Abstract
The COVID-19 vaccine has become a strategic vehicle for reducing the spread of the pandemic. However, the uptake of the vaccine by the public is more complicated than simply making it available. Based on social learning theory, this study examines the role of communication sources and institutional trust as barriers and incentives as motivators of people’s attitudes toward vaccination and actual vaccination. Data were collected via an online panel survey among Israelis aged 18–55 and then analyzed using structural equation modeling (SEM). Findings show that social media trust negatively mediates the effect of exposure to information on the vaccine on attitudes toward vaccination. However, mass media trust and institutional trust positively mediate this relationship. Incentives were effective motivators for forming positive attitudes and moderating the effect of institutional trust on attitude toward vaccination. This study facilitates a deeper understanding of health communication theory in pandemics and makes important recommendations for practitioners and policy makers.
Keywords: COVID-19, pandemic, vaccination, media trust, institutional trust, incentives
1. Introduction
In December 2020, the American FDA approved the first COVID-19 vaccine, and it has become a major strategic vehicle for diminishing the spread of the pandemic. The clear expectation of widespread global vaccination was premised on the assumption that the public would be willing to receive it if offered. However, this premise was shown to be unfounded [1], and a public health battle emerged between governments and anti-vaccination movements [2]. The public was confronted by misguided information and fake news, mainly through social media, which undermined their decision making and increased their hesitation regarding the vaccine. Consequently, COVID-19 vaccine uptake promotion campaigns were inevitable [2]. The confrontation with COVID-19 vaccine refusals intensified the importance of understanding the barriers and motivators of public vaccination and how formal and informal institutions can effectively communicate with the public about it [1]. Credible communication can reach a collective consciousness and establish attitudes and beliefs that can affect the willingness to receive the vaccine [3].
The current study aims to focus on communication barriers such as trust in communication sources and governmental institutions and motivators such as government incentives and examine their role in enhancing public willingness to be vaccinated during times of pandemic. Although there is extensive research regarding individual motivation, attitude, and concern for vaccination acceptance and refusal [4,5], the unique context of the rapid development of the COVID-19 vaccination, the worldwide pandemic, and the varied global political realities might result in different findings [6]. Additionally, recent studies in health communication regarding the COVID-19 pandemic have focused on individual health beliefs [7], individual personality [8], and perspectives or religious beliefs [9]. However, although there is a need for a deeper understanding of the effect of individual exposure to information about vaccination and what motivates or discourages a favorable decision to be vaccinated, the research on these subjects is still scarce. Therefore, based on social learning theory [10], the current study offers a conceptual framework that integrates exposure to information on vaccination with key mediating factors—believability of information sources and institutional trust—to explain attitudes toward vaccination and actual vaccination.
The contribution of the current research lies in offering a unique conceptual framework contributing to health communication literature. Specifically, it highlights the effect of trust and incentives on the learning process and consequent behavior, corresponding with the social learning theory and the health belief model. Moreover, this framework further contributes to governments and policy makers who need to have more understanding of how to communicate effectively with the public and convince them to be vaccinated during times of pandemic, overcoming the misinformation in the media and individuals’ misinformed beliefs.
1.1. Social Learning Theory and Exposure to Vaccine Information
During a pandemic, public exposure to health communication disseminated from diverse sources forms attitudes toward the communicated message and consequential behavior [11]. The response to intimidating information about the pandemic and recommendations for preventive actions highly depends on individuals’ exposure to trustworthy information sources [12]. To theoretically frame this perspective, the current study applies social learning theory (also referred to as social cognitive theory) [10,13,14], a well-established theory derived from psychology and education research [15,16,17]. It was later extended to media research dealing with the effect of media on individuals and is also part of the health belief model used to explain the adoption of preventative health behaviors [18]. Social learning theory asserts that human behavior is governed by a triadic determinism: social environment, cognitive abilities, and behavior. These three factors maintain an ongoing interaction and affect one another. The primary source of information is the social environment, including media messages, upon which the individual establishes his cognitive perceptions of the world, beliefs, expectations, and self-perception.
Next, a person uses his cognitive abilities to process the inputs he receives from the environment, develop expectations, and decide how to act. His behavior affects the environment and changes it. The changed environment provides new information to the cognitive system. Hence, social learning theory employs a basic approach that media exposure plays a vital role in social learning, demonstrating the effect of exposure to media on attitude formation and behavior. Previous research presented the relation between social learning and visual culture [19], and the effect of social learning in social commerce sites, forums, and online communities on consumer decision making and purchase intentions [20]. In the context of a pandemic, research demonstrated how exposure to information in mass media plays an essential role in addressing misinformation and changing beliefs about the source, modes of infection and prevention of the Ebola pandemic [15]. Based on this theory, it is suggested that people’s exposure to the social environment formed by traditional and social media (distributing information about the vaccine) will affect individuals’ cognitive perceptions manifested in their attitude toward vaccination. Accordingly, a positive attitude toward vaccination will be followed by a decision to act. Therefore, the following hypotheses:
Hypothesis 1 (H1).
Level of exposure to media communication regarding the COVID-19 vaccination directly affects attitudes toward vaccination.
Hypothesis 2 (H2).
Attitude toward COVID-19 vaccination is positively related to actual vaccination.
Social learning theory and the stimulus–organism–response (SOR) paradigm posit that the effect of environmental cues (the stimuli), such as exposure to information about the COVID-19 vaccine in the media on individual attitudes and behavior, is mediated by the individual’s (organism) internal state, including cognitive judgments and affective response aroused by environmental cues. These perspectives suggest that the response to exposure to information from media sources is also affected by evaluation of the media environment. Qiao et al. [21] found that while consumers use multiple sources for information about the COVID-19 vaccine, their vaccine acceptance is dependent on the level of trust in these information sources. Additionally, research indicates a possible change in trust generated by media exposure. For example, exposure to specific media content may cause affective disposition toward the content which creates an indirect positive effect on media trust [22], while consumption of misinformation is associated with a general decrease in media trust [23]. Bearing in mind the above discussion, we consider trust as an internal state of the organism (the individual) which is activated during exposure to information from media sources.
1.2. Trust in Information Sources and Attitude toward Vaccination
Trust has been an essential factor between two parties who wish to exchange values and ideas. The success of the exchange process builds trust and supports the relationship between the main actors [24], and is a vital element for the optimal function of the society [25]. Previous research has shown that trust in information sources is an important aspect of information-seeking behavior during crises [26,27]. Individuals’ trust in the institutions providing the information, such as media institutions and government agencies, affects their vaccination intentions and behavior [27].
1.2.1. Trust in the Media
People are exposed to information about COVID-19 vaccination from two primary sources: mass media sources (such as news on T.V., newspapers, and radio) and social networks, incorporating information created by people we know or follow online [7,28]. Previous research has demonstrated that an individual’s trust and credibility perception vary by information source [28,29,30].
Trust is defined as one’s confidence in the information channels to provide accurate, fair, trustworthy, and unbiased information [22]. This perception of trusted sources delivering information is an essential aspect of people’s willingness to adopt the information [31]. Thus, vaccination attitude might be affected by the trust in the validity of the information provided by the government and the media, which largely disseminate this information [27].
1.2.2. Social Media Sources and Trust
Social media sources such as Facebook and Twitter play a significant role in facilitating the exchange of relevant information during an epidemic [32,33]. The widespread public adoption of social media platforms as a tool for information seeking has led to a flood of misinformation about COVID-19 and false narratives relating to the vaccine [1,34]. Moreover, conspiracy theories have flourished due to the lack of censorship on social media platforms [35]. However, recommendations from family and friends on social media platforms may carry more weight than those from government officials or other spokespeople. Social media plays an important role in vaccination decision making [1]. Individuals tend to trust the accuracy of information when it comes from others with whom they perceive to share similar interests [36,37]. Hence, individuals’ shared interests on social media may function as a heuristic for trustworthiness [36], which contributes to the persuasive effect of the communication [38].
Previous research demonstrates that information originating on social media sites and created by other users affects individuals’ attitudes toward vaccination behaviors. These attitudes can lead to a pro-vaccination stance and are driven by the receiver perceptions of information credibility [34,38]. Moreover, Turcotte et al. [39] conclude that “Social recommendations from people perceived as quality opinion leaders led to an increase in outlet trust… These results extended beyond trusting a news outlet to indicators of future behavior”. This implies that trust further mediates the effect of exposure on attitude and behavior. Therefore
Hypothesis 3a (H3a).
Social media trust positively affects attitudes toward vaccination.
Hypothesis 3b (H3b).
The relationship between the exposure to vaccine information and attitude toward vaccination is mediated by social media trust.
1.2.3. Mass Media and Trust
Mass media is an essential source of information and still plays a significant role in influencing health-related outcomes [40]. A recent study revealed that most U.S. citizens (86%) use mass media to obtain information on the COVID-19 vaccine, as these sources are perceived as high-quality for sharing fact-based vaccine information linked to governmental, healthcare, or academic data and reports [27,28]. Moreover, obtaining information from mass media increased vaccination acceptance [28].
Trust is considered a crucial variable for mass media effects [41]. Prior research has revealed that people’s trust in mass media affects their tendency to follow preventive health suggestions from this source [27]. Niu et al. [7] found that T.V. trust was significantly associated with preventive behaviors during the COVID-19 outbreak. Moreover, individuals’ attitudes toward vaccination were related to their trust in the accuracy of information provided by the media [27]. The importance of media trust was particularly notable concerning vaccination attitudes. Recent research on college students found that although they were exposed to variety of media, the level of trust in these media sources influenced their vaccine acceptance [21]. These studies further suggest that after media exposure there is a possible effect of information evaluation (i.e., trust) on attitude formation. Hence, our hypotheses:
Hypothesis 4a (H4a).
Mass media trust positively affects attitude toward vaccination.
Hypothesis 4b (H4b).
The relationship between the exposure to vaccine information and attitude toward vaccination is mediated by mass media trust.
1.2.4. Institutional Trust
Institutional trust is used to describe citizens’ trust in actors such as governmental organizations [25]. It was found that institutional trust is a distal factor influencing individuals’ vaccination hesitancy and is part of evolving conspiracy theories emphasizing distrust of government organizations [4,34,42].
Institutional trust is an underlying factor in the effectiveness of the democratic process. It is based on citizens’ prior experience and familiarity with information about these institutions’ fair (or unfair) conduct [43]. Thus, institutional trust is based on prior knowledge about the trustworthiness of the concerned institutions. Furthermore, studies on institutional trust claim that media exposure is related to institutional trust since most of the information about the past behavior of governmental institutions originates from media sources [44]. Moreover, research on exposure to vaccine-related information reveals that while trust in information about the vaccine is positively related to attitudes and behaviors, it is not enough when associated institutions are mistrusted [45,46].
Additionally, previous research demonstrates that mistrust is a more common reason for negative attitudes toward vaccination than lack of information [47]. For instance, Vinck et al. [48] found that low institutional trust was highly associated with negative attitudes toward acceptance of Ebola vaccines, while Borah and Hwang (2021) found that trust in doctors’ vaccine recommendations positively mediates between doctor-patient communication and vaccination attitudes [47]. Thus, our hypotheses are:
Hypothesis 5a (H5a).
Institutional trust positively affects attitudes toward vaccination.
Hypothesis 5b (H5b).
The relationship between the exposure to vaccine information and attitude toward vaccination is mediated by institutional trust.
1.3. Incentives
Incentives are defined as “any action taken by the authorities that may lead to an increase in the level of vaccination coverage” [48]. This implies that there is a need for a change in citizen attitudes toward the vaccine and/or toward the action of being vaccinated which may be changed by offering some encouragement. For instance, where citizens’ hesitancy about the COVID-19 vaccine was found to inhibit the uptake of COVID-19 vaccination in the Israeli population, the government and local authorities started offering various incentives. The incentives varied from small gifts to granting a ‘green pass’, which allows citizens to participate in cultural events, eat in restaurants, stay at hotels, etc. [49]. The vaccine was also made accessible in town centers and public buildings rather than in health centers [50].
Previous research indicates that incentives affect consumer health care choices. Specifically, it was found that incentives raise the level of citizens’ consent to be vaccinated [51,52]. Thus:
Hypothesis 6 (H6).
Incentives positively affects attitude toward vaccination.
It has already been shown that coercive policies, which are the opposite of incentives, can damage trust in vaccination operations, while incentives may help in promoting vaccinations when trust in institutions is low [53,54]. While coercive policies are perceived as an ‘illiberal’ approach that strengthens the vaccination resistance, incentives create the notion of autonomy and voluntariness [55]. Recent research performed among American and Canadian adults during the COVID-19 pandemic found that respondents with a negative attitude toward being vaccinated were more affected by information about the vaccine safety as an incentive (38%) than financial incentives (18%), permission to attend the workplace (31%), coupons or discounts (8%) or tickets to sports events (19%) [56]. Though these respondents are motivated mainly by mistrust in the institutions promoting the vaccine, other incentives motivate individuals with low institutional trust to get vaccinated. In other words, the incentive becomes a motivating factor for a positive attitude toward vaccination in cases where there is less trust in the institutions that promote and support the vaccine.
Hypothesis 7 (H7).
Incentives negatively moderate the effect between institutional trust and attitude toward vaccination.
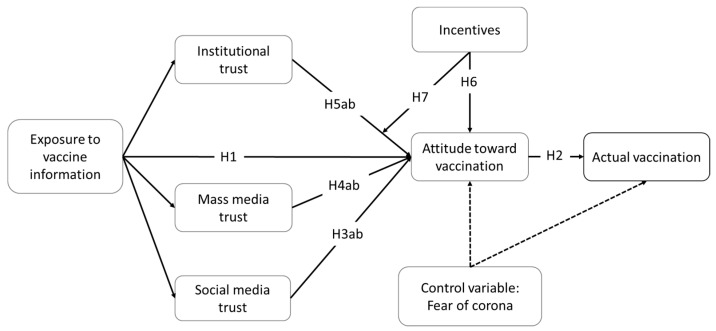
The conceptual framework is shown in Figure 1.
Figure 1.
The conceptual framework.
2. Materials and Methods
2.1. Data Collection and Sample
To test the hypotheses empirically, data were collected via a self-administered questionnaire. Israeli participants were randomly recruited via an online panel survey company, Blueberries. The university’s ethics committee where this study was conducted has confirmed that this study meets the conditions set out in the procedure for approving a study that is not a clinical trial in humans. All respondents were assured of confidentiality, and consent was obtained from all participants before the questionnaire. The questionnaires were coded for anonymous data analysis.
The unique advanced stage of Israel’s vaccination situation made Israel a valuable case study for vaccination behavior and attitudes. At the time of data collection, a high percentage of Israelis were already vaccinated against COVID-19 (especially among high-risk groups), the vaccine supply was higher than the demand, and Israel authorities were highly active with an extensive vaccination media campaign. The chosen population was restricted to adults of age 18–55. The group of people age 55+ were excluded since the majority of them were already vaccinated and contribute less to the research purpose.
Overall, 863 respondents entered the survey. Respondents who did not belong to the chosen population were screened out at the beginning of the questionnaire and did not participate in the survey. The final sample included 484 usable responses. In this sample, participants were 57% females and 43% males. The age of participants ranged from 18 to 55 years (M = 36.6, SD = 10.6). Most of the participants had an average or below-average income (69%) and post-secondary education (76%). Among them, 41% were vaccinated against the COVID-19, 19% had natural immunity due to COVID-19 infection, and 5% stated that a physician prohibited their vaccination.
2.2. Variable Measurement
The survey questionnaire scales consisted of items primarily gathered from previously validated studies, while a few specific new ones were designed for the current study (see Table 1). Where necessary, the scale items were modified to capture vaccination orientation. Actual vaccination was measured by a single item expressing participants’ actual vaccination. In this measure, respondents were asked to answer yes/no to the question: “I was vaccinated against COVID-19 at least once”. Items for attitude toward vaccination were taken from Fu et al. [57]. Mass media trust and Social media scales were taken from Peifer [22]. Institutional trust items are original and adjusted for the current study based on Ervasti et al. [25]. Similarly, the items for effect of incentives are original and designed for the current study. Here, respondents were asked to indicate their level of agreement with different statements, on a seven-point Likert scale, ranging from 1 = strongly disagree, to 7 = strongly agree. Items for exposure to vaccine information are adjusted for this study and based on Venkatesh et al. [58] and Kol et al.’s [31] orientation. Respondents were asked to indicate their level of exposure to different information sources on a seven-point Likert scale, ranging from 1 = not exposed at all, to 7 = highly exposed.
Table 1.
CFA—Item Factor Loading and Variable Reliability and Validity Measures.
| Variables and Items | Std. Coef. | AVE | CR | Cronbach’s Alpha |
|---|---|---|---|---|
| Attitude toward vaccination | 0.81 | 0.93 | 0.92 | |
|
0.83 ** | |||
|
0.95 ** | |||
|
0.92 ** | |||
| Mass media trust | 0.88 | 0.97 | 0.97 | |
|
0.96 ** | |||
|
0.96 ** | |||
|
0.96 ** | |||
|
0.87 ** | |||
| Social media trust | 0.84 | 0.95 | 0.95 | |
|
0.95 ** | |||
|
0.93 ** | |||
|
0.94 ** | |||
|
0.84 ** | |||
| Institutional trust | 0.56 | 0.90 | 0.89 | |
|
0.55 ** | |||
|
0.72 ** | |||
|
0.71 ** | |||
|
0.78 ** | |||
|
0.83 ** | |||
|
0.85 ** | |||
|
0.77 ** | |||
| Exposure to vaccine information | 0.51 | 0.80 | 0.75 | |
|
0.74 ** | |||
|
0.56 ** | |||
|
0.70 ** | |||
|
0.82 ** | |||
| Incentives | 0.46 | 0.72 | 0.67 | |
|
0.57 ** | |||
|
0.73 ** | |||
|
0.73 ** | |||
| Fear of pandemic | 0.71 | 0.88 | 0.87 | |
|
0.79 ** | |||
|
0.92 ** | |||
|
0.82 ** |
** Standardized coefficients, p < 0.01; AVE = average variance extracted; CR = composite reliability.
An additional variable was added as a control variable. Fear of pandemic was added to control for the extrinsic effect of fear during the pandemic, which can be an excuse for the people’s attitude toward vaccination and actual vaccination. The scale was adopted from Tran [59]. Here, respondents were asked to indicate their level of agreement with different statements on a seven-point Likert scale, ranging from 1 = strongly disagree, to 7 = strongly agree. Demographic variables were also gathered.
3. Results
3.1. Validity and Reliability
First, to ensure that no Common Method Bias (CMB) exists in variance, Harman’s one-factor test was used, and a single factor accounted for just 31.77 of the (total) variance, indicated that bias is no serious concern of CMB.
Next, for validity concern, a confirmatory factor analysis (CFA) was executed. An acceptable fit was found in all measurements (χ2 value (319) = 778.08, p < 0.001 (χ2/df < 3); Comparative Fit Index (CFI) = 0.956; Normed Fit Index (NFI) = 0.929; and Root Mean Square Error of Approximation (RMSEA) = 0.055). The standardized regression estimate for each factor was above 0.50, displaying acceptable fit of the measures. Table 1 displays the convergent validity and reliability measures (average variance extracted (AVE), composite reliability (CR) and Cronbach’s alpha) and Table 2 presents correlation pattern between variables and the maximum shared squared variance (MSV) indicating discriminant validity of all constructs.
Table 2.
Correlations a between Variables and the maximum shared squared variance (MSV).
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Actual vaccination | – | 0.418 ** | 0.187 ** | −0.035 | 0.138 ** | 0.089 | 0.174 ** | 0.083 |
| 2. Attitude toward vaccination | 0.511 | 0.81 | 0.418 ** | 0.084 | 0.392 ** | 0.166 ** | 0.444 ** | 0.382 ** |
| 3. Mass media trust | 0.090 | 0.175 | 0.88 | 0.525 ** | 0.552 ** | 0.187 ** | 0.300 ** | 0.219 ** |
| 4. Social media trust | 0.001 | 0.007 | 0.276 | 0.84 | 0.335 ** | 0.161 ** | 0.180 ** | 0.090 * |
| 5. Institutional trust | 0.075 | 0.154 | 0.305 | 0.112 | 0.56 | 0.191 ** | 0.256 ** | 0.300 ** |
| 6. Exposure to vaccine inform. | 0.020 | 0.028 | 0.035 | 0.026 | 0.036 | 0.52 | 0.150 ** | 0.238 ** |
| 7. Incentives | 0.120 | 0.197 | 0.090 | 0.032 | 0.066 | 0.023 | 0.46 | 0.137 ** |
| 8. Fear of pandemic | 0.084 | 0.146 | 0.048 | 0.008 | 0.090 | 0.057 | 0.019 | 0.71 |
Notes: n = 484; * p < 0.05, ** p < 0.01; a Correlations are in the upper right side while the MSV are in the lower left side; AVE are in bold diagonal.
3.2. Empirical Findings
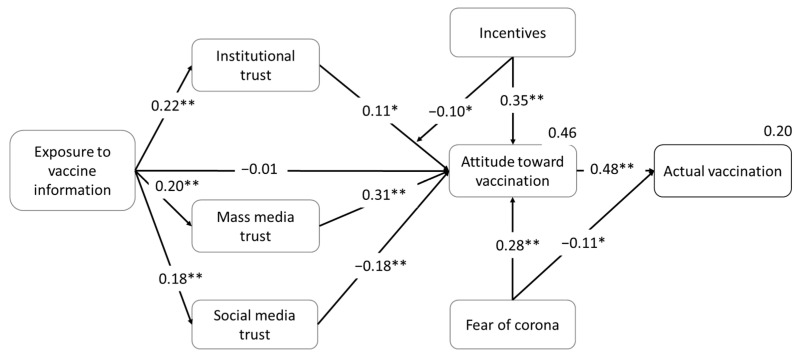
To test this study’s hypothesized relationships, a path analysis was conducted using structural equation modeling and Amos version 25 package. An interaction variable was added for the moderation of incentives. Acceptable levels of fit values (goodness of fit measures) were found, and the path model was valid (χ2 value (373) = 856.91, χ2/df < 3, p < 0.001; CFI = 0.955; NFI = 0.923; RMSEA = 0.052). The R squared for the endogenous variables indicates that the model accounts for 46% of the variance in attitude toward vaccination and 20% of the variance in actual vaccination. Table 3 presents test results of the conceptual model. The general path model, regression standardized coefficients, and their significance are shown in Figure 2.
Table 3.
Direct and indirect variable relationships.
| Relationship | Standardized Effect | Regression Weights (Direct) | ||||
|---|---|---|---|---|---|---|
| Total | Direct | Indirect | Estimate | C.R. | p | |
| Exposure to vaccine inform → Attitude toward vaccination | 0.044 | −0.011 | 0.055 | −0.014 | −0.239 | >0.05 |
| Attitude toward vaccination → Actual vaccination | 0.477 | 0.477 | 0.000 | 0.168 | 9.890 | <0.001 |
| Mass media trust → Attitude toward vaccination | 0.311 | 0.311 | 0.000 | 0.262 | 5.907 | <0.001 |
| Exposure to vaccine inform → Mass media trust | 0.204 | 0.204 | 0.000 | 0.306 | 3.939 | <0.001 |
| Social media trust → Attitude toward vaccination | −0.176 | −0.176 | 0.000 | −0.153 | −3.874 | <0.001 |
| Exposure to vaccine inform → Social media trust | 0.185 | 0.185 | 0.000 | 0.269 | 3.577 | <0.001 |
| Institutional trust → Attitude toward vaccination | 0.108 | 0.108 | 0.000 | 0.113 | 2.178 | =0.029 |
| Exposure to vaccine inform → Institutional trust | 0.217 | 0.217 | 0.000 | 0.262 | 4.075 | <0.001 |
| Incentives → Attitude toward vaccination | 0.353 | 0.353 | 0.000 | 0.417 | 6.160 | <0.001 |
| Incentives X Institutional trust → Attitude toward vaccination | −0.099 | −0.099 | 0.000 | −0.127 | −2.466 | =0.014 |
Figure 2.
The path model. Path parameters are standardized parameter estimates. R2 are in the right corners. * p < 0.05; ** p < 0.01.
Table 3 displays the variables’ direct relationships and their statistical measures. Figure 2 shows a direct positive relationship between attitude toward vaccination and actual vaccination (β = 0.48, p < 0.001). As expected, mass media trust and institutional trust have direct positive relationships with attitude toward vaccination (β = 0.31, p < 0.001; β = 0.11, p = 0.029, respectively). However, social media trust has a direct negative relationship with attitude toward vaccination (β = −0.18, p < 0.001). Therefore, H2, H4a and H5a were supported while H3a was not supported.
Additionally, the direct relationship between exposure to vaccine information and attitude is found to be insignificant (β = −0.01, p > 0.05), and significantly indirect (β = 0.06, bootstrap with 95% CI: 0.02–0.09; p = 0.012), where the relationship is mediated through its relationships with mass media trust, social media trust and institutional trust (β = 0.20, p < 0.001; β = 0.19, p < 0.001; β = 0.22, p < 0.001, respectively). Accordingly, H1 was not supported while H3b, H4b and H5b were merely generally supported.
The SEM statistics offer general results for the mediation effect. Therefore, we used Hayes’ PROCESS macro (model 4) with 5000 bootstrapped samples to check the specific mediation effect of mass media trust, social media, and institutional trust (fear of pandemic and vaccination status were added as covariates). The results indicate that the relationship between exposure to vaccine information and attitude was significantly mediated by each of the constructs: mass media trust (95% CI: = 0.013 to 0.098), social media (95% CI: = −0.058 to −0.006) and institutional trust (95% CI: = 0.002 to 0.064). These results support H3b, H4b, and H5b. Nevertheless, while mass media trust and institutional trust positively mediated this relationship, social media trust exhibits a negative mediation effect.
The effect of incentives on attitude toward vaccination is significantly positive (β = 0.35, p < 0.001). Furthermore, the regression results show that incentives negatively moderate the effect of institutional trust on attitude toward vaccination (β = −0.10, p = 0.014). This means that incentives dampen the positive relationship between institutional trust and attitude toward vaccination (see Figure 3). Hence, hypotheses H6 and H7 are supported.
Figure 3.
The moderation effect of incentives.
Additionally, regarding the control variable, fear of pandemic has a positive relationship with attitude toward vaccination (β = 0.28, p < 0.001) and negative relationship with actual vaccination (β = −0.11, p = 0.015).
4. Discussion
In times of global pandemic such as COVID-19, worldwide institutions use communication campaigns to inform the public and convince them of the vaccine’s effectiveness. At the same time, these institutions are challenged by people’s hesitancy and reluctance to get vaccinated and the misleading information from anti-vaccination movements. Many institutions and organizations do not succeed with their campaigns due to a lack of knowledge about key factors in encouraging the undecided public. Vaccine hesitancy or refusal to get vaccinated is a complex issue involving individuals’ attitudes, beliefs and concerns, group influences, and contextual influences such as the novelty of the disease [4,5]. The present study aimed to understand the role of more distal factors involved in the persuasion process: trust in information sources, institutional trust, and incentives.
The current study demonstrates three major findings: first, the relationship between exposure to information about the vaccine and attitude toward vaccination is not direct as was expected from social learning theory [10]. The effect of exposure to information about COVID-19 vaccination on attitude formation was rather indirect and mediated by individuals’ trust of the players, such as trust in governmental institutions and media (mass media and social media). These results follow previous research demonstrating the essentiality of trust in public information judgment [25,60]. In times of pandemic, trust in information sources is vital for effectively delivering the message on the importance of vaccination and its acceptance [26,27].
Second, the effect of trust on attitude is source dependent. While the effect of mass media trust and institutional trust is positive, both as antecedents and moderators, the effect of social media was negative. This information positively influenced people who believe that mass media is credible in forming a positive attitude toward COVID-19 vaccination and institutional trust. However, people who believe that social media is a credible information source were negatively influenced toward COVID-19 vaccination and formed a negative attitude toward the vaccination. The false narratives can explain this, conspiracy theories and misinformation relating to COVID-19 vaccination, which are widely spread on social media platforms [1,34] and flourish out of control [35].
Third, the use of incentives [1] such as green pass documenting vaccination, monetary incentives, or vaccine accessibility (available in safe, familiar, and convenient places) can reduce the institutional mistrust effect and enhance vaccination attitude and actual vaccination. When there is a problem of trust, incentives are an effective tool to reduce the impact of mistrust and overcome hesitancy and refusal to be vaccinated [53,54]. Unlike coercive policies that may increase people’s resistance to vaccination [55], incentives give people a feeling of freedom with their decisions. Though incentives cannot overcome distrust, they can motivate distrusting individuals to make an effort to be vaccinated [56]. Still, the line between coercive policies and incentives such as the green pass can be quite blurred. While some may see the green pass positively as promoting the health of society and mutual social responsibility, others perceive it as a basis for discrimination and penalty for those who have not been vaccinated [61].
This study has some limitations that should be considered in future research. The unique situation in which the current study was conducted (i.e., where the vaccine supply exceeded its demand) constitutes its strength. Nevertheless, future research should check this study model in different countries to strengthen the results. Additionally, the current study was conducted at a specific time point and the data were collected from a representative sample of the entire population. This exploratory cross-sectional study indicates an association among the variables. Future research should conduct a case control study to support the causality among this study’s variables. Moreover, since the conditions in local markets differ across countries, more studies should be conducted, taking into account the specific regional and cultural conditions. Next, since the pandemic is evolving and dramatically changing, it is recommended to conduct additional studies at different times to detect any shifts in public attitudes and behavior. Finally, this study excluded age break 55+ since at the data collection phase this group (and not other medically vulnerable minorities) received a very dedicated treatment by the authorities. After focused communication campaigns, it was the first group to be vaccinated. They were also given direct access to the vaccinating teams all over the country. Hence, they could not contribute much to vaccine hesitancy. Other medically vulnerable minorities (such as those with chronic diseases) were not segregated from the general population and did not enjoy the same persuasion and accessibility efforts, therefore they were perceived as part of the general population and were included in the representative sample of the general population. Aside from medically vulnerable minorities other psychological and social determinants deserve focus in future research, such as level of education, conservative news consumption, political tendency, and conspiracy beliefs [62]. In addition, groups with specific ethnics origins that are associated with low vaccination uptake [63] and pregnant women [64] should be studied.
5. Conclusions
From a theoretical perspective, this study offers a conceptual framework that enhances our understanding of the effect of information sources and incentives on the persuasive process in health communication in times of pandemic such as COVID-19. It complements social learning theory by emphasizing the mediation effect of trust in the information sources and incentives on the learning process and consequent behavior.
This study offers some suggestions and preventive actions for public service managers and policy makers from a practical perspective. First, institutional trust and mistrust do not begin in the context of a crisis such as the current pandemic. Therefore, governmental authorities should develop a positive relationship with their community and cultivate a relationship of trust over time. These relationships will help effectively communicate and convince people during crises such as the COVID-19 pandemic. Additionally, when there are various levels of trust in the different governmental institutions, it is recommended to use those institutions with higher levels of trust as the official-governmental sources of information. Second, in light of the negative effect of social media on consumer willingness to be vaccinated, it is imperative to integrate trustworthy influencers on social media such as experts, e.g., doctors, researchers, and opinion leaders, to support the pro-vaccine information in order to balance the misinformation on this source. Moreover, people who were vaccinated can become agents of change and take part and assist in the persuasion process especially on social media, creating a new social norm. Additionally, this information should be continuously maintained to control media discourse to reach a higher share of voice. Third, after every round of vaccination, the authorities need to overcome hesitancy and refusal to be vaccinated by those who did not get vaccinated. This study indicates that incentives are suitable means to motivate this population. Accordingly, policy makers are advised to integrate common incentives in their vaccination promotion campaign, such as making vaccination available in safe, familiar, and convenient places, offering monetary incentives, and issuing green pass—which allows entrance to public places and cultural events. These incentives should be adjusted to the social and cultural environment of the targeted audience.
Author Contributions
Conceptualization, D.Z.-S., O.K. and S.L.; methodology, D.Z.-S., O.K., S.F. and S.L.; software, S.F.; validation, S.L.; formal analysis, D.Z.-S., O.K., S.F. and S.L.; investigation, D.Z.-S., O.K., S.F. and S.L.; resources, D.Z.-S., O.K. and S.F.; data curation, S.F. and S.L.; writing—original draft preparation, D.Z.-S., O.K., S.F. and S.L.; writing—review and editing, D.Z.-S., O.K., S.F. and S.L.; project administration, D.Z.-S. and O.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Institutional Review Board of ARIEL UNIVERSITY (protocol code AU-SOC-SL-20210324, 24 March 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schoch-Spana M., Brunson E.K., Long R., Ruth A., Ravi S.J., Trotochaud M., Borio L., Brewer J., Buccina J., Connell N., et al. The public’s role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine. 2021;39:6004–6012. doi: 10.1016/j.vaccine.2020.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.French J., Deshpande S., Evans W., Obregon R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int. J. Environ. Res. Public Health. 2020;17:5893. doi: 10.3390/ijerph17165893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stein J.P., Krause E., Ohler P. Every (Insta)Gram Counts? Applying Cultivation Theory to Explore the Effects of Instagram on Young Users’ Body Image. Psychol. Pop. Media Cult. 2019;10:87–97. doi: 10.1037/ppm0000268. [DOI] [Google Scholar]
- 4.Coelho C.M., Suttiwan P., Arato N., Zsido A.N. On the Nature of Fear and Anxiety Triggered by COVID-19. Front. Psychol. 2020;11:3109. doi: 10.3389/fpsyg.2020.581314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDonald N.E., Eskola J., Liang X., Chaudhuri M., Dube E., Gellin B., Goldstein S., Larson H., Manzo M.L., Reingold A., et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Esaiasson P., Sohlberg J., Ghersetti M., Johansson B. How the coronavirus crisis affects citizen trust in institutions and in unknown others: Evidence from ‘the Swedish experiment’. Eur. J. Polit. Res. 2020;60:748–760. doi: 10.1111/1475-6765.12419. [DOI] [Google Scholar]
- 7.Niu Z., Qin Z., Hu P., Wang T. Health Beliefs, Trust in Media Sources, Health Literacy, and Preventive Behaviors among High-Risk Chinese for COVID-19. Health Commun. 2021:1–9. doi: 10.1080/10410236.2021.1880684. [DOI] [PubMed] [Google Scholar]
- 8.Mo P., Xing Y., Xiao Y., Deng L., Zhao Q. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin. Infect. Dis. 2020;73:ciaa270. doi: 10.1093/cid/ciaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olagoke A.A., Olagoke O.O., Hughes A.M. Intention to Vaccinate Against the Novel 2019 Coronavirus Disease: The Role of Health Locus of Control and Religiosity. J. Relig. Health. 2021;60:65–80. doi: 10.1007/s10943-020-01090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bandura A. Social Learning Theory. Prentice-Hall; Englewood Cliffs, NJ, USA: 1977. [Google Scholar]
- 11.Krishna A., Thompson T.L. Misinformation About Health: A Review of Health Communication and Misinformation Scholarship. Am. Behav. Sci. 2021;65:316–332. doi: 10.1177/0002764219878223. [DOI] [Google Scholar]
- 12.Jones S.C., Waters L., Holland O., Bevins J., Iverson D. Developing pandemic communication strategies: Preparation without panic. J. Bus. Res. 2010;63:126–132. doi: 10.1016/j.jbusres.2009.02.009. [DOI] [Google Scholar]
- 13.Bandura A. Growing Primacy of Human Agency in Adaptation and Change in the Electronic Era. Eur. Psychol. 2002;7:2–16. doi: 10.1027//1016-9040.7.1.2. [DOI] [Google Scholar]
- 14.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall, Inc.; Englewood Cliffs, NJ, USA: 1986. [Google Scholar]
- 15.Abramowitz S., McKune S.L., Fallah M., Monger J., Tehoungue K., Omidian P.A. The Opposite of Denial: Social Learning at the Onset of the Ebola Emergency in Liberia. J. Health Commun. 2017;22:59–65. doi: 10.1080/10810730.2016.1209599. [DOI] [PubMed] [Google Scholar]
- 16.Bajcar E.A., Bąbel P. How Does Observational Learning Produce Placebo Effects? A Model Integrating Research Findings. Front. Psychol. 2018;9:2041. doi: 10.3389/fpsyg.2018.02041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook D.A., Artino A.R. Motivation to learn: An overview of contemporary theories. Med. Educ. 2016;50:997–1014. doi: 10.1111/medu.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenstock I.M., Strecher V.J., Becker M.H. Social Learning Theory and the Health Belief Model. Health Educ. Behav. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 19.Yilmaz M., Yilmaz U., Demir-Yilmaz E.N. The relation between social learning and visual culture. Int. Electron. J. Elem. Educ. 2019;11:421–427. doi: 10.26822/iejee.2019450837. [DOI] [Google Scholar]
- 20.Chen A., Lu Y., Wang B. Customers’ purchase decision-making process in social commerce: A social learning perspective. Int. J. Inf. Manag. 2017;37:627–638. doi: 10.1016/j.ijinfomgt.2017.05.001. [DOI] [Google Scholar]
- 21.Qiao S., Friedman D.B., Tam C.C., Zeng C., Li X. Vaccine acceptance among college students in South Carolina: Do information sources and trust in information make a difference? medRxiv. 2020 doi: 10.1101/2020.12.02.20242982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peifer J.T. Imitation as Flattery: How TV News Parody’s Media Criticism Can Influence Perceived News Media Importance and Media Trust. J. Mass Commun. Q. 2018;95:734–756. doi: 10.1177/1077699017713002. [DOI] [Google Scholar]
- 23.Ognyanova K., Lazer D., Robertson R.E., Wilson C. Misinformation in action: Fake news exposure is linked to lower trust in media, higher trust in government when your side is in power. Harv. Kennedy Sch. Misinf. Rev. 2020 doi: 10.37016/mr-2020-024. [DOI] [Google Scholar]
- 24.Sheth J.N., Uslay C. Implications of the revised definition of marketing: From exchange to value creation. J. Public Policy Mark. 2007;26:302–307. doi: 10.1509/jppm.26.2.302. [DOI] [Google Scholar]
- 25.Ervasti H., Kouvo A., Venetoklis T. Social and Institutional Trust in Times of Crisis: Greece, 2002–2011. Soc. Indic. Res. 2019;141:1207–1231. doi: 10.1007/s11205-018-1862-y. [DOI] [Google Scholar]
- 26.Cairns G., De Andrade M., MacDonald L. Reputation, relationships, risk communication, and the role of trust in the prevention and control of communicable disease: A review. J. Health Commun. 2013;18:1550–1565. doi: 10.1080/10810730.2013.840696. [DOI] [PubMed] [Google Scholar]
- 27.Taha S.A., Matheson K., Anisman H. The 2009 H1N1 influenza pandemic: The role of threat, coping, and media trust on vaccination intentions in Canada. J. Health Commun. 2013;18:278–290. doi: 10.1080/10810730.2012.727960. [DOI] [PubMed] [Google Scholar]
- 28.Piltch-Loeb R., Merdjanoff A., Meltzer G. Anticipated mental health consequences of COVID-19 in a nationally-representative sample: Context, coverage, and economic consequences. Prev. Med. 2021;145:106441. doi: 10.1016/j.ypmed.2021.106441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clayman M.L., Manganello J.A., Viswanath K., Hesse B.W., Arora N.K. Providing health messages to Hispanics/Latinos: Understanding the importance of language, trust in health information sources, and media use. J. Health Commun. 2010;15:252–263. doi: 10.1080/10810730.2010.522697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mackay M., Colangeli T., Gillis D., Mcwhirter J., Papadopoulos A. Examining Social Media Crisis Communication during Early COVID-19 from Public Health and News Media for Quality, Content, and Corresponding Public Sentiment. J. Environ. Res. Public Health. 2021;18:7986. doi: 10.3390/ijerph18157986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kol O., Nebenzahl I.D., Lev-On A., Levy S. SNS Adoption for Consumer Active Information Search (AIS)—The Dyadic Role of Information Credibility. Int. J. Hum. Comput. Interact. 2021;37:1504–1515. doi: 10.1080/10447318.2021.1898824. [DOI] [Google Scholar]
- 32.Yoo W., Choi D.H. Predictors of expressing and receiving information on social networking sites during MERS-CoV outbreak in South Korea. J. Risk Res. 2020;23:912–927. doi: 10.1080/13669877.2019.1569105. [DOI] [Google Scholar]
- 33.Mo P.K.H., Luo S., Wang S., Zhao J., Zhang G., Li L., Li L., Xie L., Lau J.T.F. Intention to receive the covid-19 vaccination in china: Application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines. 2021;9:129. doi: 10.3390/vaccines9020129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lockyer B., Islam S., Rahman A., Dickerson J., Pickett K., Sheldon T., Wright J., McEachan R., Sheard L. Understanding Covid-19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2020;24:1158–1167. doi: 10.1111/hex.13240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oleksy T., Wnuk A., Maison D., Łyś A. Content matters. Different predictors and social consequences of general and government-related conspiracy theories on COVID-19. Pers. Individ. Differ. 2021;168:110289. doi: 10.1016/j.paid.2020.110289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang L. Online Reviews: The Impact of Power and Incidental Similarity. J. Hosp. Mark. Manag. 2015;24:633–651. doi: 10.1080/19368623.2014.929550. [DOI] [Google Scholar]
- 37.Reichelt J., Sievert J., Jacob F. How credibility affects eWOM reading: The influences of expertise, trustworthiness, and similarity on utilitarian and social functions. J. Mark. Commun. 2014;20:65–81. doi: 10.1080/13527266.2013.797758. [DOI] [Google Scholar]
- 38.Weber T.J., Muehling D.D., Kareklas I. How unsponsored, online user-generated content impacts consumer attitudes and intentions toward vaccinations. J. Mark. Commun. 2021;27:389–414. doi: 10.1080/13527266.2019.1671479. [DOI] [Google Scholar]
- 39.Turcotte J., York C., Irving J., Scholl R.M., Pingree R.J. News Recommendations from Social Media Opinion Leaders: Effects on Media Trust and Information Seeking. J. Comput. Commun. 2015;20:520–535. doi: 10.1111/jcc4.12127. [DOI] [Google Scholar]
- 40.Margolis M.A., Brewer N.T., Shah P.D., Calo W.A., Gilkey M.B. Stories about HPV vaccine in social media, traditional media, and conversations. Prev. Med. 2019;118:251–256. doi: 10.1016/j.ypmed.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 41.Tsfati Y. Does Audience Skepticism of the Media Matter in Agenda Setting? J. Broadcast. Electron. Media. 2003;47:157–176. doi: 10.1207/s15506878jobem4702_1. [DOI] [Google Scholar]
- 42.Kim H.K., Tandoc E.C. Wear or Not to Wear a Mask? Recommendation Inconsistency, Government Trust and the Adoption of Protection Behaviors in Cross-Lagged TPB Models. Health Commun. 2021:1–9. doi: 10.1080/10410236.2020.1871170. [DOI] [PubMed] [Google Scholar]
- 43.Uslaner E.M. The Moral Foundations of Trust. Cambridg University Press; Cambridg, UK: 2002. [Google Scholar]
- 44.Tsfati Y., Tukachinsky R., Peri Y. Exposure to news, political comedy, and entertainment talk shows: Concern about security and political mistrust. Int. J. Public Opin. Res. 2009;21:399–423. doi: 10.1093/ijpor/edp015. [DOI] [Google Scholar]
- 45.Borah P., Hwang J. Trust in Doctors, Positive Attitudes, and Vaccination Behavior: The Role of Doctor–Patient Communication in H1N1 Vaccination. Health Commun. 2021 doi: 10.1080/10410236.2021.1895426. [DOI] [PubMed] [Google Scholar]
- 46.Park H.K., Ham J.H., Jang D.H., Lee J.Y., Jang W.M. Political Ideologies, Government Trust, and COVID-19 Vaccine Hesitancy in South Korea: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health. 2021;18:10655. doi: 10.3390/ijerph182010655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yaqub O., Castle-Clarke S., Sevdalis N., Chataway J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 48.Vinck P., Pham P.N., Bindu K.K., Bedford J., Nilles E.J. Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in North Kivu, DR Congo: A population-based survey. Lancet Infect. Dis. 2019;19:529–536. doi: 10.1016/S1473-3099(19)30063-5. [DOI] [PubMed] [Google Scholar]
- 49.Waitzberg R., Triki N., Alroy-preis S., Lotan T., Shiran L., Ash N. The Israeli Experience with the “Green Pass” Policy Highlights Issues to Be Considered by Policymakers in Other Countries. Int. J. Environ. Res. Public Health. 2021;18:11212. doi: 10.3390/ijerph182111212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mualem M. Israeli Mayors Offer Gifts, Incentives, for People Getting Vaccinated. [(accessed on 6 December 2021)]. Available online: https://www.al-monitor.com/originals/2021/02/israel-ultra-orthodox-arabs-east-jerusalem-coronavirus.html.
- 51.Rockliffe L., Chorley A.J., McBride E., Waller J., Forster A.S. Assessing the acceptability of incentivising HPV vaccination consent form return as a means of increasing uptake. BMC Public Health. 2018;18:382. doi: 10.1186/s12889-018-5278-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yamin D., Gavious A. Incentives’ effect in influenza vaccination policy. Manag. Sci. 2013;59:2667–2686. doi: 10.1287/mnsc.2013.1725. [DOI] [Google Scholar]
- 53.Haire B., Komesaroff P., Leontini R., Raina MacIntyre C. Raising Rates of Childhood Vaccination: The Trade-off Between Coercion and Trust. J. Bioeth. Inq. 2018;15:199–209. doi: 10.1007/s11673-018-9841-1. [DOI] [PubMed] [Google Scholar]
- 54.Dubé E., MacDonald N.E. Addressing vaccine hesitancy and refusal in Canada. Cmaj. 2016;188:E17–E18. doi: 10.1503/cmaj.150707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paul K.T., Loer K. Contemporary vaccination policy in the European Union: Tensions and dilemmas. J. Public Health Policy. 2019;40:166–179. doi: 10.1057/s41271-019-00163-8. [DOI] [PubMed] [Google Scholar]
- 56.Taylor S., Landry C.A., Paluszek M.M., Groenewoud R., Rachor G.S., Asmundson G.J.G. A Proactive Approach for Managing COVID-19: The Importance of Understanding the Motivational Roots of Vaccination Hesitancy for SARS-CoV2. Front. Psychol. 2020;11:2890. doi: 10.3389/fpsyg.2020.575950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fu J.R., Ju P.H., Hsu C.W. Understanding why consumers engage in electronic word-of-mouth communication: Perspectives from theory of planned behavior and justice theory. Electron. Commer. Res. Appl. 2015;14:616–630. doi: 10.1016/j.elerap.2015.09.003. [DOI] [Google Scholar]
- 58.Venkatesh V., Thong J.Y.L., Xu X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Q. 2012;36:157–1789. doi: 10.2307/41410412. [DOI] [Google Scholar]
- 59.Tran L.T.T. Managing the effectiveness of e-commerce platforms in a pandemic. J. Retail. Consum. Serv. 2021;58:102287. doi: 10.1016/j.jretconser.2020.102287. [DOI] [Google Scholar]
- 60.Zimand-sheiner D., Levy S., Eckhaus E. Exploring negative spillover effects on stakeholders: A case study on social media talk about crisis in the food industry using a data mining technique. Sustainability. 2021;13:10845. doi: 10.3390/su131910845. [DOI] [Google Scholar]
- 61.Wilf-Miron R., Myers V., Saban M. Incentivizing Vaccination Uptake: The “green Pass” Proposal in Israel. JAMA J. Am. Med. Assoc. 2021;325:1503–1504. doi: 10.1001/jama.2021.4300. [DOI] [PubMed] [Google Scholar]
- 62.Nazlı Ş.B., Yığman F., Sevindik M., Deniz Özturan D. Psychological factors affecting COVID-19 vaccine hesitancy. Ir. J. Med. Sci. 2021:1–10. doi: 10.1007/s11845-021-02640-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Viswanath K., Bekalu M., Dhawan D., Pinnamaneni R., Lang J., McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21:818. doi: 10.1186/s12889-021-10862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cavaliere A.F., Zaami S., Pallottini M., Perelli F., Vidiri A., Marinelli E., Straface G., Signore F., Scambia G., Marchi L. Flu and tdap maternal immunization hesitancy in times of covid-19: An italian survey on multiethnic sample. Vaccines. 2021;9:1107. doi: 10.3390/vaccines9101107. [DOI] [PMC free article] [PubMed] [Google Scholar]