Abstract
Objectives
To understand the hospital-to-outpatient care transition and how the discharge process of stroke patients is managed; and to identify potential opportunities to improve these processes, while contrasting pre- and during COVID-19 experiences in Peru.
Methods
A qualitative study was conducted between February and March 2021 consisting of in-depth interviews of patients with stroke, their caregivers and healthcare personnel regarding stroke care at a national tertiary referral center for stroke care in Lima, Peru. We explored the following phases of the patients’ journeys: pre-hospitalization, emergency room, hospitalization, discharge process and post-discharge. For each phase, we explored experiences, feelings and expectations using thematic analysis.
Results
We conducted a total of 11 interviews with patients or caregivers and 7 with health care personnel and found disruption in the continuity of care for patients with stroke. Mainly, caregivers and patients referred to problems related to communication with healthcare personnel and an absence of training to provide post-discharge care at home. Potential solutions included increasing human resources and caregiver participation in care, implementation of electronic healthcare records, improving the referral system and reinforcing telemedicine services.
Conclusion
The continuity of care of patients with stroke was negatively affected during the COVID-19 pandemic. In LMICs, the impact was likely greater due to the already weak and fragmented healthcare systems. The COVID-19 pandemic presents an opportunity to improve post-stroke care services, and address patients’ experiences and feelings by developing solutions in a participatory manner.
Key Words: Stroke, COVID-19, Continuity of care, Health systems
Abbreviations: HTN, hypertension; DM, diabetes mellitus; INCN, Instituto Nacional de Ciencias Neurológicas
Introduction
The management of stroke is complex, with different actions performed by various aspects of the healthcare system at different places and times.1 The discharge process from hospitals should aim to prepare patients and caregivers to manage stroke sequelae at home and engage them with a plan for post-discharge services, including rehabilitation and management of risk factors, mainly hypertension (HTN), hyperlipidemia and diabetes mellitus (DM).
Post-stroke care is often compromised2 by fragmentation of the healthcare system. The SARS-CoV-2 (COVID-19) pandemic has exacerbated this problem by negatively impacting healthcare systems that have prioritized COVID-19 care over chronic conditions when allocating resources - leading to disruptions in continuity of care for stroke in both high-income and low- and middle-income countries.3 , 4 To date, most studies on the effects of the COVID-19 pandemic in the field of stroke have focused on the acute management of stroke, specifically measuring reductions in the number of hospitalizations worldwide and the number of procedures conducted,5 and have not examined continuity of care following discharge.
Peru has been greatly affected by the COVID-19 pandemic, having one of the highest excess death rates in the world.6 Major weaknesses of the Peruvian healthcare system, including the fragmentation of services and inequalities, were amplified during the pandemic.7 Understanding how the discharge process works in the Peruvian healthcare system, and how it changed in response to the COVID-19 pandemic, could help generate recommendations to ensure adequate long-term care and, importantly, how to improve it, which is much needed in the new post-COVID-19 pandemic world. Our study aimed to (1) understand the hospital-to-outpatient care transition and how the discharge process of stroke patients was managed; and (2) identify potential opportunities to improve the hospital-to-outpatient care transition and discharge process management, while contrasting the transitions pre- and during COVID-19 at a tertiary care hospital in Peru.
Methods
We conducted a qualitative study with a descriptive design and defined the hospital-to-outpatient care transition as the changes in care teams and care settings patients go through within the continuum of care following stroke. In our study, we focused on the transition from the hospital (acute and sub-acute management of stroke) to outpatient care, e.g., household care, outpatient consults for rehabilitation, and stroke risk factors. We defined the discharge process as those activities conducted to prepare and plan for post-discharge services and support for the patient.8
Setting
Acute stroke care in Peru is provided in tertiary hospitals located in major cities. Before the COVID-19 pandemic, less than 50% of patients who experienced a stroke returned for an outpatient appointment within one month after their discharge, only 30% accessed and completed rehabilitation treatment, and about 20% died within a year.9 , 10 This situation may have worsened during the COVID-19 pandemic.
This study focused on patients treated at the Instituto Nacional de Ciencias Neurológicas (INCN) and healthcare providers working there. The INCN is a national reference center for neurological disorders, including stroke, located in Lima, Peru's capital city. Approximately 50% of patients with stroke had hypertension and 18% had diabetes.9 , 11 While these conditions were identified and managed during hospitalization, there was an inadequate follow-up after discharge.10 , 12
Study participants
We studied the discharge process from patient, caregiver and healthcare personnel perspectives. We obtained the patients and caregivers’ names from hospital registries and clinical records from the years 2019–2020, and they were approached by a qualitative researcher through phone calls and SMS and invited to participate in the study after a brief explanation of the study purposes.
Inclusion criteria were: (1a) patients or caregivers of patients who had a stroke, had insurance provided by the Ministry of Health (Seguro Integral de Salud), and were discharged from the hospital in the prior one to three months, (1b) health care personnel providing stroke care (neurologists, cardiologists, endocrinologists, nurses and rehabilitation specialists); (2) 18 years of age or older; and (3) ability to understand the study, provide written informed consent, and communicate. We excluded those who did not agree to participate in the study.
Sampling
Participants were enrolled using convenience sampling, as we contacted patients and caregivers based on the hospital registries and healthcare personnel according to their availability.
For patients, we selected patients with different grades of neurologic deficits, which can impact their interaction with the healthcare system; with different comorbidities (DM and HTN); and patients who were discharged in 2019 and 2020 to contrast pre-COVID and post-COVID discharge processes. We created a list of patients hospitalized early (April–July) and late (August–October) 2020. The distinction between early and late 2020 was important as the COVID-19 pandemic started in March 2020 in Peru and during the first months all healthcare efforts were centered on COVID-19, leaving chronic conditions largely unattended. Thus, we hypothesized that care and the patients’ experiences might be different within the same year.
For healthcare professionals, we created a list of professionals who worked in different areas (hospitalization, outpatient consultation) and provided care to patients with stroke, and we approached them to participate in the study. In order to have a comprehensive understanding of the patients’ journeys through the different services in the INCN, we included professionals who worked in different areas.
Sample size
We estimated a sample size of 20 patients and caregivers and 12 health care personnel to explore patients’ journeys and draft the process map.13 However, the final sample size was determined by reaching saturation of information after analyzing the data in parallel with data collection. Saturation was reached at 11 patients and 8 health care personnel.
Data collection
A female researcher with a background in psychology, not affiliated with the INCN, and with experience in qualitative research methods and chronic conditions conducted individual interviews with patients, caregivers and healthcare personnel from February to March 2021 to map the patient's journey from the hospital to outpatient care. A journey map is a “diagram summarizing the service experiences patients have over time,” which is central to human-centered design as it allows the identification and planning of experiences to improve them.14 We used a semi-structured interview guide that focused on all steps a patient goes through to access post-discharge care for stroke (see Supplementary Material). Interviews were conducted in Spanish and lasted 20–40 min.
Patients were contacted and invited to participate in the study. For those who agreed to participate, a date to perform the interviews was set. Originally, the interviews were planned to take place at the hospital; however, given the risk of COVID-19 exposure, patient and caregiver interviews were conducted by phone.
For the healthcare personnel, only two interviews were conducted by phone. For the remainder, given that the participants’ workload impeded arranging a date and time for an interview, we decided to conduct in-person interviews at the hospital whenever providers had spare time and following COVID-19 protection recommendations.
Data analysis
Interviews were audio-recorded and transcribed verbatim by the qualitative researcher. Themes based on the structure of the patient journey15 (phases, experiences, values, ideas or suggestions for improvement) and emerging themes were identified after the analysis of two interviews to develop a coding framework.16 The coding framework was discussed by the qualitative researcher and the principal investigator and approved by the principal investigator. Then, data were coded by the qualitative researcher using ATLAS.ti version 7. Thematic analysis was used to compare and contrast perspectives and generate unexpected knowledge.
During data collection and analysis, the qualitative researcher and the principal investigator had periodic discussions to assess progress and clarify different aspects of the analysis (reviewing patient journey concepts, discussing the coding framework, discussing data saturation, etc.).
After organizing the data, as part of the process of sharing the study results with healthcare personnel who participated, we shared either a print or digital summary of the patient journey and suggestions to improve care.
Ethics
This study was reviewed and approved by the Institutional Review Boards of the University of Washington and INCN. Informed consent was obtained from each participant. To prevent a breach of confidentiality, only study members had access to recordings and transcripts. All personally identifiable data was removed from transcriptions and final reports.
Results
To find potential participants, we reviewed 86 clinical records of which 73 fulfilled the inclusion criteria. Of those, 34 were contacted and invited to participate and 11 were interviewed; three had been discharged in 2019 and eight in 2020 (three from April to July and five from August to October). Patient ages ranged from 49 to 75 years; six were male and five were female. Length of hospitalization ranged from 7 to 18 days. Regarding comorbidities, ten had HTN, four had dyslipidemia, and two had T2DM. Additionally, we interviewed 7 healthcare professionals including physicians, nurses and technical staff.
Phase 1: arriving at the hospital and the emergency room
Barriers reported by patients regarding presenting to the emergency room included: (1) poor awareness of stroke, (2) deficient understanding of how the system works, and (3) during the COVID-19 pandemic, limitations in mobilization and reorganization of care.
Caregivers reported that the onset of stroke started several hours before they decided to seek medical treatment. In some cases, symptoms were mild at the beginning (e.g., difficulty walking) and did not prompt them to seek care. Additionally, some caregivers did not know how to access care; they were not aware of the possibility of calling for an ambulance or where to take the patient (hospital versus institute, public versus private). Moreover, caregivers were not sure whether the mobilization restrictions allowed travel to a hospital and they had a fear of exposing patients to COVID-19.
“As you could not go out, we did not know whether to take her and expose her to COVID. She is an elderly person, and we thought that if we take her and she gets infected, then whoa. So, hesitated to take her to a hospital” – Carer_moderate_2020
When seeking care, the reorganization of care delayed arrival to an emergency room with the capacity to treat patients with stroke. Thus, patients arrived first at general hospitals where only COVID-19 patients were being treated or at private clinics with no capacity to manage acute stroke and then decided to go to the INCN, mostly after being advised by a healthcare provider or family member.
“So first we took her to (hospital), because it was where she was supposed to get care (jurisdiction) (…) and they told us that they couldn't attend because it was full COVID. They checked her and told us she was having a stroke (…) They didn't even tell us to go elsewhere. Then like crazy, we took her to a clinic (…), but they wanted me to wait three hours for her to be evaluated (…) The pain was so great that a relative told us “But, the hospital for all those things (neurological) is here in Barrios Altos”” – Carer_moderate_2020
Management at the INCN's emergency room was fast and efficient according to patients and caregivers. However, some caregivers felt criticized by the personnel due to the delays in arriving at the INCN.
Phase 2: during hospitalization
Duration of hospitalization ranged from two to twenty days and management consisted of control of risk factors and identification of location and etiology of stroke. Most caregivers noted relief that the patient was being treated and were satisfied with the care provided (e.g., detection and management of chronic conditions) during hospitalization. However, some mentioned elements of care provided to the patient were inadequate (delays in food delivery and neglecting patient hygiene).
“He couldn't sit down and he couldn't move his arm, at that time of breakfast (…) the nurses did not approach (patients) and only walked by them. They told me that breakfast was at seven (…) but he ate at nine." – Carer_moderate_2020
Communication between caregivers and healthcare personnel differed before and during COVID-19. For those who were hospitalized in 2019, it was possible to visit the patient and discuss the patient's status and care plan with healthcare personnel during the visits. However, throughout the year 2020, visiting patients was prohibited by the INCN to reduce the risk of COVID-19 transmission. Therefore, information was provided by phone calls. Caregivers mentioned difficulties communicating with healthcare personnel: for example, phones were often not working, limited information was provided, different healthcare professionals had different ways of explaining things (some were noted to be impolite), among others.
“They did not let us go in (the hospital) due to the pandemic. They called me to say how he (the patient) was evolving and asked me for medicines or diapers, and I went there only to deliver those" – Carer_severe_2020
Phase 3: discharge process
As part of the discharge process, all patients and caregivers mentioned receiving a written document including the diagnosis, prescription list and any laboratory or imaging recommended following discharge. Some patients noted that diet recommnedations were also received. Additionally, all caregivers received oral, but not written, information related to rehabilitation; those hospitalized in 2019 also received specific recommendations of what kinds of exercises to perform at home.
None of the patients or caregivers interviewed received formal training in how to provide care for patients at home (how to mobilize the patient, how to clean or wash them, how to use and take care of the nasogastric tube, etc.). On the other hand, healthcare providers mentioned that nurses were in charge of providing this information.
Some providers did mention that given the restriction against caregivers entering the hospital during the COVID-19 pandemic, communication and potential opportunities for training were missed, resulting in only a brief in-person discussion at discharge. Some patients and caregivers mentioned that contact at discharge was minimal and insufficient to explain the patient's condition and needs.
“(Before the pandemic) while the patient was hospitalized (…) we educated the family. Days before discharge, the family is asked to come to the hospital in the mornings (…) so that they can see how the patient is bathed if the patient is complicated with a tracheostomy or complication. Visiting time was sometimes used to do this or it was pre-arranged. The patient was also taught to use the affected area so that he can be independent
Q: And how have these activities to prepare patients for discharge changed, given the pandemic?
(…) the patient is practically abandoned. The interrelationship with the family has practically been lost. What we are doing (is), even when the entry of relatives is prohibited, trying to get the authorization one day before for the family member to enter with all the necessary measures such as apron, mask, gloves (so we can conduct activities)” – Provider_nursing
Phase 4: outpatient care
As for follow-up visits, all patients and caregivers were asked to request an appointment with a neurologist 14–20 days after discharge. Some patients hospitalized in 2019 had a follow-up appointment at the INCN.
“Control (at the INCN) was a great help to me because they gave me (medicine for) two or three months. The control helped. Right now, as the pandemic started and everything changed. I have to buy the pills, if I don't buy the pills his head starts to hurt” – Carer_mild_2019
However, for those hospitalized in 2020, even when they attempted to schedule a follow-up appointment, either face-to-face or through telemedicine, none of the interviewed participants managed to get one. Both patients/caregivers and healthcare providers noted two main reasons for this: (1) not having a referral and (2) the restructuring of healthcare during COVID-19.
The referral is completed by a physician requesting a higher level of care because the current establishment does not have enough capacity to treat the patient. Thus, stroke patients are referred from other hospitals to the INCN for acute management. For follow-up after discharge, some healthcare providers feel that it can be conducted at general hospitals and primary care clinics, while others considered that patients need to continue receiving care at the INCN.
The process to get a referral is as follows: at discharge, patients were provided a document that states they need a follow-up visit at the INCN. Then, patients needed to go to the general hospital, get an appointment with a physician and ask for a referral; they needed to present the referral document at the INCN when requesting an appointment. Some perceived this process as a potential risk for exposure to COVID-19.
“They refer me to the (hospital) and ask for a referral to the (INCN), I ... miss, I'm not going to expose getting infected (…) I am prone to an infection” – carer_mild_2020
As for caregivers and patients, they felt disoriented and confused when receiving recommendations to return to the INCN for follow-up and being denied the referral at the general hospital. Additionally, at the beginning of the COVID-19 pandemic, general hospitals were not providing appointments for follow-up of patients with chronic conditions.
“They told me to make an appointment for therapy, but at the (INCN) they told me that, since my mother had entered as an emergency, I had to go to the hospital where she belongs in her district. So, I went to the hospital. Because of COVID, they told me there was no attention” – Carer_severe_2020
The healthcare system's response to COVID-19 included the implementation of a telemedicine service in the INCN that allowed continuity of care for some patients. But some limitations arose: appointments covered by the national health insurance did not include an examination and were limited to covering prescriptions, and not all patients had internet access or knew how to conduct video calls, so they depended upon caregivers being present to help them.
“You have to be realistic, here in Peru many have cell phones, but not with internet. They don't know how to use smartphones or rely on their children. The children are not there either because they have to work or they have no interest in taking care of that adult” – Provider_physician
When patients and caregivers could not access appointments, some opted to go to a private clinic and purchased their medications out-of-pocket. In the case of rehabilitation, some did not receive any sessions, while others paid out-of-pocket for a therapist.
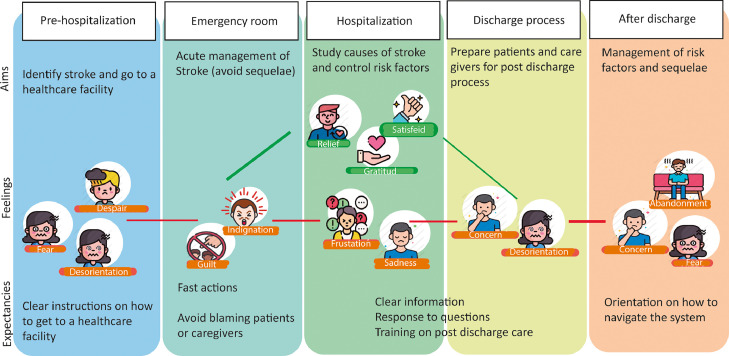
Fig. 1 shows the patient's journey according to the above-described phases. Feelings that arose because of the interaction with healthcare services changed from phase to phase. It is worth noting that during the discharge process and after discharge, patients and caregivers felt concerned, fearful, disorientated and abandoned due to the difficulties accessing follow-up care.
Fig. 1.
Journey map of patients with stoke during the COVID-19 pandemic,Lima-Peru.
Recommendations
During the interviews, we collected suggestions to improve the healthcare system regarding human resources, caregiver participation in care and administrative issues. Caregivers highlighted the need to improve communication skills of healthcare providers to adequately inform patients and caregivers, specifically over the phone which was the only way to communicate during COVID-19.
“Well, to the doctors since they are with the patient and are authorized for the treatment, let them be more precise. They (physicians) should be clearer and kinder. They should be clearer and more precise so that they give us greater peace of mind” – Carer_severe_2020
Additionally, healthcare providers highlighted the need to train and involve caregivers in the care of stroke patients through hospital-based group education sessions or community-based services. Also, pre-recorded videos or booklets were mentioned as an alternative to respecting social distancing during the COVID-19 pandemic.
As for administrative issues, care providers mentioned the importance of having electronic healthcare records to facilitate follow-up and communication between providers, and the need to improve the referral system so patients could receive the level of care required.
“The referral and counter referral system are bad. Unfortunately, I understand that it is due to an issue of oversaturation. Doctors who are in the periphery cannot manage seeing so many patients, giving them their reference and giving them what each patient deserves” - Provider_physician
Providing a clear explanation to patients and caregivers on how to navigate the healthcare system and allocating resources (human, time, technology) to conduct follow-up calls was also suggested to improve access to care after discharge and to prevent re-stroke.
Telemedicine and telerehabilitation represent an important strategy that could reduce barriers such as the need for the patient to present in person at the hospital for an appointment. However, connectivity and competence for using technology need to improve in order for these services to be accessible for everyone.
Discussion
The COVID-19 pandemic brought additional challenges to post-stroke care, further compounding pre-existing deficiencies in healthcare delivery. We conducted a qualitative study aimed at understanding the hospital-to-outpatient transition in stroke care and how the discharge process was managed, and identifying potential opportunities to improve these processes. We explored patients’ and caregivers’ experiences and feelings when interacting with the healthcare system and collected their suggestions to improve care, and this information was complemented by the perspectives of the healthcare providers. In so doing, our findings identified simple, low-cost areas for improvements when entering into the post-COVID world. Hence, our findings are in line with guaranteeing high-quality health systems, including what matters most to people, such as unravelling aspects related to competent care, user experience, health outcomes, and confidence in the system.17
Recently, the World Bank published a document highlighting the need to shift from fragmented healthcare services to patient-centered integration to improve primary care after the COVID-19 pandemic.18 An important aspect of patient-centered care is the consideration of patients’ experiences. In our study, after mapping the patients’ journeys, we identified essential changes to enhance continuity of care and improve patients and caregivers’ experiences through examining the perspectives and experiences of patients, caregivers and health providers.19, 20, 21 We found that providers were focused on managing the acute treatment of stroke and on continuing rehabilitation, while caregivers valued communication and information related to how to best take care of the patient, which is similar to what other studies have reported.21 Drawing on the information provided by the participants, our results suggest the following areas of improvement: enhancing the organization and availability of pre-hospitalization services (ambulances), reinforcing communication during hospitalization and after discharge, revising the discharge process to better educate and train both patients and caregivers regarding the challenges that post-discharge care will present, and improving communication between healthcare establishments to facilitate continuity of care that includes different levels of care Table 1 .
Table 1.
Summary of areas of improvement and recommendations.
| Phase | Areas of improvement | Recommendations |
|---|---|---|
| Arriving at the hospital and the emergency room | Communication/information related to how the health system works | Provide information to the public on how/where to access stroke care |
| Referral system to get to a hospital | ||
| During hospitalization | Communication between family/caregivers and healthcare personnel | -Allocate resources (human/time) to call family/caregivers and provide information -Train personnel on how to communicate via phone calls |
| Discharge process | Absence of formal training | -Provide formal training to caregivers using pre-recorded videos or booklets -Organize hospital-based group education sessions or community-based services |
| After discharge | Difficulties in obtaining follow-up visits related to the referral system | -Provide a clear explanation on how to navigate the healthcare system -Review the referral system and assess potential improvements -Improve telemedicine and telerehabilitation systems to increase reach |
| Feeling of abandonment due to inefficient communication between patient/caregivers and healthcare providers | Allocate resources (human/time) to conduct follow-up calls | |
| Deficient communication between providers | Implement an integrated system that registers follow-up plans and treatment needed after discharge to improve communication between providers |
Patients and caregivers had difficulty deciding to go to a healthcare establishment and difficulty finding a healthcare establishment where patients could be treated. During the COVID-19 pandemic, delays were exacerbated due to fear of becoming infected and some hospitals caring exclusively for COVID-19 patients. Thus, awareness campaigns22 , 23 coupled with updated information on how to navigate the healthcare system (e.g., how to contact a health establishment, where to get stroke treatment) could have been beneficial before, during and after the COVID-19 pandemic in Peru.
One important aspect highlighted during the hospitalization phase was the poor communication between patients and providers, which was worsened during the COVID-19 pandemic. Although phone lines were made available in the hospital wards, arranging specific hours for providers to dedicate themselves to updating caregivers regarding patient status would be appreciated by both patients and caregivers.
Despite its relevance, the discharge process was nearly absent during the COVID-19 pandemic. This process should facilitate the transition from hospital to outpatient care, help patients and caregivers identify their needs (e.g., which rehabilitation services they need and how and when to access them), and contribute to the continuity of care for stroke survivors by improving access to care.8 , 24 However, patients and caregivers were not always actively engaged in this process2 , 8 and the decrease in information and training provided during the discharge process was related to stroke patients not feeling ready to return home.2 , 25, 26, 27 We found that caregivers were not aware of the patients’ prognosis nor prepared to face the challenges of taking care of a patient with stroke at home. Sharing information about stroke sequelae, prognosis and the adaptations in activities of daily life needed from the patient and the family is important, and ensuring healthcare providers have the necessary skills to discuss prognosis and any associated uncertainty in the patient's trajectory of recovery in a compassionate manner is also appreciated by patients and families.28
As caregivers value the information they receive to take care of the patient in the best possible way, standardization of the discharge process could include sharing written or multimedia material instead of only verbal indications, as this could help caregivers better understand and adhere to home care. Quality improvement studies regarding information sharing at the time of discharge have shown that templates help reduce the frequency of omitting important medical advice.29 , 30 In the case of stroke, a quality improvement study assessing the impact of a stroke-specific discharge summary found that specific information such as recommended blood pressure and lipid targets, as well as follow-up plans, were rarely provided to patients; provision of this information increased after the implementation of a discharge summary.29 This supports the idea of implementing similar information sharing at the time of discharge to better equip patients and caregivers for managing risk factors for additional stroke and recovery.
Another important unmet need was related to follow-up in the health system, given that many patients had difficulties in accessing healthcare services after discharge.19 An explanation of how to navigate the healthcare system (e.g., how to make an appointment, how to obtain a referral) has also been highlighted as one of the most important unmet needs of caregivers.21 To improve post-stroke care recovery and stroke prevention, we suggest that each patient and care provider receive a package of information that includes the discharge summary and links to online educational videos. These videos would be developed in collaboration with physicians, therapists and care providers to demonstrate basic activities that would be conducted at home - such as changing and cleaning a nasopharyngeal tube, transferring the patient from bed to a chair or commode, or conducting range-of-motion exercises. These videos would ideally be implemented using quality improvement methods to describe and improve the implementation process while measuring effects of these educational videos upon patient outcome and care provider satisfaction.
A systematic review of studies published during the COVID-19 pandemic found that telerehabilitation could improve functional outcomes, such as the time up and go test and Berg balance scale following stroke,31 suggesting that telerehabilitation can complement in-person rehabilitation appointments. However, requirements to conduct telerehabilitation, such as high-speed internet, are not available for everyone, especially in LMIC and rural areas,32 and personnel trained in conducting telerehabilitation visits need to be in place to successfully implement telerehabilitation services.
During the COVID-19 pandemic in Peru, telemedicine was implemented as an option to improve access to care for patients with stroke and other neurological diseases in outpatient consultation. However, even after telemedicine services were introduced, access to outpatient consultation continued to be a significant barrier for patients in our study, as not all patients had access to internet services sufficient for conducting a telemedicine visit. In addition, training healthcare personnel in how to conduct telestroke services, as well as instructing patients and care providers how to access these services via computer or smartphone were additional challenges to the effective implementation and use of telemedicine services.
Our results signal a diversity of activities that need to occur in the post-stroke care phase, many of them with their own challenges. For example, we found that many of the participants’ responses fit within the capabilities, opportunity and motivation aspects of the COM-B model,10 a model used to tease out the many layers involved in behavioral change, and can therefore be used to guide further developments to improve post-discharge care of stroke. For example, capabilities could be addressed by training, opportunities by guaranteeing follow-up appointments either face-to-face or using telemedicine, and motivation by exploring unique triggers, and each of these domains requires specific tailoring for patients, caregivers and healthcare providers.
Our study had limitations related to patient selection due to difficulties reaching patients, as some phone numbers were inactivated and some did not answer the phone, potentially introducing selection bias. The respondents in our study were likely to be those who have kept in contact with healthcare services, have a stronger social network or higher socioeconomic profile, and have a better health profile in terms of severity; therefore, our results may underestimate the barriers that patients and caregivers face obtaining post-stroke care. Despite that, our findings suggest major deficiencies that ought to be corrected for all stroke patients, many of which are generalizable to many low-income settings in the world given the severity of the pandemic worldwide.
Our study focused on stroke, which can be considered as a representative condition to examine the healthcare system's response to chronic disease management. Given its acute onset and the need to manage its risk factors, particularly after discharge, studying the journeys of patients with stroke allowed a better understanding of how patients entered the system and how they transitioned to chronic care. Additionally, patient journeys helped map experiences, feelings and expectations that arose during the whole process, which is useful input when rethinking how services can be more patient-centered to secure continuity of care.
Conclusion
The continuity of care of patients with stroke was affected during the COVID-19 pandemic due to prioritization of COVID-19 care over other conditions. Caregivers and patients reported problems related to communication with healthcare personnel and lack of training to provide care to patients at home after discharge. Those involved in stroke care provided potential solutions to improve care and most of these solutions were related to human resources, caregiver participation in care and coordination of care between providers and levels of care. To improve care services after COVID-19, it is necessary to consider patients’ and caregivers’ experiences and feelings and develop solutions in a participatory manner.
Sources of funding
This study was funded by the Fogarty International Center (NIH Research Training Grant D43:TW009345) through the Northern Pacific Global Health Research Fellows Training Consortium.
Disclosures
None.
Acknowledgment
We would like to acknowledge the patients and caregivers who participated in the study and the healthcare personnel from the INCN who shared their experiences and provided feedback. Additionally, we would like to thank Julia Dettinger and Hueming Liu for proving input in the protocol, Carola Orrego for proving insight on how to conduct patient journeys, Francisco Diez-Canseco for reviewing the interview guides, and Frances Knight for proof-reading the article and providing suggestions to improve it.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jstrokecerebrovasdis.2021.106275.
Appendix. Supplementary materials
References
- 1.National Institute for Health and Care Excellence (NICE). Stroke pathway [Internet]. London (UK): NICE; 2020. Accessed 6th July, 2020. https://pathways.nice.org.uk/pathways/stroke#path=view%3A/pathways/stroke/stroke-overview.xml&content=view-index.
- 2.Chen L., Xiao L.D., Chamberlain D. An integrative review: challenges and opportunities for stroke survivors and caregivers in hospital to home transition care. J Adv Nurs. 2020 doi: 10.1111/jan.14446. [DOI] [PubMed] [Google Scholar]
- 3.Markus H.S., Brainin M. COVID-19 and stroke—a global world stroke organization perspective. Int J Stroke. 2020;15(4):361–364. doi: 10.1177/1747493020923472. [DOI] [PubMed] [Google Scholar]
- 4.Zhao J., Li H., Kung D., Fisher M., Shen Y., Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51(7):1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reddy S.T., Satani N., Beauchamp J.E.S., et al. A meta-analysis of the global impact of the COVID-19 pandemic on stroke care & the houston experience. Ann Clin Transl Neurol. 2021;8(4):929–937. doi: 10.1002/acn3.51322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Economist. Tracking COVID-19 excess deaths across countries [Internet]. London (UK): The Economist; 2021. Accessed 24th January, 2021. https://www.economist.com/graphic-detail/coronavirus-excess-deaths-tracker.
- 7.Gianella C., Iguiñiz-Romero R., Romero M.J., Gideon J. Good health indicators are not enough: lessons from COVID-19 in Peru. Health Hum Rights. 2020;22(2):317–319. [PMC free article] [PubMed] [Google Scholar]
- 8.Kable A., Baker A., Pond D., Southgate E., Turner A., Levi C. Health professionals’ perspectives on the discharge process and continuity of care for stroke survivors discharged home in regional Australia: a qualitative, descriptive study. Nurs Health Sci. 2019;21(2):253–261. doi: 10.1111/nhs.12590. [DOI] [PubMed] [Google Scholar]
- 9.Alvarado-Dulanto C.M.A., MdlÁ L., Loza-Herrera J.D., Málaga G. Pronóstico al año tras sufrir el debut de enfermedad cerebrovascular en pacientes de un hospital nacional de Lima, Perú. Rev Peru Med Exp Salud Pública. 2015;32(1):98–103. [PubMed] [Google Scholar]
- 10.Málaga G., La Cruz-Saldaña D., Busta-Flores P., Carbajal A., Santiago-Mariaca K. La enfermedad cerebrovascular en el Perú: estado actual y perspectivas de investigación clínica. Acta Med Peru. 2018;35(1):51–54. [Google Scholar]
- 11.Abanto C., Valencia A., Calle P., et al. Challenges of thrombolysis in a developing country: characteristics and outcomes in Peru. J Stroke Cerebrovasc Dis. 2020;29(7) doi: 10.1016/j.jstrokecerebrovasdis.2020.104819. [DOI] [PubMed] [Google Scholar]
- 12.Pesantes M.A., Brandt L.R., Ipince A., Miranda J.J. Diez-Canseco F. An exploration into caring for a stroke-survivor in Lima, Peru: emotional impact, stress factors, coping mechanisms and unmet needs of informal caregivers. eNeurologicalSci. 2017;6:33–50. doi: 10.1016/j.ensci.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guest G., Bunce A., Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. [Google Scholar]
- 14.Boyd H., McKernon S., Old A. Waitemata. District Health Board; Auckland: 2010. Health Service Co-Design: Working with Patients to Improve Healthcare Services. [Google Scholar]
- 15.Boyd H., McKernon S., Old A. Waitemata District Health Board; 2010. Health Service Co-Design: Working with Patients to Improve Healthcare Services: Guide and Toolkit. [Google Scholar]
- 16.Wuetherick B. Basics of qualitative research: techniques and procedures for developing grounded theory. Can J Univ Contin Educ. 2010;36(2) [Google Scholar]
- 17.Kruk M.E., Gage A.D., Arsenault C., et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–ee252. doi: 10.1016/S2214-109X(18)30386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Bank. Walking the Talk: Reimagining Primary Health Care After COVID-19. Washington, DC: The World Bank, 2021.
- 19.Guo Y., Zhang Z., Lin B., et al. The unmet needs of community-dwelling stroke survivors: a systematic review of qualitative studies. Int J Environ Res Public Health. 2021;18(4) doi: 10.3390/ijerph18042140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin B.L., Mei Y.X., Wang W.N., et al. Unmet care needs of community-dwelling stroke survivors: a systematic review of quantitative studies. BMJ Open. 2021;11(4) doi: 10.1136/bmjopen-2020-045560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zawawi N.S.M., Aziz N.A., Fisher R., Ahmad K., Walker M.F. The unmet needs of stroke survivors and stroke caregivers: a systematic narrative review. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2020;29(8) doi: 10.1016/j.jstrokecerebrovasdis.2020.104875. [DOI] [PubMed] [Google Scholar]
- 22.Wolters F.J., Paul N.L., Li L., Rothwell P.M. Sustained impact of UK FAST-test public education on response to stroke: a population-based time-series study. Int J Stroke. 2015;10(7):1108–1114. doi: 10.1111/ijs.12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lecouturier J., Rodgers H., Murtagh M.J., White M., Ford G.A., Thomson R.G. Systematic review of mass media interventions designed to improve public recognition of stroke symptoms, emergency response and early treatment. BMC Public Health. 2010;10(1):1–10. doi: 10.1186/1471-2458-10-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simbolon S., Hamid A.Y.S. The effectiveness of discharge planning stroke patient due to hypertension to improve patient satisfaction and independence. Enferm Clin. 2019;29:703–708. [Google Scholar]
- 25.Boughton M., Halliday L. Home alone: patient and carer uncertainty surrounding discharge with continuing clinical care needs. Contemp Nurse. 2009;33(1):30–40. doi: 10.5172/conu.33.1.30. [DOI] [PubMed] [Google Scholar]
- 26.Cobley C.S., Fisher R.J., Chouliara N., Kerr M., Walker M.F. A qualitative study exploring patients’ and carers’ experiences of early supported discharge services after stroke. Clin Rehabil. 2013;27(8):750–757. doi: 10.1177/0269215512474030. [DOI] [PubMed] [Google Scholar]
- 27.Connolly T., Mahoney E. Stroke survivors’ experiences transitioning from hospital to home. J Clin Nurs. 2018;27(21-22):3979–3987. doi: 10.1111/jocn.14563. [DOI] [PubMed] [Google Scholar]
- 28.Burton L.J., Forster A., Johnson J., et al. Experiences and views of receiving and delivering information about recovery in acquired neurological conditions: a systematic review of qualitative literature. BMJ Open. 2021;11(4) doi: 10.1136/bmjopen-2020-045297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mäkelä P., Haynes C., Holt K., Kar A. Written medical discharge communication from an acute stroke service: a project to improve content through development of a structured stroke-specific template. BMJ Qual Improv Rep. 2013;2(1) doi: 10.1136/bmjquality.u202037.w1095. u202037.w1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vusirikala A., Backhouse M., Schimansky S. Improving driving advice provided to cardiology patients on discharge. BMJ Open Qual. 2018;7(1):e000162. doi: 10.1136/bmjoq-2017-000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ostrowska P.M., Śliwiński M., Studnicki R., Hansdorfer-Korzon R. Telerehabilitation of post-stroke patients as a therapeutic solution in the era of the COVID-19 pandemic. Healthcare. 2021;9(6) doi: 10.3390/healthcare9060654. (Basel, Switzerland) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Inter-American Development Bank. At least 77 million rural inhabitants have no access to high-quality internet services [Internet]. Washington (US): IDB; 2020. Accessed 15th November, 2021. https://www.iadb.org/en/news/least-77-million-rural-inhabitants-have-no-access-high-quality-internet-services.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.