Abstract
Background: The purpose of this study was to assess the prevalence of psychological distress in medical students during the COVID-19 health crisis and to identify factors associated with psychological distress. Methods: A cross-sectional observational study was presented to 1814 medical students (from first to sixth year) in a French university hospital center. Sociodemographic, occupational and medical information (psychological distress measured on the French GHQ12 scale) were collected via an online anonymous self-administered questionnaire. Variables associated with psychological distress were investigated using univariate analysis and multivariate analysis (modified Poisson regression). Results: In total, 832 medical students responded (46%) and 699 completed the questionnaire in full (39%); 625 (75%) showed signs of psychological distress and 109 (15%) reported suicidal ideation. Female gender, psychological trauma during the COVID-19 health crisis, change in alcohol consumption, and difficulties with online learning emerged as risk factors for psychological distress, whereas a paid activity, a feeling of mutual aid and cooperation within the studies framework, and recognition of work appeared to be protective factors. Conclusions: Mental health care or suicide prevention should be provided to students at risk in the aftermath of the pandemic. Knowing the educational and medical factors associated with psychological distress enables areas for prevention to be identified.
Keywords: psychological distress, medical students, COVID-19 health crisis, traumatic event, distance learning
1. Introduction
Since the beginning of 2020, SARS-CoV-2 has spread to several continents and is responsible for a large number of deaths [1,2]. To reduce the risk of person-to-person viral transmission during the COVID-19 pandemic, the French government introduced various measures, including social distancing, self-quarantine, and temporarily cancelling work and school, to control the disease. Students are bearing the brunt of the economic, social and psychological consequences of the COVID-19 pandemic. There is growing concern worldwide regarding the psychological health of students and particularly of medical students. Medical schools around the world have long been considered stressful environments for students entering higher education [3]. Students enter medical school immediately after high school, often at 18 years of age, and they go through 6 years of medical education before graduation. In France, medical students take a competitive examination at the end of their first year and a national competitive examination at the end of their sixth year. During the first 3 years, students have preclinical training, then from 4th to 6th year they have clinical training. Previous research identified long hours of study, academic workload, competition with peers, conflicts in work-life balance, the emotional burden of exposure to human suffering, and considerable financial pressure as the principal stressors affecting psychological health [4,5,6,7,8]. Psychological distress broadly refers to anxiety, stress, depression, and mental health-related problems. Previous studies showed that the prevalence of psychological distress in medical students during medical training in various countries and institutions ranges from 21% to 56% [9]. Even before the COVID-19 pandemic, medical students showed higher rates of mental health issues than the general population, including generalized anxiety disorder (GAD), depression, and burnout [10,11]. Yusoff et al. reported that healthy students develop depression and stress after commencing their medical education [12]. It was also reported that physicians tend to have higher suicide rates compared to the general population [13].
Previous pandemics, such as the 2003 SARS outbreak in China, increased stress levels in healthcare students, highlighting the need for additional support for this population during public health crises [14]. The spread of the COVID-19 virus has had far-reaching consequences, and the closure of universities has led to the development of online learning, leading to student isolation. Students experiencing higher psychological distress are at a higher risk of academic failure and dropout [15,16]. In addition, medical students during internships in COVID-19 care units were involved in the management of patients infected with COVID-19 which may have exposed them to a high emotional burden.
We assume that the organizational changes in theoretical (distance learning courses) and practical (internships in COVID-19 care services) teaching caused by the health crisis are associated with psychological distress in medical students.
The objectives of the present study were to evaluate the prevalence of psychological distress in medical students during the COVID-19 health crisis and to identify personal, medical and occupational factors associated with psychological distress.
In this context, an evaluation of the prevalence of psychological distress and the associated factors in medical students in France was conducted.
2. Materials and Methods
The study design consisted of a cross-sectional questionnaire survey.
2.1. Target Population
Data were collected from 10 March to 25 March 2021. The target population was 1st- to 6th-year students registered at the Faculty of Medicine of Saint Etienne located in the Loire department which recorded the highest incidence rate of COVID-19 in the autumn of 2020 (700 cases per 100,000 inhabitants) [17]. This epidemic situation has led to an increase in the demand for care in the hospitals of the Loire department. Medical students in hospital internships were involved in the health crisis by participating in the care of patients infected with COVID-19. Students from 1st to 3rd year may have been victims of social isolation due to the distance learning course and the implementation of a lockdown period from 30 October 2020 to 15 December 2020.
2.2. Study Sample
We targeted medical students at different levels of training, at preclinical (first and second year) or clinical level (third to sixth year). All students aged at least 18 years old and registered in medicine at Saint Etienne medical school from 1st to 6th year were invited to respond voluntarily to a self-administered online survey. They received an invitation to participate in this study via their e-mail address. In total, 1814 eligible students were contacted by university email. The participants answered the online questionnaire via the LimeSurvey application (Hamburg, Germany). They received clear and comprehensible information on study objectives and procedure, and were free to decline participation. Review board approval (IRBN272021/CHUSTE) was obtained before starting the study. The average age of the eligible subjects in the study was 21 years old [Et = 1.17]; 66% were women, 65% were 1st-year students, 19% were 2nd- and 3rd-year students, and 26% were 4th-, 5th- and 6th-year medical students.
2.3. Measurements
We developed a self-reported questionnaire to collect data on demographic, occupational and medical characteristics. Self-administration time was measured to approximately 10 min.
The main endpoint (psychological distress) was assessed by the validated French version of the 12-item General Health Questionnaire (GHQ) [18], a self-report instrument measuring psychological morbidity, intended to detect psychiatric disorders in community and non-psychiatric settings [19]. The Cronbach coefficient of the GHQ-12 was evaluated by Goldberg at between 0.82 and 0.86 in general health care [20]. The Cronbach coefficient of the GHQ-12 was evaluated at 0.85 in a population of Malian students [21]. Answers were given on a 4-point scale; for instance, the item “In the last weeks, did you feel under strain?” allows for the following answers: “No”, “Not more than usual”, “More than usual”, and “Much more than usual”. When scored with the binary method (0–0–1–1), the GHQ-12 can be used as a screening tool to detect minor non-psychotic psychiatric disorders, yielding final scores that range from 0 to 12. Operationally, patients scoring ≥4 are considered “GHQ-positive” [22].
The anonymous self-administered questionnaire covered 3 areas.
Personal: gender, age, number of people at home, and financial difficulties.
Educational: seniority in medical studies, weekly study time, daily screen time, face-to-face courses in the last three months, hospital internship in the last three months, internship in COVID-19 care services, and difficulties in following distance learning courses. Perceived stress related to personal and educational life was assessed on a visual analogue scale (VAS). A cut-off at 7 points defined clinical signs suggestive of stress.
Medical: perceived health status, experience of trauma during the COVID-19 crisis, sense of mutual aid and cooperation in studies, history of anxiety disorder, history of depression, history of suicide attempts, psychotropic treatment, psychiatric care, presence of suicidal ideation, date of last consultation with general practitioner or occupational/prevention physician, sleep duration, alcohol consumption and smoking, and cannabis use.
2.4. Analysis
Age and stress levels, both quantitative variables, were transformed into categorical qualitative variables before statistical analysis.
A descriptive analysis was made of the sample’s sociodemographic, educational and medical characteristics. We chose not to investigate the association between psychological distress and suicidal ideation since suicidal ideation appears to be a complication of psychological distress.
A univariate analysis was performed to assess the association between psychological distress and sociodemographic, educational and medical factors. Chi2 and Fisher tests were applied as appropriate. The significance threshold was set at 5%. Variables significantly associated with psychological distress were introduced in a modified Poisson regression using robust variance estimations [23]. Variables with a p-value ≤ 0.2 were included in the multivariate model, and variables with a p-value < 0.05 were kept in the model. Analyses used R software (The R Foundation for Statistical Computing, Vienna, Austria) used in France.
3. Results
3.1. Sociodemographic, Educational and Medical Characteristics
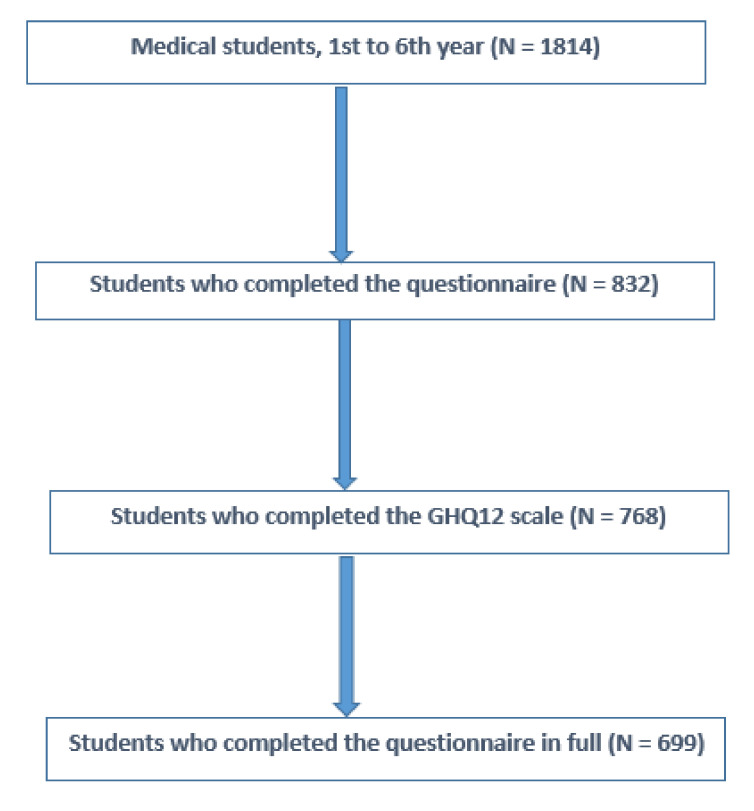
As shown in Table 1 and Table 2, out of the 1814 eligible students, 832 (73% female, 27% male) responded, giving a response rate of 46% (Figure 1). More than a third of respondents were 19 or 20 years of age. Three quarters were single. Nearly 10% reported financial difficulties. Half expressed high levels of stress related to their personal life. Nearly one third reported psychological trauma related to the COVID-19 health crisis. A minority reported increased smoking, alcohol use, or cannabis use. More than a quarter reported sleeping less than 6 hours per night. Nearly half reported never having seen a general practitioner. More than half said they spent more than 40 hours a week studying. More than three quarters reported a very high level of study-related stress. The majority reported difficulties related to personal and occupational time management. However, half reported helping each other and nearly two thirds reported recognition of their work. Nearly 15% reported suicidal ideation and 4% reported a suicide attempt.
Table 1.
Medical characteristics.
| Psychological Distress | |||||||
|---|---|---|---|---|---|---|---|
| Total | Yes (N = 625, 75.1%) |
No (N = 207, 24.9%) |
|||||
| N | % | N | % | N | % | ||
| Gender | Women | 609 | 73.2 | 470 | 77.2 | 139 | 22.8 |
| Men | 223 | 26.8 | 155 | 69.5 | 68 | 30.5 | |
| Age | 18 years | 248 | 29.8 | 197 | 79.4 | 51 | 20.6 |
| 19–20 years | 339 | 40.7 | 248 | 73.2 | 91 | 26.8 | |
| 21 years and over | 244 | 29.4 | 180 | 73.8 | 64 | 26.2 | |
| Family situation | Single | 623 | 75.0 | 466 | 25.2 | 157 | 74.8 |
| In a couple | 203 | 24.4 | 155 | 76.3 | 48 | 23.7 | |
| Widowed, Separated, Divorced | 5 | 0.6 | 4 | 80.0 | 1 | 20.0 | |
| Living alone | Yes | 32 | 3.8 | 22 | 68.8 | 10 | 31.2 |
| No | 799 | 96.1 | 196 | 24.5 | 603 | 85.5 | |
| Financial difficulties | Low | 684 | 84.3 | 519 | 75.9 | 165 | 24.1 |
| High | 78 | 9.6 | 66 | 84.6 | 12 | 15.4 | |
| Don’t know | 49 | 6.0 | 40 | 81.6 | 9 | 18.4 | |
| Perceived health status | Poor to mediocre | 99 | 13.3 | 97 | 98.0 | 2 | 2.0 |
| Moderate | 368 | 49.6 | 322 | 87.5 | 46 | 12.5 | |
| High, very high | 275 | 37.1 | 183 | 33.4 | 92 | 66.5 | |
| Perceived stress level | Low to moderate | 368 | 49.6 | 251 | 68.2 | 117 | 31.8 |
| High | 374 | 50.4 | 351 | 93.9 | 23 | 6.1 | |
| Trauma experienced during the COVID-19 crisis | No | 510 | 68.7 | 388 | 76.1 | 122 | 29.9 |
| Yes | 232 | 31.3 | 214 | 92.2 | 18 | 7.8 | |
| History of anxiety disorders | No | 650 | 87.6 | 519 | 79.8 | 131 | 20.1 |
| Yes | 92 | 12.4 | 83 | 90.2 | 9 | 9.8 | |
| History of depression | No | 688 | 92.7 | 553 | 80.4 | 135 | 19.6 |
| Yes | 54 | 7.3 | 49 | 90.7 | 5 | 903 | |
| Presence of suicidal ideation | No | 631 | 85.2 | 494 | 78.3 | 137 | 21.7 |
| Yes | 109 | 14.7 | 106 | 97.3 | 3 | 2.7 | |
| History of suicide attempts | No | 684 | 95.9 | 549 | 80.3 | 135 | 19.7 |
| Yes | 29 | 4.1 | 28 | 96.5 | 1 | 3.5 | |
| Average sleep duration | <6 h | 189 | 25.6 | 172 | 91.0 | 17 | 9.0 |
| 7–8 h | 494 | 67.0 | 389 | 78.8 | 105 | 21.2 | |
| ≥9 h | 54 | 7.3 | 37 | 68.5 | 17 | 31.5 | |
| Practice of a sport activity | Never | 219 | 29.7 | 189 | 86.3 | 30 | 13.7 |
| Rarely | 180 | 24.4 | 158 | 87.8 | 22 | 12.2 | |
| Once a week | 139 | 18.8 | 103 | 74.1 | 36 | 25.9 | |
| Several times a week | 164 | 22.2 | 124 | 75.6 | 40 | 24.4 | |
| Every day | 35 | 4.7 | 24 | 68.6 | 11 | 31.4 | |
| Frequency of alcohol consumption | Never | 324 | 44.0 | 267 | 82.4 | 57 | 17.6 |
| Less than once a month | 186 | 25.2 | 154 | 82.8 | 32 | 17.2 | |
| Between once a month and once a week | 196 | 26.6 | 156 | 79.6 | 40 | 20.4 | |
| Several times a week | 31 | 4.2 | 21 | 67.7 | 10 | 32.3 | |
| Possible changes in alcohol consumption | No, I never drink alcohol | 298 | 40.4 | 245 | 82.2 | 53 | 17.8 |
| No, I kept the same alcohol consumption | 188 | 25.5 | 141 | 75.0 | 47 | 25.0 | |
| Yes, I have cut down on my drinking a bit | 215 | 29.2 | 181 | 84.2 | 34 | 15.8 | |
| Yes, I have increased my alcohol consumption a bit | 36 | 4.9 | 31 | 86.1 | 5 | 13.9 | |
| Smoking | No | 654 | 88.8 | 525 | 80.3 | 129 | 17.7 |
| Yes | 83 | 11.2 | 73 | 87.9 | 10 | 12.1 | |
| Possible changes in smoking | No, I never smoke | 638 | 86.6 | 513 | 80.4 | 125 | 19.6 |
| No, I kept the same smoking level | 19 | 2.6 | 4 | 78.9 | 15 | 21.1 | |
| Yes, I have cut down on smoking a bit | 21 | 2.8 | 5 | 23.8 | 16 | 76.2 | |
| Yes, I have increased smoking a bit | 59 | 8.0 | 54 | 91.5 | 5 | 8.5 | |
| Cannabis use | No | 698 | 94.7 | 563 | 80.7 | 135 | 19.3 |
| Yes | 39 | 5.3 | 35 | 89.7 | 4 | 10.3 | |
| Possible changes in cannabis use | Never | 696 | 94.4 | 562 | 80.7 | 134 | 19.3 |
| No change | 25 | 3.4 | 22 | 88.0 | 3 | 12.0 | |
| Decrease | 8 | 1.1 | 7 | 12.5 | 1 | 87.5 | |
| Increase | 8 | 1.1 | 7 | 12.5 | 1 | 87.5 | |
| Date of last consultation with a general practitioner | <12 months | 165 | 22.4 | 125 | 75.8 | 40 | 24.2 |
| ≥12 months | 211 | 28.6 | 166 | 78.7 | 45 | 21.3 | |
| Never consulted a general practitioner | 362 | 49.0 | 307 | 84.8 | 55 | 15.2 | |
Table 2.
Educational characteristics.
| Psychological Distress | |||||||
|---|---|---|---|---|---|---|---|
| Total | Yes (N = 625, 75.1%) |
No (N = 207, 24.9%) |
|||||
| N | % | N | % | N | % | ||
| Seniority in medical studies | 1st year | 492 | 59.4 | 379 | 77.0 | 113 | 23.0 |
| 2nd and 3rd year | 128 | 15.4 | 94 | 73.4 | 34 | 26.6 | |
| 4th, 5th, and 6th year | 209 | 25.2 | 152 | 72.7 | 57 | 27.3 | |
| Weekly study time (hours) | <10 h | 79 | 10.8 | 64 | 19.0 | 15 | 81.0 |
| 10–19 h | 72 | 9.9 | 56 | 77.8 | 16 | 22.2 | |
| 20–29 h | 63 | 8.6 | 47 | 74.6 | 16 | 25.4 | |
| 30–39 h | 100 | 13.7 | 74 | 74.0 | 26 | 26.0 | |
| 40–49 h | 88 | 12.1 | 77 | 87.5 | 11 | 12.5 | |
| >50 h | 326 | 44.8 | 272 | 83.4 | 54 | 16.6 | |
| Sense of mutual support and cooperation | Yes | 382 | 52.5 | 277 | 72.5 | 105 | 27.5 |
| No | 346 | 47.5 | 313 | 90.5 | 33 | 9.5 | |
| Impression of recognized work | Yes | 286 | 60.7 | 192 | 67.1 | 94 | 32.9 |
| No | 442 | 39.3 | 398 | 90.0 | 44 | 10.0 | |
| Perceived level of stress related to studies | Low to moderate | 171 | 23.5 | 88 | 51.5 | 83 | 48.5 |
| High | 558 | 76.5 | 503 | 90.1 | 55 | 9.9 | |
| Face-to-face courses in the last 3 months | No | 541 | 74.3 | 443 | 81.9 | 98 | 18.1 |
| Yes, 1 day a week on average | 139 | 19.1 | 110 | 79.1 | 29 | 20.9 | |
| Yes, 2 days a week on average | 32 | 4.4 | 27 | 84.4 | 5 | 15.6 | |
| Yes, 3 days per week on average | 16 | 2.2 | 10 | 62.5 | 6 | 37.5 | |
| Hospital internship in the last 3 months | No | 439 | 60.3 | 369 | 84.0 | 70 | 16.0 |
| Yes | 289 | 39.7 | 221 | 76.5 | 68 | 23.5 | |
| Internship in COVID-19 care units | No | 567 | 77.9 | 469 | 82.7 | 98 | 17.3 |
| Yes | 161 | 22.1 | 121 | 75.2 | 40 | 24.8 | |
| Difficulties in following distance learning courses due to: | |||||||
| Time management, personal life, or occupational life | No | 76 | 12.7 | 184 | 84.4 | 34 | 15.6 |
| Yes | 524 | 87.3 | 399 | 88.7 | 43 | 11.3 | |
| Workload | No | 228 | 38.0 | 180 | 78.9 | 48 | 21.1 |
| Yes | 372 | 62.0 | 343 | 92.2 | 29 | 7.8 | |
| Lack of communication with the teaching staff | No | 341 | 56.8 | 291 | 85.34 | 50 | 14.66 |
| Yes | 259 | 43.2 | 232 | 89.6 | 27 | 10.4 | |
| Work location | No | 378 | 63.0 | 326 | 86.2 | 52 | 13.8 |
| Yes | 222 | 37.0 | 197 | 88.7 | 25 | 11.3 | |
| Lack of communication with other students | No | 481 | 80.2 | 414 | 86.0 | 67 | 14.0 |
| Yes | 119 | 19.8 | 109 | 91.6 | 10 | 8.4 | |
| Equipment | No | 524 | 87.3 | 455 | 86.8 | 69 | 13.2 |
| Yes | 76 | 12.7 | 68 | 89.5 | 8 | 10.5 | |
| Paid work outside the framework of studies | No | 570 | 78.3 | 466 | 81.8 | 104 | 18.2 |
| Yes | 158 | 11.7 | 124 | 78.5 | 34 | 21.5 | |
Figure 1.
Flowchart of the studied population.
3.2. Prevalence of Psychological Distress
A total of 625 respondents (75%) presented psychological distress.
3.3. Relations between Psychological Distress and Educational and Medical Factors on Univariate Analysis
A search for multicollinearity was conducted for the following variables: age, gender, financial difficulties, trauma experienced during the COVID-19 crisis, history of anxiety disorders, history of depression, changes in alcohol consumption, changes in smoking, paid work outside the framework of studies, sense of mutual support and cooperation, impression of recognized work, hospital internship in the last 3 months, internship in COVID-19 care units, difficulties in following distance learning courses, and date of last consultation with a general practitioner. Following this analysis, it was decided to remove the variable for an internship during the last three months due to a significant multicollinearity with other variables.
As shown in Table 3, the univariate analysis produced associations between psychological distress and the following:
Female gender, PR = 1.12 (1.02–1.23)
Age, PR = 0.98 (0.96–0.99);
1st year of medical school (major), PR = 1.11 (1.01–1.21);
Financial difficulties, PR = 1.11 (1.01–1.22);
Psychological trauma during the health crisis COVID-19, PR = 1.21 (1.11–1.29);
History of anxiety disorder, PR = 1.12 (1.03–1.22);
History of depression, PR = 1.13 (1.03–1.24);
Change in smoking, PR = 1.08 (0.99–1.19);
Change in alcohol consumption, PR = 1.08 (1.01–1.16);
Sense of mutual support and cooperation, PR = 0.80 (0.75–0.86);
Impression of recognized work, PR = 0.75 (0.69–0.82);
Hospital internship within the last three months, PR = 0.91 (0.84–0.98);
Hospital internship on a COVID-19 ward within the last three months, PR = 0.90 (0.81–0.99);
Experiencing difficulties with online learning, PR = 1.64 (1.39–1.94).
Table 3.
Factors associated with psychological distress on univariate and multivariate analysis.
| Psychological Distress | |||
|---|---|---|---|
| Variables | PR [CI] | Adjusted PR [CI] | |
| Gender | Women (ref: Men) | 1.12 [1.02–1.23] * | 1.09 [1.00–1.19] * |
| Age | 0.98 [0.96–0.99] * | 0.98 [0.95–1.01] | |
| Seniority in the medical studies | 1st year medicine main stream (ref: 4th, 5th, and 6th year) | 1.11 [1.01–1.21] * | 0.92 [0.77–1.12] |
| Financial difficulties | Yes (ref: NO) | 1.11 [1.01–1.22] * | 1.03 [0.93–1.15] |
| Trauma experienced during the COVID-19 crisis | Yes (ref: NO) | 1.21 [1.11–1.29] **** | 1.10 [1.03–1.16] ** |
| History of anxiety disorder | Yes (ref: NO) | 1.12 [1.03–1.22] ** | 1.11 [1.01–1.20] * |
| History of depression | Yes (ref: NO) | 1.13 [1.03–1.24] * | 1.01 [0.91–1.12] |
| Possible change in alcohol consumption | Yes (ref: NO) | 1.08 [1.01–1.16] * | 1.12 [1.05–1.20] ** |
| Possible change in smoking | Yes (ref: NO) | 1.08 [0.99–1.19] | 1.01 [0.92–1.11] |
| Paid work outside the framework of studies | Yes (ref: NO) | 0.90 [0.81–1.00] | 0.92 [0.82–1.03] |
| Sense of mutual support and cooperation | Yes (ref: NO) | 0.80 [0.75–0.86] **** | 0.92 [0.86–0.98] * |
| Impression of recognized work | Yes (ref: NO) | 0.75 [0.69–0.82] **** | 0.84 [0.77–0.91] *** |
| Hospital internship in the last 3 months | Yes (ref: NO) | 0.91 [0.84–0.98] * | / |
| Internship in COVID-19 care units | Yes (ref: NO) | 0.90 [0.81–0.99] * | 0.94 [0.82–1.08] |
| Difficulties in following distance learning courses | Yes (ref: NO) | 1.64 [1.39–1.94] **** | 1.50 [1.28–1.77] *** |
| Consultation with a general practitioner | Yes (ref: NO) | 0.91 [0.85–0.98] * | 0.97 [0.90–1.05] |
p-value ≤ 0.2; * p-value < 0.05; ** p-value < 0.01; *** p-value < 0.001; **** p-value< 0.0001; PR: prevalence ratio; CI: 95% confidence interval.
In contrast, psychological distress was not significantly associated with increased cannabis use or weekly study workload.
3.4. Relations between Psychological Distress and Educational and Medical Factors in Multivariate Analysis
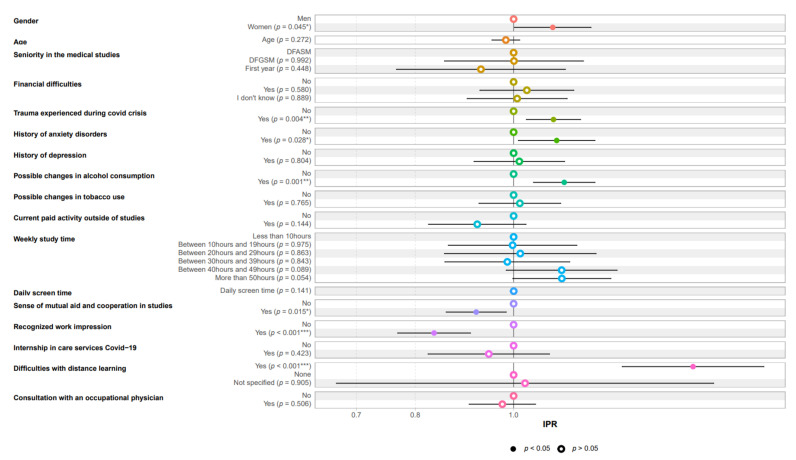
As shown in Table 3 and Figure 2, in the multivariate analysis, psychological distress remained associated with female gender, a history of anxiety disorders, psychological trauma during the health crisis, change in alcohol consumption, and difficulties in online learning. The feeling of mutual aid and cooperation within the studies framework and work recognition appeared to be protective factors.
Figure 2.
Factors associated with psychological distress in multivariate analysis.
4. Discussion
Medical students have been shown to be at higher risk of mental health disorders during training [24]. Although medical students have better access to mental health care, they are less likely to seek help than the general population, mainly due to the stigma attached to mental health disorders [25]. Our study showed a 75% prevalence of psychological distress in medical students in years 1–6. This rate was higher than for Essangri et al. in a cross-sectional online survey conducted from 8 April to 18 April 2020 which showed a 69% prevalence of psychological distress in medical students in Morocco. Meta-analyses indicated that 9–54% of students worldwide experience psychological distress. These differences can be explained by the context of the health crisis: lockdown, distance learning, fear of contracting COVID-19, and social insecurity. Students may be consumed by major uncertainties regarding their future and educational perspectives. Distance education and examinations may increase their level of uncertainty and stress, either because these involve new and unfamiliar teaching and assessment modalities or because distance supervision, communication, and monitoring by teachers has not been sufficiently clear, structured, or reassuring [26].
Our results showed greater risk of psychological distress in women. These findings are consistent with the literature. Previous mental health research highlighted female gender as a vulnerability factor for poorer mental health and well-being [27].
Nearly one third of medical students reported a traumatic event during the COVID-19 health crisis. This rate was lower than that reported by Waseem et al., who found that more than half of Pakistani medical students showed moderate to severe post-traumatic stress (54.10%) [28]. These differences could be explained by the alarming increase in the number of COVID-19 cases in Pakistan during the period in which the study was conducted. Our study showed an association between traumatic events and psychological distress, which is consistent with the findings of Lasalvia et al. that half of the 2195 healthcare workers who reported a COVID-19-related traumatic experience also reported symptoms of clinically significant anxiety [29].
Similar to Clay and Parker’s, our findings showed that a larger percentage of students decreased than increased their alcohol consumption [30]. Young people mainly use alcohol in social contexts, and drink alcohol less often and in smaller quantities but with an anxiolytic effect [26]. However, our study highlighted the significant association between psychological distress and change in alcohol consumption. This significant association was maintained after adjustment for other co-variates. These results are consistent with those of Lechner et al., who showed that more severe psychological distress in students was associated with higher alcohol consumption overall. These results underline the value of the early detection of increased alcohol consumption in the prevention of psychological distress in students.
The difficulties associated with distance learning emerged as a risk factor for students’ psychological distress. The closure of universities and public libraries and the limited access to alternative study spaces forced many students into an unaccustomed learning environment [31]. The rapid change in the system and environment could cause significant stress to medical students [32]. Due to the pandemic, which forced educational institutions to eliminate in-person teaching sessions, medical students needed to adapt to new educational environments, such as distance e-learning [33]. The rapid change in the system and environment could cause significant stress to medical students [34]. Turning to distance learning on a global scale leads to a risk of exacerbating educational inequalities, jeopardizing students’ mental health [35]. Accumulating evidence suggests that mindful coping effectively reduces stress and anxiety in college students. Improvements in self-esteem and self-efficacy would strengthen resilience and motivation towards learning and career development [36].
Students also reported difficulties with distance learning due to time management, personal life/working life balance, workload, and a lack of communication with teaching staff. Our findings highlighted the protective effect of social support against psychological distress. These results corroborate those of previous studies [37,38]. Psychological support should be tailored to each student’s needs and incorporated into the online remote curriculum [39].
The study also highlighted how mutual help in studies has a protective effect against psychological distress. Low perceived social support was significantly associated with an increased risk of psychological distress [40]. According to Cao et al., people with low perceived social support were at high risk of psychological pressure, while high perceived social support had a positive effect on anxiety and stress during the COVID-19 epidemic [41]. Moreover, poor esteem due to superiors emerged as a risk factor for psychological distress [42,43]. In our study, recognition of the work performed appeared to be a protective factor against psychological distress. This result emphasizes the benefits of supportive communication in preventing psychological distress in students.
Moreover, our study highlighted how maintaining occupational activity has a protective effect against psychological distress. These results corroborate those of previous studies. According to Essadek et al., being in a precarious financial situation significantly increased levels of depression, anxiety, and distress [44]. As shown in previous studies, there may be an increasing prevalence of food insecurity during the pandemic, negatively affecting students’ mental well-being [34,45,46]. To prevent financial insecurity for students, the French government implemented a policy of financial aid (meals at €1 and exceptional aid in case of job loss).
Strengths and Limitations
The strengths and limitations of the current study are determined by several issues. We collected data from one medical school only; this may be a somewhat unbalanced sample that does not fully represent the diversity of medical students currently in training in France. In addition, the sample in our study has a slightly different distribution from the source population with regard to gender (73% women in the sample, 66% in the population) and years of study (60% first-year students in the sample, 56% in the population). These differences in distribution may contribute to an overestimation of psychological distress. Indeed, according to our study, female gender appears to be a factor positively associated with psychological distress, while age appears to be negatively associated with psychological distress. These results are consistent with the study by Maser et al. of Canadian medical students [47]. Furthermore, 45% of the students enrolled at Saint-Etienne medical school agreed to participate in this study. Of these, 92% completed the GHQ-12 and 84% completed the questionnaire in full. The refusal and dropout rates of this study should be considered before generalizing the findings of this study.
Moreover, we adopted a convenient online survey in only one university in France, which may contribute to some bias in the study results. The e-questionnaire assessed the prevalence of psychological distress in university students adhering to WHO-recommended “social distancing” during the COVID-19 pandemic. The e-survey data were collected by globally validated standardized tools for quantitative analysis. In this cross-sectional study, the identified factors were regarded as associated factors, which could either be the causes or the results of psychological distress. Furthermore, due to the ethical requirements of anonymity and confidentiality, the contact details of the respondents were not collected. However, the use of a validated screening e-questionnaire was considered to be a cost-effective approach to explore the situation in general, and was therefore used in this study. Since the research methodology could not reach people with psychological distress under treatment, the results may not fully reflect the severity of psychological distress symptoms in students. A follow-up study could follow up the same participants to determine the persistence or transience of the perceived psychological distress. Mental health problems in medical students need to be further assessed longitudinally.
5. Conclusions
The high prevalence of psychological distress among medical students observed in our study shows the importance of promoting early detection by preventive and occupational medicine services and facilitating psychological management by psychologists. It is suggested that the government and universities should collaborate to resolve this problem and provide high-quality and timely crisis-oriented psychological services to medical students [48]. This care should be based on the implementation by the French government, since 10 March 2021, of a national platform of psychological support for students; sessions with a psychologist, of up to three meetings of 45 min each, are completely free. The identification of risk factors and protective factors for psychological distress can determine adapted means of preventing psychological distress in medical students. The deployment of distance learning should be based on pedagogical support, including frequent exchanges with teachers and other students. Longitudinal follow-up studies are required to track the progression of psychological distress in medical students and measure the long-term impact of the pandemic.
Acknowledgments
The authors thank the students for their participation.
Author Contributions
Conceptualization, C.P., P.B., B.P., C.M., and L.F.; Data Curation, C.P.; Formal analysis, T.T; Investigation, C.P. and M.V.; Methodology, C.P., P.B., C.M., and L.F.; Project administration, C.P., M.V., P.B., and C.M; Resources, P.B.; Software, T.T.; Supervision, C.P. and L.F.; Validation, C.P., M.V., P.B., B.P., C.M., T.T., and L.F.; Visualization, C.P., P.B., C.M., T.T., and L.F.; Writing—original draft, C.P.; Writing—review and editing, P.B., C.M., T.T., and L.F. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no funding for this study.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of (University Hospital Center of Saint-Etienne IRBN272021/CHUSTE, 25 February 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The date are not publicly available due to confidentiality of participants.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mizumoto K., Chowell G. Estimating Risk for Death from 2019 Novel Coronavirus Disease, China, January–February 2020. Emerg. Infect Dis. 2020;26:1251. doi: 10.3201/eid2606.200233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puthran R., Zhang M.W.B., Tam W.W., Ho R.C. Prevalence of depression amongst medical students: A meta-analysis. Med. Educ. Avr. 2016;50:456–468. doi: 10.1111/medu.12962. [DOI] [PubMed] [Google Scholar]
- 4.Adams J. Straining to describe and tackle stress in medical students. Med. Educ. 2004;38:463–464. doi: 10.1111/j.1365-2929.2004.01810.x. [DOI] [PubMed] [Google Scholar]
- 5.Bayram N., Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc. Psychiatry Psychiatr. Epidemiol. 2008;43:667–672. doi: 10.1007/s00127-008-0345-x. [DOI] [PubMed] [Google Scholar]
- 6.Hill M.R., Goicochea S., Merlo L.J. In their own words: Stressors facing medical students in the millennial generation. Med. Educ. Online. 2018;23:1530558. doi: 10.1080/10872981.2018.1530558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenthal J.M., Okie S. White Coat, Mood Indigo—Depression in Medical School. N. Engl. J. Med. 2005;353:1085–1088. doi: 10.1056/NEJMp058183. [DOI] [PubMed] [Google Scholar]
- 8.Sherina M.S., Rampal L., Kaneson N. Psychological stress among undergraduate medical students. Med. J. Malays. 2004;59:207–211. [PubMed] [Google Scholar]
- 9.Yusoff M.S.B., Rahim A. Stress, Stressors and Coping Strategies: First Year Medical Students in Malaysian Public Universities. VDM Publishing; Saarbrücken, Germany: 2011. [Google Scholar]
- 10.Dyrbye L.N., Thomas M.R., Shanafelt T.D. Systematic Review of Depression, Anxiety, and Other Indicators of Psychological Distress Among, U.S. and Canadian Medical Students. Acad. Med. Avr. 2006;81:354–373. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Mousa O.Y., Dhamoon M.S., Lander S., Dhamoon A.S. The MD Blues: Under-Recognized Depression and Anxiety in Medical Trainees. PLoS ONE. 2016;11:e0156554. doi: 10.1371/journal.pone.0156554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yusoff M.S.B., Abdul Rahim A.F., Baba A.A., Ismail S.B., Mat Pa M.N., Esa A.R. The impact of medical education on psychological health of students: A cohort study. Psychol. Health Med. 2013;18:420–430. doi: 10.1080/13548506.2012.740162. [DOI] [PubMed] [Google Scholar]
- 13.Dutheil F., Aubert C., Pereira B., Dambrun M., Moustafa F., Mermillod M., Baker J.S., Trousselard M., Lesage F.-X., Navel V. Suicide among physicians and health-care workers: A systematic review and meta-analysis. PLoS ONE. 2019;14:e0226361. doi: 10.1371/journal.pone.0226361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong J.G.W.S., Cheung E.P.T., Cheung V., Cheung C., Chan M.T.Y., Chua S.E., McAlonan G., Tsang K.W., Ip M.S.M. Psychological responses to the SARS outbreak in healthcare students in Hong Kong. Med. Teach. 2004;26:657–659. doi: 10.1080/01421590400006572. [DOI] [PubMed] [Google Scholar]
- 15.Jaisoorya T.S., Janardhan Reddy Y.C., Nair B.S., Rani A., Menon P.G., Revamma M., Jeevan C.R., Radhakrishnan K.S., Jose V., Thennarasu K. Prevalence and correlates of obsessive-compulsive disorder and subthreshold obsessive-compulsive disorder among college students in Kerala, India. Indian J. Psychiatry. 2017;59:56–62. doi: 10.4103/0019-5545.204438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ishii T., Tachikawa H., Shiratori Y., Hori T., Aiba M., Kuga K., Arai T. What kinds of factors affect the academic outcomes of university students with mental disorders? A retrospective study based on medical records. Asian J. Psychiatry. 2018;32:67–72. doi: 10.1016/j.ajp.2017.11.017. [DOI] [PubMed] [Google Scholar]
- 17.Sante Publique France; 2020. [(accessed on 3 December 2021)]. Point Épidémio Régional Spécial COVID 19 Auvergne Rhône Alpes 29 Octobre 2020. Available online: https://www.auvergne-rhone-alpes.ars.sante.fr/system/files/2020-10/20201029_PER_COVID19_ARA.VF__0.pdf. [Google Scholar]
- 18.Lesage F.-X., Martens-Resende S., Deschamps F., Berjot S. Validation of the General Health Questionnaire (GHQ-12] adapted to a work-related context. Open J. Prev. Med. 2011;1:44–48. doi: 10.4236/ojpm.2011.12007. [DOI] [Google Scholar]
- 19.Goldberg D. User’s Guide to the General Health Questionnaire. 1988. [(accessed on 29 July 2021)]. Windsor. Available online: https://ci.nii.ac.jp/naid/10016919943/
- 20.Goldberg D.P., Gater R., Sartorius N., Ustun T.B., Piccinelli M., Gureje O., Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997;27:191–197. doi: 10.1017/S0033291796004242. [DOI] [PubMed] [Google Scholar]
- 21.Yusoff M.S.B. The validity of two malay versions of the general health questionnaire (ghq) in detecting distressed medical students. ASEAN J. Psychiatry. 2010;11:135–142. [Google Scholar]
- 22.Goldberg D. The Detection of Minor Psychiatric Illness by Questionnaire. Oxford University Press; Oxford, UK: 1972. [Google Scholar]
- 23.Zou G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am. J. Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 24.Moffat K.J., McConnachie A., Ross S., Morrison J.M. First year medical student stress and coping in a problem-based learning medical curriculum. Med. Educ. 2004;38:482–491. doi: 10.1046/j.1365-2929.2004.01814.x. [DOI] [PubMed] [Google Scholar]
- 25.Saraswathi I., Saikarthik J., Senthil Kumar K., Madhan Srinivasan K., Ardhanaari M., Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study. PeerJ. 2020;8:e10164. doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glowacz F., Schmits E. Psychological distress during the COVID-19 lockdown: The young adults most at risk. Psychiatry Res. 2020;293:113486. doi: 10.1016/j.psychres.2020.113486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seedat S., Scott K.M., Angermeyer M.C., Berglund P., Bromet E.J., Brugha T.S., Demyttenaere K., de Girolamo G., Haro J.M., Jin R., et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. AMA Arch. Gen. Psychiatry. 2009;66:785–795. doi: 10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waseem M., Aziz N., Arif M.U., Noor A., Mustafa M., Khalid Z. Impact of post-traumatic stress of covid-19 on mental wellbeing of undergraduate medical students in pakistan. Pafmj. 2020;70:S220–S224. [Google Scholar]
- 29.Lasalvia A., Bonetto C., Porru S., Carta A., Tardivo S., Bovo C., Ruggeri M., Amaddeo F. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiol. Psychiatry Sci. 2020;30:e1. doi: 10.1017/S2045796020001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clay J.M., Parker M.O. Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? Lancet. Public. Health. 2020;5:e259. doi: 10.1016/S2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Byrne L., Gavin B., McNicholas F. Medical students and COVID-19: The need for pandemic preparedness. [(accessed on 6 August 2021)];J. Med. Ethics. 2020 46:623–626. doi: 10.1136/medethics-2020-106353. Available online: https://covid19.elsevierpure.com/en/publications/medical-students-and-covid-19-the-need-for-pandemic-preparedness. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bamber M.D., Kraenzle Schneider J. Mindfulness-based meditation to decrease stress and anxiety in college students: A narrative synthesis of the research. Educ. Res. Rev. 2016;18:1–32. doi: 10.1016/j.edurev.2015.12.004. [DOI] [Google Scholar]
- 33.Al-Balas M., Al-Balas H.I., Jaber H.M., Obeidat K., Al-Balas H., Aborajooh E.A., Al-Taher R., Al-Bala B. Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: Current situation, challenges, and perspectives. BMC Med. Educ. 2020:341. doi: 10.1186/s12909-020-02257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nishimura Y., Ochi K., Tokumasu K., Obika M., Hagiya H., Kataoka H., Otsuka F. Impact of the COVID-19 Pandemic on the Psychological Distress of Medical Students in Japan: Cross-sectional Survey Study. J. Med. Internet Res. 2021;23:e25232. doi: 10.2196/25232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Długosz P. The Relationship between Mental Health, Educational Burnout and Strategies for Coping with Stress among Students. A Cross-Sect. Study Polan. 2021;18:10827. doi: 10.20944/preprints202106.0267.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arima M., Takamiya Y., Furuta A., Siriratsivawong K., Tsuchiya S., Izumi M. Factors associated with the mental health status of medical students during the COVID-19 pandemic: A cross-sectional study in Japan. BMJ Open. 2020;10:e043728. doi: 10.1136/bmjopen-2020-043728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alsubaie M.M., Stain H.J., Webster L.A.D., Wadman R. The role of sources of social support on depression and quality of life for university students. Int. J. Adolesc. Youth. 2019;24:484–496. doi: 10.1080/02673843.2019.1568887. [DOI] [Google Scholar]
- 38.Kim H.C. Friends support as a mediator in the association between depressive symptoms and self-stigma among university students in South Korea. Int. J. Ment. Health. 2020;49:247–253. doi: 10.1080/00207411.2020.1781425. [DOI] [Google Scholar]
- 39.Saddik B., Hussein A., Sharif-Askari F.S., Kheder W., Temsah M.-H., Koutaich R.A., Haddad E.S., Al-Roub N.M., Marhoon F.A., Hamid Q., et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020;13 doi: 10.2147/RMHP.S273333.2020.05.10.20096933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ma Z., Zhao J., Li Y., Chen D., Wang T., Zhang Z., Chen Z., Yu Q., Jiang J., Fan F., et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiaty Sci. 2020;29:e181. doi: 10.1017/S2045796020000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pélissier C., Fontana L., For T.E., Vohito M., Sellier B., Perrier C., Fontana L., Fort E., Vohito M., Sellier B., et al. Impaired mental well-being and psychosocial risk: A cross-sectional study in female nursing home direct staff. BMJ Open. 2015;5:e007190. doi: 10.1136/bmjopen-2014-007190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vegchel N., van de Jonge J., Bakker A.B., Schaufeli W.B. Testing global and specific indicators of rewards in the Effort-Reward Imbalance Model: Does it make any difference? Eur. J. Work. Organ. Psychol. 2002;11:403–421. doi: 10.1080/13594320244000265. [DOI] [Google Scholar]
- 44.Essadek A., Rabeyron T. Mental health of French students during the Covid-19 pandemic. J. Affect. Disord. 2020;277:392–393. doi: 10.1016/j.jad.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Owens M.R., Brito-Silva F., Kirkland T., Moore C.E., Davis K.E., Patterson M.A., Miketinas D.C., Tucker W.J. Prevalence and Social Determinants of Food Insecurity among College Students during the COVID-19 Pandemic. Nutrients. 2020;12:2515. doi: 10.3390/nu12092515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wolfson J.A., Leung C.W. Food Insecurity and COVID-19: Disparities in Early Effects for US Adults. Nutrients. 2020;12:1648. doi: 10.3390/nu12061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maser B., Danilewitz M., Guérin E., Findlay L., Frank E. Medical Student Psychological Distress and Mental Illness Relative to the General Population: A Canadian Cross-Sectional Survey. Acad. Med. 2019;94:1781–1791. doi: 10.1097/ACM.0000000000002958. [DOI] [PubMed] [Google Scholar]
- 48.Essangri H., Sabir M., Benkabbou A., Majbar M.A., Amrani L., Ghannam A., Lekehal B., Mohsine R., Souadka A. Predictive Factors for Impaired Mental Health among Medical Students during the Early Stage of the COVID-19 Pandemic in Morocco. Am. J. Trop. Med. Hyg. 2020;104:95–102. doi: 10.4269/ajtmh.20-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The date are not publicly available due to confidentiality of participants.