Abstract
There is an urgent need to identify biomarkers for Alzheimer’s disease (AD), but the identification of reliable blood-based biomarkers has proven to be much more difficult than initially expected. The current availability of high-throughput multi-omics data opens new possibilities in this titanic task. Candidate Single Nucleotide Polymorphisms (SNPs) from large, genome-wide association studies (GWAS), meta-analyses exploring AD (case-control design), and quantitative measures for cortical structure and general cognitive performance were selected. The Genotype-Tissue Expression (GTEx) database was used for identifying expression quantitative trait loci (eQTls) among candidate SNPs. Genes significantly regulated by candidate SNPs were investigated for differential expression in AD cases versus controls in the brain and plasma, both at the mRNA and protein level. This approach allowed us to identify candidate susceptibility factors and biomarkers of AD, facing experimental validation with more evidence than with genetics alone.
Keywords: eQTLs, differential expression, integrative analysis, Alzheimer’s disease
1. Introduction
Alzheimer’s disease (AD) is the leading cause of dementia worldwide, affecting 36 million people nowadays, and it is expected to triple its prevalence by mid-century. Familial forms of AD are caused by mutations on the amyloid-related genes PSEN1, PSEN2, and APP, while diverse candidate genes and pathways have been reported for sporadic AD, mainly provided by genome-wide association studies (GWAS) [1,2,3,4,5,6,7]. The largest risk factor for AD identified so far is the apolipoprotein E (APOE)E4 allele, conferring up to 16-fold increased risk in the homozygous state, but despite its relevance, APOE pathogenic role in AD has not been fully elucidated yet.
The clinical major hallmarks of AD are amyloid deposits and neurofibrillary tangles. Consistently with this observation, amyloid, tau protein (T-tau), and tau phosphorylated at position threonine 181 (P-tau) have been found to be present at low levels in the cerebrospinal fluid (CSF) of AD patients when compared to controls, being the only AD biomarkers currently employed in the clinical setting [8,9,10]. Considerable efforts have been put into identifying biomarkers of the disease, especially in the prodromal stage, when early intervention is expected to reduce the burden of the disease. Diverse CSF biomarkers have been proposed, including the neurofilament light protein (NFL) [11], neurogranin (Ng) [12], the neuron-specific enolase (NSE) [13], the visinin-like protein 1 (VLP-1) [14], the monocyte chemotactic protein 1 (MCP-1) [15] or the glial fibrillary acidic protein (GFAP) [16].
The identification of blood-based biomarkers is of special interest since plasma is much more accessible than CSF, and they can be applied to the screening of large populations. The fundamentals of blood-based biomarkers relate to the disruption of the blood–brain barrier, which allows the drainage of small molecules or molecules with specific transporters [17]. However, since these molecules become considerably diluted in plasma, a biochemically complex medium, well-established blood biomarkers for AD are still not in place. In fact, Amyloid β38, β40, and β42, as well as tau proteins, have also been evaluated with uneven results [18,19,20,21]. Hence, solid conclusions about the usefulness of plasma biomarkers are still a subject of active research.
Most efforts in identifying AD biomarkers until now have been based on differential expression analysis between patients and control individuals. While a large proportion of the studies used transcriptomic data, confirmation of these differences at the protein level in CSF or plasma samples has not been straightforward, and the success in identifying reliable markers of the disease has been quite limited. Integration of different layers of information can help to better understand the physiological and pathological mechanisms leading to a biological condition, from gene defects to abnormal expression of encoded or related proteins. In addition, concordance between omics serves to reduce the usually large list of candidates derived from high throughput experiments. In this paper, we aimed at identifying novel plasma biomarkers for AD, starting from GWAS summary statistics and incorporating transcriptomic and proteomic data from both the brain and blood.
2. Materials and Methods
2.1. Genome-Wide Data
Candidate Single Nucleotide Polymorphisms (SNPs) were selected from published meta-analyses of GWAS on AD cases vs control subjects [2,3,4,5], intelligence and general cognitive function [22,23], and cortical structure [24,25,26], which is related to cognitive function and neurological diseases. A total of 2978 unique SNPs were selected (Supplementary Table S1).
2.2. Expression Quantitative Trait Loci (eQTL) Identification
The Genotype-Tissue Expression (GTEx) v7 data were used to identify genes regulated by selected candidate SNPs in 13 brain regions (Amygdala, Anterior cingulate cortex, Caudate basal ganglia, Cerebellar Hemisphere, Cerebellum, Cortex, Frontal Cortex, Hippocampus, Hypothalamus, Nucleus accumbens basal ganglia, Putamen basal ganglia, Spinal cord cervical, and Substantia nigra). Significant variant gene–SNP pairs (i.e., those showing p-value below the p-value nominal threshold, which is defined as the empirical p-value of the gene closest to the 0.05 FDR threshold) were selected.
2.3. Brain and Blood Transcriptomics
Genes whose expression was significantly altered by the presence of candidate SNPs identified in the previous step were tested for differential expression (DE) between AD cases and controls using brain transcriptomic data. The cortex gene-expression meta-analysis included Mount Sinai Brain Bank (MSBB) dataset (frontal pole, occipital visual cortex, dorsolateral prefrontal cortex, precentral gyrus, prefrontal cortex), ROSMAP (dorsolateral prefrontal cortex), and MAYO (temporal cortex) studies, and GSE15222 [27] and GSE48350 [28] (entorhinal cortex, superior frontal cortex, post-central gyrus) datasets from the GEO repository (n = 1503). Hippocampal profiles were obtained from GSE11882/GSE48350 datasets [28] and the MSBB study. Blood transcriptomic datasets included ADNI and AddNeuroMed studies (n = 734). DE analysis between cases and controls was performed using the R package limma [29] by dataset and brain region when available. For combining DE results from the different datasets, the Random Effect Model (REM) implemented in the metaDE R tool was used. Heatmap graphs were generated with the Pheatmap R package.
2.4. Proteomic Data Analysis
Expression profiles of candidate genes were evaluated at the proteomic level using blood proteomics data from the ADDN study (931 proteins) and cortex proteomics from four independent datasets (BANNER, BLSA, MAYO, and MSBB; 2658 proteins). Differential protein expression analyses were performed using the limma package, with PMI, age, and sex as covariates. Meta-analysis of brain datasets was performed as described for transcriptomic data.
2.5. Enrichment Analysis
Enrichment analysis was performed using gPROFILER [30] on significant genes/proteins (showing REM p-value < 0.05 in the differential expression meta-analyses) and GTEx results. The databases being interrogated included GO, KEGG, WikiPathways, and Reactome. Path graphs were generated using the R package rrvgo.
3. Results
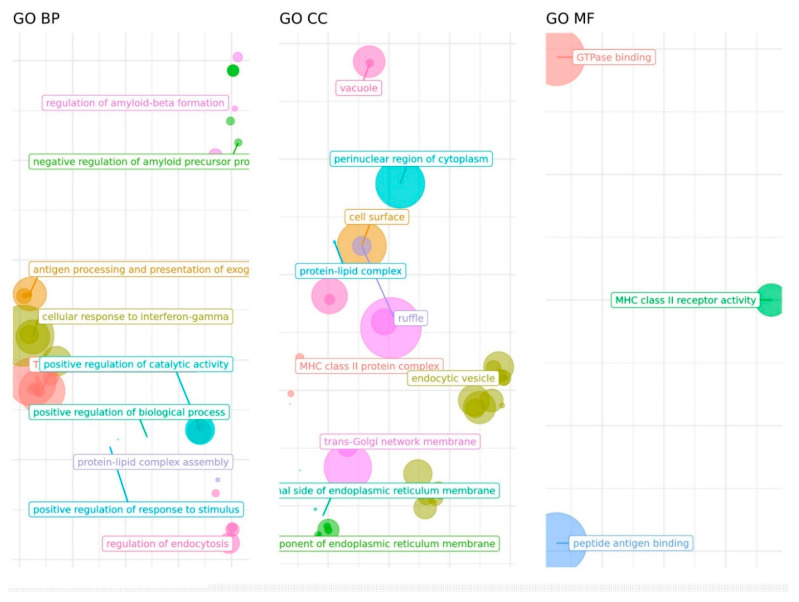
There was limited overlap between candidate SNPs from the three phenotypes: only one SNP shared by AD and cognitive performance candidate lists (rs3817334), and two SNPs in common in the cognitive performance and cortical structure lists (rs13212044 and rs13107325). Genes regulated in diverse brain tissues by the 2186th, 398th, and 412th candidate SNPs from AD, cognition, and cortical measures GWAS were explored using GTEx. We found 51, 75, and 140 regulated genes, respectively (Supplementary Tables S2–S4). Six genes from the 11p11.2 (C1QTNF4, FAM180B, MADD, MTCH2, SLC39A13, and NDUFS3) were found to be regulated by the AD and cognitive performance candidate SNPs, determined by the common rs3817334 polymorphism plus rs11605348 for the cognitive phenotype and 135 additional SNPs for the AD phenotype. There was no overlap between AD and cortical measures eQTL-regulated gene lists, whereas 24 shared genes were identified for the cognitive performance and cortical structure phenotypes (ARHGAP27, ARL17A, DCC, DEPDC1B, FMNL1, GOSR1, KANSL1, KANSL1-AS1, LINC02210, LOC107984142, LOC339192, LRRC37A, LRRC37A2, MAPT, NDUFAF2, NPIPB9, PLEKHM1, RPS26, SH2B1, SPPL2C, SULT1A1, SULT1A2, SUOX, and TUFM). The 51 AD genes were involved in immune-related functions, mainly driven by the HLA and CR1 loci, amyloid-related pathways (ABCA7, BIN1, PICALM genes), protein-lipid complexes (ABCA7, APOC2, APOC4, BIN1 genes), and vesicle trafficking (RIN3, PICALM) (Figure 1, Supplementary Table S5). By contrast, no significant enrichment was found either for cognition or cortical genes, although the 24 shared genes were mostly related to cytoskeleton and endocytosis, neurotransmitters metabolism and oxidative phosphorylation.
Figure 1.
Gene Ontology (GO) categories over-represented among genes regulated by AD eQTLs. BP: Biological Process; CC: Cellular Component, MF: Molecular Function. Distances between points represent the similarity between terms. Axes are the first 2 components of applying a Principal Component Analysis (PCA) to the (di)similarity matrix. Size of the point represents the provided scores or, in its absence, the number of genes the GO term contains.
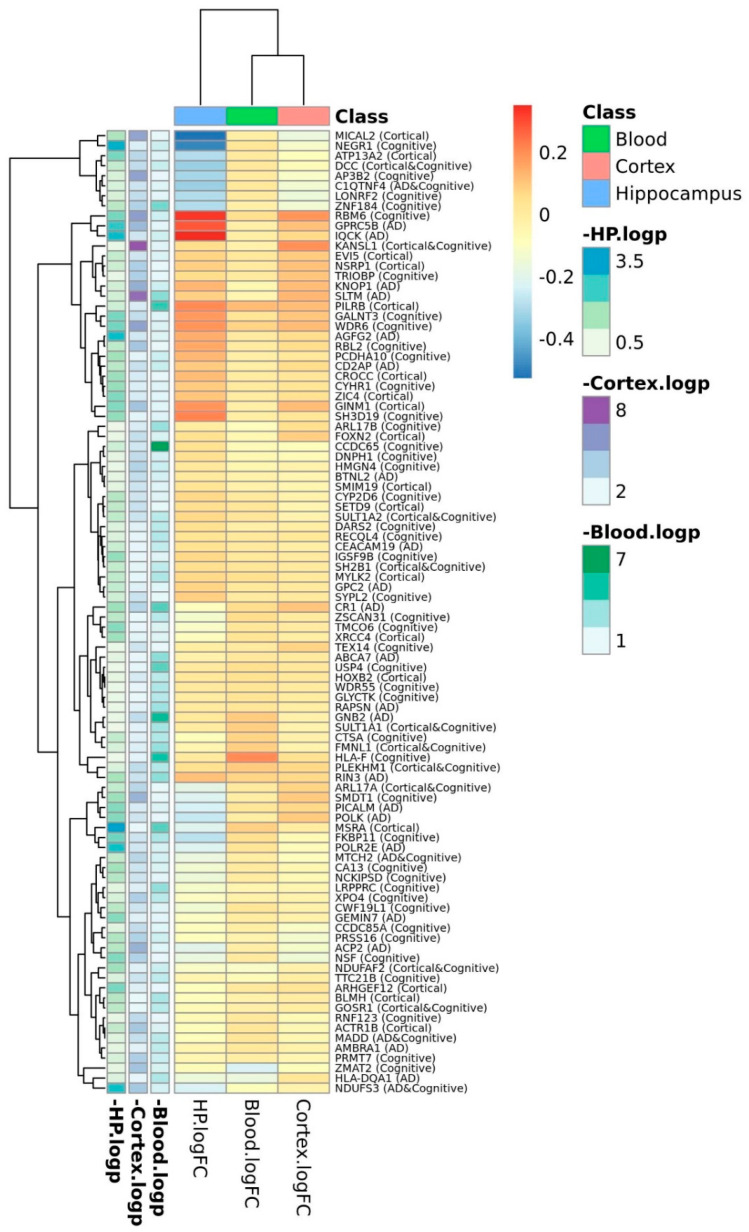
The expression patterns of the genes identified by GTEx eQTL analyses were explored using blood and brain transcriptomics (Supplementary Tables S6–S8). In the blood, 10 of the 41 (24.4%) AD genes present in the expression dataset were differentially expressed in cases vs controls, while 11 of 62 (17.7%) cortical genes, and 22 of 108 (22.4%) cognitive genes (Figure 2) were also differentially expressed in blood. In the brain cortex, 16 of 48 (33.3%), 15 of 69 (21.7%), and 39 of 119 (32.8%) AD, cortical, and cognitive-available genes were found differentially expressed in the brain, respectively. Finally, in the hippocampus, 9 of 48 (18.8%), 8 of 66 (12.1%), and 14 of 119 (11.8%) AD, cortical, and cognitive genes, respectively, were differentially expressed between cases and controls.
Figure 2.
Heatmap plot of logFC expression values between AD cases and controls at the mRNA level.
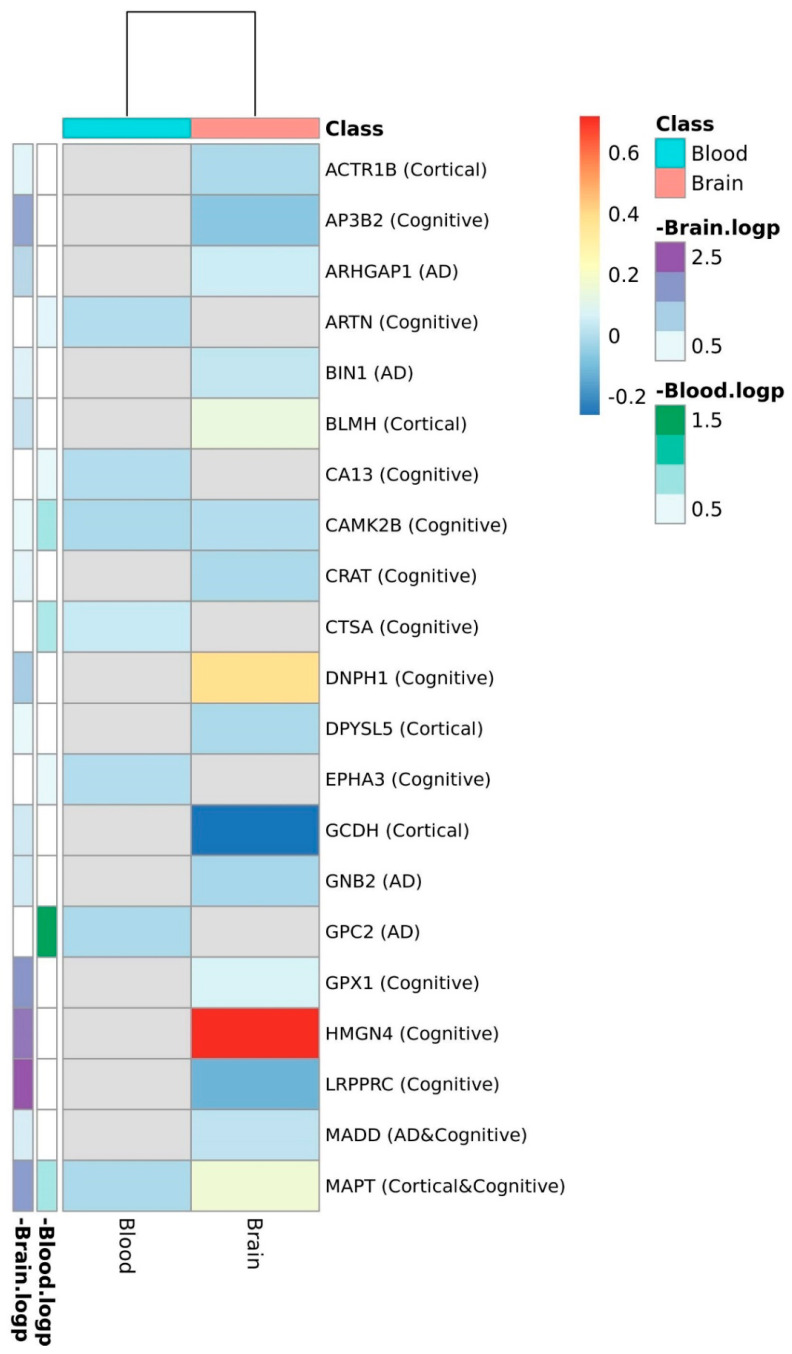
At the proteomic level, only 29 genes were represented in the brain and 9 in the blood from the total list of candidates (Figure 3, Supplementary Tables S9 and S10). The single AD candidate gene represented in the plasma dataset, GPC2, was shown to be downregulated in AD cases when compared to control subjects; neither tau protein (encoded by MAPT gene) nor the other cognitive and structural candidates represented in this dataset (ARTN, CA13, CAMK2B, CTSA, EPHA3, MAPT, MST1R, and ULBP) showed differences between AD cases and controls in plasma. In the brain, the NADH Dehydrogenase NDUFS3, the glutathione peroxidase enzyme encoded by GPX1, the chromatin-associated protein HMGN4, and tau were upregulated in AD cases, whereas TUFM (Mitochondrial Elongation Factor Tu), LRPPRC (Mitochondrial Leucine-Rich PPR Motif-Containing Protein), and AP3B2 (Adaptor protein complex 3) were downregulated.
Figure 3.
Heatmap plot of logFC expression values between AD cases and controls at the protein level. FC: Fold Change. Gene FCs were calculated as the average expression in the AD group relative to the average expression in the control group.
4. Discussion
The current approach represents an integrative analysis of multi-omic data for Alzheimer’s disease patients and control subjects, aimed at identifying blood biomarkers of this prevalent degenerative disease. Starting from candidate SNPs for AD, general cognitive function, and cortical structure reported in published meta-analyses, we used the GTEx database for identifying genes regulated by these candidate gene variants. The expression of these genes at the mRNA level in the brain and blood was explored by means of differential expression analysis between AD patients and controls. Finally, gene candidates were evaluated at the proteomic level in the blood and cortex, an analysis step hampered by the low availability of blood-based proteomic datasets and the limited range of proteins represented in high throughput proteomics compared to transcriptomics. In fact, only one AD candidate gene was represented in the ADDN blood proteomic data, the Glypican-2 (GPC2) protein, significantly downregulated in AD cases.
GPC2 is a cell surface proteoglycan that bears heparan sulfate. Heparan sulfate proteoglycans (HSPGs) are components of the cell surface and extracellular matrix, and constitute central players in the development and functions of synapses [31]. In particular, it has been reported that GPC2 levels in CSF resemble the status of adult hippocampal neurogenesis, decreasing over time according to preliminary studies [32]. Furthermore, a recent meta-analysis has shown a genome-wide significant statistical association with AD of the rs12705073 polymorphism, located in the first intron of the GPC2 gene [33,34]. The GPC2 homologue GPC5 has been shown to be downregulated in both CSF and plasma of Aβ negative MCI subjects when compared to control subjects in the Biofinder study [35]; HSPGs are present in amyloid lessons, promoting Aβ peptide and tau fibrillization and providing resistance against proteolytic breakdown [36]. GPC2 has been shown to undergo a significant upregulation when exposed to Aβ in two mouse models of AD, mainly derived from the glial cell [37,38]. In particular, GPC2 is expressed in the oligodendrocyte precursors cells (OPCs), the precursors of the myelin-producing oligodendrocyte cells. According to the ROSMAP snRNAseq data and the scREAD database, GPC2 is downregulated in OPCs from AD patients when compared with control subjects. In a previous report, we identified these cells as key drivers in AD pathogenesis [39]. In fact, myelin disturbance as an etiological agent for AD is now increasingly being studied, and a recent report confirms its key role in a murine model of AD [40]. Further studies in larger cohorts are required to validate the utility of GPC2 as an AD biomarker, and to investigate if an interaction with APOE exits in vivo, since the 34-kD glycoprotein exerts its function in lipoprotein clearance via binding to specific cell surface receptors, including the LDL receptor and diverse HSPGs. Interestingly, the two classes of membrane HSPGs, transmembrane syndecans (SDCs), and glycosylphosphatidylinositol-anchored glypicans (GPCs) have been shown to interact with ApoE modulating amyloid uptake and aggregation in a haplotype-dependent manner [41,42].
Over the past decade, the advent of high throughput omic technologies has fuelled the discovery-based approach, providing access to a large number of candidate molecules, in contrast to classical approaches, mostly focused on candidate genes from known pathways of the disease, mainly related to amyloid pathology and inflammatory response in the case of AD. Despite the application of a wide variety of sophisticated approaches for the statistical analysis of large datasets, the results have been disappointing overall, and the repertory of clinical biomarkers overall has been only slightly increased, most of them oncologic biomarkers. Strategies based on differential expression analysis have been by far the most used approach, in part because of the simplicity of logFC calculations. However, the classification accuracy of identified, differentially-expressed biomarkers is, overall, not high when validated at the proteomic level. A recent meta-analysis of proteomic candidate biomarkers for AD described six markers consistently replicated in at least three independent cohorts: alpha-2-macroglobulin (α2M)ps, pancreatic polypeptide (PP)ps, apolipoprotein A-1 (ApoA-1)ps, afaminp, insulin growth factor binding protein-2 (IGFBP-2)ps, and fibrinogen-γ-chainp [21]. Another recent meta-analysis reported that CSF T-tau, P-tau, Aβ42, NFL, and plasma T-tau were strongly associated with AD, whereas emerging CSF biomarkers such as NSE, VLP-1, HFABP, and YKL-40 were moderately associated, and plasma Aβ42 and Aβ40 were not associated with AD [19].
In conclusion, the identification of biomarkers is particularly challenging in the neurology field, AD being a good example of this complexity. Poor clinical diagnostics, long asymptomatic prodromal stages, variability in clinical features and rates of progression, besides individual genetic susceptibility, are some determinants of this situation. The combination of different levels of information at different disease stages is now possible, thanks to the availability of high throughput multi-omics technologies, opening a new era for biomarker discovery although still limited by the availability of large untargeted proteomic datasets. This report represents a preliminary study aimed at illustrating an analysis pipeline applicable to any disease with a genetic component. Further studies are therefore required to investigate the potential of GPC2 as an AD plasma biomarker, using large populations in a clinical setting.
Acknowledgments
This work has been partially supported by the ADAPTED consortium, which has received funding from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No. 115975. This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation program and the European Federation of Pharmaceutical Industries and Associations. The AddNeuroMed study is a public–private partnership supported by EFPIA companies and SMEs as part of InnoMed (Innovative Medicines in Europe), an Integrated Project funded by the European Union of the Sixth Framework program priority FP6-2004-LIFESCIHEALTH-5. Clinical leads responsible for data collection are Iwona Kłoszewska (Lodz), Simon Lovestone (London), Patrizia Mecocci (Perugia), Hilkka Soininen (Kuopio), Magda Tsolaki (Thessaloniki), and Bruno Vellas (Toulouse). Imaging leads are Andy Simmons (London), Lars-Olad Wahlund (Stockholm), and Christian Spenger (Zurich). Bioinformatics leads are Richard Dobson (London) and Stephen Newhouse (London). This dataset was downloaded from Synapse (doi:10.7303/syn2790911). The Alzheimer’s Disease Neuroimaging Initiative (ADNI) was launched in 2003 as a public–private partnership, led by Principal Investigator Michael W. Weiner, MD. The primary goal of ADNI has been to test whether serial magnetic resonance imaging (MRI), positron emission tomography (PET), other biological markers, and clinical and neuropsychological assessments can be combined to measure the progression of mild cognitive impairment (MCI) and early Alzheimer’s disease (AD). For up-to-date information, see www.adni-info.org (4 June 2021). Data collection and sharing for this project was partially funded by the ADNI (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie; Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org (accessed on 4 June 2021)). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. The Banner Sun Health Research Institute (BANNER) data were provided by Levey from Emory University. A portion of these data was generated from samples collected through the Sun Health Research Institute Brain and Body Donation Program of Sun City, Arizona. The Brain and Body Donation Program is supported by the National Institute of Neurological Disorders and Stroke (U24 NS072026 National Brain and Tissue Resource for Parkinson’s Disease and Related Disorders), the National Institute on Aging (P30 AG19610 Arizona Alzheimer’s Disease Core Center), the Arizona Department of Health Services (contract 211002, Arizona Alzheimer’s Research Center), the Arizona Biomedical Research Commission (contracts 4001, 0011, 05-901 and 1001 to the Arizona Parkinson’s Disease Consortium) and the Michael J. Fox Foundation for Parkinson’s Research. This study was downloaded from Synapse (10.7303/syn7170616). The Baltimore Longitudinal Study on Aging (BLSA) study data were generated from postmortem brain tissue collected through The National Institute on Aging’s Baltimore Longitudinal Study of Aging and provided by Allan I Levey from Emory University. This study was downloaded from Synapse (10.7303/syn3606086). The Mayo Clinic Alzheimer’s Disease Genetic Studies, led byNilüfer Ertekin-Taner and Steven G. Younkin, Mayo Clinic, Jacksonville, FL, using samples from the Mayo Clinic Study of Aging, the Mayo Clinic Alzheimer’s Disease Research Center, and the Mayo Clinic Brain Bank. Data collection was supported through funding by NIA grants P50 AG016574, R01 AG032990, U01 AG046139, R01 AG018023, U01 AG006576, U01 AG006786, R01 AG025711, R01 AG017216, R01 AG003949, NINDS grant R01 NS080820, CurePSP Foundation, and support from Mayo Foundation. This dataset was downloaded from Synapse (doi:10.7303/syn5550404). The Mount Sinai Brain Bank (MSBB) study data were provided by. Levey from Emory University based on postmortem brain tissue collected through the Mount Sinai VA Medical Center Brain Bank, provided by. Eric Schadt from Mount Sinai School of Medicine. This dataset was downloaded from Synapse (10.7303/syn3159438). The ROS/MAP study data were provided by the Rush Alzheimer’s Disease Center, Rush University Medical Center, Chicago. Data collection was supported through funding by NIA grants P30AG10161 (ROS), R01AG15819 (ROSMAP; genomics and RNAseq), R01AG17917 (MAP), R01AG30146, R01AG36042 (5hC methylation, ATACseq), RC2AG036547 (H3K9Ac), R01AG36836 (RNAseq), R01AG48015 (monocyte RNAseq), RF1AG57473 (single nucleus RNAseq), U01AG32984 (genomic and whole exome sequencing), U01AG46152 (ROSMAP AMP-AD, targeted proteomics), U01AG46161(TMT proteomics), U01AG61356 (whole genome sequencing, targeted proteomics, ROSMAP AMP-AD), the Illinois Department of Public Health (ROSMAP), and the Translational Genomics Research Institute (genomic). Additional phenotypic data can be requested at www.radc.rush.edu (accessed on 4 June 2021). This dataset was downloaded from Synapse (doi:10.7303/syn3219045). The results published here are in part based on data obtained from the AMP-AD Knowledge Portal (https://adknowledgeportal.synapse.org/ (accessed on 4 June 2021)).
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/diagnostics11122303/s1, Table S1: Candidate SNPs; Table S2: GTEx results for AD candidate SNPs; Table S3: .GTEx results for cognitive performance SNPs; Table S4: GTEx results for cortical structure candidate SNPs; Table S5: Enrichment analysis of genes regulated by AD candidate SNPs; Table S6: Blood transcriptomics; Table S7: Cortex transcriptomics; Table S8: Hippocampus transcriptomics; Table S9: Blood proteomics; Table S10: Brain proteomics.
Author Contributions
L.M. performed statistical analyses and contributed to manuscript writing; S.C.L. performed some statistical analyses and plots; A.G.-P. reviewed the manuscript; M.E.S. performed data analysis and wrote the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research has been partially funded by the ADAPTED consortium, which has received funding from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No. 115975. This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation program and the European Federation of Pharmaceutical Industries and Associations.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due that this study only makes use of publicly available data.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is available as Supplementary material.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lambert J.-C., Heath S., Even G., Campion D., Sleegers K., Hiltunen M., Combarros O., Zelenika D., Bullido M.J., Tavernier B., et al. Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer’s disease. Nat. Genet. 2009;41:1094–1099. doi: 10.1038/ng.439. [DOI] [PubMed] [Google Scholar]
- 2.Moreno-Grau S., de Rojas I., Hernández I., Quintela I., Montrreal L., Alegret M., Hernández-Olasagarre B., Madrid L., González-Perez A., Maroñas O., et al. Genome-wide association analysis of dementia and its clinical endophenotypes reveal novel loci associated with Alzheimer disease and three causality networks of AD: The GR@ACE project. Alzheimers Dement. 2019;15:1331–1347. doi: 10.1016/j.jalz.2019.06.4950. [DOI] [PubMed] [Google Scholar]
- 3.Kunkle B.W., Grenier-Boley B., Sims R., Bis J.C., Damotte V., Naj A.C., Boland A., Vronskaya M., Van Der Lee S.J., Amlie-Wolf A., et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. [(accessed on 9 June 2021)];Nat. Genet. 2019 51:414–430. doi: 10.1038/s41588-019-0358-2. Available online: https://www.nature.com/articles/s41588-019-0358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lambert J.C., Ibrahim-Verbaas C.A., Harold D., Naj A.C., Sims R., Bellenguez C., Jun G., DeStefano A.L., Bis J.C., Beecham G.W., et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. [(accessed on 12 July 2021)];Nat. Genet. 2013 45:1452–1458. doi: 10.1038/ng.2802. Available online: https://pubmed.ncbi.nlm.nih.gov/24162737/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jansen I.E., Savage J.E., Watanabe K., Bryois J., Williams D., Steinberg S., Sealock J., Karlsson I., Hägg S., Athanasiu L., et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat. Genet. 2019;51:404–413. doi: 10.1038/s41588-018-0311-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sims R., Hill M., Williams J. The multiplex model of the genetics of Alzheimer’s disease. Nat. Neurosci. 2020;23:311–322. doi: 10.1038/s41593-020-0599-5. [DOI] [PubMed] [Google Scholar]
- 7.Bekris L.M., Yu C.-E., Bird T.D., Tsuang D.W. Genetics of Alzheimer Disease. [(accessed on 11 July 2021)];J. Geriatr. Psychiatry Neurol. 2010 23:213. doi: 10.1177/0891988710383571. Available online: /pmc/articles/PMC3044597/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andreasen N., Hesse C., Davidsson P., Minthon L., Wallin A., Winblad B., Vanderstichele H., Vanmechelen E., Blennow K. Cerebrospinal fluid beta-amyloid(1-42) in Alzheimer disease: Differences between early- and late-onset Alzheimer disease and stability during the course of disease. [(accessed on 4 November 2021)];Arch. Neurol. 1999 56:673–680. doi: 10.1001/archneur.56.6.673. Available online: https://pubmed.ncbi.nlm.nih.gov/10369305/ [DOI] [PubMed] [Google Scholar]
- 9.Vanmechelen E., Vanderstichele H., Davidsson P., van Kerschaver E., van der Perre B., Sjögren M. Quantification of tau phosphorylated at threonine 181 in human cerebrospinal fluid: A sandwich ELISA with a synthetic phosphopeptide for standardization. Neurosci. Lett. 2000;285:49–52. doi: 10.1016/S0304-3940(00)01036-3. [DOI] [PubMed] [Google Scholar]
- 10.Blennow K., Wallin A., Ågren H., Spenger C., Siegfried J., Vanmechelen E. Tau protein in cerebrospinal fluid: A biochemical marker for axonal degeneration in Alzheimer disease? [(accessed on 4 November 2021)];Mol. Chem. Neuropathol. 1995 26:231–245. doi: 10.1007/BF02815140. Available online: https://pubmed.ncbi.nlm.nih.gov/8748926/ [DOI] [PubMed] [Google Scholar]
- 11.Rosengren L.E., Karlsson J.E., Sjögren M., Blennow K., Wallin A. Neurofilament protein levels in CSF are increased in dementia. [(accessed on 4 November 2021)];Neurology. 1999 52:1090–1093. doi: 10.1212/WNL.52.5.1090. Available online: https://pubmed.ncbi.nlm.nih.gov/10102440/ [DOI] [PubMed] [Google Scholar]
- 12.Kvartsberg H., Duits F.H., Ingelsson M., Andreasen N., Öhrfelt A., Andersson K., Brinkmalm G., Lannfelt L., Minthon L., Hansson O., et al. Cerebrospinal fluid levels of the synaptic protein neurogranin correlates with cognitive decline in prodromal Alzheimer’s disease. [(accessed on 4 November 2021)];Alzheimer’s & Dementia. J. Alzheimer’s Assoc. 2015 11:1180–1190. doi: 10.1016/j.jalz.2014.10.009. Available online: https://pubmed.ncbi.nlm.nih.gov/25533203/ [DOI] [PubMed] [Google Scholar]
- 13.Pametti L., Palumbo B., Cardinali L., Loreti F., Chionne F., Cecchetti R., Senin U. Cerebrospinal fluid neuron-specific enolase in Alzheimer’s disease and vascular dementia. [(accessed on 4 November 2021)];Neurosci. Lett. 1995 183:43–45. doi: 10.1016/0304-3940(94)11110-5. Available online: https://pubmed.ncbi.nlm.nih.gov/7746484/ [DOI] [PubMed] [Google Scholar]
- 14.Lee J.M., Blennow K., Andreasen N., Laterza O., Modur V., Olander J., Gao F., Ohlendorf M., Ladenson J.H. The brain injury biomarker VLP-1 is increased in the cerebrospinal fluid of Alzheimer disease patients. [(accessed on 4 November 2021)];Clin. Chem. 2008 54:1617–1623. doi: 10.1373/clinchem.2008.104497. Available online: https://pubmed.ncbi.nlm.nih.gov/18703769/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ishizuka K., Kimura T., Igata-Yi R., Katsuragi S., Takamatsu J., Miyakawa T. Identification of monocyte chemoattractant protein-1 in senile plaques and reactive microglia of Alzheimer’s disease. [(accessed on 4 November 2021)];Psychiatry Clin. Neurosci. 1997 51:135–138. doi: 10.1111/j.1440-1819.1997.tb02375.x. Available online: https://pubmed.ncbi.nlm.nih.gov/9225377/ [DOI] [PubMed] [Google Scholar]
- 16.Crols R., Saerens J., Noppe M., Lowenthal A. Increased GFAp levels in CSF as a marker of organicity in patients with Alzheimer’s disease and other types of irreversible chronic organic brain syndrome. [(accessed on 4 November 2021)];J. Neurol. 1986 233:157–160. doi: 10.1007/BF00314423. Available online: https://pubmed.ncbi.nlm.nih.gov/3522811/ [DOI] [PubMed] [Google Scholar]
- 17.Sweeney M.D., Sagare A.P., Zlokovic B.V. Blood-brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. [(accessed on 4 November 2021)];Nat. Rev. Neurol. 2018 14:133–150. doi: 10.1038/nrneurol.2017.188. Available online: https://pubmed.ncbi.nlm.nih.gov/29377008/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Janelidze S., Stomrud E., Palmqvist S., Zetterberg H., van Westen D., Jeromin A., Song L., Hanlon D., Tan Hehir C.A., Baker D., et al. Plasma β-amyloid in Alzheimer’s disease and vascular disease. Sci. Rep. 2016;6:26801. doi: 10.1038/srep26801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olsson B., Lautner R., Andreasson U., Öhrfelt A., Portelius E., Bjerke M., Hölttä M., Rosén C., Olsson C., Strobel G., et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: A systematic review and meta-analysis. Lancet Neurol. 2016;15:673–684. doi: 10.1016/S1474-4422(16)00070-3. [DOI] [PubMed] [Google Scholar]
- 20.Hill E., Goodwill A., Gorelik A., Szoeke C. Diet and biomarkers of Alzheimer’s disease: A systematic review and meta-analysis. Neurobiol. Aging. 2019;76:45–52. doi: 10.1016/j.neurobiolaging.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Rehiman S.H., Lim S.M., Neoh C.F., Majeed A.B., Chin A.V., Tan M.P., Kamaruzzaman S.B., Ramasamy K. Proteomics as a reliable approach for discovery of blood-based Alzheimer’s disease biomarkers: A systematic review and meta-analysis. Ageing Res. Rev. 2020;60:101066. doi: 10.1016/j.arr.2020.101066. [DOI] [PubMed] [Google Scholar]
- 22.Davies G., Lam M., Harris S.E., Trampush J.W., Luciano M., Hill W.D., Hagenaars S.P., Ritchie S.J., Marioni R.E., Fawns-Ritchie C., et al. Study of 300,486 individuals identifies 148 independent genetic loci influencing general cognitive function. Nat. Commun. 2018;9:1–16. doi: 10.1038/s41467-018-04362-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Savage J.E., Jansen P.R., Stringer S., Watanabe K., Bryois J., de Leeuw C., Nagel M., Awasthi S., Barr P.B., Coleman J.R.I., et al. Genome-wide association meta-analysis in 269,867 individuals identifies new genetic and functional links to intelligence. Nat. Genet. 2018;50:912–919. doi: 10.1038/s41588-018-0152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hofer E., Roshchupkin G.V., Adams H.H.H., Knol M.J., Lin H., Li S., Zare H., Ahmad S., Armstrong N.J., Satizabal C.L., et al. Genetic correlations and genome-wide associations of cortical structure in general population samples of 22,824 adults. Nat. Commun. 2020;11:1–16. doi: 10.1038/s41467-020-18367-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grasby K.L., Jahanshad N., Painter J.N., Colodro-Conde L., Bralten J., Hibar D.P., Lind P.A., Pizzagalli F., Ching C.R.K., McMahon M.A.B., et al. The genetic architecture of the human cerebral cortex. Science. 2020;367 doi: 10.1126/science.aay6690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Satizabal C.L., Adams H.H.H., Hibar D.P., White C.C., Knol M.J., Stein J.L., Scholz M., Sargurupremraj M., Jahanshad N., Roshchupkin G.V., et al. Genetic architecture of subcortical brain structures in 38,851 individuals. Nat. Genet. 2019;51:1624–1636. doi: 10.1038/s41588-019-0511-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Webster J.A., Gibbs J.R., Clarke J., Ray M., Zhang W., Holmans P., Rohrer K., Zhao A., Marlowe L., Kaleem M., et al. Genetic Control of Human Brain Transcript Expression in Alzheimer Disease. Am. J. Hum. Genet. 2009;84:445–458. doi: 10.1016/j.ajhg.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berchtold N.C., Cribbs D.H., Coleman P.D., Rogers J., Head E., Kim R., Beach T., Miller C., Troncoso J., Trojanowski J.Q., et al. Gene expression changes in the course of normal brain aging are sexually dimorphic. Proc. Natl. Acad. Sci. USA. 2008;105:15605–15610. doi: 10.1073/pnas.0806883105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ritchie M.E., Phipson B., Wu D., Hu Y., Law C.W., Shi W., Smyth G.K. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raudvere U., Kolberg L., Kuzmin I., Arak T., Adler P., Peterson H., Vilo J. g:Profiler: A web server for functional enrichment analysis and conversions of gene lists (2019 update) Nucleic Acids Res. 2019;47:W191–W198. doi: 10.1093/nar/gkz369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kamimura K., Maeda N. Glypicans and Heparan Sulfate in Synaptic Development, Neural Plasticity, and Neurological Disorders. Front. Neural Circuits. 2021;15:15. doi: 10.3389/fncir.2021.595596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lugert S., Kremer T., Jagasia R., Herrmann A., Aigner S., Giachino C., Mendez-David I., Gardier A.M., Carralot J.P., Meistermann H., et al. Glypican-2 levels in cerebrospinal fluid predict the status of adult hippocampal neurogenesis. Sci. Rep. 2017;7:46543. doi: 10.1038/srep46543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Rojas I., Moreno-Grau S., Tesi N., Grenier-Boley B., Andrade V., Jansen I.E., Pedersen N.L., Stringa N., Zettergren A., Hernández I., et al. Common variants in Alzheimer’s disease and risk stratification by polygenic risk scores. Nat. Commun. 2021;12:3417. doi: 10.1038/s41467-021-22491-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shen L., Yao X. Biomarkers. Poster presentations Biomarkers (non-neuroimaging)/Differential diagnosis Integrative analysis of summary data from GWAS and eQTL studies predicts tissue-specific gene targets for Alzheimer’s disease. Alzheimer’s Dement. 2020;16 doi: 10.1002/alz.043242. [DOI] [Google Scholar]
- 35.Whelan C.D., Mattsson N., Nagle M.W., Vijayaraghavan S., Hyde C., Janelidze S., Stomrud E., Lee J., Fitz L., Samad T.A., et al. Multiplex proteomics identifies novel CSF and plasma biomarkers of early Alzheimer’s disease. Acta Neuropathol. Commun. 2019;7:169. doi: 10.1186/s40478-019-0795-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Horssen J., Wesseling P., Van Den Heuvel L.P.W.J., De Waal R.M.W., Verbeek M.M. Heparan sulphate proteoglycans in Alzheimer’s disease and amyloid-related disorders. Lancet Neurol. 2003;2:482–492. doi: 10.1016/S1474-4422(03)00484-8. [DOI] [PubMed] [Google Scholar]
- 37.Sierksma A., Lu A., Mancuso R., Fattorelli N., Thrupp N., Salta E., Zoco J., Blum D., Buée L., De Strooper B., et al. Novel Alzheimer risk genes determine the microglia response to amyloid-β but not to TAU pathology. EMBO Mol. Med. 2020;12:e10606. doi: 10.15252/emmm.201910606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O’Callaghan P., Sandwall E., Li J.-P., Yu H., Ravid R., Guan Z.-Z., van Kuppevelt T.H., Nilsson L.N.G., Ingelsson M., Hyman B.T., et al. Heparan Sulfate Accumulation with Aβ Deposits in Alzheimer’s Disease and Tg2576 Mice is Contributed by Glial Cells. Brain Pathol. 2008;18:548–561. doi: 10.1111/j.1750-3639.2008.00152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Madrid L., Moreno-Grau S., Ahmad S., González-Pérez A., de Rojas I., Xia R., Adami P.V.M., García-González P., Kleineidam L., Yang Q., et al. Multiomics integrative analysis identifies APOE allele-specific blood biomarkers associated to Alzheimer’s disease etiopathogenesis. Aging. 2021;13:9277–9329. doi: 10.18632/aging.202950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen J.-F., Liu K., Hu B., Li R.-R., Xin W., Chen H., Wang F., Chen L., Li R.-X., Ren S.-Y., et al. Enhancing myelin renewal reverses cognitive dysfunction in a murine model of Alzheimer’s disease. Neuron. 2021;109:2292–2307.e5. doi: 10.1016/j.neuron.2021.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hudák A., Jósvay K., Domonkos I., Letoha A., Szilák L., Letoha T. The Interplay of Apoes with Syndecans in Influencing Key Cellular Events of Amyloid Pathology. Int. J. Mol. Sci. 2021;22:7070. doi: 10.3390/ijms22137070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng F., Fransson L.Å., Mani K. Reversal of apolipoprotein E4-dependent or chemical-induced accumulation of APP degradation products by vitamin C-induced release of heparan sulfate from glypican-1. Glycobiology. 2021;31:800–811. doi: 10.1093/glycob/cwaa120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is available as Supplementary material.