Abstract
A new immunochromatographic assay for rapid qualitative detection of Legionella pneumophila serogroup 1 antigen in urine specimens was used during an outbreak of legionellosis in The Netherlands. The assay seems of the utmost value in providing a rapid diagnosis of Legionnaires' disease in patients with severe community-acquired pneumonia in an outbreak setting.
Legionellosis, an infection due to Legionella species, presents in two different forms: Pontiac fever, an acute self-limiting flu-like illness, and pneumonia or Legionnaires' disease. Legionella pneumophila serogroup 1 is the cause of more than 80% of the cases of legionellosis in The Netherlands. Patients with Legionnaires' disease have a variety of signs and symptoms, but none of the clinical features is sufficiently specific to establish the diagnosis. Because the rate of mortality from untreated Legionnaires' disease ranges from 10 to 50%, rapid diagnosis and early antibiotic treatment are required (3, 5, 6, 7). Detection of L. pneumophila serogroup 1 antigen in urine specimens by radioimmunoassay and enzyme-linked immunosorbent assay methods has long been used as a tool for the diagnosis of Legionnaires' disease (1, 2, 4, 8, 9). Assays for the detection of L. pneumophila serogroup 1 antigen in urine have a sensitivity of 70% and a specificity that approaches 100% (7). Recently, an immunochromatographic assay for the rapid qualitative detection of L. pneumophila serogroup 1 antigen (Legionella NOW; Binax, Portland, Maine) in urine specimens has become available. This assay uses rabbit anti-L. pneumophila serogroup 1 antibody as the capture component and rabbit anti-L. pneumophila serogroup 1 antibody conjugated to colloidal gold as the detection component. The assay provides a test result in 15 min and is intended to aid in the presumptive diagnosis of Legionnaires' disease caused by L. pneumophila serogroup 1 in conjunction with culture and other methods. Preliminary performance data for the immunochromatographic assay report a sensitivity of 95% and a specificity of 95% (N. Moore and D. Gentile, Abstr. 99th Gen. Meet. Am. Soc. Microbiol. 1999, abstr. C-19, p. 108, 1999).
The immunochromatographic assay was extensively used during a recent outbreak of legionellosis in The Netherlands. An outbreak became apparent on 11 March 1999, when an investigative team from the Academic Medical Center, Amsterdam, detected L. pneumophila serogroup 1 antigen in urine specimens from seven patients admitted to a regional hospital in Hoorn because of severe community-acquired pneumonia (CAP). Simultaneously, L. pneumophila serogroup 1 antigen was also detected in urine specimens from two patients with severe CAP at the Laboratory of Public Health, Haarlem. Both patients were transferred from the regional hospital in Hoorn to a Haarlem hospital for respiratory support. A subsequent epidemiological investigation revealed that the nine patients had been among the 80,000 visitors of the Westfriese Flora, a flower show held annually in Bovenkarspel, The Netherlands, from 19 to 28 February 1999. On 12 March, L. pneumophila serogroup 1 antigen was detected in urine specimens from two additional patients admitted to the regional hospital in Hoorn and four patients admitted to hospitals in the Amsterdam area. In addition, the presumptive diagnosis of Legionnaires' disease was confirmed on that day by a positive direct immunofluorescence assay result for L. pneumophila in lung tissue acquired from one patient postmortem. On the same day, the National Health Department informed the general public of the outbreak through a nationwide television broadcast. In the following days, we cultured L. pneumophila serogroup 1 from sputum and lavage specimens from four patients. No other pathogens were cultured.
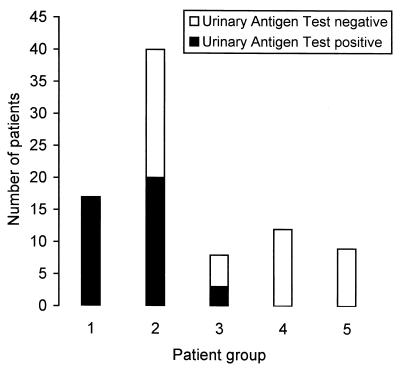
Subsequently, several institutions provided their services to other hospitals and family physicians for rapid identification of outbreak-associated cases by the immunochromatographic assay. At the Academic Medical Center, urine specimens from 86 visitors of the flower show were subjected to the immunochromatographic assay. Visitors were stratified into five patient groups according to clinical presentation. Group 1 included patients admitted to an intensive care unit because of severe pneumonia with need for respiratory support (n = 17); group 2 included patients hospitalized because of pneumonia without need for respiratory support (n = 40); group 3 included nonhospitalized patients treated for mild pneumonia (n = 8); group 4 included nonhospitalized patients who suffered or who had suffered an acute, self-limiting flu-like illness (n = 12); group 5 included patients hospitalized for reasons other than pneumonia (n = 3; carcinoma of the lung, fever of unknown origin, heart failure), hospitalized patients for whom additional clinical data were not available (n = 3), and visitors without objective symptoms (n = 3).
L. pneumophila serogroup 1 antigen was present in 40 of 86 (47%) urine specimens (Fig. 1). The immunochromatographic assay provided a presumptive diagnosis of Legionnaires' disease for 40 of 65 (62%) patients who presented with pneumonia. The immunochromatographic assay was negative for 25 of 65 (38%) patients with pneumonia. On the basis of their clinical presentations and the epidemiological timing, it was suspected that these 25 patients could have had Legionnaires' disease. The percentage of positive test results for the three pneumonia patient groups increased with the clinical severity of the pneumonia, presumably representing increased shedding of antigen from lung to urine via the blood compartment in those with more severe disease. No positive test results were obtained for the group of patients who presented with an acute, self-limiting flu-like illness.
FIG. 1.
Test results obtained by the immunochromatographic assay for detection of L. pneumophila serogroup 1 antigen in urine specimens from 86 visitors of the flower show in Bovenkarspel, The Netherlands. Visitors were stratified into five patient groups according to clinical presentation, as described in the text.
In order to study the specificity of the immunochromatographic assay, we tested corresponding urine and sputum specimens from 30 successive patients who were suspected of having serious pneumonia and who were admitted to the intensive care unit or department of pulmonology of our hospital but who had not visited the flower show. Urine specimens were tested by the immunochromatographic assay, while sputum specimens were subjected to routine bacteriological examination and were inoculated onto buffered charcoal yeast extract agar and buffered charcoal yeast extract agar with antibiotics. For this group of patients, L. pneumophila serogroup 1 antigen was not detected in urine specimens and Legionella species were not cultured from sputum specimens. Identification of pathogens cultured from the sputum specimens revealed Streptococcus pneumoniae (three samples), Haemophilus influenzae (two samples), Pseudomonas aeruginosa (three samples), Neisseria meningitidis (one sample), species of the family Enterobacteriaceae (five samples), Candida species (three samples), and Chryseobacterium meningosepticum (one sample). No bacterial pathogen was isolated from 12 patients.
Although sensitivity per se was not assessed in this setting, our findings, in conjunction with the clinical and epidemiological data for patients from this outbreak, justify the conclusion that the immunochromatographic assay for the detection of L. pneumophila serogroup 1 antigen in urine specimens is a specific assay which is of the utmost value in providing a rapid diagnosis of Legionnaires' disease, especially in patients with severe CAP in an outbreak setting. However, our data also show that clinicians and clinical microbiologists should not rely on the immunochromatographic assay as the sole test for the diagnosis of Legionnaires' disease. Furthermore, isolation and characterization of the responsible strain remain essential for epidemiological studies and identification of the source of an outbreak.
REFERENCES
- 1.Berdal B P, Farshy C E, Feely J C. Detection of Legionella pneumophila antigen in urine by enzyme-linked immunospecific assay. J Clin Microbiol. 1979;9:575–578. doi: 10.1128/jcm.9.5.575-578.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Birtles R J, Harrison T G, Samuel D, Taylor A G. Evaluation of urinary antigen ELISA for diagnosing Legionella pneumophila serogroup 1 infection. J Clin Pathol. 1990;43:685–690. doi: 10.1136/jcp.43.8.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown P D, Lerner S A. Community-acquired pneumonia. Lancet. 1998;352:1295–1302. doi: 10.1016/S0140-6736(98)02239-9. [DOI] [PubMed] [Google Scholar]
- 4.Kohler R B, Zimmerman S E, Wilson E, Allen S D, Edelstein P H, Wheat L J, White A. Rapid radioimmunoassay diagnosis of Legionnaires' disease: detection and partial characterization of urinary antigen. Ann Intern Med. 1981;94:601–605. doi: 10.7326/0003-4819-94-5-601. [DOI] [PubMed] [Google Scholar]
- 5.Meenhorst P L, van der Meer J W, Borst J. Sporadic cases of Legionnaires' disease in The Netherlands. Ann Intern Med. 1979;90:529–532. doi: 10.7326/0003-4819-90-4-529. [DOI] [PubMed] [Google Scholar]
- 6.Slack M P E. Legionella spp. In: Armstrong D, Cohen J, editors. Infectious diseases. London, United Kingdom: Harcourt Publishers Ltd.; 1999. pp. 8.20.11–8.20.13. [Google Scholar]
- 7.Stout J E, Yu V L. Legionellosis. N Engl J Med. 1997;337:682–687. doi: 10.1056/NEJM199709043371006. [DOI] [PubMed] [Google Scholar]
- 8.Tang P W, Toma S. Broad-spectrum enzyme-linked immunosorbent assay for detection of Legionella soluble antigens. J Clin Microbiol. 1986;24:556–558. doi: 10.1128/jcm.24.4.556-558.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tilton R C. Legionnaires' disease antigen detected by enzyme-linked immunosorbent assay. Ann Intern Med. 1979;90:697–698. doi: 10.7326/0003-4819-90-4-697. [DOI] [PubMed] [Google Scholar]