | −218.15 | 250.43 |
: **: p < .01, *: p < .05, ^: p < .1.
. The paratransit model was run only for respondents with disabilities (n = 161).
Among other personal and environmental variables, the overall daily trip frequency increased more (or more likely, decreased less) when a traveler was older (but not older than 65 years old) and lived in a bigger household. Car trips were positively associated with driver status and negatively associated with student status. Public transit uses were significantly lower among non-Hispanic White respondents. Taxi (including Uber/Lyft) rides decreased further among non-Hispanic Whites and homeowners. Walking frequency increased with age and decreased with homeownership. Other variables, including household income, worker status, educational attainment, single-family housing, population density, and living in an urban area, were either not significant or only marginally significant in all models.
4.3. Change in visitation to different place types
During the first year of the COVID-19 pandemic (2020), all respondents showed general trip reductions to all types of destinations (Table 4 ). Greater reductions existed for places of worship, healthcare providers, community service providers, and education facilities, while reductions to someone else’s house and retail shops were not as large. People with disabilities reduced their daily use of certain place types to a greater extent than people without disabilities (Table 4). We observed more significant trip reductions among people with disabilities for two place types—grocery stores and community service providers (p < .05). Trips to outdoor recreation facilities and healthcare service providers were also more reduced among people with disabilities, but only at a marginally significant level (p < .1).
Table 4.
Change in daily trip frequency from pre-COVID-19 to during COVID-19 by place type (n = 393).
| Variables | Total | t-statistic (pre vs. during COVID)1 |
Non-disabled | Disabled | t-statistic (Non-disabled vs. Disabled)2 |
|---|---|---|---|---|---|
| Change in grocery trip frequency | −0.65 | −10.30** | −0.46 | −0.94 | 3.76** |
| Change in restaurant trip frequency | −1.19 | −14.84** | −1.08 | −1.34 | 1.59 |
| Change in retail trip frequency | −1.06 | −15.27** | −1.00 | −1.13 | 0.89 |
| Change in house trip frequency | −1.11 | −14.36** | −1.06 | −1.17 | 0.65 |
| Change in workplace trip frequency | −1.10 | −11.25** | −1.21 | −0.96 | −1.26 |
| Change in outdoor recreation trip frequency | −0.92 | −11.87** | −0.76 | −1.15 | 2.44^ |
| Change in indoor recreation trip frequency | −1.09 | −13.81** | −1.03 | −1.18 | 0.96 |
| Change in place of worship trip frequency | −0.68 | −10.20** | −0.69 | −0.66 | −0.21 |
| Change in healthcare provider trip frequency | −0.29 | −5.98** | −0.20 | −0.42 | 2.21^ |
| Change in community service provider trip frequency | −0.21 | −4.15** | −0.09 | −0.39 | 2.83* |
| Change in education trip frequency | −0.53 | −6.62** | −0.49 | −0.60 | 0.64 |
: **: p < .01, *: p < .05, ^: p < .1 (paired samples t-tests).
: **: p < .01, *: p < .05, ^: p < .1 (independent samples t-tests).
Table 5 shows the regression model results of trip frequency change during COVID-19 by place type. The model indicates that cognitive disability was most associated with a trip reduction for multiple destination types—grocery, restaurants, outdoor recreation, indoor recreation, and healthcare providers—when other covariates were controlled. People with other types of disability (including self-care, independent living) as their primary disability type showed fewer trips to grocery stores, and those with sensory disability (including vision and hearing) reduced trips to their workplace, both of which were only marginally significant (p < .1). Unexpectedly, sensory and other disabilities were associated with increased trips to places of worship during COVID-19.
Table 5.
Regression models of trip frequency during COVID-19 by place type (n = 393).
| Grocery | Restaurants | Retail | House | Workplace | Outdoor recreation | Indoor recreation | Worship | Healthcare provider | Community service | Education facility | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Intercept) | 0.62** | 0.42* | 0.43* | 0.67** | 0.01 | 0.59** | 0.72** | 0.04 | 0.28** | 0.20^ | 0.39** |
| Daily trip frequency (pre-COVID) | 0.65** | 0.38** | 0.56** | 0.47** | 0.42** | 0.53** | 0.31** | 0.44** | 0.69** | 0.59** | 0.38** |
| Disability (cognitive) | −0.46* | −0.49* | – | – | – | −0.59* | −0.49* | – | −0.36* | – | – |
| Disability (mobility) | – | – | −0.31 | – | – | – | – | – | – | – | – |
| Disability (sensory) | −0.25 | – | – | – | 0.43^ | – | – | 0.37* | – | – | – |
| Disability (others) | −0.38^ | – | – | – | – | – | – | 0.51** | – | – | – |
| Age (years) | – | – | – | – | – | −0.01* | – | – | – | – | – |
| Age: over 65 (yes/no) | – | – | – | – | – | – | −0.33* | – | −0.21 | – | – |
| Female (yes/no) | – | – | −0.31* | −0.29* | – | – | −0.42** | −0.31** | −0.16^ | −0.11 | – |
| Household income: poverty (yes/no) | – | – | – | – | 0.25 | – | – | – | – | – | – |
| Household size | 0.10* | – | – | – | – | – | – | – | – | – | – |
| Number of children | – | – | – | 0.13^ | – | – | – | – | – | – | – |
| Married or living with a partner (yes/no) | −0.18 | 0.22 | – | – | – | – | – | – | – | – | – |
| Driver status (yes/no) | – | −0.33^ | – | −0.41* | – | – | −0.43** | – | – | – | – |
| Non-Hispanic White (yes/no) | – | −0.22 | – | – | – | – | – | – | – | −0.21* | −0.26* |
| Worker status (yes/no) | – | 0.29* | – | – | 1.22** | – | – | 0.20^ | – | – | – |
| Student status (yes/no) | – | 0.35^ | – | – | – | – | 0.43** | 0.36* | – | – | – |
| Bachelor’s degree or higher (yes/no) | – | – | – | – | −0.70** | – | – | – | – | – | – |
| Single-family housing (yes/no) | – | – | – | – | – | – | – | – | – | 0.16^ | – |
| Population density (1000 people/sq.mi.) | −0.01* | – | – | −0.01* | – | – | – | – | – | – | – |
| Urban area (yes/no) | −0.26* | – | −0.21 | – | – | – | – | – | – | – | – |
| Model fit statistics | |||||||||||
| - R-squared | 0.29 | 0.20 | 0.31 | 0.29 | 0.42 | 0.33 | 0.29 | 0.37 | 0.46 | 0.47 | 0.26 |
| - Adjusted R-squared | 0.28 | 0.18 | 0.30 | 0.28 | 0.41 | 0.32 | 0.28 | 0.36 | 0.46 | 0.46 | 0.26 |
| - AIC | 116.84 | 231.55 | 150.06 | 175.84 | 366.43 | 227.18 | 39.85 | 38.04 | −91.81 | −118.70 | 123.07 |
Note: **: p < .01, *: p < .05, ^: p < .1.
Females reduced daily trips to multiple destination types (travel to retail stores, someone else’s house, indoor recreation, and worship) significantly during the pandemic. Older adults reduced visits to indoor recreation facilities. Non-Hispanic Whites reduced their visitations to community service providers and education facilities. While workers still visited their workplace during the pandemic, those with higher educational attainment (i.e., bachelor’s degree or higher) did reduce their trips, indicating a higher possibility of working from home. Related to the built environment contexts, those living in denser urban areas reduced their travels to grocery stores and others’ houses to a greater extent but did not significantly reduce their travels to other place types, compared with those in less denser environments.
5. Discussion and conclusions
Our efforts have provided one of the first empirical studies on the impact of the COVID-19 pandemic on the activities of daily community living between people with and without disabilities. This exploratory work focuses on evaluating what impacts have been realized rather than precisely why these impacts have happened. To that end, we attempt to emphasize key outcomes and predictors of transportation-related behavior changes and then provide some key policy implications. What we offer in the implications are general observations; given the complexity and variety of disabilities and related circumstances, the findings are rather nuanced by a combination of various factors.
COVID-19 has had profound impacts on people’s livelihoods. Our survey of people with and without disabilities shows that both groups reduced their daily travel across all modes of transportation and destination types in 2020 (representing the COVID-19 pandemic), compared with 2019 (the first research question; Q1). On average, our respondents’ daily trip frequency decreased from 4.02 per day pre-COVID to 2.96 per day during COVID, and there were no statistically significant differences in daily trip frequencies between those with and without disabilities.
Differences between those with and without disabilities started to appear when we investigated travel modes (Q2). For instance, taxi trips (including ride-hailing services) were reduced more significantly among those with cognitive and sensory disabilities than other groups. Also, walking trips decreased more among individuals with mobility and sensory disabilities at the marginal significance level. Compared with pre-pandemic, the disabled respondents, especially those with cognitive disabilities, reduced their paratransit use in 2020.
Despite expected concerns over the transmission of COVID-19 on public transit (Cartenì et al., 2020), we still see evidence that people with disabilities relied as much on this form of transportation as those without disabilities during the pandemic. This is likely because some riders lack access to alternatives and may be less able to work remotely (Brough et al., 2020). This suggests the importance of ensuring that transit-dependent population have access to employment, education, healthcare, and so on in a manner that minimizes exposure to risk (Shamshiripour et al., 2020, Yıldırım and Güler, 2020). Particularly for those with disabilities, one strategy for ensuring access is to focus on expanding alternative (subsidized) transportation services (e.g., paratransit) during the pandemic. This strategy could mitigate disproportionate effects (mobility and health risks as real or perceived) to people with disabilities (Armitage and Nellums, 2020, Constantino et al., 2020, Pineda and Corburn, 2020).
By travel destination type (Q3), we observed more significant trip reductions to grocery stores and community service providers among people with disabilities during the pandemic. Community service providers have decreased their operations to respond to the pandemic, leaving people with disabilities unserved in many instances. But at the same time, home delivery of groceries and pharmaceuticals also increased during the pandemic for those who could afford them or chose to prioritize them. Thus, our findings warrant further examination of the underlying mechanisms. Travel to outdoor recreation facilities and healthcare providers by people with disabilities have also been slightly more reduced than other groups. Regression models show that cognitive disability was most associated with a trip reduction in multiple destination types when other covariates were controlled.
While these data offer insight into behaviors, they do not clarify whether or not the actions are beneficial or harmful. For instance, we cannot determine whether reduced visits to grocery stores reduced access to (healthy) food because of alternative forms of access via grocery store delivery (though that can increase the cost of delivery). For future research, it may be useful to determine the extent to which individuals rely on public transit to access grocery stores, and if a reduction in this transit reduced access to healthy food. Importantly, we are not able to determine if the reduced visits to the grocery store negatively or positively (e.g. physical and mental health) impacted participants.
Whereas access to food via grocery stores can be substituted by other means, access to open space does not have a clear alternative. Prior to this study, there was only limited knowledge about access to open space, with indications that the general public did not reduce accessing this amenity relative to other amenities (Hamidi & Zandiatashbar, 2021). Thus, it is concerning to observe a reduction in access to open space during COVID-19 for people with disabilities. Research has shown that the natural environment can help reduce stress and improve mental health (Abraham et al., 2010, Maas et al., 2006, Nutsford et al., 2013) and that this holds true for people with disabilities (Corazon et al., 2019). During a pandemic, there is an increased need for reducing stress, but reduced access to open spaces by people with disabilities is illustrative of the double jeopardy faced by people with disabilities (Armitage and Nellums, 2020, Pineda and Corburn, 2020). Now that we are aware of specific behavioral shifts in transit (e.g., to the grocery store or open space), future studies can be more targeted to identify the meaning of these changes.
Overcoming some of the hurdles of representative data collection for people with disabilities offers new opportunities for future research. We have acknowledged the limitation of estimating travel prior to COVID-19. In future research, we believe that generating longitudinal data before, during, and after significant events (such as pandemics) would provide greater clarity. To that end, we anticipate beginning to create longitudinal data for long-term assessment of people with disabilities and their travel behaviors. Our national sample does not provide an opportunity to evaluate regional characteristics, and it can be challenging to ensure a reliable longitudinal dataset without substantial resources. Thus, we also aim to conduct similar studies in targeted regions where we can isolate a variety of external factors, such as elements of the built environment and regional differences in travel restrictions, in order to address issues of time, space, and regional circumstances.
This is the first empirical transportation study we have found that focuses on collecting and analyzing data on the travel behavior and community living of people with disabilities during the COVID-19 pandemic. Prior to this study, there was limited knowledge about the degree to which changes in travel differed between people with and without disabilities due to the pandemic. While COVID-19 has had profound impacts on the entire population, the pandemic has negatively impacted individuals’ ability to participate in their community, especially among the vulnerable (Pfefferbaum & North, 2020). We believe this study can help kick-start research to recognize better how COVID-19 and future epidemics or pandemics may affect individuals with disabilities and their travel behavior. An important caveat to our findings is that we cannot conclude whether or not changes in travel are correlated with overall changes in well-being between people living with or without disabilities. We believe further study is warranted to identify the relationship to changes in travel behavior and that of well-being, including social engagement and mental and physical health.
CRediT authorship contribution statement
Keunhyun Park: Conceptualization, Funding acquisition, Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. Brent Chamberlain: Conceptualization, Funding acquisition, Data curation, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. Ziqi Song: Funding acquisition, Investigation, Resources, Validation, Writing – review & editing. Hossein Nasr Esfahani: Writing – original draft, Writing – review & editing. Jeff Sheen: Conceptualization, Funding acquisition, Project administration, Resources, Writing – review & editing. Teresa Larsen: Methodology, Project administration, Resources. Valerie Long Novack: Writing – review & editing. Carlos Licon: Funding acquisition, Writing – review & editing. Keith Christensen: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The contents of this publication were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DPCP0004). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, or HHS, and you should not assume endorsement by the Federal Government.
References
- Abedi V., Olulana O., Avula V., Chaudhary D., Khan A., Shahjouei S., Li J., Zand R. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J. Racial Ethnic Health Disparities. 2021;8(3):732–742. doi: 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham A., Sommerhalder K., Abel T. Landscape and well-being: A scoping study on the health-promoting impact of outdoor environments. Int. J. Public Health. 2010;55(1):59–69. doi: 10.1007/s00038-009-0069-z. [DOI] [PubMed] [Google Scholar]
- Altman B.M. In: Exploring Theories and Expanding Methodologies: Where we are and where we need to go Vol. 2. Barnartt S.N., Altman B.M., editors. Emerald Group Publishing Limited; 2001. Definitions of disability and their operationalization, and measurement in survey data: An update; pp. 77–100. 10.1016/S1479-3547(01)80021-X. [Google Scholar]
- Anduiza E., Galais C. Answering without reading: IMCs and strong satisficing in online surveys. Int. J. Public Opinion Res. 2017;29(3):497–519. [Google Scholar]
- Armitage R., Nellums L.B. The COVID-19 response must be disability inclusive. The Lancet Public Health. 2020;5(5):e257. doi: 10.1016/S2468-2667(20)30076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beimborn E.A., Greenwald M.J., Jin X. Accessibility, connectivity, and captivity: Impacts on transit choice. Transp. Res. Rec. 2003;1835(1):1–9. [Google Scholar]
- Blaser B., Ladner R.E. Why is Data on Disability so Hard to Collect and Understand? 2020 Research on Equity and Sustained Participation in Engineering Computing, and Technology (RESPECT) 2020;1:1–8. doi: 10.1109/RESPECT49803.2020.9272466. [DOI] [Google Scholar]
- Boarnet M.G. A broader context for land use and travel behavior, and a research agenda. J. Am. Planning Association. 2011;77(3):197–213. [Google Scholar]
- Boas T.C., Christenson D.P., Glick D.M. Recruiting large online samples in the United States and India: Facebook, mechanical turk, and qualtrics. Political Sci. Res. Methods. 2020;8(2):232–250. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brough R., Freedman M., Phillips D. Understanding Socioeconomic Disparities in Travel Behavior during the COVID-19 Pandemic (SSRN Scholarly Paper ID 3624920) Social Sci. Res. Network. 2020 doi: 10.1111/jors.12527. https://papers.ssrn.com/abstract=3624920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumbaugh, S. (2018). Travel Patterns of American Adults with Disabilities (p. 10). https://www.bts.dot.gov/sites/bts.dot.gov/files/docs/explore-topics-and-geography/topics/passenger-travel/222466/travel-patterns-american-adults-disabilities-11-26-19.pdf.
- Cartenì A., Di Francesco L., Martino M. How mobility habits influenced the spread of the COVID-19 pandemic: Results from the Italian case study. Sci. Total Environ. 2020;741:140489. doi: 10.1016/j.scitotenv.2020.140489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cdc COVID-19 Stats: COVID-19 Incidence, by Urban-Rural Classification — United States, January 22–October 31, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:1753. doi: 10.15585/mmwr.mm6946a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty K., Chatterjee M. Psychological impact of COVID-19 pandemic on general population in West Bengal: A cross-sectional study. Indian J. Psychiatry. 2020;62(3):266. doi: 10.4103/psychiatry.IndianJPsychiatry_276_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen K.M., Byrne B.C. The Built Environment and Community Integration: A Review of States’ Olmstead Plans. J. Disability Policy Studies. 2014;25(3):186–195. doi: 10.1177/1044207313493009. [DOI] [Google Scholar]
- Clifford S., Jerit J. Do attempts to improve respondent attention increase social desirability bias? Public Opinion Quarterly. 2015;79(3):790–802. [Google Scholar]
- Constantino J.N., Sahin M., Piven J., Rodgers R., Tschida J. The Impact of COVID-19 on Individuals With Intellectual and Developmental Disabilities: Clinical and Scientific Priorities. Am. J. Psychiatry. 2020;177(11):1091–1093. doi: 10.1176/appi.ajp.2020.20060780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corazon S.S., Gramkov M.C., Poulsen D.V., Lygum V.L., Zhang G., Stigsdotter U.K. I Would Really like to Visit the Forest, but it is Just Too Difficult: A Qualitative Study on Mobility Disability and Green Spaces. Scandinavian J. Disability Research. 2019;21(1):1–13. doi: 10.16993/sjdr.50. [DOI] [Google Scholar]
- Critical Care Nutrition. (2020). Reenergize Tools: Employment Status Questionnaire. https://www.criticalcarenutrition.com/docs/reenergize_def/Employment%20Status%20Questionnaire.pdf.
- Cvitkovich Y., Wister A. The Importance of Transportation and Prioritization of Environmental Needs to Sustain Well-Being among Older Adults. Environ. Behavior. 2001;33(6):809–829. doi: 10.1177/00139160121973250. [DOI] [Google Scholar]
- Daoud J.I. Multicollinearity and Regression Analysis. J. Phys. Conf. Ser. 2017;949:012009. doi: 10.1088/1742-6596/949/1/012009. [DOI] [Google Scholar]
- De Vos J. The effect of COVID-19 and subsequent social distancing on travel behavior. Transport. Res. Interdisciplinary Perspectives. 2020;5:100121. doi: 10.1016/j.trip.2020.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drum C., Oberg A., Cooper K., Carlin R. American Association on Health and Disability; 2020. COVID-19 & Adults with Disabilities: Health and Health Care Access Online Survey Summary Report; p. (p. 20).. [Google Scholar]
- Eskytė I., Lawson A., Orchard M., Andrews E. Out on the streets – Crisis, opportunity and disabled people in the era of Covid-19: Reflections from the UK. Alter. 2020;14(4):329–336. doi: 10.1016/j.alter.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing R., Cervero R. Travel and the built environment: A meta-analysis. J. Am. Planning Association. 2010;76(3):265–294. [Google Scholar]
- Fenichel E.P., Kuminoff N.V., Chowell G., Boni M.F. Skip the trip: Air Travelers’ behavioral responses to pandemic influenza. PLoS ONE. 2013;8(3):e58249. doi: 10.1371/journal.pone.0058249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujiura, G. T., & Rutkowski-Kmitta, V. (2001). Counting disability. Handbook of Disability Studies, 69–96.
- Hamidi S., Zandiatashbar A. Compact development and adherence to stay-at-home order during the COVID-19 pandemic: A longitudinal investigation in the United States. Landscape Urban Plann. 2021;205:103952. doi: 10.1016/j.landurbplan.2020.103952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotle S., Murray-Tuite P., Singh K. Influenza risk perception and travel-related health protection behavior in the US: Insights for the aftermath of the COVID-19 outbreak. Transportation Research Interdisciplinary. Perspectives. 2020;5:100127. doi: 10.1016/j.trip.2020.100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansuwan, S., Christensen, K. M., & Chen, A. (2013). Assessing the transportation needs of low-mobility individuals: Case study of a small urban community in Utah. J. Urban Planning Development, 139(2), 104–114. https://doi.org/10.1061/(ASCE)UP.1943-5444.0000142.
- Karaye I.M., Horney J.A. The impact of social vulnerability on COVID-19 in the US: An analysis of spatially varying relationships. Am. J. Prev. Med. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim C., Cheon S.H., Choi K., Joh C.-H., Lee H.-J. Exposure to fear: Changes in travel behavior during MERS outbreak in Seoul. KSCE J. Civ. Eng. 2017;21(7):2888–2895. [Google Scholar]
- Krahn G.L., Walker D.K., Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am. J. Public Health. 2015;105(S2):S198–S206. doi: 10.2105/AJPH.2014.302182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landes S.D., Turk M.A., Formica M.K., McDonald K.E., Stevens J.D. COVID-19 outcomes among people with intellectual and developmental disability living in residential group homes in New York State. Disability and Health Journal. 2020;13(4):100969. doi: 10.1016/j.dhjo.2020.100969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Moss S.E., Zhang J. The life cycle of a pandemic crisis: SARS impact on air travel. J. Int. Business Research. 2011;10(2):63. [Google Scholar]
- Lumley, T. (2020). Package ‘leaps.’ Package ‘Leaps’: Regression Subset Selection. https://cran.r-project.org/web/packages/leaps/leaps.pdf.
- Maas J., Verheij R.A., Groenewegen P.P., de Vries S., Spreeuwenberg P. Green space, urbanity, and health: How strong is the relation? J. Epidemiol. Community Health. 2006;60(7):587–592. doi: 10.1136/jech.2005.043125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madani A., Boutebal S.E., Bryant C.R. The Psychological Impact of Confinement Linked to the Coronavirus Epidemic COVID-19 in Algeria. Int. J. Environ. Res. Public Health. 2020;17(10):3604. doi: 10.3390/ijerph17103604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson, S., Schroeder, Jonathan, Van Riper, David, Kugler, Tracy, & Ruggles, Steven. (2020). National Historical Geographic Information System: Version 15.0 (15.0) . Minneapolis, MN: IPUMS. https://doi.org/10.18128/D050.V15.0.
- Milićević M. The research priorities in disability studies related to COVID-19. Beogradska Defektološka Škola. 2020;26(1):9–28. https://www.belgradeschool.com/uploads/4/6/5/1/46514917/the_research_priorities_in_disability_studies_related_to_covid-19_.pdf [Google Scholar]
- Molloy J., Tchervenkov C., Hintermann B., Axhausen K.W. Tracing the Sars-CoV-2 impact: The first month in Switzerland. Transport Findings. 2020 [Google Scholar]
- Nutsford D., Pearson A.L., Kingham S. An ecological study investigating the association between access to urban green space and mental health. Public Health. 2013;127(11):1005–1011. doi: 10.1016/j.puhe.2013.08.016. [DOI] [PubMed] [Google Scholar]
- Oppenheimer D.M., Meyvis T., Davidenko N. Instructional manipulation checks: Detecting satisficing to increase statistical power. J. Exp. Soc. Psychol. 2009;45(4):867–872. [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Cohen-Fridel S., Keisari S., Hoffman Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020;275:109–111. doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C.L., Russell B.S., Fendrich M., Finkelstein-Fox L., Hutchison M., Becker J. Americans’ COVID-19 Stress, Coping, and Adherence to CDC Guidelines. J. Gen. Intern. Med. 2020;35(8):2296–2303. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penfold C., Cleghorn N., Creegan C., Neil H., Webster S. National Centre for Social Research; London, England: 2008. Travel behaviour, experiences and aspirations of disabled people. [Google Scholar]
- Pfefferbaum B., North C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pineda V.S., Corburn J. Disability, Urban Health Equity, and the Coronavirus Pandemic: Promoting Cities for All. Journal of Urban Health. 2020;97(3):336–341. doi: 10.1007/s11524-020-00437-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst T., Budimir S., Pieh C. Depression in and after COVID-19 lockdown in Austria and the role of stress and loneliness in lockdown: A longitudinal study. J. Affect. Disord. 2020;277:962–963. doi: 10.1016/j.jad.2020.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabatello M., Landes S.D., McDonald K.E. People With Disabilities in COVID-19: Fixing Our Priorities. Am. J. Bioethics. 2020;20(7):187–190. doi: 10.1080/15265161.2020.1779396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamshiripour, A., Rahimi, E., Shabanpour, R., & Mohammadian, A. (Kouros). (2020). How is COVID-19 reshaping activity-travel behavior? Evidence from a comprehensive survey in Chicago. Transportation Research Interdisciplinary Perspectives, 7, 100216. https://doi.org/10.1016/j.trip.2020.100216. [DOI] [PMC free article] [PubMed]
- Troko J., Myles P., Gibson J., Hashim A., Enstone J., Kingdon S., Packham C., Amin S., Hayward A., Van-Tam J.N. Is public transport a risk factor for acute respiratory infection? BMC Infect. Dis. 2011;11(1):16. doi: 10.1186/1471-2334-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk M.A., Landes S.D., Formica M.K., Goss K.D. Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disability Health J. 2020;13(3):100942. doi: 10.1016/j.dhjo.2020.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau. (2020a). 65 and Older Population Grows Rapidly as Baby Boomers Age. The United States Census Bureau. https://www.census.gov/newsroom/press-releases/2020/65-older-population-grows.html.
- US Census Bureau. (2020b). About Disability. The United States Census Bureau. https://www.census.gov/topics/health/disability/about.html.
- US Census Bureau. (2020c). American Community Survey. https://www2.census.gov/programs-surveys/acs/methodology/questionnaires/2020/.
- US Census Bureau. (2020d). TIGER/Line Shapefiles. The United States Census Bureau. https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.html.
- US Census Bureau. (2020e). United States Population Growth by Region. https://www.census.gov/popclock/data_tables.php?component=growth.
- Vannette D.L., Krosnick J.A. A comparison of survey satisficing and mindlessness. Wiley Blackwell Handbook Mindfulness. 2014;1:312. [Google Scholar]
- Wang H., Xia Q., Xiong Z., Li Z., Xiang W., Yuan Y., Liu Y., Li Z., Hashimoto K. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey. PLoS ONE. 2020;15(5):e0233410. doi: 10.1371/journal.pone.0233410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z., Huimin G.u., Kavanaugh R.R. The impacts of SARS on the consumer behaviour of Chinese domestic tourists. Current Issues in Tourism. 2005;8(1):22–38. [Google Scholar]
- White G.W., Summers J.A. People with disabilities and community participation. J. Prevention & Intervention Community. 2017;45(2):81–85. doi: 10.1080/10852352.2017.1281041. [DOI] [PubMed] [Google Scholar]
- WHO. (2020). World Health Organization. https://www.who.int.
- Yıldırım M., Güler A. Factor analysis of the COVID-19 Perceived Risk Scale: A preliminary study. Death Studies. 2020:1–8. doi: 10.1080/07481187.2020.1784311. [DOI] [PubMed] [Google Scholar]