Abstract
Background: Multiple measures introduced early to restrict COVID-19 have dramatically impacted the teaching of medical and pharmacy students, exacerbated by the lack of infrastructure and experience with e-learning at the start of the pandemic. In addition, the costs and reliability of the Internet across Africa pose challenges alongside undertaking clinical teaching and practical programmes. Consequently, there is a need to understand the many challenges and how these were addressed, given increasingly complex patients, to provide future direction. Method: An exploratory study was conducted among senior-level medical and pharmacy educators across Africa, addressing four key questions, including the challenges resulting from the pandemic and how these were dealt with. Results: Staff and student members faced multiple challenges initially, including adapting to online learning. In addition, concerns with the lack of equipment (especially among disadvantaged students), the costs of Internet bundles, and how to conduct practicals and clinical teaching. Multiple activities were undertaken to address these challenges. These included training sessions, developing innovative approaches to teaching, and seeking ways to reduce Internet costs. Robust approaches to practicals, clinical teaching, and assessments have been developed. Conclusions: Appreciable difficulties to teaching arising from the pandemic are being addressed across Africa. Research is ongoing to improve education and assessments.
Keywords: Africa, COVID-19, cross country learning, e-learning, hybrid approaches, Internet platforms, mental health, medical education, pharmacy education
1. Introduction
Currently, the highest prevalence worldwide for both infectious diseases and non-communicable diseases (NCDs), as well as patients with multiple co-morbidities, including both infectious and non-infectious diseases, is found in Africa [1,2,3,4,5,6]. The prevention and management of these patients, especially those with multiple co-morbidities, will require an improved understanding of the causal determinants of individual and overlapping diseases, including potential genetic factors [7]. Alongside this, there can be co-payment issues in a number of African countries, which can also have catastrophic consequences on patients and their families [8,9,10,11,12]. Consequently, healthcare professionals (HCPs), especially physicians and pharmacists, across Africa need to be aware of potential multiple co-morbidities among their patients and their subsequent impact on patient management, as well as the costs of medicines prescribed, to improve outcomes; however, this is not always the case [13].
There are also growing concerns with high levels of inappropriate prescribing and dispensing of antimicrobials across Africa [14,15,16,17,18,19,20,21,22]. Unless addressed, this will increase antimicrobial resistance (AMR) rates, increasing morbidity, mortality, and costs [17,23,24,25]. However, the availability of trained pharmacists, coupled with the awareness of current regulations, can reduce inappropriate dispensing of antibiotics without a prescription, as seen in Kenya and Namibia [17,26,27,28], similar to other low- and middle-income countries (LMICs) [29]. For this to routinely happen, though, pharmacy education needs to be strengthened across Africa [14,30,31]. This is particularly important at this time since concerns with inappropriate prescribing and dispensing of antimicrobials across Africa have been enhanced by the COVID-19 pandemic [9,32]. Published studies suggest that 70% or more of patients with COVID-19 have received antibiotics even when not clinically indicated [33,34,35,36,37,38]. This is because less than 10% of patients with COVID-19 appear to have either fungal or bacterial co-infections warranting an antimicrobial, driving up AMR rates [39,40,41].
Alongside this, we are aware that the early instigation of preventative measures for COVID-19 across Africa has appreciably reduced routine immunisation among children, driving up future morbidity and mortality [42,43]. Lockdown and other measures, including services paused at clinics, have also increased NCD morbidity and mortality across countries [43,44,45,46]. Community pharmacists can play a key role in addressing these concerns by making vaccination services routinely available in pharmacies, ensuring patients receive their prescribed medicines on time, providing routine health checks, and instigating pertinent interventions to enhance future adherence to prescribed medicines [47,48,49]. This, though, will require appropriate training to fully implement.
Similar to other countries and continents, the pandemic has not only seriously affected people’s lives but also disrupted traditional educational approaches across Africa [43,50]. Among higher education institutions across Africa, there has been a considerable disruption of the academic calendar alongside the temporary closure of institutions. This has resulted in a stressful situation for teaching staff, parents, and students [51], which needs to be addressed going forward.
Adequate training of physicians and pharmacists is essential to deal with increasingly complex cases across Africa given the increasing prevalence of diseases and patients with co-morbidities [7,52,53,54,55]. This is seen as particularly important during the COVID-19 pandemic given the extent of misinformation that exists regarding possible medicines for the prevention and treatment of COVID-19 and their consequences [9,56]. In addition, as mentioned, the extent of inappropriate prescribing and dispensing of antibiotics for viral infections which increases AMR, necessitating pragmatic approaches to address this [17,39].
However, advancing medical and pharmacy education during the pandemic has been a major challenge across countries including African countries [50,57,58]. In the midst of the COVID-19 pandemic, universities across Africa had to respond quickly by offering online classes/courses and practical sessions for healthcare students, and these often had to be offered in smaller groups. The need for practical skills training for physicians and pharmacists is essential to enable them to perform their clinical roles, recognising that delivering both didactic and practice learning remotely is challenging. This meant that both faculty members and students had to firstly become familiar with new technologies and platforms if not already familiar with them, and faculty members needed to deliver lectures and practicals safely whilst preserving the quality and consistency of educational processes as much as possible. Students also needed to cope with issues of Internet connectivity and access to computers to fully participate in e-learning approaches [59,60,61,62,63,64,65,66,67]. The financial challenges that this situation imposed among both staff members and students across Africa were quite considerable. This was in addition to the lack of suitable equipment and facilities for online learning among many African students, especially disadvantaged students, certainly initially [68] (Table 1).
Table 1.
Summary of challenges and activities among faculty and students across Africa in response to the COVID-19 pandemic.
| Location | Challenges | Activities | |||||
|---|---|---|---|---|---|---|---|
| Transferring Courses Online | Staff Skills at the Outset of the Pandemic |
Reliability/ Cost of Internet |
Concerns with Practical Skills Learning/Good Communication between Students and Staff |
Rapid Adaptation to e-Learning, Including Virtual Platforms/ Sourcing ICT Devices |
Providing Positive Learning Experiences/Good Communication with Students |
Adapting Frameworks/ Additional Security Measures for Assessing Students |
|
| North Africa | √ | √ | √ | √ | √ | ||
| East Africa | √ | √ | √ | ||||
| Central Africa | √ | √ | √ | ||||
| Southern Africa | √ | √ | √ | √ | √ | √ | √ |
| Western Africa | √ | √ | √ | √ | √ | ||
NB: ICT = Information and communications technology.
Agreed standards are also increasingly needed to enhance online learning experiences given the current challenges, including successfully transferring courses and assessments online [61,69,70,71]. Alongside this, as mentioned, there must be good availability and access to the Internet and appropriate software packages, as well as availability of computers among students, especially those from disadvantaged backgrounds, to facilitate e-learning [50,61,62,71,72,73]. However, this was not always the case (Table 1, Supplementary Table S1 with Supplementary Table S1 containing more details for each location). Key challenges across Africa at the start of the pandemic included the need to rapidly improve staff skills to transfer courses online, the lack of suitable technology equipment among students, and the costs and availability of the Internet, as well as how to conduct practicals within COVID-19 restrictions (Table 1).
We have seen similar responses in high-income countries, including Saudi Arabia in the neighbouring region to Africa, in terms of closing medical and pharmacy schools during the early months of the pandemic and suspending all face-to-face classes. However, medical and pharmacy education in Saudi Arabia has been facilitated by significant investment in e-learning management systems and technological innovations over the years, providing direction to others [74]. Box 1 contains further details of ongoing activities across Saudi Arabia to enhance physician and pharmacy education during the COVID-19 pandemic. We are also seeing a rise in the use of technologies such as telemedicine or remote education platforms to address skill concerns among healthcare students across countries, and this will grow [75].
Box 1. Activities across Saudi Arabia to enhance e-learning and address the challenges posed by the COVID-19 pandemic.
There has been considerable investment in recent years in the e-learning infrastructure among Saudi Universities. This includes the establishment of Deanships/Centres of e-learning and distance education, enhancing a smooth transition during the pandemic [74,76].
Alongside this, e-learning management systems, online platforms, and other technological infrastructures, e.g., BlackBoard™, online apps, and platforms for collaboration and video calls, as well as other technological infrastructures put in place, including Zoom®, Microsoft Teams, and Webex® [74,76,77,78].
In 2020–2021, the Saudi Ministry of Education instructed universities to adapt a blended learning model in which all theoretical components of the curriculum should be delivered online and practical component/skills delivered on campus whenever applicable, taking all the precautionary and preventive measures [79]. This resulted in the King Saudi University (KSU) College of Medicine delivering the theoretical parts of courses online using BlackBoard™ and Zoom® platforms, with problem-based learning (PBL) shifted online using small groups [77].
Practical sessions have been classified into three categories depending on the most suitable mode of delivery—these include on-campus sessions in the labs and virtual sessions via online platforms or video demonstrations uploaded in the e-learning systems. For clinical teaching, more priority has been given to final-year medical students to be trained at the KSU medical city, while for other years, training and education has been conducted mainly in the Clinical Skills and Simulation Centre (CSSC) at the college with provisions to provide adequate orientation to the faculty members and students regarding educational and training activities to ensure smooth running of the programme [77].
In the case of pharmacy students, the use of videos has been explored to provide demonstrations of experiments, especially during the closure of colleges in the initial months [71]. This was subsequently re-visited after restrictions were eased, with the adoption of a blended learning model similar to the model for medical education.
The safe return to university campus education was implemented under the theme “Cautiously We Return” with a key aim to implement the practical and clinical components of the curriculum as well as examinations on campus—facilitated by adopting digital health technologies and applications introduced in the early phases of the pandemic to mitigate risks, e.g., all members (faculty, students and other employees) in all Saudi universities had to have an activated Tawakkalna app on their smartphones to enable entry to the universities. The Tawakkalna app is an official app and includes many advanced digital services with a high level of security and privacy features, with the app showing the current health status of the users (i.e., infected, not infected), any recent contact with an infected individual, and their COVID-19 vaccination status (i.e., fully vaccinated, vaccinated with the first dose, not vaccinated) based on Ministry of Health data through encrypted personal data [80].
Several studies have now taken place exploring the experiences of university students. They have generally reported positive experiences with e-learning and distance education during the COVID-19 pandemic in view of the investments made [71,78,79,81,82], with continued ongoing research in this area. However, this is not universal, with concerns with technical support and access to the Internet found among some medical students in Saudi Arabia [83].
We have also seen advances in e-learning approaches among a number of countries, including higher-income countries, to devise different teaching approaches. These include mobile applications for practical sessions, addressing concerns with e-exams, and universities combining to offer virtual microscopy and Zoom videoconferencing to teach pathology [84,85,86,87]. The situation in these countries, as well as Saudi Arabia (Box 1), can be different to experiences in Jordan and other LMICs with appreciably fewer resources to instigate e-learning and other approaches [50,88,89,90], as well as across Africa (Table 1).
Consequently, given the many challenges facing medical and pharmacy training in Africa during the pandemic, including pre-clinical activities [91] (Table 1), coupled with the urgency of the situation given the increasing complexity of patients across Africa, we believed it was necessary to document ongoing activities among African countries to improve medical and pharmacy education during the pandemic and the lessons learnt.
We were aware of a number of innovations across Africa during the early stages of the COVID-19 pandemic to improve patient care. These included developing finger-prick tests to rapidly detect antibodies; developing mobile apps for contact tracing, triaging, and case management; early sequencing of the genomes of SARS-CoV-2; and the development of non-invasive respirators given initial global shortages [43,92]. We now wanted to document initiatives regarding medical and pharmacy education during the pandemic across Africa, given that e-learning and other digital technologies are here to stay [93,94,95]. We believe this is the first time that such activities have been reviewed across a continent rather than individual countries, which should add strength to any future recommendations. The objective being to facilitate countries, especially African countries, to learn from each other [91,96].
We also recognise the need for students and faculty members to continually re-evaluate the changes in their educational approaches and assessment processes as the pandemic continues in order to effectively address continued challenges [97]. Alongside this, there is a need to adapt approaches to address identified gaps including improving self-regulated behaviour, with students looking out for each other [98,99,100,101,102,103]. We further recognise that preceptors should be open-minded and consider how students can participate in service provision, such as clinical pharmacy services, during pandemics [104]. This includes a greater use of virtual communication, including potentially with patients, access to electronic health records remotely where these exist to enhance analysis and treatment skills, and greater flexibility in teaching methods [104,105].
As a result, we believed it was important that there was increased understanding of the “new normal” in moving forward as a continent educating future physicians and pharmacists. This is seen as essential not only in the current pandemic but also considering the possibilities for future pandemics. Consequently, this paper sets out to understand the many challenges faced by senior-level personnel from different universities across Africa, particularly in medical and pharmacy education, as a result of the COVID-19 pandemic, and how these have been dealt with, in order to share lessons learnt and the implications for the future to improve student education. This also includes suggested research activities for the future.
2. Materials and Methods
This was principally an exploratory study among senior-level medical and pharmacy educators across Africa during the current COVID-19 pandemic, using an analytical framework with a pragmatic paradigm approach to provide future direction [106,107]. The African countries chosen provided a range of geographies, economic status (Gross Domestic Product—GDP/capita [108]), and population size [109] (Table 2).
Table 2.
Current GDP/capita and population size among participating African countries.
| Country | GDP/Capita (USD) | Population Size |
|---|---|---|
| Malawi | 625.3 | 19,129,952 |
| Uganda | 817.0 | 45,741,007 |
| Zambia | 1050.9 | 18,383,955 |
| Tanzania | 1076.5 | 59,734,218 |
| Zimbabwe | 1128.2 | 14,862,924 |
| Cameroon | 1499.4 | 26,545,863 |
| Kenya | 1838.2 | 53,771,296 |
| Nigeria | 2097.1 | 206,139,589 |
| Ghana | 2328.5 | 31,072,940 |
| Eswatini | 3415.5 | 1,160,164 |
| Namibia | 4211.1 | 2,540,905 |
| South Africa | 5090.7 | 59,308,690 |
| Botswana | 6711.0 | 2,351,627 |
Similar approaches have previously been adopted when documenting activities across Africa to combat both infectious and non-infectious diseases [4,9,14,43,110,111,112].
The questionnaire was developed following an analysis of the literature regarding key points, concerns, and activities with respect to changes in medical and pharmacy education resulting from lockdown and other measures to combat the COVID-19 pandemic (Table 1, Supplementary Table S1). Four key questions were contained in the questionnaire to address the aims and objectives of the study. These were:
What challenges has COVID-19 presented to health sciences education?
How did health sciences institutions respond immediately to the challenges presented by the COVID-19 pandemic in your country (principally medical and pharmacy education)?
What support was harnessed to help mitigate against the challenges faced by higher learning institutions?
What are the lessons that can be learnt to prepare higher learning institutions in the education of particularly physicians and pharmacists for future pandemics?
The questionnaire was subsequently distributed to senior-level co-authors in each participating country using a purposeful sampling approach [113]. The co-authors subsequently collated the replies based on their experiences, local reports, and internal institutional consultations in their own countries, most of which they were heavily involved with. In some countries, including Ghana, Nigeria, South Africa, and Zimbabwe, multiple institutions were approached with the findings initially collated and reviewed by the principal author (B.G.) with the help of the co-authors from that country. The replies to the questions were discussed among the multiple co-authors and the principal co-author until a consensus was reached. In countries with only one principal university teaching medicine and pharmacy, only one university was approached, e.g., Botswana, Eswatini, and Namibia. The lead author in that country typically collated the comments from the multiple co-authors; alternatively, the co-authors built and refined their comments, building on others in that country. As a result, a consensus was reached among all participating countries. This reflects the exploratory nature of this study coupled with its aims and objectives.
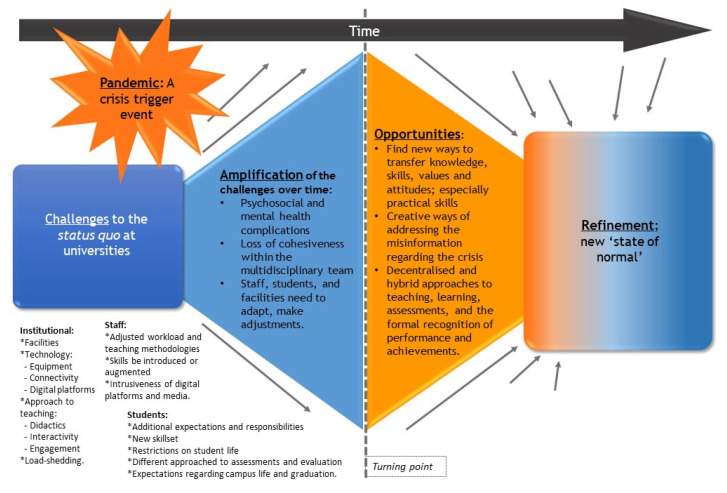
The responses were analysed using thematic analysis techniques [114,115]. Common themes across Africa in response to the four key questions were identified and subsequently collated by the co-authors, combined with other colleagues in some cases, to provide future direction (Figure 1). These built on the comprehensive answers to the four questions by the senior-level co-authors among the various African countries.
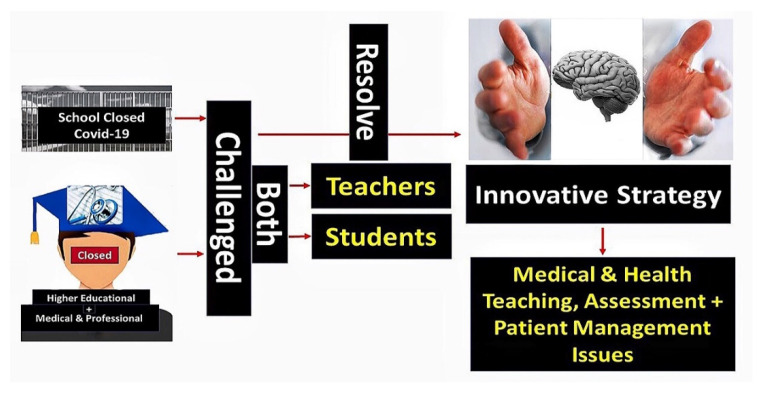
Figure 1.
Key challenges and future opportunities arising from the COVID-19 pandemic.
3. Results
The COVID-19 pandemic has resulted in considerable challenges, barriers, and shifts in the way that medical and pharmacy education are now practised among universities across Africa (Figure 2). We will split the findings down into the four questions before consolidating the findings to provide future guidance.
Figure 2.
COVID-19 and the impact on medical and pharmacy education across Africa.
3.1. What Challenges Has COVID-19 Presented to Health Sciences Education?
Table 3 provides details from respondents about the range of challenges they faced regarding the education of medical and pharmacy students. Challenges across Africa included the need for both staff and students to quickly adapt to online learning, concerns with the lack of available equipment, and the costs of Internet bundles. Alongside this, there were concerns with how to undertake practical sessions, clinical teaching, and examinations during lockdown restrictions alongside instigating problem-based learning approaches. These built off challenges discussed in Table 1. Supplementary Table S2 provides greater details for each African country.
Table 3.
Summary of key challenges faced by universities and students across Africa as a result of the pandemic.
| Country | Teaching and Learning Challenges | Resource Issues |
|||||
|---|---|---|---|---|---|---|---|
| Disruption of the Academic Calendar/ Limited Experiences with e-Learning, Shortages of Staff |
Lack of Suitable ICT Equipment, Literacy, and the Need for Hybrid Learning |
Lack of Reliable Internet Facilities/ Challenges with Home Learning |
Concerns with Practical Skills Learning as Well as Face-to-Face Learning |
Instigation of Problem-Based Learning to Address Lack of Face-to-Face Learning |
Quality Assessment/ Robustness of Examinations |
Cost of Internet/ Facilities |
|
| Botswana | √ | √ | √ | √ | √ | ||
| Cameroon | √ | √ | √ | √ | |||
| Eswatini | √ | √ | √ | √ | √ | √ | |
| Ghana | √ | √ | √ | √ | √ | ||
| Kenya | √ | √ | √ | √ | √ | √ | |
| Malawi | √ | √ | √ | √ | |||
| Namibia | √ | √ | √ | √ | √ | √ | √ |
| Nigeria | √ | √ | √ | √ | √ | √ | |
| South Africa | √ | √ | √ | √ | √ | ||
| Uganda | √ | √ | √ | √ | √ | √ | |
| Zambia | √ | √ | √ | √ | √ | √ | |
| Zimbabwe | √ | √ | √ | √ | √ | ||
3.2. How Did Health Sciences Institutions Respond Immediately to the Challenges Presented by the COVID-19 in Your Country (Principally Medical and Pharmacy Education)?
Table 4 summarises the various ways in which the universities across Africa immediately responded to the challenges in medical and pharmacy education as a result of lockdown and other measures, with greater details in Table S3.
Table 4.
Summary of immediate responses among institutions across Africa to the pandemic and its impact on educational approaches for physicians and pharmacists.
| Country | Responses to Teaching | Responses to Practicals and Clinical Teaching | |||
|---|---|---|---|---|---|
| Extensive Use of e-Learning Approaches, Including Remote Teaching and Blending/ Training of Staff |
Regular Adjustments of Academic Calendars/ Teaching Schedules |
Instigation of Social Distancing/ Sanitation Measures for Lectures |
Modification of Practicals/Contact between Students and Patients | Adaptive Approaches, Including Systematic Reviews in Small Groups/Interactive Videos/Use of Workbooks |
|
| Botswana | √ | √ | √ | √ | |
| Cameroon | √ | √ | |||
| Eswatini | √ | √ | √ | √ | |
| Ghana | √ | √ | √ | √ | |
| Kenya | √ | √ | √ | √ | √ |
| Malawi | √ | √ | √ | ||
| Namibia | √ | √ | √ | √ | √ |
| Nigeria | √ | √ | √ | √ | √ |
| South Africa | √ | √ | √ | √ | √ |
| Zambia | √ | √ | √ | √ | |
| Zimbabwe | √ | √ | √ | √ | |
This typically included extensive use of remote teaching involving the education of both staff and students. In addition, adjustments were made to the teaching schedules to take into account the new environment, as well as adjustments to practical and teaching programmes to take into account social distancing and other regulations.
3.3. What Support Was Harnessed to Help Mitigate against the Challenges Faced by Higher Learning Institutions?
Table 5 discusses the support that was harnessed by the various institutions across Africa in response to the pandemic. This included entering into agreements with Internet providers to help with the costs of e-learning approaches for medical and pharmacy students, as well as improved sanitation and hand-washing facilities. Some universities also provided psychological and moral support to staff and students to help address ongoing challenges.
Table 5.
Examples of support and other measures harnessed by health science institutions across Africa in response to the pandemic.
| Country | Support |
|---|---|
| Botswana |
|
| Cameroon |
|
| Eswatini |
|
| Ghana |
|
| Kenya |
|
| Malawi |
|
| Namibia |
|
| Nigeria |
|
| South Africa |
|
| Tanzania |
|
| Zambia |
|
| Zimbabwe |
|
NB: ICT = Information and communications technology; PPE = Personal protective equipment.
3.4. What Are the Lessons That Can Be Learnt to Prepare Higher Learning Institutions in the Education of Physicians and Pharmacists for Future Pandemics?
Table 6 discusses the lessons that have been learnt regarding the future education of medical and pharmacy students during a pandemic and beyond. This includes the fact that theoretical teaching can be smoothly taught virtually, with blended learning here to stay. However, this needs investment in skills and equipment, as well as increasing the Internet reliability and coverage and reductions in the costs of Internet bundles. Institutions also need to be made safe for future pandemics, and there needs to be greater psychological and other support for both students and staff going forward. Medical and pharmacy institutions also need to continually develop and adapt pertinent tools for practicals, clinical teaching, and examinations to address current challenges.
Table 6.
Lessons learnt from the pandemic among institutions providing medical and pharmacy education across Africa.
| Country | Lessons Learnt |
|---|---|
| Botswana |
|
| Cameroon |
|
| Eswatini |
|
| Ghana |
|
| Kenya |
|
| Malawi |
|
| Namibia |
|
| Nigeria |
|
| South Africa |
|
| Tanzania |
|
| Uganda |
|
| Zambia |
|
| Zimbabwe |
|
NB: ICT = Information and communications technology; HCP = Healthcare professionals.
3.5. Consolidated Findings and Their Implications
A number of common themes were identified regarding the impact of the COVID-19 pandemic on medical and pharmacy education across Africa as well as potential ways forward. These build on Table 3, Table 4, Table 5 and Table 6 and Box 1. They are consolidated in Table 7 to provide guidance to key stakeholders in Africa and the wider world experiencing similar problems with physician and pharmacy education.
Table 7.
Common themes regarding the impact of challenges of the COVID-19 pandemic on teaching practices and the lessons learnt.
| Question | Common Themes |
|---|---|
| Challenges faced by universities during the pandemic |
|
| Responses by health science institutions to the pandemic |
|
| How support was harnessed to help mitigate against the pandemic |
|
| Lessons learnt and ways forward |
|
4. Discussion
There is no doubt that the COVID-19 pandemic, along with measures to slow its spread across Africa—incorporating early lockdown alongside other measures, including closure of borders and higher education institutions [43,92]—has caused considerable challenges for higher education across Africa (Table 1). This is similar to many other countries [50,85,86,87,98,118].
We believe this is the first time that the implications of these multiple measures on higher institution learning, especially for medical and pharmacy students, and ways forward have been assessed across a single continent, Africa, with its considerable challenges before the start of the COVID-19 pandemic. We believe this was important given the many public health and other challenges across Africa, which include the increasing complexity of patients exacerbated by the growing number of patients with multiple co-morbidities and the challenges this brings, such as the need to consider multiple guidelines simultaneously to appropriately manage these complex cases [55,119,120,121,122]. Alongside this, concerns with the lack of ICT infrastructures and e-learning facilities among many universities in African countries before the start of the pandemic (Table 1).
Concerns with the education of physicians and pharmacists across Africa arising from the pandemic were exacerbated by the initial challenges of translating lectures to online, the lack of familiarity with online e-learning platforms among many faculty members and students, and, as mentioned, poor ICT infrastructures among many African countries (Table 1 and Table 3). This is similar to other LMICs, including Jordan [50,88,123]. There was also a considerable unplanned financial burden among both universities and students at the start of the pandemic with the need to purchase computers, tablets, and other ICT support systems necessary for e-learning, as well as the cost of Internet bundles and user fees among staff and students. These factors affected all key stakeholders involved in HCP education across Africa at the start of the pandemic. This included governments, non-governmental organisations, and the private sector, as well as the institutions, staff, and students (Table 1 and Table 3). The situation regarding medical and pharmacy education at the start of the pandemic was different, though, in Saudi Arabia, with greater infrastructure initially with its greater resources (Box 1). However, despite this, there were still a number of issues that needed addressing in Saudi Arabia at the start of the pandemic, including the optimal blending of online and face-to-face teaching, with the findings from recent studies likely to influence future teaching approaches (Box 1).
Table 3 and Table 7 document the many barriers and challenges faced by universities and higher education institutions across Africa at the start of the pandemic, especially for medical and pharmacy students. These include addressing concerns with the lack of infrastructure and competency in e-learning approaches. In addition, there were concerns about shortages of ICT equipment, especially among disadvantaged students, as well as the cost of Internet bundles. Alongside this, coping with learning at home given competing demands and the availability of quiet places to teach and learn were significant concerns. There were also concerns with conducting practicals and clinical teaching sessions with social distancing and other measures in place, including WASH, which necessitated breaking students down into smaller groups [77]. In addition, there were concerns with the need for greater investment in simulation-based learning (SBL) although countries are learning from each other to address this.
Table 4, Table 5 and Table 7 discuss the different responses among the various institutions across Africa to address these multiple challenges. These included instigating training seminars, webinars, and other types of development platforms for both staff and students, along with developing innovative approaches to e-learning, including the use of videos, turning existing university electronic media into learning management systems, and exploring the potential for hybrid teaching sessions. Whilst this may have incurred initial logistical challenges within universities, faculty development programmes have allowed for more certainty in how to approach new modalities, stimulated the development of future practice approaches, and provided opportunities for professional development [124,125,126]. Alongside this, we are aware of innovative approaches to the training of surgeons in addition to those documented (Table 4, Table 5, Table 6 and Table 7). These include enhancing video platforms and online teaching of instrument identification, suturing, and knot tying [127,128,129].
By allowing for the continuous development of academics’ educational toolboxes, opportunities arise not only for engaging with new fields of research but also for enhancing preparedness for future disruptions, including future pandemics. Capacity building was also important among countries given concerns with the lack of investment over a number of years among some of the African universities at the start of the pandemic, which are now being addressed. Flexibility was also seen as key, including calendar adjustments, given the different circumstances among the students, with some students struggling to adjust to online learning. Governments and universities also need to work more closely in the future with Internet providers to address concerns with the cost of Internet bundles.
Encouragingly, developments in e-learning and other approaches are taking place across Africa to address the many highlighted challenges (Table 4, Table 5 and Table 7). New ways to assess students have also been developed whilst seeking ways to maintain the robustness and integrity of the assessment systems. This is because security and rigour of assessments were noted as a general concern among academics in Africa early on in the pandemic, mirroring other countries [86]. These concerns are largely due to the necessary transition to online platforms, which cannot always be invigilated, and the requirement that physical assessments must be conducted outside of the authentic environment during any pandemic, e.g., objective-structured clinical assessments. Although institutions have done much to implement a variety of quality control processes, mistrust in the process is still evident in a number of African countries, and future research is needed to assess the effectiveness of different strategies to address remaining fears and provide future guidance. We will continue to monitor this. Other potential research activities emanating from African university activities during the pandemic are discussed in Table 8.
Table 8.
Potential research activities to improve the education of medical and pharmacy students during the current and future pandemics.
| Potential Research Projects |
|---|
|
Overall, different approaches have been instigated to ensure medical and pharmacy students are equipped as much as possible with the necessary skills at graduation (Table 5 and Table 7). This includes a greater need for evidence-based treatment approaches given the discourse surrounding a number of different treatments for patients with COVID-19, including hydroxychloroquine and remdesivir, that failed to improve patient care and, in some cases, actually increased morbidity, mortality, and costs [9,32,56,130,131,132,133,134]. In addition, there is a greater need for effective ways to reduce unnecessary prescribing and dispensing of antibiotics, including in patients with COVID-19, as well as to improve the management of patients with NCDs given concerns with the unintended consequences of the pandemic [17,27,43,44,135].
Table 6 and Table 7 summarise key learnings arising from the challenges posed by the pandemic and how these can be addressed going forward. This includes the fact that theoretical learning can in fact be taught virtually, with this blend of e-learning and face-to-face teaching for medical and pharmacy students here to stay. This pandemic and its consequences have also provided universities across Africa with the potential to re-think their syllabi to include hybrid learning opportunities. However, this will require the necessary infrastructure, equipment, and personnel to effectively take this forward. Activities potentially include establishing e-learning centres within universities where these currently do not exist, developing quality standards for e-learning, providing adequate technological resources, i.e., online platforms, and ensuring the necessary training for faculty members and students. This will require greater collaboration between technology firms within Africa, governments, and the universities, with greater corporate responsibility among companies [73,138]. Internet bundles also need to be affordable to all for hybrid approaches to work in the future. We will also likely see greater collaboration among universities in the future alongside continual research into appropriate teaching methods for this and future pandemics (Table 8). We will also be monitoring this.
The pandemic, including the development of innovative management and treatment approaches [43] coupled with innovative approaches to teaching, has also provided an opportunity for African universities to showcase their skills to attract future investment. We have already seen apps being developed in South Africa to rapidly assess the use of antimicrobials among patients in hospitals given current concerns [17,110,139,140], with such approaches likely to grow, building on the greater use of technologies to manage patient care across Africa and the wider world [43,75,141,142,143].
Innovative ways could also be introduced, including digital solutions, to provide increasing psychological and social support and guidance for staff and students during the pandemic given current concerns [51,65,66,144,145]. The objective being to reduce anxiety, depression, and other mental health issues associated with the pandemic. This is because challenges regarding the mental health and well-being of staff and students was a common observation across Africa (Table 3). Mental health issues among staff and students were generally linked to concerns including uncertainty with the pandemic in terms of altered working conditions. Alongside this, difficulties with maintaining a work–life balance; fear of the implications of the transition to e-learning on teaching, learning, and assessments; and the loss of face-to-face support networks, with burnout of students and lecturers an ongoing concern [146,147,148]. However, we have seen the growth of virtual support networks across universities as well as increased compassion towards one another to help address such issues. This is likely to continue.
We are aware of a number of limitations with this study. These include the fact that we only approached a limited number of universities and other personnel involved in HCP education in each country and no students. In addition, we did not cover all African countries. We also did not undertake a thorough thematic analysis of the answers to the four questions for the reasons stated. However, in view of the seniority of the co-authors and the insights they provided, we believe our findings are robust, providing direction for the future.
5. Conclusions
In conclusion, the pandemic has required higher education institutions across Africa to dramatically change the way in which they approach the training of their HCP students. This includes appreciably increasing hybrid approaches incorporating e-learning coupled with face-to-face teaching where permissible. Alongside this, instigating innovations to help with practicals and clinical teaching, as well as with assessments to ensure their quality and robustness. We have also seen key stakeholder groups come together to address concerns with ICT support for students, especially disadvantaged students, as well as the costs of Internet bundles, with such collaborative approaches likely to grow. Addressing mental health concerns among both students and staff has become increasingly essential during any pandemic, and given the experiences seen during the current pandemic, this will continue.
As the world moves further into the Fourth Industrial Revolution, paradigm shifts will continue to occur. As COVID-19 has shed light on the weaknesses and strengths of educational institutions across Africa and in many cases amplified them, the unique challenges each institution has faced with training their medical and pharmacy students to become fit-for-purpose graduates have become increasingly clear. We have seen different institutions successfully adopt a variety of strategies to address these challenges, with hybrid learning here to stay. Consequently, it is unlikely that institutions across Africa will revert to the same educational strategies that were in place prior to the COVID-19 pandemic, especially with continued investment and research into e-learning opportunities and systems. We will continue to monitor the situation to provide future guidance.
Acknowledgments
We wish to acknowledge Ngozi E. Edwin, Head of the Pharmacy Department at Eswatini Medical Christian University, for providing an interview audience during the data sourcing and collection phase. We also with to acknowledge the help of Mutsa Bwakura-Dangarembizi with comments regarding Zimbabwe.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/healthcare9121722/s1, Supplementary Table S1: Summary of activities and challenges among faculty and students across Africa in response to the COVID-19 pandemic; Supplementary Table S2: Challenges faced by Universities and students across Africa as a result of the pandemic; Supplementary Table S3: Summary of responses am ong institutions across Africa to the pandemic and its impact on educational approaches for physicians and pharmacists.
Author Contributions
A.E., A.A.A. (Adefolarin A. Amu), B.B.B.-B., F.B.T., O.Y.A., and B.G. developed the concept for the paper and orchestrated data collection. A.E., A.A.A., M.H., N.S., A.K., A.A.A. (Alian A. Alrasheedy), A.T., J.C.M. (Julius C. Mwita), G.M.R., O.P., L.L.N., B.B.B.-B., F.B.T., O.Y.A., J.A., R.I., I.A.S., A.N.G., S.O., I.C., F.K. (Felix Khuluza), D.K., F.K. (Francis Kalemeera), E.H., J.L., J.F., O.O.O., Z.S., F.O., W.C., M.M., J.C.M. (Johanna C. Meyer), G.S., A.M., O.O.M., A.C.K., J.S., S.S.B., T.Z., S.C. and B.G. contributed to data collection and analysis and suggested ways forward. B.G. wrote the first draft of the paper, which was critiqued by all authors. B.G. over saw the project. All authors approved the submission. All authors have read and agreed to the published version of the manuscript.
Funding
There was no funding for this research project or the write-up.
Institutional Review Board Statement
No ethical approval was sought as the study did not include patients. In addition, each person voluntarily provided their answers to the four questions. This is in line with similar studies conducted by the co-authors across a range of subjects in Africa and the wider world, including previous research on COVID 19, infectious diseases, and non-infectious diseases, and is in line with institutional guidance [4,9,17,32,43,110,112,149,150,151,152,153,154].
Informed Consent Statement
Not applicable.
Data Availability Statement
All available data are included in the paper.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Modjadji P. Communicable and non-communicable diseases coexisting in South Africa. Lancet Glob. Health. 2021;9:e889–e890. doi: 10.1016/S2214-109X(21)00271-0. [DOI] [PubMed] [Google Scholar]
- 2.Bigna J.J., Noubiap J.J. The rising burden of non-communicable diseases in sub-Saharan Africa. Lancet Glob. Health. 2019;7:e1295–e1296. doi: 10.1016/S2214-109X(19)30370-5. [DOI] [PubMed] [Google Scholar]
- 3.Gouda H.N., Charlson F., Sorsdahl K., Ahmadzada S., Ferrari A.J., Erskine H., Leung J., Santamauro D., Lund C., Aminde L.N., et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: Results from the Global Burden of Disease Study 2017. Lancet Glob. Health. 2019;7:e1375–e1387. doi: 10.1016/S2214-109X(19)30374-2. [DOI] [PubMed] [Google Scholar]
- 4.Godman B., Basu D., Pillay Y., Mwita J.C., Rwegerera G.M., Paramadhas B.D., Tiroyakgosi C., Okwen P.M., Niba L.L., Nonvignon J., et al. Review of Ongoing Activities and Challenges to Improve the Care of Patients With Type 2 Diabetes Across Africa and the Implications for the Future. Front. Pharm. 2020;11:108. doi: 10.3389/fphar.2020.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nkengasong J.N., Tessema S.K. Africa Needs a New Public Health Order to Tackle Infectious Disease Threats. Cell. 2020;183:296–300. doi: 10.1016/j.cell.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mwita J., Godman B. Lifestyle and Epidemiology—Poverty and Cardiovascular Diseases a Double Burden in African Population. IntechOpen; London, UK: 2021. [(accessed on 1 October 2021)]. Poverty and cardiovascular diseases in Sub-Saharan Africa. Available online: https://www.intechopen.com/predownload/772273. [Google Scholar]
- 7.Wong E.B., Olivier S., Gunda R., Koole O., Surujdeen A., Gareta D., Munatsi D., Modise T.H., Dreyer J., Nxumalo S., et al. Convergence of infectious and non-communicable disease epidemics in rural South Africa: A cross-sectional, population-based multimorbidity study. Lancet Glob. Health. 2021;9:e967–e976. doi: 10.1016/S2214-109X(21)00176-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy A., Palafox B., Walli-Attaei M., Powell-Jackson T., Rangarajan S., Alhabib K.F., Avezum A., Calik K.B., Chifamba J., Choudhury T., et al. The household economic burden of non-communicable diseases in 18 countries. BMJ Glob. Health. 2020;5:e002040. doi: 10.1136/bmjgh-2019-002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sefah I., Ogunleye O., Essah D., Opanga S., Rizvi N., Wamaitha A., Chikowe I., Khuluza F., Kibuule D., Nambahu L., et al. Rapid assessment of the potential paucity and price in-creases for suggested medicines and protection equipment for COVID-19 across developing countries with a particular focus on Africa and the implications. Front. Pharmacol. 2021;11:2055. doi: 10.3389/fphar.2020.588106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mapa-Tassou C., Katte J.C., Mba Maadjhou C., Mbanya J.C. Economic Impact of Diabetes in Africa. Curr. Diabetes Rep. 2019;19:5. doi: 10.1007/s11892-019-1124-7. [DOI] [PubMed] [Google Scholar]
- 11.Ngcamphalala C., Ataguba J.E. An assessment of financial catastrophe and impoverishment from out-of-pocket health care payments in Swaziland. Glob. Health Action. 2018;11:1428473. doi: 10.1080/16549716.2018.1428473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aregbeshola B.S., Khan S.M. Out-of-Pocket Payments, Catastrophic Health Expenditure and Poverty Among Households in Nigeria 2010. Int. J. Health Policy Manag. 2018;7:798–806. doi: 10.15171/ijhpm.2018.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fadare J.O., Enwere O.O., Adeoti A.O., Desalu O.O., Godman B. Knowledge and Attitude of Physicians Towards the Cost of Commonly Prescribed Medicines: A Case Study in Three Nigerian Healthcare Facilities. Value Health Reg. Issues. 2020;22:68–74. doi: 10.1016/j.vhri.2020.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Godman B., Haque M., McKimm J., Abu Bakar M., Sneddon J., Wale J., Campbell S., Martin A., Hoxha I., Abilova V., et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: Findings and implications for the future. Curr. Med. Res. Opin. 2019;36:301–327. doi: 10.1080/03007995.2019.1700947. [DOI] [PubMed] [Google Scholar]
- 15.Kalungia A.C., Burger J., Godman B., Costa J.O., Simuwelu C. Non-prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev. Anti-Infect. 2016;14:1215–1223. doi: 10.1080/14787210.2016.1227702. [DOI] [PubMed] [Google Scholar]
- 16.Kibuule D., Kagoya H.R., Godman B. Antibiotic use in acute respiratory infections in under-fives in Uganda: Findings and implications. Expert Rev. Anti-Infect. 2016;14:863–872. doi: 10.1080/14787210.2016.1206468. [DOI] [PubMed] [Google Scholar]
- 17.Godman B., Egwuenu A., Haque M., Malande O., Schellack N., Kumar S., Saleem Z., Sneddon J., Hoxha I., Islam S., et al. Strategies to Improve Antimicrobial Utilization with a Special Focus on Developing Countries. Life. 2021;11:528. doi: 10.3390/life11060528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Batista A.D., Rodrigues D.A., Figueiras A., Zapata-Cachafeiro M., Roque F., Herdeiro M.T. Antibiotic Dispensation without a Prescription Worldwide: A Systematic Review. Antibiotics. 2020;9:786. doi: 10.3390/antibiotics9110786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsitse T.B., Helberg E., Meyer J.C., Godman B., Massele A., Schellack N. Compliance with the primary health care treatment guidelines and the essential medicines list in the management of sexually transmitted infections in correctional centres in South Africa: Findings and implications. Expert Rev. Anti-Infect. 2017;15:963–972. doi: 10.1080/14787210.2017.1382354. [DOI] [PubMed] [Google Scholar]
- 20.Sefah I.A., Essah D.O., Kurdi A., Sneddon J., Alalbila T.M., Kordorwu H., Godman B. Assessment of adherence to pneumonia guidelines and its determinants in an ambulatory care clinic in Ghana: Findings and implications for the future. JAC—Antimicrob. Resist. 2021;3:dlab08. doi: 10.1093/jacamr/dlab080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mashalla Y., Setlhare V., Massele A., Sepako E., Tiroyakgosi C., Kgatlwane J., Chuma M., Godman B. Assessment of prescribing practices at the primary healthcare facilities in Botswana with an emphasis on antibiotics: Findings and implications. Int. J. Clin. Pract. 2017;71:e13042. doi: 10.1111/ijcp.13042. [DOI] [PubMed] [Google Scholar]
- 22.Oyeyemi A.S., Oladepo O., Adeyemi A.O., Titiloye M.A., Burnett S.M., Apera I. The potential role of patent and proprietary medicine vendors’ associations in improving the quality of services in Nigeria’s drug shops. BMC Health Serv. Res. 2020;20:567. doi: 10.1186/s12913-020-05379-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hofer U. The cost of antimicrobial resistance. Nat. Rev. Genet. 2018;17:3. doi: 10.1038/s41579-018-0125-x. [DOI] [PubMed] [Google Scholar]
- 24.Founou R.C., Founou L.L., Essack S. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS ONE. 2017;12:e0189621. doi: 10.1371/journal.pone.0189621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cassini A., Hogberg L.D., Plachouras D., Quattrocchi A., Hoxha A., Simonsen G.S., Colomb-Cotinat M., Kretzschmar M.E., Devleesschauwer B., Cecchini M., et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mukokinya M., Opanga S., Oluka M., Godman B. Dispensing of antimicrobials in Kenya: A cross-sectional pilot study and its implications. J. Res. Pharm. Pract. 2018;7:77–82. doi: 10.4103/jrpp.JRPP_17_88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kibuule D., Nambahu L., Sefah I.A., Kurdi A., Phuong T.N.T., Kwon H.-Y., Godman B. Activities in Namibia to Limit the Prevalence and Mortality from COVID-19 Including Community Pharmacy Activities and the Implications. SCH Acad. J. Pharm. 2021;10:82–92. [Google Scholar]
- 28.Kamati M., Godman B., Kibuule D. Prevalence of Self-Medication for Acute Respiratory Infections in Young Children in Namibia: Findings and Implications. J. Res. Pharm. Pract. 2019;8:220–224. doi: 10.4103/jrpp.JRPP_19_121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Markovic-Pekovic V., Grubisa N., Burger J., Bojanic L., Godman B. Initiatives to Reduce Nonprescription Sales and Dispensing of Antibiotics: Findings and Implications. J. Res. Pharm Pract. 2017;6:120–125. doi: 10.4103/jrpp.JRPP_17_12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoxha I., Malaj A., Kraja B., Bino S., Oluka M., Markovic-Pekovic V., Godman B. Are pharmacists’ good knowledge and awareness on antibiotics taken for granted? The situation in Albania and future implications across countries. J. Glob. Antimicrob. Resist. 2018;13:240–245. doi: 10.1016/j.jgar.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 31.Khan M.S., Bory S., Rego S., Suy S., Durrance-Bagale A., Sultana Z., Chhorn S., Phou S., Prien C., Heng S., et al. Is enhancing the professionalism of healthcare providers critical to tackling antimicrobial resistance in low- and middle-income countries? Hum. Resour. Health. 2020;18:10. doi: 10.1186/s12960-020-0452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haque M., Abubakar A., Ogunleye O., Sani I., Sefah I., Kurdi A., Islam S., Godman B. Changes in availability, utilization, and prices of medicines and protection equipment for COVID-19 in an Urban population of Northern Nigeria. J. Res. Pharm. Pract. 2021;10:17–22. doi: 10.4103/jrpp.JRPP_20_92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strathdee S.A., Davies S.C., Marcelin J.R. Confronting antimicrobial resistance beyond the COVID-19 pandemic and the 2020 US election. Lancet. 2020;396:1050–1053. doi: 10.1016/S0140-6736(20)32063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rawson T.M., Moore L.S.P., Zhu N., Ranganathan N., Skolimowska K., Gilchrist M., Satta G., Cooke G., Holmes A. Bacterial and Fungal Coinfection in Individuals With Coronavirus: A Rapid Review To Support COVID-19 Antimicrobial Prescribing. Clin. Infect. Dis. 2020;71:2459–2468. doi: 10.1093/cid/ciaa530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rodríguez-Álvarez M., López-Vidal Y., Soto-Hernández J.L., Miranda-Novales M.G., Flores-Moreno K., Ponce de León-Rosales S. COVID-19: Clouds Over the Antimicrobial Resistance Landscape. Arch. Med. Res. 2021;52:123–126. doi: 10.1016/j.arcmed.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Langford B.J., So M., Raybardhan S., Leung V., Soucy J.R., Westwood D., Daneman N., MacFadden D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. Dis. 2021;27:520–531. doi: 10.1016/j.cmi.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beović B., Doušak M., Ferreira-Coimbra J., Nadrah K., Rubulotta F., Belliato M., Berger-Estilita J., Ayoade F., Rello J., Erdem H. Antibiotic use in patients with COVID-19: A ‘snapshot’ Infectious Diseases International Research Initiative (ID-IRI) survey. J. Antimicrob. Chemother. 2020;75:3386–3390. doi: 10.1093/jac/dkaa326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nusrat N., Haque M., Chowdhury K., Adnan N., Lutfor A.B., Karim E., Hassan M., Rabbany A., Begum D., Hasan M.N., et al. Pilot Study on the Current Management of Children with COVID-19 In Hospitals in Bangladesh; Findings and Implications. Bangladesh J. Med. Sci. 2021;20:S188–S198. doi: 10.3329/bjms.v20i5.55615. [DOI] [Google Scholar]
- 39.Hsu J. How COVID-19 is accelerating the threat of antimicrobial resistance. BMJ. 2020;369:m1983. doi: 10.1136/bmj.m1983. [DOI] [PubMed] [Google Scholar]
- 40.Sriram A., Kalanxhi E., Kapoor G., Craig J., Balasubramanian R., Brar S., Criscuolo N., Hamilton A., Klein E., Tseng K., et al. State of the World’s Antibiotics 2021: A Global Analysis of Antimicrobial Resistance and Its Drivers. Center for Disease Dynamics, Economics & Policy; Washington, DC, USA: 2021. [(accessed on 10 September 2021)]. Available online: https://cddep.org/wp-content/uploads/2021/02/The-State-of-the-Worlds-Antibiotics-in-2021.pdf. [Google Scholar]
- 41.Nori P., Cowman K., Chen V., Bartash R., Szymczak W., Madaline T., Katiyar C.P., Jain R., Aldrich M., Weston G., et al. Bacterial and fungal coinfections in COVID-19 patients hospitalized during the New York City pandemic surge. Infect. Control. Hosp. Epidemiol. 2021;42:84–88. doi: 10.1017/ice.2020.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abbas K., Procter S.R., van Zandvoort K., Clark A., Funk S., Mengistu T., Hogan D., Dansereau E., Jit M., Flasche S., et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: A benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob. Health. 2020;8:e1264–e1272. doi: 10.1016/S2214-109X(20)30308-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ogunleye O.O., Basu D., Mueller D., Sneddon J., Seaton R.A., Yinka-Ogunleye A.F., Wamboga J., Miljković N., Mwita J.C., Rwegerera G.M., et al. Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: Successes, Challenges, and Implications for the Future. Front. Pharmacol. 2020;11:1205. doi: 10.3389/fphar.2020.01205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kluge H.H.P., Wickramasinghe K., Rippin H.L., Mendes R., Peters D.H., Kontsevaya A., Breda J. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395:1678–1680. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Palmer K., Monaco A., Kivipelto M., Onder G., Maggi S., Michel J.P., Prieto R., Prieto G., Donde S. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: Consequences for healthy ageing. Aging Clin. Exp. Res. 2020;32:1189–1194. doi: 10.1007/s40520-020-01601-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Basu S. Non-communicable disease management in vulnerable patients during Covid-19. Indian J. Med. Ethics. 2020;5:103–105. doi: 10.20529/IJME.2020.041. [DOI] [PubMed] [Google Scholar]
- 47.Hedima E.W., Adeyemi M.S., Ikunaiye N.Y. Community Pharmacists: On the frontline of health service against COVID-19 in LMICs. Res. Soc. Adm. Pharm. 2021;17:1964–1966. doi: 10.1016/j.sapharm.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cadogan C.A., Hughes C.M. On the frontline against COVID-19: Community pharmacists’ contribution during a public health crisis. Res. Soc. Adm. Pharm. 2021;17:2032–2035. doi: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al-Quteimat Om Msc B., Amer Am Rph M. SARS-CoV-2 outbreak: How can pharmacists help? Res. Soc. Adm. Pharm. 2021;17:480–482. doi: 10.1016/j.sapharm.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Al-Balas M., Al-Balas H.I., Jaber H.M., Obeidat K., Al-Balas H., Aborajooh E.A., Al-Taher R., Al-Balas B. Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: Current situation, challenges, and perspectives. BMC Med. Educ. 2020;20:341. doi: 10.1186/s12909-020-02257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tadesse S., Muluye W. The Impact of COVID-19 Pandemic on Education System in Developing Countries: A Review. Open J. Soc. Sci. 2020;8:159–170. doi: 10.4236/jss.2020.810011. [DOI] [Google Scholar]
- 52.Segafredo G., Kapur A., Robbiati C., Joseph N., de Sousa J.R., Putoto G., Manenti F., Atzori A., Fedeli U. Integrating TB and non-communicable diseases services: Pilot experience of screening for diabetes and hypertension in patients with Tuberculosis in Luanda, Angola. PLoS ONE. 2019;14:e0218052. doi: 10.1371/journal.pone.0218052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Okello S., Amir A., Bloomfield G.S., Kentoffio K., Lugobe H.M., Reynolds Z., Magodoro I.M., North C.M., Okello E., Peck R., et al. Prevention of cardiovascular disease among people living with HIV in sub-Saharan Africa. Prog. Cardiovasc. Dis. 2020;63:149–159. doi: 10.1016/j.pcad.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coetzee L., Bogler L., De Neve J.W., Barnighausen T., Geldsetzer P., Vollmer S. HIV, antiretroviral therapy and non-communicable diseases in sub-Saharan Africa: Empirical evidence from 44 countries over the period 2000 to 2016. J. Int. Aids Soc. 2019;22:e25364. doi: 10.1002/jia2.25364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rwegerera G.M., Shailemo D.H.P., Pina Rivera Y., Mokgosi K.O., Bale P., Oyewo T.A., Luis B.D., Habte D., Godman B. Metabolic Control and Determinants Among HIV-Infected Type 2 Diabetes Mellitus Patients Attending a Tertiary Clinic in Botswana. Diabetes Metab. Syndr. Obes. 2021;14:85–97. doi: 10.2147/DMSO.S285720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abena P.M., Decloedt E.H., Bottieau E., Suleman F., Adejumo P., Sam-Agudu N.A., TamFum J.-J.M., Seydi M., Eholie S.P., Mills E.J., et al. Chloroquine and Hydroxychloroquine for the Prevention or Treatment of COVID-19 in Africa: Caution for Inappropriate Off-label Use in Healthcare Settings. Am. J. Trop. Med. Hyg. 2020;102:1184–1188. doi: 10.4269/ajtmh.20-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bączek M., Zagańczyk-Bączek M., Szpringer M., Jaroszyński A., Wożakowska-Kapłon B. Students’ perception of online learning during the COVID-19 pandemic: A survey study of Polish medical students. Medicine. 2021;100:e24821. doi: 10.1097/MD.0000000000024821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kawaguchi-Suzuki M., Nagai N., Akonoghrere R.O., Desborough J.A. COVID-19 Pandemic Challenges and Lessons Learned by Pharmacy Educators Around the Globe. Am. J. Pharm. Educ. 2020;84:ajpe8197. doi: 10.5688/ajpe8197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alsoufi A., Alsuyihili A., Msherghi A., Elhadi A., Atiyah H., Ashini A., Ashwieb A., Ghula M., Hasan H.B., Abudabuos S., et al. Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS ONE. 2020;15:e0242905. doi: 10.1371/journal.pone.0242905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bouali H., Okereke M., Adebisi Y.A., Lucero-Prisno D.E., III Impact of COVID-19 on Pharmacy Education. Sci. Med. J. 2020;2:92–95. doi: 10.28991/SciMedJ-2020-02-SI-8. [DOI] [Google Scholar]
- 61.Okereke M., Williams A.E., Emmanuella N.C., Ashinedu N.U., Mairaj M.W. COVID-19: Challenges affecting the uptake of e-learning in pharmacy education in Africa. Pan. Afr. Med. J. 2020;35:70. doi: 10.11604/pamj.supp.2020.35.2.23910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Owusu-Fordjour C., Koomson C.K., Hanson D. The impact of Covid-19 on learning-the perspective of the Ghanaian student. Eur. J. Educ. Stud. 2020;7:88–101. [Google Scholar]
- 63.Barteit S., Jahn A., Banda S.S., Bärnighausen T., Bowa A., Chileshe G., Guzek D., Jorge M.M., Lüders S., Malunga G., et al. E-Learning for Medical Education in Sub-Saharan Africa and Low-Resource Settings: Viewpoint. J. Med. Int. Res. 2019;21:e12449. doi: 10.2196/12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barteit S., Guzek D., Jahn A., Bärnighausen T., Jorge M.M., Neuhann F. Evaluation of e-learning for medical education in low- and middle-income countries: A systematic review. Comput. Educ. 2020;145:103726. doi: 10.1016/j.compedu.2019.103726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fawaz M., Samaha A. E-learning: Depression, anxiety, and stress symptomatology among Lebanese university students during COVID-19 quarantine. Nurs. Forum. 2021;56:52–57. doi: 10.1111/nuf.12521. [DOI] [PubMed] [Google Scholar]
- 66.Ihm L., Zhang H., van Vijfeijken A., Waugh M.G. Impacts of the Covid-19 pandemic on the health of university students. Int. J. Health Plan. Manag. 2021;36:618–627. doi: 10.1002/hpm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.David W.H., Michelle G., Gregory D.B., Werner N., van Bettine Jansen V. COVID-19 and the academe in South Africa: Not business as usual. South. Afr. J. Sci. 2020;116:8298. [Google Scholar]
- 68.Wangenge-Ouma G., Kupe T. Uncertain Times: Re-Imagining Universities for New, Sustainable Futures. 2020. [(accessed on 9 September 2021)]. Available online: https://www.up.ac.za/media/shared/1/2020/September%202020/uncertain-times-paper_final_08092020-1.zp194357.pdf.
- 69.Wasfy N.F., Abouzeid E., Nasser A.A., Ahmed S.A., Youssry I., Hegazy N.N., Shehata M.H.K., Kamal D., Atwa H. A guide for evaluation of online learning in medical education: A qualitative reflective analysis. BMC Med. Educ. 2021;21:339. doi: 10.1186/s12909-021-02752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shehata M.H., Abouzeid E., Wasfy N.F., Abdelaziz A., Wells R.L., Ahmed S.A. Medical Education Adaptations Post COVID-19: An Egyptian Reflection. J. Med. Educ. Curric. Dev. 2020;7:2382120520951819. doi: 10.1177/2382120520951819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Almetwazi M., Alzoman N., Al-Massarani S., Alshamsan A. COVID-19 impact on pharmacy education in Saudi Arabia: Challenges and opportunities. SPJ. 2020;28:1431–1434. doi: 10.1016/j.jsps.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Almomani E.Y., Qablan A.M., Atrooz F.Y., Almomany A.M., Hajjo R.M., Almomani H.Y. The Influence of Coronavirus Diseases 2019 (COVID-19) Pandemic and the Quarantine Practices on University Students’ Beliefs About the Online Learning Experience in Jordan. Front. Public Health. 2020;8:595874. doi: 10.3389/fpubh.2020.595874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Amunga J. Leveraging technology to enhance STEM education amidst the Covid-19 pandemic: An overview of pertinent concerns. Tech. Soc. Sci. J. 2021;18:40–55. doi: 10.47577/tssj.v18i1.3044. [DOI] [Google Scholar]
- 74.Hassounah M., Raheel H., Alhefzi M. Digital Response During the COVID-19 Pandemic in Saudi Arabia. J. Med. Int. Res. 2020;22:e19338. doi: 10.2196/19338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sharma D., Bhaskar S. Addressing the Covid-19 Burden on Medical Education and Training: The Role of Telemedicine and Tele-Education During and Beyond the Pandemic. Front. Public Health. 2020;8:589669. doi: 10.3389/fpubh.2020.589669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aljaber A. E-learning policy in Saudi Arabia: Challenges and successes. Res. Comp. Int. Educ. 2018;13:176–194. doi: 10.1177/1745499918764147. [DOI] [Google Scholar]
- 77.Soliman M., Aldhaheri S., Neel K. Experience from a medical college in Saudi Arabia on undergraduate curriculum management and delivery during COVID-19 pandemic. J. Nat. Sci. Med. 2021;4:85–89. doi: 10.4103/jnsm.jnsm_11_21. [DOI] [Google Scholar]
- 78.Alrasheedy A.A., Abdulsalim S., Farooqui M., Alsahali S., Godman B. Knowledge, attitude and practice about coronavirus disease (COVID-19) pandemic and its psychological impact on students and their studies: A cross-sectional study among pharmacy students in Saudi Arabia. Risk Manag. Healthc. Policy. 2021;14:729. doi: 10.2147/RMHP.S292354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Altwaijry N., Ibrahim A., Binsuwaidan R., Alnajjar L.I., Alsfouk B.A., Almutairi R. Distance Education During COVID-19 Pandemic: A College of Pharmacy Experience. Risk Manag. Healthc. Policy. 2021;14:2099. doi: 10.2147/RMHP.S308998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Saudi Data and Artificial Intelligence Authority (SDAIA) Tawakkana Application. [(accessed on 6 September 2021)];2021 Available online: https://ta.sdaia.gov.sa/en/index.
- 81.Almaghaslah D., Alsayari A. The effects of the 2019 Novel Coronavirus Disease (COVID-19) outbreak on academic staff members: A case study of a pharmacy school in Saudi Arabia. Risk Manag. Healthc. Policy. 2020;13:795. doi: 10.2147/RMHP.S260918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shawaqfeh M.S., Al Bekairy A.M., Al-Azayzih A., Alkatheri A.A., Qandil A.M., Obaidat A.A., Al Harbi S., Muflih S.M. Pharmacy Students Perceptions of Their Distance Online Learning Experience During the COVID-19 Pandemic: A Cross-Sectional Survey Study. J. Med. Educ. Curr. Dev. 2020;7:2382120520963039. doi: 10.1177/2382120520963039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Al Zahrani E.M., Al Naam Y.A., AlRabeeah S.M., Aldossary D.N., Al-Jamea L.H., Woodman A., Shawaheen M., Altiti O., Quiambao J.V., Arulanantham S.J., et al. E- Learning experience of the medical profession’s college students during COVID-19 pandemic in Saudi Arabia. BMC Med. Educ. 2021;21:443. doi: 10.1186/s12909-021-02860-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Guadalajara H., Palazón Á., Lopez-Fernandez O., Esteban-Flores P., Garcia J.M., Gutiérrez-Misis A., Baca-García E., Garcia-Olmo D. Towards an Open Medical School without Checkerboards during the COVID-19 Pandemic: How to Flexibly Self-Manage General Surgery Practices in Hospitals? Healthcare. 2021;9:743. doi: 10.3390/healthcare9060743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Guiter G.E., Sapia S., Wright A.I., Hutchins G.G.A., Arayssi T. Development of a Remote Online Collaborative Medical School Pathology Curriculum with Clinical Correlations, across Several International Sites, through the Covid-19 Pandemic. Med. Sci. Educ. 2021;31:549–556. doi: 10.1007/s40670-021-01212-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Elsalem L., Al-Azzam N., Jum’ah A.A., Obeidat N. Remote E-exams during Covid-19 pandemic: A cross-sectional study of students’ preferences and academic dishonesty in faculties of medical sciences. Ann. Med. Surg. 2021;62:326–333. doi: 10.1016/j.amsu.2021.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Roszak M., Sawik B., Stańdo J., Baum E. E-Learning as a Factor Optimizing the Amount of Work Time Devoted to Preparing an Exam for Medical Program Students during the COVID-19 Epidemic Situation. Healthcare. 2021;9:1147. doi: 10.3390/healthcare9091147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Almaiah M.A., Al-Khasawneh A., Althunibat A. Exploring the critical challenges and factors influencing the E-learning system usage during COVID-19 pandemic. Educ. Inf. Technol. 2020;25:5261–5280. doi: 10.1007/s10639-020-10219-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ashiq K., Ashiq S., Sadia H. Pharmacy Education and Role of the Teachers During the COVID-19 Pandemic. Bangladesh J. Med. Sci. 2021;20:S183–S184. doi: 10.3329/bjms.v20i5.55418. [DOI] [Google Scholar]
- 90.Islam S. Unlearning, Relearning, and Paradigm Shift to Online Tertiary Education during the COVID-19 Pandemic in Bangladesh. Bangladesh J. Med. Sci. 2021;20:S65–S71. doi: 10.3329/bjms.v20i5.55399. [DOI] [Google Scholar]
- 91.Gaur U., Majumder M.A.A., Sa B., Sarkar S., Williams A., Singh K. Challenges and Opportunities of Preclinical Medical Education: Covid-19 Crisis and Beyond. SN Compr. Clin. Med. 2020;2:1992–1997. doi: 10.1007/s42399-020-00528-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Afriyie D.K., Asare G.A., Amponsah S.K., Godman B. COVID-19 pandemic in resource-poor countries: Challenges, experiences and opportunities in Ghana. J. Infect. Dev. Ctry. 2020;14:838–843. doi: 10.3855/jidc.12909. [DOI] [PubMed] [Google Scholar]
- 93.Rajab M.H., Gazal A.M., Alkattan K. Challenges to Online Medical Education During the COVID-19 Pandemic. Cureus. 2020;12:e8966. doi: 10.7759/cureus.8966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Thakur A., Soklaridis S., Crawford A., Mulsant B., Sockalingam S. Using Rapid Design Thinking to Overcome COVID-19 Challenges in Medical Education. Acad. Med. J. Assoc. Am. Med. Coll. 2021;96:56–61. doi: 10.1097/ACM.0000000000003718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Torda A.J., Velan G., Perkovic V. The impact of the COVID-19 pandemic on medical education. Med. J. Aust. 2020;213 doi: 10.5694/mja2.50705. [DOI] [PubMed] [Google Scholar]
- 96.Reyna J. Twelve Tips for COVID-19 friendly learning design in medical education. MedEdPublish. 2020;9:103. doi: 10.15694/mep.2020.000103.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Papapanou M., Routsi E., Tsamakis K., Fotis L., Marinos G., Lidoriki I., Karamanou M., Papaioannou T.G., Tsiptsios D., Smyrnis N., et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad. Med. J. 2021:1–7. doi: 10.1136/postgradmedj-2021-140032. [DOI] [PubMed] [Google Scholar]
- 98.Ferrel M.N., Ryan J.J. The Impact of COVID-19 on Medical Education. Cureus. 2020;12:e7492. doi: 10.7759/cureus.7492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hong J.C., Lee Y.F., Ye J.H. Procrastination predicts online self-regulated learning and online learning ineffectiveness during the coronavirus lockdown. Personal. Individ. Differ. 2021;174:110673. doi: 10.1016/j.paid.2021.110673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lucey C.R., Johnston S.C. The Transformational Effects of COVID-19 on Medical Education. JAMA. 2020;324:1033–1034. doi: 10.1001/jama.2020.14136. [DOI] [PubMed] [Google Scholar]
- 101.Jiang X., Ning Q. The Impact and Evaluation Of COVID-19 Pandemic on the Teaching Model of Medical Molecular Biology Course for Undergraduates Major in Pharmacy. Biochem. Mol. Biol. Educ. 2021;49:346–352. doi: 10.1002/bmb.21471. [DOI] [PubMed] [Google Scholar]
- 102.McKimm J. The impact of the COVID-19 pandemic on medical and health professions’ education: Thoughts and reflections. Adv. Hum. Biol. 2021;11:1–2. doi: 10.4103/aihb.aihb_115_20. [DOI] [Google Scholar]
- 103.Pelikan E.R., Lüftenegger M., Holzer J., Korlat S., Spiel C., Schober B. Learning During Covid-19: The Role of Self-Regulated Learning, Motivation, and Procrastination for Perceived Competence. Z. Erziehwiss. 2021;24:393–418. doi: 10.1007/s11618-021-01002-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Louiselle K., Elson E.C., Oschman A., Duehlmeyer S. Impact of COVID-19 pandemic on pharmacy learners and preceptors. Am. J. Health-Syst. Pharm. 2020;77:1097–1099. doi: 10.1093/ajhp/zxaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sasser C.W., Wolcott M.D., Morbitzer K.A., Eckel S.F. Lessons learned from pharmacy learner and educator experiences during early stages of COVID-19 pandemic. Am. J. Health-Syst. Pharm. AJHP. 2021;78:872–878. doi: 10.1093/ajhp/zxab076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gale N.K., Heath G., Cameron E., Rashid S., Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kaushik V., Walsh C.A. Pragmatism as a Research Paradigm and Its Implications for Social Work Research. Soc. Sci. 2019;8:255. doi: 10.3390/socsci8090255. [DOI] [Google Scholar]
- 108.World Bank GDP per Capita (US$) 2021. [(accessed on 8 September 2021)]. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD.
- 109.Worldometer African Countries by Population. 2021. [(accessed on 8 September 2021)]. Available online: https://www.worldometers.info/population/countries-in-africa-by-population/
- 110.Mwita J.C., Ogunleye O.O., Olalekan A., Kalungia A.C., Kurdi A., Saleem Z., Sneddon J., Godman B. Key Issues Surrounding Appropriate Antibiotic Use for Prevention of Surgical Site Infections in Low- and Middle-Income Countries: A Narrative Review and the Implications. Int. J. Gen. Med. 2021;14:515–530. doi: 10.2147/IJGM.S253216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Godman B., Grobler C., Van-De-Lisle M., Wale J., Barbosa W.B., Massele A., Opondo P., Petrova G., Tachkov K., Sefah I., et al. Pharmacotherapeutic interventions for bipolar disorder type II: Addressing multiple symptoms and approaches with a particular emphasis on strategies in lower and middle-income countries. Expert Opin. Pharmacother. 2019;20:2237–2255. doi: 10.1080/14656566.2019.1684473. [DOI] [PubMed] [Google Scholar]
- 112.Godman B., Basu D., Pillay Y., Almeida P., Mwita J.C., Rwegerera G.M., Anand Paramadhas B.D., Tiroyakgosi C., Patrick O., Niba L.L., et al. Ongoing and planned activities to improve the management of patients with Type 1 diabetes across Africa; implications for the future. Hosp. Pract. 2020;48:51–67. doi: 10.1080/21548331.2020.1745509. [DOI] [PubMed] [Google Scholar]
- 113.Palinkas L.A., Horwitz S.M., Green C.A., Wisdom J.P., Duan N., Hoagwood K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health. 2015;42:533–544. doi: 10.1007/s10488-013-0528-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 115.Vaismoradi M., Turunen H., Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013;15:398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 116.Mwale N., Chita J. Higher education and programme delivery in the context of COVID-19 and institutional closures: Student responses to the adoption of e-Learning at a public university in Zambia. [(accessed on 8 September 2021)];J. Learn. Dev. 2020 8:501–515. Available online: http://alternation.ukzn.ac.za/Files/books/series-02/01-Mwale.pdf. [Google Scholar]
- 117.Lates J., Kibuule D. EDITORIAL: COVID-19: Rebooting pharmacy education in resource-limited settings. Pharm. Educ. 2021:67–70. doi: 10.46542/pe.2020.202.6770. [DOI] [Google Scholar]
- 118.Nimavat N., Singh S., Fichadiya N., Sharma P., Patel N., Kumar M., Chauhan G., Pandit N. Online Medical Education in India—Different Challenges and Probable Solutions in the Age of COVID-19. Adv. Med. Educ. Pract. 2021;12:237–243. doi: 10.2147/AMEP.S295728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Campbell S.M., Meyer J.C., Godman B. Why Compliance to National Prescribing Guidelines is Important Especially across Sub-Saharan Africa and Suggestions for the Future. J. Biomed. Pharm. Sci. 2021;4:309. [Google Scholar]
- 120.Burgess P.I., Harding S.P., Kayange P.C., van Oosterhout J., García-Fiñana M., Msukwa G., Allain T.J. High mortality in subjects with both diabetes and HIV in sub-Saharan Africa. AIDS. 2018;32:2083–2084. doi: 10.1097/QAD.0000000000001929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Asante-Poku A., Asare P., Baddoo N.A., Forson A., Klevor P., Otchere I.D., Aboagye S.A., Osei-Wusu S., Danso E.K., Kwadwo Koram K., et al. TB-diabetes co-morbidity in Ghana: The importance of Mycobacterium africanum infection. PLoS ONE. 2019;14:e0211822. doi: 10.1371/journal.pone.0211822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bigna J.J., Ndoadoumgue A.L., Nansseu J.R., Tochie J.N., Nyaga U.F., Nkeck J.R., Foka A.J., Kaze A.D., Noubiap J.J. Global burden of hypertension among people living with HIV in the era of increased life expectancy: A systematic review and meta-analysis. J. Hypertens. 2020;38:1659–1668. doi: 10.1097/HJH.0000000000002446. [DOI] [PubMed] [Google Scholar]
- 123.Devkota K.R. Inequalities Reinforced Through Online and Distance Education in the Age of COVID-19: The Case of Higher Education in Nepal. Int. Rev. Educ. 2021;67:145–165. doi: 10.1007/s11159-021-09886-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mulla Z.D., Osland-Paton V., Rodriguez M.A., Vazquez E., Kupesic Plavsic S. Novel coronavirus, novel faculty development programs: Rapid transition to eLearning during the pandemic. J. Perinat. Med. 2020;48:446–449. doi: 10.1515/jpm-2020-0197. [DOI] [PubMed] [Google Scholar]
- 125.Cleland J., McKimm J., Fuller R., Taylor D., Janczukowicz J., Gibbs T. Adapting to the impact of COVID-19: Sharing stories, sharing practice. Med. Teach. 2020;42:772–775. doi: 10.1080/0142159X.2020.1757635. [DOI] [PubMed] [Google Scholar]
- 126.Sigdel S., Ozaki A., Dhakal R., Pradhan B., Tanimoto T. Medical Education in Nepal: Impact and Challenges of the COVID-19 Pandemic. Acad. Med. J. Assoc. Am. Med. Coll. 2021;96:340–342. doi: 10.1097/ACM.0000000000003888. [DOI] [PubMed] [Google Scholar]
- 127.Yuda Handaya A., Fauzi A.R., Andrew J., Hanif A.S., Tjendra K.R., Aditya A.F.K. Effectiveness of tutorial videos combined with online classes in surgical knotting course during COVID-19 pandemic: A cohort study. Ann. Med. Surg. 2021;69:102751. doi: 10.1016/j.amsu.2021.102751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.McGann K.C., Melnyk R., Saba P., Joseph J., Glocker R.J., Ghazi A. Implementation of an E-Learning Academic Elective for Hands-On Basic Surgical Skills to Supplement Medical School Surgical Education. J. Surg. Educ. 2021;78:1164–1174. doi: 10.1016/j.jsurg.2020.11.014. [DOI] [PubMed] [Google Scholar]
- 129.Wu S.-J., Fan Y.-F., Sun S., Chien C.-Y., Wu Y.-J. Perceptions of medical students towards and effectiveness of online surgical curriculum: A systematic review. BMC. 2021;21:571. doi: 10.1186/s12909-021-03014-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ferner R.E., Aronson J.K. Chloroquine and hydroxychloroquine in COVID-19. BMJ. 2020;369:m1432. doi: 10.1136/bmj.m1432. [DOI] [PubMed] [Google Scholar]
- 131.Godman B., Fadare J., Kwon H.Y., Dias C.Z., Kurdi A., Dias Godói I.P., Kibuule D., Hoxha I., Opanga S., Saleem Z., et al. Evidence-based public policy making for medicines across countries: Findings and implications for the future. J. Comp. Eff. Res. 2021;10:1019–1052. doi: 10.2217/cer-2020-0273. [DOI] [PubMed] [Google Scholar]
- 132.Charan J., Kaur R.J., Bhardwaj P., Haque M., Sharma P., Misra S., Godman B. Rapid review of suspected adverse drug events due to remdesivir in the WHO database; findings and implications. Expert Rev. Clin. Pharmacol. 2021;14:95–103. doi: 10.1080/17512433.2021.1856655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Horby P., Mafham M., Linsell L., Bell J.L., Staplin N., Emberson J.R., Wiselka M., Ustianowski A., Elmahi E., Prudon B., et al. Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2020;383:2030–2040. doi: 10.1056/NEJMoa2022926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Godman B. Combating COVID-19: Lessons learnt particularly among developing countries and the implications. Bangladesh J. Med. Sci. 2020;19:S103–S108. doi: 10.3329/bjms.v19i0.48413. [DOI] [Google Scholar]
- 135.Opanga S.A., Rizvi N., Wamaitha A., Sefah I.A., Godman B. Availability of Medicines in Community Pharmacy to Manage Patients with COVID-19 in Kenya; Pilot Study and Implications. SCH Acad. J. Pharm. 2021;10:36–42. doi: 10.36347/sajp.2021.v10i03.001. [DOI] [Google Scholar]
- 136.Godman B., Haque M., Leong T., Allocati E., Kumar S., Islam S., Charan J., Akter F., Vassalo C., Bakar M.A., et al. The Current Situation Regarding Long-Acting Insulin Analogues Including Biosimilars Among African, Asian, European, and South American Countries; Findings and Implications for the Future. Front. Publ. Health. 2021;9:671961. doi: 10.3389/fpubh.2021.671961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Godman B., McCabe H., Leong T.D., Mueller D., Martin A.P., Hoxha I., Mwita J.C., Rwegerera G.M., Massele A., de Oliveira Costa C., et al. Fixed dose drug combinations—Are they pharmacoeconomically sound? Findings and implications especially for lower- and middle-income countries. Expert Rev. Pharm. Outcomes Res. 2020;20:1–26. doi: 10.1080/14737167.2020.1734456. [DOI] [PubMed] [Google Scholar]
- 138.Djoutsop O., Vanessa Y., Kanmounye U.S. COVID-19 and Clinical Rotations in the Democratic Republic of Congo. Int J. Med. Stud. 2020;8:4–6. doi: 10.5195/ijms.2020.539. [DOI] [Google Scholar]
- 139.Skosana P.P., Schellack N., Godman B., Kurdi A., Bennie M., Kruger D., Meyer J.C. A Point Prevalence Survey of Antimicrobial Utilisation Patterns and Quality Indices Amongst Hospitals in South Africa; Findings and Implications. Expert Rev. Anti Infect Ther. 2021;19:1353–1366. doi: 10.1080/14787210.2021.1898946. [DOI] [PubMed] [Google Scholar]
- 140.Kruger D., Dlamini N.N., Meyer J.C., Godman B., Kurdi A., Lennon M., Bennie M., Schellack N. Development of a web-based application to improve data collection of antimicrobial utilization in the public health care system in South Africa. Hosp. Pract. 2021;49:184–193. doi: 10.1080/21548331.2021.1889213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Karim N., Jing L., Lee J.A., Kharel R., Lubetkin D., Clancy C.M., Uwamahoro D., Nahayo E., Biramahire J., Aluisio A.R., et al. Lessons Learned from Rwanda: Innovative Strategies for Prevention and Containment of COVID-19. Ann. Glob. Health. 2021;87:23. doi: 10.5334/aogh.3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Webster P. Virtual health care in the era of COVID-19. Lancet. 2020;395:1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Weber A.M., Dua A., Chang K., Jupalli H., Rizwan F., Chouthai A., Chen C. An outpatient telehealth elective for displaced clinical learners during the COVID-19 pandemic. BMC Med. Educ. 2021;21:174. doi: 10.1186/s12909-021-02604-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mudenda S., Mukosha M., Mwila C., Saleem Z., Kalungia A.C., Munkombwe D., Daka V., Witika B.A., Kampamba M., Chileshe M., et al. Impact of the coronavirus disease on the mental health and physical activity of pharmacy students at the University of Zambia: A cross-sectional study. Int. J. Basic Clin. Pharmacol. 2021;10:324. doi: 10.18203/2319-2003.ijbcp20211010. [DOI] [Google Scholar]
- 145.Sahu P. Closure of Universities Due to Coronavirus Disease 2019 (COVID-19): Impact on Education and Mental Health of Students and Academic Staff. Cureus. 2020;12:e7541. doi: 10.7759/cureus.7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Miguel C., Castro L., Marques Dos Santos J.P., Serrão C., Duarte I. Impact of COVID-19 on Medicine Lecturers’ Mental Health and Emergency Remote Teaching Challenges. Int. J. Environ. Res. Public Health. 2021;18:6792. doi: 10.3390/ijerph18136792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zis P., Artemiadis A., Bargiotas P., Nteveros A., Hadjigeorgiou G.M. Medical Studies during the COVID-19 Pandemic: The Impact of Digital Learning on Medical Students’ Burnout and Mental Health. Int. J. Environ. Res. Public Health. 2021;18:349. doi: 10.3390/ijerph18010349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wang J., Bu L., Li Y., Song J., Li N. The mediating effect of academic engagement between psychological capital and academic burnout among nursing students during the COVID-19 pandemic: A cross-sectional study. Nurse Educ. Today. 2021;102:104938. doi: 10.1016/j.nedt.2021.104938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Haque M., Kumar S., Charan J., Bhatt R., Islam S., Dutta S., Abhayanand J.P., Sharma Y., Sefah I., Kurdi A., et al. Utilisation, availability and price changes of medicines and protection equipment for COVID-19 in India: Findings and implications. Front. Pharmacol. 2021;11:582154. doi: 10.3389/fphar.2020.582154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Godman B., Haque M., Islam S., Iqbal S., Urmi U.L., Kamal Z.M., Shuvo S.A., Rahman A., Kamal M., Haque M., et al. Rapid Assessment of Price Instability and Paucity of Medicines and Protection for COVID-19 Across Asia: Findings and Public Health Implications for the Future. Front. Public Health. 2020;8:585832. doi: 10.3389/fpubh.2020.585832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gad M., Salem A., Oortwijn W., Hill R., Godman B. Mapping of Current Obstacles for Rationalizing Use of Medicines (CORUM) in Europe: Current Situation and Potential Solutions. Front. Pharmacol. 2020;11:144. doi: 10.3389/fphar.2020.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Miljković N., van Overbeeke E., Godman B., Kovačević M., Anastasi A., Bochenek T., Huys I., Miljković B. Practical Implications From European Hospital Pharmacists on Prospective Risk Assessment for Medicine Shortages. Front. Med. 2020;7:407. doi: 10.3389/fmed.2020.00407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Miljković N., Godman B., van Overbeeke E., Kovačević M., Tsiakitzis K., Apatsidou A., Nikopoulou A., Yubero C.G., Horcajada L.P., Stemer G., et al. Risks in Antibiotic Substitution Following Medicine Shortage: A Health-Care Failure Mode and Effect Analysis of Six European Hospitals. Front. Med. 2020;7:157. doi: 10.3389/fmed.2020.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Godman B., Wettermark B., van Woerkom M., Fraeyman J., Alvarez-Madrazo S., Berg C., Bishop I., Bucsics A., Campbell S., Finlayson A.E., et al. Multiple policies to enhance prescribing efficiency for established medicines in Europe with a particular focus on demand-side measures: Findings and future implications. Front. Pharmacol. 2014;5:106. doi: 10.3389/fphar.2014.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All available data are included in the paper.