Abstract
The impact of coronavirus disease 2019 (COVID-19) on economic and medical systems is significant, especially in the emergency department (ED). The patterns of ED visits have also changed significantly and may play a crucial role in rearranging medical resources to the most needed departments during the pandemic.
This was a retrospective study conducted in hospitals of the Cathay Health System. All patients presented to the EDs between January 21, 2020 to April 30, 2020 (pandemic stage) and January 21, 2019 to April 30, 2019 (before the pandemic stage). Basic demographics, including visit characteristics, disposition, and chief complaints, of the patients visiting the ED between these 2 periods of time will be compared and analyzed.
A total of 71,739 patients were included in the study. A reduction in ED visits was noted in 15.1% (32,950 ED visits) during the pandemic stage. ED visiting patients with the chief complaints of upper respiratory infection and social problems increased by 14.23% and 1.86%, respectively, during the pandemic period. Critical chief complaints such as cardiac arrest, chest pain and altered mental status decreased to less than the ED visits difference (−15.1%) between the pandemic and prepandemic stages, for 0%, −7.67%, and −13.8% respectively.
Rearrangement of the ED pediatric staff to the COVID-19 special units and recruiting more social workers to the ED should be performed to respond to the COVID-19 pandemic.
Keywords: coronavirus disease 2019, emergency department, emergency visits, presenting complaints
1. Introduction
Severe acute respiratory syndrome coronavirus 2 is a highly contagious novel virus that may result in both critical and fatal conditions. The virus was transmitted by droplets or contaminated hands, with an incubation period of up to 14 days. Upper respiratory infection symptom signs are frequently presented, while timely diagnosis, quarantine, and supportive treatment are crucial to further treat these patients.[1]
In late December 2019, the first cluster of coronavirus disease 2019 (COVID-19) was reported in Wuhan, China. A few months later, the COIVD-19 virus spread worldwide, and Taiwan was no exception. On January 21, 2020, the first imported case of COVID-19 was reported in Taiwan.[2] On February 28, 2020, the first in-hospital COVID-19 cluster infection occurred, and the peak pandemic period commenced. The number of COVID-19 patients rapidly increased from March to April 2020. It was not until December 19, 2020, when the number of confirmed COVID-19 cases in Taiwan reached 759.[3]
The impact of COVID-19 on economic and medical systems is significant, especially in the emergency department (ED). In contrast to the assumed condition of overcrowded health care systems, statistics from other countries have shown a reduction in ED patient volume during the COVID-19 pandemic.[4,5] The patterns of ED visits have also changed significantly during the pandemic season, with decreased ED visits in non-COVID-19 diseases, and an increased visit rates of out-of-hospital cardiac arrests, probably due to delay in seeking medical attention.[6] However, the impact of the altered trend of ED visiting patients on ED physician workload and ED medical resources arrangement were less understood.
We therefore conducted this study to evaluate the impact of the COVID-19 pandemic on the number of ED visiting patients, mode of arrival, triage level, disposition, time of visit, mode of arrival, and chief complaints, which may benefit in allocating medical resources effectively to the most needed departments, and reduce the possibility of overcrowding in the healthcare system during the pandemic.
2. Methods
2.1. Study setting
This was a retrospective study conducted in the hospitals of the Cathay Health System, including a medical center, a regional hospital, and a district hospital in northern Taiwan. One of the study hospitals is an urban medical center with an 800-bed capacity and an estimated total annual ED visit volume of 60,000. The other 2 included hospitals are both located in rural areas with capacities of 642-bed and 348-bed. The estimated annual ED visiting volumes were 48,000 and 30,000. Patients visiting the ED of these 3 hospitals between January 21, 2020 to April 30, 2020 and January 21, 2019 to April 30, 2019 will be recruited.
2.2. Study design
Patient information will be extracted from the electronic medical record (EMR) system and further divided into the “during pandemic” group, January 21, 2020 to April 30, 2020; and the “before pandemic” group, January 21, 2019 to April 30, 2019. The pandemic period was set up by the first confirmed case in Taiwan on January 21, 2020 and ended on April 30, 2020, which was the 4th day after no confirmed cases for 3 consecutive days. All patients, including children and adults who presented to the EDs, were considered eligible for recruitment between the 2 periods. Missing or duplicated data were excluded to ensure the integrity of the information.
2.3. Variables
Basic demographics, including visit characteristics, disposition, and chief complaints of the patients visiting the ED during these 2 periods of time, will be obtained. Visiting characteristics consisted of total daily visits, mode of arrival, and time of visit; chief complaints were based on patients’ narratives recorded on the EMR and sorted into 33 common discomforts. Patients were triaged to different sections based on a combination of the Canadian Triage and Acuity Scale and clinical criteria. All triage nurses received formal training and had more than 1-year of ED working experience.
2.4. Ethical statement
The present study was approved by the Institutional Review Board of Cathay General Hospital and was conducted following the Declaration of Helsinki. The need for informed consent from the patients was waived, as this was an observational study.
2.5. Statistical analysis
Our data were analyzed using IBM SPSS Statistics for Windows (version 25.0). Categorical variables were presented as numbers and percentages, while normally distributed continuous variables were presented as mean ± standard deviation. The chi-square test was used to analyze the categorical variables, and an independent t-test was used to analyze the normally distributed continuous variables. Incidence rates were calculated as the number of results of interest divided by the total number of ED visits in each period. Incidence rates were presented as the frequency of the results per 100 ED visits. We also calculated the percentage difference in the number of chief complaints between the “before pandemic” period and the “during pandemic” period.
3. Result
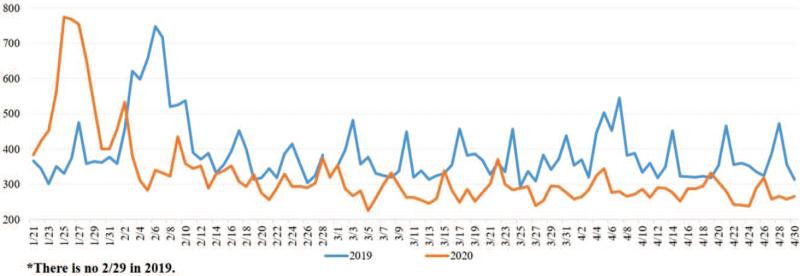
A total of 71,739 patients were included in this study. There were 38,789 ED visits before the pandemic period between January 21, 2019 and April 30, 2019; a reduction in ED visits was noted for 15.1% (32,950 ED visits) during the pandemic period (Fig. 1). The sex ratio showed a female percentage of 52.6% and 51.5%, both before and during the pandemic period, which was significantly higher than the male percentage of 47.4% and 48.5%, respectively (Table 1).
Figure 1.
Comparison of total ED volume between the 2 periods.
Table 1.
Comparisons of demographic characteristics of ED visits between the 2 time periods.
| Characteristics | Before pandemic (January 2019–April 2019) (N = 38,789) | During pandemic (January 2020–April 2020) (N = 32,950) | Difference (%) | P-value |
| Total visits/day – no. (SD) | 387.89 (86.07) | 326.30 (103.94) | −15.88 | <.001 |
| Age – no. (%) | ||||
| Age < 18 | 6009 (15.5) | 4107 (12.5) | −31.65 | <.001 |
| 18 ≤ Age < 65 | 23,480 (60.5) | 21,488 (65.2) | −8.48 | |
| Age ≥ 65 | 9300 (24.0) | 7355 (22.3) | −20.91 | |
| Sex – no. (%) | ||||
| Male | 18,373 (47.4) | 15,987 (48.5) | −12.99 | .002 |
| Female | 20,416 (52.6) | 16,963 (51.5) | −16.91 | |
| Mode of arrival∗ – no. (%) | ||||
| Walk-in | 28,035 (75.6) | 24,224 (76.9) | −13.59 | <.001 |
| Wheelchair | 3727 (10.1) | 2932 (9.3) | −21.33 | |
| Ambulance | 3771 (10.2) | 3398 (10.8) | −9.89 | |
| Being held | 1533 (4.1) | 956 (3.0) | −37.64 | |
| Triage – no. (%) | ||||
| Triage 1 | 812 (2.1) | 723 (2.2) | −10.96 | <.001 |
| Triage 2 | 5299 (13.7) | 4228 (12.8) | −20.21 | |
| Triage 3 | 29,308 (75.6) | 24,502 (74.4) | −16.40 | |
| Triage 4 | 3036 (7.8) | 3137 (9.5) | 3.33 | |
| Triage 5 | 334 (0.9) | 360 (1.1) | 7.78 | |
| Disposition – no. (%) | ||||
| Admission | 5434 (14.0) | 4444 (13.5) | −18.22 | <.001 |
| Discharge | 32,279 (83.2) | 27,687 (84.0) | −14.23 | |
| AMA | 784 (2.0) | 540 (1.6) | −31.12 | |
| Transfer | 185 (0.5) | 146 (0.4) | −21.08 | |
| Mortality | 107 (0.3) | 133 (0.4) | 24.30 | |
| Time of visit – no. (%) | ||||
| Early morning (00.00–08.00) | 7307 (18.8) | 5680 (17.2) | −22.25 | <.001 |
| Day time (08.00–17.00) | 16,697 (43.0) | 14,947 (45.4) | −10.46 | |
| Nighttime (17.00–24.00) | 14,785 (38.1) | 12,323 (37.4) | −16.65 | |
AMA = against medical advice, SD = standard deviation.
Some records missed the mode of arrival.
The mean daily ED visiting patients decreased prominently from 387.89 ± 86.07 patients per day (before the pandemic) to 326.30 ± 103.94 patients per day (during the pandemic period). Compared to the 15.5% pediatric (age < 18) and 24.0% elderly (age ≥ 65) ED visiting patients before the pandemic period, significant reductions in pediatric and elderly ED visiting patients were noted for 12.5% and 22.3%, respectively, during the pandemic period. The usage of the emergency medical services (EMS) system (ambulance) slightly increased during the pandemic period by 10.8%, compared to 10.2% before the pandemic period. A higher percentage of triage level 4 and 5 patients were seen in the pandemic period for 9.5% and 1.1%, and 7.8% and 0.9%, respectively, before the pandemic period. More patients (84.0%) were discharged during the pandemic period than before the pandemic period (83.2%) (Table 1).
Generally, most ED visiting chief complaints decreased during the pandemic period, compared to the prepandemic period. However, ED visiting patients with the chief complaints of upper respiratory infection and social problems increased by 14.23% (P-value < .01) and 1.86% (P-value = .12), respectively, during the pandemic period. Critical chief complaints, such as chest pain and altered mental status decreased to less than the ED visits difference between pandemic and prepandemic (15.1%) for −7.67% (P-value < .01) and −13.08% (P-value = .34) respectively. Meanwhile, combined the number of patients transferred from OPD, LMD, and hospitals, the percentage decreased by 7.84% compared to the prepandemic period (Table 2).
Table 2.
Chief complaints of total ED visits between periods.
| Chief Complaints | Before pandemic (January 2019–April 2019) (N = 38,789) | During pandemic (January 2020–April 2020) (N = 32,950) | Difference (%) | P-value | ||
| N | Incidence | N | Incidence | |||
| Fever | 5762 | 14.85 | 5696 | 17.29 | −1.14 | <.01 |
| URI | 4220 | 10.88 | 4823 | 14.63 | 14.23 | <.01 |
| Cellulitis | 717 | 1.85 | 570 | 1.73 | −20.50 | .44 |
| Abdominal pain | 5497 | 14.17 | 4421 | 13.42 | −19.57 | .49 |
| AGE symptoms | 4715 | 12.16 | 2448 | 7.43 | −48.05 | <.01 |
| Constipation | 172 | 0.44 | 95 | 0.29 | −44.77 | <.01 |
| GIB symptoms | 451 | 1.17 | 314 | 0.95 | −30.38 | <.01 |
| Colorectal problems | 63 | 0.16 | 58 | 0.18 | −7.94 | .26 |
| Chest pain | 1916 | 4.94 | 1769 | 5.37 | −7.67 | <.01 |
| Hypertension | 422 | 1.09 | 219 | 0.66 | −48.10 | <.01 |
| Shortness of breath | 1758 | 4.53 | 1472 | 4.47 | −16.27 | .18 |
| Dizziness | 2585 | 6.67 | 1559 | 4.73 | −39.69 | <.01 |
| Headache | 1140 | 2.94 | 613 | 1.86 | −46.23 | <.01 |
| Convulsion | 160 | 0.41 | 122 | 0.37 | −23.75 | .54 |
| Stroke symptoms | 293 | 0.76 | 247 | 0.75 | −15.70 | .77 |
| Altered mental status | 367 | 0.95 | 319 | 0.97 | −13.08 | .34 |
| Malaise | 432 | 1.11 | 272 | 0.83 | −37.04 | <.01 |
| Myalgia | 2185 | 5.63 | 1524 | 4.63 | −30.25 | <.01 |
| Glycemic problems | 186 | 0.48 | 148 | 0.45 | −20.43 | .96 |
| Urological symptoms | 1152 | 2.97 | 882 | 2.68 | −23.44 | .49 |
| Medical tube, probe, and catheter problems | 641 | 1.65 | 478 | 1.45 | −25.43 | .42 |
| Trauma | 8641 | 22.28 | 7326 | 22.23 | −15.22 | <.01 |
| Facial feature problems∗ | 1009 | 2.60 | 686 | 2.08 | −32.01 | <.01 |
| OBS-GYN related problems | 748 | 1.93 | 671 | 2.04 | −10.29 | <.01 |
| Dermatology problems | 1017 | 2.62 | 658 | 2.00 | −35.30 | <.01 |
| Cardiac arrest | 126 | 0.32 | 126 | 0.38 | 0 | .16 |
| Transfer from OPD and LMD | 386 | 1.00 | 251 | 0.76 | −34.97 | <.01 |
| Transfer from hospital | 990 | 2.55 | 1017 | 3.09 | 2.73 | <.01 |
| Psychological problems | 268 | 0.69 | 235 | 0.71 | −12.31 | .38 |
| Social problems† | 161 | 0.42 | 164 | 0.50 | 1.86 | .12 |
| Ask for screening | / | / | 84 | 0.25 | / | |
| Suggest screening by TCDC | / | / | 115 | 0.35 | / | |
| Others | 308 | 0.79 | 190 | 0.58 | −38.31 | <.01 |
N represents the raw number of cases in each period. Incidence is the number of results of interest divided by the total ED visits in each period, reported as the frequency of the outcome per 100 ED visits. The difference compares the raw number of cases between the before and during pandemic periods, presented as percentages.
AGE = acute gastroenteritis, GIB = gastrointestinal bleeding, LMD = local medical department, OBS-GYN = obstetrics-gynecology, OPD = outpatient department, TCDC = Taiwan Centers for Disease Control, URI = upper respiratory infection.
Facial feature problems, including eyes, ear, nose, and throat and dental problems.
Social problems include family violence and sexual assault.
4. Discussion
Recent studies have shown a significant reduction in ED visits during the first few weeks of the pandemic.[7] Similarly, we found a substantial decrease in total ED visits in all Cathay Health System hospitals during the pandemic period. Several factors, including social distancing policies, school closures, and media influence, may decline total ED visits.[8,9] This circumstance was especially observed among the vulnerable populations: pediatric and older patients, as parents and caregivers were reluctant to bring their children or elderlies to the hospitals in fear of being infected by COVID-19 during the ED visit. Rearrangement of the pediatric department staff to the COVID-19 special units may be performed to properly utilize medical resources during the pandemic.
According to our research, increased ED arrival via ambulance was noted during the pandemic period. A study of EMS showed that the COVID-19 pandemic was associated with negative collateral health effects; however, they found no evidence that people were reluctant to call an ambulance when they experienced critical symptoms, such as stroke or heart attack.[11] Similarly, in the present study, the proportion of patients who were triaged as level 1 slightly increased during the pandemic stage compared to the prepandemic stage. Furthermore, no difference was noted over the ED visiting chief complaint of cardiac arrest before and during the pandemic. This indicates that people would still visit the ED by activating the EMS, if necessary.
According to the chief complaints of total ED visits between the 2 periods: Firstly, it is ambiguous to conclude that the lower general ED visits observed in our study resulted from the actual low incidence of illness, injury, or care shifted to other local medical clinics. However, a significant reduction of 15.2% (P-value < .01) in trauma patients was noted in our study. This indicates less social events and less traffic mobility during the pandemic period, either due to social distance or school closure policies. A study in Spain discovered a significant decrease in the number of accidents by 74.3% during the pandemic period, compared to the prepandemic period. This study further concluded that the reduction in mobility may result in a decline in accidents and injuries.[9]
Secondly, as the classic presentation of COVID-19 is upper respiratory tract infection symptoms, such as fever, sore throat, fatigue, cough, or dyspnea,[1] ED visiting patients with the chief complaint of upper respiratory tract infection increased dramatically during the pandemic period, probably because of the fear of being infected by the COVID-19 virus[10]. These circumstances also increase the number of patients with low triage acuity levels of 4 or 5 during the pandemic period. Similarly, we also observed a significant decline in the percentages of less urgent and non-COVID-19 related ED visiting chief complaints, such as hypertension, acute gastroenteritis, constipation, and dizziness, which were noted for 48.10%, 48.05%, 44.77%, and 39.69% during the pandemic stage, compared to the prepandemic period.
Thirdly, reductions in the percentages of substantially higher urgency ED visiting chief complaints (less than the ED visits difference between pandemic and prepandemic of 15.1%), such as altered mental status (−13.08%, P-value < .34) and chest pain (−7.67%, P-value < .01), were also observed during the pandemic stage. These circumstances may be related to the lockdown policies and less social activities during the pandemic, which could further consequence in less trigger factors of vascular diseases, including physical activity, air pollution, or work-related stress.[12]
Finally, although not significant, an increased proportion of social problems was noted during the pandemic, compared to the prepandemic period in the current study. A similar result was noted in a study conducted in China, which reported that the prevalence of psychological and social problems had increased during the COVID-19 pandemic. A possible reason was assumed to be related to frequent social medical exposure.[13] Meanwhile, the “stay at home” policy during the pandemic period may lead to an increase in domestic violence, as the home is often an unsafe place for these victims.[14] Therefore, more social workers should be recruited to the ED to respond to such circumstances.
Our study has several limitations. First, this was a retrospective study that utilized the EMR system between 2019 and 2020. Hence, some important data could not be obtained. Second, although 3 different hospitals were included in this study, all hospitals were located in northern Taiwan, and further study is needed to validate our results. Finally, individual bias may occur in different triage nurses while triaging patients, although all triage nurses are required to receive formal triage training.
5. Conclusion
A significant decline in the number of pediatric ED visits and an increasing proportion of social problem visits were observed during the COVID-19 pandemic. According to the results of this study, rearrangement of the ED pediatric staff to the COVID-19 special units and recruiting more social workers to the ED should be performed to respond to the COVID-19 pandemic.
Author contributions
JYC and CCH designed the study; YWL, CTH, YTL, and JYC wrote the manuscript. JYC performed statistical analyses. The JHC, WLC, and CCH provided professional suggestions. All authors have read and approved the final manuscript.
Conceptualization: Chien-Cheng Huang, Jui-Yuan Chung.
Methodology: Jui-Yuan Chung.
Supervision: Wei-Lung Chen, Jiann-Hwa Chen, Chien-Cheng Huang.
Writing – original draft: Yen-Wen Lai, Ching-Tang Hsu, Yu-Ting Lee.
Writing – review & editing: Jui-Yuan Chung.
Footnotes
Abbreviations: COVID-19 = coronavirus disease 2019, ED = emergency department, EMR = electronic medical record, EMS = emergency medical services.
How to cite this article: Lai YW, Hsu CT, Lee YT, Chen WL, Chen JH, Huang CC, Chung JY. Analysis of COVID-19 pandemic impact on the presenting complaints of the emergency department visits. Medicine. 2021;100:51(e28406).
This work was supported by the Cathay General Hospital (Grant number CGH-MR-B10912).
The study was approved by the Institutional Review Board of Cathay General Hospital. Because this was an observational study, the need for informed consent from patients was waived.
Consent for publication is not applicable.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Zhai P, Ding Y, Wu X, Long J, Zhong Y, Li Y. The epidemiology, diagnosis, and treatment of COVID-19. Int J Antimicrob Agents 2020;55:105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bjørnsen LP, Næss-Pleym LE, Dale J, Laugsand LE. Patient visits to an emergency department in anticipation of the COVID-19 pandemic. Tidsskr Nor Laegeforen 2020;140:08. [DOI] [PubMed] [Google Scholar]
- [3].Guo H, Zhou Y, Liu X, Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci 2020;15:564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].COVID-19 Webinar 1: a Unique Insight in Highly Impacted Countries. EUSEM Academy. & Said Laribi L. March 28, 2020. 290502. Available at: https://academy.eusem.org/eusem/2020/covid-19/document?c_id=290502&cm_id=307059&type=document307059. Accessed March 28, 2020. [Google Scholar]
- [5].Lo HY, Chaou CH, Chang YC, Ng CJ, Chen SY. Prediction of emergency department volume and severity during a novel virus pandemic: Experience from the COVID-19 pandemic. Am J Emerg Med 2020;303–9. doi: 10.1016/j.ajem.2020.07.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Baugh JJ, White BA, McEvoy D, et al. The cases not seen: patterns of emergency department visits and procedures in the era of COVID-19. Am J Emerg Med 2020;476–81. doi: 10.1016/j.ajem.2020.10.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020;4:05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Pines JM, Zocchi MS, Black BS, et al. US Acute Care Solutions Research Group. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med 2021;41:201–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Saladié O, Bustamante E, Gutiérrez A. COVID-19 lockdown and reduction of traffic accidents in Tarragona province, Spain. Transp Res Interdiscip Perspect 2020;8:100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Holmes JL, Brake S, Docherty M, Lilford R, Watson S. Emergency ambulance services for heart attack and stroke during UK's COVID-19 lockdown. Lancet 2020;395:e93–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Danchin N, Marijon E. COVID-19 pandemic: preventing hospital myocardial infarction admissions or preventing acute myocardial infarction altogether? Heart 2021;107: doi: 10.1136/heartjnl-2020-318646. [DOI] [PubMed] [Google Scholar]
- [12].Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 2020;15:e0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Anurudran A, Yared L, Comrie C, Harrison K, Burke T. Domestic violence amid COVID-19. Int J Gynaecol Obstet 2020;150:255–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med 2020;76:595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]