Abstract
Background:
Public health efforts to prevent alcohol-exposed pregnancies (AEPs) primarily focus on promoting abstinence from alcohol among women if pregnant or seeking pregnancy and using effective contraception to prevent unintended pregnancies if consuming alcohol. Little is known about how programs to improve adherence to these recommendations would impact the prevalence of AEPs.
Methods:
We developed an individual-based simulation model of U.S. women of reproductive age to project the prevalence of AEPs under different public health strategies. The model varies each woman’s risk of an AEP over time depending on fertility, contraceptive use, awareness of pregnancy, sexual activity, and drinking patterns. We used the 2013–2015 National Survey on Family Growth dataset to parameterize the model.
Results:
We estimate that 54% (95% uncertainty interval: 48–59%) of pregnancies that result in a live birth in the U.S. are exposed to alcohol, 12% (10–15%) are ever exposed to ≥5 alcoholic drinks in a week and 3.0% (1.3–4.2%) to ≥9 drinks. Unintended pregnancies (either due to contraceptive failure or sex without contraceptives) account for 80% (75–87%) of pregnancies unknowingly exposed to alcohol. We project that public health efforts that focus only on promoting alcohol abstinence among women who are aware of their pregnancy or seeking pregnancy could reduce the prevalence of AEPs by at most 42% (36–48%). Augmenting this strategy with efforts to avert unintended pregnancies could yield an 80% (73–86%) reduction in the prevalence of AEPs.
Conclusions:
Promoting alcohol abstinence among women who are aware of their pregnancy or seeking pregnancy offer limited potential to reduce the prevalence of AEPs. Programs to avert unintended pregnancies are essential to achieve more substantial reductions in AEPs in the U.S.
Introduction
Alcohol consumption during pregnancy may result in harms to the brain and other organs of developing embryos and fetuses [1, 2]. Approximately 1–5% of the U.S. population are affected by Fetal Alcohol Spectrum Disorders (FASDs) -- a spectrum of physical, mental, behavioral, and/or learning disabilities with possible lifelong implications [3–5]. Fetal alcohol syndrome represents the most advanced end of this spectrum. FASD is preventable if women abstain from alcohol consumption throughout pregnancy. Yet, many women may not recognize their pregnancy until well into their first trimester and may unknowingly expose their embryo to alcohol [6]. Not every pregnancy that is exposed to alcohol results in a child with FASD [7–11], but in the absence of a scientifically-proven safe threshold for fetal alcohol exposure [12, 13], preventing alcohol-exposed pregnancies (AEPs) remains the key tactic to prevent FASDs.
Public health efforts to avert alcohol-exposed pregnancies (AEPs) usually target women who are aware of their pregnancies or women who consume alcohol, are sexually active, and do not use contraceptives. Examples of these efforts include the 2005 U.S. Surgeon General’s advisory on alcohol use in pregnancy which recommended that women who are pregnant or considering becoming pregnant refrain from alcohol use [14], and the 2016 CDC recommendation that all sexually active women of reproductive age who are non-sterile and not using contraceptives should abstain from alcohol [15].
Little is known about how these recommendations and programs to improve adherence to these recommendations impact the prevalence of AEPs, which depends not only on levels of sexual activity and alcohol consumption but also on age-specific fertility rates, contraceptive failure rates, and the delay between conception and the detection of pregnancy. The latter three key factors are not accounted for in prevalence estimates of women who are at risk for an AEP [16, 17]. Therefore, public health efforts that aim to avert AEPs through the promotion of alcohol abstinence among high-risk women may not have a meaningful impact if a substantial portion of AEPs are due to contraceptive failures.
To evaluate the performance of public health efforts to avert AEPs, we developed an individual-based model that simulates a cohort of women of reproductive age (15–44 years) in the U.S. In our model, the risk of an AEP for each simulated individual varies over time based on the woman’s fertility, choice of contraceptives, awareness of pregnancy, level of sexual activity, and drinking patterns. We used this model to estimate the prevalence of AEPs and the role that contraceptive failure and sex without contraceptives play in the proportion of pregnancies that are unknowingly exposed to alcohol. We applied this model to project the impact of several strategies, commonly considered by policymakers, on the prevalence of AEPs in the U.S.
Methods
Study Setting and Data Sources
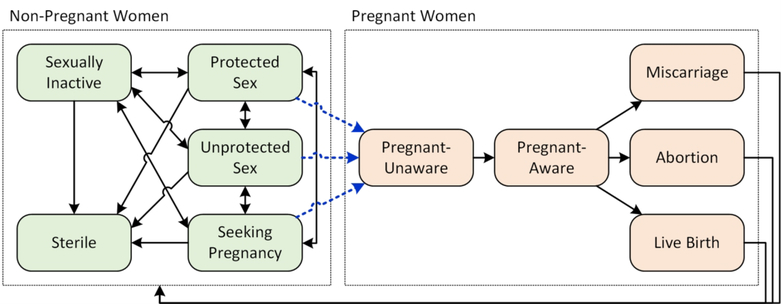
We used data from the 2013–2015 National Survey on Family Growth (NSFG) to estimate the key parameters of our simulation model including the frequency of sexual activity and alcohol consumption. The NSFG provides a nationally representative sample of the population of males and females, ages 15–44 years, living in U.S. households [18]. Data collected from 5,671 female respondents were analyzed (see the Supplementary Material for details). We divided our simulated cohort into six disjoint groups by type of sexual behavior (Fig. 1): (1) “sterile,” which refers to women who are themselves or whose partners are surgically or non-surgically sterile (and hence unable to become pregnant); (2) “sexually inactive,” nonpregnant women that did not have a single male sexual partner in the last year; (3) “protected sex,” nonpregnant women that are sexually active and using contraceptives (Table S3); (4) “unprotected sex,” nonpregnant women who are sexually active, not trying to get pregnant, and not using contraceptives; (5) “seeking pregnancy” women who are trying to get pregnant; and (6) pregnant.
Figure 1.
An individual-based state-transition model to simulate changes in a woman’s sexual-behavior group and pregnancy status over time. The blue dashed arrows represent pregnancy events that might be due to contraceptive failure (top arrow), unprotected sex (middle arrow), or seeking pregnancy (bottom arrow).
Simulation Model
Each simulated individual is initially assigned to one of the categories of sexual behavior described above, based on age-specific probability distributions informed by NSFG data (Table S1–Table S2). Simulated women can move between different categories of sexual behavior according to an age-dependent Markov process (Fig. 1, left panel) that ensures the distribution of women across age and sexual-behavior groups remains consistent with the NSFG data throughout the simulation (Fig. S6). For a simulated woman, the choice of the contraceptive method is determined at the initialization and according to the contraception use data (Table S3) and we assumed that a woman may change their contraceptive method only when they change their sexual-behavior group (i.e. switching from “inactive”, “seeking pregnancy”, “unprotected sex”, or “pregnant” to “protected sex”).
During each week, women who are sexually active may become pregnant with a probability that is determined by the woman’s age, weeks since the last menstrual period, number of sexual encounters, and choice of contraception (§S3 in the Supplementary Material). The number of sexual encounters during each week is determined randomly and based on the woman’s level of sexual activities that varies by age and the sexual-behavior group that the woman belongs to (Fig. S1).
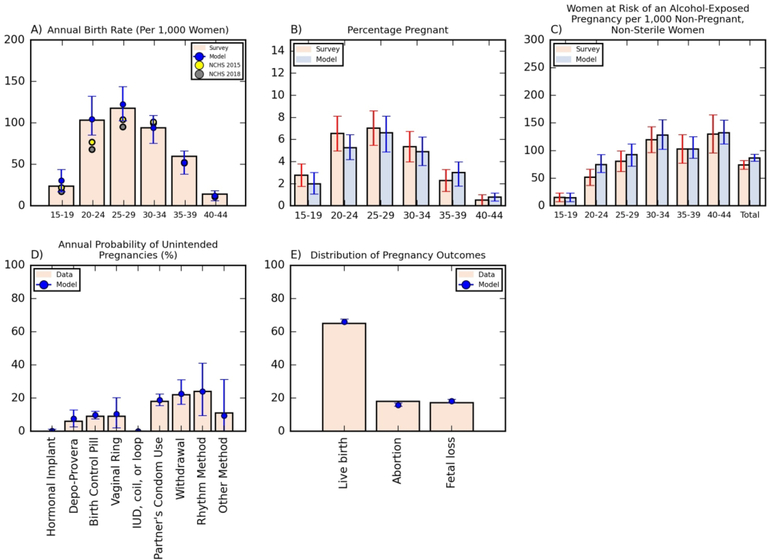
When no contraception is used, each sexual encounter may lead to pregnancy with an age-specific probability (Table S7). These probabilities are informed by existing estimates [19, 20] and are adjusted to match the U.S. age-specific annual birth rates in the U.S. (Fig. 2A). If a contraceptive method is used, the probability that a sexual encounter results in pregnancy is adjusted based on the effectiveness of the selected contraception method (§S3 in the Supplementary Material).
Figure 2.
Model validation: demonstrating the model’s ability to describe several key measures informed by the 2013–2015 National Survey on Family Growth (NSFG) (panels A-C), contraceptive effectiveness statistics [38, 39] (panel D), and the distribution of pregnancy outcomes (panel E) [40]. The age-dependent annual birth rates produced by the model are cross-validated by estimates from the 2015 and 2018 National Center for Health Statistics (NCHS) (panel A) and the distribution of pregnancy outcomes produced by our model is cross-validated by estimates from the 2010 National Vital Statistics System (panel E). See also Fig. S7 in the Supplementary Material for additional figures to validate the proposed model. Bars for survey estimates represent 95% confidence intervals and for model projections represent 95% uncertainty intervals.
Women remain unaware of their pregnancy for a certain period based on probability distributions informed by NSFG data (Table S7). Our model allows for early termination of pregnancies due to miscarriage or abortion (Fig. 1, right panel). Whether a pregnancy ends due to a miscarriage or an abortion is determined based on probabilities estimated from NSFG data (Table S6). The model assumes that the decision to abort a pregnancy is made upon becoming aware of the pregnancy. The weekly number of consumed alcoholic drinks and sexual encounters are modeled by probability distributions informed by NSFG data that depends on the age and sexual-behavior group of the simulated individual (Table S7 and §S1 in the Supplementary Material). While we recognize that correlations might exist between sexual activity, alcohol consumption, and contraceptive methods, the analysis presented in §S1 of the Supplementary Material suggests that the correlations among these parameters are low.
We allow for a 5-year warm-up period before using the model to project desired outcomes over a one-year projection period. All estimates from the model are presented as the average and 95% uncertainty intervals (the 2.5th and 97.5th percentiles) of 100 simulated cohorts. The number of simulated cohorts was chosen such that the resulting uncertainty intervals were stable (i.e. the values of the 2.5th and 97.5th percentiles of estimates did not vary appreciably when additional simulated cohorts were used). We followed the Consolidated Health Economic Evaluation Reporting Standards (CHEERS)[21] to report the results of our simulation modeling study.
Model Validation
We used multiple epidemiological and behavioral measures to establish the validity of our model, including annual birth rates (Fig. 2A), percentage of women pregnant (Fig. 2B), number of women at risk of an AEP per 1,000 non- pregnant, non-sterile women (Fig. 2C), annual probability of unintended pregnancies by contraception method (Fig. 2D), distribution of pregnancy outcomes (Fig. 2E), distribution of women in each sexual behavior group (Fig. S7A), drinking and sexual behavior rates (Fig. S7B–D), and the percentage of pregnancies that resulted in abortion or miscarriage (Fig. S7E–F). These figures confirm that our model can describe the reproductive health, drinking, and sexual behavior of female participants in the NSFG survey. Furthermore, 47% (42–51%) unintended pregnancies in our model was due to contraception failure which is consistent with the results presented by Finer et al. (2006), where it is estimated that 48% of unintended conceptions in 2001 occurred during a month when contraceptives were used [22].
To estimate the number of women at risk of an AEP (Fig. 2C), we followed the established definition of AEP risk and considered a non-sterile, non-pregnant women of reproductive age to be at risk of an AEP if she was sexually active, consumed alcohol, and did not use contraception with sex during the past month [16, 23, 24].
Simulated Strategies to Avert Alcohol-Exposed Pregnancies
Using our simulation model, we estimated the impact of five strategies that employ different mechanisms to prevent alcohol exposure in recognized or unrecognized pregnancies (Table 1). Strategy A seeks to reduce unaware AEPs by promoting the use of effective contraceptives (methods with <10% failure probability after one year of use) to avoid unintended pregnancies (Table S3). This corresponds to many policies and programs that are already in place to prevent unintended pregnancies, including publicly funded family planning and reproductive health services [25], and school-based health education programs [26].
Table 1:
Strategies to reduce the prevalence of alcohol-exposed pregnancies
| Strategy | Mechanism to Prevent an Alcohol-Exposed Pregnancy | Examples | ||||
|---|---|---|---|---|---|---|
| Urging women of reproductive age to: | ||||||
| Use effective contraceptive# if: | Use pregnancy test within a week of a missed period if: | Abstain from drinking if: | ||||
| Not seeking pregnancy | Have been sexually active in the past month | Pregnant | Trying to become pregnant | Not using contraceptive with sex | ||
| A | X | Strategies to avert unintended pregnancies (e.g., family planning services [25], and school-based health education programs [26].) | ||||
| B | X | Strategies to expand access to pregnancy tests | ||||
| C | X | X | Strategies to implement the 2005 U.S. Surgeon General’s Advisory [14] | |||
| D | X | X | X | Strategies to implement the 2016 CDC’s recommendation [15] | ||
| E | X | X | X | Integrated efforts to prevent unintended pregnancies and promote alcohol abstinence during pregnancy and while seeking pregnancy. | ||
| F | X | X | X | X | Combining Strategies B and E. | |
We defined an effective contraceptive method as a method with lower than 10% probability of unintended pregnancy after one year of use (see Table S3 in the Supplementary Material).
Strategy B attempts to avert unaware AEPs by increasing the rate at which pregnant women detect their pregnancies. We assume that a woman who complies with this strategy uses a pregnancy test within a week of a missed period if she has been sexually active in the past month.
Strategy C promotes implementation of the 2005 U.S. Surgeon General’s Advisory on Alcohol Use in Pregnancy [14] that urged pregnant women or women who are considering becoming pregnant to abstain from drinking. Strategy D promotes implementation of the CDC’s 2016 recommendation that attempted to augment the 2005 U.S. Surgeon General’s Advisory on Alcohol Use in Pregnancy[14] by also urging women who are not using contraceptives with sex to abstain from drinking [15].
Strategy E represents integrated efforts to reduce the prevalence of AEPs by both preventing unintended pregnancies and promoting alcohol abstinence among women who are pregnant or seeking pregnancy. To increase the use of effective contraceptives and to improve adherence to universal preventive measures (such as Strategies C and D), this strategy may utilize a series of evidence-based and targeted interventions including 1) school-based education programs aimed at reducing unintended pregnancies and alcohol use [27–29], 2) alcohol screening and brief interventions by health care providers or social workers which may be combined with assessment of a woman’s contraceptive needs [16, 30], and 3) targeted interventions such as BALANCE [29, 31], CHOICES [32, 33], CHOICES4HEALTH [29, 31], and EARLY [24, 34] that seeks to modify drinking and contraceptive behaviors of women who are at an increased risk of an AEP.
Finally, Strategy F augments Strategy E with efforts to increase the number of women who use a pregnancy test within a week of a missed period if have been sexually active in the past month.
Since evidence is lacking about how many women would further adhere to the recommendations considered here, we project the impact of these strategies on the prevalence of AEP and unaware AEP for varying compliance level. This will allow us to estimate the maximum reduction in the prevalence of AEP and unaware AEP that could be achieved under each strategy and also to estimate how many women should comply with each strategy to achieve the same level of reduction in the prevalence of AEP and unaware AEP.
Results
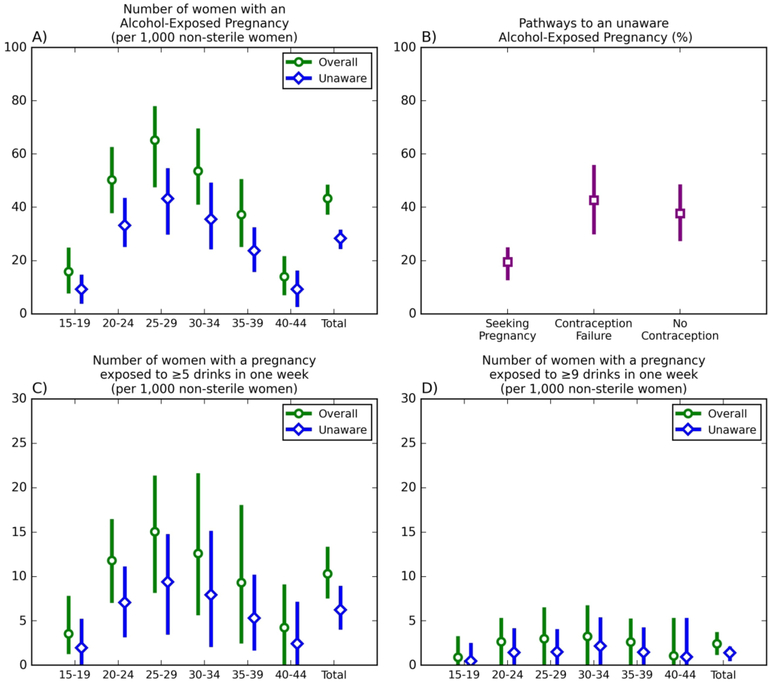
Our model suggests that among pregnancies that result in a live birth in the U.S., 54% (48–59%) are exposed to alcohol, 12% (10–15%) are ever exposed to ≥5 alcoholic drinks in a week during pregnancy and 3.0% (1.3– 4.2%) to ≥9 drinks. Unaware AEP, estimated at 28.4 (24.4–31.7) per 1,000 non-sterile U.S. women, comprise the majority of total AEPs at 43.4 (37.3–48.5) per 1,000 non-sterile U.S. women (Fig. 3A and Table 2). We estimate the prevalence of pregnancies that are exposed to ≥5 or ≥9 alcoholic drinks in a week during the pregnancy 10.3 (7.5–13.4) and 2.4 (1.2–3.8) per 1,000 non-sterile U.S. women, which is substantially lower that the prevalence of pregnancies that are exposed to any level of alcohol (i.e., 43.4 (37.3–48.5) per 1,000 non-sterile U.S. women). The prevalence of both overall and of unaware AEP differs substantially by age (Fig. 3) and are highest among 25–29 year-old women (Fig. 3A).
Figure 3.
A) Prevalence of alcohol-exposed pregnancies (AEPs) among the U.S. women of reproductive age, stratified by age. B) Percentage of unaware AEPs caused by drinking during an undetected pregnancy that resulted from trying to get pregnant (“Seeking Pregnancy”), from contraception failure (“Contraception Failure”), and from a sexual encounter while not using contraceptives (“No Contraception”). C-D) Prevalence of pregnancies among the U.S. women of reproductive age that are ever exposed for ≥5 and ≥9 alcoholic drinks during a week of pregnancy. The prevalence of unaware AEPs is defined as the number of pregnant women who drank while unaware of their pregnancy per 1,000 non-sterile women of reproductive age. Only pregnancies that result in a live birth are included in these estimates. Bars represent 95% uncertainty intervals.
Table 2.
Alcohol exposure during pregnancy by the pathway to pregnancy and the time of consuming alcohol
| Pathway to pregnancy | ||||
|---|---|---|---|---|
|
| ||||
| Time of consuming alcohol | Seeking Pregnancy | Contraceptive Failure | Sex with no contraceptives | Sum |
| Never | 7.0% | 8.2% | 10.0% | 25.2% |
| Only while pregnancy was unrecognized | 4.9% | 8.9% | 8.6% | 22.4% |
| Only while pregnancy was recognized | 7.0% | 9.9% | 9.6% | 26.5% |
| While pregnancy was recognized and unrecognized | 8.6% | 7.4% | 9.8% | 25.9% |
|
| ||||
| Sum | 27.6% | 34.4% | 38.0% | 100.0% |
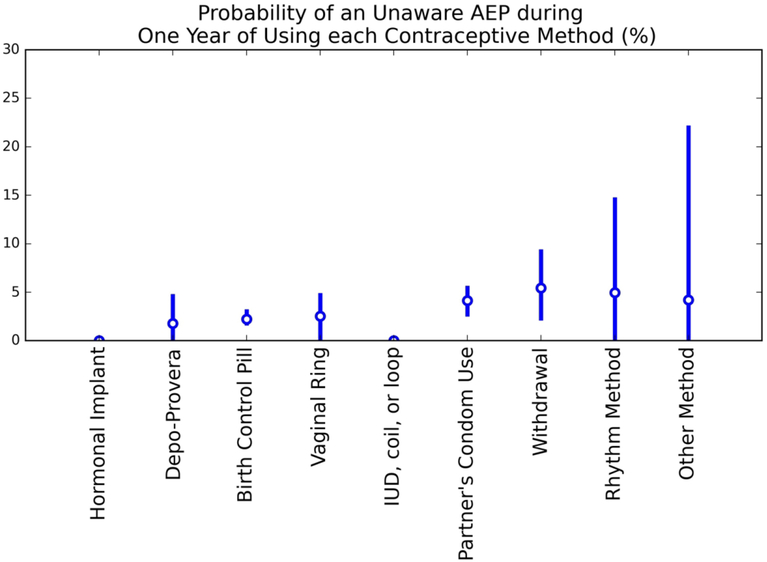
Among the three pathways leading to an unaware AEP, contraception failure is the main contributor, accounting for 43% (30–56%) of unaware AEPs (Fig. 3B). Consuming alcohol while seeking pregnancy accounts for 20% (13–25%) of unaware AEPs, and consuming alcohol while not using contraception and not seeking pregnancy contributes 38% (27–49%) to the prevalence of unaware AEPs (see also Table 2). Our model suggests that the probability of unaware AEPs is the highest among women who rely on withdrawal and rhythm method as contraceptives (Fig. 4).
Figure 4.
Probability of an unaware AEP during one year of using each contraceptive method. Here ‘Other Method’ includes contraceptive patch, diaphragm, and spermicide; less than 0.8% of women of childbearing age use these contraceptive methods (Table S3).
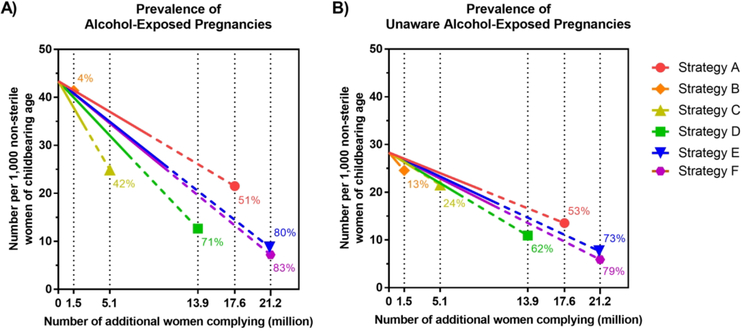
Fig. 5 displays the prevalence of AEPs and unaware AEPs as more women adhere to the recommendations of strategies listed in Table 1. Strategy A does not assume any change in the drinking behavior of its target population, and yet, it could lead to 51% (42–64%) reduction in the prevalence of AEPs if the estimated 17.6 million women of reproductive age who do not use effective contraceptives with sex start using effective contraceptives. A strategy that ensures all pregnancies are detected within one week after a missed period (Strategy B) is expected to reduce the prevalence of AEPs by 4% (0–12%).
Figure 5.
Change in the prevalence of alcohol-exposed pregnancies (AEPs) and unaware AEPs under strategies defined in Table 1. The x-axis represents the number of non-sterile, women of reproductive age who: under strategy A, switch to effective contraceptives (with less than 10% probability of failure in one year of use) from not using contraceptives at all or using ineffective methods; under strategy B detect their pregnancies within a week of a missed period; under strategy C, abstain from drinking if seeking pregnancy or pregnant; under strategy D, abstain from drinking if pregnant, seeking pregnancy or not using contraceptives with sex; under strategy E, comply with strategies A and C; and under strategy F comply with strategies A-C. Solid lines and dotted lines assume up to 0–50% and >50–100% adherence, respectively. Vertical dotted lines represent the maximum number of women that could be reached through each strategy in the U.S. The numbers next to each line represent the maximum percentage reduction in the prevalence of AEP or unaware AEP under each strategy. The slopes of these lines are provided in Table S8. See Fig. S8 for the prevalence of pregnancies that are exposed to ≥5 or ≥9 alcoholic drinks in a week during the pregnancy under strategies defined in Table 1.
Efforts to implement the 2005 U.S. Surgeon General’s Advisory on Alcohol Use in Pregnancy (Strategy C) [14], could reduce the prevalence of AEPs by 42% (36–49%) if the estimated 5.1 million women who consume alcohol while pregnant or seeking pregnancy adhere to this strategy. Implementation of the CDC’s 2016 recommendation (Strategy D) [15] could boost Strategy C and result in a 71% (63–78%) decline in the prevalence of AEPs if the estimated 13.9 million women of reproductive age who consume alcohol with unprotected sex or when pregnant comply with this recommendation. Integrated efforts to avert AEPs through prevention of both unintended pregnancies and alcohol consumption among women who seek pregnancy or are aware of their pregnancy (Strategy E) could yield a maximum reduction in the prevalence of AEPs (80% (73–86%)).
Our model suggests that under the Strategy F where all women (1) use effective contraceptives if they do not intend to become pregnant, (2) detect their pregnancies within one week of a missed period, and (3) abstain from drinking if aware of their pregnancy or seeking pregnancy, 17% (11–23%) of pregnancies are still exposed to alcohol and the prevalence of AEPs is expected to be 7.4 (5.0–10.1) per 1,000 non-sterile women of reproductive age.
Discussion
We developed a simulation model of U.S. women of reproductive age (15–44 years) to estimate the current prevalence of AEPs and to project the impact of various public health strategies to avert AEPs. We estimate that about half of pregnancies that result in a live birth in the U.S are exposed to alcohol but only 12% (10–15%) and 3.0% (1.3–4.2%) are ever exposed to ≥5 or ≥9 alcoholic drinks in a week during pregnancy.
We estimated the prevalence of unaware AEPs at 28.3 (23.5–32.2) per 1,000 non-sterile women of reproductive age. To our knowledge, this is the first study presenting an estimate of the prevalence of unaware AEPs. In the absence of this prevalence estimate to date, researchers and policymakers seeking to quantify the burden of unaware AEPs have relied on prevalence estimates of risk for AEP, which is measured as the number of women who are sexually active, consume alcohol, and do not use contraception with sex, per 1,000 non-sterile, non-pregnant women of reproductive age [16, 23, 24]. Using the same data source employed in this study – the NFSG survey, the CDC recently estimated the prevalence of risk for AEP at 73 (62–86) per 1,000 non-sterile, non-pregnant U.S. women [16]. This measure could lead to a biased estimate for the actual prevalence of unaware AEPs because it fails to account for women’s fertility, choice of contraceptives, and the delay between conception and the detection of pregnancy.
Efforts to avert AEPs have historically focused on encouraging women who are aware of their pregnancy or trying to become pregnant to abstain from drinking. Although this group of women are clearly at risk for AEP, we estimate that the prevalence of AEP would decrease by no more than 42% (36–49%) if all women in this group refrain from drinking. The limited impact of this strategy can be attributed to the observation that drinking while unaware of an unintended pregnancy contributes the most to the prevalence of AEPs -- 80% (75–87%) of unaware AEPs resulted from exposure to alcohol in unintended pregnancies (Fig. 3B and Table 2).
Our analysis suggests that increasing the use of effective contraceptives (with <10% probability of unintended pregnancy after 1 year of use) among sexually active women could reduce the prevalence of AEPs by 51% (42–64%) without assuming any change in women’s drinking behavior. This could be explained by noting that 1) among U.S. women of reproductive age who are sexually active and use contraception, a substantial portion rely on their partner’s condom use or withdrawal as their primary method (31% according to the NSFG data); these methods have high rates of failure (18% and 22% in one year of use, Table S3); and 2) women who use contraceptives wait longer to use pregnancy tests, compared with those who do not use contraceptives, and may continue to drink at pre-pregnancy levels until the pregnancy is confirmed [35].
Concerns about the high likelihood of alcohol-exposure in unintended pregnancies prompted the CDC to issue a new recommendation in 2016 to encourage all women of reproductive age who do not use contraceptives with sex to refrain from drinking. Although the broad implementation of this recommendation could clearly reduce the risk of an AEP in this subgroup, its impact on the prevalence of AEP will be bounded while a substantial proportion of women do not use effective contraceptives; our model estimates that the prevalence of AEPs would decrease by at most 71% (63–78%) if all women of reproductive age who are seeking pregnancy, know that they are pregnant, or not using contraceptives with sex abstain from drinking.
Our analysis has certain limitations. First, we used NSFG survey data to parameterize and validate our simulation model. NSFG data are based on self-reported responses to survey questions and thus may be subject to social desirability bias which might result an underestimation of the prevalence of AEP. Pregnant women may be even more likely to under-report drinking then the general population [36]. However, highly sensitive questions (such as those related to drinking, miscarriage, and abortion) were only asked in the context of an audio-computer assisted self-interview to reduce this bias [18]. Second, consistent with existing studies [16, 24, 33, 37], we counted a pregnancy as an AEP if the woman consumed any level of alcohol during the pregnancy. Not every woman who drinks during pregnancy would deliver a child with alcohol-related complications [7–11]. While we also report the prevalence of pregnancies that are ever exposed to ≥5 or ≥9 alcoholic drinks in a week during pregnancy, we note that in the absence of a safe threshold for fetal alcohol exposure [12, 35], our conservative approach to measure the burden of AEPs would be justified and is consistent with recent evidence that any level of alcohol consumption could impact craniofacial development [13].
Third, while we assumed that women in the “sterile” category of our model are unable to get pregnant, those who are surgically sterilized (e.g. through vasectomy or tubal ligation) may still become pregnant. Since pregnancy among these individuals is rare, we do not expect this assumption to have a meaningful impact on our conclusions. Fourth, while the probability of contraceptive failure could change by the duration of use and experience, we assumed that this probability only depends on the age and the number of sexual acts of a simulated woman (see §S3). Fifth, the public health strategies we considered in our analysis seek to reduce the prevalence of AEPs among all women of child-bearing age (Table 1). In practice, however, approaches that target populations based on certain risk factors such as, age, alcohol consumption patterns, and sexual behavior would be more effective and efficient in preventing AEPs. This could be a useful area to investigate as a future step. Finally, strategies we considered here may require different levels of financial and health-services resources and have consequences beyond impact on the prevalence of AEPs (for example, motivating woman to use contraceptive pills may increase their risk of sexually transmitted infections). Hence, a formal economic evaluation analysis is needed to inform decision about which strategy to invest and promote.
While our model estimates that 54% (48–59%) of pregnancies that result in a live birth in the U.S. are exposed to alcohol, only 1–5% of the U.S. population are affected by Fetal Alcohol Spectrum Disorders (FASDs) [3–5]. This suggests that only a small proportion of AEPs are exposed to high enough levels of alcohol to cause substantial harms to developing embryos and fetuses. Therefore, if the goal is to reduce the prevalence of FASDs, focusing on reducing the prevalence of AEPs (which is currently defined as a pregnancy with any level of exposure to alcohol), may not be the most efficient strategy. Further research is needed to identify the characteristics of AEPs that are at an increased risk of resulting in FASD to facilitate targeted interventions.
In conclusion, our study highlights the need for more carefully considered recommendations and serves as a call to action to examine strategies to invest in and promote to avert AEPs in the U.S in the context of their projected impact. Even if universally adopted, current recommendations regarding alcohol abstinence are expected to yield limited reductions in AEPs, and exclusively focusing on programs to implement these recommendations would not be an optimal approach. Our findings provide evidence to support the prioritization of efforts to increase access to contraceptives with high effectiveness as a key tactic to reduce AEPs, alongside interventions that seek to prevent AEPs through alcohol abstinence among women who are pregnant or trying to become pregnant.
Supplementary Material
Acknowledgements
RY is supported by grants K01AI119603 and R01AI153351 from the National Institute of Allergy and Infectious Diseases, MS was supported by grant K08HS024332 from the Agency for Healthcare Research and Quality, and ADP by R37DA015612 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Agency for Healthcare Research and Quality.
Footnotes
Conflict of Interests
RY, ADP, and MS report receiving funding from the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC). Maya Mahin is currently employed by Analysis Group, Inc., Boston, MA.
Contributor Information
Reza Yaesoubi, Department of Health Policy and Management, Yale School of Public Health, New Haven, CT..
Maya Mahin, Department of Health Policy and Management, Yale School of Public Health, New Haven. Current affiliation: Analysis Group, Inc., Boston, MA..
Geoffrey Martin, Yale-NUS College, Singapore..
A. David Paltiel, Department of Health Policy and Management, Yale School of Public Health, New Haven, CT..
Mona Sharifi, Department of Pediatrics, Yale School of Medicine, New Haven, CT.
References
- [1].Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis (vol 5, pg e290, 2017). Lancet Glob Health. 2017; 5(3):E276–E. [DOI] [PubMed] [Google Scholar]
- [2].Stratton K, Howe C, Battaglia FC. Fetal alcohol syndrome: Diagnosis, epidemiology, prevention, and treatment: National Academies Press; 1996. [Google Scholar]
- [3].May PA, Baete A, Russo J, Elliott AJ, Blankenship J, Kalberg WO, et al. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics. 2014; 134(5):855–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].May PA, Gossage JP, Kalberg WO, Robinson LK, Buckley D, Manning M, et al. Prevalence and Epidemiologic Characteristics of Fasd from Various Research Methods with an Emphasis on Recent in-School Studies. Developmental Disabilities Research Reviews. 2009; 15(3):176–92. [DOI] [PubMed] [Google Scholar]
- [5].May PA, Chambers CD, Kalberg WO, Zellner J, Feldman H, Buckley D, et al. Prevalence of Fetal Alcohol Spectrum Disorders in 4 US Communities. JAMA. 2018; 319(5):474–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Branum AM, Ahrens KA. Trends in Timing of Pregnancy Awareness Among US Women. Maternal and Child Health Journal. 2017; 21(4):715–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kesmodel US, Bay B, Wimberley T, Eriksen HL, Mortensen EL. Does binge drinking during early pregnancy increase the risk of psychomotor deficits? Alcohol Clin Exp Res. 2013; 37(7):1204–12. [DOI] [PubMed] [Google Scholar]
- [8].Kesmodel US, Eriksen HL, Underbjerg M, Kilburn TR, Stovring H, Wimberley T, et al. The effect of alcohol binge drinking in early pregnancy on general intelligence in children. BJOG. 2012; 119(10):1222–31. [DOI] [PubMed] [Google Scholar]
- [9].Kilburn TR, Eriksen HL, Underbjerg M, Thorsen P, Mortensen EL, Landro NI, et al. Low to Moderate Average Alcohol Consumption and Binge Drinking in Early Pregnancy: Effects on Choice Reaction Time and Information Processing Time in Five-Year-Old Children. PLoS One. 2015; 10(9):e0138611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Skogerbo A, Kesmodel US, Wimberley T, Stovring H, Bertrand J, Landro NI, et al. The effects of low to moderate alcohol consumption and binge drinking in early pregnancy on executive function in 5-year-old children. BJOG. 2012; 119(10):1201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Underbjerg M, Kesmodel US, Landro NI, Bakketeig L, Grove J, Wimberley T, et al. The effects of low to moderate alcohol consumption and binge drinking in early pregnancy on selective and sustained attention in 5-year-old children. BJOG. 2012; 119(10):1211–21. [DOI] [PubMed] [Google Scholar]
- [12].Moreno MA. Prenatal Alcohol Exposure No Safe Amount. Jama Pediatr. 2017; 171(8):820-. [DOI] [PubMed] [Google Scholar]
- [13].Muggli E, Matthews H, Penington A, Claes P, O’Leary C, Forster D, et al. Association Between Prenatal Alcohol Exposure and Craniofacial Shape of Children at 12 Months of Age. Jama Pediatr. 2017; 171(8):771–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].US Department of Health and Human Services. U.S. Surgeon General Releases Advisory on Alcohol Use in Pregnancy. Washington, D.C. 2005. [Google Scholar]
- [15].US Department of Health and Human Services. More than 3 million US women at risk for alcohol-exposed pregnancy. 2016. [Google Scholar]
- [16].Green PP, McKnight-Eily LR, Tan CH, Mejia R, Denny CH. Vital Signs: Alcohol-Exposed Pregnancies--United States, 2011–2013. MMWR Morb Mortal Wkly Rep. 2016; 65(4):91–7. [DOI] [PubMed] [Google Scholar]
- [17].Roberts SCM, Thompson KM. Estimating the Prevalence of United States Women with Alcohol-exposed Pregnancies and Births. Womens Health Issues. 2019; 29(2):188–93. [DOI] [PubMed] [Google Scholar]
- [18].National Center for Health Statistics (NCHS). 2013–2015 National Survey of Family Growth Public Use Data and Documentation. Hyattsville, MD: CDC National Center for Health Statistics; 2016. Available from: https://www.cdc.gov/nchs/data/nsfg/nsfg_2013_2015_userguide_maintext.pdf [Google Scholar]
- [19].Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod. 2003; 18(9):1959–66. [DOI] [PubMed] [Google Scholar]
- [20].Li D, Wilcox AJ, Dunson DB. Benchmark pregnancy rates and the assessment of post-coital contraceptives: an update. Contraception. 2015; 91(4):344–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)--explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013; 16(2):231–50. [DOI] [PubMed] [Google Scholar]
- [22].Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006; 38(2):90–6. [DOI] [PubMed] [Google Scholar]
- [23].Hanson JD, Nelson ME, Jensen JL, Willman A, Jacobs-Knight J, Ingersoll K. Impact of the CHOICES Intervention in Preventing Alcohol-Exposed Pregnancies in American Indian Women. Alcohol Clin Exp Res. 2017; 41(4):828–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ingersoll KC Sherry; Hettema Jennifer E.; Farrell-Carnahan Leah; Penberthy J. Kim. Preconceptional motivational interviewing interventions to reduce alcohol-exposed pregnancy risk. J Subst Abuse Treat. 2013; 44(4):407–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Centers for Disease Control and Prevention. The 6|18 initiative: Prevent Unintended Pregnancy 2015. Available from: https://www.cdc.gov/sixeighteen/docs/6-18-evidence-summary-pregnancy.pdf
- [26].Shackleton N, Jamal F, Viner RM, Dickson K, Patton G, Bonell C. School-Based Interventions Going Beyond Health Education to Promote Adolescent Health: Systematic Review of Reviews. J Adolesc Health. 2016; 58(4):382–96. [DOI] [PubMed] [Google Scholar]
- [27].Perry CL, Williams CL, Komro KA, Veblen-Mortenson S, Stigler MH, Munson KA, et al. Project Northland: long-term outcomes of community action to reduce adolescent alcohol use. Health Educ Res. 2002; 17(1):117–32. [DOI] [PubMed] [Google Scholar]
- [28].Skara S, Rohrbach LA, Sun P, Sussman S. An evaluation of the fidelity of implementation of a school-based drug abuse prevention program: Project Toward no Drug Abuse (TND). J Drug Educ. 2005; 35(4):305–29. [DOI] [PubMed] [Google Scholar]
- [29].Ingersoll KS, Ceperich SD, Nettleman MD, Karanda K, Brocksen S, Johnson BA. Reducing alcohol-exposed pregnancy risk in college women: Initial outcomes of a clinical trial of a motivational intervention. J Subst Abuse Treat. 2005; 29(3):173–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Delrahim-Howlett K, Chambers CD, Clapp JD, Xu R, Duke K, Moyer RJ 3rd, et al. Web-based assessment and brief intervention for alcohol use in women of childbearing potential: a report of the primary findings. Alcohol Clin Exp Res. 2011; 35(7):1331–8. [DOI] [PubMed] [Google Scholar]
- [31].Ceperich SD, Ingersoll KS. Motivational interviewing plus feedback intervention to reduce alcohol-exposed pregnancy risk among college binge drinkers: determinants and patterns of response. Journal of Behavioral Medicine. 2011; 34(5):381–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Project CHOICE Intervention Research Group. Reducing the risk of alcohol-exposed pregnancies: a study of a motivational intervention in community settings. Pediatrics. 2003; 111(5 Pt 2):1131–5. [PubMed] [Google Scholar]
- [33].Floyd RL, Sobell M, Velasquez MM, Ingersoll K, Nettleman M, Sobell L, et al. Preventing alcohol-exposed pregnancies: a randomized controlled trial. Am J Prev Med. 2007; 32(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Farrell-Carnahan L, Hettema J, Jackson J, Kamalanathan S, Ritterband LM, Ingersoll KS. Feasibility and promise of a remote-delivered preconception motivational interviewing intervention to reduce risk for alcohol-exposed pregnancy. Telemed J E Health. 2013; 19(8):597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Schölin L Prevention of harm caused by alcohol exposure in pregnancy -- Rapid review and case studies from Member States: World Health Organization; 2016. [Google Scholar]
- [36].Alvik A, Haldorsen T, Groholt B, Lindemann R. Alcohol consumption before and during pregnancy comparing concurrent and retrospective reports. Alcohol Clin Exp Res. 2006; 30(3):510–5. [DOI] [PubMed] [Google Scholar]
- [37].Hanson JD, Nelson ME, Jensen JL, Willman A, Jacobs-Knight J, Ingersoll K. Impact of the CHOICES Intervention in Preventing Alcohol-Exposed Pregnancies in American Indian Women. Alcohol Clin Exp Res. 2017; 41(4):828–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Trussell J Contraceptive failure in the United States. Contraception. 2011; 83(5):397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Centers for Disease Control and Prevention. Effectiveness of Family Planning Methods. https://www.cdc.gov/reproductivehealth/unintendedpregnancy/pdf/contraceptive_methods_508.pdf [Accessed: June 1, 2020] 2011.
- [40].Curtin SC, Abma JC, Kost K. 2010 pregnancy rates among U.S. women. NCHS health e-stat. 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.