Highlights
-
•
Food insecurity and CVD share a circular association.
-
•
Association may be stronger for racial/ethnic minorities and single mothers.
-
•
Greater investment and organization are needed to address this association.
-
•
Targeting food insecurity may reduce the nationwide burden of CVD.
Abstract
Food insecurity (FI) – a state of limited access to nutritionally adequate food – is notably more prominent among patients with cardiovascular disease (CVD) than the general population. Current research suggests that FI increases the risk of cardiovascular morbidity and mortality through various behavioral and biological pathways. Importantly, FI is more prevalent among low-income households and disproportionately affects households with children, particularly those led by single mothers. These disparities necessitate solutions specifically geared towards helping these high-risk subgroups, who also experience increased risk of CVD associated with FI. Further, individuals with CVD may experience increased risk of FI due to the financial burden imposed by CVD care. While participation in federal aid programs like the Supplemental Nutrition Assistance Program and the Special Supplemental Nutrition Program for Women, Infants, and Children has been associated with cardiovascular health benefits, residual FI and lower dietary quality among many families suggest a need for better outreach and expanded public assistance programs. Healthcare systems and community organizations can play a vital role in screening individuals for FI and connecting them with food and educational resources. While further research is needed to evaluate sociodemographic differences in the FI-CVD relationship, interventions at the policy, health system, and community levels can help address both the burden of FI and its impacts on cardiovascular health.
1. Introduction
Food insecurity (FI) is a state defined by insufficient access to nutritionally adequate food [1]. Nearly 38.3 million individuals in the United States (US) experience FI, which is associated with poor health outcomes and is posited as a risk factor for cardiovascular disease (CVD) [2]. CVD is the leading cause of morbidity and mortality in the US, affecting nearly 9.3% of the total population and accounting for 25% of all deaths [3,4]. Prior studies have reported an association between adverse social determinants of health – such as low education, low income, neighborhood deprivation, and others – and increased risk of both CVD and cardiovascular mortality [[5], [6], [7]]. Various socioeconomic and environmental factors interact to impact the risk of FI [2,8], which may, in turn, influence the risk of CVD via factors such as diet, weight, blood glucose, cholesterol, and blood pressure (Fig. 2) [9].
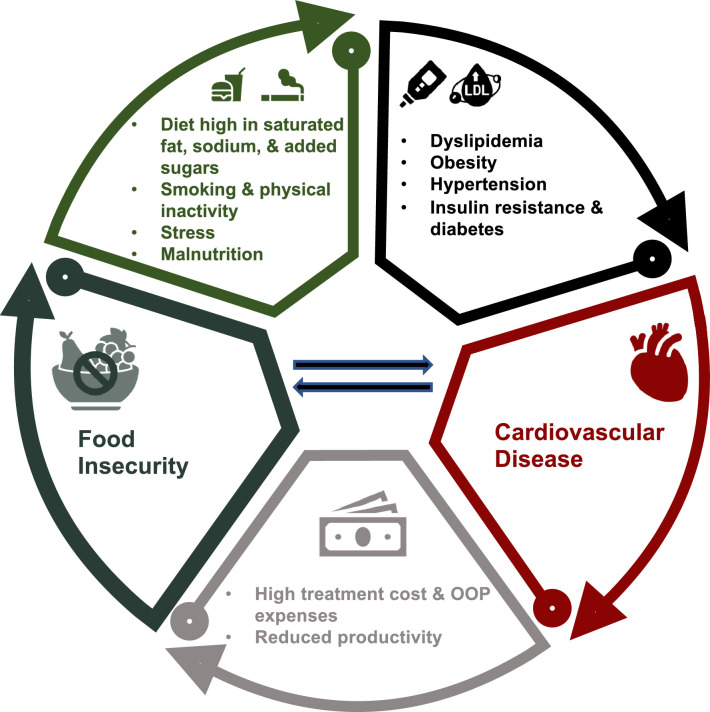
Fig. 2.
Central Illustration. The association between FI and CVD may be explained by pathways in which both conditions increase risk of the other. Food-insecure individuals may consume greater amounts of unhealthy food, including those with added sugars, high saturated fat content, and excess sodium. Individuals experiencing FI are also more likely to smoke and have low physical activity, further revealing FI's significant impact on behavioral risk factors for CVD. These lifestyle factors, combined with psychological stress and poor nutrient intake, ultimately increase risk of CVD by promoting the development of conditions such as diabetes, obesity, hypertension, and dyslipidemia. It has also been suggested that CVD can, in turn, increase patients’ risk of being food insecure due to the financial strain associated with treatment costs and reduced productivity.
Current evidence suggests FI is more common among patients with hypertension, coronary heart disease, and atherosclerotic CVD (ASCVD) than those without CVD [10,11]. The financial burden of care predisposes CVD patients to higher risk of FI, thus establishing a potential bidirectional relationship between FI and CVD [12]. With the ongoing COVID-19 pandemic resulting in a further rise in FI in the US [13,14], it is of paramount importance to understand the relationship between FI, cardiovascular risk factors, and CVD. Furthermore, while patterns of CVD vary considerably by age, sex, and race/ethnicity, little is known about variation in FI burden or the FI-CVD association by these key sociodemographic factors, or by marital and parental status.
This review discusses the determinants and current burden of FI in the US, and the pathways, mechanisms, and sociodemographic variation in the association between FI and CVD. We analyze existing programs to help alleviate FI, identify potential gaps in policy and practice, and propose evidence-based policy, community, and healthcare level interventions to address FI and reduce the burden of CVD. This is important to improve the current understanding of the relationship between FI and CVD and inform targeted approaches to address the challenges and barriers related to FI in vulnerable populations.
2. Food insecurity: measurement, current burden, and recent trends
2.1. Measurement
According to the US Department of Agriculture (USDA), food insecurity can be defined as low food security, which is characterized by “reduced quality, variety, or desirability of diet” with little reduction in food intake, or very low food security, which is indicated by disrupted eating patterns and reduced food intake (Table 1) [1]. The USDA employs the 10-question Household Food Security Module survey (18 for households with children) to determine a household's food security status [15]. The validated survey has been used to inform FI measurement models in 146 countries worldwide [[16], [17], [18]]. Clinicians and researchers screening for FI often use the 2-item Hunger Vital Sign survey as an alternative, which yields high sensitivity (96.7%) and specificity (86.2%) compared to the “gold standard” 18-item survey [19].
Table 1.
Levels of food security and their definitions.
| Level of FI | USDA Definition |
|---|---|
| High Food Security | No problems, or anxiety over, access to food. Considered food secure. |
| Marginal Food Security | Anxiety over food sufficiency and/or some problems accessing food, but no substantial change in quality or quantity of food consumed. Considered food secure. |
| Low Food Security | Reduced quality, variety, or desirability of diet, but with limited impact on food intake and eating patterns. Considered food insecure. |
| Very Low Food Security | Significant problems accessing food, such that there are multiple indications of disrupted eating patterns and reduced food intake. Considered food insecure. |
The USDA recently developed a shorter questionnaire to assess food insufficiency, a state in which a household does not have enough to eat in the past 7 days [15]. While there is overlap between FI and food insufficiency (for example, very low food security often coincides with low food sufficiency), food insufficiency reflects a more severe state in which a household does not have enough food for subsistence [15]. In addition, FI takes into account other variables, such as dietary quality and variety, anxiety over food access, and amount of food consumed. FI thus enables a more comprehensive measurement of long-term food access and dietary quality, whereas food insufficiency can help assess rapid changes in a household's food consumption. Both measures have been used in previous literature to assess the burden of limited food access, as well as its relationship with health outcomes [20,21].
2.2. Determinants and current burden
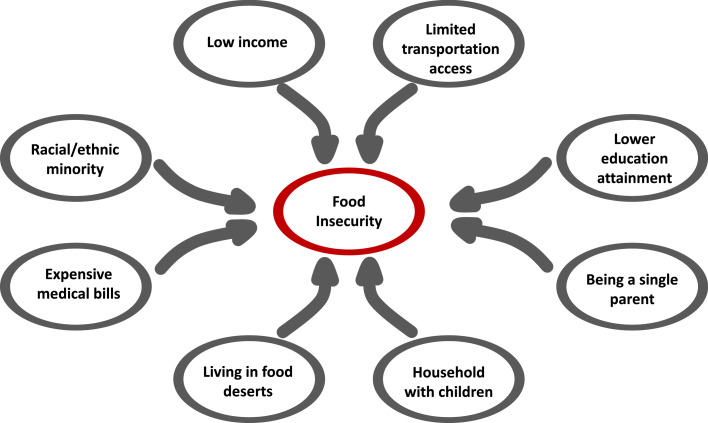
FI affected approximately 38.3 million Americans in 2020, accounting for 10.5% of US households and with a disproportionate impact on socially and economically disadvantaged populations [2,13]. FI has a higher prevalence among low-income households, affecting 28.6% and 33.1% of households with incomes <185% and <130% of the poverty threshold, respectively [2]. These socioeconomic disparities also coincide with educational attainment: 61% of older adults with a high school or less education were found to be food insecure compared to just 13.6% of those who graduated college [22]. Changes in employment status, lack of a personal vehicle, and limited access to public transportation have also been linked to FI and self-reported difficulties in accessing food (Fig. 1) [23].
Fig. 1.
Socioeconomic Risk Factors of Food Insecurity. Multiple socioeconomic factors intersect to increase risk of food insecurity. Living in an area with limited access to nutritious food and lacking transportation can both make it difficult for families to easily purchase nutritionally adequate foods. Low educational attainment and income are associated with higher risk of food insecurity. Family structure is also an important determinant because households with children (particularly those led by single parents) are more likely to be food insecure than households without children.
Prior evidence indicates that women are significantly more likely to report being food insecure than men [11]. Furthermore, among adults living alone, non-elderly men and women (11.0–11.4%) are more likely to be food insecure than the elderly (8.3%) [2]. This trend holds true for ASCVD patients, as FI is more common in nonelderly adults (25.9% for those between 18 and 39 years and 22.9% for those between 40 and 64 years) than in the elderly (7.8% for those 65 years and above) [11]. FI prevalence rates also vary considerably by household composition and marital and parental status. In 2020, households with children had higher rates (14.8%) compared to the US average (10.5%). FI rates were particularly high in families led by single men (16.3%) and single women (27.7%) [2], compared to households with children raised by married couples (9.5%). FI rates for adults living alone were fairly close to the national average (11.0% for women living alone and 11.4% for men living alone), while only 7.1% of households with more than 1 adult (but no children) were food insecure in 2020 [2].
Furthermore, there are notable racial/ethnic inequities in FI burden. In 2020, FI prevalence was considerably higher among non-Hispanic Black (NHB) (21.7%) and Hispanic (17.2%) households when compared to the national average (10.5%) and non-Hispanic white (NHW) households (7.1%). Additionally, a study of over 190,000 US adults with ASCVD found that the prevalence of FI was higher in NHB (30.1%) and Hispanic (23.4%) individuals compared to NHW patients (10.7%) [11]. The same study also found NHB or Hispanic ethnicity increased risk of FI among adults without ASCVD [11]. As of March 2021, greater than 20% of NHB and Hispanic households also reported that their children sometimes or often did not have enough to eat [24], as opposed to 10.1% of NHW households. Data from the Urban Institute's Health Reform Monitoring Survey further suggests that, in 2021, NHB (19.6%) and Hispanic households (25.7%) were still much more likely to be food insecure than NHW (11.7%) households [25].
2.3. Recent trends in the US
The nationwide prevalence of FI had a significant yearly decline from 14.9% in 2011 to 10.5% in 2019 [2]. However, this downward trend stopped in 2020, during which FI prevalence remained at 10.5%, per the CDC [2]. However, findings from the Household Pulse Survey suggest that FI rates doubled between February 2020 and April 2020, with 23% of all households experiencing FI; these rates tripled for households with children [20]. Other data suggest a more moderate, yet still notable, increase in FI [13]. This increase in FI prevalence, in conjunction with existing issues such as access to care, stable housing, and more, may predict poorer cardiovascular outcomes for high-risk population subgroups, including low-income families and racial/ethnic minorities [25].
3. Food insecurity and CVD
3.1. Current evidence
There is evidence of a possible bidirectional association between FI and CVD, with some evidence suggesting that healthcare costs associated with CVD may increase the likelihood of being food insecure [12]. According to a recent USDA study, the prevalence of CVD was 6 times higher in households with very low food security compared to food-secure households [26]. Individuals with very low food security were also found to have 2.36 times higher odds of having a 10-year CVD risk >20% compared to food-secure individuals [27]. FI is also associated with higher likelihood of cardiovascular mortality. An analysis of data from more than three thousand US counties estimated that an increase in a county's FI rate corresponded with an increase in the county's age-adjusted cardiovascular mortality rate [28]. Another survey of 27,188 US adults found that increasing severity of FI was associated with increased risk of cardiovascular and all-cause mortality, with participants experiencing very low food security having a 1.53-fold increased risk of cardiovascular mortality, compared to food-secure participants [29].
It has also been observed that individuals with ASCVD who reported being unable to pay their medical bills had nearly three-fold higher odds of experiencing FI than patients who were able to afford their bills [30]. The authors concluded that the financial burden associated with CVD treatment may increase likelihood of being food insecure, even after adjustment for insurance status. The nationwide prevalence of CVD, which was 41.5% in 2015, is projected to increase to 45.1% by 2035, while total costs for CVD are expected to increase by about 50%, setting the stage for increased financial burden – the negative impact of healthcare expenses on a patient's well-being – and FI [31]. Future study should longitudinally explore correlates of the reported FI-CVD association, including access to care, insurance type, and socioeconomic status.
3.2. Pathways and mechanisms
Multiple proposed pathways may explain the link between FI and CVD. To maximize caloric intake and avoid hunger, people in food-insecure households may consume more energy-dense, nutrient-poor foods, such as those high in refined carbohydrates, added fats, and sodium, which, calorie for calorie, cost less than more nutrient-dense foods [32]. Indeed, FI is associated with high intake of sugar-sweetened beverages and processed meats, along with low consumption of fruits and vegetables [33]. Such dietary habits are known risk factors for CVD and associated cardiovascular mortality [34,35]. Studies have also shown FI increases risk of obesity and diabetes, which is thought to result in part from unhealthy dietary choices [36,37]. Ultimately, these metabolic conditions increase risk for CVD, suggesting FI's association with CVD is mediated through worse diet quality and increased weight (Fig. 2) [38,39]. FI is associated with other behavioral risk factors for CVD, such as physical inactivity and smoking [40–42]. Additionally, food-insecure patients have reported poor medication adherence to better afford food or, conversely, forgoing heart-healthy foods to pay for medication and treatment [32].
An unhealthy diet in childhood is associated with CVD risk factors and early vascular changes in adulthood [43], [44], [45]. Unhealthy diets arising from FI can promote higher BMIs in children, which further increases risk of heart disease and atherosclerosis independent of BMI in adulthood [46]. FI is also associated with binging and overconsumption when food is available, which results in greater body fat accumulation in anticipation of future periods of food scarcity [32]. It has been hypothesized that children raised in food-insecure or impoverished households carry such behaviors into adulthood, providing another possible behavioral explanation for the link between childhood nutrition and adult cardiovascular risk [47]. Future prospective studies should explore the validity of this theory to better inform nutritional recommendations for children.
Stress can further increase risk of CVD via elevated blood pressure and heart rate [48]. Indeed, psychosocial stress and depressive symptoms stemming from adverse socioeconomic conditions such as FI have been associated with increased risk of CVD [39,49]. Poor nutrition caused by FI further increases cardiovascular risk, as deficiencies in calcium, magnesium, folate, and various vitamins have been linked to increased likelihood of heart failure [50]. Deficiency of these key micronutrients impairs the heart's physiologic metabolic reactions and promotes oxidative stress, resulting in a loss of cardiac muscle mass and function [51]. It has also been reported that prenatal nutrition may impact a child's future cardiovascular health: fetal malnutrition (stemming from poor maternal nutrition) may favor hypertension in adulthood, aligning with the theory that nutrition can dictate “fetal programming” [52,53]. Indeed, epigenetic changes associated with malnutrition and stress have been associated with elevated risk of CVD and CVD risk factors in adulthood [54]. FI thus represents a significant contributor to multiple cardiovascular risk factors that is likely mediated through behavioral and dietary changes (Fig. 2) [55].
It is known that CVD may impose financial strain on individuals and families, creating conditions for economic instability and potentially increasing risk of FI [12]. Recent evidence suggests that 45% of families with a member with ASCVD may experience significant difficulty paying medical bills, while 20% of ASCVD patients are unable to pay their medical bills [12]. The financial burden associated with CVD treatment, which varies widely based on the disease but is estimated to be about $18,953 per patient per year, can worsen a patient's ability to purchase nutritionally-adequate food [56]. Reduced productivity associated with CVD may further increase risk of FI by impairing a patient's ability to work and generate income for food and CVD treatment [57].
3.3. Variation by sociodemographic factors
The following subsections describe evidence for variations in the FI-CVD association by age, sex, race/ethnicity, and marital/parental status. Understanding such variations can help identify subgroups that are more vulnerable to FI's influence on cardiovascular risk and inform future interventions.
3.3.1. Age
An analysis of 10,455 US adults determined that FI was associated with increased 10-year cardiovascular risk for adults aged 30–59, but not adults above 60, after adjustment for race/ethnicity, BMI, educational status, health insurance status, and alcohol use [58]. It has been documented that older adults tend to eat less than younger adults, suggesting FI's impact on food access may be more severe for younger adults who consume more calories and thus require a greater quantity of nutritionally adequate food [59]. A separate longitudinal study found that very low food security was associated with higher risk of cardiovascular mortality for adults over 65 but not for those under 65 [29]. This disparity may be due to the elderly being at greater risk for CVD and overall mortality. Greater prospective evidence is needed to fully understand the cumulative effects of FI on cardiovascular health over time [60].
3.3.2. Sex
There is also some evidence suggesting that the FI-CVD association may be stronger for women than men. A large prospective study of US adults found that very low food security was associated with a significantly higher risk of cardiovascular mortality in women, but not men [29]. Similarly, a study of low-income immigrant adults found statistically-significant associations between FI and coronary heart disease, angina pectoris, and myocardial infarction for women, but not men, even after adjustment for family size and number of children in the household [21]. Food-insecure women also had higher odds of myocardial infarction (OR = 4.05) than food-insecure men (OR = 1.45), as well as higher odds of coronary heart disease (OR = 1.86 versus OR = 1.34) [21]. This disparity may be due to the greater association between FI and dyslipidemia and obesity among women [42,61]; however, the sex-based differences in CVD risk are complex and multifactorial [62]. Further research is needed to better explore possible behavioral and physiological factors that may explain these observed differences.
3.3.3. Race/Ethnicity
FI may pose a higher cardiovascular risk for racial and ethnic minorities, relative to their NHW counterparts, due to the generally higher rates of clinical risk factors such as diabetes, hypertension, and obesity, all of which contribute to worse cardiovascular outcomes [63]. Structural barriers, such as socioeconomic inequality, educational disparities, and bias and discrimination in healthcare, as well as historical practices like redlining – which subjects Black and other under-represented racial/ethnic populations to discrimination in housing – have been reported to contribute to the disproportionately higher rates of cardiovascular risk factors and CVD among racial/ethnic minorities, compared to NHW individuals [64,65].
Due to various socioeconomic constraints, it is known that NHB and Hispanic individuals are more likely to live in “food deserts,” which are areas with limited access to healthy foods, or “food swamps,” which have a disproportionately high density of fast food restaurants and convenience stores [66]. These disparities in healthy food access may thus worsen dietary quality and potentially exacerbate the burden of FI on racial/ethnic minorities [[67], [68], [69]]. Indeed, a study of 8169 women found that very low food security was associated with increased risk for obesity in NHB, Hispanic, and Asian women, but not in NHW women [70]. The stronger association between FI and obesity is supported by the higher rates of obesity among food-insecure NHB (46.1%) and Hispanic (35.7%) individuals than food-insecure NHW (32.6%) people [36].
In contrast, another longitudinal study reported that very low food security was associated with increased cardiovascular mortality risk in NHW individuals but not in non-White individuals. Variations in the FI-CVD association by race/ethnicity remain relatively under-documented in the literature. Future studies should examine racial/ethnic differences in the FI-CVD association in light of additional risk factors such as access to care, age, income and wealth, living and working conditions, and social support [29].
3.3.4. Marital and parental status
Married and divorced/widowed/separated adults with FI are more likely to be obese than never-married, food-insecure adults [36]. This is consistent with findings that FI is related to a greater likelihood of obesity among married women and widows than never-married women, which suggests that FI may have a greater impact on married and widowed adults’ cardiovascular health than never-married adults [71].
Single-parent – especially single-mother – households are more likely to experience FI than two-parent households [2]. It has been hypothesized that during times of financial stress, mothers are more likely than fathers to deprive themselves of food to support their children, resulting in unhealthy dietary behaviors that increase their risk of obesity and CVD [71,72]. The increased burden of FI on mothers may explain the higher prevalence of obesity and overweight status in this population, compared to both men and women without children, as well as food-insecure fathers [73]. The risk of obesity is further exacerbated for food-insecure single mothers relative to food-insecure, married parents and is hypothesized to increase for food-insecure single fathers as well, although the latter demographic remains poorly understood due to a lack of data on single fathers [73]. While these associations suggest parenthood and separation from one's partner may increase FI's impact on obesity and cardiovascular health, future studies should further explore possible confounding factors such as education and socioeconomic status, which may help elucidate if and why the FI/CVD association is stronger for single mothers and fathers.
4. Knowledge gaps, opportunities for interventions, and future directions
4.1. Research
Current literature supports evidence of the adverse effects of FI on CVD (and vice versa), but with notable limitations. Many studies employ a cross-sectional design, which limits the ability to establish a causal link between FI and CVD. Thus, more prospective studies should be conducted to better elucidate the temporal sequence and long-term impact of food insecurity on cardiovascular health [55]. This is particularly relevant for evaluating risk factors – such as whether food-insecure women are at greater risk of developing dyslipidemia than their male counterparts – and establishing a stronger causal relationship between FI and CVD [42]. Furthermore, there is some inconsistency in how FI is measured across studies; while most studies use the USDA or Hunger Vital Sign surveys, some rely on estimates from nonprofit food aid organizations or other surveying methods [27,28]. Future studies should use the validated USDA 18-item FI screening tool or the 2-item Hunger Vital Sign survey to allow comparability of findings across study designs and target populations. The intersections of FI with factors such as family structure, race/ethnicity, and age should also be studied to evaluate unique cardiovascular risk levels for different demographic subgroups.
4.2. Policy
Multiple federal aid programs exist to address the widespread problem of FI (Table 2). The Supplemental Nutrition Assistance Program (SNAP) – the nation's primary food assistance initiative – supplements low-income families’ food budgets with monthly benefits while providing nutrition counseling and dietary educational programs [74]. On average, receipt of SNAP benefits reduces the likelihood of being food insecure by 30%, and the likelihood of being very food insecure by 20% [75]. Participants report better health than non-recipients and have fewer sick days and doctor visits [76]. Furthermore, children receiving SNAP benefits experience lower risk of heart disease, diabetes, and hypertension in adulthood compared to those not enrolled in SNAP [77]. However, the average diet of a SNAP participant still fails to meet the USDA's Dietary Guidelines for Americans, possibly due to SNAP's lack of regulations on the foods that participants can purchase [78]. Furthermore, benefits are allotted based on national average prices for a low-cost, nutritious diet, so they are sometimes inadequate for participants living in areas with higher food prices [78]. In fact, even with expanded benefits in 2021, the average SNAP participant received $210.07 per month, which equals about $7 per day [79]. SNAP benefits also do not account for time constraints on meal preparation, a particularly noteworthy limitation for single parent households that may lack the time to prepare meals from scratch [78].
Table 2.
Federal aid programs targeting food insecurity.
| Acronym | Full Name | Benefits | Eligible Groups |
|---|---|---|---|
| SNAP [74] | Supplemental Nutrition Assistance Program | Financial assistance to purchase:
|
Anyone living in a household below a certain income and resource threshold (varies by state) |
| WIC [80] | Women, Infants, and Children |
|
|
| TEFAP [81] | The Emergency Food Assistance Program |
|
|
| NSLP [82] | National School Lunch Program |
|
|
Because over half of households receiving SNAP benefits are food insecure, additional approaches to addressing FI have been proposed, such as expansion of SNAP benefits and eligibility and development of additional public benefit programs targeted at vulnerable households, particularly those with children [83]. The continued prevalence of FI among high-risk, low-income households demands further investment and political prioritization to fund nutrition programs, which can help expand food access and reduce the risk of CVD (Table 3). In fact, the US IMPACT Food Policy Model projected that a 30% fruit and vegetable subsidy for low-income SNAP participants, coupled with a 10% price reduction in fruits and vegetables, could prevent approximately 230,000 deaths from CVD by 2030 [3]. Researchers from Stanford performed a cost-effectiveness analysis of an expanded fruit/vegetable SNAP subsidy, which found that such a financial incentive would also save costs through long-term reductions in diabetes and CVDs [84].
Table 3.
Recommendations for addressing gaps in the food insecurity/cardiovascular disease association.
| Level | Gaps | Recommendations |
|---|---|---|
| Research |
|
|
| Policy/Aid |
|
|
| Community |
|
|
| Healthcare Systems |
|
Given the higher rates of FI among households with children, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is also worth examining. WIC offers financial benefits and various counseling programs to participants [80]. Although current research suggests WIC participation has a positive impact on participants’ health [85], WIC participation has declined over the past four years, with 2020 recording the lowest number of participants despite increases in FI [86]. Additionally, unlike SNAP, WIC limits the types of foods participants can purchase with their benefits [80], which may contribute to WIC's poor retention rate, currently reported at about 55% at 6-month follow-up [87]. Social stigma, difficulty enrolling, and misinformation have all been cited as reasons women do not participate in WIC [88]. Thus, increasing WIC outreach and making benefits usable online could increase participation while also making the grocery shopping experience more convenient and stigma-free (Table 3) [89].
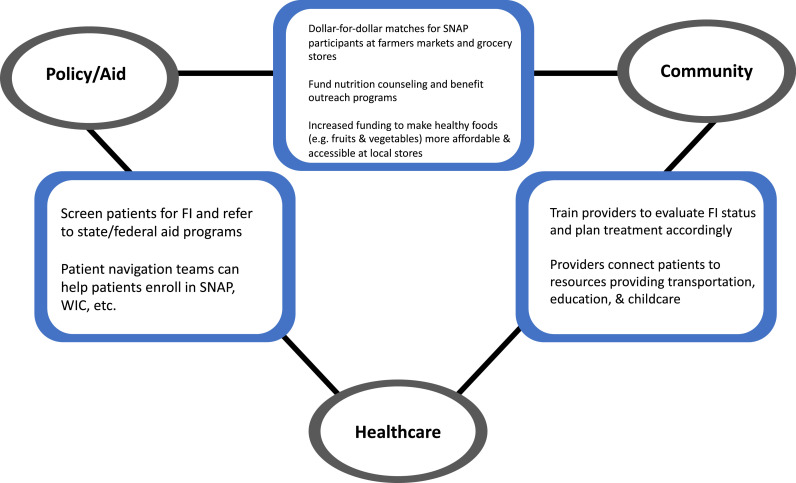
4.3. Community
Local community-based initiatives – such as nutrition counseling and education programs, community gardens, and farmers markets – have been shown to help alleviate the burden of FI [90]. Increased local and federal funding can help community food pantries and other vendors provide healthy foods to a wide range of clients, while nutrition education programs can inform patients on how to incorporate these healthier foods into their diet [90]. Collaboration among community and federal organizations may also have potential, such as dollar-for-dollar “matches” for SNAP consumers at farmers markets, which have resulted in more participants purchasing fresh local produce (Fig. 3) [78]. Increased federal funding for nutrition education and counseling programs may also be helpful, as such programs have been shown to improve cardiovascular risk profile; for example, women participating in a California nutrition counseling program experienced greater improvements in 10-year coronary heart disease risk than women who did not participate in the program [91].
Fig. 3.
Partnerships to Address the Burden of Food Insecurity on Cardiovascular Health. While challenges to food insecurity exist in the realms of policy, community, and healthcare, there are also opportunities for collaboration to address these problems in an interdisciplinary manner. For example, local farmers markets can encourage SNAP participants to spend their benefits on fruits and vegetables by offering dollar-for-dollar matches on fresh produce. Meanwhile, healthcare providers can connect patients to community organizations that help with transportation, education, and childcare, all of which can be barriers to food access. Patient navigation teams within the clinical setting can also establish connections with the federal area by helping patients enroll in SNAP, WIC, and other federal assistance programs.
Such community-oriented solutions should also take into account the food resources in a given area's built environment, particularly in food deserts and food swamps, both of which are present in many low-income neighborhoods [66]. While adding more supermarkets to these areas can mitigate the likelihood of FI, current research suggests it is insufficient in improving dietary quality [92,93]. One study found that differential local supermarket density only accounts for about 1.5% of the difference in healthy eating between low- and high-income households, while a subsidy for healthy groceries represents a more effective method to improve dietary quality [93], [94]. Food access initiatives should thus focus on improving quality of food at existing retailers and creating incentives to purchase healthy foods, as opposed to merely increasing access to stores that do not offer enough nutritious food. Community gardens and farmers markets have been shown to help improve access to fresh produce, integrating nutritious food access into the community's built environment while encouraging participation in aid programs like SNAP [78,95]. Given the reduced cardiovascular risk associated with increased fruit and vegetable intake, increasing fruit and vegetable access via these community initiatives would improve both food security status and cardiovascular health [96]. Alternatives to simply opening more grocery stores in low access areas, such as sugary drink taxes and local nutrition education programs, have also been shown to improve dietary quality among the food insecure and improve their cardiovascular outcomes [95,97,98]. Increasing access to – and incentives to buy – healthy foods at the local level can thus help address disparities in FI, dietary quality, and CVD (Fig. 3) [64,69].
4.4. Healthcare systems and physicians
A review of FI screening programs based in US hospitals, clinics, and health centers found that most programs received funding from multiple short-term sources, with several program managers expressing concern about long-term sustainability [100]. FI screening is also not yet standard clinical practice despite evidence indicating food-insecure patients appreciate being screened and referred to resources [101]. Analysis of Food for Families (a hospital-run program that connects food-insecure patients with SNAP, WIC, and food pantries) found that participants experienced moderately improved blood pressure, suggesting an association between referral to aid programs and better cardiovascular health [102]. However, only 11% of the clinic's pregnant patients (seen over a span of two years) were referred to the program, suggesting a need for more robust FI screening and referral to relevant resources [102].
An important component of referral and education by providers is to improve patient understanding of healthy foods and encourage them to consume more fruits and vegetables. Despite the well-documented impact of diet and food access on cardiovascular health, studies suggest nutrition is not sufficiently integrated into medical school curricula, with many medical students reporting inadequate nutrition knowledge or scoring poorly on nutrition-related tests [41,103]. Physicians have also reported uncertainty in how to navigate conversations following a positive FI screening, revealing the importance of properly educating care providers on nutrition and food access programs [104]. In 2015, educational sessions conducted at three residency programs and one medical school were found to improve students’ knowledge and willingness to discuss FI with patients, while follow-up surveys revealed increased discussion of FI and referral to food resources during clinical visits [105]. These improvements indicate incorporating nutrition into medical school curricula and hospital systems can help address FI at the clinical level. Training nurses, pharmacists, and other professionals to provide nutritional counseling and connect patients with relevant resources has also been proposed as a way to address rising levels of FI and obesity among patients [106].
Intervention frameworks such as SEARCH (Table 3), may further help physicians appropriately screen and treat patients experiencing FI. Implementing patient navigation teams can help patients apply for SNAP, WIC, and other benefits (Fig. 3) [100,101]. Some clinics also provide medically-tailored meals and fruit and vegetable “prescriptions” (usually vouchers or coupons to be redeemed at farmers markets or food pantries), which can further help patients obtain nutritious foods that suit their treatment and improve their cardiovascular risk profile [100]. Registered dietitians and nutrition and dietetics technicians, registered can further aid in these efforts through education, advocacy, and nutrition counseling, tailored to patient needs [107].
Additionally, providers can refer patients to community resources that address other barriers to food access, such as transportation and education (Fig. 3) [100]. These strong partnerships between health systems and community organizations may facilitate access to key food resources for individuals and communities most in need (Fig. 3) [108]. Reductions in the financial burden of care may also prove useful, as controlling drug prices and reducing out-of-pocket costs could lower patients’ risk of becoming food insecure. However, further study is needed to verify whether such changes in the healthcare system would indeed alleviate the burden of FI among CVD patients.
5. Conclusions
FI prevalence has been rising nationwide, being especially prominent among low-income households with children, racial/ethnic minorities, and single mothers [2]. Notably, FI is associated with various cardiovascular risk factors – such as hypertension, dyslipidemia, diabetes, obesity, physical inactivity, and smoking – CVD, and cardiovascular mortality. FI is more common among ASCVD patients than in the general population, suggesting a possible bidirectional relationship between FI and CVD [11,41]. This association is likely due to FI's negative impact on behavioral risk factors, stress levels, and nutritional quality, as well as the financial burden of CVD treatment that may increase risk of being food insecure (Fig. 2). Given the recent increase in FI prevalence in the US, the burden of CVD is likely to grow nationally, particularly among sociodemographic subgroups which are more vulnerable to FI's impact on cardiovascular health. To improve access to healthy foods and attenuate increased cardiovascular risk, federal aid programs such as SNAP and WIC should provide subsidies and other financial incentives to purchase fruits and vegetables. These actions would require greater investment from the federal government to fund and increase access to such initiatives. Partnerships among public assistance programs, healthcare systems, and community organizations can further improve food access and patients’ understanding of nutrition. It is also critical to conduct more longitudinal population-wide studies to evaluate the causal relationship between FI and CVD as well as the efficacy of aforementioned interventions. Future collaboration involving researchers, policy makers, and clinicians may thus establish the foundation to improving access to nutritious food and, ultimately, cardiovascular health.
CRediT authorship contribution statement
Ryan Chang: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. Zulqarnain Javed: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. Mohamad Taha: Writing – review & editing. Tamer Yahya: Visualization. Javier Valero-Elizondo: Writing – review & editing. Eric J. Brandt: Writing – review & editing. Miguel Cainzos-Achirica: Writing – review & editing. Shiwani Mahajan: Writing – review & editing. Hyeon-Ju Ali: Writing – review & editing. Khurram Nasir: Supervision.
Declaration of Conflicts Interest
Dr. Nasir is on the advisory board of Amgen and Novartis Medicine Company, and his research is partly supported by the Jerold B. Katz Academy of Translational Research. No other conflicts of interest relevant to the content of this manuscript were reported by the authors. There was also no funding received for this review.
Contributor Information
Ryan Chang, Email: ryanpchang@wustl.edu.
Zulqarnain Javed, Email: zjaved@houstonmethodist.org.
Mohamad Taha, Email: mbtaha@houstonmethodist.org.
Tamer Yahya, Email: tyahya@houstonmethodist.org.
Javier Valero-Elizondo, Email: jvalero@houstonmethodist.org.
Eric J. Brandt, Email: ebrandt@med.umich.edu.
Miguel Cainzos-Achirica, Email: mcainzosachirica@houstonmethodist.org.
Shiwani Mahajan, Email: shiwani.mahajan@yale.edu.
Hyeon-Ju Ali, Email: hryooali@houstonmethodist.org.
Khurram Nasir, Email: knasir@houstonmethodist.org.
References
- 1.Definitions of Food Security. USDA Economic Research Service. Updated September 9, 2020. Accessed June 24, 2021, 2021. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx
- 2.Key Statistics & Graphics. USDA Economic Research Service. Updated September 9, 2020. Accessed June 25, 2021, https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics/
- 3.Virani S.S., Alonso A., Aparicio H.J., et al. Heart disease and stroke statistics—2021 update. Circulation. 2021;143(8):e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 4.Deaths and Mortality. Centers for disease control and prevention. Updated April 9, 2021. Accessed July 7, 2021, https://www.cdc.gov/nchs/fastats/deaths.htm
- 5.Abdalla S.M., Yu S., Galea S. Trends in cardiovascular disease prevalence by income level in the United States. JAMA Netw Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.18150. Sep 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clark A.M., DesMeules M., Luo W., Duncan A.S., Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712–722. doi: 10.1038/nrcardio.2009.163. Nov. [DOI] [PubMed] [Google Scholar]
- 7.Havranek E.P., Mujahid M.S., Barr D.A., et al. Social determinants of risk and outcomes for cardiovascular disease. Circulation. 2015;132(9):873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 8.Leung C.W., Tester J.M. The association between food insecurity and diet quality varies by Race/Ethnicity: an analysis of national health and nutrition examination survey 2011-2014 results. J Acad Nutr Diet. 2019;119(10):1676–1686. doi: 10.1016/j.jand.2018.10.011. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Life's Simple 7. American heart association. Accessed August 25, 2021, https://www.heart.org/en/professional/workplace-health/lifes-simple-7
- 10.Berkowitz S.A., Berkowitz T.S.Z., Meigs J.B., Wexler D.J. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005-2012. PLoS ONE. 2017;12(6) doi: 10.1371/journal.pone.0179172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahajan S., Grandhi G.R., Valero-Elizondo J., et al. Scope and social determinants of food insecurity among adults with atherosclerotic cardiovascular disease in the United States. J Am Heart Assoc. 2021;0(0) doi: 10.1161/JAHA.120.020028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khera R., Valero-Elizondo J., Nasir K. Financial toxicity in atherosclerotic cardiovascular disease in the united states: current state and future directions. J Am Heart Assoc. 2020;9(19) doi: 10.1161/jaha.120.017793. Oct 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Impact of the Coronavirus on Food Insecurity in 2020 & 2021. Feeding America. Updated March 9, 2021. Accessed June 24, 2021, 2021. https://www.feedingamerica.org/sites/default/files/2021-03/National%20Projections%20Brief_3.9.2021_0.pdf
- 14.Nishiga M., Wang D.W., Han Y., Lewis D.B., Wu J.C. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17(9):543–558. doi: 10.1038/s41569-020-0413-9. 2020/09/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Measurement. USDA Economic Research Service. Updated December 18, 2020. Accessed June 24, 2021, 2021. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/measurement.aspx
- 16.Arteaga I., Wilde P. Measuring food security in the U.S. for 25 years: history, methods, findings, and opportunities. Tufts University. Updated January 27, 2021. Accessed August 15, 2021, https://sites.tufts.edu/foodsec25/files/2021/01/SettingStage_v11.pdf
- 17.Gulliford M.C., Nunes C., Rocke B. The 18 household food security survey items provide valid food security classifications for adults and children in the Caribbean. BMC Public Health. 2006;6(1):26. doi: 10.1186/1471-2458-6-26. 2006/02/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rafiei M., Nord M., Sadeghizadeh A., Entezari M.H. Assessing the internal validity of a household survey-based food security measure adapted for use in Iran. Nutr J. 2009;8 doi: 10.1186/1475-2891-8-28. 28-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gattu R.K., Paik G., Wang Y., Ray P., Lichenstein R., Black M.M. The Hunger vital sign identifies household food insecurity among children in emergency departments and primary care. Children. 2019;6(10) doi: 10.3390/children6100107. (Basel)Oct 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schanzenbach D., Pitts A. How much has food insecurity risen? evidence from the census household pulse survey institute for policy research rapid research report. Accessed June 24, 2021, 2021. https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-10-june-2020.pdf
- 21.Smith M.D., Coleman-Jensen A. Food insecurity, acculturation and diagnosis of CHD and related health outcomes among immigrant adults in the USA. Public Health Nutr. 2020;23(3):416–431. doi: 10.1017/S1368980019001952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leung C.W., Kullgren J.T., Malani P.N., et al. Food insecurity is associated with multiple chronic conditions and physical health status among older US adults. Prev Med Rep. 2020;20 doi: 10.1016/j.pmedr.2020.101211. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mui Y., Headrick G., Raja S., Palmer A., Ehsani J., Pollack Porter K. Acquisition, mobility and food insecurity: integrated food systems opportunities across urbanicity levels highlighted by COVID-19. Public Health Nutr. 2021:1–5. doi: 10.1017/S1368980021002755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ERS Charts of Note. USDA economic research service. updated May 27, 2021. Accessed July 21, 2021, https://www.ers.usda.gov/data-products/charts-of-note/charts-of-note/?topicId=14875
- 25.Waxman E., Gupta P. Food Insecurity fell nearly 30 percent between spring 2020 and 2021. 2021. May 2021. Accessed July 21, 2021. https://www.urban.org/sites/default/files/publication/104286/food-insecurity-fell-nearly-30-percent-between-spring-2020-and-2021-pdf_0.pdf
- 26.Gregory C., Coleman-Jensen A. Food insecurity, chronic disease, and health among working-age adults. 2017.
- 27.Vercammen K.A., Moran A.J., McClain A.C., Thorndike A.N., Fulay A.P., Rimm E.B. Food security and 10-year cardiovascular disease risk among U.S. adults. Am J Prev Med. 2019;56(5):689–697. doi: 10.1016/j.amepre.2018.11.016. 05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang S.Y., Eberly L.A., Roberto C.A., Venkataramani A.S., Groeneveld P.W., Khatana S.A.M. Food insecurity and cardiovascular mortality for nonelderly adults in the United States from 2011 to 2017. Circ Cardiovasc Qual Outcomes. 2021;14(1) doi: 10.1161/CIRCOUTCOMES.120.007473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun Y., Liu B., Rong S., et al. Food Insecurity is associated with cardiovascular and all-cause mortality among adults in the United States. J Am Heart Assoc. 2020;9(19) doi: 10.1161/jaha.119.014629. Oct 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valero-Elizondo J., Khera R., Saxena A., et al. Financial hardship from medical bills among nonelderly U.S. adults with atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2019;73(6):727–732. doi: 10.1016/j.jacc.2018.12.004. Feb 19. [DOI] [PubMed] [Google Scholar]
- 31.Khavjou O., Phelps D., Leib A. Projections of cardiovascular disease prevalence and costs: 2015–2035 2016. November 2016. https://www.heart.org/idc/groups/heart-public/@wcm/@adv/documents/downloadable/ucm_491513.pdf
- 32.Seligman H.K., Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6–9. doi: 10.1056/NEJMp1000072. Jul. [DOI] [PubMed] [Google Scholar]
- 33.Leung C.W., Epel E.S., Ritchie L.D., Crawford P.B., Laraia B.A. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114(12):1943–1953. doi: 10.1016/j.jand.2014.06.353. Dece2. [DOI] [PubMed] [Google Scholar]
- 34.Iqbal R., Dehghan M., Mente A., et al. Associations of unprocessed and processed meat intake with mortality and cardiovascular disease in 21 countries [Prospective Urban Rural Epidemiology (PURE) Study]: a prospective cohort study. Am J Clin Nutr. 2021 doi: 10.1093/ajcn/nqaa448. Mar 31. [DOI] [PubMed] [Google Scholar]
- 35.Pacheco L.S., Lacey J.V., Martinez M.E., et al. Sugar-sweetened beverage intake and cardiovascular disease risk in the California teachers study. J Am Heart Assoc. 2020;9(10) doi: 10.1161/jaha.119.014883. May 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pan L., Sherry B., Njai R., Blanck H.M. Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Diet. 2012;112(9):1403–1409. doi: 10.1016/j.jand.2012.06.011. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seligman H.K., Bindman A.B., Vittinghoff E., Kanaya A.M., Kushel M.B. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22(7):1018–1023. doi: 10.1007/s11606-007-0192-6. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scherer P.E., Hill J.A. Obesity, diabetes, and cardiovascular diseases: a compendium. Circ Res. 2016,;118(11):1703–1705. doi: 10.1161/circresaha.116.308999. May 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palakshappa D., Ip E.H., Berkowitz S.A., et al. Pathways by which food insecurity is associated with atherosclerotic cardiovascular disease risk. J Am Heart Assoc. 2021;0(0) doi: 10.1161/JAHA.121.021901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mendy V.L., Vargas R., Cannon-Smith G., Payton M., Enkhmaa B., Zhang L. Food Insecurity and Cardiovascular Disease Risk Factors among Mississippi Adults. Int J Environ Res Public Health. 2018;15(9) doi: 10.3390/ijerph15092016. Sep 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu Y., Eicher-Miller H.A. Food Insecurity and cardiovascular disease risk. Curr Atheroscler Rep. 2021;23(6):24. doi: 10.1007/s11883-021-00923-6. Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tayie F.A., Zizza C.A. Food insecurity and dyslipidemia among adults in the United States. Prev Med. 2009;48(5):480–485. doi: 10.1016/j.ypmed.2009.03.003. May. [DOI] [PubMed] [Google Scholar]
- 43.Vos M.B., Kaar J.L., Welsh J.A., et al. Added sugars and cardiovascular disease risk in children: a scientific statement from the American heart association. Circulation. 2017;135(19):e1017–e1034. doi: 10.1161/CIR.0000000000000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaikkonen J.E., Mikkilä V., Magnussen C.G., Juonala M., Viikari J.S., Raitakari O.T. Does childhood nutrition influence adult cardiovascular disease risk?–insights from the young finns Study. Ann Med. 2013;45(2):120–128. doi: 10.3109/07853890.2012.671537. Mar. [DOI] [PubMed] [Google Scholar]
- 45.Sattler E.L.P., Bhargava V. Food insecurity and cardiovascular risk factors in U.S. adolescents. J Appl Res Child. 2015;6(2) [PMC free article] [PubMed] [Google Scholar]
- 46.Tirosh A., Shai I., Afek A., et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011;364(14):1315–1325. doi: 10.1056/NEJMoa1006992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Olson C.M., Bove C.F., Miller E.O. Growing up poor: long-term implications for eating patterns and body weight. Appetite. 2007;49(1):198–207. doi: 10.1016/j.appet.2007.01.012. Jul. [DOI] [PubMed] [Google Scholar]
- 48.Lucini D., Norbiato G., Clerici M., Pagani M. Hemodynamic and autonomic adjustments to real life stress conditions in humans. Hypertension. 2002;39(1):184–188. doi: 10.1161/hy0102.100784. Jan. [DOI] [PubMed] [Google Scholar]
- 49.Dar T., Radfar A., Abohashem S., Pitman R.K., Tawakol A., Osborne M.T. Psychosocial stress and cardiovascular disease. Curr Treat Opt Cardiovasc Med. 26 2019;21(5):23. doi: 10.1007/s11936-019-0724-5. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lennie T.A., Andreae C., Rayens M.K., et al. Micronutrient deficiency independently predicts time to event in patients with heart failure. J Am Heart Assoc. 2018;7(17) doi: 10.1161/JAHA.117.007251. 2018/09/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sciatti E., Lombardi C., Ravera A., et al. Nutritional deficiency in patients with heart failure. Nutrients. 2016;8(7) doi: 10.3390/nu8070442. Jul 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brenner B.M., Chertow G.M. Congenital oligonephropathy: an inborn cause of adult hypertension and progressive renal injury? Curr Opin Nephrol Hypertens. 1993;2(5):691–695. Sep. [PubMed] [Google Scholar]
- 53.Olsen J.David. Barker (1938–2013) – a giant in reproductive epidemiology. Acta Obstet Gynecol Scand. 2014;93(11):1077–1080. doi: 10.1111/aogs.12378. [DOI] [PubMed] [Google Scholar]
- 54.Ordovás J.M., Smith C.E. Epigenetics and cardiovascular disease. Nat Rev Cardiol. 2010;7(9):510–519. doi: 10.1038/nrcardio.2010.104. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brown A.G.M., Esposito L.E., Fisher R.A., Nicastro H.L., Tabor D.C., Walker J.R. Food insecurity and obesity: research gaps, opportunities, and challenges. Transl Behav Med. 2019;9(5):980–987. doi: 10.1093/tbm/ibz117. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nichols G.A., Bell T.J., Pedula K.L., O'Keeffe-Rosetti M. Medical care costs among patients with established cardiovascular disease. Am J Manag Care. 2010;16(3):e86–e93. Mar. [PubMed] [Google Scholar]
- 57.Savira F., Wang B.H., Kompa A.R., et al. The impact of coronary heart disease prevention on work productivity: a 10-year analysis. Eur J Prev Cardiol. 2021;28(4):418–425. doi: 10.1093/eurjpc/zwaa037. May. [DOI] [PubMed] [Google Scholar]
- 58.Ford E.S. Food security and cardiovascular disease risk among adults in the United States: findings from the national health and nutrition examination survey, 2003-2008. Prev Chronic Dis. 2013;10:E202. doi: 10.5888/pcd10.130244. Dec 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Drewnowski A., Shultz J.M. Impact of aging on eating behaviors, food choices, nutrition, and health status. J Nutr Health Aging. 2001;5(2):75–79. [PubMed] [Google Scholar]
- 60.Rodgers J.L., Jones J., Bolleddu S.I., et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis. 2019;6(2) doi: 10.3390/jcdd6020019. Apr 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dinour L.M., Bergen D., Yeh M.C. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107(11):1952–1961. doi: 10.1016/j.jada.2007.08.006. Nov. [DOI] [PubMed] [Google Scholar]
- 62.EUGenMed T., Group C.C.S., Regitz-Zagrosek V., et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. 2015;37(1):24–34. doi: 10.1093/eurheartj/ehv598. [DOI] [PubMed] [Google Scholar]
- 63.Lopez L., Hart L.H., Katz M.H. Racial and Ethnic Health Disparities Related to COVID-19. JAMA. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. 02. [DOI] [PubMed] [Google Scholar]
- 64.Muncan B. Cardiovascular disease in racial/ethnic minority populations: illness burden and overview of community-based interventions. Public Health Rev. 2018;39:32. doi: 10.1186/s40985-018-0109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nayak A., Hicks A.J., Morris A.A. Understanding the Complexity of Heart Failure Risk and Treatment in Black Patients. Circ Heart Fail. 2020;13(8) doi: 10.1161/CIRCHEARTFAILURE.120.007264. 2020/08/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cooksey Stowers K., Jiang Q., Atoloye A., Lucan S., Gans K. Racial differences in perceived food swamp and food desert exposure and disparities in self-reported dietary habits. Int J Environ Res Public Health. 2020;17(19) doi: 10.3390/ijerph17197143. Sep 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Leung C.W., Tester J.M. The association between food insecurity and diet quality varies by Race/Ethnicity: an analysis of national health and nutrition examination survey 2011-2014 results. J Acad Nutr Diet. 2021;119(10):1676–1686. doi: 10.1016/j.jand.2018.10.011. 2019/10/01/2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ohri-Vachaspati P., DeWeese R.S., Acciai F., et al. Healthy food access in low-income high-minority communities: a longitudinal assessment-2009-2017. Int J Environ Res Public Health. Jul 3 2019;16(13) doi: 10.3390/ijerph16132354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bower K.M., Thorpe R.J., Rohde C., Gaskin D.J. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med. 2014;58:33–39. doi: 10.1016/j.ypmed.2013.10.010. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Adams E.J., Grummer-Strawn L., Chavez G. Food Insecurity is associated with increased risk of obesity in California women. J Nutr. 2003;133(4):1070–1074. doi: 10.1093/jn/133.4.1070. [DOI] [PubMed] [Google Scholar]
- 71.Hanson K.L., Sobal J., Frongillo E.A. Gender and marital status clarify associations between food insecurity and body weight. J Nutr. 2007;137(6):1460–1465. doi: 10.1093/jn/137.6.1460. [DOI] [PubMed] [Google Scholar]
- 72.Olson C.M. Food insecurity in women: a recipe for unhealthy trade-offs. Top Clin Nutr. 2005;20(4):321–328. [Google Scholar]
- 73.Martin M.A., Lippert A.M. Feeding her children, but risking her health: the intersection of gender, household food insecurity and obesity. Soc Sci Med. 2012;74(11):1754–1764. doi: 10.1016/j.socscimed.2011.11.013. 2012/06/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Supplemental nutrition assistance program (SNAP). USDA Food and Nutrition Service. Accessed June 24, 2021, https://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program
- 75.Ratcliffe C., McKernan S.M., Zhang S. How much does the supplemental nutrition assistance program reduce food insecurity? Am J Agric Econ. 2011;93(4):1082–1098. doi: 10.1093/ajae/aar026. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.AGaPD Christian. Does SNAP improve your health? Food Policy. 2015;50:11–19. doi: 10.1016/j.foodpol.2014.09.010. [DOI] [Google Scholar]
- 77.Hoynes H., Schanzenbach D.W., Almond D. Long-run impacts of childhood access to the safety net. Am Econ Rev. 2016;106(4):903–934. doi: 10.1257/aer.20130375. [DOI] [Google Scholar]
- 78.Oliveira V., Prell M., Tiehen L., Smallwood D.Design issues in USDA'S supplemental nutrition assistance program: looking ahead by looking back. 2018. doi: 10.22004/ag.econ.276253. [DOI]
- 79.SNAP Data Tables. USDA food and nutrition service updated August 13, 2021. Accessed September 12, 2021, https://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap
- 80.The special supplemental nutrition program for women, infants and children (WIC Program) fact sheet. USDA food and nutrition service. Accessed July 13, 2021, https://fns-prod.azureedge.net/sites/default/files/wic/wic-fact-sheet.pdf
- 81.The Emergency Food Assistance Program Fact Sheet. USDA Food and nutrition service. Updated January 6, 2020. Accessed July 13, 2021, https://fns-prod.azureedge.net/sites/default/files/resource-files/tefap-program-fact-sheet-2019_1.6.20.pdf
- 82.The National School Lunch Program Fact Sheet. USDA Food and Nutrition Service. Updated November 2017. Accessed July 13, 2021, https://fns-prod.azureedge.net/sites/default/files/resource-files/NSLPFactSheet.pdf
- 83.Fernald L.C.H., Gosliner W. Alternatives to SNAP: global approaches to addressing childhood poverty and food insecurity. Am J Public Health. 2019;109(12):1668–1677. doi: 10.2105/ajph.2019.305365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Choi S.E., Seligman H., Basu S. Cost effectiveness of subsidizing fruit and vegetable purchases through the supplemental nutrition assistance program. Am J Prev Med. 2017;52(5):e147–e155. doi: 10.1016/j.amepre.2016.12.013. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jackson M.I. Early childhood WIC participation, cognitive development and academic achievement. Soc Sci Med. 2015;126:145–153. doi: 10.1016/j.socscimed.2014.12.018. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Monthly Data - National Level. In: 37WIC_Monthly-6.pdf, editor.: USDA Food and nutrition service; 2021.
- 87.Di Noia J., Schultz S., Monica D. Recruitment and retention of WIC participants in a longitudinal dietary intervention trial. Contemp Clin Trials Commun. 2019;16 doi: 10.1016/j.conctc.2019.100438. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Powell L., Amsbary J., Xin H. Stigma as a communication barrier for participation in the federal government's women, infants, and children program. Qual Res Rep Commun. 2015;16(1):75–85. doi: 10.1080/17459435.2015.1086423. 2015/01/01. [DOI] [Google Scholar]
- 89.Zimmer M.C., Beaird J., Steeves E.T.A. WIC participants’ Perspectives about online ordering and technology in the WIC program. J Nutr Educ Behav. 2021;53(7):602–607. doi: 10.1016/j.jneb.2020.10.001. 2021/07/01/2021. [DOI] [PubMed] [Google Scholar]
- 90.Alaimo K. Community Responses to Food Insecurity and Hunger. presented at: Workshop on Research Gaps and Opportunities on the Causes and Consequences of Child Hunger May 29, 2013 2013; Washington, DC. https://sites.nationalacademies.org/cs/groups/dbassesite/documents/webpage/dbasse_084303.pdf
- 91.Hayashi T., Farrell M.A., Chaput L.A., Rocha D.A., Hernandez M. Lifestyle intervention, behavioral changes, and improvement in cardiovascular risk profiles in the California WISEWOMAN project. J Womens Health. 2010;19(6):1129–1138. doi: 10.1089/jwh.2009.1631. (Larchmt)Jun. [DOI] [PubMed] [Google Scholar]
- 92.Dubowitz T., Zenk S.N., Ghosh-Dastidar B., et al. Healthy food access for urban food desert residents: examination of the food environment, food purchasing practices, diet and BMI. Public Health Nutr. 2015;18(12):2220–2230. doi: 10.1017/s1368980014002742. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bonanno A., Li J. Food insecurity and food access in U.S. metropolitan areas. Applied Economic Perspectives and Policy. 2015/06/01 2015;37(2):177–204. 10.1093/aepp/ppu032
- 94.Allcott H., Diamond R., Dubé J.P., Handbury J., Rahkovsky I., Schnell M. Food deserts and the causes of nutritional inequality*. Q J Econ. 2019;134(4):1793–1844. doi: 10.1093/qje/qjz015. [DOI] [Google Scholar]
- 95.An R. Effectiveness of subsidies in promoting healthy food purchases and consumption: a review of field experiments. Public Health Nutr. 2013;16(7):1215–1228. doi: 10.1017/s1368980012004715. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lyonnais M.J., Rafferty A.P., Jilcott Pitts S., Blanchard R.J., Kaur A.P. Examining Shopping patterns, use of food-related resources, and proposed solutions to improve healthy food access among food insecure and food secure eastern north carolina residents. Int J Environ Res Public Health. 2020,;17(10) doi: 10.3390/ijerph17103361. May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Alissa E.M., Ferns G.A. Dietary fruits and vegetables and cardiovascular diseases risk. Crit Rev Food Sci Nutr. 2017;57(9):1950–1962. doi: 10.1080/10408398.2015.1040487. Jun 13. [DOI] [PubMed] [Google Scholar]
- 98.Devitt J. What really happens when a grocery store opens in a ‘Food Desert’? New York University. Updated December 10, 2019. Accessed July 19, 2021, https://www.nyu.edu/about/news-publications/news/2019/december/what-really-happens-when-a-grocery-store-opens-in-a–food-desert.html
- 99.Shahid S.M., Bishop K.S. Comprehensive approaches to improving nutrition: future prospects. Nutrients. 2019;11(8) doi: 10.3390/nu11081760. Jul 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lundeen E.A., Siegel K.R., Calhoun H., et al. Clinical-community partnerships to identify patients with food insecurity and address food needs. Prev Chronic Dis. 2017;14:E113. doi: 10.5888/pcd14.170343. Nov 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kopparapu A., Sketas G., Swindle T. Food insecurity in primary care: patient perception and preferences. Fam Med. 2020;52(3):202–205. doi: 10.22454/FamMed.2020.964431. Mar. [DOI] [PubMed] [Google Scholar]
- 102.Morales M.E., Epstein M.H., Marable D.E., Oo S.A., Berkowitz S.A. Food insecurity and cardiovascular health in pregnant women: results from the food for families program, Chelsea, Massachusetts, 2013-2015. Prev Chronic Dis. 2016;13:E152. doi: 10.5888/pcd13.160212. Nov 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Crowley J., Ball L., Hiddink G.J. Nutrition in medical education: a systematic review. Lancet Planet Health. 2019;3(9):e379–e389. doi: 10.1016/S2542-5196(19)30171-8. 09. [DOI] [PubMed] [Google Scholar]
- 104.Barnidge E., LaBarge G., Krupsky K., Arthur J. Screening for food insecurity in pediatric clinical settings: opportunities and barriers. J Commun Health. 2017;42(1):51–57. doi: 10.1007/s10900-016-0229-z. Feb. [DOI] [PubMed] [Google Scholar]
- 105.Smith S., Malinak D., Chang J., Schultz A., Brownell K. Addressing food insecurity in family medicine and medical education. Fam Med. 2017;49(10):765–771. Nov. [PubMed] [Google Scholar]
- 106.DiMaria-Ghalili R.A., Mirtallo J.M., Tobin B.W., Hark L., Van Horn L., Palmer C.A. Challenges and opportunities for nutrition education and training in the health care professions: intraprofessional and interprofessional call to action. Am J Clin Nutr. 2014;99(5 Suppl):1184s–1193s. doi: 10.3945/ajcn.113.073536. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Holben D.H., Marshall M.B. Position of the academy of nutrition and dietetics: food insecurity in the United States. J Acad Nutr Diet. 2017;117(12):1991–2002. doi: 10.1016/j.jand.2017.09.027. Dec. [DOI] [PubMed] [Google Scholar]
- 108.Loskutova N.Y., Tsai A.G., Fisher E.B., et al. Patient navigators connecting patients to community resources to improve diabetes outcomes. J Am Board Fam Med. Jan-Feb 2016;29(1):78–89. doi: 10.3122/jabfm.2016.01.150048. [DOI] [PubMed] [Google Scholar]
- 109.Patil S.P., Craven K., Kolasa K. Food insecurity: how you can help your patients. Am Fam Phys. 2018;3:143–145. [PubMed] [Google Scholar]