Abstract
Objectives
This paper presents an overview of the vaccination campaigns in France, Israel, Italy and Spain during the first eleven months from the first COVID-19 vaccine approval (Dec 2020 - Nov 2021). These four countries were chosen as they share similar socioeconomic, and epidemiological profiles and adopted similar vaccination strategies.
Methods
A rapid review of available primary data from each country was conducted. Data were collected from official government documents whenever possible, supplemented by information from international databases and local reports. The data were analysed via descriptive and graphical analysis to identify common patterns as well as significant divergences in the structural changes of countries’ healthcare systems during the pandemic, outcomes of the vaccination roll-out, and their impact on contextual policies.
Results
The four countries adopted similar interventions to protect and strengthen their healthcare systems. The effective coordination between the governance levels, ability to ensure a large supply of doses, and trust towards health authorities were amongst the determinants for more successful vaccination outcomes. The analysis reports a positive impact of the COVID-19 vaccines on epidemiological, political and economic outcomes. We observed some evidence of a negative association between increased vaccine coverage and fatalities and hospitalisation trends.
Conclusions
The strengths and weaknesses of COVID-19 pandemic crisis management along with the various strategies surrounding the vaccination roll-out campaigns may yield lessons for policymakers amidst such decisions, including for future pandemics.
Lay summary
This paper presents an overview of the vaccination campaigns in France, Israel, Italy and Spain during the first eleven months following approval of the first COVID-19 vaccine (Dec 2020 - Nov 2021). These four countries were chosen as they share similar demographic, socioeconomic, and epidemiological profiles, and adopted similar vaccinations strategies. Effective coordination between governance levels, ability to ensure a large supply of doses, and trust towards health authorities were amongst the determinants for successful outcomes of vaccination campaigns. The strengths and weaknesses of COVID-19 pandemic crisis management, along with the various strategies surrounding the vaccination roll-out campaigns may yield lessons for policymakers amidst such decisions, including for future pandemics.
Keywords: COVID-19, Vaccines, Health financing, Health policy, Pandemic, Health outcomes
Introduction
The first case of COVID-19 in Europe was confirmed in France, Italy and the Canary Islands in late January 2020, and in Israel at the end of February that year. Differences in policy responses between countries in terms of stringency and fiscal stimuli have been well documented [1], [2], [3]. By the summer of 2020, a new phase in the policy response to COVID-19 became viable when effective vaccines became a realistic possibility. Vaccine programmes offered policymakers the possibility of switching to proactive rather than reactive responses to the pandemic. In France, Italy, Spain, and Israel, more than 60% of the total population was fully vaccinated by 30th September 2021 [4].
As well as sharing the northern Mediterranean coastline, France, Italy and Spain share similar demographic, socioeconomic, and epidemiological profiles. These countries also experienced a significant first wave of COVID-19 infections in the first half of 2020. Similar socioeconomic and epidemiological profiles are also shared by Israel, although the country presents a younger (and smaller) population and was not impacted as greatly during the first COVID-19 wave. Despite such differences, we include Israel in our analysis as it has been considered to be an international benchmark for its efficiency and effectiveness in the vaccination roll-out [5, 6]. Arguably, its experience influenced vaccination campaigns worldwide, including in France, Italy and Spain. Indeed, Israel has been the pioneer country in the vaccination campaign strategy (including vaccine boosters), in the implementation of policy tools to incentivise vaccination (e.g. the Green Pass) [7], and in the production of scientific evidence on vaccine effectiveness over time [8]. While all four countries were relatively successful with their vaccination roll-out, each has chosen different strategies to encourage uptake. These differences are not only the consequence of political decisions, but they also depend on the epidemiological impact of COVID-19 in the country, organisation of the healthcare system (e.g. traditional insurance vs managed care), institutional features (e.g. central vs federal or regional governments), and demand (e.g., people willing to be vaccinated vs hesitant) and supply factors (e.g., number of vaccine centres, doses available, personnel, etc.) [9]. This paper sets out to synthesise evidence about the economic and institutional factors that contributed to the roll-out of COVID-19 vaccines between countries, and how these might have been affected by contextual issues specific to or common across countries. A comparison of campaigns and the identification of the key determinants that have led to successful strategies may inform cross-country policy learning, and set a benchmark for future COVID-19 waves and impending public health crises.
The need for policy improvements is pressing because a large share of the world's population remains unvaccinated, and recent scientific evidence shows a waning of the immune response over time [10]. Because of this, many countries have announced vaccine booster campaigns for their populations (most notably, Spain, France and Italy) following the example of Israel. Given that an efficient vaccination campaign is key to preventing the development of a more virulent variant and plays an important role in reducing the stringency of other public health measures such as social movement restrictions, it is important to analyse the success of vaccine campaigns. We aim to identify the similarities and differences between vaccination programs and strategies in parallel with other stringency measures for pandemic containment. In addition, we aim to highlight the role that the structure and financing of health care systems played in designing the vaccination programs.
A rapid review of available primary data from each country was conducted. Data sources included country official institutional websites and legal sources (e.g., Governmental agencies, Ministries of Health, National Research Institutes, etc.), supplemented by information from international databases (e.g., Our World in Data, John Hopkins, etc.) [4, 11]. The data was then analysed to identify common patterns and significant divergences in; the structural changes of countries healthcare systems during the pandemic; the vaccination roll-out across countries and its relationship with COVID-19 health outcomes including hospitalisations and number of daily fatalities; and governmental policy responses (e.g. stringency and socio-economic factors).
Graphical analysis was performed to investigate the vaccination roll-out and its relationship with COVID-19 health outcomes, policy responses and socioeconomic factors. Specifically, we compared the share of people partially and fully vaccinated against the case fatality rate, the ICU saturation rate, the strictness of the policies implemented and the unemployment rate. We use the stringency index included in the Oxford Covid-19 Government Response Tracker (OxCGRT) [12] to measure the stringency of the policies adopted. We conclude the analysis by investigating whether the health impacts of the COVID-19 pandemic may have influenced the willingness of the population to be vaccinated across countries. We used the number of deaths per 100,000 inhabitants at the regional level to report the health impact of COVID-19, whilst the willingness to get the vaccine was reported as the proportion of fully vaccinated people (%) in each region. We described the relationship in two steps: firstly, we used a graphical analysis to identify the direction and relevance of the relationship; secondly, we estimated the degree to which the two metrics are correlated.1
The paper is structured as follows: section two describes the four countries profiles including demographic, epidemiological, and healthcare system data. Organisational changes promoted to cope with the COVID-19 pandemic were also noted. Section three provides an overview of the vaccination programs across the four selected countries. Section four reports the results of our graph and descriptive analysis. In section five we discuss our findings and present our conclusion.
The economics of the COVID-19 journey: supply and demand-side
To understand the similarities and differences in vaccination strategies adopted by each country, we describe the features of each in terms of health care demand and supply and how these features evolved in response to the pandemic outbreak.
Health systems overview
Both the Italian and Spanish healthcare systems are highly decentralized and managed at a regional level. The Italian healthcare system funding is pooled at the national level and distributed to the twenty regions that are autonomous in their financing, provision and governance [1]. Likewise, the Spanish national health system provides universal healthcare through 17 Autonomous Communities. These Autonomous Communities are responsible for managing the health system, coordinating the provider networks and purchasing resources [2]. In both countries, the regions enjoy significant autonomy in determining the macrostructure of their health systems. Israel has a national health insurance system that provides for universal coverage where all Israeli citizens or residents are free to choose between four competing, non-profit-making Health Maintenance Organizations, known as health plans (HPs). Israel has a unitary system of governance; the ultimate source of authority is at the national level. The regions serve primarily to implement the policies and strategies developed at the national level [5]. France has statutory health insurance (SHI) with state-led centralized system governance and limited delegation to the regions. The national public health institution (Santé Publique) sets national health strategies and directs regional health agencies to implement their chosen measures [3].
Demand factors
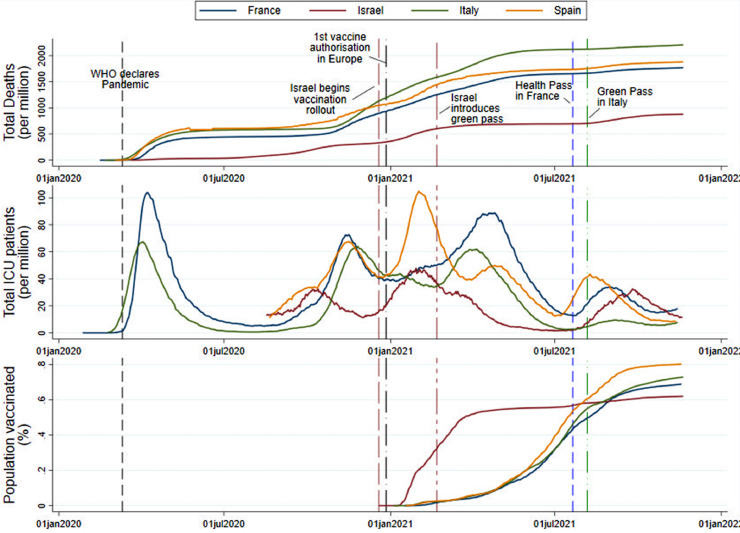
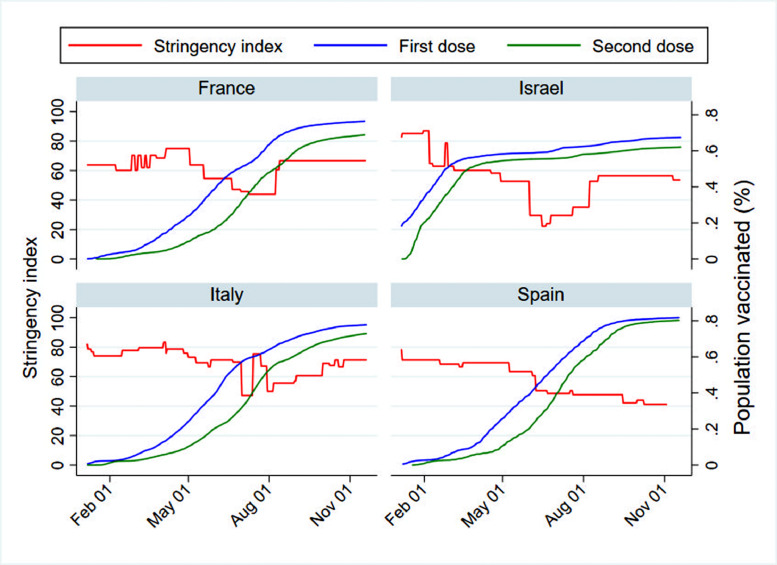
During the first year of the pandemic Italy, Spain, and France were amongst the countries most severely affected by COVID-19 in terms of fatalities and ICU hospitalisations. The rapid spread of the virus conditioned the stringency of the measures in the entire population in these three countries to alleviate the pandemic burden on the health system [1], [2], [3]. Conversely, Israel did not face the initial pressure on ICU hospitalization or the elevated pandemic mortality compared to the three countries (see Fig. 1 ). However, Israel proactively enforced an early aggressive containment strategy which in turn has delayed the viral infection spike for several weeks compared to the European countries [13].
Fig. 1.
Epidemiological trend and vaccination rollout in France, Israel, Italy and Spain.
Note: The fully vaccinated population represents the population that received the full cycle of the vaccine before the introduction of the booster. The share of the population vaccinated is based on the total population in each country. Accordingly, the percentage of fully vaccinated in Israel can be downward biased due to a relatively larger share of the young population that is currently ineligible for the COVID-19 vaccines.
Source: Authors’ analysis on data retrieved by Our World in Data [4].
Reasons for the diverse impact of COVID-19 and the consequent demand for health care may be partially attributed to socioeconomic and demographic factors (Table 1 ). Compared to the three European countries Israel has a smaller and younger population. The median age in Israel is 30.4 years, while in all the other countries is above 40 years [14]. Similarly, the overall proportion of the population above 65 years of age is above 20% in France, Italy and Spain, while in Israel is only 12%. This demographic difference may partially explain the higher mortality and hospitalisation burden faced by the three European countries compared to Israel as increasing age is associated with an increased risk of hospitalisation and death following COVID-19 infection [15]. However, Israeli inhabitants are distributed on a small geographical landmass with a high-density population ratio of 400 people per Km2. The high population density could be a risk for increased viral transmission rate and likelihood of widespread community transmission and infection. An additional risk factor to consider is the morbidity of the population. Israel and Spain present the highest share of population with two or more chronic conditions.
Table 1.
Demand factors in France, Israel, Italy and Spain.
| Italy | Spain | France | Israel | |
|---|---|---|---|---|
| Population [14, 16, 17] | 59,258,000 (2021) | 47,394,223 (2021) | 68,084,217 (2021) |
8,787,045 (2021) |
| Density people/Km2 [14] | 196 (2021) | 94 (2020) | 119 (2020) | 400 (2020) |
| Median age [14] | 47.3 years (2020) | 44.9 years (2021) | 41.7 years (2021) |
30.4 years (2021) |
| Life expectancy at birth [14] | 84 years (2021) |
83.9 years (2021) | 82.4 years (2021) | 83.1 years (2021) |
| People over 65 years old (%) [18] | 23.3 (2020) | 20 (2020) | 20.5 (2020) | 12 (2020) |
| Old age dependency ratio [18] | 36.6 (2020) | 30.4 (2020) | 33.7 (2020) | 20.8 (2020) |
| People living with 2 or more chronic conditions (%) [2, [19], [20], [21]] | 21 (2019) | 30 (2019) | 18 (2016) | 27.3 (2015) |
| Diabetes I and II prevalence (rate per 100,000) [22] | 11,408 (2019) | 10,605 (2019) | 5,011 (2019) | 5,917 (2019) |
| GDP per capita (USD) [23] | 41,492 (2020) | 38,335 (2020) | 46,442 (2020) | 41,859 (2020) |
| Unemployment rate (Q2–2021) (% of labour force) [24] | 9.8 | 15.3 | 8.2 | 5.3 |
| Years to return to pre-pandemic employment-rates (Q4–2019) [25] | 2.75 | NR | 2.75 | 5.2 |
Lastly, each country shares a similar elevated socioeconomic standard in terms of employment rate, elevated GDP per capita and generally high standard of care. This affords the funding of health resources and paves the way for rapid and successful pandemic containment plans.
Supply factors
To cope with the increased demand for health care and the potential saturation of the hospital system, a parallel increase in the supply side was observed (Table 2 ). The available data shows a common trend across the four countries, particularly in the investments supporting the intensive care services and equipment (e.g. ventilators). The highest increase was noted in Spain, where the government increased substantially the number of ICU beds per 100,000 by 93% (from 9.7 to 18.7 ICU beds per 100,000) in 2020 followed by a second increase of 23% in 2021 (from 18.7 to 23 ICU beds per 100,000) [26]. The French government also substantially increased ICU beds by 45%, introducing temporary ICU beds to cover the shortage caused by the pandemic. Similar trends in the intensive care service were seen in Italy and Israel, which both almost doubled their ICU bed capacity [27].
Table 2.
Change in supply factors before and after the COVID-19 pandemic.
| Italy | Spain | France | Israel | |||||
|---|---|---|---|---|---|---|---|---|
| Type of system [31] | National Healthcare System (NHS) |
National Healthcare System (NHS) | Statutory Health Insurance (SHI) |
National Health Insurance (NHI) |
||||
| Hospital beds per 100,000 [28, [32], [33], [34], [35]] | 320 (2019) | +60%* (2020) | 290 (2019) | NA | 580 (2019) | 574 (2020) | 290 (2019) | 290 (2020) |
| ICU beds per 100,000 [[26], [27], [28], 34, 36] | 8.7 (2019) | 11 (2020); 15 (2021) | 9.7 (2017) | 18.7 (2020); 23 (2021) | 8 (2019) | 14.6 (2020) | 8 (2019) | 12 (2021) |
| Number of doctors per 100,000 [29, 37] | 400 (2019) | +21,414 (2020–21) | 440 (2019) | NA | 340 (2019) | 339 (2020) | 319 (2019) | 319 (2020) |
| Specialists’ doctors per 100,000 [38, 39] | 318 (2019) | NA | 261 (2019) | NA | 185.4 (2019) | NA | NA | NA |
| Nurses per 100,000 [28], [29], [30] | 670 (2019) | + 31,990 (2020–21) | 590 (2019) | NA | 1,070 (2019) | 1,136 (2021) | 500 (2019) | 589 (2020) |
| Hospitals per 100,000 [29, 40] | 1.8 (2019) | NA | 1.6 (2019) | 1.6 (2020) | 5.8 (2019) | NA | 1 (2019) | 1 (2020) |
| Ambulances per 100,000 [28, 40, 41] | 1.9 (2019) | 2.1 (2020–21) | 6.2 (2019) | 6.4 (2020) | NA | NA | NA | NA |
| Ventilators per 100,000 [42], [43], [44] | 31 (2019) | 41 (2020); 42(2021) | 12 (2019) | 29 (2020) | NA | NA | 50 (2019) | 57 (2020) |
Note: * the increase is related to internal beds only. NA: data not available at the time of writing.
From the available data, we also observe a general trend in reinforcing the supply of healthcare workers across the countries. For example, the Italian health system managed to increase the number of health care workers by a significant number from 21,414 doctors in 2020 to 31,990 in 2021 [28]. Israel supported its health system by increasing the number of nurses by 17% [29]. Similarly, in France, there was an incremental increase in the number of nurses by 5% [30]. It was difficult to quantify the change in supply factors in Spain due to the lack of published and updated data from the Spanish government official communications or reports. Overall, the increase in the number of health workers suggests an attempt by policymakers to alleviate pressure by providing additional workforce support.
Health financing during the COVID-19 pandemic
An unprecedented financial effort has been made by these countries to sustain the need for increased medical resources, equipment and personnel. Table 3 summarizes the change in health financing during the COVID-19 pandemic. Public and healthcare expenditure in all countries reported a marked increase compared to the pre-pandemic period. The highest impact was observed in Spain where the government expenditure increased by 24% in 2020 compared to 2019 [45]. Comparably, the increase in government spending was 18% in Italy, 16% for Israel and 12% in France [45, 46]. A substantial increase in health expenditure was also observed compared to the pre-pandemic period, in order to increase health system resilience and provide additional support for universal health coverage during the COVID 19 pandemic.
Table 3.
Health Financing before and after the outbreak of the COVID-19 pandemic.
| Italy | Spain | France | Israel | |||||
|---|---|---|---|---|---|---|---|---|
| Total general government expenditure (% GDP) [45] | 48.6 (2019) | 57.3 (2020) | 42.1 (2019) | 52.3 (2020) | 55.4(p) (2019) | 62.1(p) (2020) | 39.9 (2019) | 46.4 (2020) |
| Health expenditure (% GDP) [46, 47]* | 8.7 (2019) | 9.7 (2020) | 9.3 (2019) | NA | 11.2 (2019) | NA | 7.6 (2019) | 8.5 (2020) |
| Spending for inpatient and curative care (% GDP) [45, 46] | 2.3 (2019) | NA | 2.3 (2019) | NA | 3 (2018) | NA | 1.7 (2019) | 1.8 (2020) |
| Investments in health (annual public budget - (million)) [46, [48], [49], [50]] | 113,810 (Euro) (2020 - pre pandemic) | 117,407 (2020); 121,370 (2021) | 115,458 (Euro) (2019) | NA | 260,247 (Euro) (2019) |
200,924 (Euro) (2020); 260,247 (Euro) (2021) |
107,411 (NIS) (2019) | 118,053 (NIS) (2020) |
| Investments in equipment (e.g. ambulance, ventilators, tests, etc.) (million) [28, 46, 50] | 6,404 (Euro) (2019) \ | 6,842 (Euro)(2020) | 9,045 (Euro) (2019) |
NA | 41,994 (Euro) (2020) |
49,994 (Euro) (2020); 100,294 (Euro) (2021) |
4,201 (NIS) (2019) |
4,555 (NIS) (2020) |
Note: * The figures for the health expenditure as the% of the GDP are retrieved from the OECD database [47] for easiness of comparison across countries. In France the official report from the Ministry of Solidarity and Health reports that in 2019 the health expenditure was equal to 8.6% of the GDP, while in 2020 it was 9.1% [51]. (p): provisional.
Vaccination programs and population preferences
Objectives and metrics for the design of vaccination roll-out strategies
The four countries shared common objectives in their vaccination strategies [52]. The common goal was the reduction of virus-caused morbidity and mortality while prioritizing the most vulnerable groups and ensuring vaccine safety. The metrics observed in relation to the campaigns and the prioritization strategies were also similar and mainly related to the availability of the doses in each country. In the initial phase, a limited number of doses were available, thus the strategy was based on the prioritization of elderly, high-risk individuals with comorbidities, and virus-susceptible individuals (e.g., health workers and caregivers) [5, 53].
On the 6th of January, Israel was able to secure all doses needed for the vaccination of the adult population by signing an agreement with Pfizer, immediately after the FDA granted conditional approval [5]. The doses were supplied, in exchange for, amongst other things, epidemiological data relevant to the assessment of vaccine safety and efficacy. On the 17th of June 2020, the European member states joined the EU Vaccine Strategy scheme to increase the development, manufacturing and deployment of vaccines against COVID-19. The EU member states also carried out negotiations with vaccine manufacturers and agreed to organize a joint procurement process resulting in a single vaccine price for all members [52]. During the first phase of the vaccine roll-out, supply problems led to a temporary reduction in deliveries. For instance, Italy suffered a 29% loss in volume supply from the 18th of January to the 1st of February, with some regions reaching up to a 60% loss of supply. Similarly, the Spanish capital of Madrid stopped vaccinating the healthcare workforce during some periods because of a 50% supply loss [54]. The limited supply was partially addressed with the rapid approval of new vaccines in January 2021 (i.e. AstraZeneca) and March 2021 (Johnson&Johnson) [55]. The approvals of these alternative vaccines allowed them to overcome vaccine shortages and plan the vaccination of specific groups, such as essential workers and care personnel [53, 56].
The issue of vaccine scarcity was further exacerbated in mid-March 2021 when France, Italy and Spain reacted to the rare adverse event related to the AstraZeneca vaccine called thrombosis with thrombocytopenia syndrome (TTS). In line with other nations, the three European countries temporarily paused the use of this vaccine [57]. Shortly after the stoppage, the EMA launched safety guidance deeming the vaccine safe and effective. France and Italy resumed vaccinations while Spain excluded some demographic groups to minimize risks [58]. A significant turning point in the ability of the three European countries to improve the vaccination roll-out has been the increased production capacity for BioNTech/Pfizer's and Moderna's mRNA vaccines. New manufacturing sites and more flexible storage conditions for BioNTech/Pfizer significantly boosted the vaccine roll-out campaigns [59].
The issues faced with vaccine supply, the early procurement agreements, as well as the different effectiveness of the vaccines in protecting against the virus influenced the proportion of the various vaccine type in relation to the total vaccine supply (see Table 4 ). As of the 18th of November 2021, BioNTech/Pfizer´s vaccine was the most widely used in all four countries, whilst Moderna and AstraZeneca´s vaccines held somewhat smaller proportions in the European countries. In Israel, BioNTech/Pfizer´s vaccine represents almost 100% of the doses inoculated, while a very small amount of Moderna vaccines have been administered. On the 21st October 2021, Israel made the Astrazeneca vaccine available for those unable to receive a shot based on the mRNA technology used in the Moderna and Pfizer's vaccines [60]. Johnson&Johnson´s vaccines were used in much lower proportions in all countries [4].
Table 4.
Vaccine distribution by manufacturing companies as the 18th of November (including booster doses).
| BioNTech/Pfizer | AstraZeneca | Moderna | Johnson&Johnson | |
|---|---|---|---|---|
| France | 80.27% | 7.63% | 11.08% | 1.03% |
| Italy | 72.64% | 13.07% | 12.69% | 1.61% |
| Spain | 70.46% | 14.06% | 12.64% | 2.84% |
| Israel | 99.8% | NA† | 0.2% | – |
Note: †data not available at the time of writing due to the recent introduction in the country.
The higher proportion of vaccines based on mRNA technology across countries is likely to increase further with booster campaigns that started on the 1st of August 2021 in Israel and mid-September in France, Italy and Spain. All of these countries are currently using mRNA technology to boost immune protection even for individuals who originally received AstraZeneca or Johnson&Johnson vaccines.
Governance and organisation of the vaccination campaign
In Italy and Spain, the vaccination program was the result of a joint effort between the central governments, the medical government agencies and the National Research Institutes, with the regional governments committed themselves to push forward the drive for vaccination and the logistics [61, 62]. In France, vaccine deployment was centralized as a collaboration between the Ministry of Health, Public France, and the operational management of logistics, which guarantees the quality of vaccines throughout the logistic chain [63]. More than 500 vaccinations centres were established in France by the end of January 2020 [64]. In Israel, the central government via the Ministry of Health managed the purchase of the vaccines. Upon arrival, vaccines are stored in one central facility that is located near the international airport and in the centre of the country servicing all Health Plans across the country. The Health Plans set up massive vaccinating centres and top-notch information systems that enabled efficient and fast queue management [5]. Additionally, the Ministry of Health, in collaboration with the Health Plans have launched campaigns to encourage immunization.
Success factors for the vaccination strategy
There were several reported reasons behind the success of each country in achieving a high rate of vaccination in such a relatively short period compared to other countries.
The success of the Spanish vaccination strategy has been attributed to three primary factorsː trust in the public health system, unbureaucratic distribution of vaccines, and strong recollection of the high death toll and infection rate during the first COVID-19 waves. The National Health system's institutions and health professionals are more highly trusted than other institutions or professional groups in the country [65].
The success of the Italian vaccination strategy was attributed to effective governance that involved all relevant stakeholders together with efficient and flexible logistics [61]. The vaccine distribution and administration were administered through a hub and spoke model, with one main hub and series of second-level territorial centres. The organization of the vaccination centres was managed at the regional level with specified guidelines on how to set up, equip and manage special local vaccination points, which in turn accelerated the dissemination of vaccine capacity [66]. In conclusion, despite the initial delay and weakness of the digital vaccine booking platforms at the regional level the central government and regions worked to overcome such issues by either strengthening regional digital platforms or utilizing a new centralized system built by the government and the Italian post [67].
In France, efficient coordination between the health authorities (i.e., Haute Autorité de Santé, Santé Publique France and the French Ministry of Health), and the effective monitoring of the vaccination progress were key determinants for the successful roll-out [68]. Additionally, the French government was able to enhance vaccine deployment by assuring a steady vaccine supply by involving more professionals and diversifying the profile of vaccinators to speed up the vaccination campaign [69].
Rosen et al. [5] pointed to three main factors in the successful vaccination campaign in Israel: vaccine supply, deployment capabilities and vaccination willingness. The Israeli campaign included rapid expansion of vaccination eligibility due to increased availability of vaccine supply, rapid deployment by the four Health Plans, and high demand rates amongst the older population.
Vaccine hesitancy
Despite the high acceptance rate demonstrated by the success of the high coverage of the population, some differences in the perception of the vaccines can be noted across countries. France and Italy faced significant vaccine hesitancy in their populations, while Israel and Spain's acceptance was relatively high.
A systematic literature review showed general vaccine acceptance rates as low as 53.7% in Italy and 58.9% in France [70]. The lack of confidence in the safety of these vaccines can be explained by the increased vaccine hesitancy observed over the last decade. Both Italy and France experienced a resurgence of measles cases in 2017/18 as a direct result of the growing vaccine hesitancy in their populations [71, 72]. To tackle this issue, both governments introduced a law making a number of vaccines mandatory (10 in Italy, 11 in France) for all individuals below the age of 16 [73, 74]. When COVID-19 vaccines became available in France, more than one-quarter of healthcare workers were either hesitant (23%) or reluctant (4%) to be vaccinated [75]. France was amongst the European countries that faced public resistance against massive vaccination campaigns [76]. In Israel, the initial rollout of the vaccine was successful in terms of the pace of vaccination. At the same time, within a few weeks it became clear that while the rate of vaccination in the general population was high, the rate of vaccination in Arab and ultra-Orthodox communities (21% and 13% of the population respectively) was substantially lower [5]. When looking at data regarding other vaccines (Influenza and HPV), it seems that the immunization rate amongst the Arab community in Israel is even higher than the general population [77]. In contrast, lower rates of childhood vaccinations amongst some groups within the ultra-Orthodox Jewish community have been described in other studies [78]. The concealment of some details of the purchase agreement with Pfizer may have also contributed to a decline in public confidence in government policy around the vaccine [79].
Conversely, in Spain, the phenomenon of vaccination hesitancy was limited. The social value and personal benefit of being vaccinated were the guiding principles in Spain's vaccination strategy left a little room for distrust or hesitancy. According to the Evolution of Social Perception of Scientific Aspects of COVID-19 survey conducted by the Spanish Institution for Science and Technology, in July 2020, 32% of the population expressed full confidence in the vaccination as soon as the vaccine would be offered by health authorities. This number increased to 58% in January 2021 and has reached 83% in May 2021 [80].
The adverse events associated with the AstraZeneca vaccine and the miscommunication surrounding it played a critical role in regard to countries vaccination hesitancy rates. In fact, the Eurofound survey revealed that vaccine hesitancy increased after the pause in the use of AstraZeneca as a result of safety fears driven by weak and unconvincing communication [81].
Incentives and penalties to increase vaccine uptake
The four countries each implemented a system of rewards and penalties to increase vaccine uptake and combat vaccine hesitancy. amongst these measures, a distinction between (dis)incentives and mandates needs to be made. In this case, mandates refer to a legal obligation to be vaccinated for specific groups of the population, while (dis)incentives refer to any financial, social and economic measures adopted by governments to increase vaccine uptake voluntarily. Whilst all countries opted to pursue incentive mechanisms to increase vaccine uptake, such as banning unvaccinated people from eating indoors at restaurants or accessing clubs or public events, governments different in the introduction of strict vaccination mandates for certain subgroups of their population. Spain was the only country amongst them that did not introduce any mandates, a difference which may reflect the diverse acceptance rate between countries.
The Italian government issued a compulsory vaccination mandate for all doctors, dentists and health professionals in April 2021 (the first country in Europe to do so) [53, 82] and imposed a health certificate (i.e., Green Pass) for vaccination status or negative swab test results (the validity of the Green Pass with the swab test is 48 h) to access public and private venues in August 2021 [83]. On September 16th, the Italian government included an additional requirement for the Green Pass certificate to be mandated in all private and public workplaces starting from the 15th October [84]. After this date, workers without a valid Green Pass were considered to be unjustifiably absent, and were not paid for each day of absence. Moreover, workers who were not vaccinated, but planned to use the Green Pass with a negative swab test result were required to bear the financial cost of the swab test (i.e. 15 Euros). The effect of this mandate has not yet been fully evaluated. In the third week of September, the daily number of first doses of vaccine increased from 50,000 to 70,0000, reaching about 80,000 in the week between the 20th and 26th September. The figures remained stable for a few days and then return to 50,000 daily administrations between the 3rd and 10th October. The number of first doses fell below 20,000 daily administrations in the last week of October. On the 20th of November, 87% of the eligible population had received at least one dose of a vaccine. Whilst the effectiveness of the mandate in Italy is still to be evaluated, its use raises important ethical and political considerations. Additionally, there is the need to assess whether this measure is cost-effective. Indeed, if the size of the working population without a Green Pass is significant (and this may change with the introduction of a booster mandate for the general population), the mandate might create spillover effects on the supply chain and productivity, ultimately harming the economic stability of the country. Despite these concerns, on the 24th of November the Italian government approved a new decree which strengthens the Green Pass requirement by introducing an additional certificate, defined by the media as “Super Green Pass” [85]. This new pass, which is complementary to the basic one, will come into force on 6 December and can be obtained only by individuals who have been vaccinated or have recovered from COVID-19 in the previous six months. It will guarantee access to shows, sporting events, indoor bars and restaurants, parties and discos, and public ceremonies, even in those areas where new restrictions on social activities will be implemented. The basic Green Pass will still be sufficient to access workplaces. The decree also imposes the booster requirement for healthcare workers, army and teaching personnel.
Israel also required the Green Pass in an early stage of the vaccination campaign (18th of February 2021) and unvaccinated individuals (including children too young to be vaccinated) were required to present a negative PCR/antigen test as a condition of entry to social and other public places [79]. At the same time, the government declared that the goal was to keep the economy open and to prevent further lockdowns. On October 3, two months after the booster dose vaccination campaign and given the relatively high avoidance rates from the population, the government adjusted the requirements to possess a valid Green Pass. Vaccinated people who received only two vaccine doses over 6 months ago will lose their Green Pass and will be denied access to many places (universities, places of entertainment, teachers in the education system and sports centres). Those whose vaccination is not valid (and individuals who are medically prevented from receiving the vaccine) can obtain a temporary Green Pass, valid for 24 h, if they perform a PCR/antigen test at their expense [86].
The French government enforced two important mandates: compulsory vaccination for selected groups and the Health Pass. The Health Pass is a QR code that allows only those who were fully vaccinated, or had a negative COVID-19 test result, into entertainment facilities and long-distance public transportation [87]. On the 9th of November, the French President announced new vaccination requirements for those aged 65 and older as a response to the rise in the number of infections in the country [88]. Starting from the 15th of December, the Health Pass will be no longer valid for this age group if they have not received the booster dose.
Spain was one of the first countries to introduce the EU Digital COVID Certificates to facilitate safe mobility and movement between EU member states [89]. However, in line with the Constitution and the low hesitancy in the country, the government protected the voluntariness of the individual to get the vaccination. Accordingly, no mandates to get the COVID certificate are in place in the county. The only two exceptions were the Autonomous Communities of Galicia and Balearic Islands that authorized, with the endorsement of their respective Supreme Courts of Justice, the requirement of the EU Digital COVID Certificate to enter nightclubs from the 8th of October 2021 [90].
Graphical analysis
Epidemiological outcomes
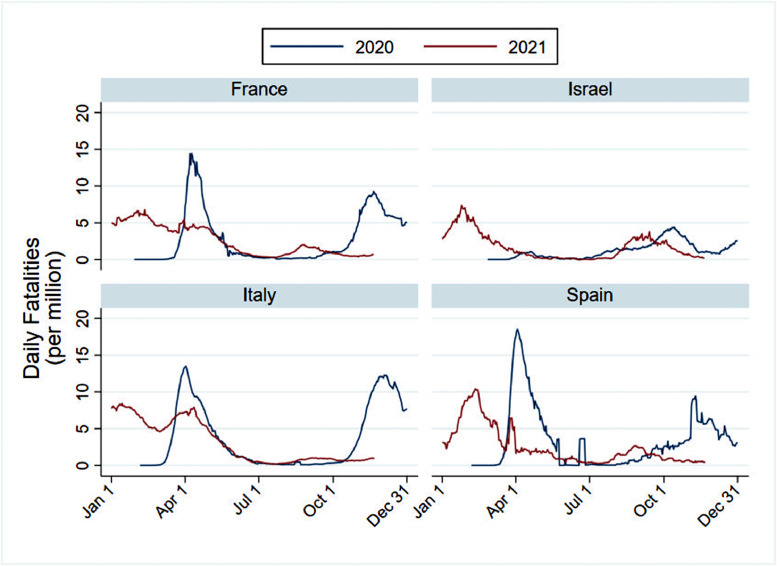
Starting with the number of deaths, we observe a common trend in all four countries, with a notably lower scale for Israel (Fig. 2 ). A marked reduction in the number of deaths is associated with the introduction of the vaccine in 2021 compared to the first quarter of 2020 when the pandemic started to display its effects. This effect is particularly visible in France, Italy and Spain. From April, the trend is opposite for France and Italy and with lower intensity in Spain. Interestingly, during the summer months (Jun – Aug), the daily trend over the last two years is almost identical, confirming the role of seasonality in the effect of the virus. An additional consideration when observing the number of deaths in the first quarter of 2021 compared to the previous year is that the lower figure can be (partly) explained by the lower number of susceptible individuals to the virus, who may have already passed away in 2020. However, the impact of the vaccines in preventing fatalities is clearly displayed after the summer months with a significant reduction in 2021 for all countries.
Fig. 2.
Distribution of fatalities before and after vaccines approval (2020 vs 2021).
Source: Authors’ analysis on data retrieved by Our World in Data [4].
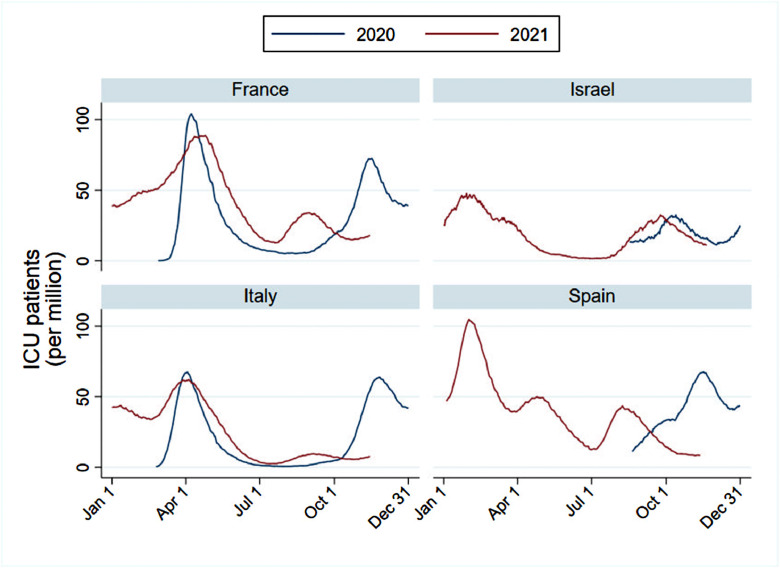
In comparing the number of ICU patients over the two years, the positive impact of the vaccine appears to be significant (Fig. 3 ). The trend In Italy and France, the two countries that report the daily data in both years, follows a similar pattern until the end of the summer, after which a marked reduction in the overall numbers is observable. In Italy, the peak of ICU hospitalisation in both years coincides but with slightly lower numbers in 2021. Whilst in France a lag effect is observable, but in this case the figures are slightly higher during the summer and September. A reason for this opaque trend observed until September can be attributed to the effect of the strict lockdowns implemented during 2020 that were relaxed during 2021 and enforced at a regional level rather than at the national one. Further, a relevant factor to consider is the willingness (or just the adherence) to comply with public health guidelines and personal hygiene measures after one year since the beginning of the pandemic and vaccines availability. Fatigue and lower risk perception might have increased risky behaviours for the virus transmission compared to 2020. This effect has been discussed in the literature [91], [92], [93]. For example, Andersson et al. [94] found a negative correlation between anticipation of COVID-19 vaccines and the willingness of individuals to comply with voluntary social distancing, adherence to hygiene guidelines, and their willingness to stay at home.
Fig. 3.
ICU admissions trend before and after vaccines approval (2020 vs 2021).
Source: Authors’ analysis on data retrieved by Our World in Data [4].
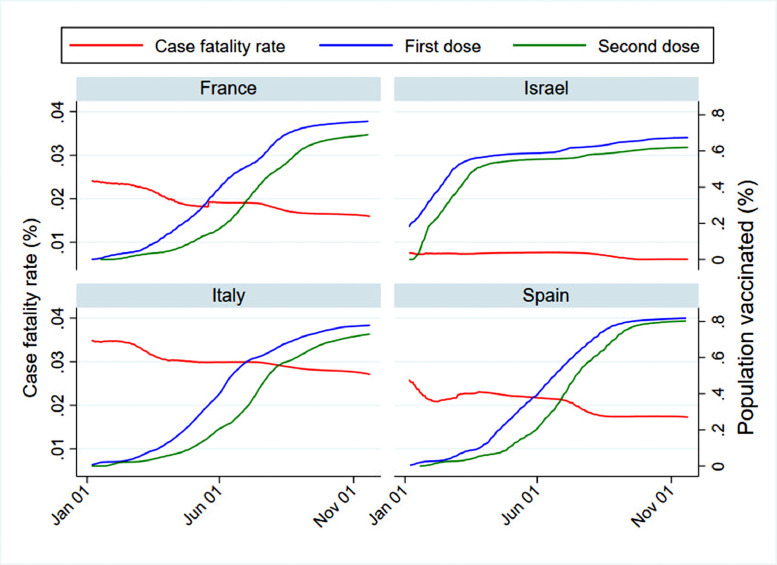
In all countries we observe a decline in case fatality as the number of fully vaccinated people increases, indicating that vaccination has a positive effect (Fig. 4 ). In France, the rate at the beginning of January was 2.5% while at the time of writing it dropped to 1.6%. Similarly, in Spain and in Italy the case fatality decreased from 2.6% to 1.7% and from 3.5% to 2.7% respectively. Israel recorded a reduction from 0.7% to 0.6% at the time of writing. This finding reinforces the evidence of the positive effect of vaccines and the role played by the intensity of the stringency and the compliance of the population in 2021 compared to the previous year.
Fig. 4.
Vaccination roll-out and case fatality rate in France, Israel, Italy and Spain.
Source: Authors’ analysis on data retrieved by Our World in Data [4].
Policy and economic outcomes
Shifting the focus from the impact of the vaccination to the stringency of the policies implemented by governments, Fig. 5 provides interesting insights on the diverse approach of the countries considered. Overall, a reduction of intensity in the social measures with the rate of people vaccinated (at least with one dose) is recorded in all countries. However, the stringency index clearly reports the tougher measures implemented in France and Italy to incentivise people to get vaccinated and fight the increasing infections. Israel presents other interesting trends. After the rapid rollout at the beginning of the year and a rate of fully vaccinated people over 60% at the end of May, the government lifted the restrictions. However, with the rise of cases during the end of the summer (August-September 2021) new restrictions were imposed. At the time of writing, the level of restrictions is at the pre-summer levels. This evidence can still be explained by the reduced compliance of individuals with voluntary protective measures, but also by the evidence of a reduction of the vaccine protection overtime (antibodies waning) [95] and the presence of a more virulent strain of the virus that requires new restrictions [96]. Consistent with this explanation and the trend observed in the figure, Israel rapidly introduced the third booster in its vaccination rollout strategy, even before the FDA approval [8]. The lower stringency implemented in Spain can be attributed to the lower hesitancy of the Spanish population to be vaccinated and high trust in the health authorities.
Fig. 5.
Comparison between the trend of vaccinated population and policy stringency (OxCGRT) in France, Israel, Italy, Spain.
Source: Authors’ analysis on data retrieved by Our World in Data [4].
The COVID-19 virus has been widely associated with negative health outcomes but also with the disruption of the global economy. In the four countries considered in this article, Spain recorded the largest GDP drop compared to 2019 with −10.8%, followed by Italy (−8,9%) and France (−7.9%), whilst Israel faced a relatively small loss (−2.1%), likely due to the lower rate of infections and deaths in the country [97]. Governments in these countries invested unprecedented resources to reduce the impact on the economy and to provide a safety net for workers who were unable to perform their activities. Vaccines are seen as the technology that can enable a return to pre-COVID-19 economic and labour market levels.
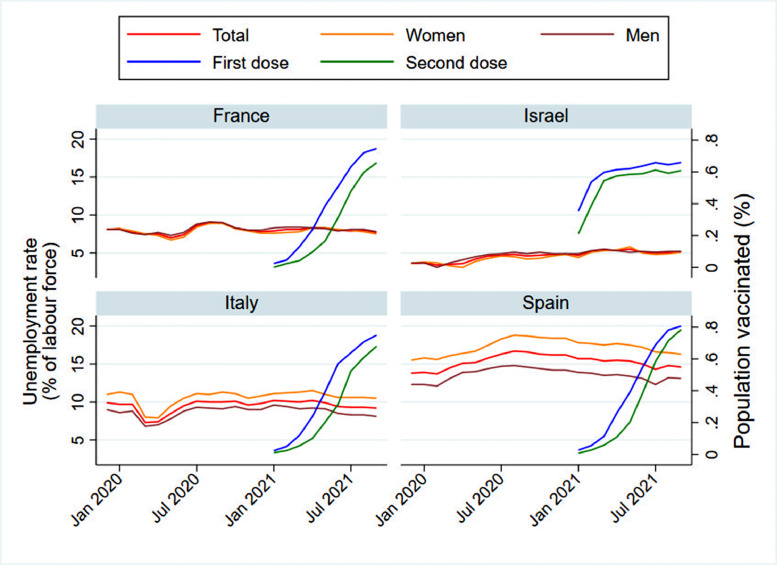
Fig. 6 reports the unemployment rates as a percentage of the total labour force and the vaccination trend in the four countries. Overall, at the time of writing, the unemployment rate in all the countries is consistent with pre-pandemic levels. Consistent with the previous trend, Israel only recorded a slight increase in the unemployment rate (4% in January 2020 versus 7% in October 2021) throughout the pandemic. The peak unemployment was recorded in March 2021 (5.4%), when the vaccination rollout was already at maximum capacity. As the levels of vaccination increase, the unemployment trend decreases and moves closer to the pre-pandemic level. On the contrary, Spain faced a much larger change in the unemployment rate (+3% at its peak), with a relatively equal impact for men and women in the labour market. Compared to Israel, the peak was reached earlier in August 2021 (16.7% overall), and a downward trend can be observed. With the introduction of vaccines beginning in January 2021, the unemployment rate returned to its pre-pandemic level (14%). France records a similar trend reaching its peak in August 2020 (9%) and with a decreasing trend over time. Looking at the Italian case, a possible divergence compared with the other countries becomes visible. The unemployment rate in March and April 2020 decreased, attributed to the reduction of the overall labour force in these months, with women exiting the market [1]. After the end of the first wave in May 2020, the unemployment rate returned to its initial levels and remained stable throughout the pandemic. Also, in Italy, we observe a decreasing trend after the introduction of the vaccine for both female and male workers.
Fig. 6.
Unemployment rate and vaccination trend in France, Israel, Italy and Spain (latest data available).
Source: Authors’ analysis on data retrieved by Our World in Data and OECD databases [4, 24].
COVID-19 experience and the willingness to get vaccinated
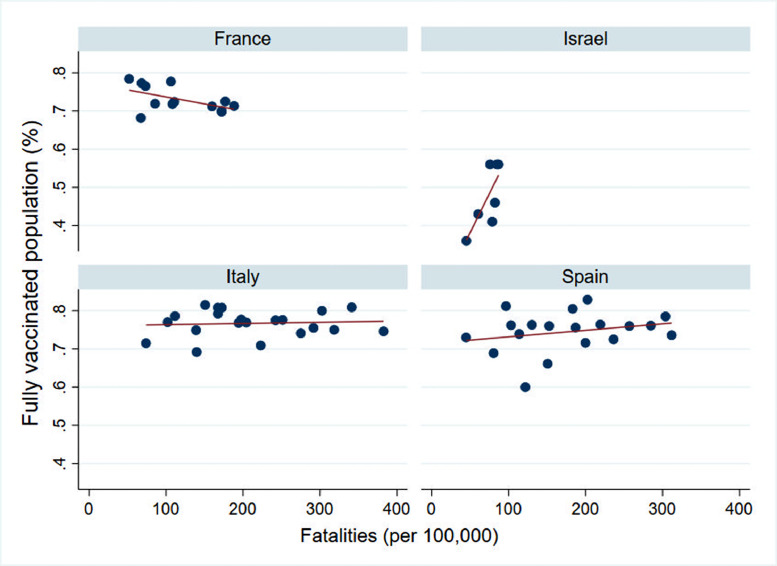
We conclude the analysis by investigating if the experience of the COVID-19 pandemic influenced the likelihood of the population to get the vaccine. Fig. 7 reports the relationship between the number of fatalities per 100,000 inhabitants and the percentage of people fully vaccinated divided by region (or district for Israel). The graphical analysis suggests a different trend in all countries. The first difference to note is that Spanish and Italian regions faced significantly more deaths than French and Israeli ones. Looking at the sign of the relationship between the two variables, France reports a clear negative relationship, showing that regions that were more severely impacted by COVID-19 had a lower percentage of people vaccinated. In Israel, Italy and Spain the relationship is positive, with a stronger effect for Israel. The Spearman's rho coefficients shed light on the sign of this relationship. For France, the Spearman's rho is equal to −0.41, but it is not statistically significant at the 95% confidence level. For Italy, the rho is equal to zero, showing no relationship between the two variables. For Spain, the rho is positive but small (0.2), and it is not statistically significant at the 95% confidence level. In conclusion, Israel reports a large Spearman's rho (0.7), but still not significant at 95% confidence level. This result is surprising because of the lower mortality rate compared with the other countries. Thus, we reject the hypothesis that previous experience with COVID-19 positively (negatively) affects the willingness to get vaccinated. However, we do notice a relevant correlation in France and Israel that might be explained by other factors, such as political, religious or social ones, that are worth further exploration as soon as more data becomes available. It is worth underlining here that the coefficients reported should be interpreted with caution. It is possible that a high mortality rate in the region led to a high rate of immunization (as might happen in Israel and Spain) or that a high rate of immunization led to a decrease in the mortality rate (as might happen in France). To overcome this potential bias, we run the analysis considering the level of cumulative deaths on the 31st of December (when the vaccination campaign was yet to commence in Europe and was at its beginning in Israel). The reported coefficients report small and not significant differences in the strength and the sign of the correlation (France −0.31; Israel 0.64; Italy 0.06; Spain 0.27).
Fig. 7.
Impact of the number of fatalities on vaccination uptake (date 26th September).
Source: Authors’ analysis on data retrieved from National Health Institutes.
Conclusions and policy implications
The availability of COVID-19 vaccines allowed policymakers to pursue policies that could prevent the spread of the virus, as opposed to more reactive policies designed to suppress infections. The success of the COVID-19 vaccination campaigns in these four countries is the result of intertwined explanatory factors related to demand and supply. These factors include: demographic aspects, economic situation, ability to secure sufficient vaccine supply, and population acceptance. Moreover, the degree of health system preparedness, responsiveness and resilience plays an important role in the success of a vaccination campaign and measures to contain the pandemic long and short-term health impacts. Based on our analysis, we observed some evidence of a negative association between increased vaccine coverage and fatalities and hospitalisation trends, which aligns with the findings from the literature [98], [99], [100]. We conclude that it is the similarities between France, Israel, Italy and Spain that define their vaccine programmes. This is particularly the case for France, Italy and Spain all of which were hard hit in the first waves of COVID-19. Each prioritised vulnerable groups when supplies of vaccines were restricted.
Some factors differentiated between the uptake of vaccines in France, Israel, Italy and Spain. The high rate and coverage of Israel's programme can in part be attributed to the securing of sufficient vaccines through bilateral agreements with their manufactures and the rapid creation of the infrastructure required to deliver vaccines. This strategy could not realistically form the basis for future policies across countries. However, the low level of vaccine hesitancy in the general population, if not in all groups, no doubt played a role in reaching high levels of vaccination. This may also be generally true in Spain, which when compared to France and Italy had lower levels of hesitancy and higher vaccination rates. Research is ongoing into the reasons for hesitancy, but cultural factors and trust in governments have been reported to influence the decision to be vaccinated. Therefore, in addition to acquiring sufficient supplies and creating an infrastructure able to deliver the vaccine, vaccine hesitancy is an important issue for policymakers to address. Countries with higher levels of hesitancy could promote targeted campaigns to increase vaccine uptake amongst hesitant groups rather than relying (only) on boosters as a mechanism to reduce the effects on the healthcare system and the economy. France, Israel and Italy have all implemented restrictions for unvaccinated people to both protect public health and incentivise vaccination.
In terms of prioritisation, each country chose to vaccinate essential workers and vulnerable groups first. This strategy is designed to reduce morbidity and mortality. It could be argued that an alternative strategy would have been one that prioritised financial wellbeing. Following such a strategy would mean prioritising those whose activities contribute to maintaining incomes and employment. Other policies were put in place across the four countries to ameliorate the financial effects of stringency and these also, to some extent, supported those whose financial wellbeing was curtailed whilst vulnerable people were prioritised for vaccination. However, few if any examples exist where vaccination programmes prioritised the financially most active groups. Therefore, no conclusions can be drawn from our analyses about the prioritisation of vaccines during a pandemic when supplies are restricted.
The strengths and weaknesses of COVID-19 pandemic crisis management along with the various strategies surrounding the vaccination roll-out campaigns may yield lessons for policymakers amidst such decisions, including for future pandemics. The findings of our analysis are provisional. Indeed, the analysis covers only the first eleven months of the vaccination campaigns and is based on descriptive analysis. Future data availability and an in-depth analysis of booster campaigns will add to the present findings. Moreover, vaccine hesitancy amongst different subgroups, such as minorities and migrant populations, were not examined in the study and could be an opportunity for further investigation.
Declarations
Funding: None
Competing interests: None declared
Ethical approval: Not required
Patient Consent: Not required
Acknowledgement
We thank Chiara Berardi for her insightful comments on the outline of the paper. We also thank Madeleine Hinwood and Andrew Greenland for their assistance with the final edits of the manuscript.
Footnotes
Spearman's rho was preferred on the Pearson coefficient as the relationship of the two variables violates the linearity assumption
Reference
- 1.Berardi C., Antonini M., Genie M.G., Cotugno G., Alessandro L., Melia A., et al. The COVID-19 pandemic in Italy: policy and technology impact on health and non-health outcomes. Health Policy Technol. 2020 doi: 10.1016/j.hlpt.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henríquez J., Gonzalo-Almorox E., García-Goñi M., Paolucci F. The first months of the COVID-19 pandemic in Spain. Health Policy Technol. 2020;9(4):560–574. doi: 10.1016/j.hlpt.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desson Z., Weller E., McMeekin P., Ammi M. An analysis of the policy responses to the COVID-19 pandemic in France, Belgium, and Canada. Health Policy Technol. 2020;9(4):430–446. doi: 10.1016/j.hlpt.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., et al. A global database of COVID-19 vaccinations. Nature Human Behav. 2021;5(7):947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 5.Rosen B., Waitzberg R., Israeli A. Israel's rapid rollout of vaccinations for COVID-19. Isr J Health Policy Res. 2021;10(1):6. doi: 10.1186/s13584-021-00440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The New York Times. How Israel Became a World Leader in Vaccinating Against Covid-19 2021 [Available from: https://www.nytimes.com/2021/01/01/world/middleeast/israel-coronavirus-vaccines.html.
- 7.Wilf-Miron R., Myers V., Saban M. Incentivizing Vaccination Uptake: the “Green Pass” Proposal in Israel. JAMA. 2021;325(15):1503–1504. doi: 10.1001/jama.2021.4300. [DOI] [PubMed] [Google Scholar]
- 8.Bar-On Y.M., Goldberg Y., Mandel M., Bodenheimer O., Freedman L., Kalkstein N., et al. Protection of BNT162b2 Vaccine Booster against Covid-19 in Israel. N Engl J Med. 2021 doi: 10.1056/NEJMoa2114255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wouters O.J., Shadlen K.C., Salcher-Konrad M., Pollard A.J., Larson H.J., Teerawattananon Y., et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet North Am Ed. 2021;397(10278):1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naaber P., Tserel L., Kangro K., Sepp E., Jürjenson V., Adamson A., et al. Dynamics of antibody response to BNT162b2 vaccine after six months: a longitudinal prospective study. The Lancet Regional Health - Europe. 2021 doi: 10.1016/j.lanepe.2021.100208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hale T., Hangrist N., Kira B., Petherick A., Phillips T., Webster S. Variation in government responses to COVID-19. Version 60 Blavatnik School of Government Working Paper. 2020.
- 13.Leshem E., Afek A., Kreiss Y. Buying Time with COVID-19 Outbreak Response. Israel Emerg Infect Dis. 2020;26(9):2251–2253. doi: 10.3201/eid2609.201476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Worldometers. Population 2021 [Available from: https://www.worldometers.info/.
- 15.Hawkins R.B., Charles E.J., Mehaffey J.H. Socio-economic status and COVID-19–related cases and fatalities. Public Health. 2020;189:129–134. doi: 10.1016/j.puhe.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.ISTAT. Indicatori demografici ISTAT; 2021 [updated 3 May 2021. Available from: https://www.istat.it/it/files//2021/05/REPORT_INDICATORI-DEMOGRAFICI-2020.pdf.
- 17.INE. Cifras de población 2021 [Available from: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176951&menu=ultiDatos&idp=1254735572981.
- 18.World Bank. World Bank Open Data 2021 [updated 15 Sep 2021. Available from: https://data.worldbank.org/.
- 19.Durand-Zaleski I. Health system overview - France: the Commonwealth Fund; 2020 [Available from: https://www.commonwealthfund.org/sites/default/files/2020-12/2020_IntlOverview_FRANCE.pdf.
- 20.ISTAT. Annuario statistico italiano 2020. Rome; 2020.
- 21.Hayek S., Ifrah A., Enav T., Shohat T. Prevalence, Correlates, and Time Trends of Multiple Chronic Conditions Among Israeli Adults: estimates From the Israeli National Health Interview Survey, 2014-2015. Prev Chronic Dis. 2017;14:E64. doi: 10.5888/pcd14.170038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.IHME. GBD 2019 2021 [updated 10 Jul 2021. Available from: https://vizhub.healthdata.org/gbd-compare/.
- 23.OECD. Gross domestic product (GDP) (indicator) 2021.
- 24.OECD. Unemployment rate (indicator) 2021 [updated 16 Oct 2021.
- 25.OECD. OECD Employment Outlook 2021 2021.
- 26.El Pais. El sobreesfuerzo de las UCI: el doble de camas desde el inicio de la crisis 2021 [Available from: https://elpais.com/sociedad/2021-02-11/el-sobreesfuerzo-de-las-uci-el-doble-de-camas-desde-el-inicio-de-la-crisis.html.
- 27.Annane D., Federici L., Chagnon J.-.L., Diehl J.L., Dreyfuss D., Guiot P., et al. Intensive care units, the Achilles heel of France in the COVID-19 battle. The Lancet Regional Health – Europe. 2021;2 doi: 10.1016/j.lanepe.2021.100046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Corte dei Conti. Rapporto 2021 sul coordinamento della finanza pubblica. 2021.
- 29.OECD. Health resources 2021 [Available from: https://data.oecd.org/health.htm#profile-Health%20resources.
- 30.DRESS. Demographics of healthcare professionals 2021 [Available from: https://drees.shinyapps.io/demographie-ps/.
- 31.Tikkanen R., Osborn R., Mossialos E., Djordjevic A., Wharton G. International Profiles of Health Care Systems 2020 2020.
- 32.OECD . 2021. Hospital beds (indicator) [updated 16 Oct 2021. [Google Scholar]
- 33.D'Arienzo M., Di Silverio P., Gnerre P., Palermo C. Se crolla anche l'ultimo baluardo. 2020 20 November 2020.
- 34.Israeli Ministry of Health. Hospital beds 2021 [updated January 2021. Available from: https://www.health.gov.il/PublicationsFiles/beds2021.pdf.
- 35.DREES. Entre fin 2019 et fin 2020, la capacité d'accueil hospitalière a progressé de 3,6% en soins critiques et de 10,8% en hospitalisation à domicile. 2021 September 2021.
- 36.Lefrant J.Y., Fischer M.O., Potier H., Degryse C., Jaber S., Muller L., et al. A national healthcare response to intensive care bed requirements during the COVID-19 outbreak in France. Anaesth Crit Care Pain Med. 2020;39(6):709–715. doi: 10.1016/j.accpm.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Israeli Ministry of Health. Number of doctors in Israel: trends and policy proposals. 2021.
- 38.I. Stat. Personale sanitario 2021 [Available from: http://dati.istat.it/Index.aspx?DataSetCode=DCIS_PERS_SANIT.
- 39.La Moncloa. 7.207 nuevos especialistas en Ciencias de la Salud se incorporan al SNS tras concluir su periodo de formación 2021 [Available from: https://www.lamoncloa.gob.es/serviciosdeprensa/notasprensa/sanidad14/Paginas/2021/130821_especialistas-sns.aspx.
- 40.Italian Ministry of Health. Strutture di ricovero e cura pubbliche e private accreditate 2020 [updated 15 Jun 2021. Available from: https://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=&id=5451&area=statisticheSSN&menu=vuoto.
- 41.Ministerio de Sanidad. Urgencias y emergencias 112/061: gobierno de Espana; 2021 [Available from: https://pestadistico.inteligenciadegestion.mscbs.es/publicoSNS/N/sistema-de-informacion-de-atencion-primaria-siap/urgencias-y-emergencias-112-061.
- 42.The Knesset. Data on ventilators in Israel 2020 [Available from: https://fs.knesset.gov.il/23/Committees/23_cs_bg_573712.pdf.
- 43.Presidenza del Consiglio dei Ministri. Analisi distribuzione aiuti 2021 [Available from: https://app.powerbi.com/view?r=eyJrIjoiNTE2NWM3ZjktZGFlNi00MzYxLWJlMzEtYThmOWEzYjA1MGNhIiwidCI6ImFmZDBhNzVjLTg2NzEtNGNjZS05MDYxLTJjYTBkOTJlNDIyZiIsImMiOjh9.
- 44.La Moncloa. Sanidad distribuye a las comunidades autónomas 7.776 respiradores desde el mes de marzo 2020 [updated 19 Oct 2020. Available from: https://www.lamoncloa.gob.es/serviciosdeprensa/notasprensa/sanidad14/Paginas/2020/191020-respiradores.aspx.
- 45.Eurostat. Government revenue, expenditure and main aggregates 2021 [updated 21Jul 2021. Available from: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=gov_10a_main&lang=en.
- 46.Israeli Central Bureau of Statistics. National expenditure on health, by type of expenditure and service 2021 [Available from: https://www.cbs.gov.il/he/publications/doclib/2019/3.shnatonhealth/st03_01.xls.
- 47.OECD. Health spending (indicator) 2021.
- 48.Camera dei Deputati. Misure per fronteggiare l'emergenza coronavirus 2021 [Available from: https://temi.camera.it/leg18/temi/misure-sanitarie-per-fronteggiare-l-emergenza-coronavirus.html.
- 49.Ministerio de Sanidad. Diferentes series de gasto sanitario 2021 [Available from: https://www.mscbs.gob.es/estadEstudios/estadisticas/sisInfSanSNS/pdf/diferentesSeriesGastoSanitario.pdf.
- 50.French Government. Budget General - Prévention sécurité sanitaire et offre de soins. France; 2021.
- 51.DRESS. Les dépenses de santé en 2020 2021 [updated 15/09/2021. 15/09/2021:[Available from: https://drees.solidarites-sante.gouv.fr/communique-de-presse/les-depenses-de-sante-en-2020.
- 52.European Commission. EU Vaccines Strategy 2021 [Available from: https://ec.europa.eu/info/live-work-travel-eu/coronavirus-response/public-health/eu-vaccines-strategy_en.
- 53.Italian Government . Gazzetta Ufficiale della Repubblica Italiana; 2021. Raccomandazioni ad interim sui gruppi target della vaccinazione anti-SARS-COV-2/COVID-19; pp. 1–13. [Google Scholar]
- 54.BBC. Coronavirus vaccine delays halt Pfizer jabs in parts of Europe 2021 [Available from: https://www.bbc.com/news/world-europe-55765556.
- 55.Legge D.G., Kim S. Equitable Access to COVID-19 Vaccines: cooperation around Research and Production Capacity Is Critical. J Peace Nuclear Disarmament. 2021;4(sup1):73–134. [Google Scholar]
- 56.Ministère des Solidarités et de la Santé. Decision to anticipate vaccination of health workers France: ministère des Solidarités et de la Santé, 2021 [Available from: https://solidarites-sante.gouv.fr/IMG/pdf/avis_du_cosv_28_janvier_2021_-_la_vaccination_des_professionnels_de_sante_de_moins_de_50_ans.pdf.
- 57.CNBC. More EU nations suspend AstraZeneca shot as regulator says benefits still outweigh the risks 2021 [Available from: https://www.cnbc.com/2021/03/16/more-eu-countries-halt-astrazeneca-shot-as-ema-reviews-side-effects-.html.
- 58.DW. AstraZeneca: germany, other European countries to resume use of vaccine 2021 [Available from: https://www.dw.com/en/astrazeneca-germany-other-european-countries-to-resume-use-of-vaccine/a-56922088.
- 59.European Medicines Agency. Increase in vaccine manufacturing capacity and supply for COVID-19 vaccines from AstraZeneca, BioNTech/Pfizer and Moderna 2021 [updated 26/03/2021. Available from: https://www.ema.europa.eu/en/news/increase-vaccine-manufacturing-capacity-supply-covid-19-vaccines-astrazeneca-biontechpfizer-moderna.
- 60.The Times of Israel. Israel to offer AstraZeneca vaccines starting Thursday 2021 [Available from: https://www.timesofisrael.com/israel-to-offer-astrazeneca-vaccines-starting-thursday/.
- 61.Presidenza del Consiglio dei Ministri. Piano Vaccinale AntiCOVID. 2021.
- 62.Amiel S. Euronews; 2021. How struggling spain became one of europe's vaccination champions.https://www.euronews.com/2021/09/03/how-struggling-spain-became-one-of-europe-s-vaccination-champions [Available from: [Google Scholar]
- 63.Santé publique France. Vaccination contre la COVID-19: un défi logistique et scientifique: santé publique France; 2020 [updated 28Dec 2020.
- 64.Gandré C., Or Z. Transition measures: planning services: european Observatory of Health System and Policies; 2021 [Available from: https://eurohealthobservatory.who.int/monitors/hsrm/all-updates/hsrm/france/transition-measures-planning-services.
- 65.Jovell A., Blendon R.J., Navarro M.D., Fleischfresser C., Benson J.M., Desroches C.M., et al. Public trust in the Spanish health-care system. Health Expect. 2007;10(4):350–357. doi: 10.1111/j.1369-7625.2007.00466.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Italian Government. Linee di indirizzo organizzativo e strutturale dei punti vaccinali territoriali straordinari relativi alla campagna di vaccinazione anti SARS-COV-2/COVID-19. 2021.
- 67.Carotti B., Sgueo G. Isituto di Ricerche sulla Pubblica Amministrazione (IRPA); 2021. In viaggio tra piani vaccinali, prenotazioni online e decentramento amministrativo. [Google Scholar]
- 68.Santé publique France . Santé publique France; 2021. Vaccination contre la COVID-19: le rôle de santé publique france.https://www.santepubliquefrance.fr/dossiers/coronavirus-covid-19/vaccination-contre-la-covid-19/articles/vaccination-contre-la-covid-19-le-role-de-sante-publique-france [updated 28 Sep 2021. Available from: [Google Scholar]
- 69.Haute Autorité de Santé . Haute Autorité de Santé; 2021. Vaccination contre la covid-19: impliquer davantage de professionnels pour accélérer la campagne.https://www.has-sante.fr/jcms/p_3245564/fr/vaccination-contre-la-covid-19-impliquer-davantage-de-professionnels-pour-accelerer-la-campagne [Available from: [Google Scholar]
- 70.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Signorelli C., Odone A., Ricciardi W., Lorenzin B. The social responsibility of public health: italy's lesson on vaccine hesitancy. Eur J Public Health. 2019;(1464–360X (Electronic)) doi: 10.1093/eurpub/ckz135. [DOI] [PubMed] [Google Scholar]
- 72.Bernadou A., Astrugue C., Méchain M., Le Galliard V., Verdun-Esquer C., Dupuy F., et al. Measles outbreak linked to insufficient vaccination coverage in Nouvelle-Aquitaine Region, France, October 2017 to July 2018. Euro surveillance: bulletin Europeen sur les maladies transmissibles = Eur Commun Dis Bull. 2018;23(30) doi: 10.2807/1560-7917.ES.2018.23.30.1800373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Burioni R., Odone A. Signorelli C. Italy's policy shift on immunization. Infect Dis. 2018;18:26–27. [Google Scholar]
- 74.Ministère des Solidarités et de la Santé. Vaccins obligatoires 2018 [updated 17 Feb 2021. Available from: https://solidarites-sante.gouv.fr/prevention-en-sante/preserver-sa-sante/vaccination/vaccins-obligatoires/.
- 75.Paris C., Bénézit F., Geslin M., Polard E., Baldeyrou M., Turmel V., et al. COVID-19 vaccine hesitancy among healthcare workers. Infectious Dis Now. 2021;51(5):484–487. doi: 10.1016/j.idnow.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.France24. French protesters against Covid-19 health restrictions clash with police in Paris 2021 [Available from: https://www.france24.com/en/europe/20210724-french-protesters-against-covid-19-health-restrictions-clash-with-police-in-paris.
- 77.Shahbari N.A.E., Gesser-Edelsburg A., Davidovitch N., Brammli-Greenberg S., Grifat R., Mesch G.S. Factors associated with seasonal influenza and HPV vaccination uptake among different ethnic groups in Arab and Jewish society in Israel. Int J Equity Health. 2021;20(1):201. doi: 10.1186/s12939-021-01523-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stein Zamir C. Israeli A. Knowledge, Attitudes and Perceptions About Routine Childhood Vaccinations Among Jewish Ultra-Orthodox Mothers Residing in Communities with Low Vaccination Coverage in the Jerusalem District. Matern Child Health J. 2017;21(5):1010–1017. doi: 10.1007/s10995-017-2272-5. [DOI] [PubMed] [Google Scholar]
- 79.Rosen B., Waitzberg R., Israeli A., Hartal M., Davidovitch N. Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel's COVID-19 vaccination program. Isr J Health Policy Res. 2021;10(1):43. doi: 10.1186/s13584-021-00481-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Spanish Foundation for Science and Technology . FECYT; 2021. 83% of the spanish population trusts in vaccination against covid, 25 points more than in january.https://www.fecyt.es/en/news/83-spanish-population-trusts-vaccination-against-covid-25-points-more-january [Available from: [Google Scholar]
- 81.Eurofund. Vaccinations during COVID-19 2021 [Available from: https://www.eurofound.europa.eu/data/covid-19/vaccinations.
- 82.Misure urgenti per il contenimento dell'epidemia da COVID-19, in materia di vaccinazioni anti SARS-CoV-2, di giustizia e di concorsi pubblici., n. 44 (2021).
- 83.Misure urgenti per fronteggiare l'emergenza epidemiologica da COVID-19 e per l'esercizio in sicurezza di attivita' sociali ed economiche., (2021).
- 84.COVID-19, Estensione dell'obbligatorieta' del green pass [press release]. Italian Governement, 9 September 2021 2021.
- 85.Italian Government. Decree 24th November 2021 [Available from: https://www.corriere.it/politica/21_novembre_24/testo-pdf-nuovo-decreto-super-green-pass-dc456138-4d4a-11ec-8b01-c023696b7b18.shtml?refresh_ce.
- 86.Israeli Ministry of Health. Green Pass: ministry of Health; 2021 [Available from: https://corona.health.gov.il/directives/green-pass-info/.
- 87.Ministère des Solidarités et de la Santé. Consignes obligation vaccinale passe sanitaire 2021 [Available from: https://solidarites-sante.gouv.fr/IMG/pdf/consignes_obligation_vaccinale_passe_sanitaire_110821.pdf.
- 88.Politico. Macron ties French vaccine passports to booster shots 2021 [Available from: https://www.politico.eu/article/france-ties-seniors-vaccine-passports-to-booster-shots/.
- 89.La Moncloa. Spain has issued more than 18 million EU Digital COVID Certificates 2021 [cited 2021 18 Nov 2021]. Available from: https://www.lamoncloa.gob.es/lang/en/gobierno/news/Paginas/2021/20210812_covid-certificate.aspx.
- 90.El Pais. La justicia balear avala exigir el certificado covid para entrar en las discotecas 2021 [Available from: https://elpais.com/sociedad/2021-10-01/la-justicia-balear-avala-exigir-el-certificado-covid-para-entrar-en-las-discotecas.html.
- 91.Lerner J.S., Li Y., Valdesolo P., Kassam K.S. Emotion and Decision Making. Annu Rev Psychol. 2015;66(1):799–823. doi: 10.1146/annurev-psych-010213-115043. [DOI] [PubMed] [Google Scholar]
- 92.Cohn A., Engelmann J., Fehr E., Maréchal M.A. Evidence for Countercyclical Risk Aversion: an Experiment with Financial Professionals. Am Econ Rev. 2015;105(2):860–885. [Google Scholar]
- 93.Meier A. The German Socio-Economic Panel (SOEP); 2019. Emotions, risk attitudes, and patience. diw berlin. [Google Scholar]
- 94.Andersson O., Campos-Mercade P., Meier A.N., Wengström E. Anticipation of COVID-19 vaccines reduces willingness to socially distance. J Health Econ. 2021;80 doi: 10.1016/j.jhealeco.2021.102530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Prevention CfDCa. Understanding How COVID-19 Vaccines Work 2021 [Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/how-they-work.html.
- 96.Dolgin E. COVID vaccine immunity is waning - how much does that matter? Nature. 2021;597(7878):606–607. doi: 10.1038/d41586-021-02532-4. [DOI] [PubMed] [Google Scholar]
- 97.OECD. Quarterly GDP (indicator) 2021 [Available from: 10.1787/b86d1fc8-en.
- 98.Sheikh A., McMenamin J., Taylor B., Robertson C. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet North Am Ed. 2021;397(10293):2461–2462. doi: 10.1016/S0140-6736(21)01358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lopez Bernal J., Andrews N., Gower C., Gallagher E., Simmons R., Thelwall S., et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N Engl J Med. 2021;385(7):585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Haas E.J., Angulo F.J., McLaughlin J.M., Anis E., Singer S.R., Khan F., et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397(10287):1819–1829. doi: 10.1016/S0140-6736(21)00947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]