Abstract
Introduction
Carpal tunnel syndrome (CTS) is the most common compressive neuropathy. Patients who have unilateral symptoms are frequently found to have bilateral CTS by electrodiagnostic (EDx) study. We aimed to (a) study the prevalence and identify the predictive factors for bilateral CTS diagnosed by EDx; and (b) develop a model to predict bilateral CTS.
Methods
The retrospective clinical and EDx data of patients with CTS were collected and analyzed using the Chi-squared test and multiple logistic regression analysis. A model was fitted, and the best cutoff point determined. Calibration and discrimination performance of the model were performed.
Results
A total of 327 patients with a mean age of 50.0 years were enrolled. Most were women (82.6%), and the most common presenting symptom was hand numbness (93.6%). The median duration of symptoms was 60 days. The prevalence of bilateral CTS was 80.7%. In the multivariate analysis, the predictive factors for bilateral CTS were the presence of bilateral symptoms (AOR 6.7 [95%CI 3.1–14.3]), thenar muscle weakness (AOR 3.9 [95%CI 1.3–11.6]), and age ≥ 45 years (AOR 2.5 [95%CI 1.3–4.6]). The logistic regression model was fitted, and the best cutoff point determined. The area under the receiver operating curve (AUC) was 0.76. The respective optimism-corrected C index and Somers’ D was 0.762 and 0.524.
Conclusion
The prevalence of bilateral CTS was 80.7%. Our findings suggest bilateral CTS was predicted with adequate diagnostic accuracy by bilateral symptoms, age ≥ 45 years, and thenar muscle weakness.
Introduction
Carpal tunnel syndrome (CTS) is a clinical syndrome characterized by numbness, tingling, burning, and/or pain associated with localized compression of the median nerve at the wrist [1]. CTS is the most common cause of compressive neuropathy [2]. Presenting symptoms usually include numbness, paresthesia, and pain in the area of the cutaneous supply of the median nerve [3, 4]. Some patients report weakness and atrophy of the thenar area, interfering with hand function.
The diagnostic yield of CTS based on a general physical examination is poor [5–8], so electrodiagnostic (EDx) studies have been adopted because of their greater sensitivity and specificity [2], particularly before treatment or surgical intervention [9].
Although presenting symptoms may be unilateral, CTS is commonly found bilaterally. Previous studies reported the prevalence of bilateral CTS between 59 and 87% [10–13]. The factors associated with bilateral CTS are age and BMI [14]. Approximately half the patients who presented with unilateral symptoms were found to have bilateral CTS by electrodiagnostic study. There is an increased risk of symptomatic CTS in patients with an abnormal neurophysiologic study (i.e., prolonged median sensory latency without symptoms over 6 years) [15]. Most patients with unilateral symptomatic CTS but bilateral CTS (diagnosed by EDx) later present bilateral symptoms [10]. We aimed to determine the prevalence of bilateral CTS and to identify predictive factors for bilateral CTS. We also sought to explore whether these factors could be implemented as a predictive tool for bilateral CTS.
Materials and methods
A retrospective study was conducted in Khon Kaen Hospital, Thailand, between March 2020 and March 2021. The study was reviewed and approved by the Khon Kaen Hospital Ethics Committee for Human Research (KEXP63009), performed according to the ethical principles described in the Declaration of Helsinki and all methods were performed in accordance with the relevant guidelines and regulations. Informed consent was waived for this study. The study population included patients who underwent electrodiagnostic study between January 2012 and December 2018. Our inclusion criteria included (a) was ≥ 18 years age, (b) underwent electrodiagnostic study on both hands, and (c) was diagnosed with CTS by EDx in at least one hand. Exclusion criteria were polyneuropathy or concomitant cervical radiculopathy. We excluded patients who had undergone treatment with steroid injection or carpal tunnel decompression before the EDx study.
We reviewed the medical records of the CTS patients. EDx studies were performed by board-certified rehabilitation physicians using the Nicolet Biomedical Viking quest system (Nicolet Biomedical, Madison, WI, USA). The diagnostic criteria and severity of CTS were graded according to the American Association of Neuromuscular and Electrodiagnostic Medicine AANEM: (1) mild CTS is defined as prolonged sensory latency (>3.5 msec) with normal motor nerve conduction study (NCS); (2) moderate CTS is defined as abnormal median sensory (>3.5 msec) and motor latency (>4.2 msec); and, (3) severe CTS is defined as the abnormalities mentioned above with evidence of axonal loss defined by low amplitude or absent sensory nerve action potential (SNAP), low amplitude or absence of thenar compound muscle action potential (CMAP) or needle EMG showing signs of membrane instability [1, 16].
Statistical analysis
The sample size calculation for model development for binary outcomes requires there be more than 20 events per candidate predictor parameter (EPP) to prevent overfitting [17]. Chi-squared and Fisher’s Exact test were performed to determine factors associated with bilateral CTS. The variables included in this study were sex, age (≥45 years), obesity (BMI≥30 kg/m2) [18–20], diabetes, thyroid disease, connective tissue disorders, thenar weakness, thenar atrophy, bilateral complaints, duration of symptoms (≥90 days). The cut-off point for the duration of symptoms was calculated using Youden’s index [21]. When the p-value was < 0.2, these variables were included in the logistic regression analysis to determine the predictive factors for bilateral CTS. The predictive model was constructed using a stepwise selection method [22] then the model was fitted, and the risk score and probability of having bilateral CTS in each individual calculated. The best cutoff point was the change in the risk score that most effectively separated patients with and without bilateral CTS within in the Receiver Operator Characteristic (ROC) curve using Youden’s index [21]. The area under the ROC curve was defined as excellent (≥ 0.90); adequate (0.70–0.89); or, poor (< 0.70) [23]. A P < 0.05 was considered statistically significant. The data were resampled using the bootstrapping technique of 1000 iterations to evaluate the internal validity of the model [24]. The optimism-corrected discrimination index of the model was evaluated using the C-statistic and the optimism-corrected calibration index was expressed as the Somers’ D rank correlation, whereby D = 2C-1 [25]. A C-index of 0.5 indicated no discrimination, and a value of 1.0 indicated perfect discrimination of patients with different outcomes [25]. A higher Somers’ D indicated a better performance of the model. Statistical analyses were performed using Stata version 13.1 (Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.).
Results
A total of 327 patients (270 women, 57 men), mean age 50 ± 11 years, met the inclusion criteria. Most (56.3%) patients complained of unilateral hand problems. The three most common complaints were hand numbness (93.6%), pain (58.1%), and weakness (16.5%). The median duration of symptoms was 60 days. Nearly one-third of patients had an underlying disease: hypertension (17.1%), thyroid disease (2.8%), and/or diabetes mellitus (5.2%) (Table 1).
Table 1. Demographic data (n = 327).
| Variables | n (%) |
|---|---|
| Age (yrs), mean (SD) | 50.0 (11.0) |
| Sex, n (%) | |
| Men | 57 (17.4%) |
| Women | 270 (82.6%) |
| Underlying, n (%) | 88 (26.9%) |
| Hypertension | 56 (17.1%) |
| Diabetes | 17 (5.2%) |
| Thyroid disease | 9 (2.8%) |
| Duration of symptoms (days), median (IQR) | 60 (30–180) |
| Side of symptoms, n (%) | |
| Right | 72 (22.0%) |
| Left | 112 (34.3%) |
| Bilateral | 143 (43.7%) |
| Presenting symptoms, n (%) | |
| Numbness | 306 (93.6%) |
| Pain | 190 (58.1%) |
| Weakness | 54 (16.5%) |
| Atrophy | 23 (7.0%) |
Most patients (n = 264, 80.7%) had EDx diagnosed bilateral CTS. Most (93%) patients with initial complaints of bilateral symptoms had bilateral CTS. In patients presenting with unilateral symptoms, more than two-thirds (71.2%) were diagnosed with bilateral CTS. When comparing the EDx abnormality in patients with unilateral symptoms who had bilateral CTS, only half of the symptomatic hands had more severe CTS (51.9%), and nearly half presented a similar EDx severity. Only 2.3% of CTS symptomatic hands were less severe on the asymptomatic side (Table 2).
Table 2. Nerve conduction study results in 327 patients.
| Variables | N (%) |
|---|---|
| Unilateral abnormality | 63 (19.3%) |
| Mild | 32 (50.8%) |
| Moderate | 21 (33.3%) |
| Severe | 10 (15.9%) |
| Bilateral abnormality | 264 (80.7%) |
| Right | |
| Mild | 63 (23.9%) |
| Moderate | 141 (53.4%) |
| Severe | 60 (22.7%) |
| Left | |
| Mild | 75 (28.4%) |
| Moderate | 137 (51.9%) |
| Severe | 52 (19.7%) |
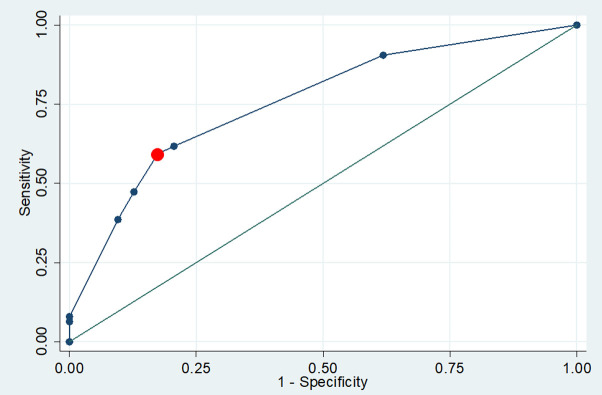
Factors associated with bilateral CTS were bilateral symptoms, BMI ≥ 30 kg/m2, age ≥ 45 years, duration of symptoms ≥ 90 days, the presence of thenar muscle weakness, and thenar muscle atrophy. Sex and diabetes mellitus were not found associated with bilateral CTS (Table 3). In the multivariate analysis, predictive factors for bilateral CTS included the presence of bilateral symptoms (AOR 6.7 [95% CI 3.1–14.3]), thenar muscle weakness (AOR 3.9 [95% CI 1.3–11.6]), and age ≥ 45 years (AOR 2.5 [95% CI 1.3–4.6]) (Table 4). According to the logistic regression, the bilateral CTS score = 0.1 + (1.4 x thenar muscle weakness) + (1.9 x bilateral symptoms) + (0.9 x AGE ≥ 45 years). Scoring: thenar muscle weakness: no = 0, yes = 1; Bilateral symptoms: no = 0, yes = 1; and age ≥45 years: no = 0, yes = 1. The best cutoff score was 2.0, which had a sensitivity of 59.5%, a specificity of 82.5%, a positive likelihood ratio of 3.4, and a negative likelihood ratio of 0.5. The area under the ROC curve (AUC) was 0.76 (95% CI 0.70–0.82) (Fig 1). After resampling, the respective 1000-replication bootstrap yielded an optimism-corrected C index, and Somers’ D was 0.762 and 0.524.
Table 3. Factors associated with bilateral CTS.
| Variables (n) | Unilateral, n (%) | Bilateral, n (%) | P-value |
|---|---|---|---|
| (n = 63) | (n = 264) | ||
| Age<45 years (96) | 29 (30.2) | 67 (69.8) | 0.001 |
| Age≥45 years (231) | 34 (14.7) | 197 (85.3) | |
| Women (270) | 50 (18.5) | 220 (81.5) | 0.56 |
| Men (57) | 13 (22.8) | 44 (77.2) | |
| BMI < 30 kg/m2 (177)* | 59 (21.1) | 221 (78.9) | 0.029 |
| BMI ≥ 30 kg/m2 (150) | 4 (8.5) | 43 (91.5) | |
| No DM (310)* | 61 (19.7) | 249 (80.3) | 0.54 |
| DM (17) | 2 (11.8) | 15 (88.2) | |
| No thyroid disease (318)* | 59 (18.6%) | 259 (81.4%) | 0.067 |
| Thyroid disease (9) | 4 (44.4%) | 5 (55.6%) | |
| No connective tissue disease (320)* | 61 (19.1%) | 259 (80.9%) | 0.62 |
| Connective tissue disease (7) | 2 (28.6%) | 5 (71.4%) | |
| Duration <90 days (168) | 40 (23.8) | 128 (76.2) | 0.034 |
| Duration ≥90 days (159) | 23 (14.5) | 136 (85.5) | |
| Unilateral symptoms (184) | 54 (29.4) | 130 (70.7) | <0.001 |
| Bilateral symptoms (143) | 9 (6.3) | 134 (93.7) | |
| No thenar muscle weakness (273)* | 59 (21.6) | 214 (78.4) | 0.022 |
| Thenar muscle weakness (54) | 4 (7.4) | 50 (92.6) | |
| No thenar muscle atrophy (304)* | 62 (20.4) | 242 (79.6) | 0.060 |
| Thenar muscle atrophy (23) | 1 (4.3) | 22 (95.7) |
*Fisher’s exact test.
Table 4. Unadjusted and adjusted odds ratio between different variable and bilateral CTS.
| Unadjusted OR (95%CI) | P value | Adjusted OR (95%CI) | P value | |
|---|---|---|---|---|
| Unilateral symptom | 1 | 1 | ||
| Bilateral symptoms | 6.2 (2.9–13.0) | <0.001 | 6.7 (3.1–14.3) | <0.001 |
| No thenar muscle weakness | 1 | 1 | ||
| Thenar muscle weakness | 3.4 (1.2–9.9) | 0.022 | 3.9 (1.3–11.6) | 0.015 |
| Age < 45 years | 1 | 1 | ||
| Age ≥ 45 years | 2.5 (1.4–4.4) | 0.002 | 2.5 (1.3–4.6) | 0.003 |
| BMI < 30 kg/m2 | 1 | |||
| BMI ≥ 30 kg/m2 | 2.9 (1.0–8.3) | 0.029 | NS | NS |
| Duration <90 days | 1 | |||
| Duration ≥90 days | 1.9 (1.1–3.3) | 0.034 | NS | NS |
| No thenar muscle atrophy | 1 | |||
| Thenar muscle atrophy | 5.6 (0.7–42.6) | 0.094 | NS | NS |
| No thyroid disease | 1 | |||
| Thyroid disease | 0.3 (0.1–1.1) | 0.067 | NS | NS |
Abbreviations: OR = Odds ratio, NS = not significant.
Fig 1. ROC curves–plot of sensitivity versus 1-specificity values for the model: Bilateral CTS score = 0.1 + (1.4 x thenar muscle weakness) + (1.9 x bilateral symptoms) + (0.9 x AGE ≥ 45 yrs).
Scoring: thenar muscle weakness: no = 0, yes = 1; Bilateral symptoms: no = 0, yes = 1; and age ≥45 years: no = 0, yes = 1. The best cutoff score was 2.0.
Discussion
This study aimed to determine the prevalence of bilateral CTS and factors associated with CTS. The prevalence of bilateral CTS was 80.7%. The prevalence of bilateral CTS was in line with previous studies that documented 59–87% [10–13]. In patients with only unilateral symptoms, bilateral CTS was found in 71.2%.
The present study identified bilateral symptoms, thenar muscle weakness, age ≥ 45 years, duration of symptoms ≥ 90 days, BMI ≥30 kg/m2, and thenar muscle atrophy as associated with bilateral CTS, which is consistent with previous studies. Kouyoumdjian et al. showed that age and severity of CTS are factors associated with bilateral CTS [14]. We also found that longer duration of symptoms was an independent factor associated with bilateral CTS; however, our duration (90 days) was shorter than previous studies. For example, Lewańska et al. found that bilateral CTS had a longer duration of symptoms (i.e., 4.01 years in bilateral CTS and 1.7 years in unilateral CTS) [13]. Similarly, Bagatur et al. reported that the duration of symptoms was longer in bilateral CTS (3 years) than unilateral CTS (1 year). Padua et al. confirmed that most patients with unilateral symptomatic CTS, but bilateral CTS diagnosed by EDx, showed bilateral symptoms later [10]. This finding is consistent with Bagatur et al. who also found that among patients with unilateral symptoms, 76% developed symptoms in the non-operated hand in a mean interval of 3.2 years [11]. Bagatur et al. pointed out that bilaterality may be time-dependent, and clinicians should inform patients with unilateral CTS about the risk of developing CTS in the contralateral hand [11, 13].
Although CTS was more common in women [26], we did not find any association between sex and bilateral CTS, i.e., women did not show a higher proportion of bilateral CTS than unilateral CTS. Diabetes mellitus (DM) was not found to be associated with bilateral CTS. Interestingly, recent epidemiological studies also found no significant association between DM and CTS [27].
The multivariate analysis revealed that patients with bilateral symptoms, thenar muscle weakness, and age ≥ 45 years had a greater probability of having bilateral CTS (OR 6.7, 3.9, and 2.5, respectively). We developed an algorithm for estimating the probability of having bilateral CTS. The diagnostic accuracy of the model was considered adequate (AUC 0.76). The respective optimism-corrected C index and Somers’ D was 0.762 and 0.524, indicating moderate accuracy.
The study has some limitations because the research was retrospective, so relevant data regarding occupations requiring repetitive tasks, previous wrist trauma or handedness were incomplete. We excluded patients who had previous interventional treatment for CTS or did not have electrodiagnostic study on both hands. This exclusion may limit the generalizability of the study. The diagnosis of CTS in an asymptomatic hand was based on the sensory and motor conduction studies across the wrist of the median nerve. In such cases, we did not perform a further combined sensory index (CSI). CSI is a summary score of three sensory latency differences: (a) transpalmar latency differences (palmdiff), (b) the median ulnar comparison with the ring finger (ringdiff), and (c) the median radial comparison with the thumb (thumbdiff), providing greater diagnostic sensitivity and specificity of CTS [28]. This may result in an underestimation of the prevalence of bilateral CTS. Some variables such as age, BMI, and duration of carpal tunnel syndrome were dichotomized which may reduce statistical power and information [29]. The model developed in our study has not been externally validated thus the generalizability of the results may be limited. Future studies should be prospective, and all variables related to CTS and bilateral CTS development should be included. In case of negative findings from routine EDx study, CSI should be considered. Long-term follow-up should be done to determine the significance of the findings of bilateral CTS.
Conclusion
The prevalence of bilateral CTS was 80.7%. Our findings suggest bilateral symptoms, age ≥ 45 years, and thenar muscle weakness can predict bilateral CTS with adequate diagnostic accuracy.
Supporting information
(XLSX)
Acknowledgments
The authors thank (a) Dr. Thananit Sungkomkunhang for guidance throughout the study and (b) Mr. Bryan Roderick Hamman under the aegis of the Publication Clinic KKU, Thailand, for assistance with the English-language presentation.
List of abbreviations
- AOR
adjusted odds ratio
- AUC
Area under the receiver operating characteristic curve
- CTS
carpal tunnel syndrome
- CMAP
compound muscle action potential
- EDx
electrodiagnosis
- EMG
Electromyography
- NCS
nerve conduction study
- OR
odds ratio
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Werner RA, Andary M. ELECTRODIAGNOSTIC EVALUATION OF CARPAL TUNNEL SYNDROME. Muscle & Nerve. 2011. Oct;44(4):597–607. doi: 10.1002/mus.22208 [DOI] [PubMed] [Google Scholar]
- 2.Robinson LR. Electrodiagnosis of Carpal Tunnel Syndrome. Phys Med Rehabil Clin N Am. 2007;18:733–46. doi: 10.1016/j.pmr.2007.07.008 [DOI] [PubMed] [Google Scholar]
- 3.Kouyoumdjian JA. [Carpal tunnel syndrome: clinical and epidemiological study in 668 cases]. Arq Neuropsiquiatr. 1999. Jun;57(2A):202–7. doi: 10.1590/s0004-282x1999000200007 [DOI] [PubMed] [Google Scholar]
- 4.Bicer M, Yanmaz MN, Cabalar M. Evaluation of 45 patients with Carpal tunnel syndrome. Medical Journal of Bakirkoy. 2015;11(4):159–61. [Google Scholar]
- 5.Walters C, Rice V. An evaluation of provocative testing in the diagnosis of carpal tunnel syndrome. Mil Med. 2002. Aug;167(8):647–52. [PubMed] [Google Scholar]
- 6.Hansen PA, Micklesen P, Robinson LR. Clinical utility of the flick maneuver in diagnosing carpal tunnel syndrome. American Journal of Physical Medicine & Rehabilitation. 2004. May;83(5):363–67. doi: 10.1097/01.phm.0000124439.14757.99 [DOI] [PubMed] [Google Scholar]
- 7.El Miedany Y, Ashour S, Youssef S, Mehanna A, Meky FA. Clinical diagnosis of carpal tunnel syndrome: old tests-new concepts. Joint Bone Spine. 2008. Jul;75(4):451–7. doi: 10.1016/j.jbspin.2007.09.014 [DOI] [PubMed] [Google Scholar]
- 8.Dale AM, Descatha A, Coomes J, Franzblau A, Evanoff B. Physical examination has a low yield in screening for carpal tunnel syndrome. Am J Ind Med. 2011. Jan;54(1):1–9. doi: 10.1002/ajim.20915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sonoo M, Menkes DL, Bland JDP, Burke D. Nerve conduction studies and EMG in carpal tunnel syndrome: Do they add value? Clin Neurophysiol Pract. 2018;3:78–88. doi: 10.1016/j.cnp.2018.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Padua L, Padua R, Nazzaro M, Tonali P. Incidence of bilateral symptoms in carpal tunnel syndrome. J Hand Surg Br. 1998. Oct;23(5):603–6. doi: 10.1016/s0266-7681(98)80010-7 [DOI] [PubMed] [Google Scholar]
- 11.Bagatur AE, Zorer G. The carpel tunnel syndrome is a bilateral disorder. Journal of Bone and Joint Surgery-British Volume. 2001. Jul;83B(5):655–58. doi: 10.1302/0301-620x.83b5.11350 [DOI] [PubMed] [Google Scholar]
- 12.Vicuna P, Idiaquez JF, Jara P, Pino F, Carcamo M, Cavada G, et al. Electrophysiological severity of carpal tunnel syndrome according to age in adult patients. Revista Medica De Chile. 2017. Oct;145(10):1252–58. doi: 10.4067/S0034-98872017001001252 [DOI] [PubMed] [Google Scholar]
- 13.Lewańska M. The bilaterality of idiopathic carpal tunnel syndrome among manual workers. Int J Occup Med Environ Health. 2020. Mar;33(2):151–61. doi: 10.13075/ijomeh.1896.01517 [DOI] [PubMed] [Google Scholar]
- 14.Kouyoumdjian JA. Carpal tunnel syndrome. Age, nerve conduction severity and duration of symptomatology. Arq Neuropsiquiatr. 1999. Jun;57(2B):382–6. doi: 10.1590/s0004-282x1999000300007 [DOI] [PubMed] [Google Scholar]
- 15.Werner RA, Gell N, Franzblau A, Armstrong TJ. Prolonged median sensory latency as a predictor of future carpal tunnel syndrome. Muscle Nerve. 2001. Nov;24(11):1462–7. doi: 10.1002/mus.1169 [DOI] [PubMed] [Google Scholar]
- 16.Dumitru D, Amato A, Zwarts M. Electrodiagnostic medicine. Philadelphia: Hanley & Belfus, Inc.; 2001 [Google Scholar]
- 17.Ogundimu EO, Altman DG, Collins GS. Adequate sample size for developing prediction models is not simply related to events per variable. Journal of Clinical Epidemiology. 2016. Aug;76:175–82. doi: 10.1016/j.jclinepi.2016.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lam N, Thurston A. Association of obesity, gender, age and occupation with carpal tunnel syndrome. Aust N Z J Surg. 1998. Mar;68(3):190–3. doi: 10.1111/j.1445-2197.1998.tb04743.x [DOI] [PubMed] [Google Scholar]
- 19.Shiri R, Pourmemari MH, Falah-Hassani K, Viikari-Juntura E. The effect of excess body mass on the risk of carpal tunnel syndrome: a meta-analysis of 58 studies. Obes Rev. 2015. Dec;16(12):1094–104. doi: 10.1111/obr.12324 [DOI] [PubMed] [Google Scholar]
- 20.Pangsuwan S. A study of the prevalence and risk factors of carpal tunnel syndrome in employees at the Royal Irrigation Hospital. Journal of Science and Technology. 2017;9(17):163–73. [Google Scholar]
- 21.Hajian-Tilaki K. The choice of methods in determining the optimal cut-off value for quantitative diagnostic test evaluation. Statistical Methods in Medical Research. 2018. Aug;27(8):2374–83. doi: 10.1177/0962280216680383 [DOI] [PubMed] [Google Scholar]
- 22.Chowdhury MZI, Turin TC. Variable selection strategies and its importance in clinical prediction modelling. Family Medicine and Community Health. 2020. Mar;8(1). doi: 10.1136/fmch-2019-000262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salter K, Jutai JW, Teasell R, Foley NC, Bitensky J, Bayley M. Issues for selection of outcome measures in stroke rehabilitation: ICF activity. Disability and Rehabilitation. 2005. Mar;27(6):315–40. doi: 10.1080/09638280400008545 [DOI] [PubMed] [Google Scholar]
- 24.Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. Bmc Medicine. 2015. Jan;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996. Feb;15(4):361–87. doi: [DOI] [PubMed] [Google Scholar]
- 26.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999. Jul;282(2):153–8. doi: 10.1001/jama.282.2.153 [DOI] [PubMed] [Google Scholar]
- 27.Low J, Kong A, Castro G, de la Vega PR, Lozano J, Varella M. Association Between Diabetes Mellitus and Carpal Tunnel Syndrome: Results From the United States National Ambulatory Medical Care Survey. Cureus. 2021. Mar;13(3). doi: 10.7759/cureus.13844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robinson LR, Micklesen PJ, Wang L. Strategies for analyzing nerve conduction data: superiority of a summary index over single tests. Muscle Nerve. 1998. Sep;21(9):1166–71. doi: [DOI] [PubMed] [Google Scholar]
- 29.Altman DG, Royston P. Statistics notes—The cost of dichotomising continuous variables. British Medical Journal. 2006. May;332(7549):1080–80. doi: 10.1136/bmj.332.7549.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.