Abstract
The COVID-19 pandemic disrupted routine vaccinations for children and adolescents. However, it remains unclear whether the impact has been different for children and adolescents from low-income families. To address this, we compared monthly routine vaccination use per 1000 vaccine-eligible children and adolescents enrolled in Louisiana Medicaid in the years before (2017–2019) and during the COVID-19 pandemic (2020). Compared to the 2017–2019 average vaccination rates, we found a 28% reduction in measles, mumps, and rubella (MMR), a 35% reduction in human papillomavirus (HPV), and a 30% reduction in tetanus, diphtheria, pertussis (Tdap) vaccinations in 2020. Vaccine uptake was lower in April 2020 after the declaration of a state of emergency and in late summer when back-to-school vaccinations ordinarily occur. We found little evidence of recovery in later months. Our findings suggest that a substantial number of disadvantaged children may experience longer periods of vulnerability to preventable infections because of missed vaccinations.
Keywords: Vaccines, Childhood Immunizations, COVID-19, Pandemic
1. Introduction
The COVID-19 pandemic has caused major disruptions in 2020 in primary care and reduced rates of routine vaccinations for disease prevention among children and adolescents [1], [2], [3], [4]. A recent Centers for Disease Control and Prevention (CDC) report documented substantial reductions in routine childhood vaccine administration at the height of the pandemic’s first wave between March and May 2020 [4]. Notably, while vaccinations rebounded in the summer of 2020, these gains were insufficient to offset losses that had occurred during the peak of shelter-in-place orders and stay-at-home directives ordered by many jurisdictions across the United States [4].
Delayed or missed childhood vaccinations have the potential to increase vulnerability to disease and poor health [5]. For example, unvaccinated children who develop measles – preventable with the measles, mumps, and rubella vaccine (MMR) – are at risk of hospitalization, pneumonia, encephalitis (swelling of the brain) and, in some cases, death (1 to 3 out of 1000) [6]. Human papillomavirus (HPV) – the most common sexually transmitted disease – has been linked to cervical, anogenital, and oropharyngeal as well has head and neck cancer, yet only around half of adolescents receive recommended vaccinations for HPV [7].
Children from low-income families exhibited lower vaccination adherence rates prior to the pandemic and are at heightened risk for COVID-19-related care disruptions [8]. Yet, research describing the pandemic’s impact on vaccinations among children from low-income families is lacking. Furthermore, child vaccination delivery peaks annually in the late summer months as children return to school [9]. However, due to the pandemic, the 2020–2021 school year for many children was characterized by remote learning rather than in-person instruction. The implications of this shift in instruction modalities for childhood vaccination has yet to be explored.
Shortly after confirming its first case of COVID-19 in early March 2020, Louisiana experienced the fastest growth rate of COVID-19 infections worldwide [10]. As a result, on March 13, 2020, Governor John Bel Edwards ordered public schools in Louisiana to refrain from in-person instruction [11]. Schools in Louisiana would be prevented from returning to in-person instruction through the remainder of the 2019–2020 school year and several school districts throughout the state, including New Orleans public schools, began the 2020–2021 school year remotely [12].
In this study, we examined the impact of the COVID-19 pandemic and its related disruptions to traditional in-person schooling on routine vaccinations for MMR (among those aged 1–8 years), HPV (among those aged 9–17 years), and tetanus, diphtheria, and pertussis (Tdap) (among those aged 11–18 years) for low-income children and adolescents insured through Louisiana’s Medicaid and Children’s Health Insurance (CHIP) programs. Our focus on Louisiana was motivated by the relatively large proportion of children in the state living in low-income families, the high reliance on public health insurance (in 2019 there were 707,500 Medicaid enrollees aged 18 and under [13] and approximately 50% of the state’s children are publicly insured [14]), and the comparatively low rates of childhood vaccination adherence in the state [8] with a 7-vaccine series completion rate among children aged 19–35 months old of 72.1% in 2018 [15]. Moreover, Louisiana has a relatively stable beneficiary population as it provides 12-month continuous eligibility for children regardless of changes in income or family size until renewal [16] and, overall, at least 98% of the state’s Medicaid beneficiaries are enrolled for twelve or more months [17].
2. Methods
We used data from the universe of Medicaid claims for the state of Louisiana from January 2017 through December 2020. Vaccinations were identified using claims based on the Current Procedural Terminology (CPT) codes from Centers for Disease Control and Prevention (CDC) Immunization Information Systems [18]. We listed detailed CPT codes in Appendix Table 1. We measured monthly rates of vaccinations per 1000 vaccine-eligible enrollees based on CDC recommended guidelines [19]. In some cases, we used wider age ranges to account for children who received their vaccination earlier or later than recommended. Age ranges were as follows: 1–8 years of age for MMR, 9–17 years of age for HPV, and 11–18 years of age for Tdap. In total, there were 109,101 claims for MMR vaccinations, 109,127 claims for HPV vaccinations, and 58,606 claims for Tdap vaccinations. We focused on these three vaccines given their inclusion in HEDIS measures Immunizations for Adolescent and Childhood Immunization Status and their recent profiling in Morbidity and Mortality Weekly Report (MMWR) by the CDC [4].
We compared the rate of monthly vaccine administrations within each eligible age group in 2020 to average rates from 2017 to 2019 to estimate the impact of disruptions in routine vaccine uptake due to COVID-19. For each vaccine, we created a variable for the monthly per-1000 rate of children enrolled in Medicaid who received recommended doses of the vaccines. We then estimated a linear regression model with calendar month indicators and interaction terms between calendar months and an indicator for the year 2020. The interaction terms can be interpreted as the change in vaccination rates in 2020 compared to the average rate in the same month from 2017 through 2019. Exact regression specifications are included in the appendix for reference. The study was approved by the Tulane University Institutional Review Board and follows the applicable Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
3. Results
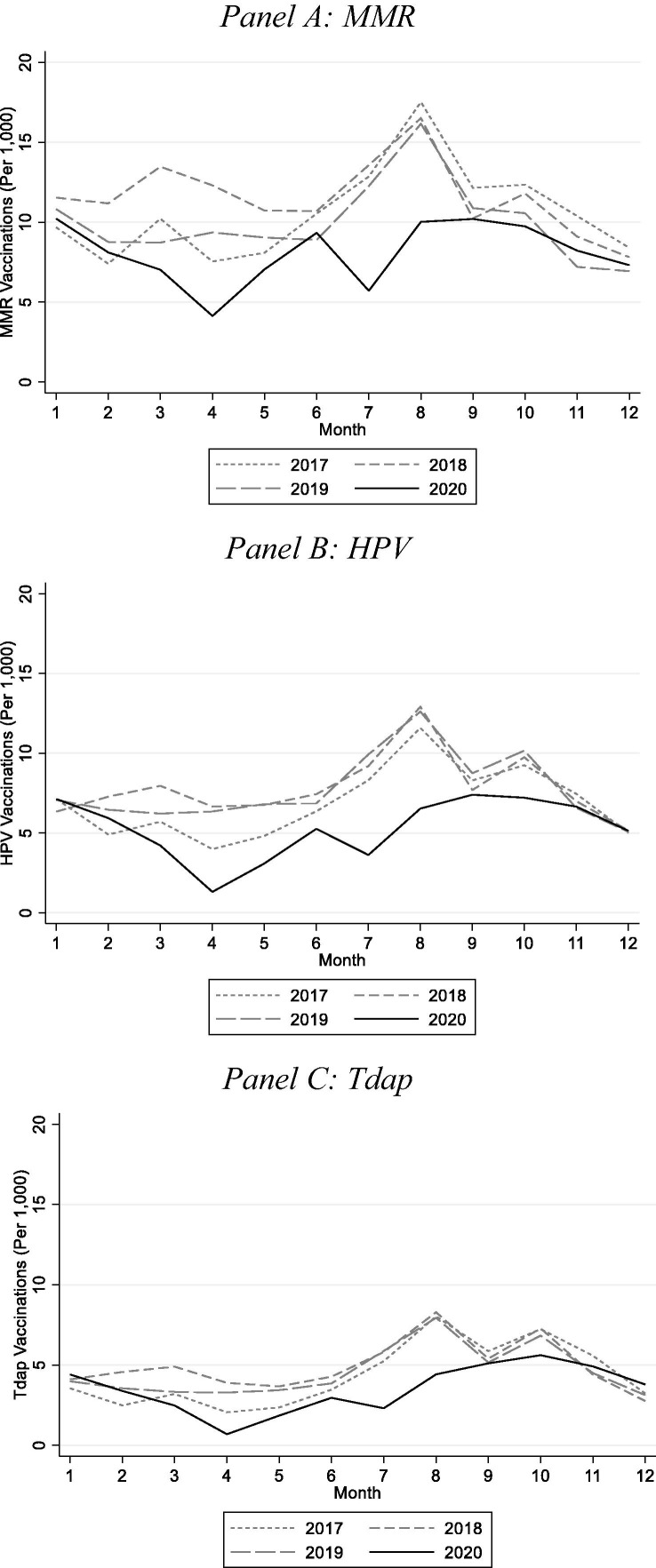
Overall, compared to pre-pandemic vaccination rates between 2017 and 2019, we observed a marked decrease in vaccination rates for MMR, HPV, and Tdap in 2020. Reductions were exceptionally large in April (i.e., the month following the stay-at-home orders) and July (i.e., following the summer COVID-19 spike in cases) (see Fig. 1 ). Also apparent in Fig. 1 is the lack of a late summer spike in routine vaccinations in 2020 corresponding to a return to school. In each of the three years prior to the pandemic, vaccine administration for MMR, HPV, and Tdap peaked in August as children and adolescents prepared for a return to school. However, we observed no such peak in 2020 indicating that the transition to remote learning precipitated by the COVID-19 pandemic was associated with a substantial number of missed or delayed vaccinations. Fig. 1 shows that while utilization rates returned to prior year levels by the end of 2020, the rebound did make up for the total loss in vaccinations.
Fig. 1.
Vaccination Rate Plots for 2017–2020 (by Month). Notes: Ages included were 1 to 8 for MMR, 9 to 17 for HPV, and 11 to 18 for Tdap.
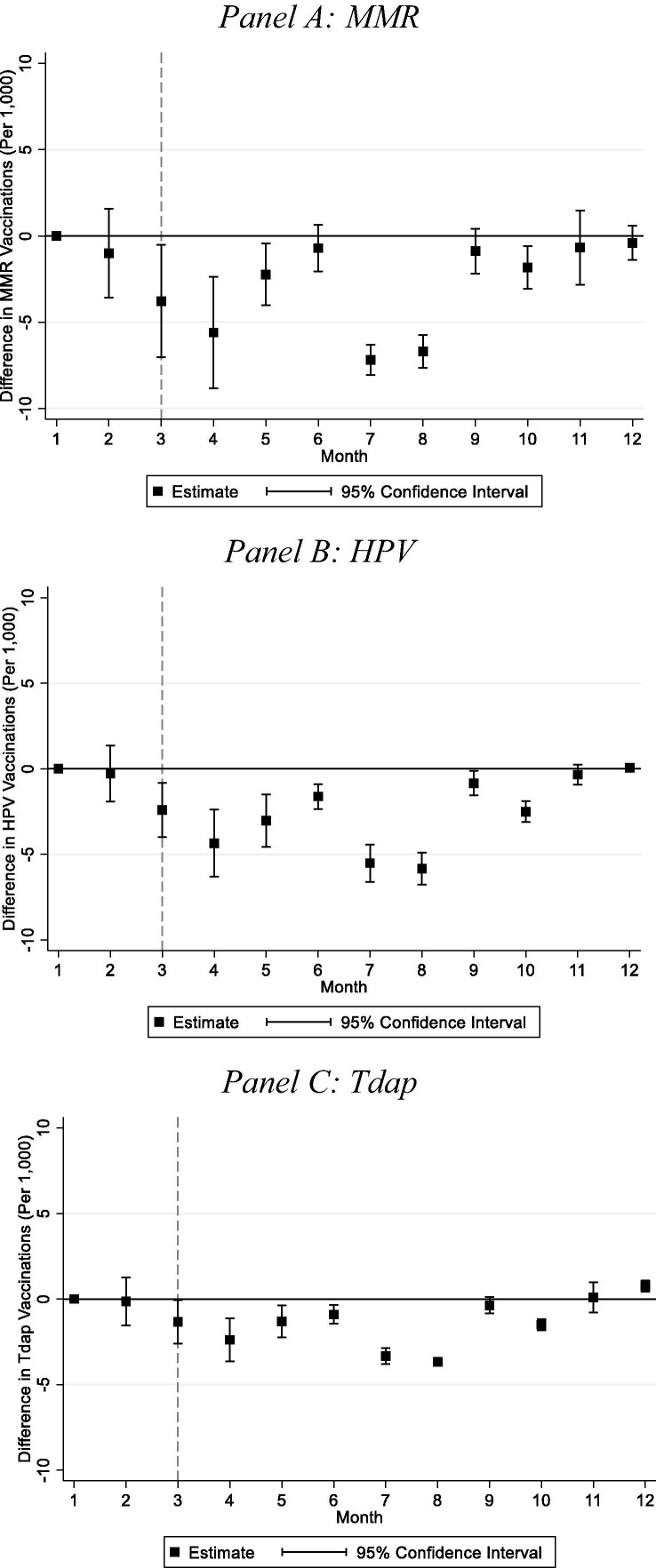
Fig. 2 plots the coefficients and confidence intervals from our regression model described above. Each point on the plot represents the change in vaccinations administered in each month in 2020 compared to the same months in 2017–2019. Generally, vaccination rates in January and February 2020 were similar to those in the pre-pandemic period. However, beginning in March 2020, trends diverged and by April 2020 vaccinations for MMR, HPV, and Tdap were significantly lower than in the previous years. Our regression estimates indicate that MMR vaccinations fell by 5.60 per 1000 (95% CI, −8.83 to −2.37), HPV vaccination rates fell by 4.36 per 1000 (95% CI, −6.32 to −2.39), and Tdap vaccination rates fell by 2.39 per 1000 (95% CI, −3.64 to −1.13) in April 2020 compared to the average rates in previous April months (see Appendix Table 2).
Fig. 2.
Vaccination Rate Comparisons for 2020 Versus Corresponding Months (2017–2019). Notes: N = 48 monthly averages (e.g., four years by 12 months). Mean vaccinations per 1000 eligible Louisiana Medicaid enrollees. Ages included were 1 to 8 for MMR, 9 to 17 for HPV, and 11 to 18 for Tdap. See Eq. (2) in the online appendix for regression specification.
Estimates in Fig. 2 also indicate substantial declines in vaccination rates in July and August 2020 compared to earlier years. MMR vaccination rates fell by 7.18 per 1000 (95% CI, −8.07 to −6.30) in July and by 6.70 per 1000 (95% CI, −7.66 to −5.75) in August 2020 compared to earlier years; HPV vaccination rates fell by 5.52 per 1000 (95% CI, −6.61 to −4.43) in July and by 5.84 per 1000 (95% CI, −6.78 to −4.90) in August 2020 compared to earlier years; and Tdap vaccination rates fell by 3.34 per 1000 (95% CI, −3.81 to −2.87) in July and by 3.67 per 1000 (95% CI, −3.91 to −3.43) in August 2020 compared to earlier years (see Appendix Table 2).
Lastly, we estimated the change in vaccination rates for the pandemic period of our sample compared to average rates prior to the outbreak of COVID-19 in Louisiana. This amounted to replacing the interaction terms in our regression model with an indicator for the pandemic months of March through December 2020. Despite a rebound in the later months of 2020, rates for all three vaccines that we examined were lower in 2020 than in the pre-pandemic years. Specifically, MMR vaccinations fell by 28% (3.00 per 1000, 95% CI, −4.52 to −1.48), HPV vaccinations fell by 35% (2.64 per 1000, 95% CI, −3.81 to −1.48), and Tdap vaccinations fell by 30% (1.40 per 1000, 95% CI, −2.19 to −0.60) (see Appendix Table 3).
4. Discussion
We found lower uptake of routine child and adolescent vaccinations for MMR, HPV, and Tdap in 2020 compared to prior years for Louisiana Medicaid beneficiaries. The magnitude of our findings is comparable to previous studies from outside the US (e.g., one study in the UK found MMR reductions of about 20% [20] while a study in Singapore measured MMR reductions in the range of 26–74% and up to a 10% reduction in Tdap) [21].
The nearly 30% reduction in MMR vaccination rates for Louisiana Medicaid beneficiaries means that more children are vulnerable to measles, mumps, and rubella as coverage of 90–95% is needed to maintain herd immunity [22] and even small reductions in MMR vaccination can have significant consequences for affected communities [23]. The impact of a 35% reduction in the HPV vaccination rate among adolescents in Louisiana Medicaid will take time to assess as it takes years for cancer to develop. Finally, the 30% reduction in Tdap vaccination represents missed opportunities that are particularly important because adolescents often do not receive preventative care and some may not get the vaccinations they missed in future periods [24].
While the reductions in routine vaccinations in April 2020 following the stay-at-home orders are consistent with the literature, we additionally documented significant relative reductions in July and August 2020 prior to school enrollments. Two factors likely explain the reductions in vaccination rates in July and August. First, the “second wave” of COVID-19 infections peaked in Louisiana in July 2020 and health care use declined for Medicaid beneficiaries of all ages. Second, the data indicated an uptick in vaccine administration during the month of August in the pre-pandemic period, coinciding with a return to school. The shift to remote learning experienced by many children in Louisiana in 2020 may have eliminated this annual back-to-school spike in vaccinations. This finding is notable given the outsized role that back-to-school vaccinations play in ensuring adherence to recommended vaccine guidelines. This also complements prior research that found reductions in childhood vaccinations in the early months of the pandemic but lacked data covering the late summer months necessary to identify this effect [1], [2], [3].
4.1. Limitations
The primary limitation of our study is that, despite working with the universe of Medicaid claims, we are not able to document all vaccinations for children in Louisiana’s Medicaid program. Our data include vaccinations administered in settings that generate a claim to be paid by the state’s Medicaid program. Examples of such settings include hospitals, doctor’s offices, clinics, and federally qualified health centers. Medicaid beneficiaries who are vaccinated in settings that do not generate a Medicaid claim will not be observed in our data. However, our estimates of the impact of the COVID-19 pandemic on vaccination rates will not be biased by these omissions unless the share of beneficiaries vaccinated in a non-claim generating setting changed in 2020 relative to prior years in our sample.
5. Conclusions
The disruption in primary care and in-person schooling due to the COVID-19 pandemic had a significant impact on the uptake of routine childhood vaccinations for MMR, HPV, and Tdap among children and adolescents enrolled in Louisiana Medicaid. We found reductions in vaccinations that are comparable to declines in all non-influenza vaccinations during the pandemic. However, this represents the first study, to our knowledge, to focus on vaccinations among children in low-income families that are likely to face unique challenges in recouping missed or delayed health care. Future research should assess the long-term effects of delayed or missed routine child and adolescent vaccinations as a result of the COVID-19 pandemic on morbidity and mortality.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Brigham Walker reports financial support was provided by The Commonwealth Fund (#20202883d). Brigham Walker reports a relationship with ConcertAI that includes: employment.].
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.12.022.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Santoli JM. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR Morbidity and mortality weekly report. 2020;69. [DOI] [PubMed]
- 2.Bramer C.A., Kimmins L.M., Swanson R., Kuo J., Vranesich P., Jacques‐Carroll L.A., et al. Decline in child vaccination coverage during the COVID-19 pandemic—Michigan Care Improvement Registry, May 2016-May 2020. Am J Transplant. 2020;20(7):1930–1931. doi: 10.1111/ajt.16112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Leary S.T., Trefren L., Roth H., Moss A., Severson R., Kempe A. Number of childhood and adolescent vaccinations administered before and after the COVID-19 outbreak in Colorado. JAMA Pediatrics. 2021;175(3):305. doi: 10.1001/jamapediatrics.2020.4733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel Murthy B., Zell E., Kirtland K., Jones-Jack N., Harris LaTreace, Sprague C., et al. Impact of the COVID-19 Pandemic on Administration of Selected Routine Childhood and Adolescent Vaccinations—10 US Jurisdictions, March–September 2020. Morb Mortal Wkly Rep. 2021;70(23):840–845. doi: 10.15585/mmwr.mm7023a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salmon D.A., Dudley M.Z., Glanz J.M., Omer S.B. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine. 2015;33:D66–D71. doi: 10.1016/j.vaccine.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 6.Clemmons N.S., Gastanaduy P.A., Fiebelkorn A.P., Redd S.B., Wallace G.S. Measles—United States, January 4–April 2, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(14):373. [PMC free article] [PubMed] [Google Scholar]
- 7.Kim J.J., Goldie S.J. Health and economic implications of HPV vaccination in the United States. N Engl J Med. 2008;359(8):821–832. doi: 10.1056/NEJMsa0707052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill H.A., Yankey D., Elam-Evans L.D., Singleton J.A., Pingali S.C., Santibanez T.A. Vaccination coverage by age 24 months among children born in 2016 and 2017—National Immunization Survey-Child, United States, 2017–2019. Morb Mortal Wkly Rep. 2020;69(42):1505–1511. doi: 10.15585/mmwr.mm6942a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Leary ST, Cataldi J, Lindley MC, et al. US Primary Care Providers’ Experiences and Practices Related to Routine Pediatric Vaccination During the COVID-19 Pandemic. [DOI] [PMC free article] [PubMed]
- 10.Louisiana Office of the Governor Briefing. COVID-19 Louisiana Response. 2020. Last accessed August 17, 2020 from: https://gov.louisiana.gov/assets/docs/covid/govCV19Brief-2.pdf
- 11.Louisiana Office of the Governor Briefing. Gov. Edwards Signs Proclamation Aimed to Slow the Spread of COVID-19 in Louisiana. 2020. Last accessed August 17, 2020 from: https://gov.louisiana.gov/index.cfm/newsroom/detail/2403
- 12.Nola Ready - COVID-19 in New Orleans. NOLA-PS Announces First Day of School to Start with Distance Learning. 2020. Last accessed August 17, 2020 from: https://ready.nola.gov/incident/coronavirus/update/nola-ps-announces-first-day-of-school-to-start-wit/
- 13.Kaiser Family Foundation. Medicaid Enrollment by Age. 2019. Last accessed December 7, 2021 from: https://www.kff.org/medicaid/state-indicator/medicaid-enrollment-by-age/?dataView=1¤tTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- 14.Kaiser Family Foundation. Medicaid in Louisiana Fact Sheet. 2019. Last accessed August 17, 2021 from: https://files.kff.org/attachment/fact-sheet-medicaid-state-LA
- 15.Louisiana Department of Health. 7 Vaccination Series Completion, Children Ages 19-35 Months Old. 2018. Last accessed December 7, 2021 from: https://ldh.la.gov/assets/oph/Center-PHCH/Center-PH/immunizations/7SeriesRates_2018.pdf
- 16.Kaiser Family Foundation. State Adoption of 12-Month Continuous Eligibility for Children’s Medicaid and CHIP. 2020. Last accessed December 7, 2021 from: https://www.kff.org/health-reform/state-indicator/state-adoption-of-12-month-continuous-eligibility-for-childrens-medicaid-and-chip/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- 17.MACPAC. An Updated Look at Rates of Churn and Continuous Coverage in Medicaid and CHIP. 2021. Last accessed December 7, 2021 from: https://www.macpac.gov/wp-content/uploads/2021/10/An-Updated-Look-at-Rates-of-Churn-and-Continuous-Coverage-in-Medicaid-and-CHIP.pdf
- 18.Centers for Disease Control and Prevention. “CPT Codes Mapped to CVX Codes”. https://www2a.cdc.gov/vaccines/iis/iisstandards/vaccines.asp?rpt=cpt. Published 2021. Accessed August 20, 2021.
- 19.Centers for Disease Control and Prevention. Immunization Schedules. 2021. Last accessed from: https://www.cdc.gov/vaccines/schedules/index.html
- 20.McDonald H.I., Tessier E., White J.M., et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Eurosurveillance. 2020;25(19):2000848. doi: 10.2807/1560-7917.ES.2020.25.19.2000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhong Y., Clapham H.E., Aishworiya R., Chua Y.X., Mathews J., Ong M., et al. Childhood vaccinations: hidden impact of COVID-19 on children in Singapore. Vaccine. 2021;39(5):780–785. doi: 10.1016/j.vaccine.2020.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Black F.L. The role of herd immunity in control of measles. Yale J Biol Med. 1982;55(3–4):351. [PMC free article] [PubMed] [Google Scholar]
- 23.Sugerman D.E., Barskey A.E., Delea M.G., et al. Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally undervaccinated. Pediatrics. 2010;125(4):747–755. doi: 10.1542/peds.2009-1653. [DOI] [PubMed] [Google Scholar]
- 24.Humiston S.G., Rosenthal S.L. Challenges to vaccinating adolescents: vaccine implementation issues. Pediatr Infect Dis J. 2005;24(6):S134–S140. doi: 10.1097/01.inf.0000166161.12087.94. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.