Abstract
Background:
The Lapidus procedure using planar saw resection has often been criticized for complications related to excessive shortening and elevation of the first ray. The goal of this study was to assess the amount of shortening that occurs when using a cutting guide for controlled saw resection of the first tarsometatarsal (TMT) joint surfaces, along with assessment of deformity correction in all 3 anatomic planes.
Methods:
A prospective multicenter study with IRB approval included 35 hallux valgus subjects evaluated at baseline and 6 months following instrumented triplane first TMT arthrodesis without lesser metatarsal osteotomies.
Results:
The average first ray bone segment length loss was 3.1 mm (95% confidence interval [CI] 2.4-3.7) in the anteroposterior (AP) radiographic assessment and 2.4 mm (95% CI 1.7-3.1) in the sagittal plane. The mean preoperative radiographic measurements were 1.7 degrees (dorsiflexion) for sagittal plane angle, 13.8 degrees for intermetatarsal angle (IMA), and 5.1 for tibial sesamoid position (TSP). Improvements were seen postoperatively for all measures with a mean difference of –0.2 degrees (95% CI –1.0 to 0.6) for sagittal plane angle, –9.2 degrees (95% CI –10.1 to –8.3 degrees) for IMA, and –3.5 (95% CI –4.0 to –3.1) for TSP. Five of the patients reported lesser metatarsal pain preoperatively, and no patients complained of lesser metatarsalgia at 6-month follow-up.
Conclusions:
Minimal length loss of the first ray can be expected following instrumented triplane TMT arthrodesis while achieving full 3-dimensional deformity correction and reducing the risk of lesser metatarsalgia.
Level of Evidence:
Level II, prospective comparative study.
Keywords: lapidus, triplane, tarsometatarsal arthrodesis, shortening osteotomy, lesser metatarsalgia
Introduction
Lapidus arthrodesis is a common procedure for hallux valgus correction that has received increasing attention for its ability to correct at the apex of the deformity and enable a correction in all 3 planes including sagittal plane correction. 23 The Lapidus procedure is often criticized for producing first ray shortening and a perceived association with transfer metatarsalgia. However, all osteotomies performed result in some bone loss, and some are more prone than others to shortening due to the geometry of the bone cuts. The analysis of first ray shortening with hallux valgus repair and subsequent lesser metatarsal weight transfer has been discussed by many authors. 4,15,17,19,22,26,42,44 Radiographic measures of shortening have traditionally been limited to anteroposterior (AP) radiographs, which can be confounded by motion in the sagittal and frontal planes. Specifically, a plantar-deviated metatarsal will measure shorter than a neutrally aligned metatarsal. Studies specifically related to the Lapidus bunionectomy with planar cuts ranged from 3.1 mm to 7.5 mm of shortening. 3,5,10,13,25 Currently, there is a perception that manual joint preparation by curettage may be a more appropriate method to reduce shortening and complications. 3,10,25,35 This perception may be inaccurate, as it has been found that the range of shortening using this technique ranges from 0.86 to 5.0 mm. 3,10,25,35 Additionally, there are other issues of curettage technique that may play a role in the incidence of nonunions. 20
The purpose of our study was to analyze shortening of the first ray segment as well as the other planar positions after performing triplane tarsometatarsal (TMT) arthrodesis for hallux valgus (HV) utilizing a cutting guide for controlled saw resection and subchondral bone removal. The authors hypothesized that using an instrumented system, appropriate removal of the articular cartilage would be accomplished while avoiding excessive shortening previously published as >4.0 mm. 4
Methods
A multicenter prospective study received institutional review board approval to analyze the long-term outcomes of the Lapiplasty procedure (Treace Medical Concepts, Inc, Ponte Vedra, FL). While this current study is ongoing, we obtained data after 6 months’ follow-up from the time of surgery to analyze the amount of segmental loss of the first ray length. This was included as one of the secondary endpoints (change in radiographic angular/positional alignment before and after the procedure), with one of the time frames being 6 months.
Inclusion criteria for the study included patients at least 18 years old with HV, intermetatarsal angles (IMAs) ranging from 10 to 22 degrees, and HV angles (HVAs) ranging from 16 to 40 degrees. All patients were to be able to bear weight early (immediate to 3 weeks) and sign written informed consent. Exclusion criteria included previous hallux valgus surgery; body mass index >40; glycated hemoglobin (HbA1c) ≥7; evidence of peripheral neuropathy; moderate to severe arthrosis of the first metatarsophalangeal (MTP) joint complex; current use of nicotine; and use of immunosuppressant drugs. Specific to this analysis, patients were only included if the cut guide was used to make the planar saw cuts. This resulted in 8 subjects from one site being excluded from this analysis.
A total of 35 subjects enrolled in the study had postoperative data at 6 months. Mean age was 41.5 years (95% confidence interval [CI] 37.7-45.3), mean body mass index was 26.7 (95% CI 24.9-28.6), and all patients were female (100%). The left foot was involved for 48.6% of patients (n = 17). One patient had diabetes (2.9%) but still met inclusion criteria.
All radiographic measurements were performed by 2 independent radiologists with mean values reported, with the exception of the sagittal length measurement, which was only measured by one of the independent radiologists because of unavailability of the surgeon to measure for medical reasons. If differences between readers were greater than predefined limits, a reconciliation process ensued to remediate discrepancies. Radiographic measurements to quantify the length of the first and second metatarsals were made to a common 2-dimensional radiographic axis preoperatively and postoperatively. In order to evaluate the length of the metatarsal in the AP projection, the anatomic axis of the first and second metatarsal was determined. A perpendicular line was made at the most distal aspect of the second metatarsal, and the distance from the distal aspect of the first metatarsal to this perpendicular line was recorded (Figure 1). 16,27,28 The sagittal view length measurement of the first ray was measured from the most anterior concavity of the medial cuneiform to the most distal aspect of the first metatarsal head (Figure 2). The sagittal first metatarsal angle relative to the second metatarsal was measured pre- and postoperatively as per Usuelli et al 43 (Figure 3).
Figure 1.

Preoperative measurement of length of first ray. The measurement of the most distal aspect of the first metatarsal to the perpendicular of the anatomic axis of the second metatarsal. A negative value corresponds to a first metatarsal that is shorter than the second.
Figure 2.

Length of first ray in sagittal view. Measured from the most distal aspect of the metatarsal head to the most distal aspect of the medial cuneiform concavity at the navicular- cuneiform articulation.
Figure 3.

Sagittal metatarsal angle measurement of the first metatarsal relative to the second. A positive value indicates relative dorsiflexion of the first metatarsal.
The operative procedure has been described earlier in detail (Supplemental Video). 31,36,39,40 Although severity-based algorithms would advocate distal metatarsal procedures for lower IMAs, it was the authors’ preference to address the deformity from an anatomic basis at the center of rotation and angulation. 18 The main principle of the technique was a “correct then cut” method using a precision standardized cutting guide that allowed for minimal bone resection of joint surfaces while aligning the first ray in 3 dimensions. After the first TMT joint was mobilized, the metatarsal was aligned in all 3 planes while reducing the intermetatarsal angle. Radiographic assessment was then performed. A precision cut guide was then applied and cuts were made on each side of the joint. The jig was then removed, and the joint was prepped in a standard fashion. After realignment of the segments, fixation was applied. The authors preferred biplanar fixation to promote early weightbearing and micro-motion as described by Perren. 30 Standard weightbearing radiographs were taken pre- and postoperatively (Figure 4).
Figure 4.
Preoperative and postoperative anteroposterior and lateral radiographic assessment.
Summary statistics included mean and 95% confidence intervals for continuous variables and descriptive statistics for categorical variables. Statistical analyses were performed using SAS, version 9.4 (SAS Institute, Inc, Cary, NC).
Results
The mean AP measurement of the first metatarsal length relative to the second metatarsal was –2.0 mm preoperatively (95% CI –2.8 to –1.2) and –5.1 mm (95% CI –6.1 to –4.1) at 6 months postoperatively, resulting in a net mean AP shortening of 3.1 mm (95% CI 2.4-3.7) (Table 1). The mean sagittal length of the first ray preoperative was 77.6 mm (95% CI 73.5-81.8), and the mean at 6 months postoperative was 75.3 mm (95% CI 71.2-79.3), resulting in a net mean sagittal shortening of 2.4 mm (95% CI 1.7-3.1). The mean intermetatarsal angle (IMA) was 13.8 degrees preoperatively (95% CI 13.0-14.6) and 4.6 degrees at 6 months postoperatively (95% CI 3.8-5.4), resulting in a change of –9.2 degrees (95% CI –10.1 to –8.3). The mean hallux valgus angle (HVA) was 26.4 degrees preoperatively (95% CI 24.3-28.4) and 6.1 degrees at 6 months postoperatively (95% CI 4.4-7.8), resulting in a change of –20.3 degrees (95% CI –23.0 to –17.6 degrees). The sagittal plane metatarsal angle results revealed a preoperative mean of 1.7 degrees (95% CI 1.2-2.3; dorsiflexion) and a 6-month postoperative mean of 1.5 degrees (95% CI 0.7-2.3), resulting in an overall change in the sagittal angle of –0.2 degrees (95% CI –1.0 to 0.6). Mean tibial sesamoid position (TSP) preoperatively was 5.1 (95% CI 4.7-5.6) and 1.6 (95% CI 1.3-1.8) at 6 months postoperatively, resulting in a net difference of –3.5 (95% CI –4.0 to –3.1).
Table 1.
Evaluation of First Ray Alignment and Positioning After Triplanar First Tarsometatarsal Arthrodesis.a
| Variable | n | Mean (95% Confidence Interval) |
|---|---|---|
| Anteroposterior first metatarsal length (mm) | ||
| Preoperative | 35 | –2.0 (–2.8, –1.2) |
| 6-mo | 35 | –5.1 (–6.1, –4.1) |
| Change | 35 | –3.1 (–3.7, –2.4) |
| Sagittal first ray length (mm) | ||
| Preoperative | 34 | 77.6 (73.5, 81.8) |
| 6-mo | 34 | 75.3 (71.2, 79.3) |
| Change | 34 | –2.4 (–3.1, –1.7) |
| Intermetatarsal angle (IMA) (degrees) | ||
| Preoperative | 35 | 13.8 (12.0, 14.6) |
| 6-mo | 35 | 4.6 (3.8, 5.4) |
| Change | 35 | –9.2 (–10.1, –8.3) |
| Hallux valgus angle (HVA) (degrees)* | ||
| Preoperative | 35 | 26.4 (24.3, 28.4) |
| 6-mo | 35 | 6.1 (4.4, 7.8) |
| Change | 35 | –20.3 (–23.0, –17.6) |
| Sagittal metatarsal angle (degrees)* | ||
| Preoperative | 35 | 1.7 (1.2, 2.3) |
| 6-mo | 35 | 1.5 (0.7, 2.3) |
| Change | 35 | –0.2 (–1.0, 0.6) |
| Tibial sesamoid position (TSP) | ||
| Preoperative | 35 | 5.1 (4.7, 5.6) |
| 6-mo | 33 | 1.6 (1.3, 1.8) |
| Change | 33 | –3.5 (–4.0, –3.1) |
a Mean with 95% confidence intervals are shown. Changes for first metatarsal length, first ray length, IMA, and TSP were significant at P < .001.
Five of the patients had preoperative lesser metatarsal pain. There were no second or third metatarsal osteotomies performed. At 6-month follow-up, none of the patients reported lesser metatarsal pain. One patient (2.9%) had a fifth metatarsal osteotomy for a tailor’s bunion. None of the patients had additional first metatarsal osteotomies. Four of the patients (11.4%) had an Akin osteotomy, and 2 patients (5.7%) had hammertoe correction. No other procedures were performed other than the index procedures.
Discussion
Our data support minimal bone segment loss after triplanar first TMT arthrodesis. The mean shortening on conventional AP radiographs was 3.1 mm (95% CI 2.4-3.7) and the mean shortening on the sagittal view was 2.4 mm (95% CI 1.7-3.1). These results are in the range of shortening reported in the literature for curettage techniques and less than that reported for manual planar cuts. This is in part achieved by the method of “correct then cut” technique using a uniform cut guide and standard set of landmarks. A reproducible metered technique is key to gaining correction while accessing the subchondral bone to facilitate osseous union. The technique in this series uses an instrumented cut that references more distal cuneiform anatomic landmarks and limits bone removal from both the cuneiform and first metatarsal to that which is essential to promote fusion and allow for metatarsal realignment (Figure 5). The method of “correct then cut” allows the first metatarsal to be aligned in 3 dimensions, reducing the IMA, especially in the transverse plane. In doing so, the ray will relatively lengthen (Figure 6). This geometric change is observed when 2 collinear lines that are initially angulated are then reduced to one combined line. Removing 3-4 mm of length through a carefully prepared fusion site maintains relative length. It should be noted that proper 3-dimensional alignment is also vital to produce first ray weightbearing function. Prior to correction of HV, it is common for patients to have a degree of plantar pain at the lesser MTPs. 9 This is not a by-product of an intrinsically short first ray, but rather abnormal first ray mechanics produced by the deformity itself.
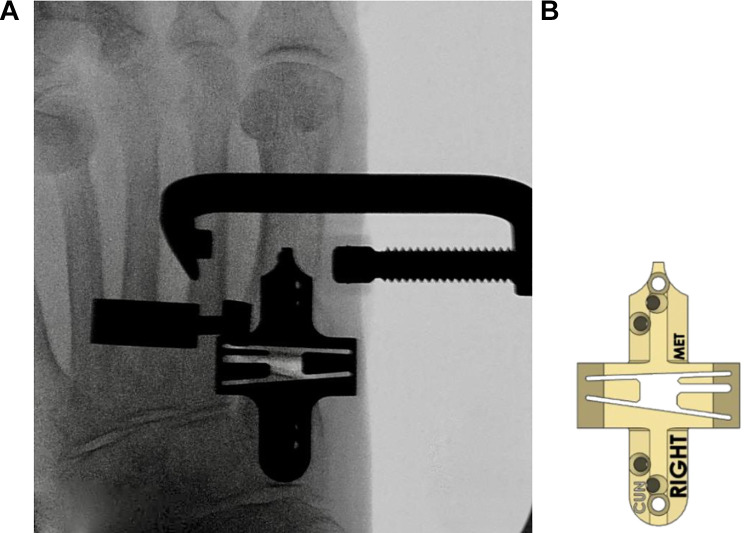
Figure 5.
(A) Precise osseous cuts with use of the bone cutting guide. Note that the medial landmark on the cuneiform is far distal to the medial cortical wall. This alignment method reduces overall bone removal while producing proper angular correction. (B) Example of right foot cut guide.
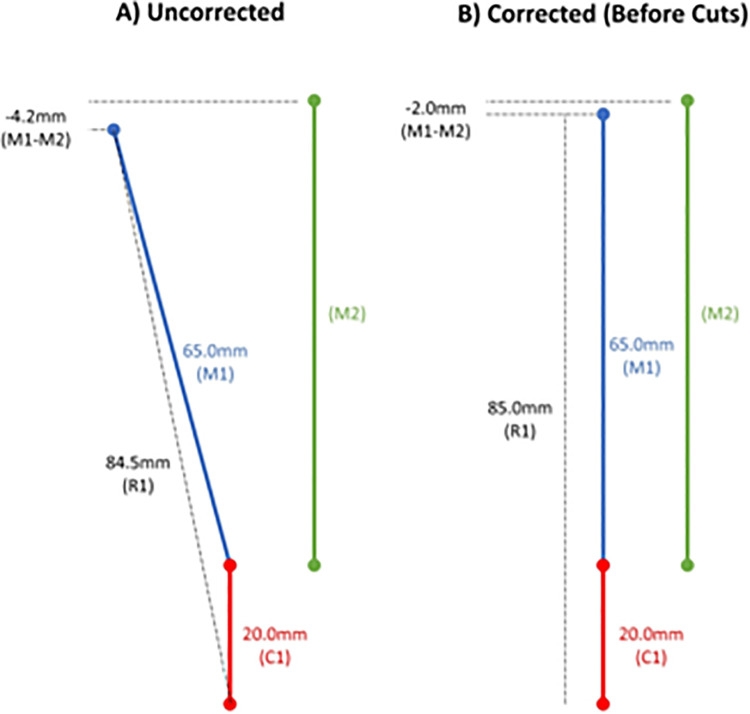
Figure 6.
Schematic diagram representing the first and second ray of the right foot before and after correction (before removing bone cuts). In this theoretical example, the length of the first metatarsal relative to the second metatarsal increases with IMA reduction and resulting collinearity in the corrected position. IMA, intermetatarsal angle.
Average shortening by osseous cuts (planar resection) ranges in the literature from 3.14 to 7.5 mm. 3,5,10,14,25,33 Literature review of shortening by curettage techniques range from 0.86 to 5.0 mm. 3,10,25,35 One can easily see the variances in technique and subsequent end results. The reported shortening in AP radiographs of 3.1 mm (95% CI 2.4-3.7) of bone segment length loss for first TMT fusion was consistent in our study and on the low end of that reported in the literature.
It is also important to note that other operative procedures for HV correction report shortening and risks of transfer metatarsalgia. Ahn et al 1 reported in their study of 185 patients that transfer metatarsalgia did not occur if shortening of the first metatarsal was less than 5.8 mm in their chevron osteotomy cases. Tóth et al 42 reported on shortening of the first metatarsal in 240 patients to be 3.8 ± 1.8 mm after Wilson osteotomy. Carr and Boyd 4 reported to not shorten the first metatarsal more than 3 to 4 mm. Lastly, Seki et al 38 reported on 30 feet undergoing the minimally invasive distal osteotomy, and their findings revealed a shortening of 7.4 ± 2.5 mm.
First ray shortening is actually necessary to achieve fusion when performing TMT arthrodesis by removal of all cartilage to the subchondral plate. Johnson et al 20 found a residual layer of calcified cartilage after curettage and determined that the average depth of cartilage on each side of the first TMT joint was 0.86 mm. This makes functional alignment a priority. Historically, shortening may have been mistakenly attributed as the main cause of lesser ray overload when in fact a lack of first ray realignment in 3 dimensions may be a more likely cause. Malposition in any or all of the 3 cardinal body planes results in abnormal first ray function potentially causing a lesser MTP overload. Kaipel et al 21 evaluated a population of 91 patients (102 feet) and failed to show any biomechanical evidence supporting the theory that increased relative metatarsal length increases plantar loading parameters under the metatarsal head and predisposes patients to the development of primary metatarsalgia. 21
Traditional thinking among foot and ankle surgeons is that first ray length has an immediate and dramatic effect on lesser MTP joint overload. 15,34,42,44 The literature mostly reflects shortening of the ray as a limitation of certain procedures and advises against techniques that are perceived to produce shortening. The first ray is a complex mechanical unit composed of multiple joints spanning from the talonavicular joint to the hallux interphalangeal joint. These joints and their mechanical function are interrelated as are the soft tissues that act on the first ray. One example is the “windlass effect” of the plantar fascia, which has a profound influence on overall first ray function. 6
Our experience is that complete 3-dimensional realignment of the first ray has a more dramatic effect on preserving normal first ray function than just length. This concept has been supported by Rush et al 32 and Goldberg and Singh. 15 The authors have seen this to be true with triplane TMT arthrodesis, with the current results demonstrating minimal average shortening of the first ray of 2.4 and 3.1 mm in lateral and AP radiographs, respectively. And the incidence of lesser metatarsal overload was nonexistent at 6 months postoperation. In fact, the authors have almost completely abandoned the use of prophylactic lesser metatarsal osteotomies to prevent overload. This is in agreement with King et al, 24 who measured decreased weightbearing force under the second MTP joint or improved load-sharing following Lapidus procedure for hallux valgus. This also is substantiated by other authors using foot pressure studies. 11
Another question to consider is the methods by which we measure the first ray length. There are numerous methods to perform this task and none are universally accepted. 7,12,29,41 The most common technique is to compare the relative difference in length in AP radiographs between the first and second metatarsals distally. 7,9 Although a traditional measure, there are shortcomings with this technique because of potential variations in the sagittal plane angulation before and after both osteotomy and TMT fusion. When the first ray is dorsiflexed, it measures longer when compared to the second in an AP radiograph (Figure 7). 29 An inverse relationship is found to be true in AP radiographs when the first ray is plantarflexed. It is important to point out in these examples that there has not been a change in absolute length but rather the projection of it in 2D radiographs. A plantarflexed position of the first metatarsal is desirable from a functional standpoint and counterintuitively results in a relative shortening of the first ray on AP radiographs. Hence, for a more complete understanding of the first ray shortening, we also measured it in lateral radiographs.
Figure 7.
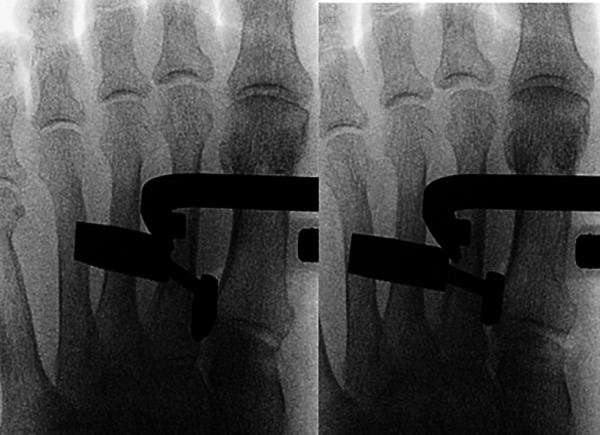
Radiographs depicting changes in AP appearance of length with first metatarsal neutral on left and dorsiflexed on right. Dorsiflexion gives the perception of elongation in a 2-dimensional AP radiograph. Conversely, in a plantarflexed position, the first metatarsal will appear as relatively shortened. AP, anteroposterior.
A length-ratio comparison of the first and second metatarsals may be more clinically applicable. 37,41 Schemitsch et al 37 stated the relative length of the first to second metatarsal should be 0.825 to avoid lesser metatarsalgia. We measured the relative lengths of the first and second rays and found a ratio postoperatively of 0.93 in our study. With the availability of weightbearing CT scans, the accuracy and/or consistency of 2-dimensional length measures could be determined. We feel it is imperative that we look at the first ray in 3 dimensions. If we only prioritize the relative length on the AP radiograph and do not look at the lateral projection or sesamoid axial view, we cannot understand the true functional position of the first ray. First-ray weightbearing function through the windlass mechanism is necessary for normal biomechanical function of this segment. 6,8,32 A stable and well-aligned first ray improves overall foot function by increasing the efficiency of the peroneus longus in stabilizing the medial column. 2 First ray malfunction may result in lesser MTP overload.
The authors acknowledge that radiographic studies have certain shortcomings, as these measurements can be affected by variations in imaging techniques. Length measurements may change based on radiographic tube angle. This calls into question not only the accuracy of the measurements but also the reproducibility and comparison of these measurements between studies. We attempted to control some of these issues by having the radiographs read by 2 independent board-certified radiologists using prescribed methodology. Future studies will incorporate 3-dimensional CT analysis and may shed light on the true significance of metatarsal length relationships following triplanar TMT arthrodesis for HV correction.
Conclusion
Triplane first TMT arthrodesis consistently had minimal bone removal and yielded satisfactory results with maintenance or even improvement in sagittal plane alignment, without any subsequent cases of lesser metatarsalgia at 6 months postoperation.
Supplemental Material
Supplemental Material, FAO960678-ICMJE for Analysis of Shortening and Elevation of the First Ray With Instrumented Triplane First Tarsometatarsal Arthrodesis by Daniel J. Hatch, Paul Dayton, William DeCarbo, Jody P. McAleer, Justin J. Ray, Robert D. Santrock and W. Bret Smith in Foot & Ankle Orthopaedics
Acknowledgments
The authors would like to thank Mindi Dayton, William Duke, Robert Taylor, Dane Wukich, Trapper Lalli, G. Tye Liu, and Shana Zink; radiologists Avneesh Chhabra and Jennifer Koay; and biostatistician Lauren Hill.
Footnotes
Ethics Approval: Ethical approval for this study was obtained from Western Institutional Review Board (IRB # 20182567).
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Daniel J. Hatch, DPM, FACFAS; Paul Dayton, DPM, FACFAS; William DeCarbo, DPM, FACFAS; Jody P. McAleer, DPM, FACFAS; Robert D. Santrock, MD; W. Bret Smith, DO, MS report grants and personal fees from Treace Medical Concepts, Inc., during the conduct of the study. ICMJE forms for all authors are available online.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The data in this study is an interim look at the data from the ALIGN3D registered clinical trial, which is funded by Treace Medical Concepts, Inc: NCT03740282.
Supplemental Material: A supplemental video for this article is available online.
ORCID iD: Justin J. Ray, MD,  https://orcid.org/0000-0001-7349-8979
https://orcid.org/0000-0001-7349-8979
References
- 1. Ahn J, Lee HS, Seo JH, Kim JY. Second metatarsal transfer lesions due to first metatarsal shortening after distal chevron metatarsal osteotomy for hallux valgus. Foot Ankle Int. 2016;37(6):589–595. [DOI] [PubMed] [Google Scholar]
- 2. Bierman RA, Christensen JC, Johnson CH. Biomechanics of the first ray. Part III. Consequences of lapidus arthrodesis on peroneus longus function: a three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2001;40(3):125–131. [DOI] [PubMed] [Google Scholar]
- 3. Boffeli TJ, Hyllengren SB. Can we abandon saw wedge resection in Lapidus fusion? A comparative study of joint preparation techniques regarding correction of deformity, union rate, and preservation of first ray length. J Foot Ankle Surg. 2019;58(6):1118–1124. [DOI] [PubMed] [Google Scholar]
- 4. Carr CR, Boyd BM. Correctional osteotomy for metatarsus primus varus and hallux valgus. J Bone Joint Surg Am. 1968;50(7):1353–1367. [PubMed] [Google Scholar]
- 5. Catanzariti AR, Mendicino RW, Lee MS, Gallina MR. The modified Lapidus arthrodesis: a retrospective analysis. J Foot Ankle Surg. 1999;38(5):322–332. [DOI] [PubMed] [Google Scholar]
- 6. Chan F, Bowlby MA, Christensen JC. Medial column biomechanics: nonsurgical and surgical implications. Clin Podiatr Med Surg. 2020;37(1):39–51. [DOI] [PubMed] [Google Scholar]
- 7. Chauhan D, Bhutta MA, Barrie JL. Does it matter how we measure metatarsal length? Foot Ankle Surg. 2011;17(3):124–127. [DOI] [PubMed] [Google Scholar]
- 8. Coughlin MJ, Jones CP, Viladot R, et al. Hallux valgus and first ray mobility: a cadaveric study. Foot Ankle Int. 2004;25(8):537–544. [DOI] [PubMed] [Google Scholar]
- 9. Cronin S, Conti M, Williams N, Ellis SJ. Relationship between demographic and radiographic characteristics and second ray pathology in hallux valgus patients. Foot Ankle Orthop. 2020;5(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dahlgren N, Johnson JL, Huntley SR, et al. First tarsometatarsal fusion using saw preparation vs. standard preparation of the joint: a cadaver study. Foot Ankle Orthop. Published online October 28, 2019. doi:10.1177/2473011419S00154 [DOI] [PubMed] [Google Scholar]
- 11. Dietze A, Bahlke U, Martin H, Mittlmeier T. First ray instability in hallux valgus deformity: a radiokinematic and pedobarographic analysis. Foot Ankle Int. 2013;34(1):124–130. [DOI] [PubMed] [Google Scholar]
- 12. Domínguez G MPV. Metatarsus adductus angle in male and female feet: normal values with two measurement techniques. J Am Podiatr Med Assoc. 2008;98(5):364–369. [DOI] [PubMed] [Google Scholar]
- 13. Fleming JJ, Kwaadu KY, Brinkley JC, Ozuzu Y. Intraoperative evaluation of medial intercuneiform instability after Lapidus arthrodesis: intercuneiform hook test. J Foot Ankle Surg. 2015;54(3):464–472. [DOI] [PubMed] [Google Scholar]
- 14. Fleming L, Savage TJ, Paden MH, Stone PA. Results of modified Lapidus arthrodesis procedure using medial eminence as an interpositional autograft. J Foot Ankle Surg. 2011;50(3):272–275. [DOI] [PubMed] [Google Scholar]
- 15. Goldberg A, Singh D. Treatment of shortening following hallux valgus surgery. Foot Ankle Clin. 2014;19(2):309–316. [DOI] [PubMed] [Google Scholar]
- 16. Grebing BR, Coughlin MJ. Evaluation of Morton’s theory of second metatarsal hypertrophy. J Bone Joint Surg Am. 2004;86(7):1375–1386. [DOI] [PubMed] [Google Scholar]
- 17. Harris RI, Beath T. The short first metatarsal. J Bone Joint Surg. 1949;31(3):553–565. [PubMed] [Google Scholar]
- 18. Hatch DJ, Santrock RD, Smith B, Dayton P, Weil L. Triplane hallux abducto valgus classification. J Foot Ankle Surg. 2018;57(5):972–981. [DOI] [PubMed] [Google Scholar]
- 19. Helal B. Surgery for adolescent hallux valgus. Clin Orthop Relat Res. 1981;(157):50–63. [PubMed] [Google Scholar]
- 20. Johnson JT, Schuberth JM, Thornton SD, Christensen JC. Joint curettage arthrodesis technique in the foot: a histological analysis. J Foot Ankle Surg. 2009;48(5):558–564. [DOI] [PubMed] [Google Scholar]
- 21. Kaipel M, Krapf D, Wyss C. Metatarsal length does not correlate with maximal peak pressure and maximal force. Clin Orthop Relat Res. 2011;469(4):1161–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Karataglis D, Dinley RJ, Kapetanos G. Comparative study between Wilson and Mitchell metatarsal osteotomies for the treatment of hallux valgus in adults. Acta Orthop Belg. 2001;67(2):149–156. [PubMed] [Google Scholar]
- 23. Kimura T, Kubota M, Taguchi T, Suzuki N, Hattori A, Marumo K. Evaluation of first-ray mobility in patients with hallux valgus using weight-bearing CT and a 3-D analysis system: a comparison with normal feet. J Bone Joint Surg Am. 2017;99(3):247–255. [DOI] [PubMed] [Google Scholar]
- 24. King CM, Hamilton GA, Ford LA. Effects of the lapidus arthrodesis and chevron bunionectomy on plantar forefoot pressures. J Foot Ankle Surg. 2014;53(4):415–419. [DOI] [PubMed] [Google Scholar]
- 25. McInnes BD, Bouché RT. Critical evaluation of the modified Lapidus procedure. J Foot Ankle Surg. 2001;40(2):71–90. [DOI] [PubMed] [Google Scholar]
- 26. Merkel KD, Katoh Y, Johnson EW, Chao EY. Mitchell osteotomy for hallux valgus: long-term follow-up and gait analysis. Foot Ankle. 1983;3(4):189–196. [DOI] [PubMed] [Google Scholar]
- 27. Morton DJ. The Human Foot: Its Evolution, Physiology and Functional Disorders. New York: Columbia University Press; 1935. [Google Scholar]
- 28. Nilsonne H. Hallux rigidus and its treatment. Acta Orthop Scand. 1930;1(1-4):295–303. [Google Scholar]
- 29. Osher L, Blazer MM, Buck S, Biernacki T. Accurate determination of relative metatarsal protrusion with a small intermetatarsal angle: a novel simplified method. J Foot Ankle Surg. 2014;53(5):548–556. [DOI] [PubMed] [Google Scholar]
- 30. Perren S. Evolution of the internal fixation of long bone fractures. J Bone Joint Surg B. 2002;84(8):1093–1110. [DOI] [PubMed] [Google Scholar]
- 31. Ray JJ, Koay J, Dayton PD, Hatch DJ, Smith B, Santrock RD. Multicenter early radiographic outcomes of triplanar tarsometatarsal arthrodesis with early weightbearing. Foot Ankle Int. 2019;40(8):955–960. [DOI] [PubMed] [Google Scholar]
- 32. Rush SM, Christensen JC, Johnson CH. Biomechanics of the first ray. Part II: metatarsus primus varus as a cause of hypermobility. A three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2000;39(2):68–77. [DOI] [PubMed] [Google Scholar]
- 33. Saffo G, Wooster MF, Stevens M, Desnoyers R, Catanzariti AR. First metatarsocuneiform joint arthrodesis: a five-year retrospective analysis. J Foot Surg. 1989;28(5):459–465. [PubMed] [Google Scholar]
- 34. Sammarco GJ, Idusuyi OB. Complications after surgery of the hallux. Clin Orthop Relat Res. 2001;391:59–71. [DOI] [PubMed] [Google Scholar]
- 35. Sangeorzan BJ, Hansen ST, Jr. Modified Lapidus procedure for hallux valgus. Foot Ankle. 1989;9(6):262–266. [DOI] [PubMed] [Google Scholar]
- 36. Santrock RD, Smith B. Hallux valgus deformity and treatment: a three-dimensional approach: modified technique for Lapidus procedure. Foot Ankle Clin. 2018;23(2):281–295. [DOI] [PubMed] [Google Scholar]
- 37. Schemitsch E, Horne G. Wilson’s osteotomy for the treatment of hallux valgus. Clin Orthop Relat Res. 1989;240:221–225. [PubMed] [Google Scholar]
- 38. Seki H, Oki S, Suda Y, et al. Three-dimensional analysis of the first metatarsal bone in minimally invasive distal linear metatarsal osteotomy for hallux valgus. Foot Ankle Int. 2020;41(1):84–93. [DOI] [PubMed] [Google Scholar]
- 39. Smith WB, Dayton P, Santrock RD, Hatch DJ. Understanding frontal plane correction in hallux valgus repair. Clin Podiatr Med Surg. 2018;35(1):27–36. [DOI] [PubMed] [Google Scholar]
- 40. Smith WB, Santrock RD, Hatch DJ, Dayton P. Intraoperative multiplanar alignment system to guide triplanar correction of hallux valgus deformity. Tech Foot Ankle Surg. 2017;16(4):175–182. [Google Scholar]
- 41. Tanaka Y, Takaura Y, Kumai T, Samoto N, Tamai S. Radiographic analysis of hallux valgus: a two dimensional coordinate system. J Bone Joint Surg Am. 1995;77(2):205–213. [DOI] [PubMed] [Google Scholar]
- 42. Tóth K, Huszanyik I, Kellermann P, Boda K, Róde L. The effect of first ray shortening in the development of metatarsalgia in the second through fourth rays after metatarsal osteotomy. Foot Ankle Int. 2007;28(1):61–63. [DOI] [PubMed] [Google Scholar]
- 43. Usuelli F, Palmucci M, Montrasio UA, Malerba F. Radiographic considerations of hallux valgus versus hallux rigidus. Foot Ankle Int. 2011;32(8):782–788. [DOI] [PubMed] [Google Scholar]
- 44. Walker AK, Harris TG. The role of first ray insufficiency in the development of metatarsalgia. Foot Ankle Clin. 2019;24(4):641–648. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, FAO960678-ICMJE for Analysis of Shortening and Elevation of the First Ray With Instrumented Triplane First Tarsometatarsal Arthrodesis by Daniel J. Hatch, Paul Dayton, William DeCarbo, Jody P. McAleer, Justin J. Ray, Robert D. Santrock and W. Bret Smith in Foot & Ankle Orthopaedics